The effect of ultrasound-guided erector spinae plane block combined with dexmedetomidine for postoperative pain management in lumbar spine surgery: A case-based discussion
- Department of Women, Child, General and Specialistic Surgery, University of Campania “L. Vanvitelli”, Naples, Italy
Background: Ultrasound-guided erector spinae plane blocks (US-ESPB) can be valid resources of simple and safe execution in a multimodal approach to postoperative pain management in lumbar spine surgery. It has been shown that the use of multimodal anesthesia reduces the use of intraoperative and postoperative opioids, and also improves analgesia. A growing body of evidence supports that the adjuvant use of dexmedetomidine in locoregional anesthesia significantly prolongs the analgesia and potentiates the effect of the block, without clinically significant side effects.
Case presentation: A series of six consecutive patients received bilateral ultrasound-guided erector spinae plane blocks with local anesthetics and dexmedetomidine as part of a multimodal analgesic therapy after lumbar spine surgery. Treatment adequacy was evaluated using numerical rating scale (NRS) and overall benefit of analgesic score (OBAS); overall the observed results were satisfactory for all patients.
Conclusion: Bilateral US-ESPB appears to be helpful in providing adequate postoperative analgesia after lumbar spine surgery. It is simple and safe, and so it is unique when compared to other blockages. The addition of Dexmedetomidine as an adjuvant seems to improve analgesic effectiveness and durability.
Key summary points
1. Ultrasound-guided erector spinae plane blocks (US-ESPB) can be valid resources of simple and safe execution in a multimodal approach to postoperative pain management in lumbar spine surgery.
2. Dexmedetomidine is a highly selective alpha-2 agonist with sedative, analgesic properties.
3. The adjuvant use of dexmedetomidine in locoregional anesthesia significantly prolongs the analgesia and potentiates the effect, without clinically significant side effects.
4. The use of multimodal techniques can allow substantial opioid-sparing effect and can reduce pain.
Background
The erector spinae plane (ESP) block was first described by Forero et al. (1) in 2016 for the treatment of chronic neuropathic chest pain. Over the past 4 years, publications related to the ESP block have increased significantly. It is currently used for postoperative pain control in thoracic, abdominal, bariatric surgery, breast surgery, and even spine surgery.
Ultrasound-guided erector spinae plane blocks (US-ESPB) can be valid resources of simple and safe execution in a multimodal approach to postoperative pain management in lumbar spine surgery (2).
It has been shown that the use of multimodal anesthesia by improving analgesia reduces the use of intraoperative and postoperative opioids (3). A growing body of evidence supports the adjuvant use of dexmedetomidine in locoregional anesthesia significantly prolongs the analgesia and potentiates the effect, without clinically significant side effects (4, 5).
The US-ESPB is a block of the paraspinal fascial plane. The needle is placed between erector spinae muscle and thoracic transverse processes. By administering local anesthetic the dorsal and ventral branches of thoracic and abdominal spinal nerves are blocked. ESP block is usually performed using a linear ultrasound probe with in-plane technique (1). This block is able to guarantee a good analgesia of the anterior, posterior and lateral thoracic and abdominal walls. The benefits of ESP block are not yet demonstrated. The specific mechanism is still controversial (6, 7).
We hereby present a series of six consecutive patients who received bilateral US-ESPB with ropivacaine, lidocaine and dexmedetomidine in lumbar spine surgery.
Objectives
The purpose of this case-based discussion is to evaluate opioid consumption during surgery and in the postoperative period. Furthermore, secondary objectives are: the evaluation of pain control through the Numerical Rating Scale (NRS) at 6-12-24 h after surgery, at rest and in motion and patient satisfaction assessed with the overall benefit of analgesic (OBAS) score.
Case presentation
Patients were invited to read and sign an informed consent to use their personal data in the publication of this series of cases for scientific and clinical purposes.
Six Caucasian patients, four males and two females aged 40–60 years, were recruited; all patients used chronic opioid therapy for low back pain which had not improved after physiotherapy and motor rehabilitation. For this reason, spinal decompression surgery was necessary.
Patients were premedicated with midazolam 0.03 mg/kg and dexamethasone 4 mg intravenously. Induction of general anesthesia was obtained with propofol (2 mg/kg intravenously), rocuronium (0.6 mg/kg intravenously) for neuromuscular blockade, remifentanyl (0.1 mcg/kg/min) for tracheal intubation, and desflurane with minimal alveolar concentration (MAC) 1 for maintenance.
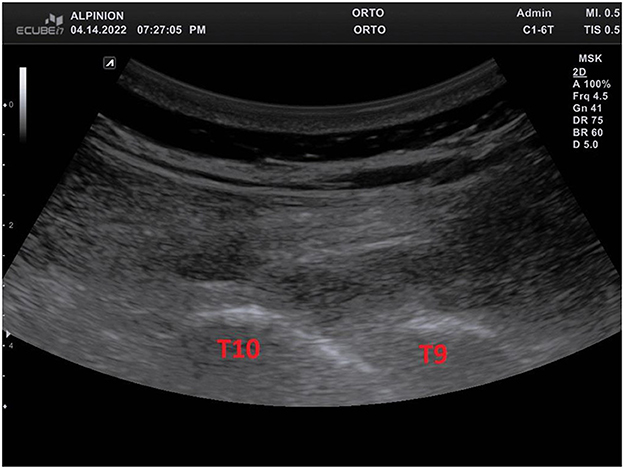
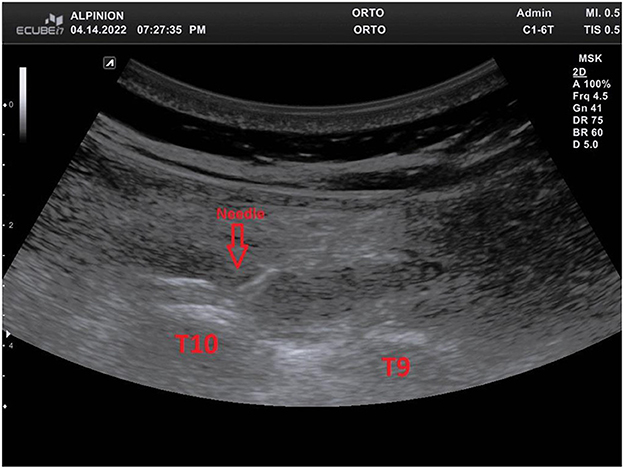
After obtaining the prone position, bilateral US-ESPB was performed with a high frequency convex probe (3.5 MHz 50 mm) positioned in longitudinal orientation at the level of the T10 transverse process (identified under ultrasound guidance), about 3 cm from the midline (Figure 1). A needle block (21G 85 mm) was inserted in plane, with a craniocaudal direction, until its tip hit the transverse process of T10 (Figure 2). After hydrolocation with 3 mL of saline solution, a volume of 20 mL containing ropivacaine 75 mg, lidocaine 100 mg and dexmedetomidine 0.5 μg/kg was injected deep to the erector spinae muscle, and the procedure repeated on the other side. There were no hemodynamic changes following the bilateral blocks. For all patients, remifentanil was stopped about 15 min after surgery because hemodynamic parameters allowed it. No additional rocuronium boluses were needed to maintain curarization. Around 30 min before the end of surgery, patients received paracetamol 1,000 mg, ketorolac 30 mg, ondansetron 4 mg. Opioid consumption during and after the intervention was recorded, and pain was evaluated using NRS at rest and on movement at 6-12-24 h following surgery and OBAS scores on discharge. Postoperative pain treatment included paracetamol 1,000 mg every 8 h, and ketorolac when needed up to 90 mg/day. Analgesic rescue therapy in case reported NRS were above 6 consisted of morphine 10 mg i.m. every 4 h, titrated on age and weight.
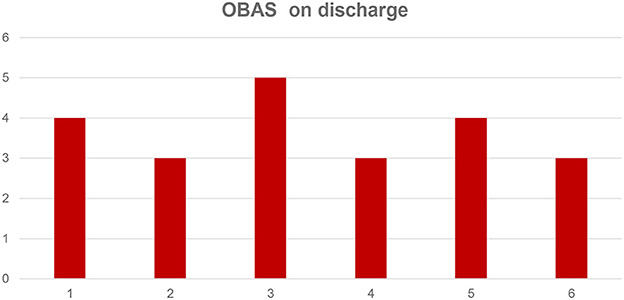
During all the observation period, all patients reported NRS values below 4 at rest and below 5 on movement, while OBAS scores lower than 5 (Table 1, Figure 3). We observed minimal opioid consumption over the first 24 h and high level of satisfaction in all patients. None required rescue analgesia with morphine during this period.
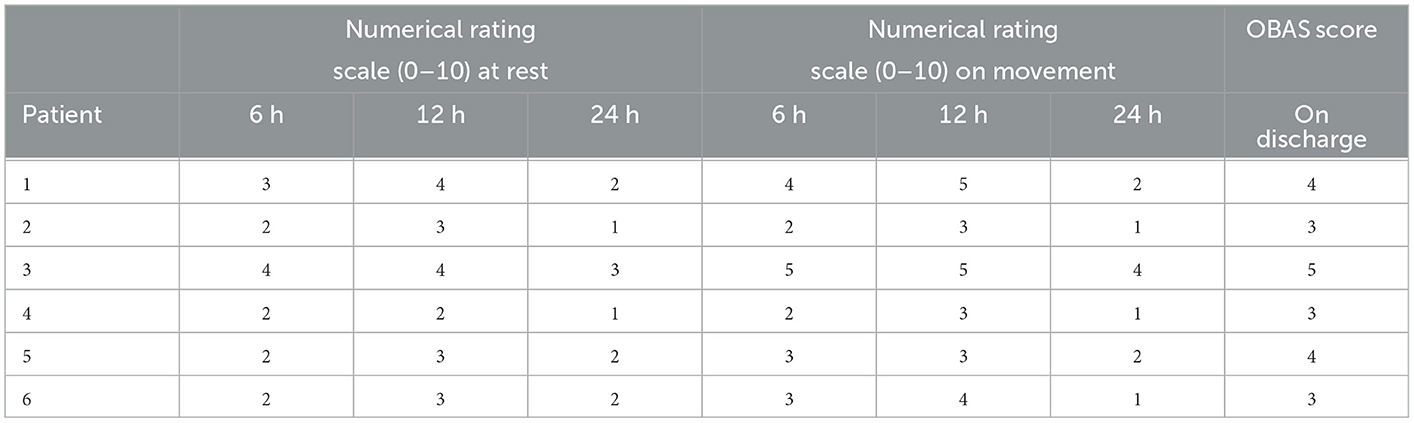
Table 1. Numerical rating scale at 6, 12, 24 h postoperatively at rest and on movement and overall benefit of analgesic score (OBAS) on discharge.
Discussion
Lumbar spine surgery is the most common surgery for the treatment of back and leg pain (2). To our knowledge, this is the first case-series illustrating the efficacy and safety of dexmedetomidine as adjuvant to local anesthetics in US-ESPB for lumbar spine surgery.
Dexmedetomidine is a highly selective alpha-2 adrenoreceptor agonist without any effect on the GABA receptor (8). The average length of analgesia provided by bilateral US-ESPB was between 6 and 8 h (9) and can be increased by the use of dexmedetomidine. In a recent manuscript, it has been shown that patients with chronic pain, who make chronic use of opioids before surgery, benefit from opioid-free anesthesia. These patients are at a higher risk of acute postoperative severe pain and therefore increased use of postoperative opioids. This has been shown to increase the risk of chronic post-surgical pain (10).
Lumbar spine surgery causes severe pain (11). Studies show that opioid-based intravenous patient-controlled analgesia is frequently used to manage pain after spinal decompression surgery (12). In these patients, the side effects of opioid use may occur, for example nausea or vomiting and hypotension, but also more serious side effects such as loss of consciousness and respiratory depression. It is important to remember also the side effect related to regional anesthesia techniques. For example the epidural anesthesia and paravertebral blocks can determinate inadvertent motor blockade, urinary retention, pneumothorax, hemodynamic instability, epidural hematoma and so on (13). US-ESPB can be useful as a safe and effective method for regional analgesia. It may improve postoperative recovery, shortens hospitalization stay and determinate an opioid-sparing effect (14, 15).
Ueshima et al. demonstrated a pain reduction after lumbar spine surgery in patients who received ESP blocks (16). Based on this data, we performed bilateral preoperative ESP blocks at T10 level in patients undergoing lumbar spine surgery and also found a significant reduction in the need for intraoperative and postoperative opioids, better post-operative pain control, greater patient satisfaction, early mobilization in accordance with ERAS protocols. The advantage of US-ESPB is its procedural simplicity. Sonoanatomy is easily recognizable, vital structures such as the pleura and spinal cord are distant from the block site. ESP block doesn't determinate autonomic blockade while it accompanies paravertebral and thoracic epidural techniques. Thus, it offers greater hemodynamic stability and lower requirements for extensive monitoring. An indwelling catheter can also be inserted with this technique, extending the duration of analgesia as required (17, 18).
Our preliminary experience suggests that US-ESPB with dexmedetomidine can be safely implemented in multimodal analgesic regimen after lumbar spine surgery. The observed results encourage further exploration of the analgesic and opioid sparing potential of dexmedetomidine, also in relation to chronic postoperative pain that frequently ensues these surgical approaches. Our article has several limitations. The number of patients, only 6, is not large enough to evaluate the clinical efficacy of dexmedetomidine as a local anesthetic adjuvant; further large-scale studies are needed. The effectiveness of ESPB in reducing opioid use has already been demonstrated for other surgeries, It is necessary to conduct studies on the mechanism of action of peripheral dexmedetomidine as an adjuvant in ESPB and whether it can improve pain control in patients using opioids for chronic pain.
Conclusion
Bilateral US-ESPB appears to be helpful in providing adequate postoperative analgesia after lumbar spine surgery. It is simple and safe, which makes it unique compared to other blockages and the addition of Dexmedetomidine as an adjuvant seems to improve analgesic effectiveness and durability. Prospective and randomized clinical trials will be needed to establish its clinical role.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics statement
This case series is based on the data collected from the medical records for a standard clinical therapy, and therefore the approval of the Ethics Committee was not required. All patients provided written informed consent for participation and the trials were conducted in accordance with the International Conference on Harmonization Good Clinical Practice guidelines and the provisions of the 2008 Declaration of Helsinki. Patient approval for the publication was obtained.
Author contributions
FC, PS, and MCP: conceptualization. VP and LG: data collection. FC, CP, and MCP: writing case-series and editing. MBP and CA: supervision. All authors read and approved the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ESP, erector spinae plane; US-ESPB, ultrasound-guided erector spinae plane block; NRS, numerical rating scale; OBAS, overall benefit of analgesic score; MAC, minimal alveolar concentration.
References
1. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuro- pathic pain. Reg Anesth Pain Med. (2016) 41:621–7. doi: 10.1097/AAP.0000000000000451
2. Liu MJ, Zhou XY, Yao YB, Shen X, Wang R, Shen QH. Postoperative analgesic efficacy of erector spinae plane block in patients undergoing lumbar spinal surgery: a systematic review and meta-analysis. Pain Ther. (2021) 10:333–47. doi: 10.1007/s40122-021-00256-x
3. Mulier J. Perioperative opioids aggravate obstructive breathing in sleep apnea syndrome: mechanisms and alternative anesthesia strategies. Curr Opin Anesthesiol. (2016) 29:129–33. doi: 10.1097/ACO.0000000000000281
4. Gao Z, Xiao Y, Wang Q, Li Y. Comparison of dexmedetomidine and dexamethasone as adjuvant for ropivacaine in ultrasound-guided erector spinae plane block for video-assisted thoracoscopic lobectomy surgery: a randomized, double-blind, placebo-controlled trial. Ann Transl Med. (2019) 7:668. doi: 10.21037/atm.2019.10.74
5. Coviello A, Esposito D, Galletta R, Maresca A, Servillo G. Opioid-free anesthesia—dexmedetomidine as adjuvant in erector spinae plane block: a case series. J Med Case Rep. (2021) 15:1. doi: 10.1186/s13256-021-02868-5
6. Elsharkawy H, Pawa A, Mariano ER. Interfascial plane blocks: back to basics. Reg Anesth Pain Med. (2018) 43:341–6. doi: 10.1097/AAP.0000000000000750
7. Hamilton DL, Manickam BP. Is the erector spinae plane (ESP) block a sheath block. Anaesthesia. (2017) 72:915–6. doi: 10.1111/anae.13912
8. Cristiano L, Coppolino F, Donatiello V, Paladini A, Sansone P, Passavanti MB, et al. Use of dexmedetomidine in transfemoral transcatheter aortic valve implantation (tf-TAVI) procedures. Adv Ther. (2020) 37:2337–43. doi: 10.1007/s12325-020-01342-w
9. Singh S, Chaudhary NK. Bilateral ultasound guided erector spinae plane block for postoperative pain management in lumbar spine surgery: a case series. J Neurosurg Anesthesiol. (2019) 31:354. doi: 10.1097/ANA.0000000000000518
10. Beloeil H. Opioid-free anesthesia. Best Pract Res Clin Anaesthesiol. (2019) 33:353–60. doi: 10.1016/j.bpa.2019.09.002
11. Gerbershagen HJ, Aduckathil S, van Wijck AJ, Pee- len LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. (2013) 118:934–44. doi: 10.1097/ALN.0b013e31828866b3
12. Bohl DD, Louie PK, Shah N, Mayo BC, Ahn J, Kim TD, et al. Multimodal versus patient-controlled analgesia after an anterior cervical decompression and fusion. Spine (Phila Pa 1976). (2016) 41:994–8. doi: 10.1097/BRS.0000000000001380
13. Gottschalk A, Freitag M, Tank S, Burmeister MA, Kreil S, Kothe R, et al. Quality of postoperative pain using an intraoperatively placed epidural catheter after major lumbar spinal surgery. Anesthesiology. (2004) 101:175–80. doi: 10.1097/00000542-200407000-00027
14. Sansone P, Giaccari LG, Faenza M, Di Costanzo P, Izzo S, Aurilio C, et al. What is the role of locoregional anesthesia in breast surgery? A systematic literature review focused on pain intensity, opioid consumption, adverse events, and patient satisfaction. BMC Anesthesiol. (2020) 20:290. doi: 10.1186/s12871-020-01206-4
15. Coppolino F, Sansone P, Passavanti MB, Pace MC, Sepolvere G, Aurilio C. The role of an ultrasound-guided block of the deep plane of the serratus muscle in a modified ERAS protocol for cardiac surgery. Open Anesthesia J. (2020) 14:49–51. doi: 10.2174/2589645802014010049
16. Ueshima H, Inagaki M, Toyone T, Otake H. Efficacy of the erector spinae plane block for lumbar spinal surgery: a retrospective study. Asian Spine J. (2018) 13:254–7. doi: 10.31616/asj.2018.0114
17. Singh S, Choudhary NK, Lalin D, Verma VK. Bilateral ultrasound-guided erector spinae plane block for postoperative analgesia in lumbar spine surgery: a randomized control trial. J Neurosurg Anesthesiol. (2020) 32:330–4. doi: 10.1097/ANA.0000000000000603
Keywords: erector spinae plane block, dexmedetomidine, multimodal analgesia, lumbar surgery, pain management
Citation: Coppolino F, Sansone P, Porfidia C, Passavanti MB, Pota V, Giaccari LG, Aurilio C and Pace MC (2023) The effect of ultrasound-guided erector spinae plane block combined with dexmedetomidine for postoperative pain management in lumbar spine surgery: A case-based discussion. Front. Anesthesiol. 2:984225. doi: 10.3389/fanes.2023.984225
Received: 01 July 2022; Accepted: 18 January 2023;
Published: 03 March 2023.
Edited by:
Sabry Ayad, Cleveland Clinic, United StatesReviewed by:
Abhijit Nair, Ministry of Health, OmanKe Peng, The First Affiliated Hospital of Soochow University, China
Copyright © 2023 Coppolino, Sansone, Porfidia, Passavanti, Pota, Giaccari, Aurilio and Pace. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Francesco Coppolino, francesco.coppolino@unicampania.it
 Francesco Coppolino
Francesco Coppolino Pasquale Sansone
Pasquale Sansone Carmela Porfidia
Carmela Porfidia  Vincenzo Pota
Vincenzo Pota Luca Gregorio Giaccari
Luca Gregorio Giaccari