Introduction: Developing long-term neural interfaces for prosthetic control remains challenging[1]. Microchannel neural interfaces (MNIs) overcome some difficulties with neural recording: reducing microchannel diameter, increases recorded signal amplitude and selectivity[2],[3]. However, in vivo, small microchannels (< 50 μm ⌀) become obstructed by fibrous tissue[4]-[6]. Basement membrane (BM) protein coatings improve neural regeneration in vitro[7]. We hypothesise that coating the MNI lumen with BM protein will improve nerve regeneration.
Materials and Methods: MNIs with 150 µm by 200 µm by 5 mm microchannels were prepared by bonding silicone and metal foil sheets[8] and coated with mixed BM proteins (10 µg/cm² Collagen-IV + 1 µg/cm² Laminin-2 + 175 ng/cm² Nidogen-1): the BM group. The control group was unmodified MNIs.
In vivo procedures complied with the UK's Animals (Scientific Procedures) Act (1986 rev. 2013). Adult, male, Lewis rats (N=24) were randomised to 4 groups (n=6): 4 weeks BM; 4 weeks control; 8 weeks BM; 8 weeks control. MNIs were implanted by resecting the sciatic nerve, at mid-thigh. MNIs were secured using proximal and distal epineurial sutures (9-0 polyamide, S&T).
Sciatic function index (SFI) was monitored weekly[9]. After 4 and 8 weeks MNIs were evaluated using wax histology[10]. Nerve morphometry immediately proximal and distal to MNIs was assessed.
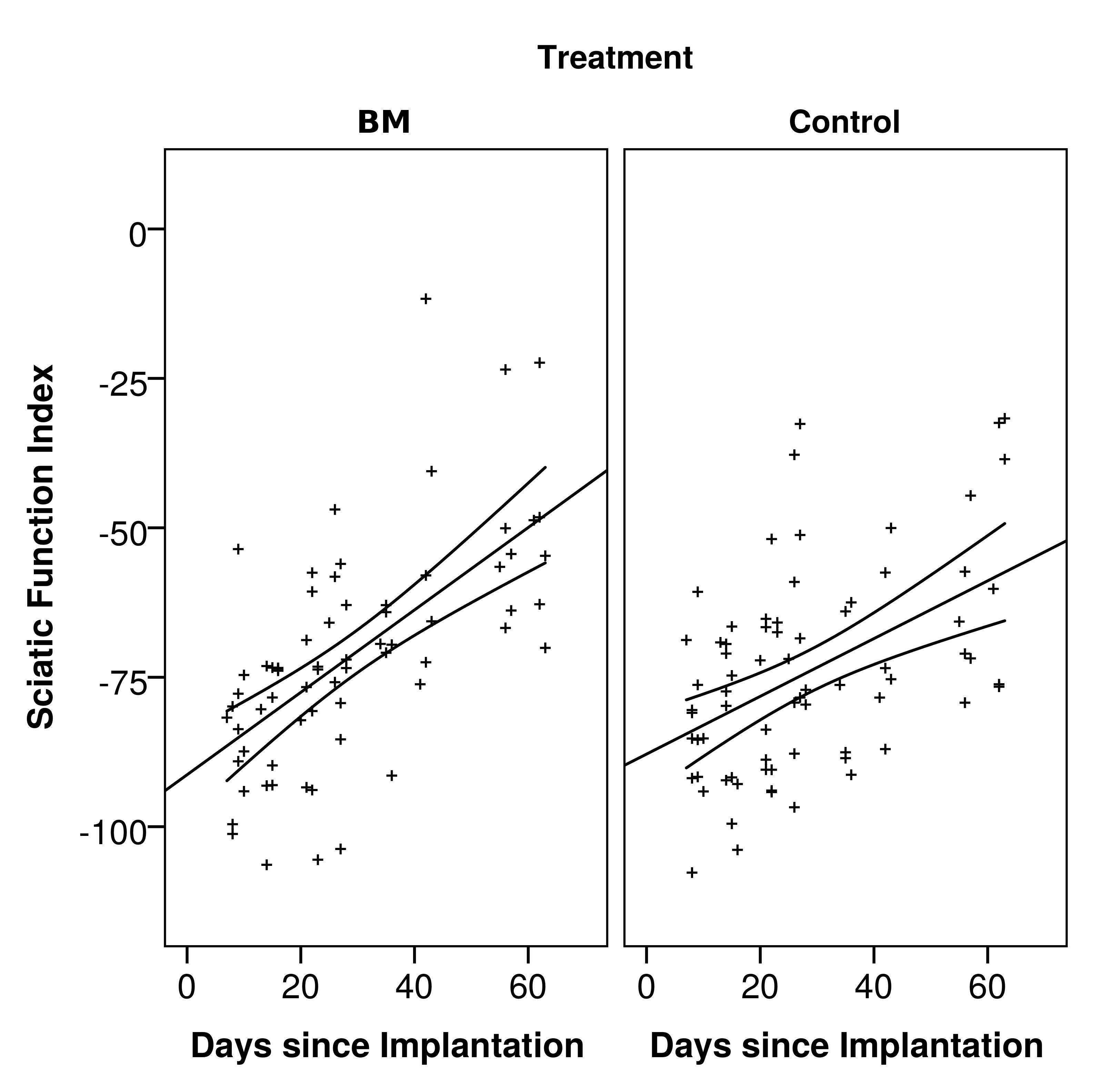
Results: A single animal was lost to follow-up (4 weeks control). SFI increased over 8 weeks in both groups (fig 1., p<0.001). There was no significant difference in SFI rate between groups, circa +0.57 units per day (p=0.9286).
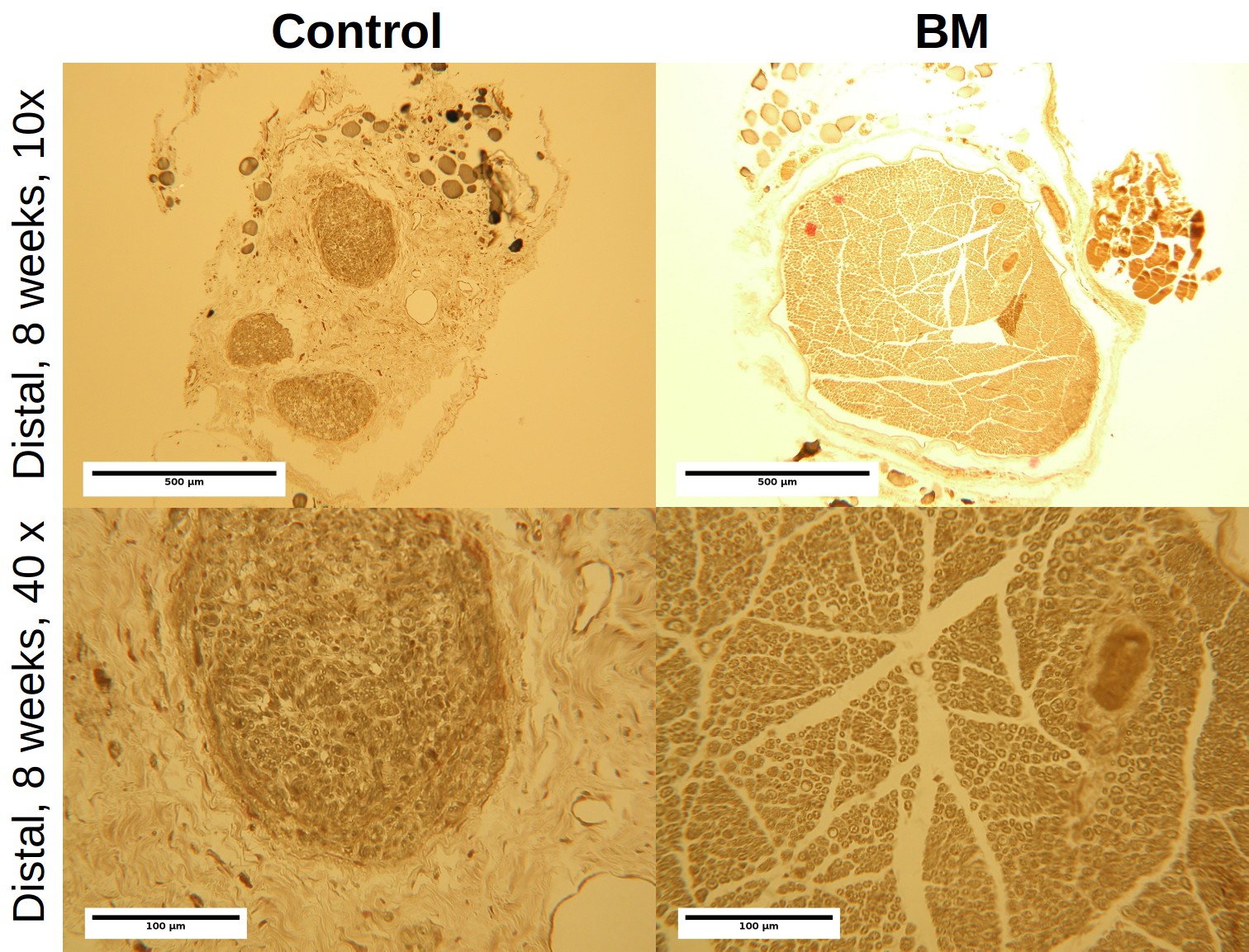
Distal axon diameters were greater in the control group at 4 weeks (p<0.001), and greater in the BM group at 8 weeks (fig 2, p<0.001). Axon density was greater proximal to MNIs in the control group and, greater distally in the BM group (not significant, p≥0.188).
Control group electrode impedance fell significantly following implantation (p=0.01), but not in the BM group (p≥0.133). 1 kHz impedance was not significantly different between the groups at 4 or 8 weeks (p≥0.089).
Discussion: There was no difference in functional recovery between control and BM groups. As with long nerve defects complete recovery was not observed[11]. Histology indicated frustrated axon growth in the control group, while BM encouraged axon growth through the MNI increasing distal axon densities. MNIs may act as nerve guides, directing axon regrowth. Axon density and diameter were lower than for healthy nerve. Axon diameters were similar to previous MNI studies[4], but smaller than non-resected nerve interfaces[12].
Conclusion: BM proteins did not noticeably improve outcomes; however, alternative MNI lumen coatings may improve nerve regeneration. We are now developing the next generation MNIs by increasing the open cross sectional area, reducing feature size, and including amplification and multiplexing.
We would like to thank Gillian Hughes and Roberta Ferro de Godoy for assistance with the in vivo work.; We would like to thank Alexander Mosse and Elliot Magee for assistance with device manufacture.; HL would like to thank the EPSRC (UK) for funding through the M3S Doctoral Training Centre (EP/G036675/1) and the UCL Doctoral Prize Fellowship schemes.
References:
[1] Durand et al 2014 doi:10.1088/1741-2560/11/2/020201
[2] FitzGerald et al 2009 doi: 10.1109/TBME.2009.2013960
[3] FitzGerald et al 2008 doi: 10.1109/TBME.2007.909533
[4] FitzGerald et al 2012 doi:10.1088/1741-2560/9/1/016010
[5] Lacour et al 2009 doi:10.1109/TNSRE.2009.2031241
[6] Srinivasan et al 2015 doi:10.1016/j.biomaterials.2014.11.035
[7] Lancashire et al 2013 ESB Conference pp32
[8] Lancashire et al 2015 J Neural Eng (in review)
[9] Bain et al 1989 PRS 83(1) pp129-136
[10] Di Scipio et al 2008 doi:10.1002/jemt.20577
[11] Li et al 2014 doi:10.1016/j.biomaterials.2014.06.049
[12] Wark et al 2014 doi:10.1088/1741-2560/11/4/046027