- 1Department of Internal Medicine, Hadassah-Hebrew University Medical Center, Jerusalem, Israel
- 2Department of Clinical Microbiology and Infectious Diseases, Hadassah-Hebrew University Medical Center, Jerusalem, Israel
- 3Clalit Health Services, Jerusalem Research Center, Jerusalem, Israel
Objectives: Invasive Candida infections pose a major public health problem worldwide and is a major cause of nosocomial bloodstream infection. Our aim was to assess dynamics in incidence, species distribution and antifungal susceptibility of candidemia episodes in Jerusalem, to better understand the epidemiology of invasive isolates and to better direct therapy.
Methods: We analyzed the incidence dynamics, species distribution and susceptibility pattern of 899 candidemia episodes during 2005–2016 in Jerusalem.
Results: The overall incidence of candidemia was relatively low of 0.62 per 1,000 admissions. Candida albicans was the leading pathogen (39.4%); however, there was a shift toward non-albicans species, with Candida glabrata predominating among them (40%). As expected, more than one-third of candidemias occurred in intensive care units. However, the distribution between species varied and Candida tropicalis was the leading pathogen in hematology-oncology patients. The susceptibility of isolates to antifungals remained stable throughout the years. Only a minority of Candida albicans isolates were non-susceptible to fluconazole (3.3%), however, an unexpectedly high resistance rate (37.8%) was observed in Candida parapsilosis isolates. We found an alarming rate of caspofungin resistance in Candida glabrata (33.6%) and Candida krusei (67%); this may reflect misclassification of resistance by the E-test method.
Conclusions: This is the first comprehensive candidemia analysis in the Jerusalem area that should serve as a basis for decision-making regarding appropriate antifungal treatment in the hospital setting. The exceptional high resistance rate amongst Candida parapsilosis emphasizes the importance of antifungal susceptibility monitoring in medical centers serving large urban areas to better direct appropriate treatment.
Introduction
Candida species are a frequent cause of nosocomial bloodstream infection (BSI), with an incidence of 0.4–1.5/1,000 admissions and a high mortality rate of 15–49%, despite the availability of potent antifungal agents (Pfaller et al., 2010).
In the recent years, a shift in the distribution of Candida species with increased incidence of non-albicans species surpassing Candida albicans was described (Pfaller et al., 2010). In the SENTRY Antimicrobial Surveillance Program, which monitors global incidence of candidemia and antifungal susceptibilities, non-albicans Candida accounted for 52% of candidemia during 2013 with a predominance of Candida glabrata and Candida parapsilosis (Castanheira et al., 2016). One of the major issues regarding candidemia is the high geographical variance in the distribution of Candida species. For example, in the North America ARTEMIS study, C. glabrata which can pose a therapeutic challenge, was the main cause of non-albicans candidemia and accounted for 21.1% of cases; whereas in Latin America, Candida tropicalis was the leading cause (13.2%) (Pfaller et al., 2010).
Resistance to antifungal agents varies among Candida species. Triazole resistance rates among 3,107 Candida species were reported in the SENTRY during 2010–2011 as 5.8–13.5% (Pfaller et al., 2013). In 2013, fluconazole non-susceptibility was uncommon among isolates of C. albicans and C. tropicalis globally, whereas a high rate of fluconazole non-susceptibility was noted among C. glabrata and C. parapsilosis (20.7 and 19%, respectively) (Castanheira et al., 2016). Resistance to echinocandin was low among all Candida species and ranged 0–2.8% (Castanheira et al., 2016). These antifungal susceptibility differences between Candida species may lead to different mortality rates. In a study examining fatal cases of candidemia, 61.5, 50, and 41.2% of C. glabrata, C. parapsilosis and C. albicans isolates, contributed to mortality, respectively (Cheng et al., 2005).
In light of these changes, this study aimed to analyze data of candidemias over a 12-year period in Jerusalem, a large urban area characterized by socially variable population, to estimate incidence and trends in the abundance of various Candida species, as well as their resistance patterns. Such data may facilitate decision making regarding the initiation of antifungal drugs and the adequate empiric choice.
Materials and Methods
Subjects and Study Design
The study was conducted at Hadassah Medical Center, which is divided into two campuses, one is a tertiary hospital comprising 750 beds and the other is a secondary level hospital of 350 beds. Both hospitals serve a population of 1,000,000 in Jerusalem and the surroundings. Together, the two campuses have 8 main intensive care units (ICUs), 6 internal medicine wards, 4 surgery departments and 3 hematology-oncology departments including bone marrow transplantation. All patients admitted to the hospital who developed candidemia from January 2005 to December 2016 were included in the study. The first episode of candidemia was included for each patient, unless there was more than one episode occurring at least 30 days apart. Candida blood isolates from cultures taken 48 h following the admission day were considered nosocomial. Microbiologic data that included identification and antifungal susceptibilities of Candida species were retrieved from the electronic information system of the clinical microbiology laboratory. Demographic and clinical data were collected retrospectively from patient electronic medical records. The study was approved by the local IRB.
Species Identification and Antifungal Susceptibility Testing
During 2005–2012, Candida species were identified from BSI using CHROMagar Candida (HiLabs, Israel) and API ID 32 C (bioMerieux, France), therefore up to third of the rare isolates identified by API ID 32 C may have been misidentified (Cendejas-Bueno et al., 2010). From 2012 and on, isolates were identified mainly by matrix-assisted laser desorption ionization time of flight mass spectrometry (MALDi TOF-MS, VITEK MS, bioMerieux, France). Susceptibility testing was performed as part of routine patient care, using the E-test method according to manufacturer's instructions (bioMerieux, France). Candida isolates were tested for fluconazole, voriconazole, caspofungin, and amphotericin susceptibilities.
Susceptibility results were interpreted according to the Clinical and Laboratory Standards Institute (CLSI) M60 breakpoints (CLSI, 2017). The MIC endpoints of the E-test were elevated to the next 2-fold dilution concentration, which matched the dilution schema of the microdilution method. Candida krusei was considered universally resistant to fluconazole. In cases in which no clinical or efficacy data were available, we used the proposed epidemiologic cutoff value (ECV) criteria, according to the CLSI M59 document (CLSI, 2018). For the purpose of analyses, we defined resistant isolates as those that were non-susceptible by CLSI breakpoints (MIC > susceptibility CBP), or non wild-type (WT) when ECV criteria were used (MIC > ECV). In cases of Candida glabrata, isolates with fluconazole MIC >32 μg/ml were considered resistant. All Candida species and antifungal susceptibilities in this study are available as supplementary data (Supplementary Table 1). Interpretive breakpoints and ECVs used in this study are available in Supplementary Table 2.
Antifungals Consumption Data Analysis
From January 2007 through December 2016, data on the hospital use of fluconazole and echinocandins were obtained from computerized hospital databases. Data about echinocandin use was available from 2011. Consumption was expressed as daily defined doses (DDDs) and normalized per 1,000 patient-days. One DDD is the standard adult dose of an antimicrobial agent for 1 day treatment, defined by the WHO.
Statistics
All incidence rates were calculated using the summed numbers of inpatient days at Hadassah Medical Center during the study period as the denominator, and are presented per 1,000 inpatient days. Categorical variables were analyzed using the Fisher exact test and continuous variables using the Mann–Whitney U-test. We evaluated a possible trend for increase in resistance using a logistic regression model of resistance according to year. All analyses were performed using the R software (version 3.3.3).
Results
Epidemiology
Eight hundred ninety-nine candidemia episodes of 889 unique patients were analyzed. Ten patients had two episodes separated by at least 30 days; therefore, each episode was considered independently for analysis. In 20 episodes (2.2%), more than one candida species was identified (poly-candidemia), consequently the analysis included 919 Candida isolates. Ninety-seven percent (n = 872) of the episodes were nosocomial. During the study period, the annual rate of candidemia did not change markedly and the incidence was stable, with an overall 0.62 episodes per 1,000 hospital admissions. The male to female ratio was 1.7. The adult to pediatric candidemia ratio was 2:1, concordant with the hospital age admission ratio.
During the study period, C. albicans was the predominant pathogen (n = 368, 39.4%), followed by C. glabrata (n = 176, 18.8%), C. tropicalis (n = 168, 18 %), C. parapsilosis (n = 135, 14.4%), C. krusei (n = 54, 5.7%), and other Candida species (n = 32, 3.4%). C. albicans was the most common species isolated in adults (34.5%), followed by C. glabrata (22.4%); whereas in children, C. albicans was isolated in 50%, followed by C. parapsilosis (17.7%). Candida auris was not isolated.
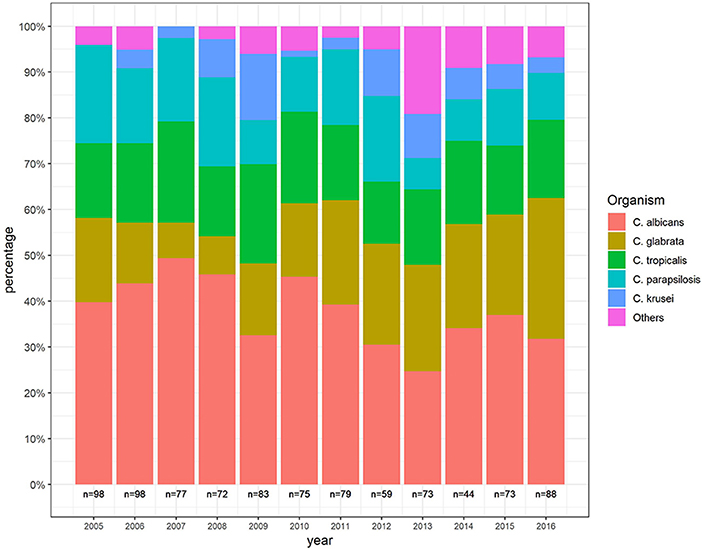
Over the years, the proportion of C. albicans decreased from 39.6 to 33.7% and the proportion of C. glabrata increased from 17.7 to 28.9%, representing about 40% of non-albicans species. The proportion of C. parapsilosis decreased over the years. Similar trends were not demonstrated in other species (Figure 1).
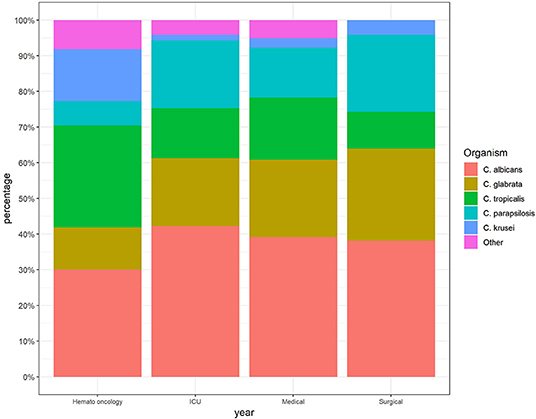
The incidence of candidemia was the highest in ICUs and hemato-oncology wards (5.8 and 5 per 1,000 admissions, respectively), whereas in internal medicine and surgery wards, the incidence was low and stable over the study period (1.3 and 0.4 per 1,000 admissions, respectively. The proportion of C. glabrata isolates was higher in patients hospitalized in the internal medicine and surgery wards, while in the hemato-oncology wards, the rate of C. tropicalis was higher (Figure 2).
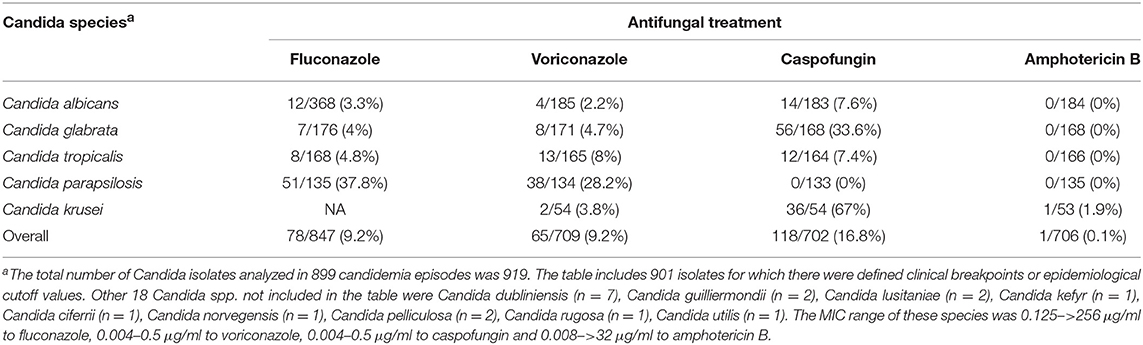
Antifungal Susceptibility Patterns (Figure 3)
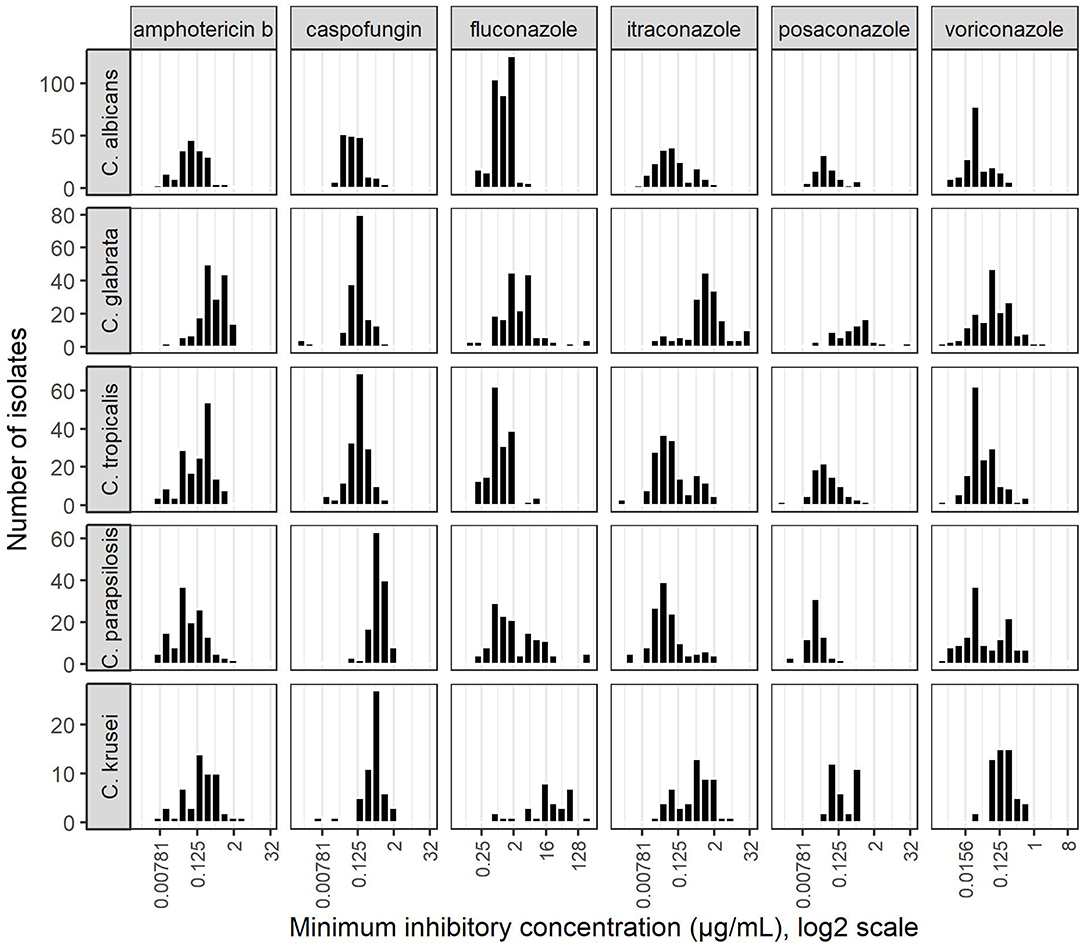
Among the three main groups of antifungals, polyenes, represented by amphotericin B, had the highest susceptibility rates (99.9% of Candida species examined were WT according to the CLSI published ECVs). Most C. albicans, C. tropicalis and C. krusei isolates were triazole susceptible (excluding fluconazole in C. krusei cases), or fluconazole SDD (MIC ≤ 32 μg/ml) in C. glabrata cases. Resistance rates for fluconazole and voriconazole among C. parapsilosis isolates were unexpectedly high, 37.8 and 28.2%, respectively (Table 1) with a bimodal MIC distribution (Figure 3).
Within the echinocandins, most C. albicans, C. tropicalis and C. parapsilosis isolates were caspofungin susceptible (resistance rates ranging 0–7.6%). We found high caspofungin resistance rates among C.glabrata and C. krusei isolates, 33.6 and 67.0%, respectively (Table 1).
Triazole resistance did not change significantly among C. albicans and C. tropicalis isolates since 2005 (p-values 0.69, 0.46 for fluconazole, and 0.88, 0.16 for voriconazole; respectively). One third of C. parapsilosis isolates were resistant to fluconazole in 2015 (3/9), and half in 2016 (4/8), yet this trend was not statistically significant due to low sample numbers (p = 0.71). Likewise, there was no increase in caspofungin resistance over the study period (p = 1).
As for drug usage, fluconazole had a stable demand of DDD/1,000 patient-days during 2011–2016 (range 23.3–29.8, mean 26.3, median 26.3). Conversely, an increased use of echinocandins through 2011–2016 was noticed due to higher demands from the ICUs and hemato-oncology wards (range 0.4–1.18, mean 0.98, median 1.18).
Discussion
Given the high geographical variance in the distribution and resistance patterns of Candida species, in this study we analyzed candidemia data over 12 years in a large tertiary center in Israel to better understand contemporary trends that might affect treatment decision making. We found a stable incidence of candidemia (0.62 episodes per 1,000 hospital admissions) and increased rate of non-albicans candidemia, mainly attributed to C. glabrata accounting for 40% of the non-albicans cases as similar to other reports (Pfaller et al., 2010, 2019). Species distribution varied according to age group and admitting ward. Fluconazole consumption over the study period was stable, concordant with low level resistance rate to fluconazole among Candida species totally. Specifically, C. parapsilosis isolates had a high rate of resistance to fluconazole as well as voriconazole (37.8, 28.2%, respectively). Increasing echinocandin consumption was not translated to a general increase of resistance to caspofungin, though a high rate of resistance was noted amongst C. glabrata and C. krusei isolates (33.6 and 67.0%, respectively).
Species Distribution
Similar to our findings, an increased rate of C. glabrata candidemia during the last decade was documented in another tertiary center covering the central district of israel (Eliakim-Raz et al., 2016). Former studies linked the increased rate of C. glabrata candidemia to increased fluconazole use (Lortholary et al., 2011). However, high-risk patients in our database did not receive fluconazole prophylaxis, consistent with hospital policy, and there was no increase of fluconazole use from 2007 to 2016. Another study (Ben-Ami et al., 2012) found that recent exposure to antibacterial drugs increased the risk of BSI with fluconazole-resistant Candida isolates, suggesting that the effects of antibacterial drugs may have significant impact on azole resistance in Candida species. This may explain the increased incidence of C. glabrata in our study (Figure 1).
Our analysis also points to a difference in species distribution according to the admitting ward and age group, that can potentially impact empiric treatment choices: As opposed to the general shift toward C. glabrata, the main cause to non-albicans candidemia in the hemato-oncology wards was C. tropicalis (28.6% overall), a generally fluconazole susceptible isolate. C. tropicalis originates from the gastrointestinal (GI) tract and has been described in the past as a common cause of candidemia in neutropenic patients (Wingard et al., 1979). Species distribution according to age group underscored C. parapsilosis as the main cause of non-albicans candidemia in pediatric patients which may reflect increased use of central lines in this population and mandates appropriate empiric treatment considering the high resistance rate to azoles found in this study among these isolates (Trofa et al., 2008).
Antifungal Susceptibility
The susceptibility analysis in this study was based on E-test, an agar-based method widely used in many laboratories for its simplicity. E-test has high categorical and essential agreement with the recommended CLSI broth microdilution method (BMD) (Matar et al., 2003).
The low susceptibility rate to fluconazole and voriconazole (62.2 and 71.8%, respectively) among C. parapsilosis in this study is meaningful as this is a common non-albicans species with increasing prevalence (Pfaller et al., 2019) that may be nosocomially transmitted by hand carriage and cause catheter-related candidemia (Van Asbeck et al., 2007). Generally, fluconazole is considered a highly effective drug against this pathogen, with resistance rates of roughly 3.9% (Pfaller et al., 2019); however, some investigators have reported a rise in the incidence of invasive infections due to fluconazole-resistant strains (Pfaller et al., 2014). This rise is worrisome due to the potential of nosocomial horizontal transmission of resistant strains (Trofa et al., 2008). A national Israeli candidemia study (Ben-Ami et al., 2012) and a recent study from a different district of Israel (Eliakim-Raz et al., 2016), have found markedly lower fluconazole resistance rate among C. parapsilosis as compared to ours (13.3 and 11.1% respectively). These local differences reflect the limitations of national based monitoring of Candida spp. distribution and antifungal susceptibility profile that can miss such variances and outline an unoptimized therapy, even in a small country as Israel.
We hypothesize that the decreased fluconazole susceptibility shown here, alongside with the bimodal MIC distribution of fluconazole and voriconazole as shown in Figure 3, and a stable demand of fluconazole over the years, reflect the presence of regional resistant clones. These clones may harbor mutations in ERG11 or overexpress ERG11, a gene encoding lanosterol 14α-demethylase which is the target enzyme for fluconazole (Souza et al., 2015). Clonality among C. parapsilosis was mainly investigated in outbreak settings in other studies. In an outbreak of 28 C. parapsilosis BSI in an ICU in Brazil, typing of 21 fluconazole resistant strains revealed 9 isolates that were considered genetically related with only a minority of patients previously exposed to fluconazole. This cluster suggested the horizontal transmission of fluconazole resistant C. parapsilosis (Pinhati et al., 2016). A study that analyzed resistant C. parapsilosis by microsatellite typing, confirmed a clonal origin of the strains with all strains harboring a common mutation leading to a Y132F amino-acid substitution in the ERG11 gene (Souza et al., 2015). Similar to the Brazilian outbreak, the same underlying genomic mechanism may be responsible for our findings and further study examining the possibility of clonality and molecular resistance patterns is currently underway.
Altogether, we did not find an increase in caspofungin resistance among Candida isolates. This is in concordance with other studies from the last decade (Posteraro et al., 2015). Nonetheless, the increased echinocandin use during the last 4 years of the study, specifically in hemato-oncology wards, necessitates continuous monitoring of the echinocandin resistance rate.
We suspect that the low proportion of caspofungin susceptibility among C. glabrata and C. krusei (66.4 and 33%, respectively) is due to the low reliability of the caspofungin E-test for these two species. The revised CLSI recommendations refer to a risk of misclassifying caspofungin susceptible C. glabrata and C. krusei as resistant when tested by the E-test, compared to the BMD method (Pfaller et al., 2012). In addition, a study of a large set of C. glabrata isolates in Israel (Ben-Ami et al., 2014) found low essential agreement (47.8%) between BMD and E-test when caspofungin was tested according to an ECV of 0.12 μg/mL (Pfaller et al., 2011), which is the current susceptibility breakpoint (CLSI, 2017). This breakpoint was found to be unreliable to discriminate between resistant and susceptible isolates because the MIC distribution curve differed from that of the CLSI, and clustered between 0.25 and 0.5 μg/mL, similar to our isolates that also clustered around these values (Figure 3). Therefore, C. glabrata susceptibility results, as determined by the E-test method for caspofungin should be interpreted with caution; and the validation of susceptibility results with BMD may be advisable for invasive strains (Ben-Ami et al., 2014).
Conclusions
We observed an increasing proportion of non-albicans BSI, similar to other study groups worldwide, with varied species distribution according to admitting ward and age; however, antifungal resistance did not significantly increase over the years. We found a high rate of fluconazole and voriconazole non-susceptibility among C. parapsilosis isolates. This may represent a local clonal phenomenon and highlights the importance of prudent selection of empiric therapy. Our reported high rate of caspofungin resistance among C. glabrata and krusei may reflect misclassification of resistance by the E-test. Ongoing surveillance of the epidemiology and antifungal resistance of Candida isolates in different geographic regions as well as large urban areas is imperative as it enables tracking clonal patterns with concordant resistance mechanisms; this promotes better selection of empiric antifungal therapy.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Author Contributions
SI: acquisition of data and analysis, drafting of article and critical revision. SA: acquisition of laboratory data, drafting of article and critical revision. AI: analysis of data. AL: acquisition of data and analysis. RN-P: drafting of article and critical revision. MK: conception and design of study, acquisition and analysis of data, drafting of article and critical revision, final approval of manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcimb.2019.00352/full#supplementary-material
References
Ben-Ami, R., Hilerowicz, Y., Novikov, A., and Giladi, M. (2014). The impact of new epidemiological cutoff values on Candida glabrata resistance rates and concordance between testing methods. Diagn. Microbiol. Infect. Dis. 79, 209–213. doi: 10.1016/j.diagmicrobio.2014.02.008
Ben-Ami, R., Olshtain-Pops, K., Krieger, M., Oren, I., Bishara, J., Dan, M., et al. (2012). Antibiotic exposure as a risk factor for fluconazole-resistant Candida bloodstream infection. Antimicrob. Agents Chemother. 56, 2518–2523. doi: 10.1128/AAC.05947-11
Castanheira, M., Messer, S. A., Rhomberg, P. R., and Pfaller, M. A. (2016). Antifungal susceptibility patterns of a global collection of fungal isolates: results of the SENTRY Antifungal Surveillance Program (2013). Diagn. Microbiol. Infect. Dis. 85, 200–204. doi: 10.1016/j.diagmicrobio.2016.02.009
Cendejas-Bueno, E., Gomez-Lopez, A., Mellado, E., Rodriguez-Tudela, J. L., and Cuenca-Estrella, M. (2010). Identification of pathogenic rare yeast species in clinical samples: comparison between phenotypical and molecular methods. J. Clin. Microbiol. 48, 1895–1899. doi: 10.1128/JCM.00336-10
Cheng, M. F., Yang, Y. L., Yao, T. J., Lin, C. Y., Liu, J. S., Tang, R. B., et al. (2005). Risk factors for fatal candidemia caused by Candida albicans and non-albicans Candida species. BMC. Infect. Dis.5:22. doi: 10.1186/1471-2334-5-22
CLSI (2017). Performance Standards for Antifungal Susceptibility Testing of Yeasts, 1st edn. CLSI Supplement M60. Wayne, PA: Clinical and Laboratory Standards Institute.
CLSI (2018). Epidemiological Cutoff Values for Antifungal Susceptibility Testing, 2nd edn. CLSI Supplement M59. Wayne, PA: Clinical and Laboratory Standards Institute.
Eliakim-Raz, N., Babaoff, R., Yahav, D., Yanai, S., Shaked, H., and Bishara, J. (2016). Epidemiology, microbiology, clinical characteristics, and outcomes of candidemia in internal medicine wards—a retrospective study. Int. J. Infect. Dis. 52, 49–54. doi: 10.1016/j.ijid.2016.09.018
Lortholary, O., Desnos-Ollivier, M., Sitbon, K., Fontanet, A., Bretagne, S., and Dromer, F. (2011). Recent exposure to caspofungin or fluconazole influences the epidemiology of candidemia: a prospective multicenter study involving 2,441 patients. Antimicrob. Agents Chemother. 55, 532–538. doi: 10.1128/AAC.01128-10
Matar, M. J., Ostrosky-Zeichner, L., Paetznick, V. L., Rodriguez, J. R., Chen, E., and Rex, J. H. (2003). Correlation between E-test, disk diffusion, and microdilution methods for antifungal susceptibility testing of fluconazole and voriconazole. Antimicrob. Agents Chemother. 47, 1647–1651. doi: 10.1128/AAC.47.5.1647-1651.2003
Pfaller, M. A., Castanheira, M., Lockhart, S. R., Ahlquist, A. M., Messer, S. A., and Jones, R. N. (2012). Frequency of decreased susceptibility and resistance to echinocandins among fluconazole-resistant bloodstream isolates of Candida glabrata. J. Clin. Microbiol. 50, 1199–1203. doi: 10.1128/JCM.06112-11
Pfaller, M. A., Diekema, D. J., Andes, D., Arendrup, M. C., Brown, S. D., Lockhart, S. R., et al. (2011). Clinical breakpoints for the echinocandins and Candida revisited: integration of molecular, clinical, and microbiological data to arrive at species-specific interpretive criteria. Drug Resist. Updat. 14, 164–176. doi: 10.1016/j.drup.2011.01.004
Pfaller, M. A., Diekema, D. J., Gibbs, D. L., Newell, V. A., Ellis, D., Tullio, V., et al. (2010). Results from the artemis disk global antifungal surveillance study, 1997 to 2007: A 10.5-year analysis of susceptibilities of Candida species to fluconazole and voriconazole as determined by CLSI standardized disk diffusion. J. Clin. Microbiol. 48, 1366–1377. doi: 10.1128/JCM.02117-09
Pfaller, M. A., Diekema, D. J., Turnidge, J. D., Castanheira, M., and Jones, R. N. (2019). Twenty years of the SENTRY Antifungal Surveillance Program: results for Candida species from 1997–2016. Open Forum Infect. Dis. 6, S79–S94. doi: 10.1093/ofid/ofy358
Pfaller, M. A., Jones, R. N., and Castanheira, M. (2014). Regional data analysis of Candida non-albicans strains collected in United States medical sites over a 6-year period, 2006–2011. Mycoses 57, 602–611. doi: 10.1111/myc.12206
Pfaller, M. A., Messer, S. A., Woosley, L. N., Jones, R. N., and Castanheira, M. (2013). Echinocandin and triazole antifungal susceptibility profiles for clinical opportunistic yeast and mold isolates collected from 2010 to 2011: application of new CLSI clinical breakpoints and epidemiological cutoff values for characterization of geographic. J. Clin. Microbiol. 51, 2571–2581. doi: 10.1128/JCM.00308-13
Pinhati, H. M. S., Casulari, L. A., Souza, A. C. R., Siqueira, R. A., Damasceno, C. M. G., and Colombo, A. L. (2016). Outbreak of candidemia caused by fluconazole resistant Candida parapsilosis strains in an intensive care unit. BMC Infect. Dis. 16:433. doi: 10.1186/s12879-016-1767-9
Posteraro, B., Spanu, T., Fiori, B., De Maio, F., De Carolis, E., Giaquinto, A., et al. (2015). Antifungal susceptibility profiles of bloodstream yeast isolates by Sensititre YeastOne over nine years at a large Italian teaching hospital. Antimicrob. Agents Chemother. 59, 3944–3955. doi: 10.1128/AAC.00285-15
Souza, A. C. R., Fuchs, B. B., Pinhati, H. M. S., Siqueira, R. A., Hagen, F., Meis, J. F., et al. (2015). Candida parapsilosis resistance to fluconazole: molecular mechanisms and in vivo impact in infected Galleria mellonella Larvae. Antimicrob. Agents Chemother. 59, 6581–6587. doi: 10.1128/AAC.01177-15
Trofa, D., Gácser, A., and Nosanchuk, J. D. (2008). Candida parapsilosis: an emerging fungal pathogen. Am. Soc. Microbiol. 21, 606–625. doi: 10.1128/CMR.00013-08
Van Asbeck, E. C., Huang, Y. C., Markham, A. N., Clemons, K. V., and Stevens, D. A. (2007). Candida parapsilosis fungemia in neonates: genotyping results suggest healthcare workers hands as source, and review of published studies. Mycopathologia 164, 287–293. doi: 10.1007/s11046-007-9054-3
Keywords: Candida species, resistance, antifungal treatment, antifungal susceptibility, epidemiology
Citation: Israel S, Amit S, Israel A, Livneh A, Nir-Paz R and Korem M (2019) The Epidemiology and Susceptibility of Candidemia in Jerusalem, Israel. Front. Cell. Infect. Microbiol. 9:352. doi: 10.3389/fcimb.2019.00352
Received: 30 July 2019; Accepted: 30 September 2019;
Published: 11 October 2019.
Edited by:
Jose L. Lopez-Ribot, University of Texas at San Antonio, United StatesReviewed by:
Rhys Alexander Farrer, University of Exeter, United KingdomAlexandre Alanio, Paris Diderot University, France
Copyright © 2019 Israel, Amit, Israel, Livneh, Nir-Paz and Korem. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maya Korem, bWF5YWtAaGFkYXNzYWgub3JnLmls
 Sarah Israel
Sarah Israel Sharon Amit
Sharon Amit Ariel Israel3
Ariel Israel3 Ran Nir-Paz
Ran Nir-Paz Maya Korem
Maya Korem