Clinical Relevance of Troponin T Profile Following Cardiac Surgery
- 1Department of Cardiovascular Surgery, Bern University Hospital and University of Bern, Bern, Switzerland
- 2Institute of Radiology, Inselspital, Bern University Hospital and University of Bern, Bern, Switzerland
- 3Department of Cardiology, Barts Heart Center, Barts Health NHS Trust, London, United Kingdom
- 4William Harvey Institute, Queen Mary University, London, United Kingdom
Background: Peak post-operative cardiac troponin T (cTnT) independently predicts mid- and long-term outcome of cardiac surgery patients. A few studies however have reported two peaks of cTnT over the first 48–72 h following myocardial reperfusion. The aim of the current study was to better understand underlying reasons of these different cTnT profiles and their possible relevance in terms of clinical outcome.
Methods: All consecutive adult cardiac surgical procedures performed with an extra-corporeal circulation during a >6 years period were retrospectively evaluated. Patients with a myocardial infarction (MI) < 8 days were excluded. cTnT profile of patients with at least one value ≥1 ng/mL value were categorized according to the time occurrence of the peak value. Univariable and multivariable analysis were performed to identify factors influencing early vs. late increase of cTnT values, and to verify the correlation of early vs. late increase with clinical outcome.
Results: Data of 5,146 patients were retrieved from our prospectively managed registry. From 953 with at least one cTnT value ≥1 ng/mL, peak occurred ≤ 6 h (n = 22), >6 to ≤ 12 h (n = 366), >12 to ≤ 18 h (n = 176), >18 to ≤ 24 h (171), >24 h (218). Age (OR: 1.023; CI: 1.016–1.030) and isolated CABG (OR: 1.779; CI: 1.114–2.839) were independent predictors of a late increase of cTnT over a limit of 1 ng/ml (p < 0.05), whereas isolated valve procedures (OR: 0.685; CI: 0.471–0.998) and cross-clamp duration (OR: 0.993; CI: 0.990–0.997) independently predicted an early elevation (p < 0.05). Delayed elevation as opposed to early elevation correlated with a higher rate of post-operative complications including MI (19.8 vs. 7.2%), new renal insufficiency (16.3 vs. 6.7%), MACCE (32.0 vs. 15.5%), or death (7.4 vs. 4.4%).
Conclusion: Profile of cTnT elevation following cardiac surgery depends on patients' intrinsic factors, type of surgery and duration of cross-clamp time. Delayed increase is of higher clinically relevance than prompt post-operative elevation.
Introduction
Biomarkers of myocardial injury invariably increase following cardiac surgical interventions. Reasons essentially include the direct surgical trauma to the cardiac tissue, the quality of the myocardial protection, the type of surgery (1, 2), the duration of ischemic cross clamp time (3–7), as well as conditions related to the patient himself, such as the renal function (8–11). Several studies have attempted to define biomarkers' cut-off values to predict outcome after cardiac surgery (1, 12–15). The results appear however inconsistent, partially because of inter-institutional variations in terms of overall patients' management, but also because of variations in methodological approaches. In addition and maybe more importantly, these biomarkers are not assessed in a continuous manner but only at certain time points. In other words, our current practice does not allow to precisely measure the peak of release. As a consequence, the use of cut-off values can currently not be implemented in routine practice (16). Recent guidelines on the diagnosis of perioperative myocardial infarction (PMI) have even warned about misinterpretation (17, 18).
Cardiac troponin T (cTnT), because of its high sensitivity, has lately been increasingly investigated as possible clinically relevant marker of perioperative myocardial damage. But like for other biomarkers, the difficulty in assessing its clinical relevance comes from the fact that the timing of peak elevation is not known. It has also been previously suggested that the post-operative cTnT evolution is in fact bimodal with an early peak occurring at around 6 h and a later peak occurring at 24–36 h (14, 19–21). Therefore, it would be advantageous to better understand the factors that influence the profile of post-operative cTnT evolution and possibly identify groups of patients based on their expected peak of TnT release. In addition, it is of interest to clarify if a certain cTnT elevation has the same clinical significance if it occurs rapidly after the end of surgery of later during the post-operative evolution.
In the current analysis of a prospectively collected population of several thousands of cardiac surgery patients, we first intended to characterize the post-operative profiles of cTnT evolution and verify their possible dependence on patients- or surgery-related factors. Additionally, we aimed at evaluating the clinical relevance of these profiles in terms of complications, such as PMI, stroke and death.
Methods
Study Design and Patients Population
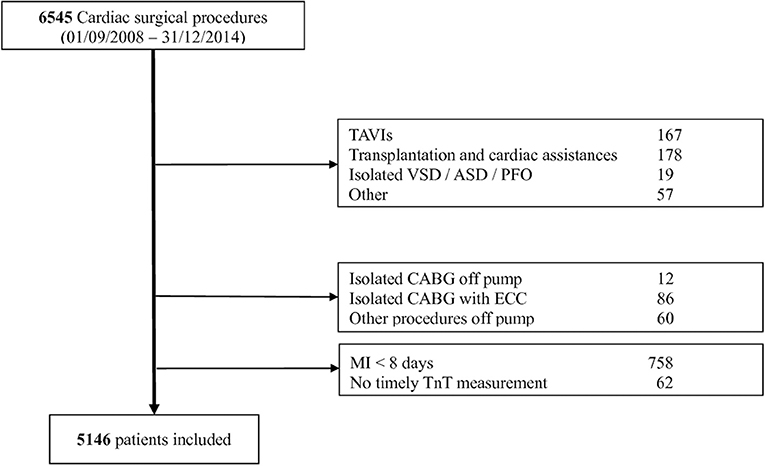
Retrospective single center study including all consecutive adult patients undergoing a cardiac surgery procedure, between September 2008 and December 2014, and identified from a prospectively updated registry (Intellect 1.7, Dendrite Clinical Systems, Henley-on-Thames, UK). TAVIs, heart transplantation, procedures related to a cardiac assist system, isolated septal procedures as well as other procedures, such as trauma, embolectomy, pace-makers were excluded. For the sake of homogeneity of the study groups and because isolated CABG procedures are practically always performed with a mini extra-corporeal circuit (MECC) in our institution, the few CABG procedures performed with regular ECC or off-pump were excluded. Finally, patients with a myocardial infarction (MI) diagnosed <8 days before surgery were also excluded in order to guarantee a normal basal cTnT level (Figure 1). The cantonal ethics committee approved the current analysis as part of our regularly performed quality control. All patients provided informed consent regarding the collection of their data in our registry and their pseudonymization before analysis. All raw data supporting the conclusions of this manuscript can be made available by the authors, without undue reservation, to any qualified researcher.
Surgical Procedures
Surgical procedures were standardized and performed typically via a full sternotomy using a mini extracorporeal circulation (MECC) for isolated CABG or a standard ECC for other procedures, and moderate systemic hypothermia (32°C). A single shot low volume (100 ml) cardioplegia (Cardioplexol™, Laboratory Dr. G. Bichsel AG, Unterseen, Switzerland) was used for isolated CABG procedures and repeated after 45–60 min in case of prolonged cross-clamp time. In other procedures, the cardiac arrest was induced with 100 ml Cardioplexol™ and followed every 20 min with blood cardioplegia. Anesthesia was also standardized and included the use of fentanyl, midazolam and isoflurane.
Biomarkers Assessment
cTnT and CK-MB were routinely assessed 2–3 times during the first 24 post-operative hours. If clinically indicated, cTnT was further followed until the values started decreasing. Both TnT and CK-MB were measured using an electrochemoluminescent enzyme immunoassay on a Modular analytics E170 platform (Roche Diagnostics, Mannheim, Germany). The upper limit of normal was 0.014 ng/ml for the cTnT assay. For the purpose of the study, the time of cTnT assessment was calculated from the time at the end of the cardiopulmonary bypass and peak values of each patient were then categorized in one of the following categories: ≤6, >6 to ≤12, >12 to ≤18, >18 to ≤24, >24 h. Unfortunately, cTnT was not systematically recorded prior to surgery and a baseline value cannot be provided.
Data Acquisition and Definitions
All variables were retrieved from our institutional prospectively maintained electronic registry, checked for completeness and plausibility by two independent data managers, and if needed completed or corrected with the aid of clinical records. The diagnosis of a perioperative MI was made according to the Third Universal Definition of Myocardial Infarction and the SYNTAX trial as previously described (22). MACCE, major adverse cardiovascular or cerebrovascular event, was defined as a composite of all-cause mortality, MI, or stroke. Stroke was defined by episodes of neurological dysfunction related to a focal cerebral infarction that was confirmed by imaging. A new renal insufficiency was defined by a new need of dialysis or, in patients with preoperative creatinine < 2 mg/dl, by a post-operative value of creatinine that increased above 2 mg/dl and reached at least twice the preoperative value.
Statistics
Continuous variables are summarized as mean ± SD if normally distributed or as geometric mean with reference range, and comparisons were made using linear or Poisson regression, respectively. Dichotomous variables are expressed in absolute numbers and percentages, and comparisons were made using Fishers exact test. Non-parametric tests for trend were used to assess the relationships between the five different time intervals with respect to pre-, intra-, and post-operative data. Multivariable logistic regression modeling was used to assess independent associations between predictors and the period of peak cTnT occurrence. All tests were two-sided and p < 0.05 were considered statistically significant. All statistical analysis were performed with Stata (version 12, Stat Corp, College Station, Texas, USA).
Results
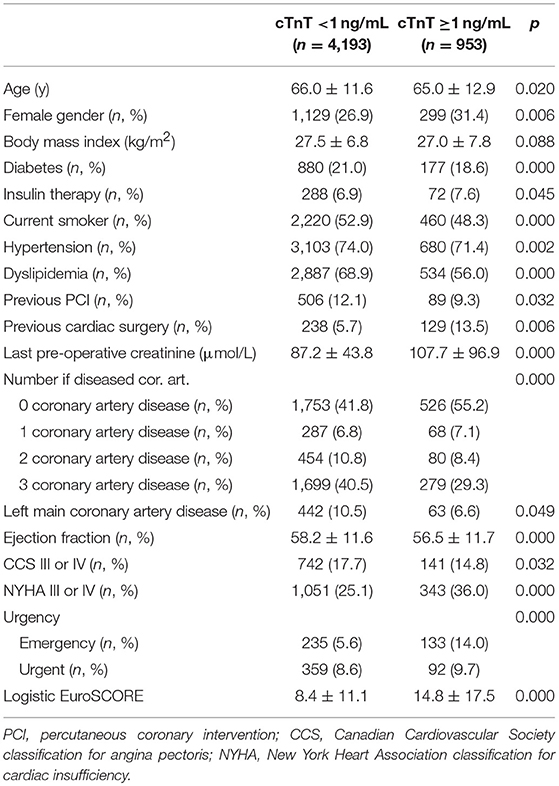
A total of 6,545 patients were considered (Figure 1) from which 1,399 were excluded, mostly due to a recent MI (n = 758; 11.6%). The study group consisted then of 5,146 patients of whom 953 (18.5%) presented at least one post-operative cTnT value ≥1 ng/mL. The characteristics of these patients and their difference with those whose cTnT value remained under 1 ng/ml are presented in Table 1A (patients characteristics), Table 1B (procedure characteristics), and Table 1C (post-operative outcomes).
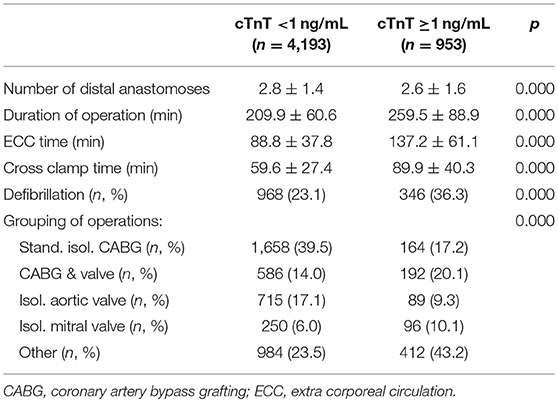
Table 1B. Procedure characteristics of patients with elevated vs. “normal” post-operative cTnT values.
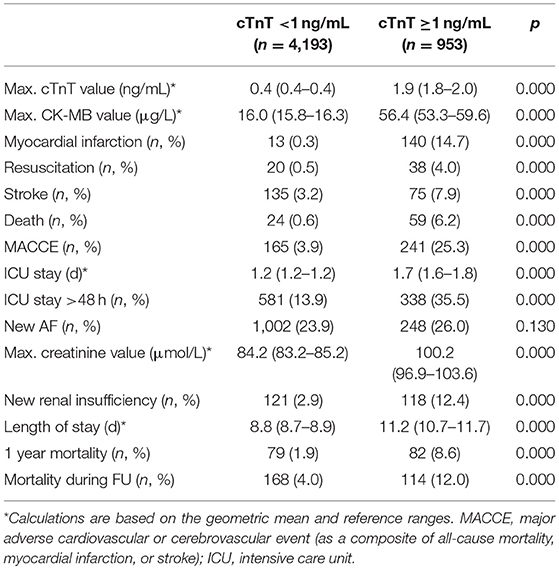
Table 1C. Post-operative outcomes of patients with elevated vs. “normal” post-operative cTnT values.
The profile of cTnT evolution critically varied depending on the period when the peak occurred (Figure 2). When considering only patients with at least one value ≥1 ng/mL, a few patients' (Table 2A) and procedures' (Table 2B) characteristics also significantly varied with the period of cTnT peak occurrence. Age, diabetes, preoperative renal function, coronary artery disease and a history of previous cardiac intervention were all intrinsic parameters that significantly differed between patients with an early vs. late elevation of cTnT. In addition, isolated CABG, isolated valve procedures and prolonged ECC are operative parameters that were also associated with different post-operative cTnT profiles. Interestingly, gender, ejection fraction, NYHA category and urgency/emergency, although differently represented between patients with a max cTnT ≥1 ng/mL, were not associated with different post-operative cTnT profiles.
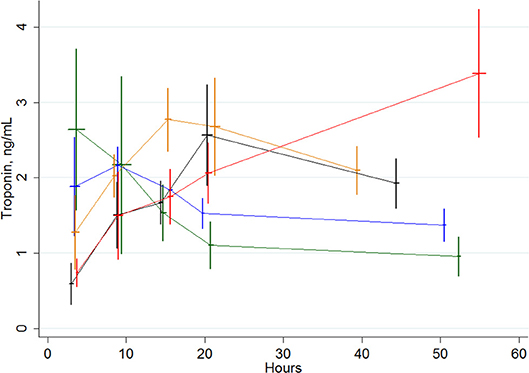
Figure 2. Evolution of cTnT values in subgroups of patients with a peak of cTnT of ≥1 ng/mL and occurring ≤ 6 h (green curve), between >6 to ≤ 12 h (blue curve), between >12 and ≤ 18 h (orange curve), between >18 and ≤ 24 h (black curve) and >24 h (red curve). Vertical bars are standard deviations for the cTnT values. Horizontal bars are standard deviations for the time of blood sampling.
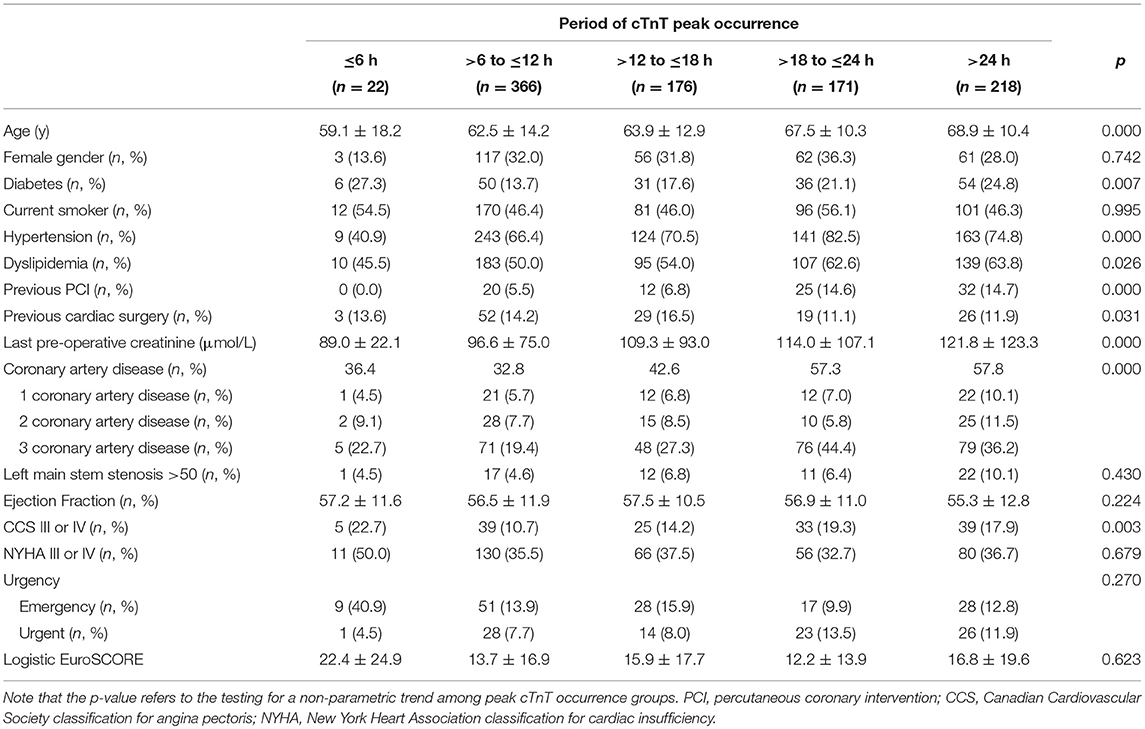
Table 2A. Patient characteristics according to the post-operative period of cTnT peak occurrence in patients with elevated cTnT course (≥1 ng/mL).
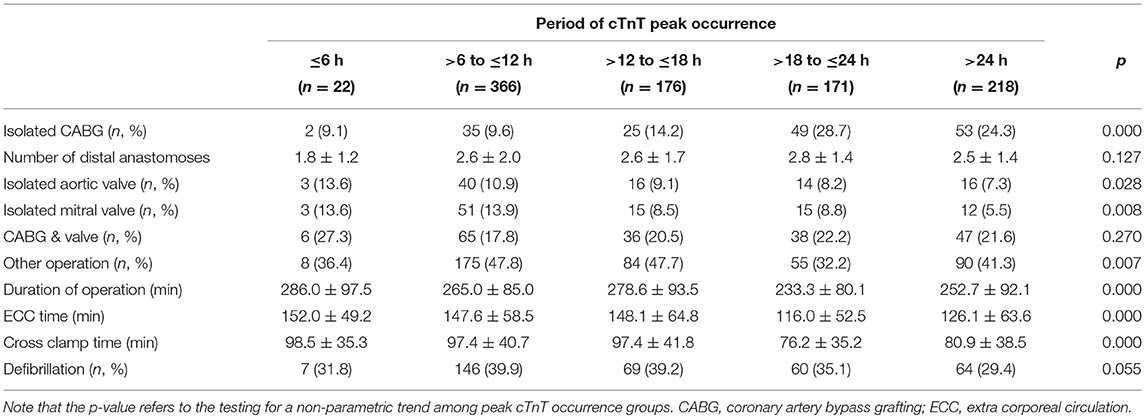
Table 2B. Procedure characteristics according to the post-operative period of cTnT peak occurrence in patients with elevated cTnT course (≥1 ng/mL).
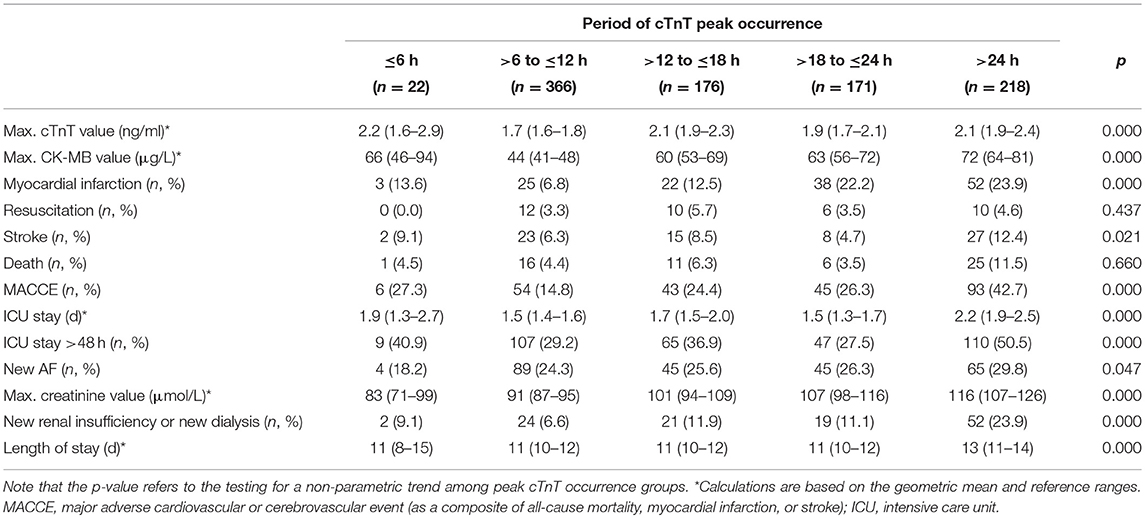
Table 2C. Post-operative outcomes according to the post-operative period of cTnT peak occurrence in patients with elevated cTnT course (≥1 ng/mL).
All parameters that appeared in this univariate analysis as differently represented between the early vs. late peak of cTnT, as well as logitic EuroSCORE were considered for a multivariable analysis, that was thus conducted to identify the pre-operative and operative parameters, which could have had an influence on the time of peak occurrence (Table 3). It appeared that age (OR: 1.019) and isolated CABG (OR: 1.779) independently influenced the occurrence of a late elevation of cTnT over 1 ng/ml, whereas isolated valve procedures (OR: 0.685) and cross-clamp time (OR: 0.993) independently influenced the occurrence of an early elevation over 1 ng/ml. Interestingly, parameters which independently influenced the late increase of cTnT were slightly different in patients whose cTnT remained below 1 ng/ml (Table 3). Among them, age (OR: 1.023), previous cardiac surgery (OR: 1.562), pre-operative renal insufficiency (OR: 1.402), and logistic EuroSCORE (OR: 1.014) had a highly significant effect (p < 0.005).
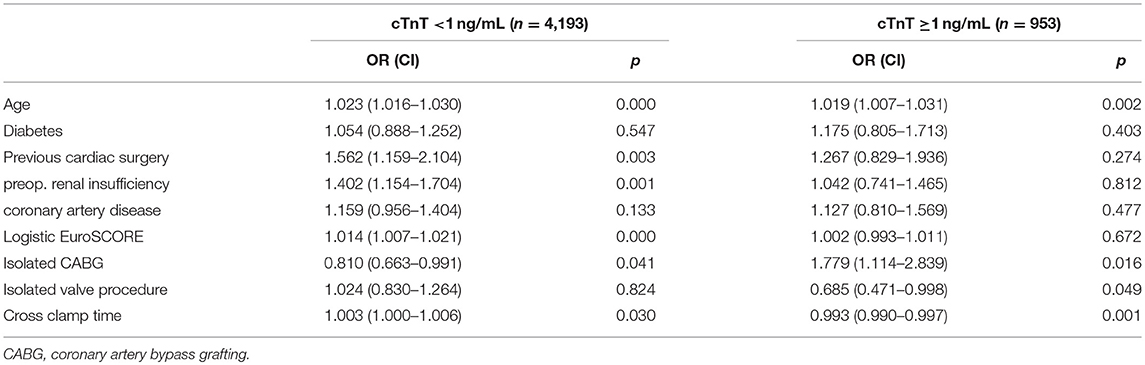
Table 3. Association of preoperative and operative risks with late (>12 h) occurrence of a peak TnT from multivariable analysis, stratified by high (≥1 ng/mL) vs. normal cTnT.
Outcomes also varied between patients with early vs. late elevation of cTnT over 1 ng/ml (Tables 2C, 4A and 4B). Complications, and especially PMI but also resuscitation, stroke, death, MACCE or new development of a renal insufficiency were all significantly associated with both early and late peak of post-operative cTnT. However, late cTnT peak (>12 h) was associated with a higher rate of PMI (19.8 vs. 7.2%), death (7.4 vs. 4.4%), MACCE (32.0 vs. 15.5%) or incidence of a new renal insufficiency (16.3 vs. 6.7%).
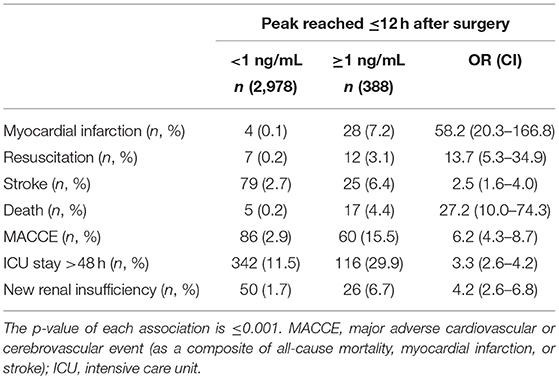
Table 4A. Univariable association of high peak TnT (≥1 ng/mL) with post-operative complications, stratified by early TnT peak.
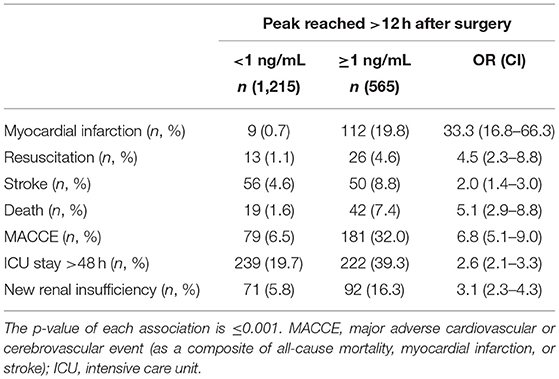
Table 4B. Univariable association of high peak TnT (≥1 ng/mL) with post-operative complications, stratified by late TnT peak.
Discussion
In 2000, Carrier et al. suggested that peak of cTnT following a CABG procedure, occurs around 4–7 h post-reperfusion in a subgroup of patients who will not develop a PMI. Conversely, patients who eventually developed a complication, including a PMI, presented post-operative values of cTnT that kept increasing with a peak occurring between 24 and 48 h post-chest closure (14). This observation was later confirmed by others (19–21). In the current analysis, we approached the patients not from the side of their complication but from the side of their post-operative cTnT profile. We found that several groups can be defined according to the time of the peak occurrence. Approximately 40% of the patients with a post-operative elevation of cTnT over 1 ng/ml had their cTnT peak occurring before 12 h whereas 60% had a delayed increase of cTnT with a peak that occurred later than 12 h. Various time of peak occurrence were also found for those patients with a maximal post-operative cTnT value that remained below 1 ng/ml. Among these later patients, we found that patient's age, history of previous cardiac surgery, pre-operative renal insufficiency and EuroSCORE were independently associated with a late increase of TnT. However, only age independently predicted a late increase over 1 ng/ml whereas the duration of cross-clamp time had an influence on the early increase of cTnT values. Interestingly, isolated CABG procedures were independently associated to a late increase of cTnT whereas isolated valve procedures were associated to an early peak of cTnT.
In fact, several factors have been demonstrated or suggested to influence the post-operative elevation of cTnT values. These include factors related to the surgical procedure as well as factors related to the patient himself. For instance, the duration of cross-clamp time, especially when prolonged over 60 min, is well-known to increase the post-operative values of cTnT (3–7, 12, 23). In addition, the results of the current study seem to indicate that this elevation occurs rather in the early post-operative hours. The type of surgery also seems to play a role. Indeed, cTnT after isolated CABG procedures are not as elevated as after valve surgery or interventions combining CABG and valve surgery. Nesher et al. (1) reported a cTnT value of 0.9 ± 1.5, 1.2 ± 2.9, and 1.3 ± 1.2 ng/ml after isolated CABG, valve procedures or combination of both, respectively (n = 1,515, 229, and 174, respectively). Lurati Buse (2) recently reported TnT values of 0.38 ng/ml (IQR: 0.20–0.71) vs. 0.55 ng/ml (0.31–1.07) after isolated CABG vs. other procedures. The reason why we observed an early peak of cTnT after valve surgery as opposed to a later peak after isolated CABG procedures is not clear but may reflect a better cardioplegic protection in CABG vs. valve patients and would fit to the previously mentioned higher level of post-operative cTnT after valve surgery. In fact, valve surgery candidates typically present a left ventricular hypertrophy, i.e., an increase of their cardiac muscle mass, which in turn could proportionally increase the post-operative cTnT value (24–26).
Non-surgical factors also influence the post-operative elevation of cTnT values. Age for instance has recently been shown to be associated with higher cTnT values (27, 28). The pre-operative renal function has also a clear impact on the post-operative cTnT values (9–11). In a very recent study (8) performed in 11,847 patients with chest pain in the emergency room, the authors observed that reduced estimated glomerular filtration rate (eGFR) was the strongest predictor of an elevated troponin level.
A second aspect of our study concerned the clinical relevance of early vs. late increase of cTnT values in terms of prediction of post-operative complications. In fact, we observed that it was rather the elevation over a cut-off value of 1 ng/ml that was determinant. Nevertheless, it also appeared that an early post-operative elevation of cTnT–with a peak value occurring before 12 h—followed by a reduction, was associated with a lower rate of complications, including MI, MACCE and death, as compared to patients with a late increase of cTnT values. This could be explained by the influence of the previously mentioned factors (age, history of previous cardiac surgery, pre-operative renal insufficiency and EuroSCORE) which all have a clear influence on the post-operative outcome. Conversely, early peak of cTnT may rather reflect surgery related factors, such as the duration of ischemia and the quality of the myocardial protection.
The current study has obviously certain limitations including the fact that it is a retrospective study. All data were however prospectively collected, reviewed and completed by a dedicated team of data managers. Another limitation is the choice of a cut-off value of cTnT that is associated with an increased risk of complications. A real cut-off value has indeed not been clearly defined yet however several previous publications, including one from our group, have found a cut-off value around 1 ng/ml, the cut-off value we eventually set, to be reasonably representative of the reality in most cardiac surgery centers (1, 12, 15, 22, 29). Another aspect that was not taken into account is the level of cTnT increase. Although it looks like the average value of the peak was very similar in all time categories, it would be reasonable to expect a higher risk of post-operative complications in patients with higher cTnT values. Finally, the type of ECC and cardioplegia was different for isolated CABG as for other procedures. The combination of MECC and Cardioplexol™ is indeed especially advantageous in isolated CABG and could thus have had an effect on the overall results presented here (30).
As opposed to several articles which focus on specific subgroups of patients, we based the design of our study on the fact that the elevation of cTnT and other markers of perioperative myocardial damage is currently assessed without distinction between subgroups. In that sense, we thought of including a general population of cardiac surgery patients that would also be representative of the activity in most centers. It is true that doing so could have introduced some bias. On the other hand, with a collection of more than five thousands of patients and, we believe, data of high quality, it was possible to run a multivariable analysis including a relatively large series of parameters including subgroups. Finally, it is with this general approach that we could identify some of these subgroups as being associated with different post-operative TnT profiles. For instance isolated CABG procedures appeared related to rather late increase of TnT whereas isolated valve procedures were more related to early peak of TnT. Nevertheless, this information must be interpreted with caution considering the fact that the cut-off value between normal and elevated cTnT groups clearly distinguished two different profiles of patients.
The fact that we cannot provide reliable baseline (pre-operative) values of cTnT and that we cannot totally exclude that some patients had already an elevated starting value prior to surgery can also be seen as a limitation. However, all patients with documented MI during the 8 days prior to surgery have been excluded. In addition and according to recent published papers on cTnT in unstable angina (31), we estimate that even in patients with a possible pre-operative cTnT elevation, this value would most probably still be under 0.1 ng/ml (100 ng/L). For cardiac surgical patients however, it is well-known that the surgical trauma itself contributes to a much higher elevation of cTnT values. In that sense, we estimate that a possible preoperative elevation of cTnT should be considered as neglectable as compared to the inevitable and much higher elevation that follows the surgical trauma. More importantly, we think it is reasonable to estimate that the preoperative cTnT value did not have an influence on the profile of post-operative cTnT elevation.
Our analysis focused on post-operative cTnT. However, several centers use rather troponin I (TnI) or CK-MB as marker of post-operative myocardial damage. We have collected CK-MB values for the same patients and at the same times and although CK-MB was not studied as extensively as cTnT, data displayed in Tables 1C, 2C seem to follow a similar pattern as cTnT. Whereas, similar results would be obtained for TnI cannot be guaranteed and should thus be studied separately. Basically however, values of TnI and cTnT, although not directly proportional tend to follow similar profiles. In that sense, it could reasonably be expected that the results would be similar for TnI.
In conclusion, it seems that besides the severity of post-operative cTnT elevation, the time of peak expression is also of importance. We showed that early peaks of post-operative cTnT values rather reflect difficulties that occurred during the surgical procedure whereas later increases are more related to patients' intrinsic factors. Interestingly, both early and late elevations of cTnT are associated with an increased risk of complications but this risk appears critically higher in case of a late elevation.
Author Contributions
HT, BG, and VG conceived the original idea and planned the design of the present study. PD, JK, and VG computed the data. HT, PD, JK, BG, and VG analyzed the data. BG and HT performed the statistical analysis. HT wrote the manuscript with the support of all authors. All authors discussed the results and participated to the elaboration of the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank Mrs. Bettina Kohler and Monika Sperisen for the excellent support regarding the data collection and their verification.
References
1. Nesher N, Alghamdi AA, Singh SK, Sever JY, Christakis GT, Goldman BS, et al. Troponin after cardiac surgery: a predictor or a phenomenon? Ann Thorac Surg. (2008) 85:1348–54. doi: 10.1016/j.athoracsur.2007.12.077
2. Lurati Buse GAL, Bolliger D, Seeberger E, Kasper J, Grapow M, Koller MT, et al. Troponin T and B-Type natriuretic peptide after on-pump cardiac surgery: prognostic impact on 12-month mortality and major cardiac events after adjustment for postoperative complications. Circulation (2014) 130:948–57. doi: 10.1161/CIRCULATIONAHA.113.007253
3. Al-Sarraf N, Thalib L, Hughes A, Houlihan M, Tolan M, Young V, et al. Cross-clamp time is an independent predictor of mortality and morbidity in low- and high-risk cardiac patients. Int J Surg. (2011) 9:104–9. doi: 10.1016/j.ijsu.2010.10.007
4. Braathen B, Tønnessen T. Cold blood cardioplegia reduces the increase in cardiac enzyme levels compared with cold crystalloid cardioplegia in patients undergoing aortic valve replacement for isolated aortic valve stenosis. J Thorac Cardiovasc Surg. (2010) 139:874–80. doi: 10.1016/j.jtcvs.2009.05.036
5. Doenst T, Borger MA, Weisel RD, Yau TM, Maganti M, Rao V. Relation between aortic cross-clamp time and mortality–not as straightforward as expected. Eur J Cardiothor Surg. (2008) 33:660–5. doi: 10.1016/j.ejcts.2008.01.001
6. Takeda S, Nakanishi K, Ikezaki H, Kim C, Sakamoto A, Tanaka K, et al. Cardiac marker responses to coronary artery bypass graft surgery with cardiopulmonary bypass and aortic cross-clamping. J Cardiothor Vasc Anesth. (2002) 4:421–5. doi: 10.1053/jcan.2002.125150
7. Brown JR, Hernandez F Jr, Klemperer JD, Clough RA, DiPierro FV, Hofmaster PA, et al. Cardiac troponin T levels in on- and off-pump coronary artery bypass surgery. Heart Surgery Forum (2007) 10:E42–6. doi: 10.1532/HSF98.20061105
8. Carlsson AC, Bandstein N, Roos A, Hammarsten O, Holzmann MJ. High-sensitivity cardiac troponin T levels in the emergency department in patients with chest pain but no myocardial infarction. Int J Cardiol. (2017) 228:253–9. doi: 10.1016/j.ijcard.2016.11.087
9. Bjurman C, Petzold M, Venge P, Farbemo J, Fu MLX, Hammarsten O. High-sensitive cardiac troponin, NT-proBNP, hFABP and copeptin levels in relation to glomerular filtration rates and a medical record of cardiovascular disease. Clin Biochem. (2015) 48:302–7. doi: 10.1016/j.clinbiochem.2015.01.008
10. Chung JZY, Dallas Jones GR. Effect of renal function on serum cardiac troponin T — population and individual effects. Clin Biochem. (2015) 48:807–10. doi: 10.1016/j.clinbiochem.2015.05.004
11. Pfortmueller CA, Funk GC, Marti G, Leichtle AB, Fiedler GM, Schwarz C, et al. Diagnostic performance of high-sensitive troponin T in patients with renal insufficiency. Am J Cardiol. (2013) 112:1968–72. doi: 10.1016/j.amjcard.2013.08.028
12. Mohammed AA, Agnihotri AK, van Kimmenade RR, Martinez-Rumayor A, Green SM, Quiroz R, et al. Prospective, comprehensive assessment of cardiac troponin T testing after coronary artery bypass graft surgery. Circulation (2009) 120:843–50. doi: 10.1161/CIRCULATIONAHA.108.837278
13. Omar AS, Sudarsanan S, Hanoura S, Osman H, Sivadasan PC, Shouman Y, et al. Kinetics of highly sensitive troponin T after cardiac surgery. BioMed Res Int. (2015) 2015:57456. doi: 10.1155/2015/574546
14. Carrier M, Pellerin M, Perrault LP, Solymoss BC, Pelletier LC. Troponin levels in patients with myocardial infarction after coronary artery bypass grafting. Ann Thorac Surg. (2000) 69:435–40. doi: 10.1016/S0003-4975(99)01294-1
15. Baggish AL, MacGillivray TE, Hoffman W, Newell JB, Lewandrowski KB, Lee-Lewandrowski E, et al. Postoperative troponin-T predicts prolonged intensive care unit length of stay following cardiac surgery. Crit Care Med. (2004) 32:1866–71. doi: 10.1097/01.CCM.0000139692.19371.7C
16. Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD et al. Third universal definition of myocardial infarction. J Am Coll Cardiol. (2012) 60:1581–98. doi: 10.1016/j.jacc.2012.08.001
17. van Beek DE, van Zaane B, Buijsrogge MP, van Klei WA. Implementation of the third universal definition of myocardial infarction after coronary artery bypass grafting: a survey study in Western Europe. J Am Heart Assoc. (2015) 4:e001401. doi: 10.1161/JAHA.114.001401
18. Wildi K, Gimenez MR, Twerenbold R, Reichlin T, Jaeger C, Heinzelmann A, et al. Misdiagnosis of myocardial infarction related to limitations of the current regulatory approach to define clinical decision values for cardiac troponin. Circulation (2015) 131:2032–40. doi: 10.1161/CIRCULATIONAHA.114.014129
19. Fransen EJ, Diris JH, Maessen JG, Hermens WT, van Dieijen-Visser MP. Evaluation of “new” cardiac markers for ruling out myocardial infarction after coronary artery bypass grafting. Chest (2002) 122:1316–21. doi: 10.1378/chest.122.4.1316
20. Peivandi AA, Dahm M, Opfermann UT, Peetz D, Doerr F, Loos A, et al. Comparison of cardiac troponin I versus T and creatine kinase MB after coronary artery bypass grafting in patients with and without perioperative myocardial infarction. Herz (2004) 29:658–64. doi: 10.1007/s00059-004-2543-y
21. Lehrke S, Steen H, Sievers HH, Peters H, Opitz A, Müller-Bardorff M, et al. Cardiac troponin T for prediction of short- and long-term morbidity and mortality after elective open heart surgery. Clin Chem. (2004) 50:1560–7. doi: 10.1373/clinchem.2004.031468
22. Göber V, Hohl A, Gahl B, Dick F, Eigenmann V, Carrel TP, et al. Early troponin T and prediction of potentially correctable in-hospital complications after coronary artery bypass grafting surgery. PLoS ONE (2013) 8:e74241. doi: 10.1371/journal.pone.0074241
23. Matt P, Arbeleaz E, Schwirtz G, Doebele T, Eckstein F. Low-volume, single-shot crystalloid cardioplegia is safe for isolated aortic valve replacement. Thorac Cardiovasc Surg. (2012) 60:360–2. doi: 10.1055/s-0031-1295565
24. Ascione R, Caputo M, Gomes WJ, Lotto AA, Angelini GD, Suleiman MS. Myocardial injury in hypertrophic hearts of patients undergoing aortic valve surgery using cold or warm blood cardioplegia. Eur J Cardiothor Surg. (2002) 21:440–6. doi: 10.1016/S1010-7940(01)01168-X
25. Rosjo H, Andreassen J, Edvardsen T, Omland T. Prognostic usefulness of circulating high-sensitivity troponin T in aortic stenosis and relation to echocardiographic indexes of cardiac function and anatomy. Am J Cardiol. (2011) 108:88–91. doi: 10.1016/j.amjcard.2011.02.346
26. Fernandez-Jimenez R, Lopez-Romero P, Suarez-Barrientos A, Garcia-Rubira JC, Fernandez-Ortiz A, Fuster V, et al. Troponin release overestimates infarct size in presence of left ventricular hypertrophy. JACC (2012) 60:640–1. doi: 10.1016/j.jacc.2012.02.067
27. Mueller-Hennessen M, Lindhal B, Giannitsis E, Biener M, Vafaie M, deFilippi CR, et al. Diagnostic and prognostic implications using age- and gender-specific cut-offs for high-sensitivity cardiac troponin T–sub-analysis from the TRAPID-AMI study. Int J Cardiol. (2016) 209:26–33. doi: 10.1016/j.ijcard.2016.01.213
28. Javierre C, Ricart A, Manez R, Farrero E, Carrio ML. Rodriguez-Castro D, et al. Age and sex differences in perioperative myocardial infarction after cardiac surgery. Interact Cardiovasc Thorac Surg. (2012) 15:28–32. doi: 10.1093/icvts/ivr130
29. Kovacevic R, Majkic-Singh N, Ignjatovic S, Otasevic P, Obrenovic R, Paris M, et al. Toponin T levels in detection of perioperative myocardial infarction after coronary artery bypass surgery. Clin Lab (2004) 50:437–45.
30. Immer FF, Ackermann A, Gygax E, Stalder M, Englberger L, Eckstein FS, et al. Minimal extracorporeal circulation is a promising technique for coronary artery bypass grafting. Ann Thorac Surg. (2007) 84:1515–20. doi: 10.1016/j.athoracsur.2007.05.069
Keywords: cardiac surgery, CABG, troponin, cardiac biomarkers, complications
Citation: Tevaearai Stahel HT, Do PD, Klaus JB, Gahl B, Locca D, Göber V and Carrel TP (2018) Clinical Relevance of Troponin T Profile Following Cardiac Surgery. Front. Cardiovasc. Med. 5:182. doi: 10.3389/fcvm.2018.00182
Received: 20 August 2018; Accepted: 03 December 2018;
Published: 13 December 2018.
Edited by:
Massimo Caputo, University of Bristol, United KingdomReviewed by:
Pradeep Narayan, Rabindranath Tagore International Institute of Cardiac Sciences (RTIICS), IndiaAntonio Miceli, Istituto Clinico Sant'Ambrogio, Italy
Copyright © 2018 Tevaearai Stahel, Do, Klaus, Gahl, Locca, Göber and Carrel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hendrik T. Tevaearai Stahel, hendrik.tevaearai@gmail.com
 Hendrik T. Tevaearai Stahel
Hendrik T. Tevaearai Stahel Peter D. Do
Peter D. Do Jeremias Bendicht Klaus
Jeremias Bendicht Klaus Brigitta Gahl
Brigitta Gahl Didier Locca
Didier Locca Volkhard Göber1
Volkhard Göber1