Introduction: Chronic wounds are characterized by an inadequate blood supply and revascularization is the mainstay for treatment of these patients. Different types of wound dressings are available to manage these affections, all of them with limited clinical success[1].
Ions have an important role in repair and regenerative processes in skin wounds[2]. Calcium in particular, has been reported to stimulate fibroblast proliferation, keratinocyte migration and improve angiogenesis[3].
The aim of this study was to develop a new calcium releasing biodegradable dressing based on the combination of Polylactic Acid (PLA) and Calcium Phosphate glass nanoparticles that promotes wound vascularization and healing.
Materials and Methods: Dressings consist in electrospun nanofibers of PLA with embedded glass soluble nanoparticles , synthesized by sol-gel method. Release of calcium was measured using a calcium quantification assay kit. Diabetic mice (C57BLKS/J) were ulcerated by clamping and then removing a pair of magnetic disks. PLA, PLAGlass dressings and commercially available wound dressings were applied to the wounds and changed daily. Appearance of the wound was recorded by digital imaging. Histological analysis was performed using Haematoxylin/Eosin and Masson´s trichrome staining. Cell proliferation and angiogenesis were assessed using antibodies against the proliferation marker Ki76 and CD31, respectively. Statistical analyses were performed using ANOVA and Tukey´s multiple comparison test.
Results: Treatment with PLAGlass dressings significantly reduced the wound area, compared with the PLA- or commercial dressings-treated wounds.
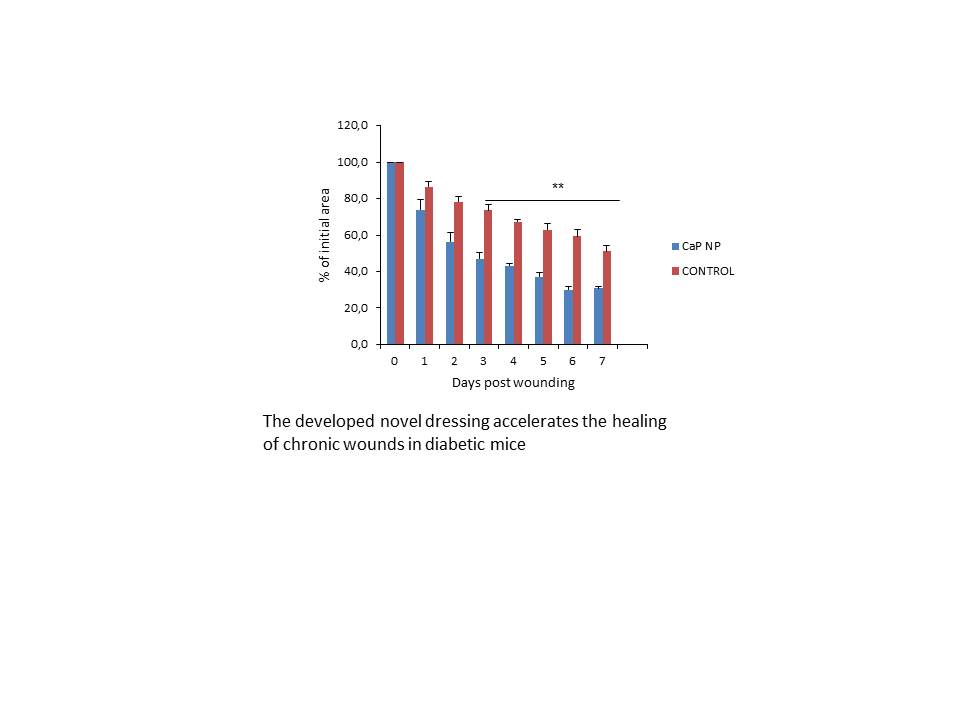
Eight days after implantation, the neoepithelial lengths in the PLAGlass-treated wounds were longer than those in the PLA- and commercial dressings-treated wounds. Similar amount of infiltrating inflammatory cells were observed in all treated groups. PLAGlass-treated wounds had more mature collagen development and higher number of positive Ki67 keratinocytes in the re-epithelized area compared with wounds treated with the other dressings. Higher number of CD31-positive structures was found in wounds treated with PLAGlass compared with the other treatments. Over a period of 24 hours, the calcium released by the PLAGlass dressings was ~ 5mM. There was no detectable calcium released by PLA-and commercial dressings.
Discussion and Conclusions: Our results indicate that PLAGlass dressings could efficiently promote the migration and proliferation of keratinocytes as well as collagen deposition and angiogenesis in chronic wounds. We propose this novel PLAGlass dressing as an efficient strategy to treat diabetic wound healing.
References:
[1] Beranoski S, Ayello EA. Adv Skin Wound Care 25, 87, 2012.
[2] Lansdown AB Wound Repair Regen 10, 271, 2002.
[3] Aguirre A, González A, Navarro M, Castaño O, Planell JA, Engel E. Eur Cell Mater. 24, 90, 2012.