The hidden (overlooked) impact of living through a pandemic: How parents of children with disabilities fared during COVID-19?
- 1Department of Specialized Education Services, University of North Carolina at Greensboro, Greensboro, NC, United States
- 2Department of Special Education, Ondokuz Mayıs University, Samsun, Turkey
- 3Department of Special Education, Çanakkale Onsekiz Mart University, Çanakkale, Turkey
- 4Department of Special Education, Kilis 7 Aralık University, Kilis, Turkey
- 5Department of Educational Science, Kilis 7 Aralık University, Kilis, Turkey
- 6Department of Child Care and Youth Services, Ondokuz Mayıs University, Samsun, Turkey
Objective: The purpose of this study was to investigate the impact of the COVID-19 pandemic on the quality of life of families of children with disabilities and the mediating roles of perceived social support, perceived parental self-efficacy, psychological health, psychological resilience, and perceived family burden on this relationship.
Background: Children with disabilities and their families are among the most affected populations from the restrictions imposed to prevent the spread of COVID-19 virus, as the special education and rehabilitation services they had been receiving were interrupted.
Method: A correlational survey design was used to collect data from 824 parents of children with disabilities in Turkey. Path analysis was used to examine the direct and indirect effects of COVID-19 on family quality of life.
Results: Results indicated that COVID-19 had a significant total effect on family quality of life and perceived social support, parental self-efficacy and psychological resilience had a mediating role on the relationship between impact of the COVID-19 pandemic and family quality of life. Perceived social support was found to the strongest mediator of the relationship between the impact of COVID-19 and the family quality of life, while perceived family burden did not have a statistically significant association with these variables.
Conclusion: Family quality of life for children with disabilities decreased as the impact of COVID-19 pandemic increased. Perceived social support, parental self-efficacy and psychological resilience had mediating roles in the relationship between the impact of the COVID-19 pandemic and family quality of life.
Implications: COVID-19 has resulted in disruption of special education and rehabilitation services for children with disabilities and their families. Changes in daily routines have brought up additional responsibilities to parents of children with disabilities. These additional responsibilities may adversely affect and increase the burden and stress families of children with disabilities experience. The high levels of stress in families negatively affect the welfare and quality of life and result in decreased parental attention to support their children. Findings of this study show the mediating link of perceived social support, parental self-efficacy and psychological resilience in the relationship between the impact of the COVID-19 pandemic and family quality of life. Policymakers and service providers should develop and implement specific care actions to support children with disabilities and their families during and after the pandemic.
Introduction
Traumatic events such as wars, natural disasters, or outbreaks can result in changes in the current order of society and have a negative impact on the way in which people live. For example, the H1N1 virus outbreak that emerged in 2009 negatively affected societies and reduced people’s quality of life (van Hoek et al., 2011). Similarly, the COVID-19 pandemic, which emerged in Wuhan, a city in Hubei province of China caused many people to worry about the disease; social distancing and other measures were taken to prevent the spread of the virus and seriously affected a large part of the global population. Chronic or long-lasting natural disasters such as epidemics are considered to be the second type of traumatic event a person can experience (Volpe, 1996). In this context, it is possible to consider the COVID-19 pandemic as a traumatic experience. Research evidence suggests that when a traumatic event occurs a person’s thought process can change (Zimbardo et al., 2012); post-traumatic stress disorder (Dekel and Monson, 2010), depression (Lilly et al., 2011) and various psychological symptoms can be seen in individuals after traumatic experiences, and the quality of life of individuals and their families can be negatively affected. The extent of the symptoms varies (Janoff-Bulman, 1992) and mediated by factors such as perceived social support, psychological health, psychological resilience, and perceived family burden (Eker, 2016).
COVID-19 pandemic, children with special needs and their families
School closures due to the COVID-19 pandemic have caused students of all levels to be deprived of face-to-face education, and this change has affected millions of children as well as their families. During the pandemic, schools have supported students’ learning through various forms of distance education, and this home-schooling process have imposed great responsibilities on families. Children with special needs are among the most affected by the COVID-19 pandemic (a traumatic event), since the basis of special education and rehabilitation services is individualization, and it is not possible to provide individualized education services based on the needs of each student using distance education practices (United Nations, 2020). Studies show that families of children with disabilities experience higher levels of stress due to the additional responsibilities of raising a child with disabilities, and this stress negatively affects the family’s wellbeing and quality of life (Osborne et al., 2008). Families of children with disabilities are required to provide more intense and systematic support to their children at home during the pandemic so that their learning is not interrupted. It is predicted that this additional responsibility, which is directly related to parental competencies, will adversely affect and increase the burden and stress of the family. When the effects of the economic, health and psychological problems brought about by the COVID-19 pandemic are added to the responsibilities for the care of their children, the families of children with disabilities who already experience higher levels of stress compared to families of typically developing children have entered an even more stressful period and their quality of life is likely to be adversely affected.
Children with special needs and their families during the pandemic in Turkey
In Turkey, shortly after the initial date of the first reported COVID-19 case in March 2020, Ministry of National Education (MoNE) declared a decision to shift from traditional face to face education to home-based distance education. The distance education in Turkey is implemented through an online platform named Education Information Network [Eğitim Bilişim Ağı (EBA)]. The EBA included course videos, virtual classes, evaluation materials, online books, and a library link. Course videos and classes were delivered both through EBA TV channels and website at a pre-determined schedule. Hundreds of course videos were recorded by special education teachers on various topics such as math, science, language, social studies, and daily life skills for children with special needs (MoNE, 2020). Despite all the measures taken, remote or distance education services were suitable and sufficient for most children with special needs, especially for those who need intensive and individualized support. Therefore, parents of children with special needs assumed a new role during the pandemic to support development and learning of their children when resources were limited.
Impact of pandemic on children with disabilities and their families
Although it is a relatively new subject, there are various studies in the literature to determine the effects of the COVID-19 pandemic, a traumatic event, on typically developing children and their families. These studies have reported that emotional (Racine et al., 2020; Yeasmin et al., 2020; Lee V. et al., 2021; Sultana et al., 2021) and behavioral problems such as anxiety and depression increased significantly in children (Patrick et al., 2020; Romero et al., 2020) and children’s quality of life decreased (Adıbelli and Sümen, 2020) with the effect of the traumatic event (i.e., COVID-19 pandemic). One of the most significant social effects of the COVID-19 pandemic is the increase in isolation between family members and its negative effect on family relationships (Ahmen et al., 2020; Uzun et al., 2021). Over time, the combination of changing parenting demands due to isolation and increased care burden can lead to increased negativity and weakened relationships between parents and their children (Prime et al., 2020).
In addition to the studies conducted with typically developing children and their families, extant literature includes studies that have examined the impact of the traumatic event, COVID-19 pandemic, on children with disabilities and their families. Findings of these studies have shown that the rapid changes in social life associated with restrictions put in place to prevent the spread of COVID-19 virus resulted in increased anxiety in families of children with disabilities and negatively impacted the mood and behaviors of both children and their families (Asbury et al., 2021; Gayatri and Irawaty, 2021). In addition, the measures taken to prevent the spread of the virus have interrupted the educational and support services children with disabilities and their families have been receiving (Jeste et al., 2020; Warner-Richter and Lloyd, 2020; Jesus et al., 2021). Researchers have also noted that inability to receive educational and support services much needed for these children and families can increase the stress level of parents (Navas et al., 2022; Werner et al., 2022) and cause behavior problems and challenges in children (Narzisi, 2020). The high levels of stress in families negatively affect the welfare and quality of life and result in decreased parental attention to support their children (Osborne et al., 2008; Ali et al., 2021; Ueda et al., 2022). This, in turn, adversely impacts the development and learning of children with disabilities (Bruder et al., 2021). Researchers have also emphasized the importance of protecting the mental health of parents and providing social supports to families during this pandemic (Gayatri and Irawaty, 2021; Navas et al., 2022) where the social support received by parents has been decreasing (Warner-Richter and Lloyd, 2020; Willner et al., 2020) while parenting stress has been increasing (Chen et al., 2020; Willner et al., 2020; Lee S. J. et al., 2021). The fact that families have very limited or no social supports due to the restrictions in place makes the effects of pandemic on child development and family life even more serious.
Factors that influence family quality of life
Family burden and social support
Described as the difficulties and challenges experienced by families as a consequence of someone’s illness (Sales, 2003), the concept of burden includes: (a) objective burdens: loss of income, restriction of social activities, disruption of family routines, and (b) subjective burdens: emotional distress about the child. Family burden is generally evaluated under four main categories that include: psychological, physical, social, and economic burden (Chou, 2000). Studies show that the family burden perceived by parents of children with disabilities increases as the social support received is decreasing (Carlson and Miller, 2017), perceived quality of life decreases with the increase in the burden of care (Tayaz and Koc, 2018), and the quality of life increases with the increase in perceived social support (Toprak, 2018). Moreover, research has shown that as the family burden increases, psychological resilience of parents of children with disabilities decreases (Bildirici, 2014) and as the social support perceived by families increases, psychological resilience increases, and psychological symptoms such as depression and anxiety decrease. In other words, increase social support positively affects psychological health (Kına, 2019). In the light of these findings, we predicted that perceived family burden and social support may have a mediating role in the relationship between the effect of the traumatic event (COVID-19 pandemic) and quality of life of children with disabilities and their families.
Psychological resilience and health
The existence of social isolation, feelings of uncertainty and perceived life threat during the pandemic may cause people to experience depression and anxiety (Xiang et al., 2020), mental health deterioration (Koçak and Harmanci, 2020); consequently, it may cause a decrease in the quality of life (Monson et al., 2017). From this point of view, in this study, the mediating role of the psychological health variable, which evaluates the depression and anxiety symptoms seen in the families of children with disabilities during the COVID-19 pandemic, was examined. Determining the mediating role of psychological health is considered important in terms of identifying psychological interventions to reduce the depression and anxiety symptoms of families of children with disabilities during the pandemic. In addition, considering that the family quality of life increases as the psychological resilience increases (Demiray, 2019), it is predicted that psychological resilience may play a mediating role in the relationship between the effect of the traumatic event and the quality of life.
Perceived parental self-efficacy
Another variable that is positively associated with quality of life noted in the literature is parental self-efficacy (Kasser and Zia, 2020; Tehranineshat et al., 2020). Perceived parental self-efficacy is the ability of a parent to fulfill the tasks related to his/her child and make a decision or believe in using his/her abilities (Montigny and Lacharité, 2004). Individuals with high self-efficacy beliefs make more effort to accomplish tasks; do not easily withdraw when faced with difficult situations; and becomes persistent and patient to complete tasks (Aksoy and Diken, 2009). For this reason, self-efficacy is considered to be a coping skill that has a significant protective effect on people exposed to trauma (Bosmans et al., 2015). Based on these findings, we predicted that perceived self-efficacy of parents may have a mediating role in the relationship between the effect of the traumatic event (COVID-19 pandemic) and family quality of life.
Current study
In contrast to the studies in the literature conducted separately with different participant groups, the present study examined the mediating effects of perceived family burden, perceived social support, psychological resilience and psychological health on the relationship between the effect of the traumatic event (COVID-19 pandemic) and family quality of life. The findings from this study have potential to contribute the efforts to reduce or eliminate the negative effects of the ongoing pandemic by providing information on how children with disabilities and their families are directly and indirectly affected. Therefore, the purpose of the current study was to examine the relationship between perceived influence of the traumatic event (COVID-19 pandemic) and quality of life of families of children with disabilities and to investigate mediating roles of parent-level variables on this relationship. The following research questions guided the present study:
1. What were the levels of influence of the traumatic event (i.e., COVID-19 pandemic), family quality of life, perceived family burden, perceived social support, psychological resilience, psychological health, and perceived parental self-efficacy for parents and families of children with disabilities during the COVID-19 pandemic?
2. What was the direct and indirect impact of the traumatic event (COVID-19 pandemic) on the quality of life of families who had children with disabilities?
3. Was the impact of the traumatic event (COVID-19 pandemic) on family quality of life mediated by perceived family burden, perceived social support, psychological resilience, psychological health, and perceived parental self-efficacy?
Methods
Participants and recruitment
A total of 824 parents of children with disabilities participated in the present study. To recruit participants, researchers contacted the administrators of special education schools located in seven different cities, each representing one geographic area in Turkey; explained the purpose and procedures of the study; and provided informed consent forms, a link for the online questionnaire, and paper copies of the questionnaire used to collect data. School administrations or teachers provided parents with information about the study. Those who were willing to participate in the study completed the online or paper forms and returned them to the schools or researchers. Recruitment activities resulted in 853 parents of children with disabilities completing and returning the survey. A total of 29 questionnaires completed using the paper forms were excluded from the study due to incomplete data. Nineteen forms were excluded because the Demographic Information Form was not completed at all or in its entirety and 10 forms were excluded as more than 50% of the items across the forms were missing. Therefore, data obtained from 824 parents of children with disabilities were included in the analysis. Of the 824 questionnaires, 570 (67%) were completed using paper forms while 283 (33%) were completed using the online forms. Investigation of mean scale scores obtained from online or paper forms resulted in no significant difference between the two methods of data collection. Of the 824 parents, 733 (89%) were mothers and 91 (11%) were fathers. The mean age of participants was 38.80 (SD = 7.34), range = 22–66 years). Demographic information about participating parents is provided in Table 1.
Participants had a total of 926 children with disabilities. Of those, 600 were boys (65%) and 295 were girls (32%). Children were diagnosed with a variety of different disabilities including autism (24%), intellectual disability (23%), learning disabilities (18%), speech and language disorder (11%), multiple disabilities (7%), attention deficit/hyperactivity disorder (6%), physical disability (5%), hearing impartment (4%), and visual impairment (1%). Severity of the disability they had ranged from mild (39%) to moderate (38%) to severe (17%). At the onset of the study, 28% of children attended to preschool programs, 34% attended to primary schools, 16% attended to middle schools and 11% attended to high schools.
Instruments
Seven different data collection tools were used to collect data in this study. These included: (1) Demographic Information Form, (2) Impact of Event Scale, (3) Family Quality of Life Scale, (4) Family Burden Assessment Scale, (5) Revised Parental Social Support Scale, (6) General Health Questionnaire, and (7) Brief Resilience Scale. Brief information about each data collection instrument is provided below.
Demographic Information Form
Developed by the research team, this form was used to collect demographic information about children with disabilities, their parents, and other family members from the parents who participated in the study. The form included items about participants’ age, gender, education and job status (items 1–17), their perceived parental self-efficacy (item 25; 10-point Likert scale, 1 – I am not competent at all and 10 – I am very competent) and the impact of pandemic in child development and learning (items 26–30; 10-point Likert scale, 1 – Not affected at all and 10 – Highly affected).
Impact of Event Scale-Revised
Originally developed by Horowitz et al. (1979) to measure the degree of distress an individual feels in response to trauma, the IES was revised twice by Weiss and Marmar (1997) and Creamer et al. (2003). The revised form was adapted into Turkish by Çorapçıoğlu et al. (2006). The scale includes 22 items under three subscales (i.e., Intrusion, Avoidance, and Hyperarousal) and each item is rated using a 5-point Likert scale (0 – Not at all to 4 – Extremely). Scale total score ranges between 0 and 88 and higher scores indicate increased impact of distress due to the traumatic event. The Cronbach’s alpha internal consistency coefficient was 0.94 for entire scale and ranged between 0.87 and 0.94 for subscales (Çorapçıoğlu et al., 2006). In the present study, the Impact of Event Scale-Revised (IES-R) was used to measure the impact of COVID-19 pandemic, a traumatic event, on quality of life of families with children with disabilities.
Family Quality of Life Scale
The Family Quality of Life Scale (FQLS) was developed by Hoffman et al. (2006) to assess family ratings of importance and satisfaction with five domains in relation to quality of life: Family Interaction, Parenting, Emotional Well-Being, Physical/Material Well-Being, and Disability-Related Supports. Meral and Cavkaytar (2013) adapted the scale into Turkish. The FQLS includes 25 items rated on a 5-point Likert scale (1 = Very dissatisfied and 5 = Very satisfied). Scale total score ranges between 25 and 125 and higher scores indicate an increased quality of life. The Cronbach’s alpha internal consistency coefficient was 0.92 for entire scale and ranged between 0.71 and 0.81 for subscales (Meral and Cavkaytar, 2013). In the present study, the FQLS was used to evaluate quality of life of families of children with disabilities during COVID-19 pandemic and how it was impacted and mediated by different variables.
Family Burden Assessment Scale
The scale was developed by Yıldırım-Sarı and Başbakkal (2008) to measure the family burden perceived by parents of children with disabilities. The scale consists of 43 items and subscales: Economic Burden, Perception of Inadequacy, Social Burden, Physical Burden, Emotional Burden, and Time Requirement. In this study, 29 items under four subscales (i.e., Economic Burden, Physical Burden, Emotional Burden, and Time Requirement) were used. The items on the scale are rated using a 5-point Likert scale (1 = Never and 5 = Always). Scale score for 29 items ranges between 29 and 155, higher scores indicating increased family burden. The Cronbach’s alpha internal consistency coefficient was 0.92 while the test-retest reliability coefficient was 0.98. The internal consistency coefficients for the four subscales ranged between 0.72 and 0.89 (Yıldırım-Sarı and Başbakkal, 2008). In this study, the Family Burden Assessment Scale (FBAS) was used based on the assumption that there may be a change in perceived family burden due to the interruption of children’s education during the COVID-19 pandemic, and that the perceived level of family burden may play a mediating role in the effects of the COVID-19 pandemic on the quality of family life.
Revised Parental Social Support Scale
The scale was developed by Kaner (2010) to assess perceptions of parents of children with disabilities about social support they receive. The Revised Parental Social Support Scale (PSSS-R) consists of two parts: perceived social support and satisfaction with social support. The perceived social support part consisted of 28 items under 4 subscales (Social Companionship Support, Information Support, Emotional Support, and Care Support) was used in the present study. The items in the scale were rated using a 4-point Likert scale (1 = Not at all and 4 = Always present). Scale score for 28 items ranges between 28 and 122, higher scores indicating increased social support. The Cronbach’s alpha internal consistency coefficients for the four subscales ranged between 0.84 and 0.96 and Spearman–Brown split half reliability coefficients ranged from 0.86 to 0.92 (Kaner, 2010). In this study, The PSSS-R was used based on the assumption that while the social support needed by families of children with disabilities increases during the COVID-19 pandemic, actual social support they receive has decreased and that level of perceived social support play a mediating role in the effects of the COVID-19 pandemic on the quality of family life.
General Health Questionnaire
The General Health Questionnaire (GHQ) was developed by Goldberg (1972) to detect symptoms of psychological health problems such as depression and anxiety. The scale has 12, 28, 30, and 60-question forms. The 12-item was adapted into Turkish by Kilic et al. (1997). The items on the scale are rated using a 4-point Likert scale (0 = Not at all and 3 = Very often). Scale total score ranges between 0 and 36 and higher scores indicate increased risk for psychological health issues. The Cronbach’s alpha internal consistency coefficient was 0.88 for the scale (Kilic et al., 1997). In this study, the GHQ was used to examine how the psychological health of families with children with disabilities was affected and how psychological health affected other variables during the COVID-19 pandemic.
Brief Resilience Scale
Scale was developed by Smith et al. (2008) to measure individuals’ ability to bounce back or recover from stressful life events and adapted into Turkish by Doğan (2015). The Brief Resilience Scale (BRS) includes 6 items under one dimension; each item is rated using a 5-point Likert type scale (1 = strongly disagree and 5 = strongly agree). Scale total score ranges between 6 and 30 and higher scores indicate increased psychological resilience. The Cronbach’s alpha internal consistency coefficient was 0.83 for the scale (Doğan, 2015). In this study, the BRS was used based on the assumption that psychological resilience is an important factor helping families of children with disabilities to cope with the difficulties faced during the COVID-19 pandemic and that the psychological resilience of families may play a mediating role in the relationship between effects of the COVID-19 pandemic and the quality of family life.
Data collection and analysis
Following the approvals from the institutional review board of Ondokuz Mayıs University and the Ministry of National Education, the researchers distributed the online and paper surveys to potential participants using the procedures described in section “Participants and recruitment” above. Data collection activities lasted 4 months between August and November 2020. Data collected though the online questionnaire were downloaded as a spreadsheet from the survey system. Data collected using paper forms entered into the same spreadsheet by two researchers. Once the data entry was completed, the spreadsheet was cleaned and transferred into data analysis software. SPSS version 27 was used to calculate descriptive statistics and check assumptions for the path analysis while Mplus version 7 was used for path analysis.
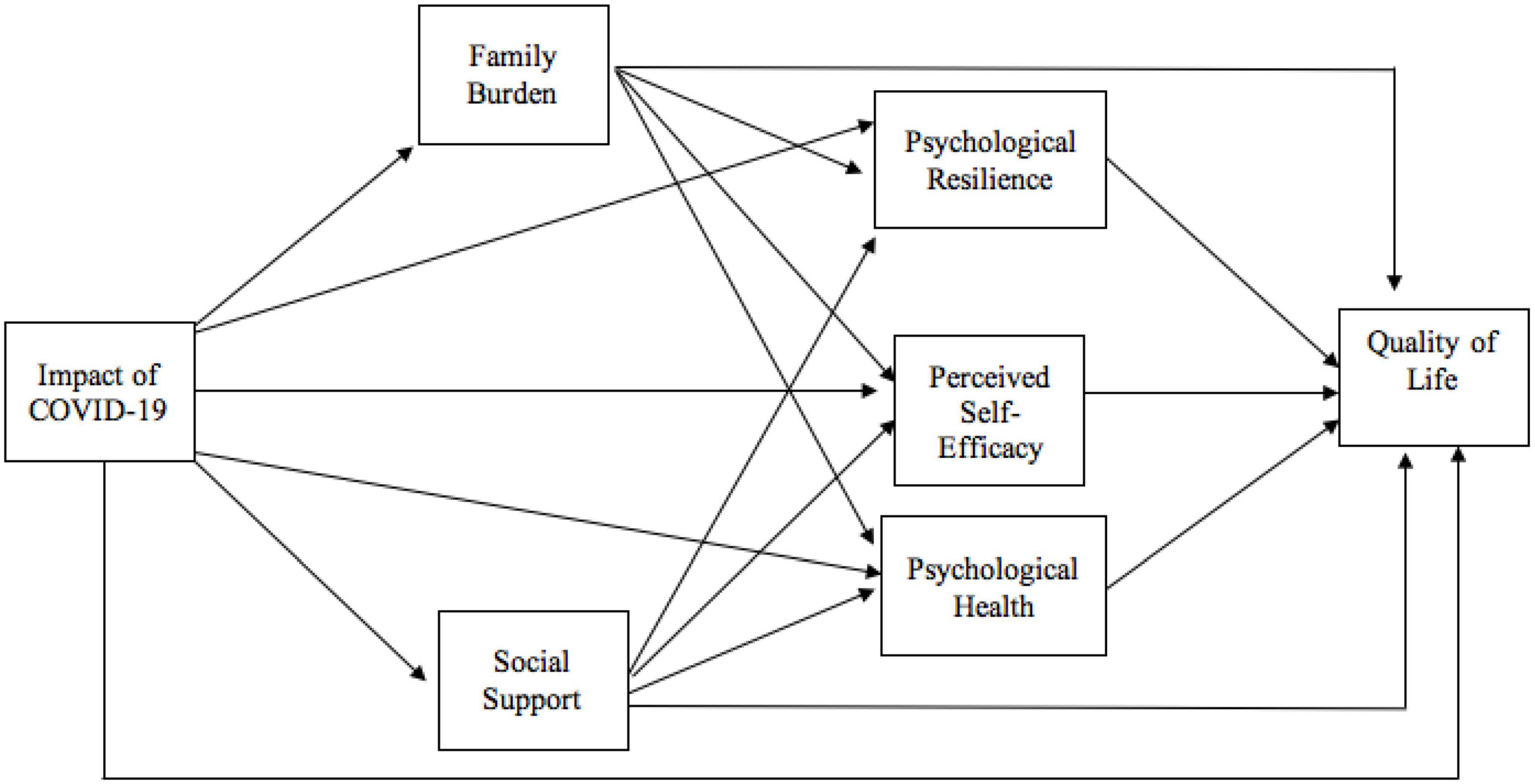
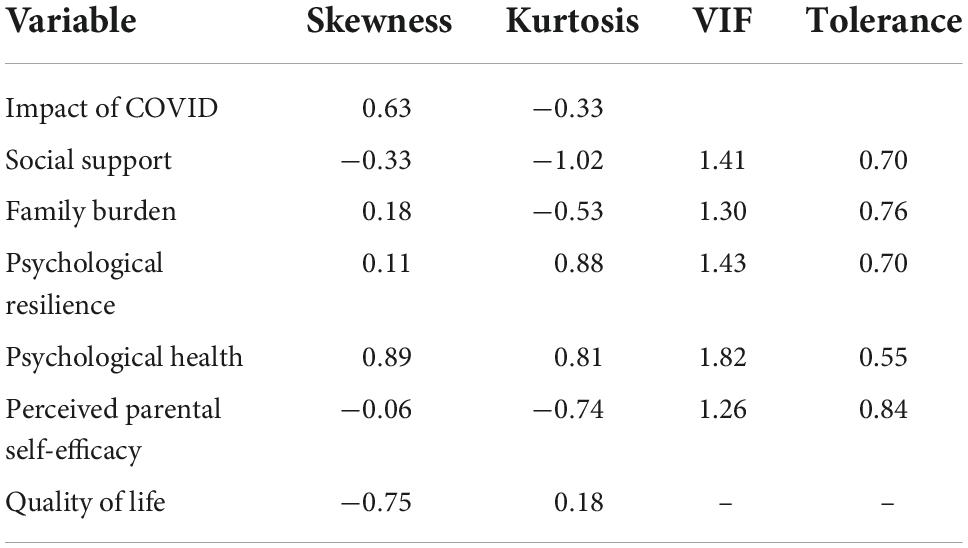
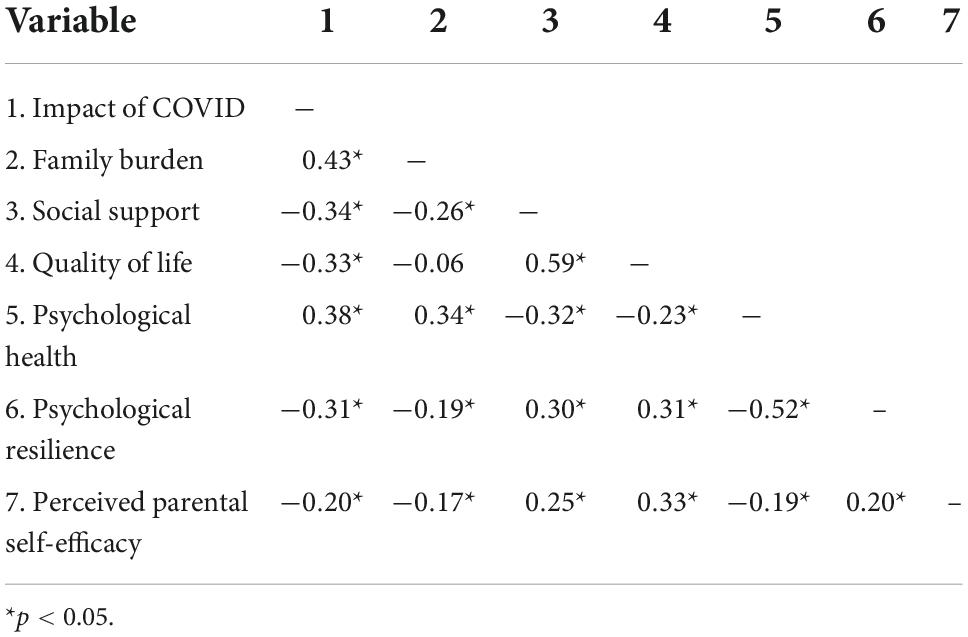
In terms of the data analysis, first, the theoretical path analysis shown in Figure 1 was tested. In this initial model, the impact of COVID-19 was the exogenous variable while the other variables were the endogenous variables. It was hypothesized that (1) there should be direct and indirect effects from the impact of COVID-19 to quality of life and (2) indirect effects are mediated through (a) perceived social support and family burden, and (b) psychological resilience, psychological health and perceived parental self-efficacy. Prior to testing the model, three assumptions of the path analysis (i.e., multivariate normality, linearity, and multicollinearity) were checked. For multivariate normality assumption, skewness, and kurtosis values (see Table 2) as well as normal PP and QQ plots were examined for all variables. To check the linearity assumption, bivariate correlations between each of the studied variables and outcome variable (i.e., quality of life) were computed (see Table 3). For multicollinearity assumption, bivariate correlations between variables, variance inflation factor (VIF) and tolerance values were examined (see Tables 2, 3).
As seen in Table 2, all skewness and kurtosis values were between −2 and 2 indicating that normality assumption were met for all variables. Similarly, normal PP and QQ plots also indicated no concerns of non-normality. In terms of multicollinearity assumption, there were not very high bivariate correlation (e.g., r > 0.95) between any of the variables (see Table 3); all VIF values were between 1 and 10; and all tolerance values were higher than 0.10 (Hair et al., 1998), indicating that this assumption was also met. When the bivariate correlations among variables presented in Table 3 were examined, it was seen that all variables had significant association with the quality of life except family burden indicating that the linearity assumption was met for all variables other than family burden variable. Thus, the family burden variable was removed from the hypothesized model shown in Figure 1 and the path analysis model was run without this variable.
The fit indices of the new model were found to be chi square: χ2 (3) = 163.97 and p < 0.01, CFI = 0.86, TLI = 0.32, RMSEA = 0.25, and SRMR = 0.07. Based on the historical criteria suggested by Kline (2005) for the evaluation of model-fit [χ2 p > 0.05, Comparative Fit Index (CFI) > 0.95, Tucker-Lewis Index (TLI) >0.95, Root Mean Square Error of Approximation (RMSEA) = 0.06, and Standardized Root Mean Square Residual (SRMR) = 0.08], the model-fit statistics for the new path model was determined to be poor. Thus, the model was modified further; a path from psychological resilience to psychological health was added based on the statistical and theoretical suggestions (see Figure 2). The fit indices of for this path model were chi-square: χ2 (2) = 0.53 and p = 0.77, CFI = 1.00, TLI = 1.00, RMSEA = 0.0.01 with a 90% CI of (0.00, 0.04) and SRMR = 0.01. Based on the historical criteria described above, these model-fit statistics were determined to be very good. This new model was named as the final path model (see Figure 2) and used for the analysis in this study. A bootstrap with 1,000 iterations was carried out to obtain coefficients of total, direct, and indirect effects. Due to bootstrapping, unstandardized coefficients were provided in the results. Annotated Mplus codes, standardized path coefficients and data used for analyses are available upon request.

Figure 2. Final path model. Dashed line represents modification; *p < 0.05; all effects are unstandardized effects.
Results
Descriptive analysis
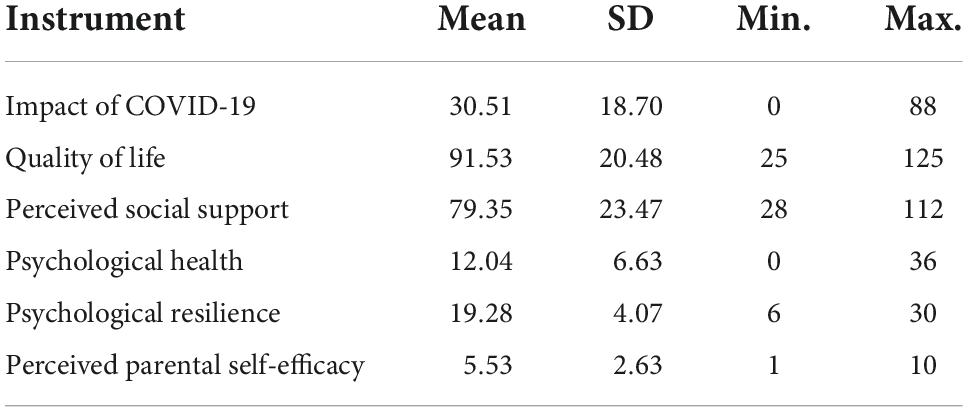
Descriptive statistics were calculated for each variable included in the final path model and the results were presented in Table 4. The mean score obtained from the Impact of Event Scale-Revised was 30.51 (SD = 18.79) indicating mild impact of COVID-19 on families while the mean score obtained from the Family Quality of Life Scale was 91.53 (SD = 20.48) indicating moderately high quality of life for families of children with disabilities during COVID-19 pandemic.
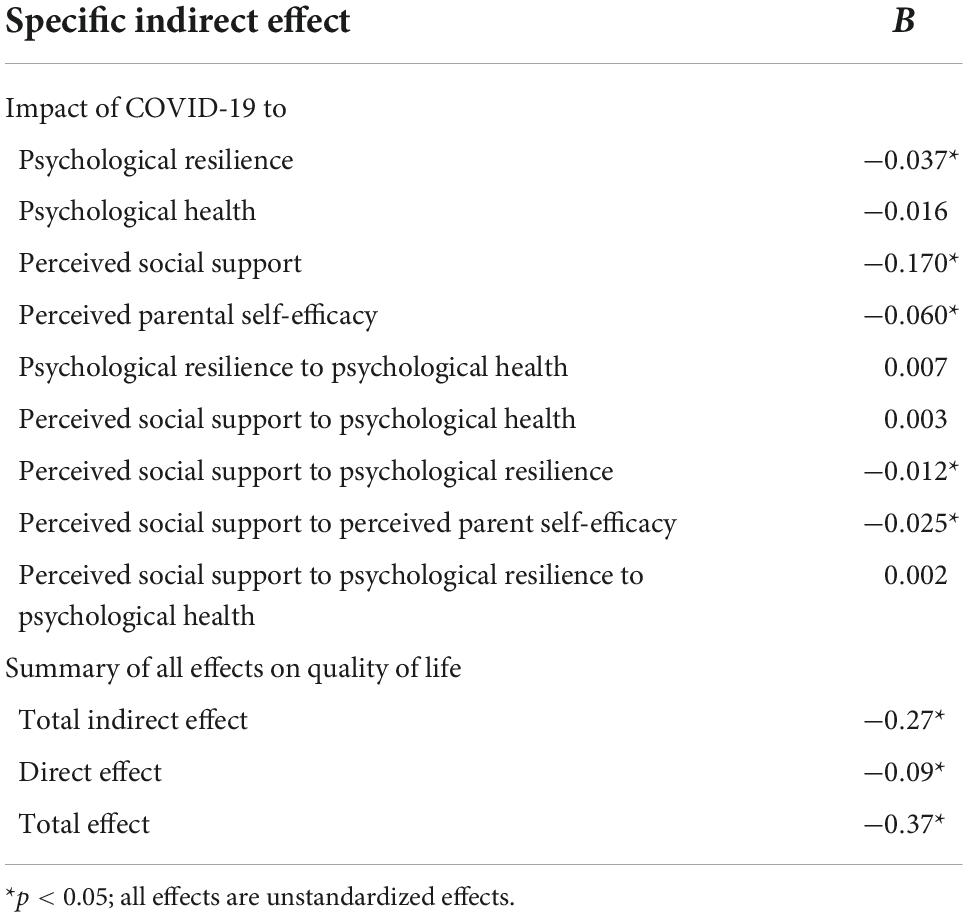
Results of direct, indirect, and total effects
As shown in Table 5, the traumatic event (COVID-19) had a significant total effect on family quality of life (B = −0.36). The −0.36 effect on quality of life was partially direct (−0.09) and partially indirect (−0.27). Both direct and total indirect effects were significant (p < 0.05). There were nine specified indirect paths from the impact of COVID to the family quality of life, four of which were not statistically significant. The five significant pathways were (a) impact of COVID to psychological resilience to quality of life with an indirect component of −0.037, (b) impact of COVID to perceived social support to quality of life with an indirect component of −0.17, (c) impact of COVID to perceived parental self-efficacy to quality of life with an indirect component of −0.06, (d) impact of COVID to perceived social support to psychological resilience to quality of life with an indirect component of −0.012, and (e) impact of COVID to perceived social support to perceived parental self-efficacy to quality of life with an indirect component of −0.025. The strongest indirect effect between COVID-19 and family quality life was through perceived social support and followed by perceived parental self-efficacy and then psychological resilience. Psychological health did not play a statistically significant role to mediate the impact of COVID on family quality of life.
As shown in Table 6, the traumatic event (COVID-19) had significant total effects on perceived social support (B = −0.42), psychological resilience (B = −0.07), psychological health (B = 0.14) and perceived parental self-efficacy (B = −0.01). The −0.42 effect on social support was entirely direct, as was specified in the final model (see Figure 2). The −0.07 effect on psychological resilience was partially direct (B = −0.05, p < 0.001) and partially indirect through social support (B = −0.02, p < 0.001) and direct and indirect effects were significant. The 0.14 effect on psychological health was partially direct (B = 0.08, p < 0.001) and partially indirect (B = 0.06, p < 0.001). The −0.01 effect on parent self-efficacy was also partially direct (−0.006, p < 0.001) and partially indirect (−0.004, p < 0.001).
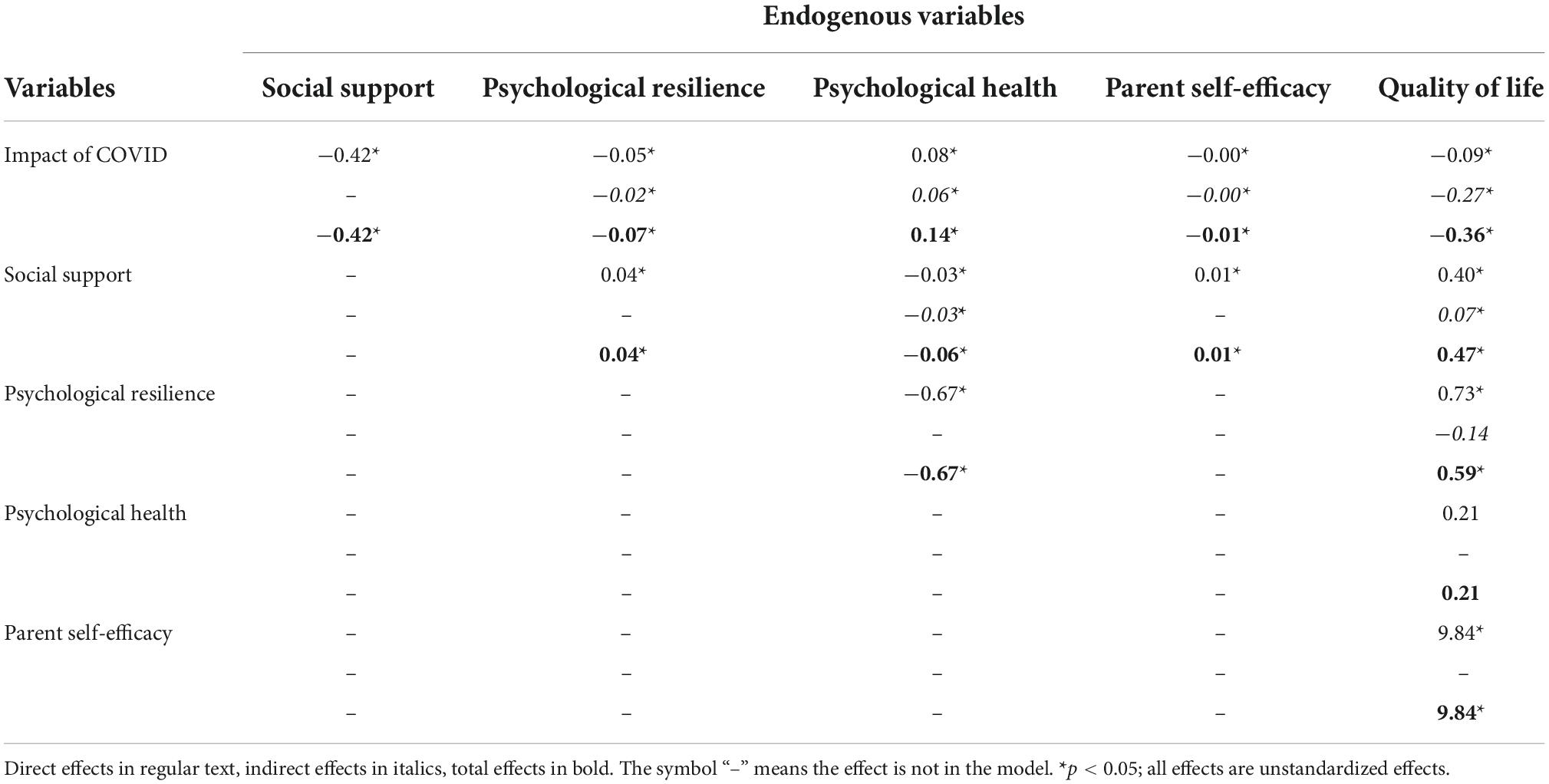
Table 6. Bootstrapped coefficients of total, direct, and indirect effects on endogenous variables in the final path model.
As seen in Figure 2, perceived social support was not affected by any of the endogenous variables. Psychological resilience was directly affected by perceived social support (B = 0.04, p < 0.001). Psychological health was affected by perceived social support (B = −0.06, p < 0.001) and psychological resilience (B = −0.67, p < 0.001). The −0.06 effect from perceived social support was partially direct (B = −0.03, p < 0.001) and partially indirect (B = −0.03, p < 0.001), and the indirect effect was entirely mediated by psychological resilience. Perceived parental self-efficacy was affected by perceived social support only with an entirely direct component of 0.01 (p < 0.001).
According to the model specification, family quality of life was significantly affected by perceived social support (B = 0.47, p < 0.001), psychological resilience (B = 0.59, p < 0.001), and perceived parental self-efficacy (B = 9.84, p < 0.001). The 0.47 effect from perceived social support was partially direct (B = 0.40, p < 0.001) and partially indirect (B = 0.07, p < 0.001). The 0.59 effect from psychological resilience to quality of life was comprised of a significant direct effect of 0.73 and an insignificant indirect effect of −0.14. Family quality of life was also affected by perceived parental self-efficacy with a direct component of 9.84.
Discussion
The present study investigated the effects of the COVID-19 pandemic on the quality of life of families who have children with disabilities and the mediating roles of perceived family burden, social support, parental self-efficacy, psychological health, and psychological resilience on this relationship. In the following section, the main findings of the study are discussed in relation to current literature and recommendations were made to support children with disabilities and their families during the COVID-19 pandemic. Limitations of the study are also discussed.
A main finding of the current study is that the quality of life of families who have children with disabilities decreased as the impact of the traumatic event (COVID-19 pandemic) increased. Studies conducted with families of children with different disabilities prior to or during the COVID-19 pandemic showed that families usually have lower levels of quality of life in comparison to families of children with typical development (Al Awaji et al., 2021; Ueda et al., 2022). For example, research has shown that families of children with intellectual disability (Bertelli et al., 2011), autism spectrum disorder (Cohen et al., 2014), cerebral palsy (Barros et al., 2019), and multiple disabilities (Chou et al., 2011) have relatively lower levels of quality of life. Traumatic events such as the COVID-19 pandemic increases the anxiety, fear, and depression levels of individuals (Roy et al., 2020) and creates an extra psychological burden on individuals who have to stay at home or implement social restrictions because of the fear of getting sick (Van Bavel et al., 2020; Bruder et al., 2021). In this respect, many families of children with disabilities have had restrictions in their lives which have limited their access to special education and rehabilitation services for themselves and their children. These adverse changes in their daily lives during COVID-19 pandemic resulted in decreased quality of life for families of children with disabilities (Ali et al., 2021). Therefore, it is critical to provide therapy and rehabilitation services to children with disabilities and their families through alternative methods such as telehealth technologies to mitigate the negative influences of the pandemic (Rosenbaum et al., 2021).
Findings in this study also revealed that perceived social support, parental self-efficacy and psychological resilience have mediating roles in the relationship between impact of the traumatic event (COVID-19 pandemic) and family quality of life. Perceived social support had a statistically significant negative relationship with the impact of the COVID-19 pandemic and a statistically significant positive relationship with family quality of life. This means that the COVID-19 pandemic reduces the social support perceived by parents of children with disabilities and reduced social support adversely impacts the quality of family life for children with disabilities. Extant literature contains many studies showing the positive association between perceived social support and quality of life (Mathew and Nair, 2017; Boehm and Carter, 2019). The more social support mothers receive in relation to care of their children, the higher their family quality of life is (Kasser and Zia, 2020). Findings of the current study support the notion that the effect of having a child with disability on family quality of life is mediated by the resilience of the parents and the social support they receive (Ueda et al., 2022) and that social support is an important mediating variable in the relationship between resilience and quality of life (Mathew and Nair, 2017). This finding warrants the need for providing social services and psychological supports to children with disabilities and their families during the pandemic (Amor et al., 2021).
Considering the pandemic as a traumatic experience (Volpe, 1996), it seems likely that families of children with disabilities will exhibit post-traumatic stress symptoms during and after the COVID-19 pandemic (Ueda et al., 2022). Some researchers (e.g., Weiss, 2002) consider having social support as one of the variables that will minimize the effects of traumatic stress. Social support is also an important mediator that affects the quality of life (Wang and Xu, 2017). Inadequate social support resources on the other hand result in an increase in psychological problems such as anxiety and depression (Harms et al., 2019). In short, the social support that a person receives during a traumatic experience plays a pivotal role in the effects of the trauma (Navas et al., 2022). Altogether these findings show that the supportive characteristics of the environments in which families of children with disabilities live can reduce the negative psychological effects that may occur during and after the COVID-19 pandemic. As a result, it can be concluded that strong social support is an important factor in maintaining the quality of life of families during the pandemic. Therefore, authorities should make sure that families of children with disabilities have access to educational, social and emotional support resources and services to alleviate the negative impact of the pandemic and improve symptoms associated with increase stress (Navas et al., 2022; Werner et al., 2022).
In addition to perceived social support, perceived parental self-efficacy mediated the relationship between the impact of the traumatic event (COVID-19 pandemic) and family quality of life. Perceived parental self-efficacy had a small but statistically significant negative relationship with the impact of the COVID-19 pandemic and a statistically significant positive relationship with family quality of life. This result indicates that families with high perceived parental self-efficacy also have high quality of life. Literature contains several studies noting the positive correlation between perceived parental self-efficacy and family quality of life (Kasser and Zia, 2020; Tehranineshat et al., 2020). Considering that one dimension of family quality of life is parenting (Meral and Cavkaytar, 2013) and the parenting dimension is closely related to parental self-efficacy, positive correlation between parental self-efficacy and family quality of life was an expected finding. The more individuals are confident in their abilities, the more active they are and the more persistently they work to achieve their goals (Hinz et al., 2019). Therefore, efforts should be made to empower parents so that they can support development and educational needs of their children when in-person professional support is limited or not available (Buendia, 2021; Panes and Torrentira, 2021; Wolstencroft et al., 2021).
Another variable that mediated the relationship between the impact of COVID-19 pandemic and family quality of life is psychological resilience. Individuals with high psychological resilience tend to use positive coping strategies (Ong et al., 2018) and can adapt more easily to stressful situations (Windle et al., 2011). In the present study, psychological resilience had a statistically significant negative relationship with the impact of COVID-19 pandemic on families and a statistically significant positive relationship with family quality of life. The main role of psychological resilience in mediating the decreased perception of family quality of life shown by the present study is in line with and extend previous evidence that the negativity of the psychological effects of COVID-19 pandemic is moderated by psychological resilience and personality traits (Osimo et al., 2021) and that these effects were also correlated with behavioral wellbeing including emotional eating (Cecchetto et al., 2021). Thus, findings of the present study show that the benefits of psychological resilience are not limited to the personal/individual sphere, but rather they extend to socially relevant environments, such as family.
Psychological resilience, which includes being able to stand strong and recover from difficulties (Ong et al., 2018), is seen as a very valuable characteristic for families of children with disabilities. The high psychological resilience the families have may help them be affected less adversely by the COVID-19 pandemic. Research has noted that social network, good coping strategies, flexibility, and communication are among the factors that will positively impact resilience during the pandemic (Gayatri and Irawaty, 2021). Thus, it is important for families to have healthy communication among its members, and build social support networks with extended family, siblings, or close friends using technology during these stressful times (Gayatri and Irawaty, 2021; Lee S. J. et al., 2021).
Another noteworthy finding of the current study is the positive correlation between the impact of COVID-19 pandemic on families of children with disabilities and their psychological health. In this respect, as the impact of COVID-19 increases, symptoms for psychological health issues such as depression and anxiety increase. In addition, psychological resilience and perceived social support mediated the impact of the COVID-19 pandemic on psychological health with the former variable having stronger impact indicating that parents with high psychological resilience also have high psychological health. Previous studies also showed that traumatic experiences negatively affect psychological health (Eker, 2016) and psychological health is associated with psychological resilience (Anderson et al., 2019).
Traumatic experiences pose a threat to the psychological integrity of the person and the coping mechanisms used may be insufficient (Eker, 2016). On the contrary, sometimes individuals may start to feel stronger after traumatic experiences, and gain benefits that improve and strengthen the person, such as an increase in social relations (Hasdemir, 2018). From this perspective, it seems possible for individuals to experience positive changes after traumatic experiences. These positive developments, defined as post-traumatic growth, are associated with high psychological resilience (Özçetin and Hiçdurmaz, 2017). Being able to protect mental health against traumatic experiences and even develop positive emotions is closely related to the psychological resilience of the individual (Bonnano and Mancini, 2008). While many parents of children with disabilities who face serious difficulties in their daily lives have higher levels of stress (Baker-Ericzén et al., 2005), anxiety (Baxter et al., 2000), and depression (Singer, 2006), some families are more resilient and adapt better when these challenges are present (Gerstein et al., 2009). As a result, findings of the present study and other studies emphasize that individuals with better psychological resilience have better psychological wellbeing and improved quality of life and. In this direction, supporting psychological resilience of families during the COVID-19 pandemic becomes important in protecting psychological health and quality of life for parents of children with disabilities.
An unexpected finding of the present study was that the correlation between perceived family burden and quality of life was not statistically significant, although perceived family burden was positively correlated with the impact of the COVID-19 pandemic on families. Contrary to the expectation that families with higher family burden will have a lower quality of life, Macit (2017) reported that there is no significant relationship between family burden and quality of life. Although having a child with disability increases the burden of family members (Bruder et al., 2021), it may not cause a difference in families’ perceptions of quality of life. This result can be explained by the positive effects a child with disability may bring to the family such as happiness (Bayat, 2005).
Despite the negative impacts of COVID-19 pandemic reported in many studies, several recent studies have described positive influence of the lockdown experienced during the pandemic on children with disabilities and their families. For example, studies reported that family members’ spending more time together during the lockdown helped them to build stronger relationships (Wolstencroft et al., 2021; Rakap et al., 2022). Some parents noted that interactions between their children with and without special needs improved during the pandemic (Embregts et al., 2021). Rosenbaum et al. (2021) found that families of children with disabilities saved time, effort, and money when services were provided via telehealth technologies during the pandemic in comparison to in-person services prior to pandemic. Moreover, Rogers et al. (2021) and Asbury et al. (2021) reported that parents of children with special needs noted a decrease in the severity and number of challenging behaviors exhibited by their children due to elimination of daily pressures such as getting ready for school or going to the supermarket.
Limitations
There are at least four limitations of this study that should be considered while interpreting the findings. The first limitation is related to the total number of items in the questionnaire package. The questionnaire package included a total of 166 items across different forms and scales. The lengths of questionnaire might have impacted how participants responded to the questions, especially questions at the end of the questionnaire package. Research shows that participants may be bored, have fatigue, skip items, or respond the items randomly by the end of the long survey packages (Porter et al., 2004). The relatively low internal consistency coefficient calculated for the Brief Resilience Scale may be attributed the fact that this scale was at the end of the survey package. Future research should control for the length of questionnaires and lengthy questionnaires should be administered in more than one session. Second, perceived parental self-efficacy was measured using a single item in the Demographic Information Form. Therefore, there is not data in relation to reliability of this measure. Third limitation is about causality of the findings. This study used correlational survey design which does not allow to claim causality by its nature as there may be reciprocal relationships between variables (Büyüköztürk, 2018). For example, while the COVID-19 pandemic affects family quality of life, family quality of life can also affect how families are affected by the COVID-19 pandemic. The last limitation is related to characteristics of participants. In this study, 89% of the participants were mothers and 11% were fathers; majority of participants were graduates of primary school and from mid-SES backgrounds. Future research should include more homogeneous participant groups.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ondokuz Mayıs University Social Science Institutional Review Board. The patients/participants provided their written informed consent to participate in this study.
Author contributions
SR, MV-B, SK, MK, and HS contributed to the conception and design of the study. SR, UB, and HS organized the database. HS and UB performed the data analysis. SR and MV-B wrote the first draft of the manuscript. MK, SK, and UB wrote sections of the manuscript. All authors contributed to the manuscript revision, read, and approved the submitted version.
Funding
This study was supported by Grant #120K259 from the Scientific and Technological Research Council of Turkey (TUBITAK) to the Ondokuz Mayıs University, Samsun, Turkey.
Acknowledgments
We thank Campbell McDermid for reading earlier drafts of this manuscript and providing valuable feedback. We also thank the reviewers whose comments and suggestions helped improve this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The opinions expressed are those of the authors, not the funding agency.
References
Adıbelli, D., and Sümen, A. (2020). The effect of the coronavirus (COVID-19) pandemic on health-related quality of life in children. Children Youth Services Rev. 119:105595. doi: 10.1016/j.childyouth.2020.105595
Ahmen, D., Buheji, M., and Fardan, S. M. (2020). Re-emphasising the future family role in “care economy” as a result of covid-19 pandemic spillovers. Am. J. Econ. 10, 332–338. doi: 10.5923/j.economics.20201006.03
Aksoy, V., and Diken, İH. (2009). Annelerin ebeveynlik öz yeterlik algıları ile gelişimi risk altında olan bebeklerin gelişimleri arasındaki ilişkiyi inceleyen araştırmalara bir bakış. Ankara Üniversitesi Eğitim Bilimleri Fakültesi Özel Eğitim Dergisi 101, 59–68. doi: 10.1501/Ozlegt_0000000133
Al Awaji, N., Aldhahi, M., Akil, S., Awad, S., and Mortada, E. (2021). Quality of life, needs and fears of mothers of children with disabilities in Saudi Arabia during the COVID-19 lockdown. Int. J. Environ. Res. Public Health 18:11442. doi: 10.3390/ijerph182111442
Ali, U., Bharuchi, V., Ali, N. G., and Jafri, S. K. (2021). Assessing the quality of life of parents of children with disabilities using WHOQoL BREF during COVID-19 pandemic. Front. Rehabilitation Sci. 2:708657. doi: 10.3389/fresc.2021.708657
Amor, A. M., Navas, P., Verdugo, M. Á, and Crespo, M. (2021). Perceptions of people with intellectual and developmental disabilities about COVID-19 in Spain: a cross-sectional study. J. Intell. Disabil. Res. 65, 381–396. doi: 10.1111/jir.12821
Anderson, M. I., Daher, M., and Simpson, G. K. (2019). A predictive model of resilience among family caregivers supporting relatives with traumatic brain injury (TBI): a structural equation modelling approach. Neuropsychol. Rehabil. 30, 1–22. doi: 10.1080/09602011.2019.1620787
Asbury, K., Fox, L., Deniz, E., Code, A., and Toseeb, U. (2021). How is COVID-19 affecting the mental health of children with special educational needs and disabilities and their families? J. Autism Dev. Disord. 51, 1772–1780. doi: 10.1007/s10803-020-04577-2
Baker-Ericzén, M. J., Brookman-Frazee, L., and Sthamer, A. (2005). Stress level and adaptability in parents of toddlers with and without autism spectrum disorders. Res. Practice Persons Severe Disabil. 30, 194–204. doi: 10.2511/rpsd.30.4.194
Barros, A. L. O., de Gutierrez, G. M., Barros, A. O., and Santos, M. (2019). Quality of life and burden of caregivers of children and adolescents with disabilities. Special Care Dentistry 394, 380–388. doi: 10.1111/scd.12400
Baxter, C., Cummins, R. A., and Yiolitis, L. (2000). Parental stress attributed to family members with and without disability: a longitudinal study. J. Intell. Dev. Disabil. 25, 105–118. doi: 10.1080/13269780050033526
Bayat, M. (2005). How family members’ perceptions of influences and causes of autism may predict assessment of their family quality of life. Dissertation Abstracts Int. Section B: Sci. Eng. 66, 57–79.
Bertelli, M., Bianco, A., Rossi, M., Scuticchio, D., and Brown, I. (2011). Relationship between individual quality of life and family quality of life for people with intellectual disability living in Italy. J. Intell. Disabil. Res. 55, 1136–1150. doi: 10.1111/j.1365-2788.2011.01464.x
Bildirici, F. (2014). Özel Eğitime Gereksinimi Olan Çocuğa Sahip Ailelerde Aile Yükü Ile Psikolojik Dayanıklılık Arasındaki Ilişki [Yayınlanmamış yüksek lisans tezi]. Ýstanbul: Haliç Üniversitesi.
Boehm, T. L., and Carter, E. W. (2019). Family quality of life and its correlates among parents of children and adults with intellectual disability. Am. J. Intell. Dev. Disabil. 124, 99–115. doi: 10.1352/1944-7558-124.2.99
Bonnano, G. A., and Mancini, A. D. (2008). La capacidad humana para seguir adelante frente a un posible trauma. Pediatrics 65, 69–75.
Bosmans, M. W., Hofland, H. W., De Jong, A. E., and Van Loey, N. E. (2015). Coping with burns: the role of coping self-efficacy in the recovery from traumatic stress following burn injuries. J. Behav. Med. 38, 642–651. doi: 10.1007/s10865-015-9638-1
Bruder, M. B., Lutz, T. M., and Ferreira, K. E. (2021). Parents of children with disabilities in the early months of COVID-19: knowledge, beliefs and needs. Dev. Disabil. Network J. 1:8.
Buendia, D. L. P. (2021). Cross cultural approach: lived experiences of children with special needs during pandemic in their family’s perspectives. Int. J. Adv. Res. Educ. Soc. 3, 88–97.
Carlson, J. M., and Miller, P. A. (2017). Family burden, child disability, and the adjustment of mothers caring for children with epilepsy: role of social support and coping. Epilepsy & Behavior 68, 168–173. doi: 10.1016/j.yebeh.2017.01.013
Cecchetto, C., Aiello, M., Gentili, C., Ionta, S., and Osimo, S. A. (2021). Increased emotional eating during COVID-19 associated with lockdown, psychological and social distress. Appetite 160:105122. doi: 10.1016/j.appet.2021.105122
Chen, S. Q., Chen, S. D., Li, X. K., and Ren, J. (2020). Mental health of parents of special needs children in China during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 17:9519. doi: 10.3390/ijerph17249519
Chou, K. R. (2000). Caregiver burden: a concept analysis. J. Pediatric Nursing 15, 398–407. doi: 10.1053/jpdn.2000.16709
Chou, Y. C., Chiao, C., and Fu, L. Y. (2011). Health status, social support, and quality of life among family carers of adults with profound intellectual and multiple disabilities (PIMD) in Taiwan. J. Intell. Dev. Disabil. 36, 73–79. doi: 10.3109/13668250.2010.529803
Cohen, S. R., Holloway, S. D., Domínguez-Pareto, I., and Kuppermann, M. (2014). Receiving or believing in family support? contributors to the life quality of Latino and non-Latino families of children with intellectual disability. J. Intell. Disabil. Res. 58, 333–345. doi: 10.1111/jir.12016
Çorapçıoğlu, A., Yargıç, İ, Geyran, P., and Kocabaşoğlu, N. (2006). Olayların Etkisi Ölçeği (IES-R) türkçe versiyonunun geçerlilik ve güvenilirliği. New Symposium J. 44, 14–22.
Creamer, M., Bell, R., and Failla, S. (2003). Psychometric properties of the impact of event scale–revised. Behav. Res. Ther. 41, 1489–1496.
Dekel, R., and Monson, C. M. (2010). Military-related post-traumatic stress disorder and family relations: current knowledge and future directions. Aggress. Violent Behav. 15, 303–309. doi: 10.1016/j.avb.2010.03.001
Demiray, G. (2019). Özel Gereksinimli Çocuğu Olan Ailelerde Yaşam Kalitesi, Umutsuzluk ve Yılmazlık Arasındaki Ilişkilerin Incelenmesi [Yayınlanmamış yüksek lisans tezi]. Ýstanbul: Marmara Üniversitesi, Eğitim Bilimleri Enstitüsü.
Doğan, T. (2015). Kısa psikolojik sağlamlık ölçeğinin Türkçe uyarlaması: Geçerlik ve güvenirlik çalışması. J. Happiness Well-Being 3, 93–102. doi: 10.19128/turje.181073
Eker, Ý (2016). Travmatik Yaşantıların Psikolojik Sağlığa Etkisi: Travmanın Türü, Zaman Yönelimi, Dünyaya Ilişkin Varsayımlar ve Ruminasyonlar Açısından Bir Inceleme [Yayınlanmamış yüksek lisans tezi]. Ankara: Ankara Üniversitesi, Sosyal Bilimler Enstitüsü.
Embregts, P. J. C. M., Heerkens, L., Frielink, N., Giesbers, S., Vromans, L., and Jahoda, A. (2021). Experiences of mothers caring for a child with an intellectual disability during the COVID-19 pandemic in the Netherlands. J. Intell. Disabil. Res. 65, 760–771. doi: 10.1111/jir.12859
Gayatri, M., and Irawaty, D. K. (2021). Family resilience during COVID-19 pandemic: a literature review. Family J. 30, 132–138. doi: 10.1177/10664807211023875
Gerstein, E. D., Crnic, K. A., Blacher, J., and Baker, B. L. (2009). Resilience and the course of daily parenting stress in families of young children with intellectual disabilities. J. Intell. Disabil. Res. 53, 981–997. doi: 10.1111/j.1365-2788.2009.01220.x
Goldberg, D. P. (1972). The Detection of Psychiatric Illness by Questionnaire. Maudsley Monograph No. 21. Oxford: Oxford University Press.
Hair, J., Anderson, R., Tatham, R., and Black, W. (1998). Multivariate Data Analysis, 5th Edn. Hoboken NJ: Prentice Hall.
Harms, C. A., Cohen, L., Pooley, J. A., Chambers, S. K., Galvao, D. A., and Newton, R. U. (2019). Quality of life and psychological distress in cancer survivors: the role of psycho-social resources for resilience. Psycho-Oncology 28, 271–277. doi: 10.1002/pon.4934
Hasdemir, D. (2018). Effects of Refugee Trauma on Interpreters: A Qualitative Analysis of Vicarious Traumatization and Coping [Yüksek lisans tezi]. Ankara: Middle East Technical University.
Hinz, A., Friedrich, M., Kuhnt, S., Zenger, M., and Schulte, T. (2019). The influence of self-efficacy and resilient coping on cancer patients’ quality of life. Eur. J. Cancer Care 28:e12952. doi: 10.1111/ecc.12952
Hoffman, L., Marquis, J., Poston, D., Summers, J. A., and Turnbull, A. (2006). Assessing family outcomes: psychometric evaluation of the beach center family quality of life scale. J. Marriage Family 68, 1069–1083. doi: 10.1111/j.1741-3737.2006.00314.x
Horowitz, M., Wilner, N., and Alvarez, W. (1979). Impact of event scale: a measure of subjective stress. Psychosomatic Med. 41, 209–218. doi: 10.1097/00006842-197905000-00004
Janoff-Bulman, R. (1992). Shattered Assumptions: Towards a New Psychology of Trauma. Mumbai: FreePress.
Jeste, S., Hyde, C., Distefano, C., Halladay, A., Ray, S., Porath, M., et al. (2020). Changes in access to educational and healthcare services for individuals with intellectual and developmental disabilities during COVID-19 restrictions. J. Intell. Disabil. Res. 64, 825–833. doi: 10.1111/jir.12776
Jesus, T. S., Bhattacharjya, S., Papadimitriou, C., Bogdanova, Y., Bentley, J., and Arango-Lasprilla, J. C. (2021). Lockdown-related disparities experienced by people with disabilities during the first wave of the COVID-19 pandemic: Scoping review with thematic analysis. Int. J. Environ. Res. Public Health 18, 1–24. doi: 10.3390/ijerph18126178
Kaner, S. (2010). Yenilenmiş ana-baba sosyal destek ölçeğinin psikometrik özellikleri. Eğitim Bilim 35, 15–29.
Kasser, S. L., and Zia, A. (2020). Mediating role of resilience on quality of life in individuals with multiple sclerosis: a structural equation modeling approach. Arch. Phys. Med. Rehabil. 101, 1152–1161. doi: 10.1016/j.apmr.2020.02.010
Kilic, C., Rezaki, M., Rezaki, B., Ozgen, G., Sagduyu, A., and Ozturk, M. O. (1997). General Health Questionnaire (GHQ-12 & GHQ-28): psychometric properties and factor structure of the scales in a Turkish primary care sample. Soc. Psychiatry Psychiatr. Epidemiol. 32, 327–331. doi: 10.1007/BF00805437
Kına, D. (2019). 23 Yaş Üstü Bireylerde Travma Sonrası Büyüme Düzeyinin Travmatik Yaşantı Türü, Algılanan Sosyal Destek, Dünyaya Ilişkin Varsayımlar, Psikolojik Sağlamlık ve Ruhsal Belirti Düzeyi Değişkenleri ile Yordanması [Yüksek lisans tezi]. İzmir: Ege Üniversitesi, Sosyal Bilimler Enstitüsü.
Kline, T. J. (2005). Psychological Testing: A Practical Approach to Design and Evaluation. New York, NY: Sage Publications. doi: 10.4135/9781483385693
Koçak, Z., and Harmanci, H. (2020). Covıd-19 pandemi sürecinde ailede ruh sağlığı. Karatay Sosyal Araştırmalar Dergisi 5, 180–204.
Lee, S. J., Ward, K. P., Chang, O. D., and Downing, K. M. (2021). Parenting activities and the transition to home-based education during the COVID-19 pandemic. Children Youth Services Rev. 122:105585. doi: 10.1016/j.childyouth.2020.105585
Lee, V., Albaum, C., Tablon Modica, P., Ahmad, F., Gorter, J. W., Khanlou, N., et al. (2021). The impact of COVID-19 on the mental health and wellbeing of caregivers of autistic children and youth: a scoping review. Autism Res. 14, 2477–2494. doi: 10.1002/aur.2616
Lilly, M. M., Valdez, C. E., and Graham-Bermann, S. A. (2011). The mediating effect of world assumptions on the relationship between trauma exposure and depression. J. Interpersonal Violence 26, 2499–2516. doi: 10.1177/0886260510383033
Macit, Y. (2017). Evde Bakım Hizmeti Alan Engelli Bireye Sahip Ailelerin Bakım Verme Yükleri Ile Yaşam Kalitelerinin Belirlenmesi Amasya Örneği [Yüksek lisans tezi]. Konya: Selçuk Üniversitesi Sağlık Bilimleri Enstitüsü.
Mathew, R. T., and Nair, B. P. (2017). Quality of life and resilience in relation to perceived social support among mothers of children with learning disability. Indian J. Health Wellbeing 8, 665–667.
Meral, B. F., and Cavkaytar, A. (2013). Beach center aile yaşam kalitesi ölçeğinin Türkçe uyarlama, geçerlik ve güvenirlik çalışması. Eğitim Bilim 38, 48–60.
Monson, E., Caron, J., McCloskey, K., and Brunet, A. (2017). Longitudinal analysis of quality of life across the trauma spectrum. Psychol. Trauma: Theory Res. Practice Policy 9:605. doi: 10.1037/tra0000254
Montigny, F., and Lacharité, C. (2004). Fathers’ perceptions of the immediate postpartal period. J. Obstetric Gynecol. Neonatal Nursing 33, 328–339. doi: 10.1177/0884217504266012
Narzisi, A. (2020). Handle the autism spectrum condition during coronavirus (COVID-19) stay at home period: ten tips for helping parents and caregivers of young children. Brain Sci. 10:207. doi: 10.3390/brainsci10040207
Navas, P., Verdugo, M. Á, Martínez, S., Amor, A. M., Crespo, M., and Deliu, M. M. (2022). Impact of COVID-19 on the burden of care of families of people with intellectual and developmental disabilities. J. Appl. Res. Intell. Disabil. 35, 577–586. doi: 10.1111/jar.12969
Ong, H. L., Vaingankar, J. A., Abdin, E., Sambasivam, R., Fauziana, R., Tan, M.-E., et al. (2018). Resilience and burden in caregivers of older adults: moderating and mediating effects of perceived social support. BMC Psychiatry 181:27. doi: 10.1186/s12888-018-1616-z
Osborne, L. A., McHugh, L., Saunders, J., and Reed, P. (2008). Parenting stress reduces the effectiveness of early teaching interventions for autistic spectrum disorders. J. Autism Dev. Disord. 38, 1092–1103. doi: 10.1007/s10803-007-0497-7
Osimo, S. A., Aiello, M., Gentili, C., Ionta, S., and Cecchetto, C. (2021). The influence of personality, resilience, and alexithymia on mental health during COVID-19 pandemic. Front. Psychol. 12:630751. doi: 10.3389/fpsyg.2021.630751
Özçetin, Y. S. Ü, and Hiçdurmaz, D. (2017). Kanser deneyiminde travma sonrası büyüme ve psikolojik sağlamlık. Psikiyatride Güncel Yaklaşımlar 9:388397. doi: 10.18863/pgy.290285
Panes, R. G., and Torrentira, M. C. Jr. (2021). Empowering the parents as home-partners in the implementation of basic education learning continuity plan during Covid-19 pandemic in the Philippines. Asia Pacific J. Educ. Perspect. 8, 66–71.
Patrick, S. W., Henkhaus, L. E., Zickafoose, J. S., Lovell, K., Halvorson, A., Loch, S., et al. (2020). Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics 146:e2020016824.
Porter, S. R., Whitcomb, M. E., and Weitzer, W. H. (2004). Multiple surveys of students and survey fatigue. New Direct. Institutional Res. 2004, 63–73.
Prime, H., Wade, M., and Browne, D. T. (2020). Risk and resilience in family well-being during the COVID-19 pandemic. Am. Psychol. Assoc. 75, 631–643. doi: 10.1037/amp0000660
Racine, N., Cooke, J. E., Eirich, R., Korczak, D. J., McArthur, B., and Madigan, S. (2020). Child and adolescent mental illness during COVID-19: a rapid review. Psychiatry Res. 292:113307. doi: 10.1016/j.psychres.2020.113307
Rakap, S., Vural-Batik, M., Karnas, M., Kalkan, S., Bayrakdar, U. M., and Sari, H. I. (2022). Caught off guard: Parenting children with disabilities during COVID-19 pandemic. J. Progress. Educ.
Rogers, G., Perez-Olivas, G., Stenfert Kroese, B., Patel, V., Murphy, G., Rose, J., et al. (2021). The experiences of mothers of children and young people with intellectual disabilities during the first COVID-19 lockdown period. J. Appl. Res. Intell. Disabil. 34, 1421–1430. doi: 10.1111/jar.12884
Romero, E., López-Romero, L., Domínguez-Álvarez, B., Villar, P., and Gómez-Fraguela, J. A. (2020). Testing the effects of COVID-19 confinement in Spanish children: the role of parents’ distress, emotional problems and specific parenting. Int. J. Environ. Res. Public Health 17:6975. doi: 10.3390/ijerph17196975
Rosenbaum, P. L., Silva, M., and Camden, C. (2021). Let’s not go back to ‘normal’! lessons from COVID-19 for professionals working in childhood disability. Disabil. Rehabil. 43, 1022–1028. doi: 10.1080/09638288.2020.1862925
Roy, D., Tripathy, S., Kar, S. K., Sharma, N., Verma, S. K., and Kaushal, V. (2020). Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J. Psychiatry 51:102083. doi: 10.1016/j.ajp.2020.102083
Sales, E. (2003). Family burden and quality of life. Qual. Life Res. 12, 33–41. doi: 10.1023/A:1023513218433
Singer, G. H. (2006). Meta-analysis of comparative studies of depression in mothers of children with and without developmental disabilities. Am. J. Mental Retardation 111, 155–169. doi: 10.1352/0895-8017(2006)111[155:MOCSOD]2.0.CO;2
Smith, B. W., Dalen, J., Wiggins, K., Tooley, E., Christopher, P., and Bernard, J. (2008). The brief resilience scale: assessing the ability to bounce back. Int. J. Behav. Med. 15, 194–200. doi: 10.1080/10705500802222972
Sultana, S., Khan, A. H., Hossain, S., Ansar, A., Sikder, T., and Hasan, T. (2021). Prevalence and predictors of post-traumatic stress symptoms and depressive symptoms among Bangladeshi students during COVID-19 mandatory home confinement: a nationwide cross-sectional survey. Children Youth Services Rev. 122:105830. doi: 10.1016/j.childyouth.2020.105880
Tayaz, E., and Koc, A. (2018). Assessment of relationship between perceived care burden and quality of life in disabled persons caregivers. Bakırköy Tıp Dergisi 14, 44–52. doi: 10.5350/BTDMJB.20160726012929
Tehranineshat, B., Mohammadi, F., Tazangi, R. M., Sohrabpour, M., Parviniannasab, A. M., and Bijani, M. (2020). A study of the relationship among burned patients’ resilience and self-efficacy and their quality of life. Patient Preference Adherence 14, 1361–1369. doi: 10.2147/PPA.S262571
Toprak, F. (2018). Zihinsel Engelli ve Üstün Yetenekli Çocuğa Sahip Ailelerin Yaşam Doyumları, Yaşam Kaliteleri ve Sosyal Destek Algılarının Karşılaştırılması [Yayınlanmamış yüksek lisans tezi]. Ankara: Hacettepe Üniversitesi, Sosyal Bilimler Enstitüsü.
Ueda, R., Okada, T., Kita, Y., Ukezono, M., Takada, M., Ozawa, Y., et al. (2022). Quality of life of children with neurodevelopmental disorders and their parents during the COVID-19 pandemic: a 1-year follow-up study. Sci. Rep. 12:4298. doi: 10.1038/s41598-022-08273-2
United Nations (2020). Policy Brief: The Impact of COVID-19 on Children. New York, NY: United Nations.
Uzun, H., Hamiden-Karaca, N., and Metin, Ş (2021). Assesment of parent-child relationship in Covid-19 pandemic. Children Youth Services Rev. 120:105748. doi: 10.1016/j.childyouth.2020.105748
Van Bavel, J. J., Baicker, K., Boggio, P. S., Capraro, V., Cichocka, A., Cikara, M., et al. (2020). Using social and behavioral science to support COVID-19 pandemic response. Nat. Hum. Behav. 4, 460–471. doi: 10.1038/s41562-020-0884-z
van Hoek, A. J., Underwood, A., Jit, M., Miller, E., and Edmunds, W. J. (2011). The impact of pandemic influenza H1N1 on health-related quality of life: a prospective population-based study. PLoS One 6:e17030. doi: 10.1371/journal.pone.0017030
Volpe, J. S. (1996). Traumatic Stress: An Overview. Available online at: http://www.nccm.org/article1.htm (accessed April 3, 2021).
Wang, Z., and Xu, J. (2017). Association between resilience and quality of life in Wenchuan Earthquake Shidu parents: the mediating role of social support. Commun. Mental Health J. 53, 859–863. doi: 10.1007/s10597-017-0099-6
Warner-Richter, M., and Lloyd, C. M. (2020). Considerations for Building Post-covid Early Care and Education Systems that Serve Children with Disabilities. Bethesda, MD: Child Trends.
Weiss, D., and Marmar, C. (1997). “The impact of event scale-revised,” in Assessing Psychological Trauma and PTSD, eds J. Wilson and T. Keane (New York, NY: Guilford). doi: 10.1037/t12199-000
Weiss, M. J. (2002). Hardiness and social support as predicators of stress in mothers of typical children, children with autism, and children with mental retardation. Autism 6, 115–130. doi: 10.1177/1362361302006001009
Werner, S., Hochman, Y., Holler, R., and Shpigelman, C. N. (2022). Burden and growth during COVID-19: comparing parents of children with and without disabilities. J. Child Family Stud. 31, 1535–1546. doi: 10.1007/s10826-022-02282-5
Willner, P., Rose, J., Stenfert Kroese, B., Murphy, G. H., Langdon, P. E., Clifford, C., et al. (2020). Effect of the COVID-19 pandemic on the mental health of carers of people with intellectual disabilities. J. Appl. Res. Intell. Disabil. 33, 1523–1533. doi: 10.1111/jar.12811
Windle, G., Bennett, K. M., and Noyes, J. (2011). A methodological review of resilience measurement scales. Health Qual. Life Outcomes 9:8. doi: 10.1186/1477-7525-9-8
Wolstencroft, J., Hull, L., Warner, L., Akhtar, T. N., Mandy, W., and Skuse, D. (2021). ‘We have been in lockdown since he was born’: a mixed methods exploration of the experiences of families caring for children with intellectual disability during the COVID-19 pandemic in the UK. BMJ Open 11:e049386. doi: 10.1136/bmjopen-2021-049386
Xiang, Y. T., Yang, Y., Li, W., Zhang, L., Zhang, Q., Cheung, T., et al. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7, 228–229. doi: 10.1016/S2215-0366(20)30046-8
Yeasmin, S., Banik, R., Hossain, S., Hossain, N., Mahumud, R., Salma, R., et al. (2020). Impact of COVID-19 pandemic on the mental health of children in Bangladesh: a cross-sectional study. Children Youth Services Rev. 117:105277. doi: 10.1016/j.childyouth.2020.105277
Yıldırım-Sarı, H., and Başbakkal, Z. (2008). Zihinsel yetersiz çocuğu olan aileler için aile yükü değerlendirme ölçeğinin geliştirilmesi. Atatürk Üniversitesi Hemşirelik Yüksekokulu Dergisi 11, 86–95.
Keywords: COVID-19 pandemic, family quality of life, children with disabilities, social support, family burden, parental self-efficacy, psychological resilience
Citation: Rakap S, Vural-Batik M, Kalkan S, Karnas M, Sari HI and Bayrakdar U (2022) The hidden (overlooked) impact of living through a pandemic: How parents of children with disabilities fared during COVID-19? Front. Educ. 7:827230. doi: 10.3389/feduc.2022.827230
Received: 01 December 2021; Accepted: 08 November 2022;
Published: 28 November 2022.
Edited by:
Susana Castro-Kemp, University College London, United KingdomReviewed by:
Lin-Ju Kang, Chang Gung University, TaiwanSilvio Ionta, Université de Lausanne, Switzerland
Copyright © 2022 Rakap, Vural-Batik, Kalkan, Karnas, Sari and Bayrakdar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Salih Rakap, s_rakap@uncg.edu
 Salih Rakap
Salih Rakap Meryem Vural-Batik2
Meryem Vural-Batik2  Halil Ibrahim Sari
Halil Ibrahim Sari