Repeated sudden sensorineural hearing loss with intralabyrinthine hemorrhage in a patient with Glanzmann thrombasthenia: case report
- 1National Institute of Sensory Organs, National Hospital Organization Tokyo Medical Center, Tokyo, Japan
- 2Department of Otolaryngology, National Hospital Organization Tokyo Medical Center, Tokyo, Japan
- 3Department of Otolaryngology, Head and Neck Surgery, Keio University School of Medicine, Tokyo, Japan
- 4Department of Otolaryngology, Head and Neck Surgery, Tokai University School of Medicine, Isehara, Japan
Glanzmann thrombasthenia is a rare congenital bleeding disorder. Recent advances in magnetic resonance imaging (MRI) have made it possible to detect micro-lesions in the inner ear, such as intralabyrinthine hemorrhage, a rare disorder that causes sudden hearing loss or vertigo. We present a case of 62-year-old female with Glanzmann thrombasthenia. Over a 10-year period, the patient had experienced seven episodes of left-sided sudden hearing loss (SHL). Although each episode was treated with steroids, her left-ear hearing level gradually worsened. Head T1-weighted MRI performed 27 days after onset of the sixth SHL episode showed hyperintense lesions throughout the left inner ear. The patient was diagnosed with intralabyrinthine hemorrhage. When a patient with hematologic disease or who is on anticoagulant therapy presents with SHL or vertigo, T1-weighted MRI should be performed within 1 month of symptom onset to confirm intralabyrinthine hemorrhage.
1 Introduction
Glanzmann thrombasthenia is a rare bleeding disorder caused by inherited deficiencies in platelet glycoprotein (Grainger et al., 2018). Its most common clinical presentation is chronic ease of bruising, epistaxis, and gum bleeding (Nurden et al., 2021). Intracranial hemorrhage is present in 1%−2% of cases (Botero et al., 2020). In this report, we present a unique patient with thrombasthenia.
2 Case presentation
A 62-year-old female presented with a sensation of fullness in her left ear. The patient was diagnosed with Glanzmann thrombasthenia after experiencing several incidences of otorrhagia at the age of 1 year. Platelet aggregation tests showed aggregation with ristocetin but not with adenosine disphosphoric acid (ADP), collagen, or epinephrine. Flow cytometry showed no expression of CD41 (glycoprotein IIb) and normal expression of CD61 (glycoprotein IIIa) and CD42b (glycoprotein Ibα) on the platelet surface. The patient's identical twin sister also has thrombasthenia. The patient had visited a gastroenterologist regularly for hepatitis C. Pure tone audiometry (PTA) of the patient revealed left-sided sudden sensorineural hearing loss (SSNHL). The patient received a 12-day treatment consisting of tapered oral administration of prednisolone (15 mg/day). On day 27, the patient underwent head magnetic resonance imaging (MRI). T1-weighted (T1-W) and T2-fluid attenuated inversion recovery (T2-FLAIR) images revealed a slight hyperintense lesion in the middle turn of the left cochlea. T2-weighted (T2-W) MRI images showed no significant findings bilaterally in the inner ears.
Over a 10-year period, the patient experienced recurrences of left SSNHL six times. Although each episode was treated with steroids, her left-ear PTA gradually worsened, eventually resulting in profound hearing loss on the left side (Figure 1; Table 1). Serological exam for autoimmune disorder was not performed because there were no symptoms of suspected autoimmune disorder such as joint symptoms or skin manifestations.
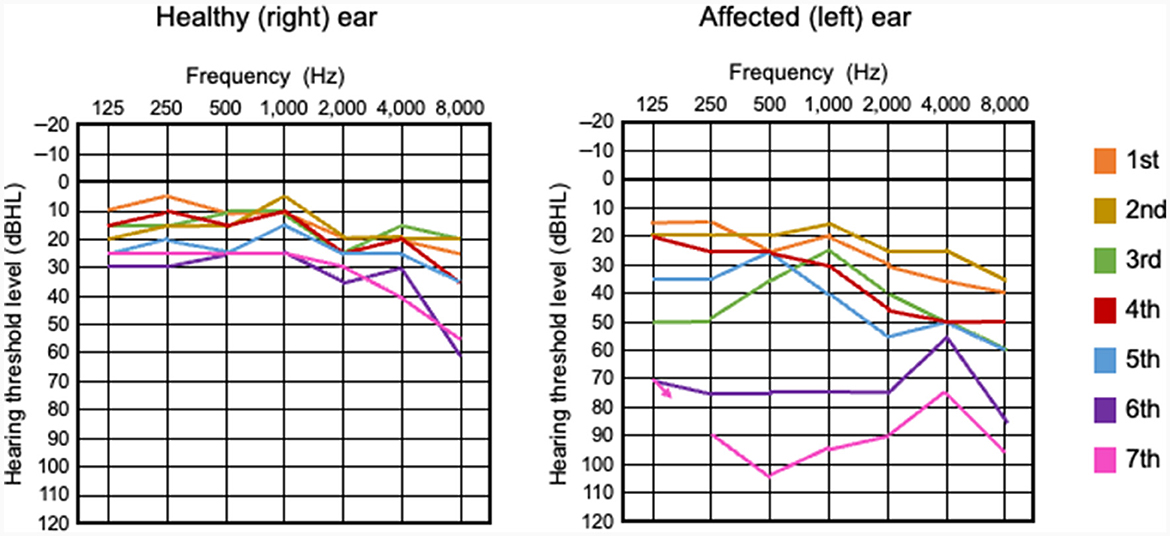
Figure 1. Pure tone audiometry for 62-year-old patient with Glanzmann thrombasthenia. Hearing levels of the unaffected right ear (left panel) and the affected left ear (right panel) for the patient's seven episodes of sudden sensorineural hearing loss (SSNHL) recurring over a 10-year period. While hearing levels of the healthy right ear slightly worsened with age, hearing levels of the affected left ear worsened at all tested frequencies over time and the patient experienced profound SSNHL. dBHL, decibel hearing level; fuchsia-colored arrow (right panel) indicates no response at the maximum sound pressure of the audiometer in the affected left ear.
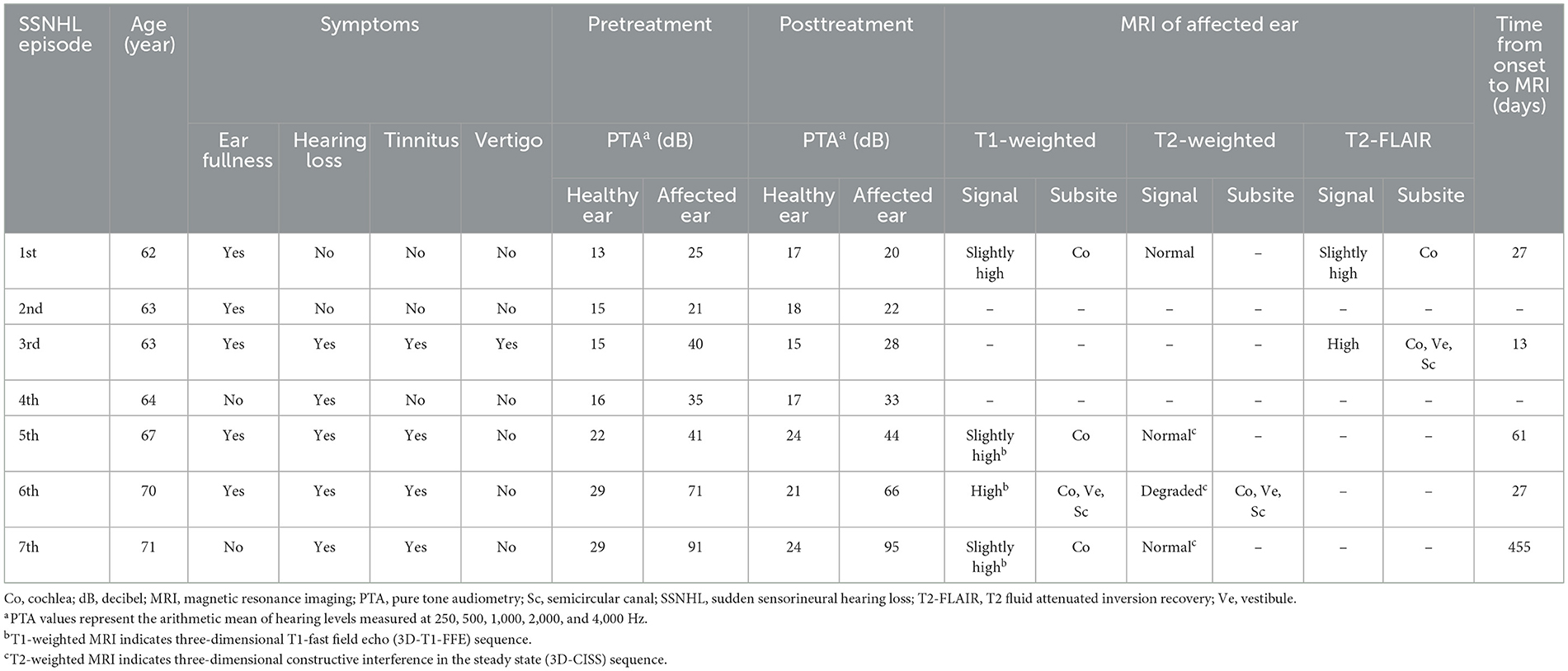
Table 1. Clinical and audiological characteristics of each SSNHL episode in patient with Glanzmann thrombasthenia.
During the sixth SSNHL episode, her left hearing thresholds were greatly elevated. MRI performed 27 days after onset of the sixth episode showed hyperintense lesions throughout the left inner ear, including the cochlea, vestibule, and semicircular canal (Figure 2A). Three-dimensional T1-fast field echo (3D-T1-FFE) sequence imaging was used for this assessment. Magnetic resonance cisternography (heavy T2-W imaging) (Mamata et al., 1998) obtained with three-dimensional constructive interference in the steady state (3D-CISS) showed signal degradation throughout the affected inner ear (i.e., left ear) compared to the unaffected inner ear (Figure 2B). The patient was diagnosed with intralabyrinthine hemorrhage. In this patient, we believe that Glanzmann thrombasthenia may have caused repeated SSNHL due to repeated intralabyrinthine hemorrhage. All scans were performed at 1.5 Tesla MRI.
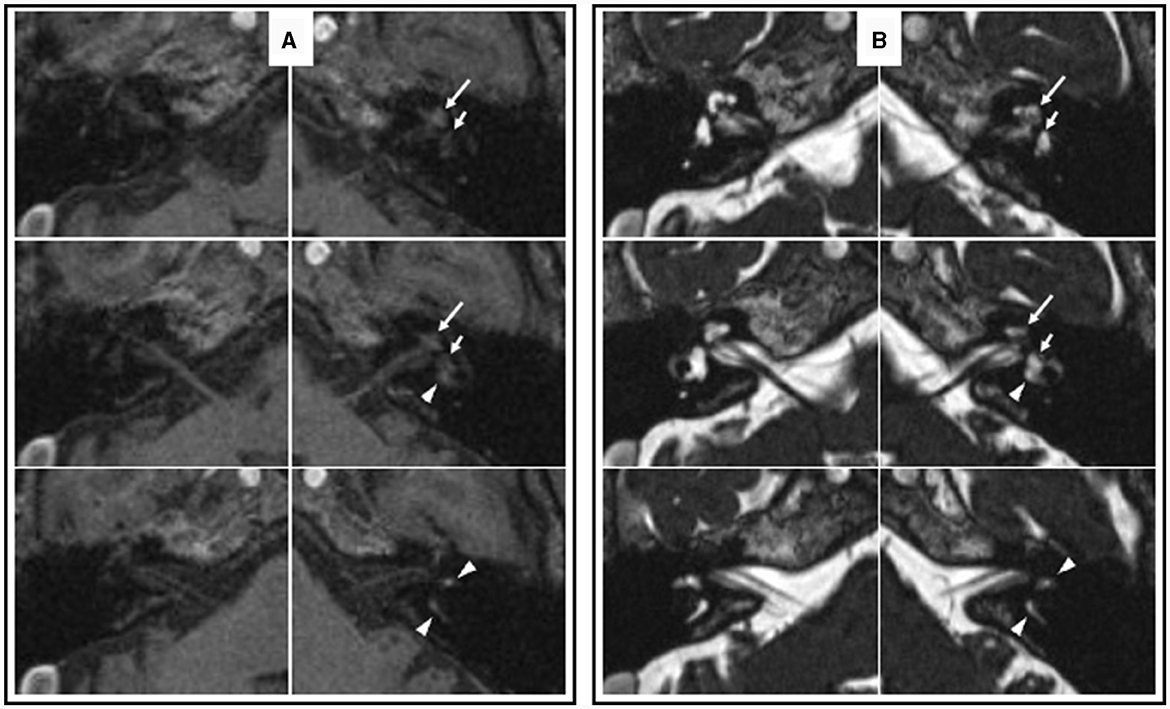
Figure 2. Axial magnetic resonance images acquired during the sixth SSNHL episode in the patient with Glanzmann thrombasthenia. (A) 3D T1-FFE images show increased signal intensity throughout the left labyrinth, including the cochlea (long arrow), vestibule (short arrow), and semicircular canals (arrowhead). (B) 3D-CISS images show slight signal degradation throughout the left labyrinth, including the cochlea (long arrow), vestibule (short arrow), and semicircular canals (arrowhead). 3D-T1-FFE, three-dimensional T1-fast field echo. 3D-CISS, three-dimensional constructive interference in the steady state.
At the age of 72 years, the patient underwent a simultaneous comprehensive vestibular assessment (SCVA) to evaluate the function of the whole inner ear. The caloric test and video head impulse test (vHIT) showed left-sided canal paresis. Cervical vestibular evoked myogenic potentials (cVEMPs) and ocular vestibular evoked myogenic potentials (oVEMPs) on the left-side were undetectable. Although the patient did not report vertigo or dizziness, SCVA confirmed the presence of left vestibular dysfunction, suggesting that vestibular compensation was present.
3 Discussion
Recent advances in MRI have made it possible to detect micro-lesions in the inner ear, such as intralabyrinthine hemorrhage. Although the 2019 Clinical Practice Guideline: Sudden Hearing Loss (Update) recommends head MRI or auditory brainstem responses (ABR) for evaluating retrocochlear pathology (e.g., vestibular schwannoma) in patients with SSNHL (Chandrasekhar et al., 2019), the guideline did not specify the time frame within which MRI or ABR should be performed. On T1-W and T2-FLAIR MRI images, intralabyrinthine hemorrhages appear as areas of high signal intensity; however, on T2-W MRI images, the signal intensity of intralabyrinthine hemorrhages can vary (Cervantes and Barrs, 2015). T1-W imaging is essential to identify intralabyrinthine hemorrhage (Cervantes and Barrs, 2015). Lammers et al. (2019) recommended performing T1-W MRI and 3D-FLAIR MRI at 3-14 days after symptom onset to detect intralabyrinthine hemorrhage. However, as with the present case, MRI may be able to detect intralabyrinthine hemorrhage within 1 month of symptom onset. The period of time after onset at which intralabyrinthine hemorrhage is detectable on MRI may vary depending on the severity of the hemorrhage.
Intralabyrinthine hemorrhage is reported to be associated with sickle cell disease, chronic myelomonocytic leukemia, Von Hippel-Lindau syndrome, viral labyrinthitis, tumor, cholesterol granuloma, lupus erythematosus, trauma, coagulopathy (e.g., use of anticoagulant medications), among other diseases and conditions (Naganawa et al., 2009; Cervantes and Barrs, 2015). Schlegelberger et al. (1986) reported a case of hearing loss and triphalangia of the thumbs in a 22-year-old woman with Glanzmann thrombasthenia, but no information on the onset and the characteristics of the hearing loss was described (Corazzi et al., 2023). We are unaware of any reports of intralabyrinthine hemorrhage in patients with Glanzmann thrombasthenia. Even when the onset of hearing loss is not obvious, Glanzmann thrombasthenia might be included in the differential diagnosis of hearing loss.
To the best of our knowledge, there have been no reports of intralabyrinthine hemorrhage with repeated ipsilateral SSNHL occurring over a 10-year period. A cautionary note is that the definition of SSNHL in this case differs from the 2019 Clinical Practice Guideline (Chandrasekhar et al., 2019). SSNHL was defined as an audiogram at the onset of each episode having one of the following two patterns: (1) if the hearing loss was first or the previous hearing loss was cured, the interaural difference was ≥15 dB at one or more frequencies. (2) If the previous hearing loss was not cured, the hearing thresholds of one or more frequencies on the affected side increased by 15 dB or more compared to the previous stable hearing thresholds on the affected side. In our patient, hemorrhage may have caused the microstructure of the inner ear to become increasingly fragile, resulting in repeated episodes intralabyrinthine hemorrhage.
4 Conclusion
When a patient with hematologic disease or who is on anticoagulant therapy presents with SSNHL, T1-W MRI and 3D-FLAIR MRI should be performed within 1 month of symptom onset to confirm intralabyrinthine hemorrhage. Examination for retrocochlear pathology should also be considered.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
NT: Writing – original draft. KW: Conceptualization, Writing – review & editing. HO: Conceptualization, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. A Grant-in-Aid for Scientific Research (C) (21K09574) from the Japan Society for Promotion of Science supported this work.
Acknowledgments
We thank Dr. Azumi Miyazawa for her advice on interpreting the MRI images.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Botero, J. P., Lee, K., Branchford, B. R., Bray, P. F., Freson, K., Lambert, M. P., et al. (2020). Glanzmann thrombasthenia: genetic basis and clinical correlates. Haematologica 105, 888–894. doi: 10.3324/haematol.2018.214239
Cervantes, S. S., and Barrs, D. M. (2015). Sudden sensorineural hearing loss associated with intralabyrinthine hemorrhage. Otol. Neurotol. 36, e134–e135. doi: 10.1097/MAO.0000000000000474
Chandrasekhar, S. S., Tsai Do, B. S., Schwartz, S. R., Bontempo, L. J., Faucett, E. A., Finestone, S. A., et al. (2019). Clinical practice guideline: sudden hearing loss (update). Otolaryngol. Head Neck Surg. 161(1_suppl), S1–S45. doi: 10.1177/0194599819859885
Corazzi, V., Migliorelli, A., Bianchini, C., Pelucchi, S., and Ciorba, A. (2023). Hearing loss and blood coagulation disorders: a review. Hematol. Rep. 15, 421–431. doi: 10.3390/hematolrep15030043
Grainger, J. D., Thachil, J., and Will, A. M. (2018). How we treat the platelet glycoprotein defects; Glanzmann thrombasthenia and Bernard Soulier syndrome in children and adults. Br. J. Haematol. 182, 621–632. doi: 10.1111/bjh.15409
Lammers, M. J. W., Young, E., Fenton, D., Lea, J., and Westerberg, B. D. (2019). The prognostic value and pathophysiologic significance of three-dimensional fluid-attenuated inversion recovery (3D-FLAIR) magnetic resonance imaging in idiopathic sudden sensorineural hearing loss: a systematic review and meta-analysis. Clin. Otolaryngol. 44, 1017–1025. doi: 10.1111/coa.13432
Mamata, Y., Muro, I., Matsumae, M., Komiya, T., Toyama, H., Tsugane, R., et al. (1998). Magnetic resonance cisternography for visualization of intracisternal fine structures. J. Neurosurg. 88, 670–678. doi: 10.3171/jns.1998.88.4.0670
Naganawa, S., Ishihara, S., Iwano, S., Sone, M., and Nakashima, T. (2009). Detection of presumed hemorrhage in the ampullar endolymph of the semicircular canal: a case report. Magn. Reson. Med. Sci. 8, 187–191. doi: 10.2463/mrms.8.187
Nurden, P., Stritt, S., Favier, R., and Nurden, A. T. (2021). Inherited platelet diseases with normal platelet count: phenotypes, genotypes and diagnostic strategy. Haematologica 106, 337–350. doi: 10.3324/haematol.2020.248153
Keywords: inner ear, hearing loss, hemorrhage, magnetic resonance imaging, thrombasthenia
Citation: Tsuzuki N, Wasano K and Ozawa H (2024) Repeated sudden sensorineural hearing loss with intralabyrinthine hemorrhage in a patient with Glanzmann thrombasthenia: case report. Front. Audiol. Otol. 2:1351382. doi: 10.3389/fauot.2024.1351382
Received: 12 December 2023; Accepted: 29 January 2024;
Published: 20 February 2024.
Edited by:
Sofia Waissbluth, Pontificia Universidad Católica de Chile, ChileReviewed by:
Paul Hinckley Delano, University of Chile, ChileLuminita Radulescu, Grigore T. Popa University of Medicine and Pharmacy, Romania
Copyright © 2024 Tsuzuki, Wasano and Ozawa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Koichiro Wasano, wasano@a5.keio.jp
 Nobuyoshi Tsuzuki1,2,3
Nobuyoshi Tsuzuki1,2,3  Koichiro Wasano
Koichiro Wasano Hiroyuki Ozawa
Hiroyuki Ozawa