Efficacy of omadacycline in the treatment of Legionella pneumonia: a case report
- 1Department of Pharmacy, The Second Xiangya Hospital, Central South University, Institute of Clinical Pharmacy, Central South University, Changsha, China
- 2Department of Pharmacy, Traffic Hospital of Hunan Province, Changsha, China
- 3Department of Chemistry and Bioengineering, Yichun University, Yichun, China
- 4Department of Pharmacy, Foresea Life Insurance Shaoguan Hospital, Shaoguan, China
- 5Department of Pharmacy, Xiangya Hospital, Central South University, Changsha, China
- 6Hunan Key Laboratory of the Research and Development of Novel Pharmaceutical Preparations, Changsha Medical University, Changsha, China
Legionella, one of the main pathogens that causes community-acquired pneumonia, can lead to Legionella pneumonia, a condition characterized predominantly by severe pneumonia. This disease, caused by the bacterium Legionella pneumophila, can quickly progress to critical pneumonia and is often associated with damage to multiple organs. As a result, it requires close attention in terms of clinical diagnosis and treatment. Omadacycline, a new type of tetracycline derivative belonging to the aminomethylcycline class of antibiotics, is a semi-synthetic compound derived from minocycline. Its key structural feature, the aminomethyl modification, allows omadacycline to overcome bacterial resistance and broadens its range of effectiveness against bacteria. Clinical studies have demonstrated that omadacycline is not metabolized in the body, and patients with hepatic and renal dysfunction do not need to adjust their dosage. This paper reports a case of successful treatment of Legionella pneumonia with omadacycline in a patient who initially did not respond to empirical treatment with moxifloxacin. The patient also experienced electrolyte disturbance, as well as dysfunction in the liver and kidneys, delirium, and other related psychiatric symptoms.
1 Introduction
Legionella pneumonia is a form of pneumonia caused by Legionella infection. Predominant symptoms include fever, cough, and shortness of breath, accounting for 2–9% of community-acquired pneumonia cases (Stout and Yu, 1997). Legionella pneumonia progresses more rapidly compared to other respiratory atypical pathogen pneumonia, and without timely treatment, patients can develop severe pneumonia, respiratory failure, shock, acute renal failure, and multi-organ dysfunction within a short period of time (Brown, 2004; Dooling et al., 2015; Chahin and Opal, 2017). As many as 44% of patients may need to be transferred to the intensive care unit (ICU), with a case-fatality rate of up to 10%-15% (Brown, 2004; Dooling et al., 2015; Chahin and Opal, 2017). Therefore, early diagnosis and appropriate antibiotic treatment can improve the outcomes for Legionella patients. Currently, the preferred therapeutic agents are macrolides and respiratory quinolones (Dennis and Anthony, 2016). However, studies have shown that drug resistance should be considered when quinolones are ineffective in treating Legionella (Bruin et al., 2014; Shadoud et al., 2015), and quinolones may cause delirium and other neurological adverse reactions (Stahlmann and Lode, 1999). Omadacycline is a novel tetracycline that has demonstrated anti-Legionella activity in both in vivo and in vitro studies (Dubois, 2020). Its concentration in alveolar macrophages (AM) and alveolar epithelial cell lining fluid (ELF) is higher than that of other novel tetracyclines, making it suitable for treating community-acquired pneumonia (Burgos and Rodvold, 2019). Furthermore, omadacycline does not have the central nervous system adverse effects associated with quinolones (Stahlmann and Lode, 1999). It also has safety advantages for individuals with liver and kidney insufficiency or quinolone intolerance, providing a new treatment option for severe Legionella pneumonia. In the reported case, the patient showed a favorable outcome after receiving omadacycline treatment for Legionella pneumonia. The patient was emergently sent to the ICU due to their critical condition and was empirically treated with meropenem and moxifloxacin, which are commonly used for severe pneumonia. However, the patient’s condition rapidly deteriorated after the third day of treatment, exhibiting delirium, delusions, agitation, excitement, extubation behavior, and other related psychiatric symptoms, which may be attributed to adverse reactions associated with moxifloxacin (Stahlmann and Lode, 1999). Additionally, the patient experienced acute hepatic and renal insufficiency. Considering the possibility of Legionella infection, the treatment was changed to omadacycline, with an initial dose of 200mg followed by a maintenance dose of 100mg once daily intravenously. This treatment showed good efficacy.
2 Case description
The patient is a 44-year-old male with a history of hypertension for over three years, currently undergoing treatment with benazepril hydrochloride. His blood pressure control is suboptimal, with self-monitored systolic pressure recorded at 150 mmHg. He also has a history of hyperlipidemia for more than 10 years and regularly takes atorvastatin calcium for lipid reduction. On September 26, 2023, he was admitted to our hospital with symptoms of “recurring fever for five days, worsening with chest discomfort and shortness of breath for over a day.” The patient experienced onset of symptoms in the community. On September 21, 2023, without any apparent precipitating factors, he developed high fever, peaking at 39.7°C, accompanied by chills, sore throat, cough, and expectoration. He was treated at a local hospital, where his blood pressure was measured at 82/59 mmHg, and norepinephrine was administered for blood pressure support. A chest radiograph showed minor inflammation in the lower left lung, but no specific treatment was administered. The patient’s condition continued to fluctuate, leading to his visit to our hospital’s emergency department on September 26.
On the first day of admission, the patient was conscious, with a peak temperature of 40.3°C, pulse rate of 138 beats per minute, respiratory rate of 24 breaths per minute, and blood pressure of 167/81 mmHg. His oxygenation index was 217, and the inflammatory markers were elevated: white blood cell count 12.18×10^9/L, C-reactive protein (CRP) 200 mg/L, and procalcitonin (PCT) 9.17 ng/mL. Liver function tests showed alanine transaminase 255 U/L, aspartate transaminase 79 U/L, albumin 38 g/L, and creatinine (CREA) 467 µmol/L. Initial treatment included 1g of meropenem followed by 0.5g every 8 hours, in combination with 400mg of moxifloxacin daily for anti-infection therapy.
On the third day of admission, patient was still febrile (40°C), blood pressure dropped to 91/49 mmHg, and oxygenation index was 89. He exhibited symptoms of delirium, delusion, agitation, excitement, tube-pulling behavior, suggestive of potential adverse reactions to moxifloxacin. Inflammatory markers showed a significant increase from previous levels: CRP 470 mg/L, PCT 16.25 ng/mL; renal function deteriorated: CREA 850 µmol/L. Continuous renal replacement therapy was initiated. Due to the rapid progression of the disease, the anti-infection regimen was adjusted, discontinuing meropenem and moxifloxacin, and switching to omadacycline (Zhejiang Hisun Pharmaceutical Co., Ltd. No:6221203–11827), starting with a 200-mg dose followed by 100 mg daily, intravenous drip.
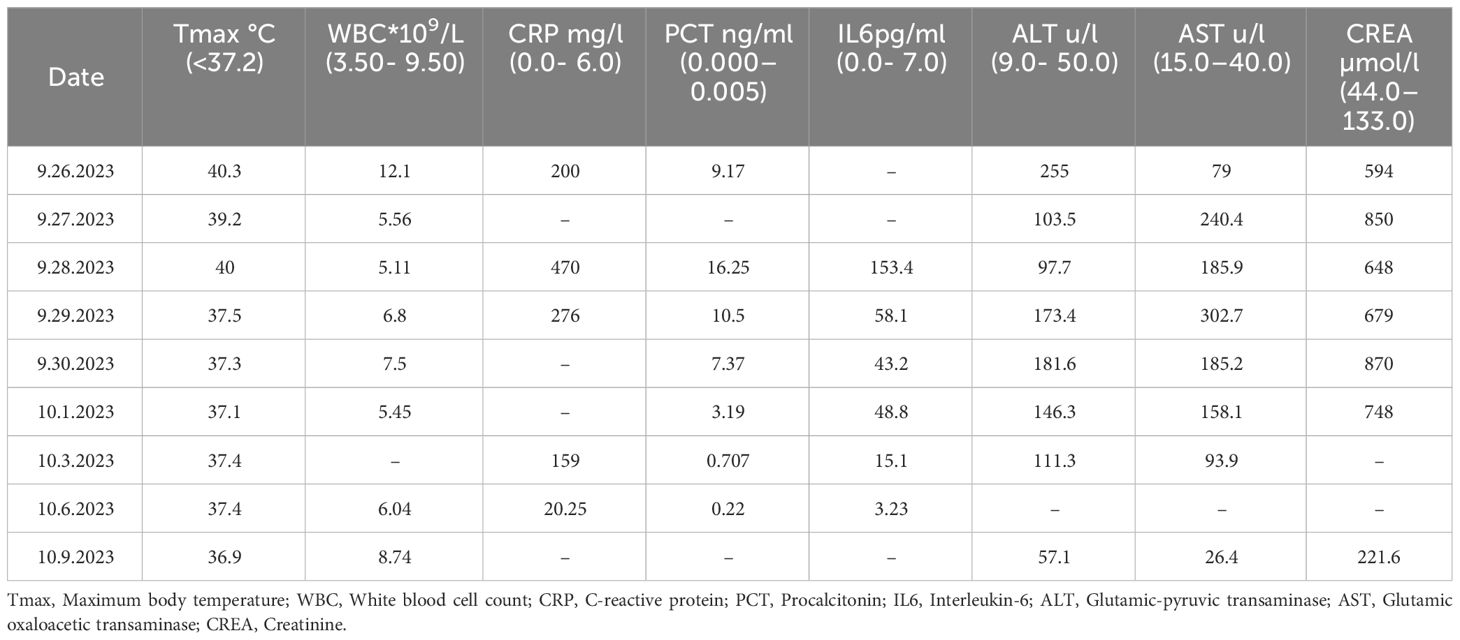
On September 29, metagenomic next-generation sequencing of blood samples identified Legionella pneumophila with a sequence count of 4 and a coverage of less than 0.01%. No other pathogenic bacteria were found. The mNGS test was done at our hospital’s molecular testing center, cfDNA was extracted from 200 µL plasma using a QIAamp® Circulating Nucleic Acid Kit (Qiagen) following the manufacturer’s protocol. The patient remained on omadacycline treatment for a duration of 10 days. As the oral form of omadacycline was unavailable in China at that time, the injectable preparation was consistently used throughout the treatment course. His body temperature decreased rapidly after the drug was administered, and his inflammatory markers as well as liver and kidney functions gradually improved. Specific data can be seen in Table 1. On October 7, a lung CT scan indicated absorption of the consolidation in the lower lobes of both lungs, suggesting an improvement in the infection (Figure 1). The patient was transferred to a local hospital for continued treatment on October 10.
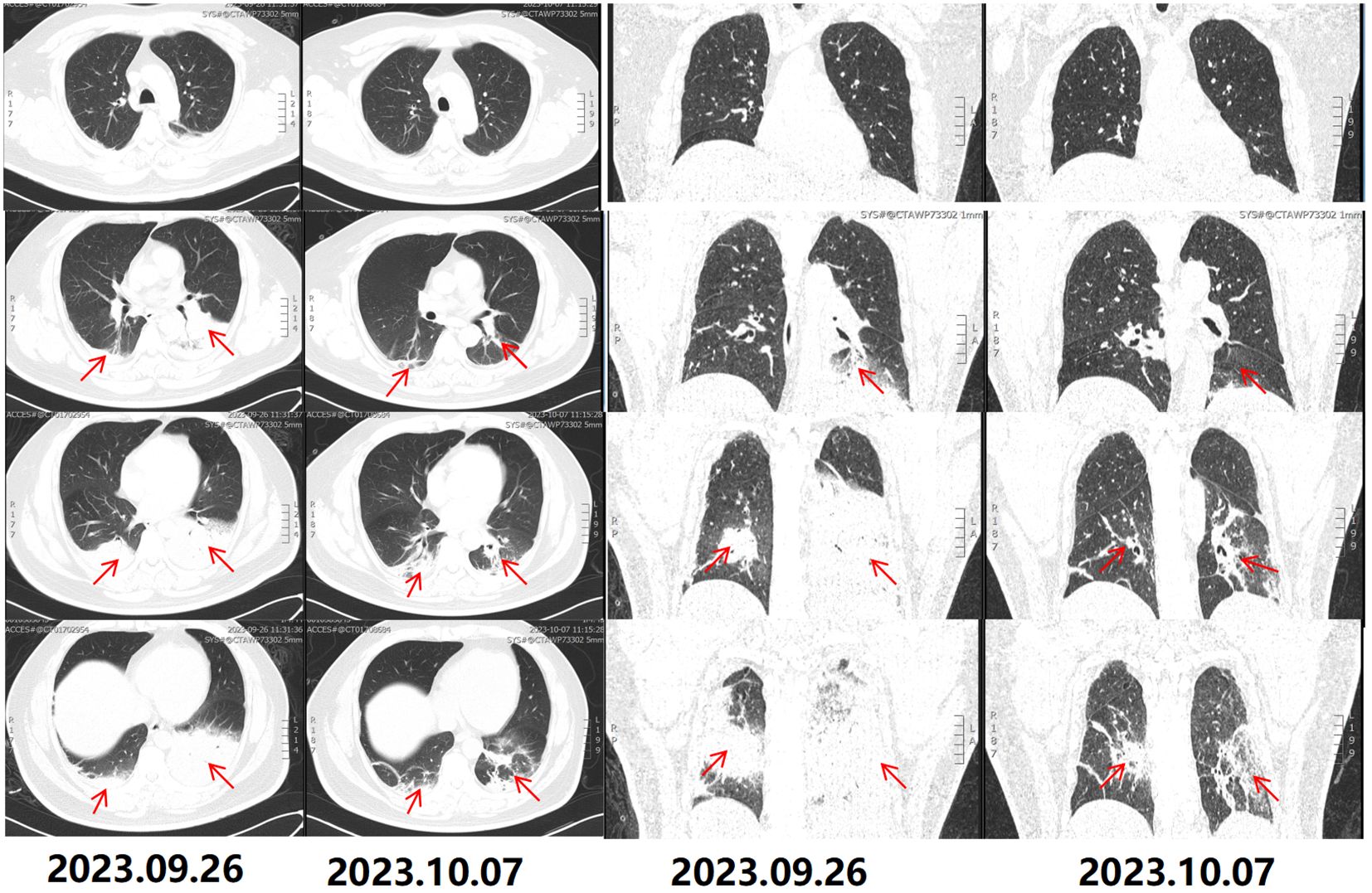
Figure 1 CT scans upon hospital admission. The chest CT on September 26, 2023, reveals bilateral lower lobe consolidation, suggestive of infection, with multiple small and slightly enlarged lymph nodes in the mediastinum. Follow-up lung CT on October 7, 2023, shows partial resolution of the bilateral lower lobe consolidation, indicating improvement of the infection, with the mediastinal lymph nodes unchanged. The red arrows indicate lung consolidation.
3 Discussion
Legionella is a type of bacteria that can cause pneumonia. It is commonly acquired in the community and has an incubation period of 2–14 days. Symptoms of Legionella pneumonia include high fever, cough, chills, difficulty breathing, and neurological abnormalities (Cunha, 2016). When treating community-acquired pneumonia, it is important to choose antibiotics that are effective against Legionella, such as fluoroquinolones, macrolides, and tetracyclines (Metlay, 2019). For severe cases, a combination of β-lactams and macrolides or respiratory quinolones is recommended (Metlay, 2019). For more severe infections, a shorter treatment course of 7–10 days may be feasible with intravenous/oral azithromycin. However, other antibacterials should be administered for a total duration of 10–21 days (Amsden, 2005). However, studies have shown that Legionella can develop resistance to these antibiotics, particularly quinolones (Jonas, 2003). In vitro cultures of Legionella using quinolones have rapidly induced resistant strains, and mutations in the gyrA region of Legionella has been associated with this resistance (Hennebique et al., 2017). This suggests that the empirical use of quinolones may contribute to poor outcomes in severe Legionella pneumonia.
Omadacycline tosylate is a novel tetracycline antibiotic that incorporates a lipophilic side group at the C9 position of the D-ring of minocycline. This modification helps overcome the two primary resistance mechanisms of tetracycline, namely efflux pumps and ribosomal protective proteins (LaPlante et al., 2022). It has good activity against various types of bacteria, including Gram-positive, Gram-negative, atypical pathogens, and anaerobes (Editing Group for Multidisciplinary Expert Consensus on the Rational Use of Tetracyclines Commonly Used in Clinical Practice, 2023). It is particularly effective against atypical pathogens like Mycoplasma, Chlamydia and Legionella, making it suitable for treating pneumonia caused by these pathogens (Editing Group for Multidisciplinary Expert Consensus on the Rational Use of Tetracyclines Commonly Used in Clinical Practice, 2023). Omadacycline has a plasma protein binding rate of only about 21%, a high tissue penetration rate, and can be widely distributed throughout the body in most tissues (Lin et al., 2016). Among the new generation tetracyclines, omadacycline has the highest concentration in lung tissue, and the concentration of omadacycline in alveolar macrophages (AM) and alveolar epithelial cell lining fluid (ELF) is higher than that of eravacycline and tigecycline, which makes it suitable for the treatment of lung infections (Gotfried et al., 2017). Common adverse reactions to omadacycline include gastrointestinal symptoms and elevated transaminases (Lin et al., 2023). In this case, the patient did not experience any of these adverse reactions during treatment under our care and observation. Studies have shown that after the treatment with omacycline, there were no statistically significant differences in pharmacokinetics (PK) parameters between healthy subjects and patients with liver or renal insufficiency and the drug was well tolerated, suggesting that no dose adjustment is necessary for the use of omadacycline in patients with hepatic and renal insufficiency (Berg et al., 2018; Kovacs et al., 2020). Studies confirmed that in both the intention-to-treat population and clinically evaluable populations, omadacycline demonstrated non-inferiority in early clinical response rates and investigator-assessed clinical response rates compared to moxifloxacin for the treatment of adult community-acquired bacterial pneumonia (Stets et al., 2019). This suggests that omadacycline is a viable alternative to moxifloxacin, providing more options for clinical treatment of community-acquired bacterial pneumonia.
4 Conclusion
Legionella pneumonia can rapidly lead to severe and critical illness, causing damage to vital organs. Omadacycline, a new tetracycline with a distinctive aminomethyl structure, has a broader range of antibacterial activity. This report proposes that omadacycline could offer a fresh approach to treating Legionella pneumonia, even in patients with liver and kidney dysfunction.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by ethics committees of the Second Xiangya Hospital of Central South University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article. Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
Author contributions
YW: Writing – original draft, Investigation, Writing – review & editing. S-MY: Writing – original draft, Investigation. S-MH: Writing – original draft, Investigation. W-XX: Writing – original draft. Y-WW: Writing – original draft. QQ: Writing – review & editing. JQ: Writing – review & editing, Conceptualization.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. We thank the support from the Degree & Postgraduate Education Reform Project of Central South University (2023JGB123, 2024JGB061) and the Fundamental Research Funds for the Central Universities of Central South University (No. 2022XQLH154).
Acknowledgments
The authors wish to thank the patient for his support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Amsden, G. W. (2005). Treatment of legionnaires’ disease. Drugs 65, 605–614. doi: 10.2165/00003495-200565050-00003
Berg, J. K., Tzanis, E., Garrity-Ryan, L., Bai, S., Chitra, S., Manley, A., et al. (2018). Pharmacokinetics and safety of omadacycline in subjects with impaired renal function. Antimicrob. Agents Chemother. 62, e02057–e02017. doi: 10.1128/AAC.02057-17
Brown, R. B. (2004). Legionella pneumonia: the spectrum continues to expand. Chest 125, 1979–1980. doi: 10.1378/chest.125.6.1979
Bruin, J. P., Koshkolda, T., EP, I. J., Lück, C., Diederen, B. M., Den Boer, J. W., et al. (2014). Isolation of ciprofloxacin-resistant Legionella pneumophila in a patient with severe pneumonia. J. Antimicrob. Chemother. 69, 2869–2871. doi: 10.1093/jac/dku196
Burgos, R. M., Rodvold, K. A. (2019). Omadacycline: a novel aminomethylcycline. Infect. Drug Resist. 12, 1895–1915. doi: 10.2147/IDR
Chahin, A., Opal, S. M. (2017). Severe pneumonia caused by Legionella pneumophila: Differential diagnosis and therapeutic considerations. Infect. Dis. Clin. North Am. 31, 111–121. doi: 10.1016/j.idc.2016.10.009
Dennis, L. K., Anthony, S. F. (2016). Harrison’s Infectious Diseases, 3rd Edition. United State: McGraw-Hill.
Dooling, K. L., Toews, K. A., Hicks, L. A., Garrison, L. E., Bachaus, B., Zansky, S., et al. (2015). Active bacterial core surveillance for legionellosis - United States, 2011-2013. MMWR Morb Mortal Wkly Rep. 64, 1190–1193. doi: 10.15585/mmwr.mm6442a2
Dubois, J. (2020). In vitro and intracellular activities of omadacycline against Legionella pneumophila. Antimicrob. Agents Chemother. 64, e01972–e01919. doi: 10.1128/AAC.01972-19
Editing Group for Multidisciplinary Expert Consensus on the Rational Use of Tetracyclines Commonly Used in Clinical Practice (2023). Multidisciplinary expert consensus on the rational use of tetracyclines commonly used in clinical practice. Zhonghua Yi Xue Za Zhi 103, 2281–2296. doi: 10.3760/cma.j.cn112137-20230313-00389
Gotfried, M. H., Horn, K., Garrity-Ryan, L., Villano, S., Tzanis, E., Chitra, S., et al. (2017). Comparison of omadacycline and tigecycline pharmacokinetics in the plasma, epithelial lining fluid, and alveolar cells of healthy adult subjects. Antimicrob. Agents Chemother. 61 (9), e01135-17. doi: 10.1128/AAC.01135-17
Hennebique, A., Bidart, M., Jarraud, S., Beraud, L., Schwebel, C., Maurin, M., et al. (2017). Digital PCR for detection and quantification of fluoroquinolone resistance in Legionella pneumophila. Antimicrob. Agents Chemother. 61, e00628–e00617. doi: 10.1128/AAC.00628-17
Jonas, D. (2003). Development and mechanism of fluoroquinolone resistance in Legionella pneumophila. J. Antimicrob. Chemother. 51, 275–280. doi: 10.1093/jac/dkg054
Kovacs, S. J., Ting, L., Praestgaard, J., Sunkara, G., Sun, H., Stein, D. S., et al. (2020). An open-label study of the impact of hepatic impairment on the pharmacokinetics and safety of single oral and intravenous doses of omadacycline. Antimicrob. Agents Chemother. 64, e01650–e01620. doi: 10.1128/AAC.01650-20
LaPlante, K. L., Dhand, A., Wright, K., Lauterio, M. (2022). Re-establishing the utility of tetracycline-class antibiotics for current challenges with antibiotic resistance. Ann. Med. 54, 1686–1700. doi: 10.1080/07853890.2022.2085881
Lin, W., Flarakos, J., Du, Y., Hu, W., He, H., Mangold, J., et al. (2016). Pharmacokinetics, distribution, metabolism, and excretion of omadacycline following a single intravenous or oral dose of 14C-omadacycline in rats. Antimicrob. Agents Chemother. 61, e01784–e01716. doi: 10.1128/aac.01784-16
Lin, F., He, R., Yu, B., Deng, B., Ling, B., Yuan, M. (2023). Omadacycline for treatment of acute bacterial infections: a meta-analysis of phase II/III trials. BMC Infect. Dis. 23, 232. doi: 10.1186/s12879-023-08212-0
Metlay, J. P. (2019). Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the american thoracic society and infectious diseases society of america. Am. J. Respir. Crit. Care Med. 200, e45–e67. doi: 10.1164/rccm.201908-1581ST
Shadoud, L., Almahmoud, I., Jarraud, S., Etienne, J., Larrat, S., Schwebel, C., et al. (2015). Hidden selection of bacterial resistance to fluoroquinolones in vivo: the case of Legionella pneumophila and humans. Ebiomedicine 2, 1179–1185. doi: 10.1016/j.ebiom.2015.07.018
Stahlmann, R., Lode, H. (1999). Toxicity of quinolones. Drugs 58, 37–42. doi: 10.2165/00003495-199958002-00007
Stets, R., Popescu, M., Gonong, J. R., Mitha, I, Nseir, W., Madej, A., et al. (2019). Omadacycline for community-acquired bacterial pneumonia. N. Engl. J. Med. 380, 517–527. doi: 10.1056/NEJMoa1800201
Keywords: omadacycline, Legionella pneumonia, Legionella, novel tetracycline, moxifloxacin
Citation: Wang Y, Yi S-M, Huang S-M, Xu W-X, Wei Y-W, Qu Q and Qu J (2024) Efficacy of omadacycline in the treatment of Legionella pneumonia: a case report. Front. Cell. Infect. Microbiol. 14:1380312. doi: 10.3389/fcimb.2024.1380312
Received: 01 February 2024; Accepted: 03 May 2024;
Published: 21 May 2024.
Edited by:
Marion Skalweit, Case Western Reserve University, United StatesReviewed by:
Stavros Panagiotou, The University of Manchester, United KingdomRobbie Christian, United States Department of Veterans Affairs, United States
Ronald Balczon, University of South Alabama, United States
Copyright © 2024 Wang, Yi, Huang, Xu, Wei, Qu and Qu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jian Qu, qujianstanley@csu.edu.cn
†These authors have contributed equally to this work
 Yao Wang1,2†
Yao Wang1,2†  Qiang Qu
Qiang Qu Jian Qu
Jian Qu