Approaches to Biofunctionalize Polyetheretherketone for Antibacterial: A Review
- 1Department of Bone and Joint Surgery, Renji Hospital, School of Medicine, Shanghai Jiaotong University, Shanghai, China
- 2Department of Orthopedics, Renji Hospital, School of Medicine, Shanghai Jiaotong University, Shanghai, China
Due to excellent mechanical properties and similar elastic modulus compared with human cortical bone, polyetheretherketone (PEEK) has become one of the most promising orthopedic implant materials. However, implant-associated infections (IAIs) remain a challenging issue since PEEK is bio-inert. In order to fabricate an antibacterial bio-functional surface, modifications of PEEK had been widely investigated. This review summarizes the modification strategies to biofunctionalize PEEK for antibacterial. We will begin with reviewing different approaches, such as surface-coating modifications and controlled release of antimicrobials. Furthermore, blending modifications and 3D printing technology were discussed. Finally, we compare the effects among different approaches. We aimed to provide an in-depth understanding of the antibacterial modification and optimize the design of the PEEK orthopedic implant.
Introduction
The ideal orthopedic implant should possess good histocompatibility, good mechanical properties close to bone tissue, good bone–implant integration, and adequate antibacterial property (Liu et al., 2019). Currently, titanium is widely used in orthopedic clinical implants, followed by stainless steel, Mg, and other metals (Kim et al., 2020; Yang et al., 2020). However, the stress shielding effect of metal implants cannot be solved so far, which eventually leads to bone loss and loosening of implants (Heary et al., 2017; Mishchenko et al., 2020). Therefore, it is of great clinical and scientific significance to develop novel orthopedic implant materials. Among these, polyetheretherketone (PEEK) is a widely explored alternative orthopedic implant material. Since it was approved as a medical implant material by the FDA in the late 1990s, many researchers have paid attention to its application prospects in the field of orthopedic (Panayotov et al., 2016).
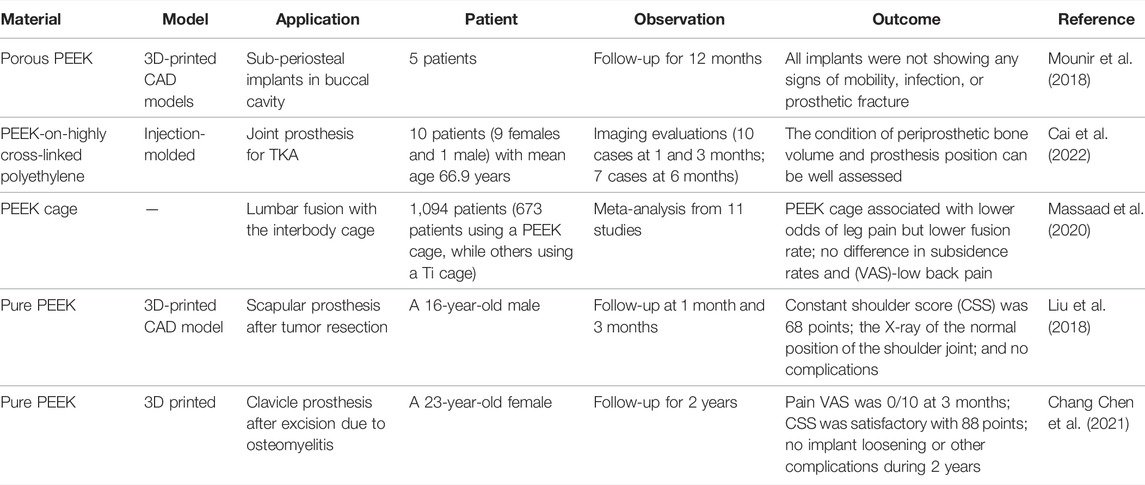
The average rate of orthopedic implant-associated infections (IAIs) is about 2–5%, even up to 30% of open fractures (Kuehl et al., 2019), which bring serious physical and psychological trauma to patients and generate a lot of medical expenses (Wang and Tang, 2019). Hip and knee arthroplasty has been a very mature technology in the treatment of terminal arthritis. Periprosthetic joint infections (PJIs) are the most serious complication, although the incidence is not high; it can be divided into acute and chronic infection based on the choice of clinical treatment (Otto-Lambertz et al., 2017). Whether the biofilm formatted on the surface of the prosthesis is one of the important factors determining acute or chronic infection needs further investigation. Compared with the treatment of acute infection by antibiotics, the treatment of chronic infection is more difficult. Two-stage revision is still the gold standard at present (Matar et al., 2021). PJI can lead to prosthesis loosening and dislocation, etc., and even if the infection is controlled by treatment, the long-term reoperation rate of joint revision is higher than that of uninfected patients (Clauss et al., 2020). In IAI, the most commonly cultured pathogens are Gram-positive; many other microorganisms can also be found (Figure 1). One of the reasons for the poor prognosis of IAI is failing to identify the pathogen species of infection at the first time. In addition, granulation tissue generated around the implant forms the immune depression area, which is prone to infection and colonization (Arciola et al., 2018). This is due to biofilm formation and then diffuses infection of surrounding tissues resulting in poor response to antibiotic therapy and may eventually lead to loosening or even shedding of the implants (Naik et al., 2015). Single-celled bacteria form biofilm through four stages: bacterial surface attachment, small colony formation, bacterial biofilm maturation, and dispersion separation (Bjarnsholt, 2013). The bacteria in the multilayer form of biofilm are in a static or dormant period, so they can resist clinical antibiotic treatment and phagocytes of the immune system (Zimmerli and Sendi, 2017; Masters et al., 2019). Therefore, the formation of bacterial biofilm will seriously affect the role of antibiotics and make treatment difficult. Until now, the incidence rate of IAI has not declined significantly even with strict aseptic techniques and application of broad-spectrum antibiotics (Wang and Tang, 2019). The modifications of implant materials to inhibit the initial bacterial adhesion and the formation of biofilms have great prospects in reducing the rate of IAI. Seeking new antibacterial implant materials is another way (Jiao et al., 2021), which requires abundant research resources. As new material needs to meet the requirements of biomechanics, histocompatibility, and osseointegration, meanwhile, it needs stable chemical properties, easy plasticity, low cost, and convenience for mass production. Consequently, surface biofunctionalization including chemical and physical modifications by antibacterial nanoparticles or compounds of existing approved materials to achieve antibacterial properties is a more efficient approach.
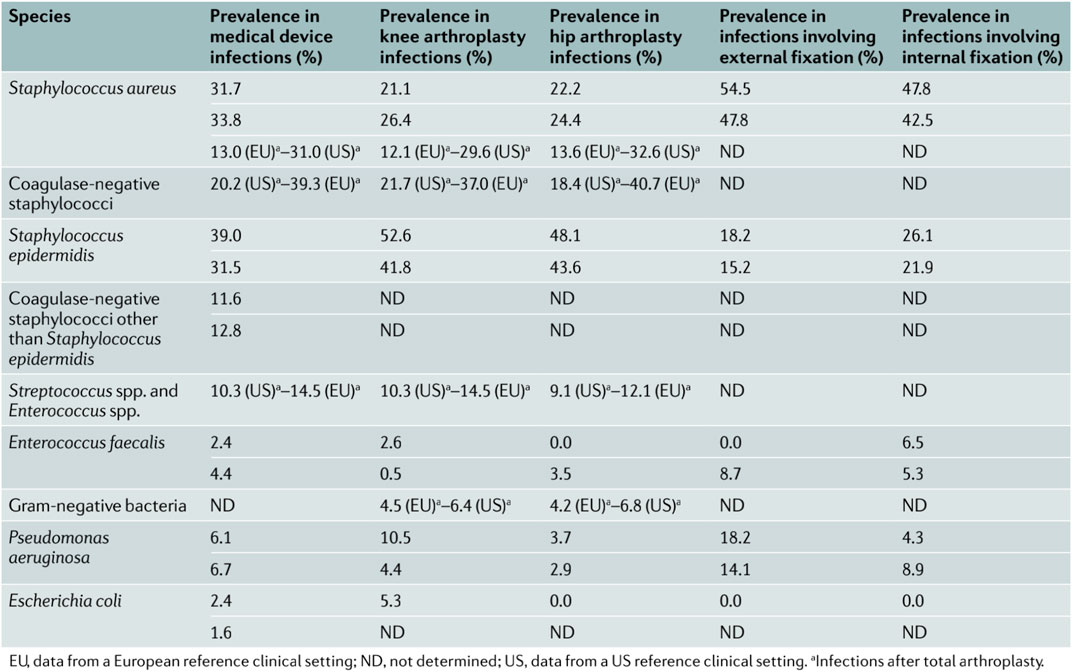
FIGURE 1. Major bacteria causing implant-associated infections. Reproduced from Arciola et al (2018). Copyright (2018), with permission from Springer Nature.
PEEK is an ideal bone substitute material due to its bio-inert property, safety, non-toxicity, wear-resistance, transmit radiation, strong plasticity, and mechanical properties close to the human cortical bone (Ya-Shum et al., 2018; Ma Z. et al., 2020; He et al., 2021). It had been successfully used as a biomaterial for arthroplasty construction and trauma and dental implant applications (Table 1). However, it also has drawbacks, for example, the unique structure leads to surface hydrophobicity that inhibits protein and cell adhesion (Ji et al., 2020), resulting in poor osseointegration and failure of the implant (Liao et al., 2020). In addition, it is easier to colonize bacteria and form biofilms due to its bio-inert property (Bock et al., 2017). Therefore, to make PEEK more suitable for orthopedic implant materials, it must be biofunctionalized to improve biocompatibility, osseointegration, and antibacterial properties. In recent years, the development of biomaterial modification has been greatly promoted relying on the progress of nanotechnology (Hochella et al., 2019). Modified biomaterials, such as nano-hydroxyapatite, have shown improved osseointegration over micro-hydroxyapatite (Panayotov et al., 2016; Lowe et al., 2020). PEEK also can get better modification effects and less inflammatory reaction due to nanotechnology (Gu et al., 2020). Nowadays, a large number of research studies have been carried out successfully in vitro and in vivo (Torstrick et al., 2018; Chepurnyi et al., 2020; Liu et al., 2020), but there is still a lack of in-depth understanding of the modification of antibacterial properties.
The clinical application of PEEK implants has continuously reported cases of infection (Roman et al., 2014; Chen et al., 2019; Tarallo et al., 2020; Hacherl et al., 2021). In this review, we focused on the antibacterial modification strategies of PEEK. Meanwhile, the biocompatibility and osseointegration are also taken into consideration on that the rapid integration of implant and surrounding tissue being crucial for preventing bacterial adhesion and colonization (Stones and Krachler, 2016). Because the implants cannot be absolutely sterile due to exposure to the air during the operation and there is no guarantee of any microbial colonization in the body for decades, only antibacterial modifications of the implant surface are futile. The formation of bacterial biofilm can be regarded as the competition of adhesion between bacteria and surrounding tissue cells (Subbiahdoss et al., 2009; Busscher et al., 2012), which was called “race for the surface,” as first proposed by Gristina (1987). Ultimately, the objective of this article was to discuss the advantages and disadvantages of different modifications hoping to inspire and reference future research in this field.
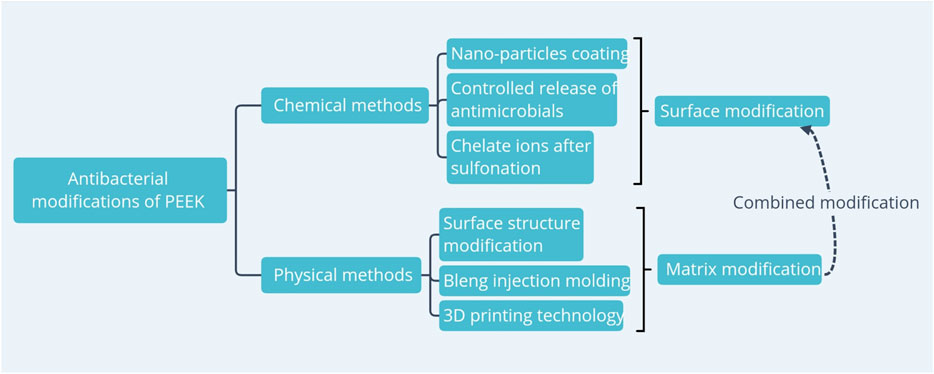
Current Research on Biofunctionalized PEEK With Antibacterial
At present, there are many approaches to biofunctionalize PEEK for antibacterial, and fruitful results have been achieved (Poulsson et al., 2019). According to the biofunctionalization approaches as well as 3D printing technology, it can be divided into chemical modification and physical modification (Figure 2). Chemical modification is to functionalize the PEEK with antimicrobial particles or antimicrobial compounds. Physical modifications include changing the PEEK surface structure and particle blending and injection molding to form composites to meet application requirements. The authors screened the parts involving antibacterial properties in PEEK modification research in recent years, summarized, and discussed them hierarchically.
Chemical Modification
Nanoparticle Coating
The coating technique is the earliest and most widely used in PEEK surface modifications, such as magnetron sputtering (Liu et al., 2017), plasma treatment (Zhang Y. et al., 2021), and bioglass immobilization (Huo et al., 2021b). The advantage is that it can directly improve the biocompatibility, osseointegration, and antimicrobial properties of the PEEK, without destroying the mechanical properties of its matrix. However, there are drawbacks, such as the risk of coating peeling, which may lead to bone resorption and implant failure (Niu et al., 2020), and the cytotoxic risk of metal particles (AshaRani et al., 2009). To minimize the excessive absorption of metal particles, improvements can be made in terms of enhancing the firmness of the coating and the controlled release of the minimum effective concentration of metal ions. At present, there are two main ideas. One is to make nano-metal particle composites to enhance their adhesion. It is reported in the literature that silver nanocluster–silica composite was sprayed on the surface of PEEK composites by radio frequency sputtering. It was proved that it retained good antibacterial properties by bacterial experiments in vitro, while improving the stability of the coating, and silica regulating the release of silver ions, thereby reducing cytotoxicity (Ur Rehman et al., 2017). Another approach is adding a controlled release coating on the particles to achieve the purpose of stabilizing the metal nanoparticles and controlling the release of metal ions. J. Kratochvíl and other scholars deposited copper nanoparticles on the surface of PEEK and further coated it with the fluorocarbon plasma polymer (C: F) film. The experimental results showed that when the thickness of the composite coating was 10 nm, it not only increased the coating stability and controlled release but also retained the antibacterial properties of copper ion and hindered the formation of biofilms (Kratochvíl et al., 2018). The same approach can be applied to silver nanoparticle coatings (Kylian et al., 2017). However, considering that orthopedic implants often exist in the human body for several years or even decades, no matter how low the cytotoxicity is in the short term, the risk of long-term excessive release and absorption of metals must be considered and verified. There is currently a lack of long-term in vivo trials of surface-modified PEEK coated with nano-metallic particles, thus lacking strong evidence for an in-depth discussion of its safety and antibacterial efficacy.
To avoid the cytotoxicity of metal particles, some researchers have explored non-metallic nanoparticles with antibacterial activity. Wang et al (2016) prepared red selenium and gray selenium nanocoatings on the surface of PEEK and found that short-term (<3 days) inhibited Pseudomonas aeruginosa, which could reduce infection and inhibit the formation of biofilms. Compared with nano-Ag particles, selenium nano-ions have been proven to be healthier, safer, and less cytotoxic (Perla and Webster, 2005). Buwalda et al (2020) immobilized ethylene glycol and dimethylamino ethyl acrylate on the surface of PEEK by UV radiation, and in vitro experiments demonstrated that it had a good inhibitory effect on E. coli and S. aureus. Non-metallic coatings also need to consider the antibacterial efficiency, such as the antimicrobial peptide of GL13K and 1-ethyl-3-(3-dimethyl aminopropyl) carbodiimide-mixed coating, of which 1-ethyl-3-(3-dimethyl aminopropyl) carbodiimide-mixed coating exhibited better antimicrobial performance than pure GL13K coating (Hu et al., 2021). Our group also carried out some work on biofunctionalized PEEK. We found that the PEEK surface modified with hydrofluoric acid and nitric acid (AFN) could promote M2 polarization of the macrophages and stimulate the differentiation of osteoblasts (Huo et al., 2021a).
In addition to that, PEEK was biofunctionalized with mesoporous bioactive glass (MBG) and loaded with A-485 for attenuating inappropriately activated immune responses and inhibiting osteoclastogenesis, thus promoting osteogenesis (Figure 3). Also, this MBG could also perform as long-lasting antibacterial agents for antibacterial. The advantage of PEEK surface coating modification is that the approach is simple and conducive to large-scale production, but the release of functional particles, the cytotoxicity of exfoliated particles, and the tissue inflammatory response still require in-depth research and long-term observation in the animal in vivo experiments.
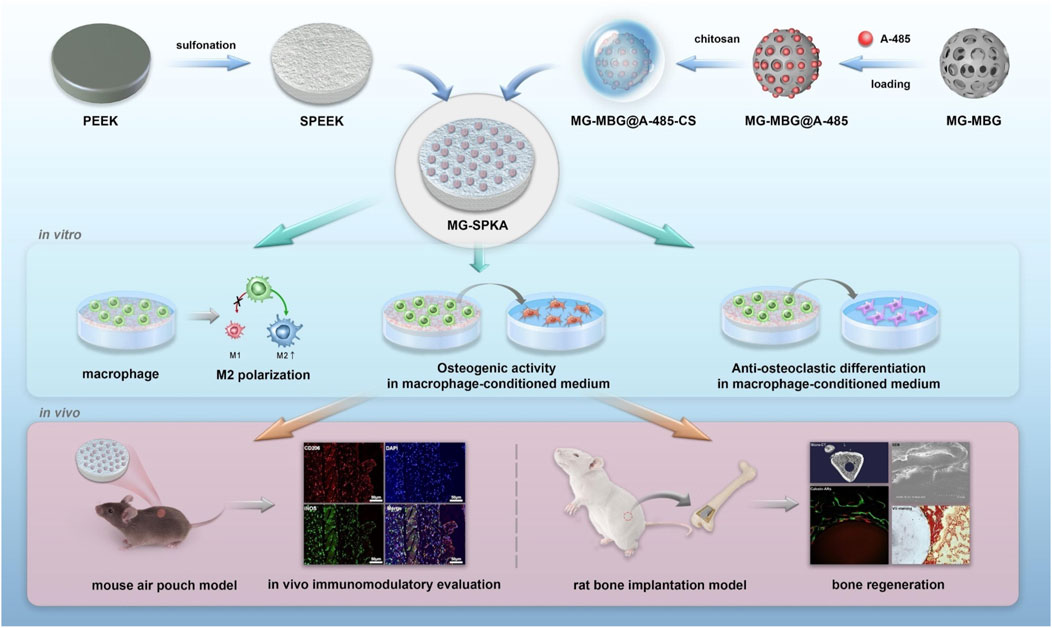
FIGURE 3. Schematic diagram of the process used to prepare and evaluate the PEEK materials. Reproduced from Huo et al (2021c). Copyright (2021), with permission from Elsevier.
Controlled Release of Antimicrobial Agents
The most common modification for antibacterial compounds or drugs is further polymerization on porous PEEK surfaces by polydopamine (PDA) coating. Polydopamine is inspired by mussels foot proteins and reported by Lee et al (2007) and has rapidly become a widely used method for surface decoration of materials, which can form functional nanocoatings on almost all material surfaces and can further polymerize other compounds (El Yakhlifi and Ball, 2020). Moreover, PDA coating exhibits synergistic antibacterial properties and can be used for photothermal therapy (Niyonshuti et al., 2020; Singh et al., 2020); thus, it has enormous potential in the biomedical field. The PEEK-PDA surface after antibacterial modification has also been proved with good biocompatibility and osseointegration (Table 2).
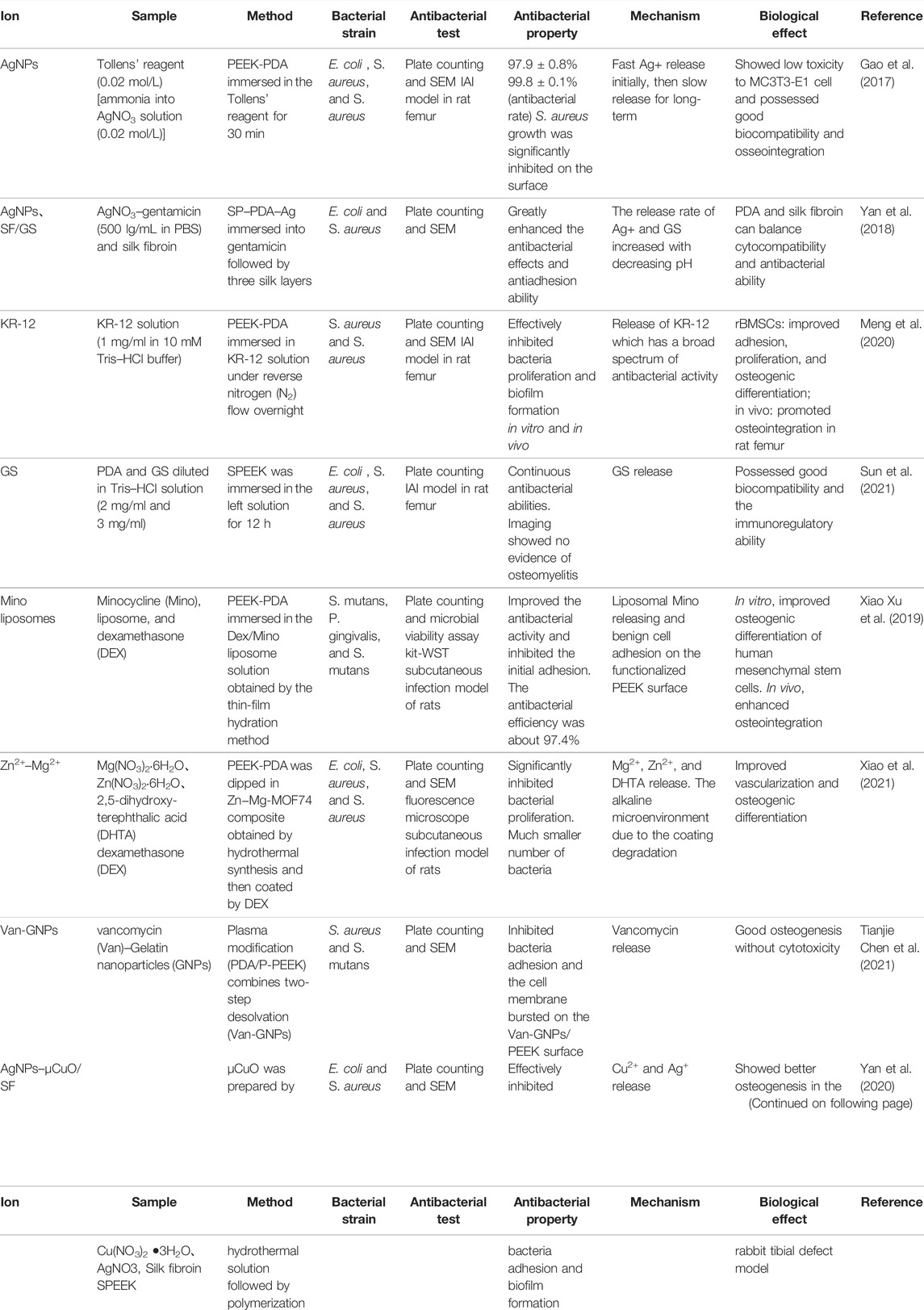
TABLE 2. Controlled release of antimicrobial agents on the PEEK-PDA (2 mg/ml dopamine hydrochloride) surface.
Silver nanoparticles (AgNPs) can destroy bacteria walls (Choi et al., 2008). AgNPs were reduced from [Ag(NH3)2]+ utilizing the reducibility of the catechol in PDA, which exhibited superior and long-term antibacterial properties against E. coli and S. aureus. However, there were no notable differences in not only pro-inflammatory but also anti-inflammatory gene expression between PEEK–PDA–Ag and blank groups which was significantly lower than that in the PEEK group due to the immunosuppressive effect of AgNPs (Gao et al.bgmj, 2017). In addition to antibacterial nanoparticles, integrating antibiotics are also one of the common modification approaches without worrying about the toxicity of metal ions. Sun et al (2021) prepared the SP-GS/PDA functional surface, which rapidly released gentamicin (GS) in the SBF solution. Its antibacterial activity sustained high during the initial 3 days but lost on day 4 due to the little residual content of GS. The long-term stable release of antibiotics with sub-lethal concentration is an urgent problem to be solved. However, Yan et al. (2018) explained different experimental results, and they believed that during the first day, neither AgNPs nor GS alone improved antibacterial activity significantly, yet the combination of them enhanced the antibacterial properties greatly. Thereafter, surface modification with AgNPs and copper oxide microspheres (μCuO) was explored. Yan et al (2020) proposed SP-CuO/Ag-enhanced osteogenesis while ensuring antibacterial properties. It can be seen that the effect of combined modification by multiple antibacterial particles is not a simple superposition, which needs further experimental exploration in the future. The biofunctionalized PEEK which is suitable for implant needs to not only enhance antibacterial properties but also improve histocompatibility and bone osteointegration. Some scholars have made attempts in this regard: Xu X. et al. (2019) considered that dexamethasone (DEX) was an osteoinducing and anti-inflammatory factor easing foreign body response to PEEK implants. They prepared PEEK-DEX/Mino liposome that was proved to be anti-inflammatory and osteogenic besides not reducing antibacterial properties. Modification of combined antibacterial metal nanoparticles was also explored. Compared with Zn−Mg-MOF74/PDA composite, DEX@Zn−Mg-MOF74/PDA composite coating on PEEK showed similar antibacterial properties but better osteogenic gene expressions (OPN and OCN) of rBMSCs observed by RT-PCR (Xiao et al., 2021). PDA coating has the advantage of simple operation and can integrate a variety of modification factors through interlayer. However, these experiments lack research on the wear resistance and stability of PDA coating. Chen et al. believed that the binding strength could be improved by argon plasma surface modification before PDA coating onto the PEEK (Chen et al., 2021). More similar attempts need to be verified in the future.
In addition, other coating modification techniques have also been applied: lawsone, an antibacterial compound that can be applied topically in vivo (Sultana et al., 2021), was made into a suspension with the bioactive glass powder and chitosan by Ur Rehman et al. (2018). It was found that lawsone maintained good antibacterial properties without affecting the biological activity of the material itself. Brushite (CaHPO4·2H2O) and gentamicin were coated on PEEK through a layer-by-layer (LBL) method with varied cycles. The antibacterial efficiency and osseointegration ability exhibited differences due to the number of cycles (Xue et al., 2020). Different modification techniques will change the release concentration and time of antimicrobial compounds. Considering that too high concentration of a local drug may affect bone healing and produce cytotoxicity and very long release time may lead to local bacterial resistance. Ideal antimicrobial compound coating modification should have broad-spectrum antibacterial, low toxicity, controlled release at minimum effective concentration, and ideal release time. In addition, some problems in this modification method to be verified are: whether the coating is stable; whether the antibacterial activity and release rate will be affected in vivo; as a bone implant, it will withstand different stress and friction; whether it can maintain the effective antimicrobial drug concentration per unit area. In a word, the surface coating approaches of PEEK antibacterial modification have been fruitful, but so far, most of the research is based on in vitro experiments, and the safety and effectiveness of in vivo experiments, especially under biomechanics conditions still lack long-term observation.
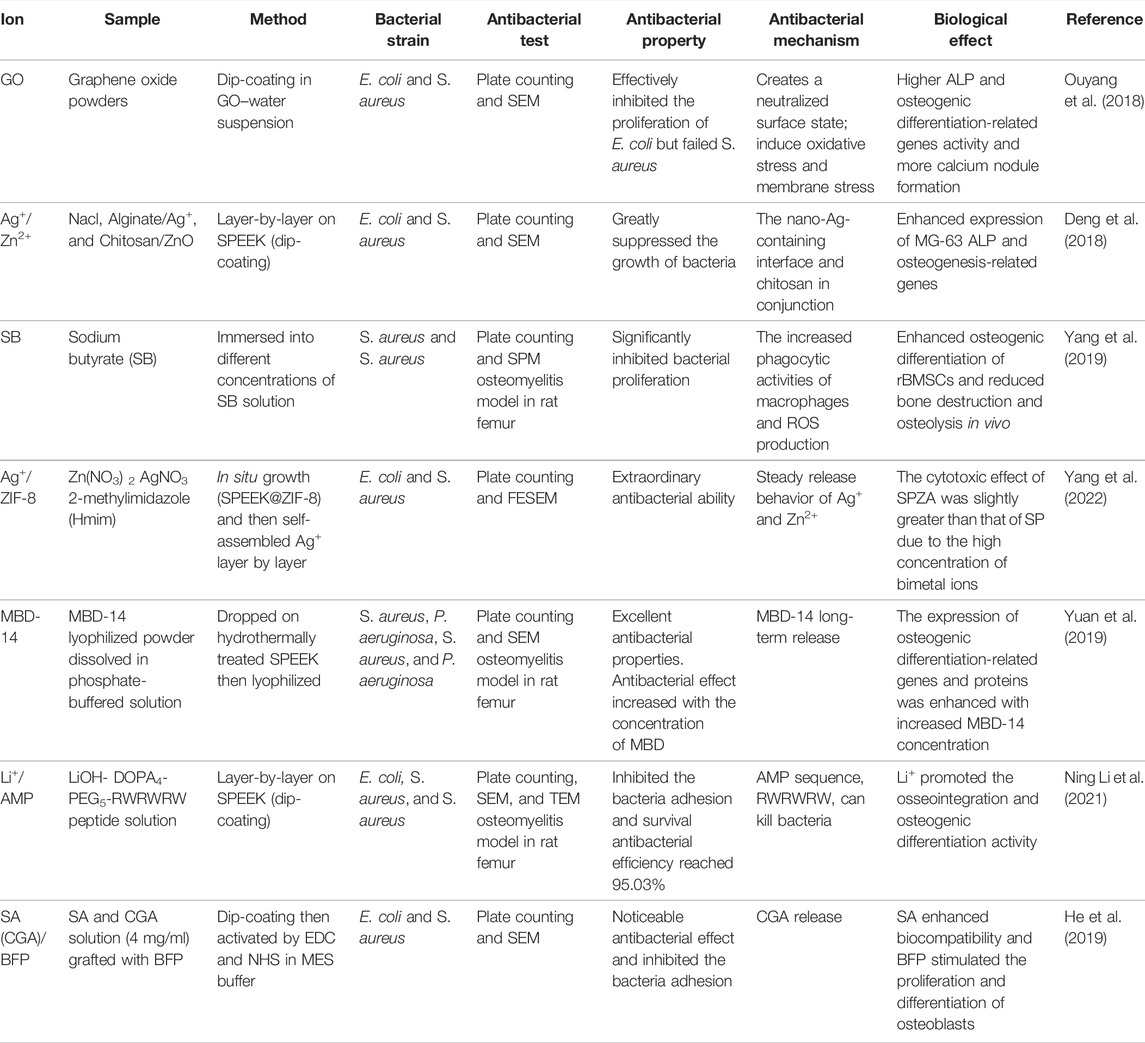
Chelated Antibacterial Ions After Sulfonation of PEEK
Sulfonated PEEK (SPEEK) fabricated by concentrated sulfuric acid makes the surface of PEEK form a negatively charged (-SO3H) interface, which repels the bacterial biofilm that is also negatively charged, thereby having antibacterial properties (Tomoglu et al., 2019). In addition, it can rely on ionic bonds to further chelate antibacterial ions to improve antibacterial performance (Table 3). Compared with the multi-coating adhesion methods, this approach retains the three-dimensional micro-nanostructure of the contact interface and may have stronger coating stability because of the chelation of positive and negative ion bonds. Silver is still one of the most widely used ions, and scholars have been exploring more synergies with other particles (Sikder et al., 2018; Yu et al., 2021). For example, compared with Ag-SPEEK, Ag/Zn-SPEEK (dual Ag+ and Zn2+-decorated SPEEK) retained similar antibacterial properties but showed better cytocompatibility and osseointegration (Deng et al., 2018). In addition, the multiple assembly methods of modified ions produced different effects. Yang et al. (2022) fabricated zeolitic imidazolate framework-8 (ZIF-8) on SPEEK from 2-methylimidazole and Zn2+, which possessed a high Ag+-loading capacity. Experimental results demonstrated that SPZA had more effective antibacterial properties. The improvement of antibacterial activity was obtained not only by the synergy between different metal ions but also by the mixed modification of metal ions and antibacterial compounds. Li+ could enhance cell attachment, proliferation, differentiation, and implant−bone interface osseointegration of the antibacterial AMP coating on SPEEK (Li N. et al., 2021). Considering that antibiotics may lead to drug resistance and metal particles may lead to cytotoxicity, scholars pay attention to antimicrobial peptides (AMPs). However, AMPs are easily inactivated attributing to inducing autoimmune responses (Brandwein et al., 2017); consequently, an AMP from human elements is crucial to endophyte application. Recombinant mouse beta-defensin-14 (MBD-14) which has high homology as well as human beta-defensin-3 (HBD-3) was embellished on the SPEEK. The experimental result indicated that SP-MBD had good antibacterial activity, biocompatibility, and osteogenesis (Yuan et al., 2019). According to this idea, Yang et al. (2019) loaded sodium butyrate, a fermentation product of gut microbiota, onto the SPEEK surface and found that SB-SPEEK exhibited superior anti-infection capacity and induced new bone formation in vitro and in vivo. We can also combine AMPs and osteogenic promoters. Chlorogenic acid (CGA) has excellent antibacterial properties, and grafted peptide (BFP) is one of the most effective bone-inducing growth factors. He et al. (2019) fabricated a hydrogel of compound coating with sodium alginate (SA) on the SPEEK surface and revealed that SPEEK@SA (CGA)@BFP effectively inhibited bacterial proliferation and showed better bioaffinity. Any antibacterial modification method cannot sacrifice bone integrity and biocompatibility, and the detection of cytotoxicity is a crucial experiment before entering the clinical trial. Therefore, the research on antibacterial substances from biological sources has broad prospects.
However, sulfur may have negative effects on the human body, such as the synthesis of low-valent sulfurous compounds, to generate oxygen-free radicals, and damaged cells (Meng et al., 2005). Therefore, whether the corrosion and chemical composition changes of PEEK caused by concentrated sulfuric acid sulfonation can meet the safety requirements of long-term in vivo bone implants is worthy of further study. The balance of safety and antibacterial properties was explored by Ouyang et al. (2016). The research team washed SPEEK with water at different temperatures to obtain different residual sulfide concentrations on the surface. The higher the water temperature, the lower the residual sulfide concentration. In vitro experiments found that the antibacterial properties of SPEEK after treatment were not significantly reduced, especially the inhibitory effect on Staphylococcus aureus. The in vivo result was consistent with the in vitro experiments. In addition, the porous structure of SPEEK may have a profound impact on its biological properties. However, there is a lack of biomechanical research on bifunctional SPEEK in the aforementioned studies.
Physical Modification
Surface Structure Modification
As mentioned in the introduction, the surface structure of PEEK affects cell adhesion and is prone to bacterial film formation. When bacteria attach to nanopillars smaller than their volume, the bacterial wall will rupture (Wang et al., 2017), so the formation of a micro-nano three-dimensional structure can enhance its biological activity and antibacterial properties. At present, there are many approaches to modify the surface structure of PEEK, such as UV irradiation, plasma treatment (Liu et al., 2021), fluorination (Chen et al., 2017), and nitration (Li et al., 2019), while all reported excellent antibacterial properties. The most widely used approach is sulfonation. Different sulfonation times can form different nano-network structures on the surface of PEEK, which can improve biocompatibility. But too long sulfonation time will lead to a disordered porous structure (Figure 4). The literature proved that sulfonation for 5 min was the ideal time to modify the surface structure of PEEK (Ma R. et al., 2020). In addition, based on sulfonation, other structural modification methods such as plasma shock can be combined to form three-dimensional micro-nanostructures with specific functional groups, which can further improve cell adhesion and antibacterial activity (Wang et al., 2018).

FIGURE 4. Sulfonation of PEEK. (I) Sulfonation times: 0.5 min (SPEEK0.5), 1 min (SPEEK1), 3 min (SPEEK3), 5 min (SPEEK5), and 7 min (SPEEK7); untreated PEEK as the control. (II) Quantitative comparison of water contact angles. (a) S concentration of each group measured by EDS (the marks represent p < 0.05); (b) pH values at 1, 4, 7, 14, 21, and 28 days. (A–F) Morphology of the SPEEK surface characterized by SEM (left row) and chemical composition characterized by EDS (right row). Reproduced from Ma R. et al (2020). Copyright (2020), with permission from SAGE Publications.
Blend Injection Molding
Blending modification is to mix inorganic active substances into organisms to form biocomposites. This method has been proven by research studies to apply to the modification of bone endophytes and improve osteogenic activity and biocompatibility (Hajiali et al., 2017; Pang et al., 2019). Blend injection molding is characterized by improving the biomechanical properties of PEEK. As we know, the elastic modulus of pure PEEK (3.7–4.0 GPa) is lower than that of human cortical bone (7–30 GPa) (Ching et al., 2009). Tantalum is one of the metal materials that have been a hot topic studied in recent years. It has excellent histocompatibility and osseointegration, but the elastic modulus is too high. Scholars combined tantalum and PEEK into composite materials that proved to have good osseointegration and mechanical properties but with limited antibacterial property (Zhu et al., 2019; Hu et al., 2022). The antibacterial properties and osteogenic activity were further enhanced by further chelating the antibacterial compound genistein after sulfonation (Mei et al., 2021; Luo et al., 2022). Therefore, we believe that the relevant research on injection molding after particle blending should be tested to explore the changes in biomechanics.
At present, the antibacterial properties of blending modification have been extensively explored such as the common blending with antibacterial metal particles. PEEK and nano-zinc–magnesium silicate (nZMS) in different proportions have good antibacterial properties. When the nZMS content is 50%, the best antibacterial properties and mechanical properties are obtained (Tang et al., 2019). However, some scholars have found that metal particles affect histocompatibility or osseointegration performance after blending, so non-metallic particles are used. Silicon oxide and Si3N4 particles were incorporated into PEEK by melt blending, which had proved good antimicrobial properties with improved biocompatibility and osteogenic properties (Pezzotti et al., 2018; Hu et al., 2022). In addition to nanoparticles, antibacterial compounds can also be modified by blending: it was reported that chitosan, nanohydroxyapatite, and PEEK were made into mixed suspensions with different ratios, and all of them had good antibacterial effects on S. aureus and E. coli; moreover, chitosan could increase the stability of nanohydroxyapatite–PEEK binding (Abdulkareem et al., 2019). Blending modification still needs further research. In addition to the changes in biomechanical properties mentioned previously, most of the bioactive substances by blending modification are located in the matrix, which cannot be guaranteed with uniform and effective distribution, so the improvement of the surface properties is limited. For example, silver nanoparticles-coated PEEK has been shown to have antibacterial activity. However, the composite-mixed silver nanoparticles or silver ions with the PEEK powder through injection molding exhibited uneven particle distribution and failed to inhibit the bacteria adhering to the surface of the PEEK composite (Jaekel, 2012). To solve this problem, we can make improvements in two aspects. One is through the modification of the surface structure; the PEEK composite will form a micro-nanostructure on the surface, which can make the co-polymer-mixed particles obtain greater surface exposure, resulting in improved bioactivity and antimicrobial properties (Niu et al., 2020). Another approach is injection molding by 3D printing technology with a reasonable distribution of particles. It can be concluded that the modification of PEEK does not need to be limited to a single approach, and the synergy of two or even more modification methods can be explored, which provides more and better possibilities for the development of PEEK implant.
Some nanomaterials can generate heat under the irradiation of near-infrared light to inhibit bacterial growth. The blending modification of PEEK and photothermal materials can be applied to photothermal therapy. Most bacteria die at 55°C due to protein denaturation (Pan et al., 2016). At the same time, near-infrared rays can penetrate tissue well with high safety. Taking advantage of these properties, the research on antibacterial properties of nanomaterials with photothermal effects has grown exponentially in recent years, such as graphene composite nanomaterials and noble metal particles or compounds (Xu J.-W. et al., 2019; Song et al., 2020). Among them, graphene and its derived materials also have a good drug-controlled release effect (Mousavi et al., 2020). Photothermal materials have broad prospects in the field of biomedicine.
3D Printing Technology
At present, 3D-printed PEEK implants have entered medical application (Basgul et al., 2018; Atef et al., 2021), which have also been extended to composites mixed with other bioactive particles (Oladapo et al., 2020; Manzoor et al., 2021; Rodzeń et al., 2021b), which can achieve mechanical properties close to human cortical bone and good contact interface biological activity (Li S. et al., 2021; Rodzeń et al., 2021a). Some 3D-printed composite antibacterial scaffolds reported in the literature also demonstrated their potential for antibacterial modification of materials (Yang et al., 2018; Allen et al., 2020; Wang et al., 2021). This research is of great significance to the development of PEEK in the medical field. Oladapo et al (2021) elaborates on the scientific mechanism and some solutions for modifying PEEK by 3D printing. 3D printing technology can better control the distribution of each nanoparticle, solve the problem of insufficient exposure of antibacterial particles at the contact interface in blend injection molding to a certain extent, and also make the distribution of surface-modified particles more uniform and controllable, thereby improving biomechanics, surface properties, and antimicrobial activity of modified PEEK. Deng et al (2017) have produced 3D-printed PEEK decorated with nano-silver particles: in vitro experiments have shown that it has obvious inhibitory effects on Gram-positive bacteria (S. aureus) and Gram-negative bacteria (E. coli) and can destroy the biofilm formed After that, a “PDA–Ag–PDA” sandwich structure was further fabricated by 3D printing on a mesh-structured PEEK surface. In vitro experiments verified its intelligent-controlled release. When the pH decreased due to bacterial metabolism, Ag+ was released, and the experiments in mice also proved its good antibacterial properties and osseointegration (Deng et al., 2020). The 3D printing technique can also be used in photothermal therapy. It was reported in the literature that the antimicrobial drug-loaded hydroxyapatite (HA) coating was attached to the surface of a 3D-printed graphene/PEEK scaffold by electrophoretic deposition, and then the drug was released on-demand by near-infrared irradiation showing good bactericidal effect on Escherichia coli and MRSA (Zhu et al., 2021). At present, there are few reports on the antibacterial properties of 3D-printed PEEK. It may be because of the current shortcomings of 3D printing technology: first, its resolution is limited, the yield is low, and there are still difficulties and challenges in the manufacture of some sophisticated or complex structures (Tahayeri et al., 2018). Second, unlike sulfonation and other structural modifications to form a porous surface, 3D-printed PEEK forms a grid structure of both surface and matrix (Figure 5), so the mechanical property changes require further experimental research. However, it is believed that with the advancement of technology, especially the development of nanotechnology (Laird et al., 2021), 3D-printed PEEK must have broad prospects for the improvement of its osseointegration and antibacterial properties.

FIGURE 5. Modification of 3D-printed PEEK. (I) SEM images of the 3D-printed PEEK/graphene composite scaffold before and after drug-laden hydroxyapatite-coating deposition. Adapted with permission from Zhu et al (2021). Copyright (2021) American Chemical Society. (II) SEM overview of the 3D-printed PEEK scaffolds. (A) SEM zoom images, (B) 3D-printed PEEK, (C) AgNP-decorated PEEK, (D) apatite-decorated PEEK, (E) “PDA–Ag–PDA–apatite” multilayers on PEEK, and (F) “PDA–apatite–PDA–Ag” multilayers on PEEK. Red arrows point to AgNPs. Adapted with permission from Deng et al (2020). Copyright (2020) American Chemical Society.
Outlook
IAI is a besorgniserregend complication of orthopedic surgery with poor prognosis due to biofilm formation. The crucial factor is the initial bacteria adhesion onto implant interfaces. Therefore, it is very important to endow orthopedic implants with antibacterial properties. However, there are still a lot of experiments that need to be explored at present and in the future. First, the bacterial strains used in this literature are relatively single; E. coli and S. aureus are mostly used to represent Gram-negative and -positive bacteria. However, most implant infections in clinic are iatrogenic infections, the types of pathogens are diverse, and the incidence of drug-resistant bacteria is high. Therefore, the use of mixed pathogens in antibacterial experiments may better simulate implant infection than a single bacterial strain. Second, postoperative implant infections often occur within 4 weeks (Zhou et al., 2020) or even within 3 months (Borchardt and Tzizik, 2018). Considering the potential cytotoxicity and drug resistance risk of long-term antibacterial particles or compounds, the combination of chemical and physical modification should be explored more. The antibacterial particles or compounds on a physically modified PEEK provide a strong bactericidal effect in the early stage; then, the antibacterial structure alone can promote the attachment of surrounding tissues and the ability to resist the formation of biofilm achieving long-term antibacterial ability. Meanwhile, most of the surface chemical modifications of PEEK adopt conventional antibacterial metal particles or antibacterial drugs, while our group has reported the application potential of some non-antibacterial compounds in the treatment of IAI. Zhang et al (2020), Zhang S. et al (2021a), and Zhang S. et al (2021b) successively found and proved the antibacterial properties of flufenamic acid, diclofenac, and felodipine against implant biofilm and even drug-resistant bacteria such as MRSA infection. Finally, orthopedic implants not only need to resist long-term chemical erosion in vivo but also need to bear a variety of physical stress, such as friction, anti-fatigue, shear force, and violence due to different injury mechanisms. So, there is still a large amount of research work to be completed for the successful clinical transformation of antibacterial biofunctionalized PEEK: the stability of the coating under different stresses; whether the antibacterial substances could be released evenly and effectively; the granular reaction in vivo, and so on. The biomechanical examination also needs to be repeated after long-term implantation in vivo, and the detection of residual coating and the analysis of tissue around the implant are worthy of further exploration. In addition, with the improvement of 3D printing accuracy in the future, it will have a revolutionary impact on implant materials such as PEEK.
Conclusion
PEEK is the most exciting orthopedic implant material in the past 20 years. A large number of research studies have investigated the biofunctionalization of PEEK with antibacterial. Good antibacterial properties are not only one of the key elements for the success of implants but also can be used to treat difficult clinical diseases such as infection and osteomyelitis. This review summarized the research results of many scholars in recent years and analyzed the approaches to biofunctionalize PEEK for antibacterial and specific methods of modification and then looked forward to the future research direction and problems to be further solved, contributing to the development of the antibacterial scheme of polyetheretherketone.
Author Contributions
YW was responsible for literature retrieval, analysis, and manuscript writing. SZ and B’eN were responsible for manuscript revision and opinion supplement. XQ was responsible for writing guidance and manuscript review. BY was responsible for guidance, hot spot analysis, cooperative division of labor, and final review before submission.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abdulkareem, M. H., Abdalsalam, A. H., and Bohan, A. J. (2019). Influence of Chitosan on the Antibacterial Activity of Composite Coating (PEEK/HAp) Fabricated by Electrophoretic Deposition. Prog. Org. Coat. 130, 251–259. doi:10.1016/j.porgcoat.2019.01.050
Allen, B., Moore, C., Seyler, T., and Gall, K. (2020). Modulating Antibiotic Release from Reservoirs in 3D‐printed Orthopedic Devices to Treat Periprosthetic Joint Infection. J. Orthop. Res. 38 (10), 2239–2249. doi:10.1002/jor.24640
Arciola, C. R., Campoccia, D., and Montanaro, L. (2018). Implant Infections: Adhesion, Biofilm Formation and Immune Evasion. Nat. Rev. Microbiol. 16 (7), 397–409. doi:10.1038/s41579-018-0019-y
AshaRani, P. V., Low Kah Mun, G., Hande, M. P., and Valiyaveettil, S. (2009). Cytotoxicity and Genotoxicity of Silver Nanoparticles in Human Cells. ACS Nano 3 (2), 279–290. doi:10.1021/nn800596w
Atef, M., Mounir, M., Shawky, M., Mounir, S., and Gibaly, A. (2021). Polyetheretherketone Patient-Specific Implants (PPSI) for the Reconstruction of Two Different Mandibular Contour Deformities. Oral Maxillofac. Surg. 10, 1–11. doi:10.1007/s10006-021-00984-6
Basgul, C., Yu, T., MacDonald, D. W., Siskey, R., Marcolongo, M., and Kurtz, S. M. (2018). Structure-property Relationships for 3D-Printed PEEK Intervertebral Lumbar Cages Produced Using Fused Filament Fabrication. J. Mater. Res. 33 (14), 2040–2051. doi:10.1557/jmr.2018.178
Bjarnsholt, T. (2013). The Role of Bacterial Biofilms in Chronic Infections. APMIS 121 (136), 1–58. doi:10.1111/apm.12099
Bock, R. M., Jones, E. N., Ray, D. A., Sonny Bal, B., Pezzotti, G., and McEntire, B. J. (2017). Bacteriostatic Behavior of Surface Modulated Silicon Nitride in Comparison to Polyetheretherketone and Titanium. J. Biomed. Mater. Res. 105 (5), 1521–1534. doi:10.1002/jbm.a.35987
Borchardt, R. A., and Tzizik, D. (2018). Update on Surgical Site Infections. Jaapa 31 (4), 52–54. doi:10.1097/01.Jaa.0000531052.82007.42
Brandwein, M., Bentwich, Z., and Steinberg, D. (2017). Endogenous Antimicrobial Peptide Expression in Response to Bacterial Epidermal Colonization. Front. Immunol. 8, 1637. doi:10.3389/fimmu.2017.01637
Busscher, H. J., van der Mei, H. C., Subbiahdoss, G., Jutte, P. C., van den Dungen, J. J., Zaat, S. A., et al. (2012). Biomaterial-associated Infection: Locating the Finish Line in the Race for the Surface. Sci. Transl Med. 4 (153), 153rv10. doi:10.1126/scitranslmed.3004528
Buwalda, S., Rotman, S., Eglin, D., Moriarty, F., Bethry, A., Garric, X., et al. (2020). Synergistic Anti-fouling and Bactericidal Poly(ether Ether Ketone) Surfaces via a One-step Photomodification. Mater. Sci. Eng. C 111, 110811. doi:10.1016/j.msec.2020.110811
Cai, Z., Qu, X., Zhao, Y., Yuan, Z., Zheng, L., Long, T., et al. (2022). Preliminary Study on Immediate Postoperative CT Images and Values of the Modular Polyetheretherketone Based Total Knee Arthroplasty: An Observational First-In-Human Trial. Front. Surg. 9. doi:10.3389/fsurg.2022.809699
Chen, C., Yin, Y., Xu, H., Li, Z., Wang, F., and Chen, G. (2021). Personalized Three-Dimensional Printed Polyether-Ether-Ketone Prosthesis for Reconstruction after Subtotal Removal of Chronic Clavicle Osteomyelitis: a Case Report. Medicine 100 (17), e25703. doi:10.1097/md.0000000000025703
Chen, M., Ouyang, L., Lu, T., Wang, H., Meng, F., Yang, Y., et al. (2017). Enhanced Bioactivity and Bacteriostasis of Surface Fluorinated Polyetheretherketone. ACS Appl. Mater. Inter. 9 (20), 16824–16833. doi:10.1021/acsami.7b02521
Chen, T., Chen, Q., Fu, H., Wang, D., Gao, Y., Zhang, M., et al. (2021). Construction and Performance Evaluation of a Sustained Release Implant Material Polyetheretherketone With Antibacterial Properties. Mater. Sci. Eng. C 126, 112109. doi:10.1016/j.msec.2021.112109
Chen, Y., Zhang, L., Qin, T., Wang, Z., Li, Y., and Gu, B. (2019). Evaluation of Neurosurgical Implant Infection Rates and Associated Pathogens: Evidence from 1118 Postoperative Infections. Neurosurg. Focus 47 (2), E6. doi:10.3171/2019.5.Focus18582
Chepurnyi, Y., Chernogorskyi, D., Kopchak, A., and Petrenko, O. (2020). Clinical Efficacy of Peek Patient-specific Implants in Orbital Reconstruction. J. Oral Biol. Craniofac. Res. 10 (2), 49–53. doi:10.1016/j.jobcr.2020.01.006
Ching, W. Y., Rulis, P., and Misra, A. (2009). Ab Initio elastic Properties and Tensile Strength of Crystalline Hydroxyapatite. Acta Biomater. 5 (8), 3067–3075. doi:10.1016/j.actbio.2009.04.030
Choi, O., Deng, K. K., Kim, N.-J., Ross, L., Surampalli, R. Y., and Hu, Z. (2008). The Inhibitory Effects of Silver Nanoparticles, Silver Ions, and Silver Chloride Colloids on Microbial Growth. Water Res. 42 (12), 3066–3074. doi:10.1016/j.watres.2008.02.021
Clauss, M., Hunkeler, C., Manzoni, I., and Sendi, P. (2020). Debridement, Antibiotics and Implant Retention for Hip Periprosthetic Joint Infection: Analysis of Implant Survival after Cure of Infection. J. Bone Jt. Infect. 5 (1), 35–42. doi:10.7150/jbji.40924
Deng, L., Deng, Y., and Xie, K. (2017). AgNPs-decorated 3D Printed PEEK Implant for Infection Control and Bone Repair. Colloids Surf. B: Biointerfaces 160, 483–492. doi:10.1016/j.colsurfb.2017.09.061
Deng, Y., Shi, X., Chen, Y., Yang, W., and Chen, Z. G. (2020). A Bacteria-Triggered pH-Responsive Osteopotentiating Coating on 3D-Printed Polyetheretherketone Scaffolds for Infective Bone Defect Repair. Ind. Eng. Chem. Res. 59 (26), 12123–12135. doi:10.1021/acs.iecr.0c02107
Deng, Y., Yang, L., Huang, X., Chen, J., Shi, X., Yang, W., et al. (2018). Dual Ag/ZnO‐Decorated Micro‐/Nanoporous Sulfonated Polyetheretherketone with Superior Antibacterial Capability and Biocompatibility via Layer‐by‐Layer Self‐Assembly Strategy. Macromol. Biosci. 18 (7), 1800028. doi:10.1002/mabi.201800028
El Yakhlifi, S., and Ball, V. (2020). Polydopamine as a Stable and Functional Nanomaterial. Colloids Surf. B: Biointerfaces 186, 110719. doi:10.1016/j.colsurfb.2019.110719
Gao, C., Wang, Y., Han, F., Yuan, Z., Li, Q., Shi, C., et al. (2017). Antibacterial Activity and Osseointegration of Silver-Coated Poly(ether Ether Ketone) Prepared Using the Polydopamine-Assisted Deposition Technique. J. Mater. Chem. B 5 (47), 9326–9336. doi:10.1039/c7tb02436c
Gristina, A. G. (1987). Biomaterial-centered Infection: Microbial Adhesion versus Tissue Integration. Science 237 (4822), 1588–1595. doi:10.1126/science.3629258
Gu, X., Sun, X., Sun, Y., Wang, J., Liu, Y., Yu, K., et al. (2020). Bioinspired Modifications of PEEK Implants for Bone Tissue Engineering. Front. Bioeng. Biotechnol. 8, 631616. doi:10.3389/fbioe.2020.631616
Hacherl, C.-C., Patel, N. A., Jones, K., Ruh, N. B., Gendreau, J. L., Abraham, M. E., et al. (2021). Characterizing Adverse Events of Cranioplasty Implants after Craniectomy: A Retrospective Review of the Federal Manufacturer and User Facility Device Experience Database. Cureus 13 (7), e16795. doi:10.7759/cureus.16795
Hajiali, F., Tajbakhsh, S., and Shojaei, A. (2017). Fabrication and Properties of Polycaprolactone Composites Containing Calcium Phosphate-Based Ceramics and Bioactive Glasses in Bone Tissue Engineering: A Review. Polym. Rev. 58 (1), 164–207. doi:10.1080/15583724.2017.1332640
He, M., Huang, Y., Xu, H., Feng, G., Liu, L., Li, Y., et al. (2021). Modification of Polyetheretherketone Implants: From Enhancing Bone Integration to Enabling Multi-Modal Therapeutics. Acta Biomater. 129, 18–32. doi:10.1016/j.actbio.2021.05.009
He, X., Deng, Y., Yu, Y., Lyu, H., and Liao, L. (2019). Drug-loaded/grafted Peptide-Modified Porous PEEK to Promote Bone Tissue Repair and Eliminate Bacteria. Colloids Surf. B: Biointerfaces 181, 767–777. doi:10.1016/j.colsurfb.2019.06.038
Heary, R. F., Parvathreddy, N., Sampath, S., and Agarwal, N. (2017). Elastic Modulus in the Selection of Interbody Implants. J. Spine Surg. 3 (2), 163–167. doi:10.21037/jss.2017.05.01
Hochella, M. F., Mogk, D. W., Ranville, J., Allen, I. C., Luther, G. W., Marr, L. C., et al. (2019). Natural, Incidental, and Engineered Nanomaterials and Their Impacts on the Earth System. Science 363 (6434), eaau8299. doi:10.1126/science.aau8299
Hu, C.-C., Kumar, S. R., Vi, T. T. T., Huang, Y.-T., Chen, D. W., and Lue, S. J. (2021). Facilitating GL13K Peptide Grafting on Polyetheretherketone via 1-Ethyl-3-(3-Dimethylaminopropyl)carbodiimide: Surface Properties and Antibacterial Activity. Ijms 23 (1), 359. doi:10.3390/ijms23010359
Hu, G., Zhu, Y., Xu, F., Ye, J., Guan, J., Jiang, Y., et al. (2022). Comparison of Surface Properties, Cell Behaviors, Bone Regeneration and Osseointegration between Nano Tantalum/PEEK Composite and Nano Silicon Nitride/PEEK Composite. J. Biomater. Sci. Polym. Edition 33 (1), 35–56. doi:10.1080/09205063.2021.1974812
Huo, S., Meng, X., Zhang, S., Yue, B., Zhao, Y., Long, T., et al. (2021a). Hydrofluoric Acid and Nitric Acid Cotreatment for Biofunctionalization of Polyetheretherketone in M2 Macrophage Polarization and Osteogenesis. J. Biomed. Mater. Res. 109 (6), 879–892. doi:10.1002/jbm.a.37079
Huo, S., Wang, F., Lyu, Z., Hong, Q., Nie, B. e., Wei, J., et al. (2021b). Dual-functional Polyetheretherketone Surface Modification for Regulating Immunity and Bone Metabolism. Chem. Eng. J. 426, 130806. doi:10.1016/j.cej.2021.130806
Huo, S., Wang, F., Lyu, Z., Hong, Q., Nie, B. e., Wei, J., et al. (2021c). Dual-Functional Polyetheretherketone Surface Modification for Regulating Immunity and Bone Metabolism. Chem. Eng. J. 426 (32), 130806. doi:10.1016/j.cej.2021.130806
Jaekel, D. J. (2012). Development and Fabrication of Silver Composite PEEK to Prevent Microbial Attachment and Periprosthetic Infection. Philadelphia, PA: Drexel BIOMED 74, 1.
Ji, Y., Zhang, H., Ru, J., Wang, F., and Wei, J. (2020). Creating Micro-submicro Structure and Grafting Hydroxyl Group on PEEK by Femtosecond Laser and Hydroxylation to Synergistically Activate Cellular Response. Mater. Des. 199, 109413. doi:10.1016/j.matdes.2020.109413
Jiao, J., Zhang, S., Qu, X., and Yue, B. (2021). Recent Advances in Research on Antibacterial Metals and Alloys as Implant Materials. Front. Cel. Infect. Microbiol. 11, 693939. doi:10.3389/fcimb.2021.693939
Kim, T., See, C. W., Li, X., and Zhu, D. (2020). Orthopedic Implants and Devices for Bone Fractures and Defects: Past, Present and Perspective. Engineered Regen. 1, 6–18. doi:10.1016/j.engreg.2020.05.003
Kratochvíl, J., Štěrba, J., Lieskovská, J., Langhansová, H., Kuzminova, A., Khalakhan, I., et al. (2018). Antibacterial Effect of Cu/C:F Nanocomposites Deposited on PEEK Substrates. Mater. Lett. 230, 96–99. doi:10.1016/j.matlet.2018.07.082
Kuehl, R., Tschudin-Sutter, S., Morgenstern, M., Dangel, M., Egli, A., Nowakowski, A., et al. (2019). Time-dependent Differences in Management and Microbiology of Orthopaedic Internal Fixation-Associated Infections: an Observational Prospective Study with 229 Patients. Clin. Microbiol. Infect. 25 (1), 76–81. doi:10.1016/j.cmi.2018.03.040
Kylian, O., Kratochvil, J., Petr, M., Kuzminova, A., Slavinska, D., Biederman, H., et al. (2017). Ag/C:F Antibacterial and Hydrophobic Nanocomposite Coatings. Funct. Mater. Lett. 10 (3), 1750029–1750021. doi:10.1142/s1793604717500291
Laird, N. Z., Acri, T. M., Chakka, J. L., Quarterman, J. C., Malkawi, W. I., Elangovan, S., et al. (2021). Applications of Nanotechnology in 3D Printed Tissue Engineering Scaffolds. Eur. J. Pharmaceutics Biopharmaceutics 161, 15–28. doi:10.1016/j.ejpb.2021.01.018
Lee, H., Dellatore, S. M., Miller, W. M., and Messersmith, P. B. (2007). Mussel-inspired Surface Chemistry for Multifunctional Coatings. Science 318 (5849), 426–430. doi:10.1126/science.1147241
Li, N., Bai, J., Wang, W., Liang, X., Zhang, W., Li, W., et al. (2021). Facile and Versatile Surface Functional Polyetheretherketone with Enhanced Bacteriostasis and Osseointegrative Capability for Implant Application. ACS Appl. Mater. Inter. 13 (50), 59731–59746. doi:10.1021/acsami.1c19834
Li, S., Wang, T., Hu, J., Li, Z., Wang, B., Wang, L., et al. (2021b). Surface Porous Poly-Ether-Ether-Ketone Based on Three-Dimensional Printing for Load-Bearing Orthopedic Implant. J. Mech. Behav. Biomed. Mater. 120, 104561. doi:10.1016/j.jmbbm.2021.104561
Li, Y., Wang, J., He, D., GuoxiongZhuWu, G., Wu, G., and Chen, L. (2019). Surface Sulfonation and Nitrification Enhance the Biological Activity and Osteogenesis of Polyetheretherketone by Forming an Irregular Nano-Porous Monolayer. J. Mater. Sci. Mater. Med. 31 (1), 11. doi:10.1007/s10856-019-6349-0
Liao, C., Li, Y., and Tjong, S. C. (2020). Polyetheretherketone and its Composites for Bone Replacement and Regeneration. Polymers 12 (12), 2858. doi:10.3390/polym12122858
Liu, C., Bai, J., Wang, Y., Chen, L., Wang, D., Ni, S., et al. (2021). The Effects of Three Cold Plasma Treatments on the Osteogenic Activity and Antibacterial Property of PEEK. Dental Mater. 37 (1), 81–93. doi:10.1016/j.dental.2020.10.007
Liu, D., Fu, J., Fan, H., Li, D., Dong, E., Xiao, X., et al. (2018). Application of 3D-Printed PEEK Scapula Prosthesis in the Treatment of Scapular Benign Fibrous Histiocytoma: A Case Report. J. Bone Oncol. 12, 78–82. doi:10.1016/j.jbo.2018.07.012
Liu, X., Chen, C., Zhang, H., Tian, A., You, J., Wu, L., et al. (2019). Biocompatibility Evaluation of Antibacterial Ti–Ag Alloys with Nanotubular Coatings. Ijn Vol. 14, 457–468. doi:10.2147/ijn.S193569
Liu, X., Gan, K., Liu, H., Song, X., Chen, T., and Liu, C. (2017). Antibacterial Properties of Nano-Silver Coated PEEK Prepared through Magnetron Sputtering. Dental Mater. 33 (9), e348–e360. doi:10.1016/j.dental.2017.06.014
Liu, Y., Rath, B., Tingart, M., and Eschweiler, J. (2020). Role of Implants Surface Modification in Osseointegration: A Systematic Review. J. Biomed. Mater. Res. 108 (3), 470–484. doi:10.1002/jbm.a.36829
Lowe, B., Hardy, J. G., and Walsh, L. J. (2020). Optimizing Nanohydroxyapatite Nanocomposites for Bone Tissue Engineering. ACS Omega 5 (1), 1–9. doi:10.1021/acsomega.9b02917
Luo, S., Wang, P., Ma, M., Pan, Z., Lu, L., Yin, F., et al. (2022). Genistein Loaded into Microporous Surface of Nano Tantalum/PEEK Composite with Antibacterial Effect Regulating Cellular Response In Vitro, and Promoting Osseointegration In Vivo. J. Mech. Behav. Biomed. Mater. 125, 104972. doi:10.1016/j.jmbbm.2021.104972
Ma, R., Wang, J., Li, C., Ma, K., Wei, J., Yang, P., et al. (2020a). Effects of Different Sulfonation Times and post-treatment Methods on the Characterization and Cytocompatibility of Sulfonated PEEK. J. Biomater. Appl. 35 (3), 342–352. doi:10.1177/0885328220935008
Ma, Z., Zhao, X., Zhao, J., Zhao, Z., Wang, Q., and Zhang, C. (2020). Biologically Modified Polyether Ether Ketone as Dental Implant Material. Front. Bioeng. Biotechnol. 8. doi:10.3389/fbioe.2020.620537
Manzoor, F., Golbang, A., Jindal, S., Dixon, D., McIlhagger, A., Harkin-Jones, E., et al. (2021). 3D Printed PEEK/HA Composites for Bone Tissue Engineering Applications: Effect of Material Formulation on Mechanical Performance and Bioactive Potential. J. Mech. Behav. Biomed. Mater. 121, 104601. doi:10.1016/j.jmbbm.2021.104601
Massaad, E., Fatima, N., Kiapour, A., Hadzipasic, M., Shankar, G. M., and Shin, J. H. (2020). Polyetheretherketone versus Titanium Cages for Posterior Lumbar Interbody Fusion: Meta-Analysis and Review of the Literature. Neurospine 17 (1), 125–135. doi:10.14245/ns.2040058.029
Masters, E. A., Trombetta, R. P., de Mesy Bentley, K. L., Boyce, B. F., Gill, A. L., Gill, S. R., et al. (2019). Evolving Concepts in Bone Infection: Redefining "biofilm", "acute vs. Chronic Osteomyelitis", "the Immune Proteome" and "local Antibiotic Therapy". Bone Res. 7, 20. doi:10.1038/s41413-019-0061-z
Matar, H. E., Bloch, B. V., Snape, S. E., and James, P. J. (2021). Outcomes of Single- and Two-Stage Revision Total Knee Arthroplasty for Chronic Periprosthetic Joint Infection. Bone Jt. J. 103-B (8), 1373–1379. doi:10.1302/0301-620x.103b8.bjj-2021-0224.r1
Mei, S., Wang, F., Hu, X., Yang, K., Xie, D., Yang, L., et al. (2021). Construction of a Hierarchical Micro & Nanoporous Surface for Loading Genistein on the Composite of Polyetheretherketone/tantalum Pentoxide Possessing Antibacterial Activity and Accelerated Osteointegration. Biomater. Sci. 9 (1), 167–185. doi:10.1039/d0bm01306d
Meng, X., Zhang, J., Chen, J., Nie, B., Yue, B., Zhang, W., et al. (2020). KR-12 Coating of Polyetheretherketone (PEEK) Surface via Polydopamine Improves Osteointegration and Antibacterial Activity In Vivo. J. Mater. Chem. B 8 (44), 10190–10204. doi:10.1039/d0tb01899f
Meng, Z., Liu, Y., and Wu, D. (2005). Effect of Sulfur Dioxide Inhalation on Cytokine Levels in Lungs and Serum of Mice. Inhalation Toxicol. 17 (6), 303–307. doi:10.1080/08958370590922625
Mishchenko, O., Ovchynnykov, O., Kapustian, O., and Pogorielov, M. (2020). New Zr-Ti-Nb Alloy for Medical Application: Development, Chemical and Mechanical Properties, and Biocompatibility. Materials 13 (6), 1306. doi:10.3390/ma13061306
Mounir, M., Atef, M., Abou-Elfetouh, A., and Hakam, M. M. (2018). Titanium and Polyether Ether Ketone (PEEK) Patient-specific Sub-periosteal Implants: Two Novel Approaches for Rehabilitation of the Severely Atrophic Anterior Maxillary ridge. Int. J. Oral Maxillofac. Surg. 47 (5), 658–664. doi:10.1016/j.ijom.2017.11.008
Mousavi, S. M., Low, F. W., Hashemi, S. A., Lai, C. W., Ghasemi, Y., Soroshnia, S., et al. (2020). Development of Graphene Based Nanocomposites towards Medical and Biological Applications. Artif. Cell Nanomedicine, Biotechnol. 48 (1), 1189–1205. doi:10.1080/21691401.2020.1817052
Naik, K., Srivastava, P., Deshmukh, K., Monsoor S, M., and Kowshik, M. (2015). Nanomaterial-Based Approaches for Prevention of Biofilm-Associated Infections on Medical Devices and Implants. J. Nanosci Nanotechnol 15 (12), 10108–10119. doi:10.1166/jnn.2015.11688
Niu, Y., Guo, L., Hu, F., Ren, L., Zhou, Q., Ru, J., et al. (2020). Macro-Microporous Surface with Sulfonic Acid Groups and Micro-nano Structures of PEEK/Nano Magnesium Silicate Composite Exhibiting Antibacterial Activity and Inducing Cell Responses. Ijn Vol. 15, 2403–2417. doi:10.2147/ijn.S238287
Niyonshuti, , Krishnamurthi, V. R., Okyere, D., Song, L., Benamara, M., Tong, X., et al. (2020). Polydopamine Surface Coating Synergizes the Antimicrobial Activity of Silver Nanoparticles. ACS Appl. Mater. Inter. 12 (36), 40067–40077. doi:10.1021/acsami.0c10517
Oladapo, B. I., Ismail, S. O., Bowoto, O. K., Omigbodun, F. T., Olawumi, M. A., and Muhammad, M. A. (2020). Lattice Design and 3D-Printing of PEEK with Ca10(OH)(PO4)3 and In-Vitro Bio-Composite for Bone Implant. Int. J. Biol. Macromolecules 165 (Pt A), 50–62. doi:10.1016/j.ijbiomac.2020.09.175
Oladapo, B. I., Zahedi, S. A., Ismail, S. O., and Omigbodun, F. T. (2021). 3D Printing of PEEK and its Composite to Increase Biointerfaces as a Biomedical Material- A Review. Colloids Surf. B: Biointerfaces 203, 111726. doi:10.1016/j.colsurfb.2021.111726
Otto-Lambertz, C., Yagdiran, A., Wallscheid, F., Eysel, P., and Jung, N. (2017). Periprosthetic Infection in Joint Replacement. Deutsches Ärzteblatt Int. 114 (20), 347. doi:10.3238/arztebl.2017.0347
Ouyang, L., Deng, Y., Yang, L., Shi, X., Dong, T., Tai, Y., et al. (2018). Graphene-Oxide-Decorated Microporous Polyetheretherketone with Superior Antibacterial Capability and In Vitro Osteogenesis for Orthopedic Implant. Macromol. Biosci. 18 (6), 1800036. doi:10.1002/mabi.201800036
Ouyang, L., Zhao, Y., Jin, G., Lu, T., Li, J., Qiao, Y., et al. (2016). Influence of Sulfur Content on Bone Formation and Antibacterial Ability of Sulfonated PEEK. Biomaterials 83, 115–126. doi:10.1016/j.biomaterials.2016.01.017
Pan, W.-Y., Huang, C.-C., Lin, T.-T., Hu, H.-Y., Lin, W.-C., Li, M.-J., et al. (2016). Synergistic Antibacterial Effects of Localized Heat and Oxidative Stress Caused by Hydroxyl Radicals Mediated by Graphene/iron Oxide-Based Nanocomposites. Nanomedicine: Nanotechnology, Biol. Med. 12 (2), 431–438. doi:10.1016/j.nano.2015.11.014
Panayotov, I. V., Orti, V., Cuisinier, F., and Yachouh, J. (2016). Polyetheretherketone (PEEK) for Medical Applications. J. Mater. Sci. Mater. Med. 27 (7), 118. doi:10.1007/s10856-016-5731-4
Pang, H., Tian, H., Qiu, S., Wang, N., and Wang, Y.-Q. (2019). Progress of Titanium Strut for Cervical Reconstruction with Nano-Graphene Oxide Loaded Hydroxyapatite/polyamide Composite and Interbody Fusion after Corpectomy with Anterior Plate Fixation. Artif. Cell Nanomedicine, Biotechnol. 47 (1), 3094–3100. doi:10.1080/21691401.2019.1637883
Perla, V., and Webster, T. J. (2005). Better Osteoblast Adhesion on Nanoparticulate Selenium- A Promising Orthopedic Implant Material. J. Biomed. Mater. Res. 75A (2), 356–364. doi:10.1002/jbm.a.30423
Pezzotti, G., Marin, E., Adachi, T., Lerussi, F., Rondinella, A., Boschetto, F., et al. (2018). Incorporating Si3 N4 into PEEK to Produce Antibacterial, Osteocondutive, and Radiolucent Spinal Implants. Macromol. Biosci. 18 (6), 1800033. doi:10.1002/mabi.201800033
Poulsson, A. H. C., Eglin, D., and Geoff Richards, R. (2019). “Surface Modification Techniques of PEEK, Including Plasma Surface Treatment,” in PEEK Biomaterials Handbook. 2nd Edn (ElsevierNetherlands), 179–201. doi:10.1016/b978-0-12-812524-3.00011-9
Rodzeń, K., McIvor, M. J., Sharma, P. K., Acheson, J. G., McIlhagger, A., Mokhtari, M., et al. (2021a). The Surface Characterisation of Fused Filament Fabricated (FFF) 3D Printed PEEK/Hydroxyapatite Composites. Polymers 13 (18), 3117. doi:10.3390/polym13183117
Rodzeń, K., Sharma, P. K., McIlhagger, A., Mokhtari, M., Dave, F., Tormey, D., et al. (2021b). The Direct 3D Printing of Functional PEEK/Hydroxyapatite Composites via a Fused Filament Fabrication Approach. Polymers 13 (4), 545. doi:10.3390/polym13040545
Roman, H. K., Berthier, P., Rouillon, T., Jean-Philippe, P., and Pierre, C. (2014). Severe Infectious Complications after PEEK-Derived Implant Placement: Report of Three Cases. J. Oral Maxillofac. Surg. Med. Pathol. 26 (4), 477–482. doi:10.1016/j.ajoms.2013.04.006
Sikder, P., Grice, C. R., Lin, B., Goel, V. K., and Bhaduri, S. B. (2018). Single-Phase, Antibacterial Trimagnesium Phosphate Hydrate Coatings on Polyetheretherketone (PEEK) Implants by Rapid Microwave Irradiation Technique. ACS Biomater. Sci. Eng. 4 (8), 2767–2783. doi:10.1021/acsbiomaterials.8b00594
Singh, I., Dhawan, G., Gupta, S., and Kumar, P. (2020). Recent Advances in a Polydopamine-Mediated Antimicrobial Adhesion System. Front. Microbiol. 11, 607099. doi:10.3389/fmicb.2020.607099
Song, J., Liu, H., Lei, M., Tan, H., Chen, Z., Antoshin, A., et al. (2020). Redox-Channeling Polydopamine-Ferrocene (PDA-Fc) Coating to Confer Context-dependent and Photothermal Antimicrobial Activities. ACS Appl. Mater. Inter. 12 (7), 8915–8928. doi:10.1021/acsami.9b22339
Stones, D. H., and Krachler, A. M. (2016). Against the Tide: the Role of Bacterial Adhesion in Host Colonization. Biochem. Soc. Trans. 44 (6), 1571–1580. doi:10.1042/bst20160186
Subbiahdoss, G., Kuijer, R., Grijpma, D. W., van der Mei, H. C., and Busscher, H. J. (2009). Microbial Biofilm Growth vs. Tissue Integration: "The Race for the Surface" Experimentally Studied. Acta Biomater. 5 (5), 1399–1404. doi:10.1016/j.actbio.2008.12.011
Sultana, T., Hossain, M., Rahaman, S., Kim, Y. S., Gwon, J.-G., and Lee, B.-T. (2021). Multi-functional Nanocellulose-Chitosan Dressing Loaded with Antibacterial Lawsone for Rapid Hemostasis and Cutaneous Wound Healing. Carbohydr. Polym. 272, 118482. doi:10.1016/j.carbpol.2021.118482
Sun, A. a., Lin, X., Xue, Z., Huang, J., Bai, X., Huang, L., et al. (2021). Facile Surface Functional Polyetheretherketone with Antibacterial and Immunoregulatory Activities for Enhanced Regeneration toward Bacterium-Infected Bone Destruction. Drug Deliv. 28 (1), 1649–1663. doi:10.1080/10717544.2021.1960924
Tahayeri, A., Morgan, M., Fugolin, A. P., Bompolaki, D., Athirasala, A., Pfeifer, C. S., et al. (2018). 3D Printed versus Conventionally Cured Provisional crown and Bridge Dental Materials. Dental Mater. 34 (2), 192–200. doi:10.1016/j.dental.2017.10.003
Tang, X., Dai, J., Sun, H., Nabanita, S., Petr, S., Wang, D., et al. (2019). Mechanical Strength, Surface Properties, Cytocompatibility and Antibacterial Activity of Nano Zinc-Magnesium Silicate/Polyetheretherketone Biocomposites. J. Nanosci Nanotechnol 19 (12), 7615–7623. doi:10.1166/jnn.2019.16727
Tarallo, L., Giorgini, A., Novi, M., Zambianchi, F., Porcellini, G., and Catani, F. (2020). Volar PEEK Plate for Distal Radius Fracture: Analysis of Adverse Events. Eur. J. Orthop. Surg. Traumatol. 30 (7), 1293–1298. doi:10.1007/s00590-020-02701-7
Tomoglu, S., Caner, G., Arabaci, A., and Mutlu, I. (2019). Production and Sulfonation of Bioactive Polyetheretherketone Foam for Bone Substitute Applications. Int. J. Polymeric Mater. 68 (18), 1167–1176. doi:10.1080/00914037.2018.1539985
Torstrick, F. B., Lin, A. S. P., Potter, D., Safranski, D. L., Sulchek, T. A., Gall, K., et al. (2018). Porous PEEK Improves the Bone-Implant Interface Compared to Plasma-Sprayed Titanium Coating on PEEK. Biomaterials 185, 106–116. doi:10.1016/j.biomaterials.2018.09.009
Ur Rehman, M. A., Bastan, F. E., Nawaz, Q., Goldmann, W. H., Maqbool, M., Virtanen, S., et al. (2018). Electrophoretic Deposition of Lawsone Loaded Bioactive Glass (BG)/chitosan Composite on Polyetheretherketone (PEEK)/BG Layers as Antibacterial and Bioactive Coating. J. Biomed. Mater. Res. 106 (12), 3111–3122. doi:10.1002/jbm.a.36506
Ur Rehman, M. A., Ferraris, S., Goldmann, W. H., Perero, S., Bastan, F. E., Nawaz, Q., et al. (2017). Antibacterial and Bioactive Coatings Based on Radio Frequency Co-sputtering of Silver Nanocluster-Silica Coatings on PEEK/Bioactive Glass Layers Obtained by Electrophoretic Deposition. ACS Appl. Mater. Inter. 9 (38), 32489–32497. doi:10.1021/acsami.7b08646
Wang, M., Bhardwaj, G., and Webster, T. (2017). Antibacterial Properties of PEKK for Orthopedic Applications. Ijn Vol. 12, 6471–6476. doi:10.2147/ijn.S134983
Wang, M., and Tang, T. (2019). Surface Treatment Strategies to Combat Implant-Related Infection from the Beginning. J. Orthopaedic Translation 17, 42–54. doi:10.1016/j.jot.2018.09.001
Wang, M., Yang, Y., Chi, G., Yuan, K., Zhou, F., Dong, L., et al. (2021). A 3D Printed Ga Containing Scaffold with Both Anti-infection and Bone Homeostasis-Regulating Properties for the Treatment of Infected Bone Defects. J. Mater. Chem. B 9 (23), 4735–4745. doi:10.1039/d1tb00387a
Wang, Q., Mejía Jaramillo, A., Pavon, J. J., and Webster, T. J. (2016). Red Selenium Nanoparticles and gray Selenium Nanorods as Antibacterial Coatings for PEEK Medical Devices. J. Biomed. Mater. Res. 104 (7), 1352–1358. doi:10.1002/jbm.b.33479
Wang, S., Deng, Y., Yang, L., Shi, X., Yang, W., and Chen, Z.-G. (2018). Enhanced Antibacterial Property and Osteo-Differentiation Activity on Plasma Treated Porous Polyetheretherketone with Hierarchical Micro/nano-Topography. J. Biomater. Sci. Polym. Edition 29 (5), 520–542. doi:10.1080/09205063.2018.1425181
Xiao, T., Fan, L., Liu, R., Huang, X., Wang, S., Xiao, L., et al. (2021). Fabrication of Dexamethasone-Loaded Dual-Metal-Organic Frameworks on Polyetheretherketone Implants with Bacteriostasis and Angiogenesis Properties for Promoting Bone Regeneration. ACS Appl. Mater. Inter. 13 (43), 50836–50850. doi:10.1021/acsami.1c18088
Xu, J.-W., Yao, K., and Xu, Z.-K. (2019). Nanomaterials with a Photothermal Effect for Antibacterial Activities: an Overview. Nanoscale 11 (18), 8680–8691. doi:10.1039/c9nr01833f
Xu, X., Li, Y., Wang, L., Li, Y., Pan, J., Fu, X., et al. (2019b). Triple-functional Polyetheretherketone Surface with Enhanced Bacteriostasis and Anti-inflammatory and Osseointegrative Properties for Implant Application. Biomaterials 212, 98–114. doi:10.1016/j.biomaterials.2019.05.014
Xue, Z., Wang, Z., Sun, A. a., Huang, J., Wu, W., Chen, M., et al. (2020). Rapid Construction of Polyetheretherketone (PEEK) Biological Implants Incorporated with Brushite (CaHPO4·2H2O) and Antibiotics for Anti-infection and Enhanced Osseointegration. Mater. Sci. Eng. C 111, 110782. doi:10.1016/j.msec.2020.110782
Ya-Shum, C., Chen Lin, J.-H., Wu, Y.-R., Chang, C.-W., Chang, K.-C., Chen, C. C., et al. (2018). Characterizing the Differentiation of Osteoprogenitor Cells on Surface Modified Polyether-Ether-Ketone. Surf. Coat. Techn. 350, 904–912. doi:10.1016/j.surfcoat.2018.03.071
Yan, J., Xia, D., Zhou, W., Li, Y., Xiong, P., Li, Q., et al. (2020). pH-responsive Silk Fibroin-Based CuO/Ag Micro/nano Coating Endows Polyetheretherketone with Synergistic Antibacterial Ability, Osteogenesis, and Angiogenesis. Acta Biomater. 115, 220–234. doi:10.1016/j.actbio.2020.07.062
Yan, J., Zhou, W., Jia, Z., Xiong, P., Li, Y., Wang, P., et al. (2018). Endowing Polyetheretherketone with Synergistic Bactericidal Effects and Improved Osteogenic Ability. Acta Biomater. 79, 216–229. doi:10.1016/j.actbio.2018.08.037
Yang, C., Ouyang, L., Wang, W., Chen, B., Liu, W., Yuan, X., et al. (2019). Sodium Butyrate-Modified Sulfonated Polyetheretherketone Modulates Macrophage Behavior and Shows Enhanced Antibacterial and Osteogenic Functions during Implant-Associated Infections. J. Mater. Chem. B 7 (36), 5541–5553. doi:10.1039/c9tb01298b
Yang, X., Chai, H., Guo, L., Jiang, Y., Xu, L., Huang, W., et al. (2022). Corrigendum to 'In Situ Preparation of Porous Metal-Organic Frameworks ZIF-8@Ag on Poly-Ether-Ether-Ketone with Synergistic Antibacterial Activity' [Colloids Surf. B: Biointerfaces 205 (2021) 111920]. Colloids Surf. B: Biointerfaces 209 (Pt 2), 112179. doi:10.1016/j.colsurfb.2021.112179
Yang, Y., Chu, L., Yang, S., Zhang, H., Qin, L., Guillaume, O., et al. (2018). Dual-functional 3D-Printed Composite Scaffold for Inhibiting Bacterial Infection and Promoting Bone Regeneration in Infected Bone Defect Models. Acta Biomater. 79, 265–275. doi:10.1016/j.actbio.2018.08.015
Yang, Y., He, C., Dianyu, E., Yang, W., Qi, F., Xie, D., et al. (2020). Mg Bone Implant: Features, Developments and Perspectives. Mater. Des. 185, 108259. doi:10.1016/j.matdes.2019.108259
Yu, Y., Sun, Y., Zhou, X., Mao, Y., Liu, Y., Ye, L., et al. (2021). Ag and Peptide Co-decorate Polyetheretherketone to Enhance Antibacterial Property and Osteogenic Differentiation. Colloids Surf. B: Biointerfaces 198, 111492. doi:10.1016/j.colsurfb.2020.111492
Yuan, X., Ouyang, L., Luo, Y., Sun, Z., Yang, C., Wang, J., et al. (2019). Multifunctional Sulfonated Polyetheretherketone Coating with Beta-Defensin-14 for Yielding Durable and Broad-Spectrum Antibacterial Activity and Osseointegration. Acta Biomater. 86, 323–337. doi:10.1016/j.actbio.2019.01.016
Zhang, S., Qu, X., Jiao, J., Tang, H., Wang, M., Wang, Y., et al. (2021a). Felodipine Enhances Aminoglycosides Efficacy against Implant Infections Caused by Methicillin-Resistant Staphylococcus aureus, Persisters and Biofilms. Bioactive Mater. 4, 272–289. doi:10.1016/j.bioactmat.2021.11.019
Zhang, S., Qu, X., Tang, H., Wang, Y., Yang, H., Yuan, W., et al. (2021b). Diclofenac Resensitizes Methicillin‐Resistant Staphylococcus aureus to β ‐Lactams and Prevents Implant Infections. Adv. Sci. 8 (13), 2100681. doi:10.1002/advs.202100681
Zhang, S., Tang, H., Wang, Y., Nie, B. e., Yang, H., Yuan, W., et al. (2020). Antibacterial and Antibiofilm Effects of Flufenamic Acid against Methicillin-Resistant Staphylococcus aureus. Pharmacol. Res. 160, 105067. doi:10.1016/j.phrs.2020.105067
Zhang, Y., Wu, H., Yuan, B., Zhu, X., Zhang, K., and Zhang, X. (2021c). Enhanced Osteogenic Activity and Antibacterial Performance In Vitro of Polyetheretherketone by Plasma-Induced Graft Polymerization of Acrylic Acid and Incorporation of Zinc Ions. J. Mater. Chem. B 9 (36), 7506–7515. doi:10.1039/d1tb01349a
Zhou, W., Peng, X., Ma, Y., Hu, Y., Wu, Y., Lan, F., et al. (2020). Two-staged Time-dependent Materials for the Prevention of Implant-Related Infections. Acta Biomater. 101, 128–140. doi:10.1016/j.actbio.2019.10.023
Zhu, C., He, M., Sun, D., Huang, Y., Huang, L., Du, M., et al. (2021). 3D-Printed Multifunctional Polyetheretherketone Bone Scaffold for Multimodal Treatment of Osteosarcoma and Osteomyelitis. ACS Appl. Mater. Inter. 13 (40), 47327–47340. doi:10.1021/acsami.1c10898
Zhu, H., Ji, X., Guan, H., Zhao, L., Zhao, L., Liu, C., et al. (2019). Tantalum Nanoparticles Reinforced Polyetheretherketone Shows Enhanced Bone Formation. Mater. Sci. Eng. C 101, 232–242. doi:10.1016/j.msec.2019.03.091
Keywords: PEEK, antibacterial properties, modification technology, polyetheretherketone, implant materials
Citation: Wang Y, Zhang S, Nie B, Qu X and Yue B (2022) Approaches to Biofunctionalize Polyetheretherketone for Antibacterial: A Review. Front. Bioeng. Biotechnol. 10:895288. doi: 10.3389/fbioe.2022.895288
Received: 13 March 2022; Accepted: 31 March 2022;
Published: 13 May 2022.
Edited by:
Rui Guo, Jinan University, ChinaReviewed by:
Wei Luo, Donghua University, ChinaDejian Li, Fudan University Pudong Medical Center, China
Copyright © 2022 Wang, Zhang, Nie, Qu and Yue. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bing Yue, advbmp2@163.com
 Yihan Wang
Yihan Wang Shutao Zhang1,2
Shutao Zhang1,2  Xinhua Qu
Xinhua Qu Bing Yue
Bing Yue