Introduction: Decontamination of infected dental implants is considered to be a critical step in the successful treatment of peri-implantitis. No standard cleaning protocol has yet been defined and current treatments often fail the requirement to efficiently remove microbial biofilm and inhibit reinfection[1]. In this study, an in vitro assay is developed to dynamically observe biofilm regrowth after decontamination. Oxidative agents were systematically compared and a potentially more efficient cleaning procedure is presented.
Materials and Methods: In short, the bioluminescent strain S. epidermidis Xen43 was used as a model strain. Grit-blasted, acid-etched titanium coins were immersed in an inoculated TSB suspension and incubated at 37°C for 16 h to allow biofilm formation. Afterwards, contaminated samples were cleaned with either dH2O, 5% H2O2 or 5% H2O2 + 1 g/l TiO2 particles in the presence or absence of UV-A (n = 3). After an exposure time of 1 min, samples were placed in fresh media and incubated in a multi-mode plate reader. Luminescence was recorded every 15 min for 16 h. Additional samples were prepared for SEM images before, directly after and 16 h after decontamination.
Results and Discussion: After 16 h incubation, the entire implant surface was covered by a thick, mature biofilm. Rinsing with dH2O had no visible effect on the biofilm, while few remaining bacteria clusters were found for all oxidative treatments. None of the tested combinations could fully prevent biofilm regrowth 16 h after decontamination (Figure 1).
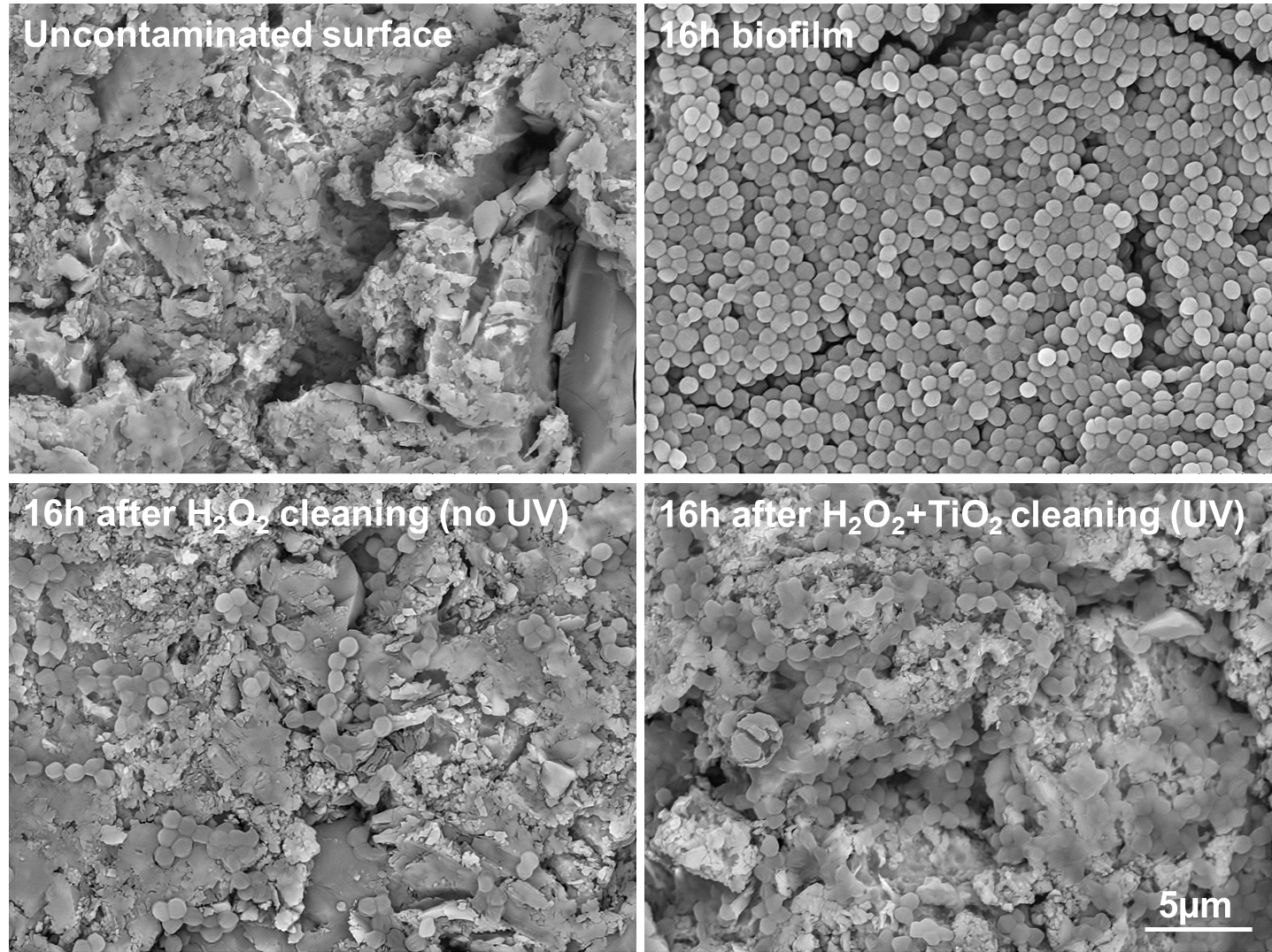
Figure 1: SEM images before and after cleaning
The summarised results for the luminescence assay are shown in Figure 2.
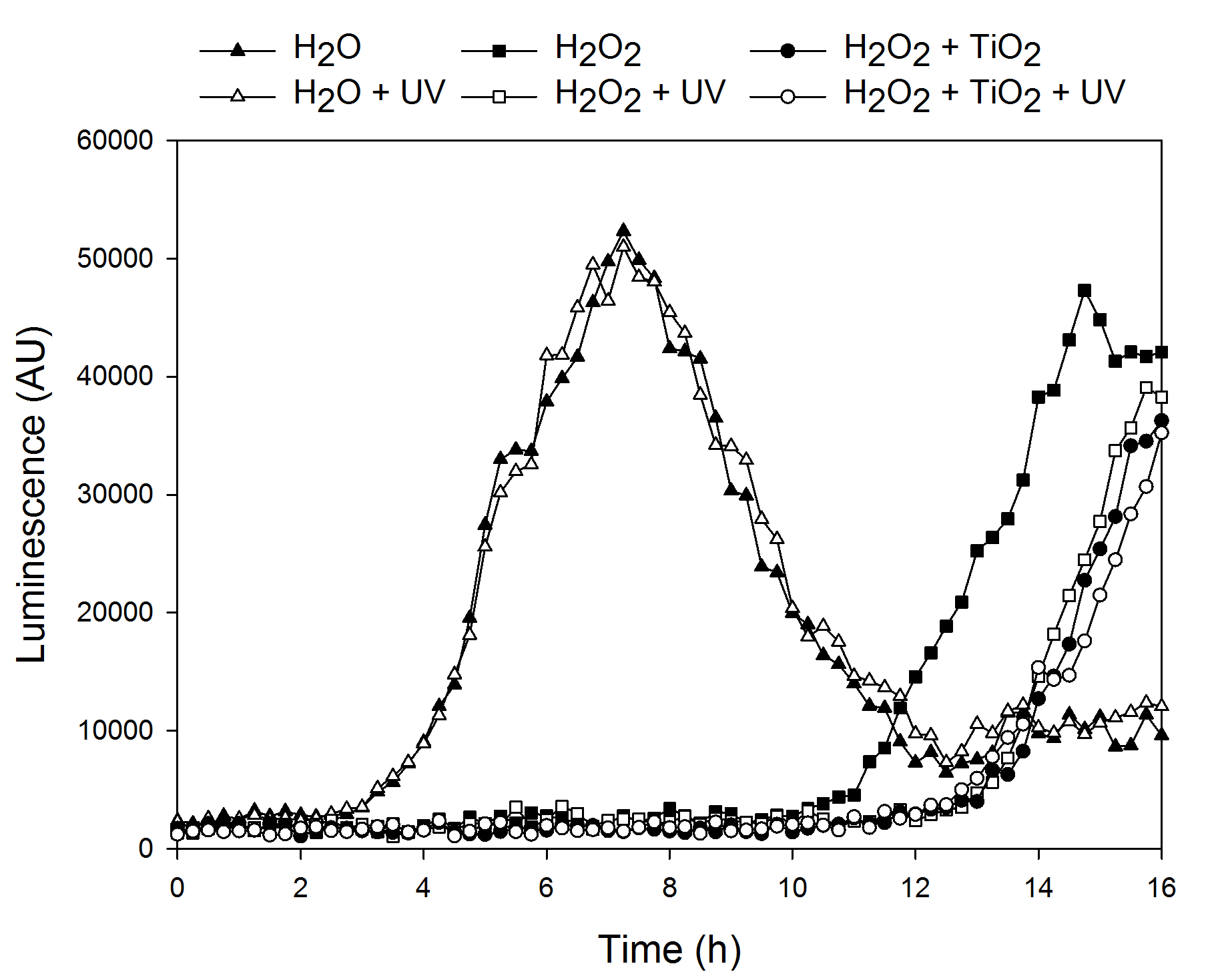
Figure 2: Bacteria regrowth after decontamination
Bacteria regrowth for samples treated with non-irradiated H2O2 was observed approx. 9 h after decontamination. After 14 ¾ h, a peak in luminescence was observed which correlates with ~108 CFU/ml (correlation curve not shown). The exponential rise was followed by a drop in luminescence, possibly due to metabolic changes. Cleaning with H2O2 (UV) and H2O2-TiO2 (with and without UV) was found to delay bacteria regrowth for 2 - 3 h when compared to 5% H2O2. This can be attributed to the increased generation of oxidising species. Interestingly, no UV irradiation was required to achieve an improved cleaning outcome for treatments which contained TiO2 particles. An EPR study (data not shown) indicated the presence of superoxide radicals for H2O2 + TiO2 in darkness which may prolong the bactericidal effect during surgical treatment.
Conclusion: A dynamic in vitro model was successfully developed to observe the effect of antibacterial agents on bacteria regrowth. A combination of H2O2, TiO2 and UV could delay regrowth compared to currently used H2O2 and may therefore be used as a cleaning agent for peri-implantitis in the future.
EUREKA Eurostars E!8320 NuGel
References:
[1] N. Claffey, E. Clarke, I. Polyzois, et al (2008) J Clin Periodontol 35: 316-332