Patient-centered perspectives on perioperative care
- 1NorthStar Anesthesia, Irving, TX, United States
- 2Department of Anesthesiology, Wayne State University, Detroit, MI, United States
- 3Outcomes Research Consortium, Cleveland, OH, United States
- 4Central Michigan University College of Medicine, Saginaw, MI, United States
- 5Medical College of Wisconsin Affiliated Hospitals, Milwaukee, WI, United States
Introduction: The collection and evaluation of patient-reported outcomes is essential to the development of patient and family centered care. Current patient surveying techniques are limited by delayed response times and restriction to specific health systems. The use of random-domain intercept technology (RDIT), by Real-Time Interactive World-Wide Intelligence (RIWI, Toronto, ON, Canada) mitigates current barriers by creating a dynamic real-time feedback environment and providing a mass sampling technique.
Methods: RDIT was employed to survey a wide sample of respondents across the United States (US). Respondents who self-identified as having had a surgical procedure or cared for someone having a surgical procedure were included in the analysis.
Results: 1,004 participants completed the survey and answered questions regarding demographics, perioperative details, sentiments on postoperative recovery, postoperative clinical endpoints, sentiments on healthcare professionals, and opinions on future surgical care.
Discussion: The results of this cross-sectional study identified areas with potential for improvement in the patient perioperative experience that could improve the patient experience. This novel use of RDIT provided a valuable tool for real-time feedback and mass sampling allowing the creation of a dynamic healthcare environment that fosters timely and targeted improvements to patient experiences and outcomes.
1 Introduction
In patient-centered and family-centered care, major components in a patient’s care plan include personal beliefs, fears, and opinions. While previous medical decision-making emphasized accurate diagnosis and treatments, the evolution towards patient and family-centered care requires incorporating specific patient satisfaction measures to improve healthcare outcomes (1). Currently, US-based patient satisfaction surveys have been collected using the Press Ganey and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) surveys (2).
The Press Ganey survey is a model used to survey patients on their level of satisfaction when interacting with their physician or other healthcare provider. By collecting insight on a patient's attitude towards their healthcare providers, the latter can make changes to the environment to incite positive change (2). The HCAHPS survey system was the first standardized national patient surveying system to be developed and implemented in the US. The goal of HCAHPS is to collect information on patient insight regarding their most recent hospital admission, and includes questions about how patients viewed their interaction with all hospital staff (2).
While the Press Ganey and HCAHPS survey systems have identified opportunities to improve patient care and outcomes, there are limitations that prevent a more dynamic evolution from occurring. HCAHPS surveys are mailed out to randomly selected patients anywhere between 48 h to six weeks post-discharge. The variability in survey distribution may result in deferred patient-reported responses which ultimately could cause a delay in action taken by the health system to improve patient care (3). The Press Ganey survey system has been utilized across many healthcare systems, but lacks nationwide standardization and usage (2).
Real-Time Interactive World-Wide Intelligence (RIWI) is a commercial company utilizing random-domain intercept technology (RDIT) that shows promise when used to collect patient-reported outcomes on perioperative experiences. RDIT presents survey opportunities to random individuals while on a connected internet browser. By utilizing RDIT, patient surveys can be distributed on a national scale, with no restriction by geographical barriers. However, it is limited to those with access to the internet and may not reach all potentially relevant populations. The electronically distributed survey also allows for real-time feedback and responses to be collected which mitigates delays caused by paper surveys. The electronic distribution method allows healthcare systems to quickly identify negative contributors to a patient’s experience and promote changes to be implemented in a time-efficient manner.
Hitherto, this technology has been successfully implemented to gauge population sentiments on a variety of topics in politics, public health, and governmental initiatives (3–6). This novel use of RIWI’s surveying methodologies allows healthcare providers across institutions to gain more patient insight and evolve in the direction of patient-centered care and improved patient outcomes. This paper aims to investigate the use of RDIT as a platform to survey and collect patient-reported outcomes on perioperative care across the United States.
2 Materials and methods
We developed a questionnaire to be administered to individuals who self-reported having had surgery or cared for someone who did during the study time frame. Study data was collected from United States residents aged 18 and up through a cross-sectional survey. RIWI (RIWI Corp, Toronto, ON, Canada, https://riwi.com/) (7) was employed via the use of patented RDIT to distribute the surveys to participants. RDIT allows the survey to be accessed on any electronic device with web-browser capabilities. When an individual browsing the web accesses an inactive web domain, RIWI uses RDIT to present the participant with the opportunity to complete a survey. The individual is presented with the consent and anonymity statements and they can opt-out of the survey at any time without consequence. There are no incentives or rewards for completing a survey and there are no consequences for choosing not to complete or abandoning a survey. This study was designated as IRB exempt with the following designation number “WSU IRB HPR Number: 2023 126”.
RIWI utilizes application programs, closed website domains, and public internet pages to collect relevant information in the form of online surveys. This technology does not collect personal identifiable information but does allow for geographical information along with demographic information the respondent provides to be collected. Because of the vast number of access points, diverse populations across the globe are able to be reached while maintaining responder anonymity. In this study, variables collected regarding our perioperative experience questionnaire included age, gender, ethnicity, highest level of education, emergent or elective surgery, type of procedure (joint, abdominal, thoracic, or neurological surgery), procedure location, plan of care postoperatively, patient attitudes and perceptions of various members of their care team, satisfaction with return to normal functioning, pain after their procedure, pain medicine requirements, postoperative nausea and vomiting, and most important information regarding their procedure. Only surveys that were fully completed were eligible for variable analysis; if a participant chose not to complete the survey, their responses were not advanced to the data pool. The survey remained available online until a total of at least 1,000 completes was obtained.
All study data was obtained in both raw format and a weighted format corresponding to national population numbers derived from census data. Weighting was applied to age and gender as per the US Census Bureau projections, generated based on the most recent national census data available for the US. Respondent weight values were generated post-stratification using a raking algorithm. If required, custom weighting may be possible (8). The application provides statistical analysis using Pearson's chi-square statistic and the p-value for the hypothesis test of independence of the observed frequencies in the contingency table (from weighted cross tabulation). The expected frequencies are computed based on the marginal sums under the assumption of independence (8). Numerical results were rounded to the nearest digit.
3 Results
A total of 2,373 unique users began the survey, and 1,004 (42.3%) of those users completed the survey in its entirety. The respondents who began answering questions, but did not wish to complete the survey could opt to end the survey at any stage.
3.1 Demographics
Among the 2,373 respondents, gender was closely represented with 44% being female (51% weighted). The largest age proportion was 16–35 year olds (combined 51%, 31% weighted), and the most represented race was white (38%, 43% weighted) as other races represented 4%–15% each (4%–14% weighted). The highest level of education was primary school for 20% (20% weighted) of participants, master’s degree or higher for 30% (30% weighted), and a range between 12%–20% (12%–20% weighted) for educational level in between (Figure 1).

Figure 1. Demographics (unweighted). Data represents all 2,373 respondents. Numerical results were rounded to the nearest digit.
For the remainder of the responses, the survey was closed when 1,000 completed questionnaires were obtained (4 additional responses were captured while the survey was being closed). By design, respondents were directed down a decision tree based on their responses. Those who had had a surgical procedure within the prior 10 years vs. those who had not were presented with relevant questions. Hence, the questions differed in the total number of responses (Figure 2). At the end of the survey, all 1,004 respondents were again presented with opinion-based questions.
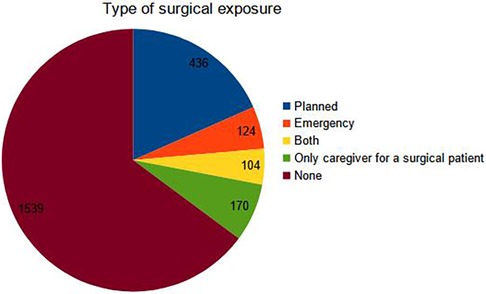
Figure 2. Respondent experience as a surgical patient or caregiver. Data represents all 2,373 respondents. Numerical results were rounded to the nearest digit.
3.2 Perioperative details
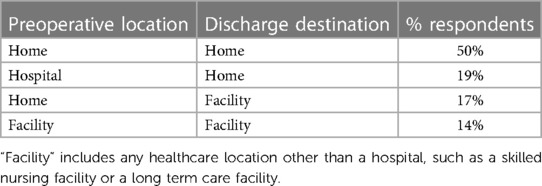
Half of the respondents reported having surgery in a hospital setting, with abdominal and joint surgeries representing about a third of the total number of procedures each (Figure 3). Half of the respondents reported presenting to surgery from home and being discharged back home (Table 1).
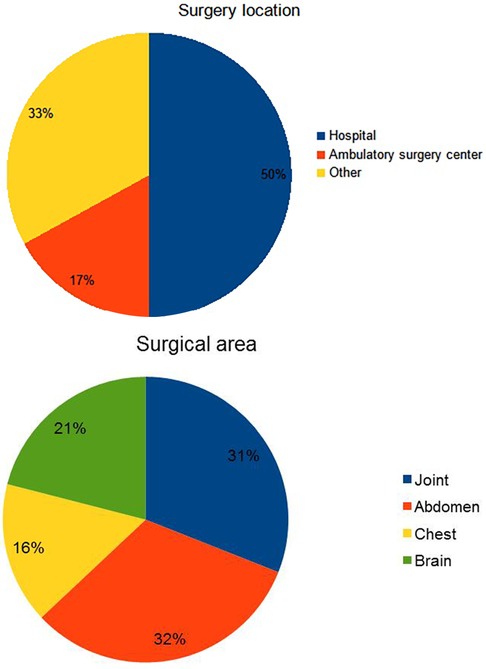
Figure 3. Perioperative details. Data includes respondents who were surgical patients or caregivers. Numerical results were rounded to the nearest digit.
3.3 Sentiments on postoperative recovery
The majority of respondents (38%), reported the recovery being “as expected”, while a combined 37% reported better than expected and a combined 25% reported worse than expected recovery. A combined two thirds of the respondents agreed that they had received adequate information to prepare them for recovery, while a combined one third reported disagreeing with that statement (Figure 4).
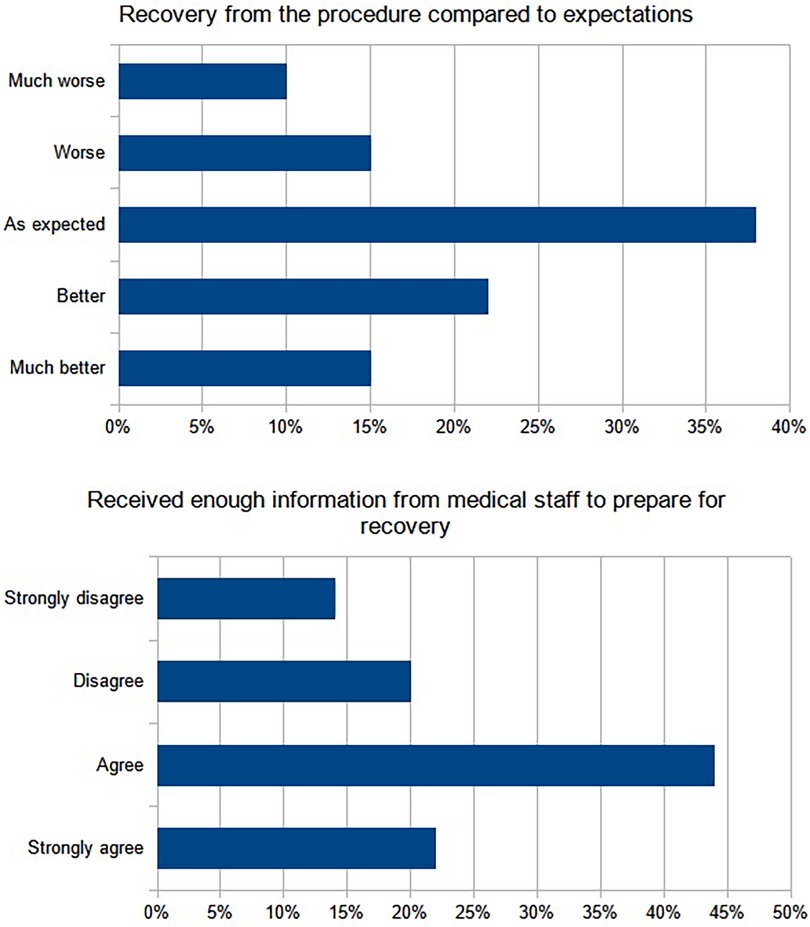
Figure 4. Sentiments on postoperative recovery. Data includes respondents who were surgical patients or caregivers. Numerical results were rounded to the nearest digit.
3.4 Postoperative clinical endpoints
About a third of the respondents reported significant postoperative pain lasting 1 week to 1 month after the procedure, while a combined 27% reported postoperative pain lasting more than 3 months. Analgesic intake was reported for less than 1 week in 30% of respondents, but more than 3 months in a combined 21%. Significant postoperative nausea or vomiting was reported to be less than 1 week by 29% of respondents. Return to baseline or better level of functioning was reported by the majority of patients (40%) to take a week or less, while a combined 23% reported more than 3 months (Figure 5).
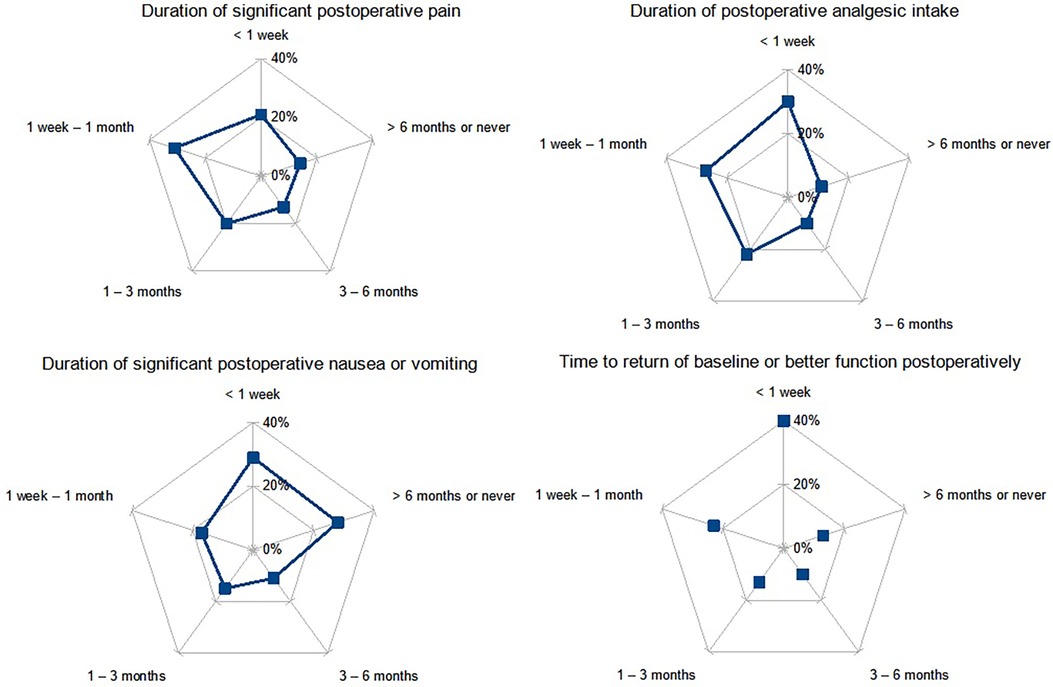
Figure 5. Postoperative clinical endpoints. Data includes respondents who were surgical patients or caregivers. Numerical results were rounded to the nearest digit.
3.5 Sentiments on healthcare professionals
Participants were asked to provide their sentiments on the healthcare teams taking care of them before, during, and after the surgical procedure. The recovery nursing teams (23%), postoperative ward care nursing teams (23%), and surgical teams (20%) were the most remembered. In a combined 69% of the cases, those teams left an overall positive impression while that impression was reported as “very negative” in 11%. When asked about the anesthesia team taking care of them, about three quarters of respondents reported the impression that the team seemed well-prepared to take care of them and 10% reported the impression that the team was “definitely not” prepared. A small fraction of respondents (6%) did not recall their anesthesia team (Figure 6).
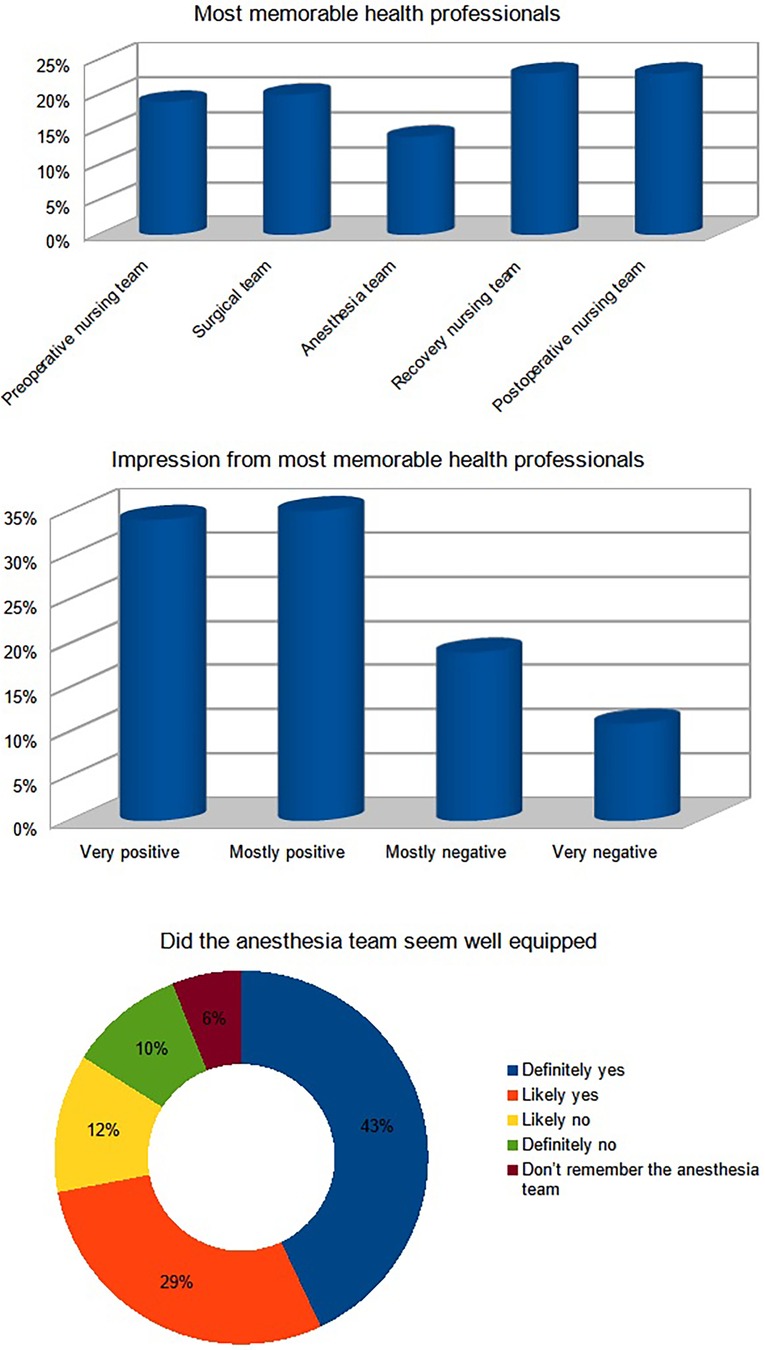
Figure 6. Sentiments on healthcare professionals. Data includes respondents who were surgical patients or caregivers. Numerical results were rounded to the nearest digit.
3.6 Participant opinions on future surgical care
The last part of the survey collected 1,004 responses. In it, respondents were asked to provide their opinion on preparation for future surgical procedures as viewed by a patient. A combined 60% of respondents reported it would be important to know and like the anesthesia team while a combined 40% reported it would not be important. While some respondents indicated wanting specific information from the anesthesia preoperatively, 54% did not wish to request any of the presented options. Some respondents agreed that a good way to prepare for a surgical procedure would include education, emotional support, or meeting healthcare representatives, while the majority (57%) did not. A combined 35% of respondents indicated they would prepare for surgery by reading material provided by their healthcare providers or by their own research, 13% indicated they would prefer relaxation and spiritual techniques, and 52% indicated that they would not do anything in particular (Figure 7).
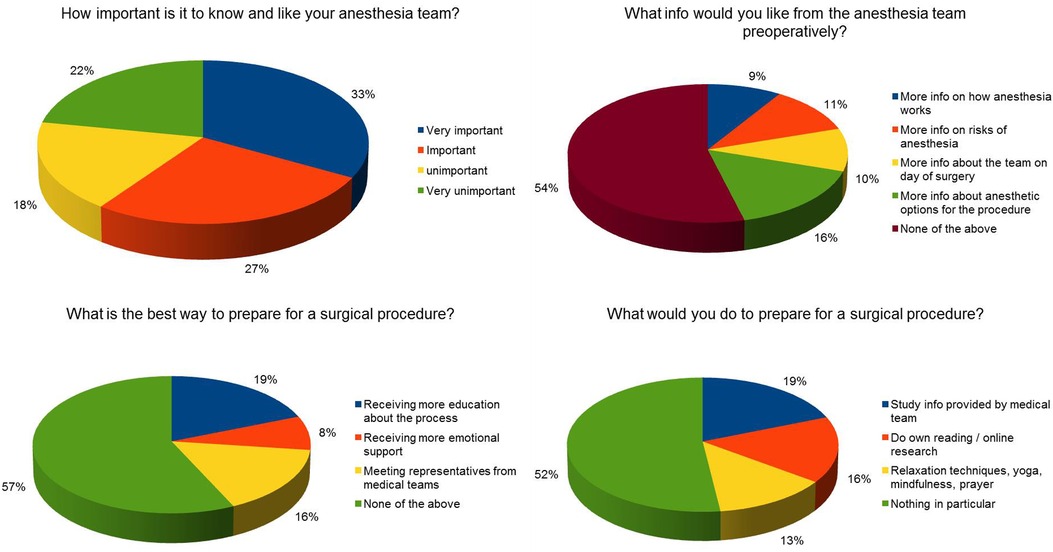
Figure 7. Participant opinions on future surgical care. Data includes respondents who were surgical patients or caregivers. Numerical results were rounded to the nearest digit.
4 Discussion
This report is the first direct clinical survey on perioperative care utilizing RDIT. It is important to note the major differences between this study survey methodology and those of traditional patient surveys, and hence the difference in the interpretation of the results of this study.
Traditional surveys are administered to patients and the percentage of respondents greatly influences the validity of the results. In this study, the survey was distributed to the general population of US-based internet users, and isolated the group who identified as surgical patients or their caregivers. Additionally, traditional surveys are time-consuming and require a relatively larger group of personnel to administer and analyze. Our survey was designed by a core group of clinicians and the entire deployment and analysis phase took three days for 1,004 completed responses. Finally, the majority of current survey data highlights clinical issues from the point of view of the clinician or the medical institution. The aim of this study was to pilot a survey that provided responses from the point of view of the patient.
At the time of data collection, the highest proportion of survey respondents identified themselves as being in the 16–24 year old range. While this may be due to younger individuals being more technologically adept and having more access than individuals from older generations, this resulted in the overall survey responses to be skewed towards the younger age demographic. Regardless of age, the majority respondent choice of the best way to prepare for a surgery, was “none of the above” to all survey questions regarding surgery preparedness. These results suggest a lack of effectiveness in how patient health information is being conveyed. Along with the traditional practice of providing emotional support and effective patient-provider interaction, additional methods may be required to help patients feel more prepared for their procedures.
Regarding postoperative analgesic use, about half of the respondents indicated significant postoperative pain up to 1 month after the surgical procedure, and a similar proportion indicated utilizing analgesics for the same amount. This mirroring of trends indicates that respondents generally received a proportionate and adequate amount of pain medication to effectively control their pain. This may be attributed to recent trends in limiting the use of postoperative analgesics and more awareness on the part of the patient regarding their appropriate use (Figure 5).
When analyzing specific procedure types, the second largest group identified themselves as having undergone joint surgery. Of those, a significant number used pain medications chronically, for over 6 months (data not shown). While most orthopedic surgeries generally report a high rate of surgical success, a significant portion of respondent patients appeared to be chronically dependent on pain medications which has been observed in large population studies of joint replacement patients (9). This study finding suggests that further investigations may be required to differentiate how a “successful” patient outcome defined from a healthcare provider compares to that of the patient's personal perspective.
4.1 Limitations
This study has the known limitations inherent to survey-based research, including selection bias and non-representative sample, where responses may not be generalizable beyond the completed responses. However, this novel use of RDIT and the extrapolation to Census data helps mitigate some of those limitations. The low ratio of completed responses to contacted survey respondents is traditionally a major limitation of survey based research, but plays less of a role in this study given the methodology described above. Individuals with no internet access and those who were randomly not selected to complete the survey were naturally excluded from the analysis. Due to the study survey questions consisting of multiple choice options, respondents were not able to expand in more detail on their responses when selecting the “none of the above” or “other” survey answer options. Future surveys that provide options with more specific answer choices such as a free response section for patients to write in themselves may eliminate such barriers, but would also mitigate some of the inherent advantages of this study methodology. Due to the novel use of electronics to survey participants, there is a lack of human-to-human interaction when filling out the survey. Some participants may not feel satisfied responding if there is not an empathetic human party that they are directly sharing their reflections with.
5 Conclusion
In conclusion, the use of RDIT as a patient surveying tool provides real-time feedback data and eliminates the lag period to implementing quality improvement initiatives. This patient-centered approach is a novel and significant stride towards identifying and addressing potential areas of dissatisfaction to optimize healthcare delivery. By creating a more patient-friendly engaged environment, patients may become more aware, adherent, and compliant to addressing their healthcare plans, ultimately leading to improved patient outcomes.
RDIT overcomes many of the obstacles observed with traditional surveying methods by providing real-time feedback and expanding geographical reach. As with all surveys, RDIT and survey responses are limited to the number of participants that complete an entire survey as only fully completed surveys are analyzed. While further survey distributions will be required to strengthen the validity of RDIT as a survey method, the scope of information that can be gathered from this type of survey demonstrates the potential of this technology in a healthcare setting.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the [patients/participants OR patients/participants legal guardian/next of kin] was not required to participate in this study in accordance with the national legislation and the institutional requirements. Patients were asked to confirm voluntarily participating in this survey before they were presented with the questions.
Author contributions
WS: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing. KG: Project administration, Writing – original draft, Writing – review & editing. NA-S: Writing – review & editing. LL: Writing – review & editing. GM: Project administration, Writing – review & editing. MJ: Funding acquisition, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank Mariam Harajli MD and Nick Mazur DO for their contributions to the data analysis and identification of significant trends.
Conflict of interest
WS: Edwards Lifesciences: Medical Advisory Board consultant (ended 2022). Takeda Pharmaceuticals: Respiratory Adjudication Committee member, ongoing trial (2023- ). Ether Innovations LLC: founding CEO.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor AT declared a shared parent affiliation with the author WS at the time of review.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ng JHY, Luk BHK. Patient satisfaction: concept analysis in the healthcare context. Patient Educ Couns. (2019) 102(4):790–6. doi: 10.1016/j.pec.2018.11.013
2. Pfeifer GM. Is it time to revise HCAHPS? Am J Nurs. (2019) 119(11):14. doi: 10.1097/01.NAJ.0000605292.00285.d5
3. HCAHPS: Patients’ Perspectives of Care Survey (2021). Available online at: https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/hospitalhcahps (accessed July 26, 2023).
4. Sargent RH, Laurie S, Moncada L, Weakland LF, Lavery JV, Salmon DA, et al. Masks, money, and mandates: a national survey on efforts to increase COVID-19 vaccination intentions in the United States. PLoS One. (2022) 17(4):e0267154. doi: 10.1371/journal.pone.0267154
5. Tandon S, Vishwanath T. Capturing Sensitive Information from Difficult-to-Reach Populations: Evidence from a Novel Internet-based Survey in Yemen. JEL Classification: D12; I31; I38; O10; O53 (2022).
7. RIWI Corp. Available online at: https://riwi.com/ (accessed July 26, 2023).
Keywords: perioperative, patient-reported, patient-centered, survey, random-domain intercept technology, patient sentiment, perioperative quality improvement
Citation: Saasouh W, Ghanem K, Al-Saidi N, LeQuia L, McKelvey G and Jaffar M (2024) Patient-centered perspectives on perioperative care. Front. Anesthesiol. 3:1267127. doi: 10.3389/fanes.2024.1267127
Received: 26 July 2023; Accepted: 18 March 2024;
Published: 2 April 2024.
Edited by:
Alparslan Turan, Cleveland Clinic, United StatesReviewed by:
Firoozeh Madadi, Shahid Beheshti University of Medical Sciences, IranAveek Jayant, Homi Bhabha Cancer Hospital and Research Centre, India
© 2024 Saasouh, Ghanem, Al-Saidi, LeQuia, McKelvey and Jaffar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wael Saasouh wsaasouh@dmc.org
 Wael Saasouh
Wael Saasouh Kristina Ghanem
Kristina Ghanem Neil Al-Saidi
Neil Al-Saidi Lindsey LeQuia5
Lindsey LeQuia5