ACL replacement using a decellularised xenograft tendon
-
1
UCL, Institute of Orthopaedicsand Musculoskeletal Science, United Kingdom
-
2
Queen Mary University of London, School of Engineering and Materials, United Kingdom
Introduction: Biodegradable scaffolds do not initially possess the mechanical properties necessary for reconstruction and the use of naturally derived scaffolds and other alternative materials for ACL reconstruction have been considered [1]. Decellularised scaffold derived from tendon and containing minimal residual cellular material is an option for repair of the ACL. The aim of this study is to investigate the biological compatibility, remodeling and function of a decellularised porcine tendon to replace the ACL in an ovine model of ACL replacement.
Materials and Methods: Following resection of the right ACL in a sheep, double bundles of the decellularised porcine tendon were threaded through the tibial tunnel in 12 animals. Porcine superficial digital flexor tendons were decellularised[2] and then chemically cross-linked[3]. In 6 of these animals an EndobuttonTM (Smith and Nephew) suspension device was used and in the others the tendon was suspended from a polymeric device (StratisTM, Covidien). The double bundle of the tendon was passed through the tibial tunnel and was fixed in place using an Arthrex soft screw TM. The animals underwent force-plate analysis pre-operatively, at six and 12 weeks after operation to measure the ground reaction force. Joint stiffness and function (extension, flexion and rotation) were evaluated at post mortem by measuring the range of flexion in both the operated and non-operated leg. Using a semi-quantitative scoring scheme, 2 independent observers scored the tendon for mid-joint tendon remodelling, fragmentation of the tendon and new ligamentous tissue. Within the bone tunnels a-cellular calcification, together with new bone formation was semi- quantitatively scored. In addition, we assessed the presence of Sharpey’s-like fibres and tendon remodelling.
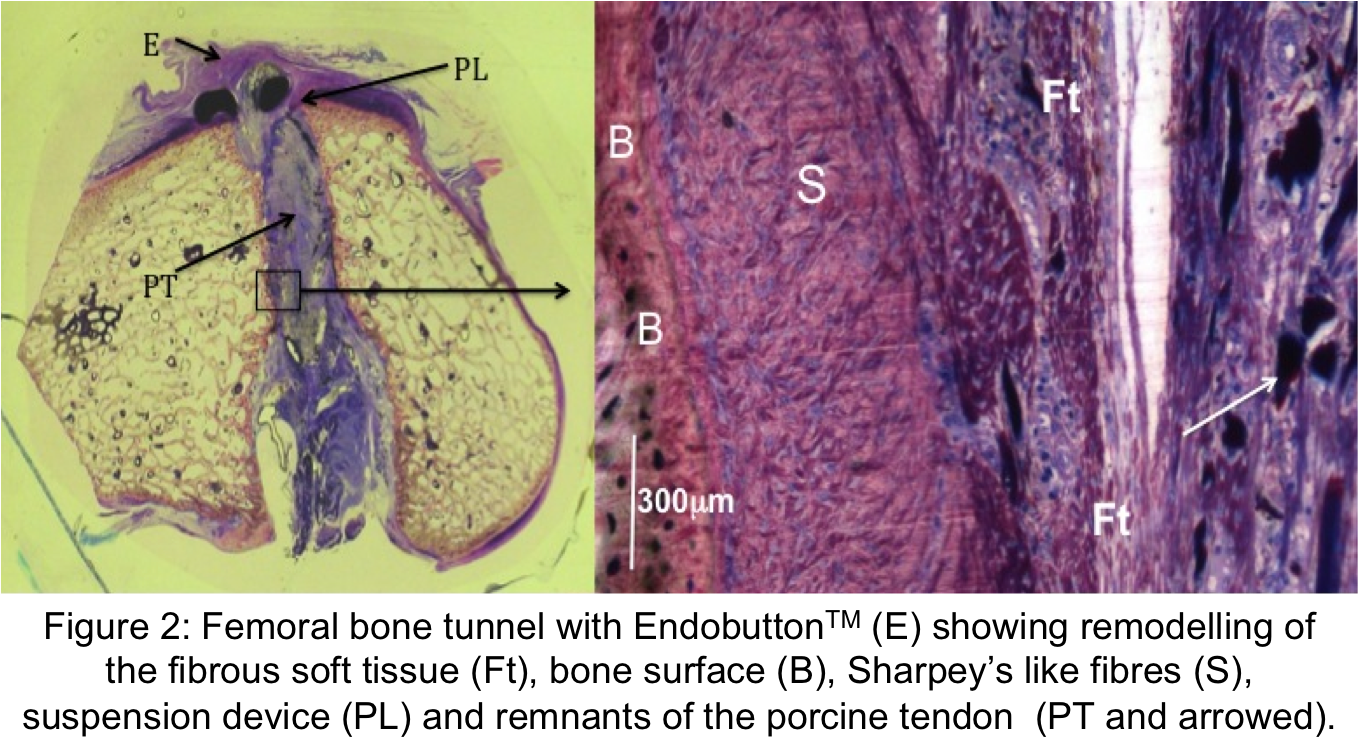
Results: The postoperative ground reaction forces (GRF) at 5, 8 and 11 weeks were lower when compared to pre-operative data. GRF in the operated leg of the Endobutton cohort was significantly lower at 5 weeks (p=< 0.005) and 8 weeks (p=<0.05) compared with the StratisTM device, but was statistically similar at 11 weeks with average GRFs of 92% and 85% respectively. There was no significant difference in joint stiffness between operated and contra-lateral stifle joints at 12 weeks. In all but 2 animals the original double bundle had remodelled into a single ligament. Remodelling and fragmentation of the porcine tendon was accompanied by cellular invasion and collagen formation. The semi quantitative scores showed that there was no significance difference in the level of remodelling between the two suspension devices (figure 1). In all cases greater tissue formation occurred around the margins of the porcine tendon identified by more finely crimped collagen, vascularisation and a larger number of cells. To a lesser extent this also occurred between the bundles of the porcine tendon in the central region. A synovial membrane surrounded the tendon where it crossed the joint space. The semi quantitative scores showed that there was no significance difference in the level of remodelling between the two suspension devices in the femoral bone tunnels (figure 1). Calcification of the tendon within the femoral bone tunnels was by an a-cellular process, and in other regions, associated with the fragmented tendon a more cellular calcification process occurred, with lines of osteoblast-like cells identified on the surface of the tendon fibres. Intramembranous bone formation and tunnel widening was seen with the EndobuttonTM. In all bone tunnels Sharpey’s-like fibres anchoring the soft tissue with the bone surface was seen (figure 2).
Discussion: This study shows that a decellularised xenograft may be used in an ovine model to repair the ACL where the porcine tendon remodelled into functional tissue. The rate of this process was not sensitive to the femoral suspension device used, however, functional recovery was affected. Across the joint the tendon was remodelled with the formation of crimped collagen and a synovial membrane. In the bone tunnels the tendon remodelled and was replaced by newly formed bone anchored to the tunnel surface by Sharpey’s like fibres.

References:
[1] Tischer et al. Arch Orthop Trauma Surg. 2007 Nov;127(9):735-41. Jarman-Smith et al.
[2] Jarman-Smith et al. J Mater Sci Mater Med, 2004. 15(8): p. 925-32.
[3] Oliver et al. Br J Exp Pathol, 1972. 53(5): p. 540-9.
Keywords:
Regenerative Medicine,
Tissue Regeneration,
acellullar matrix
Conference:
10th World Biomaterials Congress, Montréal, Canada, 17 May - 22 May, 2016.
Presentation Type:
General Session Oral
Topic:
Biomaterials evaluation in animal models
Citation:
Blunn
G and
Hing
K
(2016). ACL replacement using a decellularised xenograft tendon.
Front. Bioeng. Biotechnol.
Conference Abstract:
10th World Biomaterials Congress.
doi: 10.3389/conf.FBIOE.2016.01.02088
Copyright:
The abstracts in this collection have not been subject to any Frontiers peer review or checks, and are not endorsed by Frontiers.
They are made available through the Frontiers publishing platform as a service to conference organizers and presenters.
The copyright in the individual abstracts is owned by the author of each abstract or his/her employer unless otherwise stated.
Each abstract, as well as the collection of abstracts, are published under a Creative Commons CC-BY 4.0 (attribution) licence (https://creativecommons.org/licenses/by/4.0/) and may thus be reproduced, translated, adapted and be the subject of derivative works provided the authors and Frontiers are attributed.
For Frontiers’ terms and conditions please see https://www.frontiersin.org/legal/terms-and-conditions.
Received:
27 Mar 2016;
Published Online:
30 Mar 2016.
*
Correspondence:
Dr. Gordon Blunn, UCL, Institute of Orthopaedicsand Musculoskeletal Science, London, United Kingdom, g.blunn@ucl.ac.uk
Dr. Karin Hing, Queen Mary University of London, School of Engineering and Materials, London, United Kingdom, k.a.hing@qmul.ac.uk