Unveiling the nexus of postoperative fever and delirium in cardiac surgery: identifying predictors for enhanced patient care
- 1Department of Cardio-Thoracic Surgery, Nanjing Drum Tower Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Nanjing, China
- 2Department of Cardio-Thoracic Surgery, Nanjing Drum Tower Hospital, The Afliated Hospital of Nanjing University Medical School, Nanjing, China
- 3Department of Critical Care Medicine, Xiangya Hospital of Central South University, Changsha, China
Background: Postoperative delirium (POD) is a significant complication observed in cardiac surgery patients, characterized by acute cognitive decline, fluctuating mental status, consciousness impairment, and confusion. Despite its impact, POD often goes undiagnosed. Postoperative fever, a common occurrence after cardiac surgery, has not been comprehensively studied in relation to delirium. This study aims to identify perioperative period factors associated with POD in patients undergoing cardiopulmonary bypass, with the potential for implementing preventive interventions.
Methods: In a prospective observational study conducted between February 2023 and April 2023 at the Department of Cardio-Thoracic Surgery, Nanjing Drum Tower Hospital, Affiliated Hospital of Nanjing University Medical School, a total of 232 patients who underwent cardiac surgery were enrolled. POD assessment utilized the Confusion Assessment Method for the ICU (CAM-ICU), while high fever was defined as a bladder temperature exceeding 39°C. Statistical analysis included univariate and multivariate analyses, logistic regression, nomogram development, and internal validation.
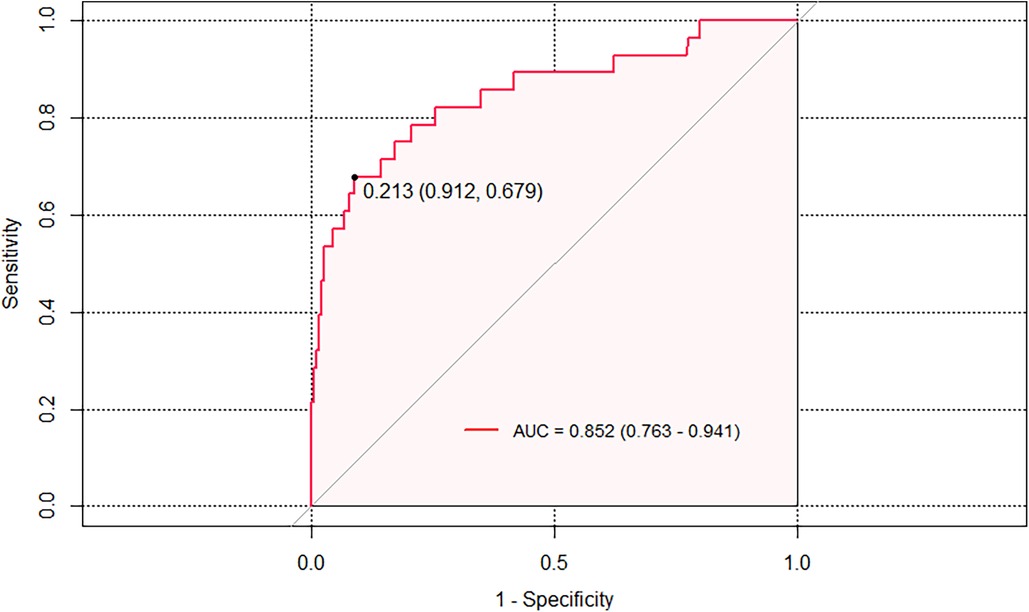
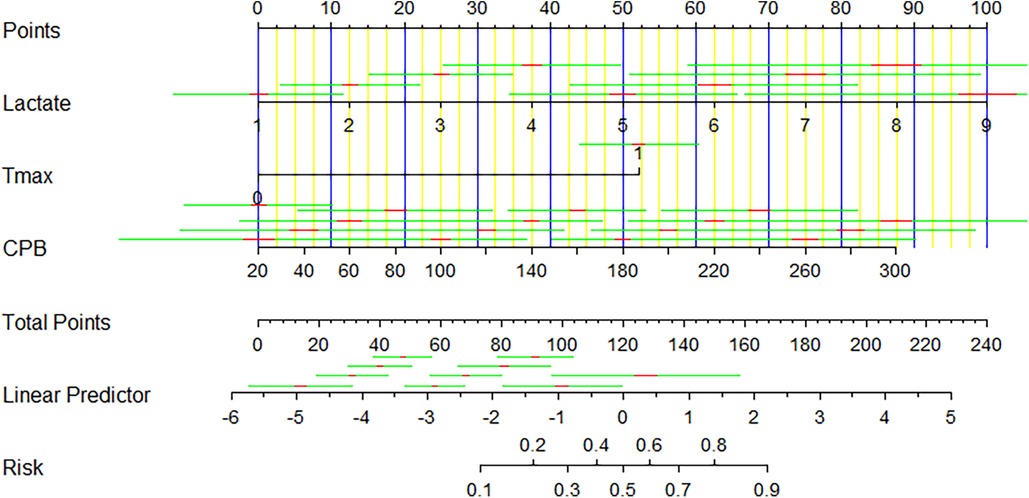
Result: The overall incidence of postoperative delirium was found to be 12.1%. Multivariate analysis revealed that postoperative lactate levels [odds ratio (OR) = 1.787], maximum temperature (OR = 11.290), and cardiopulmonary bypass time (OR = 1.015) were independent predictors of POD. A predictive nomogram for POD was developed based on these three factors, demonstrating good discrimination and calibration. The prediction model exhibited a C-statistic value of 0.852 (95% CI, 0.763–0.941), demonstrating excellent discriminatory power. Sensitivity and specificity, based on the area under the receiver operating characteristic (AUROC) curve, were 91.2% and 67.9%, respectively.
Conclusion: This study underscores the high prevalence of POD in cardiac surgery patients and identifies postoperative lactate levels, cardiopulmonary bypass duration, and postoperative fever as independent predictors of delirium. The association between postoperative fever and POD warrants further investigation. These findings have implications for implementing preventive strategies in high-risk patients, aiming to mitigate postoperative complications and improve patient outcomes.
1. Introduction
Delirium is a disease characterized by acute cognitive decline, fluctuating mental status, consciousness impairment, lack of attention, or confusion (1). It is a recognized adverse prognostic marker in intensive care unit (ICU) patients, associated with increased incidence, mortality, and the development of long-term neurocognitive deficits (2). The incidence of postoperative delirium in cardiac surgery patients ranges from 16% to 73% (3–7), and is associated with early postoperative mortality, prolonged hospitalization, discharge to long-term care facilities, functional and cognitive decline, and increased healthcare costs (8, 9). While delirium is typically considered a short-term cognitive impairment, long-term consequences, such as functional and cognitive decline, are possible.
Given the high incidence of postoperative delirium in cardiac surgery patients, and its impact on functional outcomes and quality of life, it is essential to study the association between delirium and functional outcomes in this population. However, cardiac surgeons, anesthesiologists, intensivists, and nurses may fail to recognize delirium in up to 84% of patients (10, 11). Although the EuroSCORE, a cardiac surgical risk assessment system, is associated with postoperative mortality and delirium, no studies have reported on the association between postoperative fever and delirium (7, 12, 13). Postoperative fever is more common in cardiac surgery and is associated with increased cerebral embolic load after cardiopulmonary bypass and increased release of chemotactic factors (14).
Therefore, this study aims to determine the preoperative, operative, and postoperative fever-related factors associated with postoperative delirium in patients undergoing cardiopulmonary bypass. Successful identification of these factors could lead to preventative interventions in high-risk patients, with the hope of preventing subsequent complications.
2. Materials and methods
2.1. Study design
Participants between February 2023 and April 2023, we conducted a prospective observational study at the Department of Cardio-Thoracic Surgery. The study was ethically approved by the institutional review board was registered on the Chinese Clinical Trial Registry (ChiCTR2000038762).
2.2. Participants
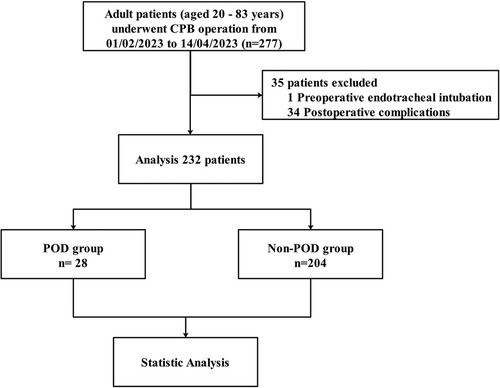
Between February 1, 2023, and April 14, 2023, this study recruited patients who underwent cardiac surgery under general anesthesia for cardiopulmonary bypass with the inclusion criteria of being admitted to the Cardio-Thoracic Surgery ICU for more than 24 h and providing written informed consent after receiving information sheets and potential risk disclosures. Exclusion criteria included patients under the age of 18, those diagnosed with delirium and stroke during admission, those with a Glasgow Coma Scale score of ≤8 points who required intubation and mechanical ventilation, those who were deeply sedated (as determined by Richmond Agitation Sedation Scale scores of −4 and −5), and those with alcohol withdrawal reactions (15), patients with infective endocarditis and preoperative fever. A total of 232 eligible patients were enrolled (Figure 1), and measures were taken to ensure the validity and robustness of the research findings.
Delirium is a challenging condition to diagnose in the intensive care unit (ICU), and many patients may go unrecognized. Despite the use of many delirium assessment instruments in published studies, the most widely used instrument is the Confusion Assessment Method (CAM) (16). CAM has a sensitivity of 94% and specificity of 89% compared to the gold standard diagnosis by psychiatrists (17). CAM-ICU was developed to accurately diagnose delirium in ICU patients who are often unable to speak due to mechanical ventilation. CAM-ICU has a sensitivity of 95% and specificity of 89% (16, 18).
2.3. Definition of end-points
In surgical patients who do not have permanent neurological impairment, postoperative delirium (POD) is identified using the Confusion Assessment Method for the ICU (CAM-ICU) (18) and evaluated twice daily for seven consecutive days. This method allows for consistent monitoring and diagnosis of POD, which is a common complication after surgery and can have significant negative effects on patient outcomes (19).
We define high fever as bladder temperature greater than 39°C and continuously monitor body temperature for 24 h postoperatively. This definition of high fever allows for consistent and accurate measurement of postoperative fever, which can indicate a pathological state and may require further evaluation and treatment.
2.4. Statistical analysis
In this study, we conducted a comprehensive analysis of the data using a range of statistical methods. Continuous variables were assessed for normality using the Kolmogorov–Smirnov test and reported either as mean ± standard deviation or median with interquartile ranges (Q1–Q3), depending on their distribution. Student's t-test and Mann–Whitney U-test were used to analyze normally and non-normally distributed continuous variables, respectively. Categorical variables were presented as frequencies and percentages and analyzed using either chi-squared test or Fisher's exact test. All statistical analyses were two-tailed, and a P-value less than 0.05 was considered statistically significant. Additionally, we employed single-variable binary logistic regression analysis to assess the relationship between various variables and the outcome, calculating odds ratios and 95% confidence intervals.
2.5. Model development
After conducting univariate analysis, variables that demonstrated statistical significance with a P-value less than 0.05 were included in a stepwise (backward: conditional) multivariate logistic regression analysis model to establish a predictive model. Furthermore, we constructed a nomogram using the variables with a P-value less than 0.05 in the multivariate analysis to facilitate clinical decision-making. This approach allowed us to identify the most significant predictors of the outcome of interest and develop a useful tool to aid in clinical management.
2.6. Model performance and internal validation
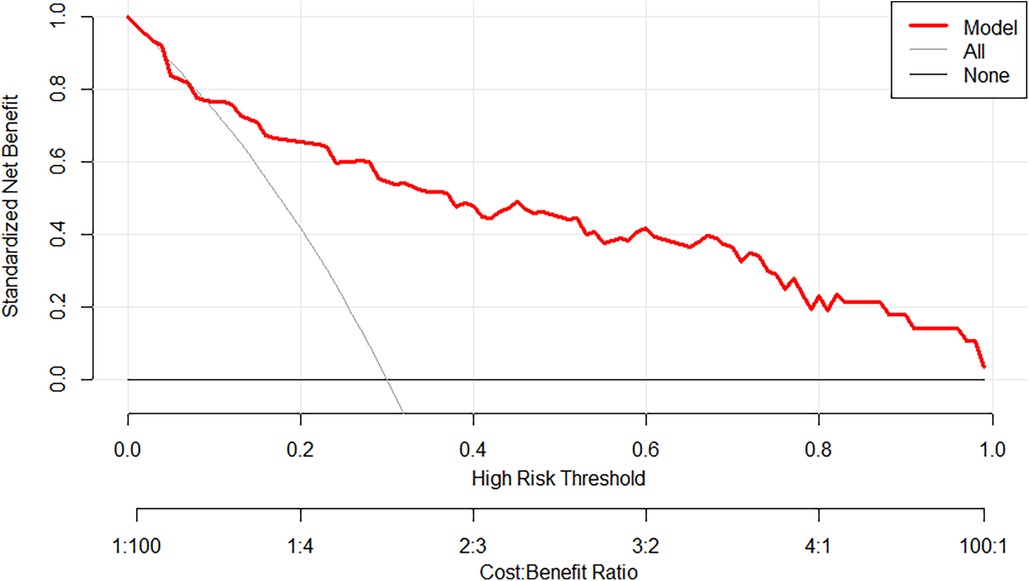
To assess the performance of the developed nomogram for predicting the probability of postoperative neurological complications in aortic surgery, we conducted internal validation using the bootstrap method with 1,000 resamples, evaluating both discrimination and calibration. The discrimination ability was assessed using the C-statistic, equivalent to the area under the receiver operating characteristic (ROC) curve (20). Calibration was assessed by plotting calibration curves and calculating the Brier score, which is the squared difference between observed and predicted probabilities (21). Furthermore, we conducted a decision curve analysis (DCA) to assess the clinical usefulness of the nomogram across various threshold probabilities. The statistical analysis was performed using IBM SPSS Statistics 26 and R.4.2.2, and significance was determined at P < 0.05. This rigorous approach enabled us to gain valuable insights into the data and identify potential predictors of the outcome of interest.
3. Results
3.1. Patients baseline characteristics
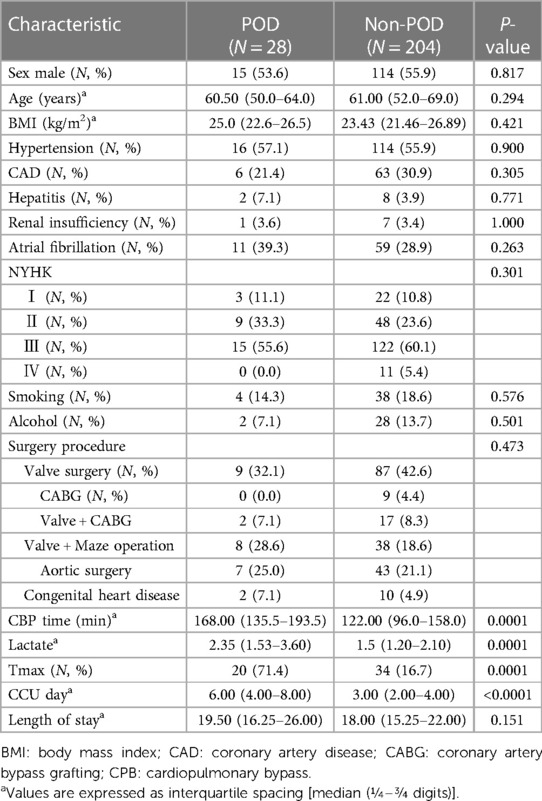
During the research period from February 1, 2023, to April 14, 2023, our analysis included a total of 232 patients, as shown in Figure 1. Preoperative risk factors, such as age, gender, BMI, hypertension, NYHA class, as well as important intraoperative risk factors, including surgical category and cardiopulmonary bypass time (CPB), were identified, as presented in Table 1. The overall incidence of POD was found to be 12.1%, as shown in Table 1, and was significantly associated with CPB and postoperative lactate levels. Moreover, there were significant variations in Tmax between the POD and Non-POD groups. POD was also found to be related to ICU length of stay.
3.2. Identifying predictors
The results of multivariate analysis for POD are listed in Table 2, For this phase of the analysis, three variables were determined to be statistically significant. Multivariate analysis identified that lactate [Odds ratio (OR) = 1.787, 95% CI, 1.192–2.785], Tmax (OR = 11.290, 95% CI, 4.369–32.129), and CPB time (OR = 1.015, 95% CI, 1.004–1.026) were independent predictors for POD (Table 2).
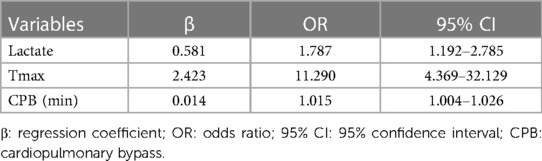
Table 2. Multivariable logistic regression analysis of independent risk factors for POD after cardiac surgery.
3.3. Model performance and internal validation
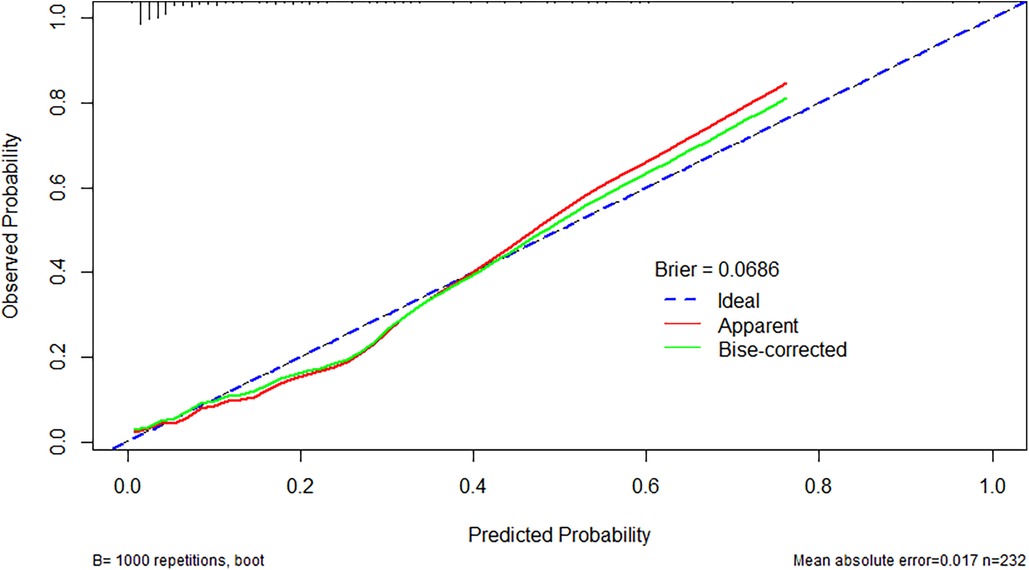
The prediction model exhibited a C-statistic value of 0.852 (95% CI, 0.763–0.941), demonstrating excellent discriminatory power. Sensitivity and specificity, based on the area under the receiver operating characteristic (AUROC) curve, were 91.2% and 67.9%, respectively (Figure 2). The apparent calibration curve closely approximated the ideal 45° line, indicating consistent agreement between observed and predicted probabilities within the development cohort (Figure 3). To mitigate any potential overoptimism in the model, internal validation using the 1,000 bootstrap approach was performed, which confirmed its robust discrimination ability with a Brier score of 0.0686 (Figure 3). Utilizing these three candidate variables, we constructed a nomogram for predicting the probability of postoperative delirium (Figure 4). Furthermore, decision curve analysis demonstrated a favorable net clinical benefit (Figure 5).
4. Discussion
Postoperative fever after cardiac surgery is a well-known phenomenon (22, 23). It primarily arises from surgical tissue injury and the release of pro-inflammatory cytokines during CPB (22, 24, 25). Consequently, the etiology of fever in the majority of cases is non-infectious (26), particularly within the first 48 h post-surgery (27). While infections appear to be relatively rare (22, 23, 28), they represent a significant complication for patients with implanted cardiac prosthetic devices, being associated with high incidence and mortality rates (27, 29). Therefore, empirical antibiotic therapy is frequently initiated in patients experiencing postoperative fever after cardiac surgery, especially when prosthetic materials are used, potentially leading to overtreatment. Despite the recognized significance of CPB in the development of postoperative inflammation and fever following certain types of cardiac surgeries involving prosthetic materials, a comprehensive evaluation of the natural course of postoperative inflammation and fever related to CPB and implanted prosthetic materials is yet to be undertaken.
Although postoperative fever following cardiac surgery is a common occurrence (30), with an incidence as high as 38%, its etiology and significance remain incompletely understood (31). There are competing theories regarding its underlying pathophysiology. Fever may reflect an inflammatory response, which could be attributed to the surgical trauma itself or to the interaction between blood and foreign surfaces within the cardiopulmonary bypass (CPB) circuit (25, 32). Additionally, fever may serve as an indicator of altered hypothalamic thermoregulatory center function, signaling brain injury (33, 34).
Regardless of the underlying causes, fever has been demonstrated to be associated with adverse postoperative complications (25), including unfavorable cerebral outcomes (34, 35). In a recent study involving 300 patients, we described a significant relationship between postoperative hyperthermia at 6 weeks following coronary artery bypass graft surgery and decline in neurocognitive function (25). The association between fever and stroke following bypass surgery remains unclear. However, even mild hyperthermia (1–2°C) in non-cardiac surgical cases has been shown to result in poorer outcomes, such as increased infarct size, deteriorating neurological function, and elevated mortality rates (25, 36).
The fluctuation in serum lactate levels serves as a reliable prognostic biomarker for mortality in critically injured patients (37). Another study demonstrates that lactate values reflect ischemia reperfusion more rapidly and reliably than novel biomarkers (38). Elevated lactate levels in cardiac surgery patients during the perioperative period are associated with adverse postoperative outcomes. Perioperative lactate levels can serve as a predictor for the occurrence of POD in elderly trauma patients (39, 40). In our study, postoperative hyperlactatemia reflects the circulatory state during surgery and therefore correlates with the development of POD. Our research findings are consistent with these study results.
5. Conclusion
In conclusion, our study findings indicate that POD is highly prevalent among cardiac surgery patients. Postoperative lactate levels, cardiopulmonary bypass duration, and postoperative fever emerge as independent predictive factors for the development of postoperative delirium. Furthermore, the identification of postoperative fever, which is one of the intraoperative variables, may be related with the occurrence of POD.
6. Limitation
In summary, our study has some limitations that should be taken into consideration when interpreting the findings. Firstly, our study was performed at a single center, which could potentially restrict the generalizability of the findings. Secondly, the relatively small sample size could have an impact on the statistical power of the study. Additionally, the study's observational design prevents the establishment of causal relationships, and there may be additional factors not considered in the analysis. External validation of the predictive nomogram is necessary before its clinical implementation.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Institutional review board of The Nanjing Drum Tower Hospital of the Affiliated Hospital of Nanjing University Medical School. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
Y-pW and B-bS conducted a comprehensive literature review and performed the statistical analysis. D-jW, MG, and Z-yW were responsible for the study's conception and design. HJ, SL, and QL carried out data collection and managed the database. Y-pW and C-cZ drafted the manuscript. Y-pW and QL made substantial contributions to manuscript revisions and finalization. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by Jiangsu Province Capability Improvement Project through Science, Technology and Education (ZDXK202229) and supported by fundings for Clinical Trials from the Affiliated Drum Tower Hospital, Medical of School of Nanjing University (2022-LCYJ-MS-12).
Acknowledgments
Our research team would like to express our gratitude to Zhihua Zhang's team at the Department of Epidemiology and Biostatistics, School of Public Health, Anhui Medical University for their valuable assistance in conducting the statistical analysis for this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1237055/full#supplementary-material
References
1. Naik R, Ely E, Elavarasi A. Sedoanalgesia and delirium. In: Text book of critical care. New Delhi: Jaypee (2016). p. 116–30.
2. Evans AS, Weiner MM, Arora RC, Chung I, Deshpande R, Varghese R, et al. Current approach to diagnosis and treatment of delirium after cardiac surgery. Ann Card Anaesth. (2016) 19:328–37. doi: 10.4103/0971-9784.179634
3. Santos FS, Velasco IT, Fráguas R Jr. Risk factors for delirium in the elderly after coronary artery bypass graft surgery. Int Psychogeriatr. (2004) 16:175–93. doi: 10.1017/S1041610204000365
4. Hudetz JA, Patterson KM, Iqbal Z, Gandhi SD, Byrne AJ, Hudetz AG, et al. Ketamine attenuates delirium after cardiac surgery with cardiopulmonary bypass. J Cardiothorac Vasc Anesth. (2009) 23:651–7. doi: 10.1053/j.jvca.2008.12.021
5. Smith LW, Dimsdale JE. Postcardiotomy delirium: conclusions after 25 years? Am J Psychiatry. (1989) 146:452–8. doi: 10.1176/ajp.146.4.452
6. Prakanrattana U, Prapaitrakool S. Efficacy of risperidone for prevention of postoperative delirium in cardiac surgery. Anaesth Intensive Care. (2007) 35:714–9. doi: 10.1177/0310057X0703500509
7. Afonso A, Scurlock C, Reich D, Raikhelkar J, Hossain S, Bodian C, et al. Predictive model for postoperative delirium in cardiac surgical patients. Semin Cardiothorac Vasc Anesth. (2010) 14:212–7. doi: 10.1177/1089253210374650
8. Murray AM, Levkoff SE, Wetle TT, Beckett L, Cleary PD, Schor JD, et al. Acute delirium and functional decline in the hospitalized elderly patient. J Gerontol. (1993) 48:M181–6. doi: 10.1093/geronj/48.5.m181
9. McCusker J, Cole M, Dendukuri N, Belzile É, Primeau F. Delirium in older medical inpatients and subsequent cognitive and functional status: a prospective study. CMAJ. (2001) 165:575–83.11563209
10. Eden BM, Foreman MD. Problems associated with underrecognition of delirium in critical care: a case study. Heart Lung. (1996) 25:388–400. doi: 10.1016/S0147-9563(96)80082-3
12. Tan MC, Felde A, Kuskowski M, Ward H, Kelly RF, Adabag AS, et al. Incidence and predictors of post-cardiotomy delirium. Am J Geriatr Psychiatry. (2008) 16:575–83. doi: 10.1097/JGP.0b013e318172b418
13. Koster S, Oosterveld FG, Hensens AG, Wijma A, van der Palen J. Delirium after cardiac surgery and predictive validity of a risk checklist. Ann Thorac Surg. (2008) 86:1883–7. doi: 10.1016/j.athoracsur.2008.08.020
14. Keijmel SP, Zwartkruis IM, Jongenotter J, Geuzebroek GS, Kouijzer IJ. Postoperative inflammation and fever after elective aortic valve and aortic root replacement: a retrospective cohort study. Open Forum Infect Dis. (2023) 10:ofad015. doi: 10.1093/ofid/ofad015
15. Gao Y, Gong S, Zhou W, Li X, Gan X. Frequency and risk factors of subsyndromal delirium in the intensive care units: a prospective cohort study. Neuropsychiatr Dis Treat. (2023) 19:1003–16. doi: 10.2147/NDT.S407156
16. Brown CH IV. Delirium in the cardiac surgical intensive care unit. Curr Opin Anaesthesiol. (2014) 27:117. doi: 10.1097/ACO.0000000000000061
17. Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. (1990) 113:941–8. doi: 10.7326/0003-4819-113-12-941
18. Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, et al. Evaluation of delirium in critically ill patients: validation of the confusion assessment method for the intensive care unit (CAM-ICU). Crit Care Med. (2001) 29:1370–9. doi: 10.1097/00003246-200107000-00012
19. Pang Y, Li Y, Zhang Y, Wang H, Lang J, Han L, et al. Effects of inflammation and oxidative stress on postoperative delirium in cardiac surgery. Front Cardiovasc Med. (2022) 9:1049600. doi: 10.3389/fcvm.2022.1049600
20. Pabinger I, van Es N, Heinze G, Posch F, Riedl J, Reitter EM, et al. A clinical prediction model for cancer-associated venous thromboembolism: a development and validation study in two independent prospective cohorts. Lancet Haematol. (2018) 5:e289–98. doi: 10.1016/S2352-3026(18)30063-2
21. Steyerberg EW, Vergouwe Y. Towards better clinical prediction models: seven steps for development and an ABCD for validation. Eur Heart J. (2014) 35:1925–31. doi: 10.1093/eurheartj/ehu207
22. Livelli FD Jr., Johnson RA, McEnany MT, Sherman E, Newell J, Block PC, et al. Unexplained in-hospital fever following cardiac surgery. Natural history, relationship to postpericardiotomy syndrome, and a prospective study of therapy with indomethacin versus placebo. Circulation. (1978) 57:968–75. doi: 10.1161/01.cir.57.5.968
23. Andrade C, Olvera S, Reyes P. Fever and infection after heart surgery. A prospective study of 75 cases. Arch Inst Cardiol Mex. (1989) 59:487–91.2604490
24. Warltier DC, Laffey JG, Boylan JF, Cheng DC. The systemic inflammatory response to cardiac surgery: implications for the anesthesiologist. J Am Soc Anesthesiol. (2002) 97:215–52.
25. Mitchell JD, Grocott HP, Phillips-Bute B, Mathew JP, Newman MF, Bar-Yosef S. Cytokine secretion after cardiac surgery and its relationship to postoperative fever. Cytokine. (2007) 38:37–42. doi: 10.1016/j.cyto.2007.04.009
26. Mookhoek A, Korteland NM, Arabkhani B, Di Centa I, Lansac E, Bekkers JA, et al. Bentall procedure: a systematic review and meta-analysis. Ann Thorac Surg. (2016) 101:1684–9. doi: 10.1016/j.athoracsur.2015.10.090
27. Rhee C, Sax PE. Evaluation of fever and infections in cardiac surgery patients. Semin Cardiothorac Vasc Anesth. (2015) 19:143–53. doi: 10.1177/1089253214538524
28. Miholic J, Hiertz H, Hudec M, Laczkovics A, Domanig E. Fever, leucocytosis and infection after open heart surgery. A log-linear regression analysis of 115 cases. Thorac Cardiovasc Surg. (1984) 32:45–8. doi: 10.1055/s-2007-1023343
29. Machelart I, Greib C, Wirth G, Camou F, Issa N, Viallard JF, et al. Graft infection after a Bentall procedure: a case series and systematic review of the literature. Diagn Microbiol Infect Dis. (2017) 88:158–62. doi: 10.1016/j.diagmicrobio.2017.03.002
30. O’Mara SK. Management of postoperative fever in adult cardiac surgical patients. Dimens Crit Care Nurs. (2017) 36:182–92. doi: 10.1097/DCC.0000000000000248
31. Thong WY, Strickler AG, Li S, Stewart EE, Collier CL, Vaughn WK, et al. Hyperthermia in the forty-eight hours after cardiopulmonary bypass. Anesth Analg. (2002) 95:1489–95. doi: 10.1097/00000539-200212000-00006
32. Hindman BJ. Emboli, inflammation, and CNS impairment: an overview. Heart Surg Forum. (2002) 5:249–53.12538140
33. Beamer NB, Coull BM, Clark WM, Hazel JS, Silberger JR. Interleukin-6 and interleukin-1 receptor antagonist in acute stroke. Ann Neurol. (1995) 37:800–5. doi: 10.1002/ana.410370614
34. Grocott HP, Mackensen GB, Grigore AM, Mathew J, Reves J, Phillips-Bute B, et al. Postoperative hyperthermia is associated with cognitive dysfunction after coronary artery bypass graft surgery. Stroke. (2002) 33:537–41. doi: 10.1161/hs0202.102600
35. Cook DJ. Cerebral hyperthermia and cardiac surgery: consequences and prevention. Semin Thorac Cardiovasc Surg. (2001) 13:176–83. doi: 10.1053/stcs.2001.23557
36. Reith J, Jorgensen HS, Pedersen PM, Nakayama H, Raaschou HO, Jeppesen LL, et al. Body temperature in acute stroke: relation to stroke severity, infarct size, mortality, and outcome. Lancet. (1996) 347:422–5. doi: 10.1016/s0140-6736(96)90008-2
37. Régnier M-A, Raux M, Le Manach Y, Asencio Y, Gaillard J, Devilliers C, et al. Prognostic significance of blood lactate and lactate clearance in trauma patients. J Am Soc Anesthesiologists. (2012) 117:1276–88. doi: 10.1097/ALN.0b013e318273349d
38. Balcı E, Demir ZA, Yiğit Özay H, Vardar K, Karduz G, Aksu U, et al. Effects of upper limb ischemia-reperfusion on regional oxidative stress during aortic surgery with moderate hypothermia. J Card Surg. (2021) 36:1361–9. doi: 10.1111/jocs.1540
39. Ozay HY, Bindal M, Turkkan S, Beyoglu MA, Yekeler E, Turan S. Delirium development after lung transplantation: an intraoperative assessment. Transplant Proc. (2022) 7:1906–12. doi: 10.1016/j.transproceed.2022.03.069
Keywords: cardiac surgery, fever, CPB, postoperative delirium, prediction model
Citation: Wang Y-p, Shen B-b, Zhu C-c, Li L, Lu S, Wang D-j, Jin H, Liu Q, Wang Z-y and Ge M (2023) Unveiling the nexus of postoperative fever and delirium in cardiac surgery: identifying predictors for enhanced patient care. Front. Cardiovasc. Med. 10:1237055. doi: 10.3389/fcvm.2023.1237055
Received: 8 June 2023; Accepted: 25 October 2023;
Published: 10 November 2023.
Edited by:
Marija Vavlukis, University Clinic for Cardiology, Ss. Cyril and Methodius University in Skopje, North MacedoniaReviewed by:
Biljana Kuzmanovska, Saints Cyril and Methodius University of Skopje, North MacedoniaMirjana Shosholcheva, Saints Cyril and Methodius University of Skopje, North Macedonia
Gereon Schälte, University Hospital RWTH Aachen, Germany
© 2023 Wang, Shen, Zhu, Li, Lu, Wang, Jin, Liu, Wang and Ge. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hua Jin jhdqq2011@qq.com Qi Liu lq243727710@163.com Zhe-yun Wang wangzheyungl@163.com Min Ge gemin2000@outlook.com
†These authors have contributed equally to this work
 Ya-peng Wang
Ya-peng Wang Bei-bei Shen2,†
Bei-bei Shen2,†