Scoop and treat: from an historical controversy to the emergency future
- 1Lille University School of Medicine, Lille, France
- 2Rush University Medical Center, Chicago, IL, United States
- 3Faculty of Health Sciences, Ben Gurion University of the Negev, Beersheba, Israel
- 4French Military Health Service, Paris Fire Brigade, Paris, France
- 5Neurology Service, Lille Catholic Institute Hospital Group, GHICL (Groupe Hospitalier de l'Institut Catholique de Lille), Lomme, France
- 6ULR 2694 METRICS, Lille University, Lille, France
Within the intricate narrative of emergency medical services (EMS), there lies a rich and evolving history of innovation and strategy, a saga that weaves through the fabric of prehospital emergency care. At the heart of this narrative is a compelling dichotomy, often whimsically encapsulated as the “stay and play” vs. “scoop and run” philosophies. These seemingly polar approaches to emergency care represent a tapestry of diverse opinions and practices, each tailored to its unique environmental context, clinical demands, and the relative availability of prehospital and hospital resources. Our comprehensive review delves into the historical evolution of these notions, tracing their roots from the ancient world to the present day. We cast a particular focus on the French model of “prehospital medicalization” and the Anglophone “Scoop and Run” approach, exploring their distinct trajectories and influences. Additionally, we turn our gaze to the Israeli system, a unique hybrid shaped by the American prehospital framework yet distinctively molded by the region's enduring conflict. By drawing on an array of interviews, historical records, and scholarly discourse, this document presents an in-depth exploration of the development of prehospital emergency medicine and its pivotal role in contemporary healthcare. Through this investigation, we aim to elucidate the historical tensions surrounding these concepts, shedding light on their implications for the landscape of modern emergency medical services and the intricate web of factors that shape their organization.
Introduction
In the ever-evolving tapestry of emergency medical services (EMS), a striking narrative unfolds—one of medical advances and the honing of provider skills that have, over time, reshaped the landscape of prehospital care. This story is marked by a crucial, ongoing debate: the extent and nature of care to be administered before reaching the hospital. It's a dilemma that has persisted since the dawn of the twentieth century, epitomized by the dichotomy often whimsically dubbed “stay and play” vs. “scoop and run.” This simplistic binary belies a complex array of strategies deployed worldwide, each reflecting its unique milieu.
Particularly noteworthy is Israel's approach, an intriguing adaptation of the American model, deeply entwined with the region's tumultuous history. “Scoop and Run,” with its emphasis on rapid transportation, particularly in trauma cases, stands in stark contrast to the philosophy of “field medicalization,” which advocates for initiating treatment at the scene to prevent prehospital mortality and to ensure patients are expediently directed to the appropriate specialized hospital care.
Our manuscript ventures deep into the heart of this historical conundrum, shedding light on the pivotal role of emergency medicine in the modern healthcare narrative. Weaving together threads from both historical and scholarly sources, we offer a panoramic view of this dynamic field, taking into account a spectrum of factors—from environmental and resource considerations to technology, cost, and the potential for EMS training.
Data sources
The intricate historical debate at the heart of emergency medical services demands a meticulous dissection, one that requires an engagement with well-reasoned arguments, a thorough appraisal of logical reasoning, and a critical examination of the credibility of contrasting viewpoints. Our endeavor was to immerse ourselves in a detailed exploration of case studies and a multitude of interpretations, aiming to probe the certainties and unearth scientific revelations. Our quest was shaped by a commitment to neutrality, a principle eloquently outlined by scholars Barnes and Pestré (1–6).
Because of the nature of our text, our technique was based on an objective and practical approach that did not adhere to the established norms (PRISMA). We delved into an array of historical documents and scholarly works, supplementing this research with insightful conversations with two key figures: Sarah Salvis (MSc-EMT) and General René Noto (MD). Sarah Salvis, our initial guide in navigating the rich history of North American emergency medical services, provided invaluable primary sources. General Noto, a pivotal figure in the evolution of emergency medicine in France, shared his expertise, particularly in his efforts to innovate and reform first aid training for firefighters.
Moreover, our research journey took us through venerable archives like the Sapeurs-Pompiers de Paris and the Harvard Library. We scoured academic platforms such as Pubmed and Google Scholar, meticulously analyzing articles that discussed the “scoop and run” and “stay and play” paradigms. Our objective was not to champion any particular stance but rather to gain a profound understanding of the historical, social, political, and medical contexts that frame this vital discourse in emergency medicine.
Actors
The tapestry of emergency healthcare is a mosaic of diverse professionals, each playing a pivotal role in this critical domain.
• At the forefront are Emergency Physicians, who adeptly navigate the complexities of life-threatening conditions, initiating intensive care, stabilizing patients, and striving to prevent avoidable deaths. In France, these physicians have been trailblazers in prehospital medicalization. In contrast, in English-speaking countries, while primarily stationed in hospitals, they also frequently respond to emergency calls.
• Physician Assistants and Nurses, integral to the medical team, operate under the guidance of physicians, delivering a wide range of medical services. Notably, outside the Franco-Germanic model, their presence in out-of-hospital settings is rare, yet their contributions within hospitals are indispensable.
• Paramedics, synonymous with out-of-hospital emergency response, often navigate these high-pressure situations in ambulances. Their scope and autonomy vary dramatically across countries, enjoying more independence in Anglo-American systems, while in others, they support physicians or nurses. Notably, this role is absent in France where it is replaced by ambulance drivers, who do not yet play a caring role.
• Firefighters, skilled in both firefighting and rescue operations, in certain countries, also provide initial medical assistance, a role that has grown in prominence as medical emergencies outpace fire-related calls.
• Emergency Medical Technicians (EMTs) play a versatile role, executing basic medical procedures, assisting paramedics and firefighters, and functioning across various organizations, including public ambulance services and fire departments.
• Military Personnel, trained for high-stress medical scenarios in challenging environments, are particularly active during armed conflicts. Their expertise in reducing avoidable deaths often extends to contributing significantly to the development of civilian prehospital systems.
• Bystanders, often the first on the scene, serve as crucial initial links in the emergency care chain, summoning emergency services and providing basic aid, sometimes under the guidance of medical advisors.
The roles and expertise of these professionals vary globally, a reflection of the diverse healthcare models and training standards that shape the emergency healthcare landscape.
Doctrines
Prehospital medicalization
Sometimes and wrongly described as a “stay and play” approach, prehospital medicalization aims to begin medical treatment in the field before or during evacuation. This doctrine's goal is to treat the patient right away in order to stop any future harm or injury. In the American continent, the idea has been around since pre-Columbian times. In his Codex of Florence, Book X, which spans the years 1558 to 1577 (7), Bernardino de Sahagun (1499–1590) discussed the Amerindian use of plants and incantations to cure war casualties.
Ambroise Paré (1509–1599) promoted the use of analgesics, the ejection of foreign bodies, the realignment of fractured bones, the dissection of connective tissues, the suturing of wounds, and the reduction of fractures in 1537 (8). The “Edit du Roy Portant creation d'Offices de Médecins and Chirurgiens des Armées du Roy” was released in 1708 to help armies and military clinics. Dominique-Jean Larrey (1766–1842) and Pierre-François Percy (1754–1825) suggested the use of flying ambulances with physicians on board during the Mayence war in 1792 (9). The idea of field hospitals and mobile medical units evolved through time, culminating in the modern “prehospital medicalization” strategy that emphasizes giving sick or injured patients prompt medical assistance before and during transportation.
Emergency medicine underwent more important advancements in the late 19th and early twentieth century. Amiral Rigault de Genouilly (1807–1873) and Napoleon III (1808–1873) are responsible for the establishment of the “Société centrale de sauvetage des naufragés” in 1865 (10). The Public Health Council released Avis and directions to follow in the event of a public roadway accident in 1870. A forward care service that combined first aid, lifting, and evacuation of the injured was formed during the Siege of Paris in 1871. Natchel (11) produced the “Oeuvres des ambulances urbaines de Saint-Louis” in 1884. In 1870, the International Red Cross and military assistance organizations were founded. In 1889, the General Inspection of Public Health and Sanitation established a call center, staffed with doctors and nurses, which led to the creation of the first six SAMU/SMUR facilities in Paris. In 1912, Maurice Marcille (1871–1941) and a Schneider engineer invented the first mobile operating room (or “autochir”) (12). To help disabled individuals be transported onboard ships or submarines, Pierre Bellille invented the Bellille stretcher. During World War I, several innovations were made, one of which was the “petites Curies” transportable radiological unit (13).
Dr. Cot originally introduced the idea of prehospital medical transport to the military Parisian Fire Brigade in 1927. Putting his military experience to benefit the civilian environment, *Dr. Cot made the idea of medical transport understandable to the wider public (14). Emergency medical treatment underwent a significant improvement in 1944 when Professor Bourret (1918–1993) founded the Passive Defense's mobile surgical ambulance (15). The concept reached new heights with Lt. Alexis Santini's (1914–1997) first helicopter transfer during the Indochina War in the 1950s (16).
A pivotal moment came in 1957, when A. Ruscoe Clarke (1908–1959) advocated for this model for road trauma cases at the St. John Ambulance Brigade Surgeons' Conference in Harrogate. This was a period of burgeoning development of rapid medical care in France during the 1960s and 1970s, emphasizing field care for early life-saving interventions (17). The establishment of “EMNIR” in 1964 (18) and the evolution of the term SAMU in 1972 and 1986 (19, 20) further illustrated the growth of this philosophy.
French prehospital medicalization, prioritizing immediate care and life-saving interventions for critical patients, has continually adapted over time. In cases of myocardial infarction, for example, it allows for precise diagnosis, swift initiation of therapy, and prompt transfer to specialized hospital services, exemplifying the philosophy's emphasis on rapid, yet thorough, patient care.
Scoop and run
In the lexicon of emergency medical services, the “Scoop and Run” approach, a hallmark of English-speaking countries, presents a striking contrast to its French counterpart. This method is underpinned by a principle that resonates with urgency: in the throes of a medical emergency, time is a critical, often elusive ally. The central tenet here is straightforward yet profound – hasten the patient's journey to hospital care, eschewing extensive on-site advanced medical treatment in favor of rapid transportation. This philosophy posits that the swifter a patient is delivered into the capable hands of hospital medical care, the better their odds of survival. It's a strategy that places its bets on speed and efficiency. Within this framework, emergency medical technicians (EMTs) and paramedics become the linchpins of a system designed to manage the majority of crises directly in the field, acting swiftly to stabilize and transport. Countries like the United States, United Kingdom, and Israel have become strongholds of this approach. In these nations, the emergency medical systems are tailored to prioritize rapid response and transit times. This strategy, in its essence, is a race against time, with the ultimate goal of delivering patients into the sanctum of hospital care with the utmost speed, thereby maximizing their chances of recovery and survival.
The history of emergency medical services (EMS) and the concept of “scoop and run” has evolved over several centuries. This concept dates back to the first century BC when Celse recommended compressing or ligating the vessels to stop bleeding. The ancient Roman Empire had military hospitals called valetudinaria with pick-up cavalry for injured soldiers in exchange for bonuses.
In 1597, Henri IV (1553–1610) built field hospitals for the wounded and “trained hippomobiles” for combat evacuations. In the seventeenth century, Stephen Bradwell provided instructions for addressing a range of medical issues (21). However, it wasn't until the nineteenth century that ambulance services really began to take shape. One European skeptic said, “What difference would that make?” when asked why the hospital in his city did not offer ambulance service. Regardless, the patient has to be sent to the hospital (Leonard, 1885–1989). Most people who needed emergency treatment and ambulance transfers received their first aid from a kind bystander or from the “hospitality of a neighboring store or office” (22). Patients were moved between hospitals using makeshift transportation methods before there were official ambulance networks. Others employed litters, pushcarts, delivery wagons, private vehicles, hire-chairs, gigs, and flys, while some depended on omnibus drivers. Wheeled litter has proven to be a highly popular mode of transportation over short distances. Rural patients had to utilize the company carts, farm carts, wagons, private or public coaches, and post-chaises for greater distances (23). Thanks to Dr. Edward Barry Dalton (1834–1872), the first civil ambulance service was founded in 1866 for the Commercial Hospital in Cincinnati and the Bellevue Hospital in New York City (24, 25).
Over the centuries, the concept of “scoop and run” has evolved in the field of pre-hospital care. The St. John Ambulance Association, established in England in the nineteenth century, provided transportation to hospitals for wounded patients (26). In the United States, the influential White Paper highlighted the fragmentation and deficiencies in pre-hospital care systems, leading to the development of EMS reforms (27).
To address physician shortages, physician assistants (PAs) emerged in the 1970s (28). Mobile critical care units were introduced in Jerusalem in 1973, and the concept of paramedics was brought to Israel by Dr. Nancy Caroline (29). Israeli paramedics gained more independence in the 1980s, and mobile critical care units expanded to rural areas in the 1990s (30). In Israel, the Medical Directorate of the Red Cross began training paramedics in 2006, and paramedics were granted the authority to certify fatalities in 2013 (31–33). In 2015, Israeli ambulance services no longer required a physician on board, and physician assistants were introduced in 2019 (34).
In conclusion, the concept of “scoop and run” has evolved throughout history, with adaptations for trauma care supported by scientific literature (35, 36).
Discussion
Systems description
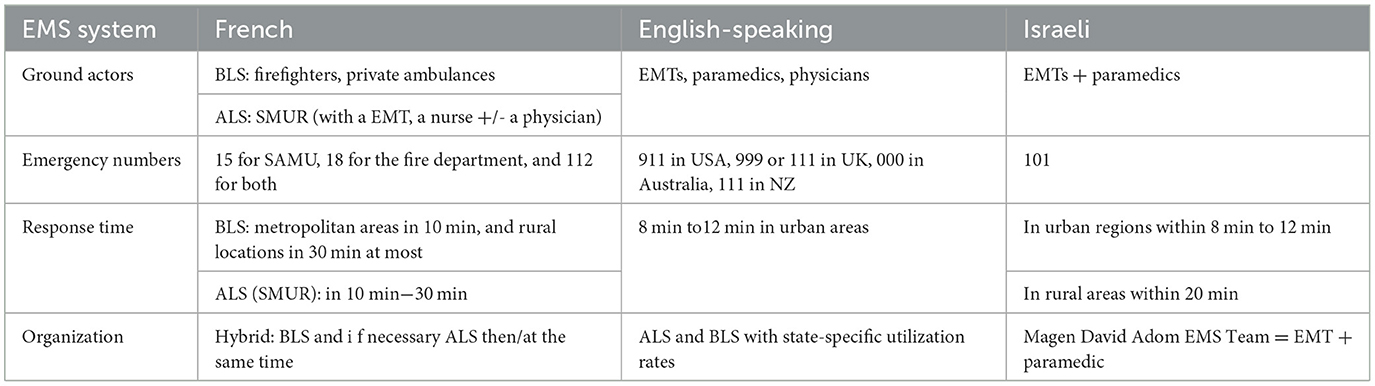
English-speaking, French and Isareli EMS systems are summed up into Table 1.
French actual system
The French pre-hospital system operates through 13 regional subdivisions, each with its own EMS organization called “SAMU,” “SMUR,” and fire departments. The system is centralized, with national telephone numbers for medical emergencies (15 for SAMU, 18 for the fire department, and 112 for both) (37). Response times aim for BLS ambulances to reach metropolitan areas in 10 min, medical teams in 10 min−20 min, and rural locations in 30 min at most. French EMS providers consist of firefighters/EMT, nurses, and emergency physicians.
French medical intensive care ambulances are equipped with advanced life support technology, resembling resuscitation rooms, and offer pre-hospital treatment and transportation for patients with specific needs, such as newborns and pediatric patients (37).
The French system follows a hybrid approach, combining elements of both “scoop and run” and “stay and play” strategies depending on the patient's condition, context, and location (38). The organization includes BLS ambulances (mainly firefighters), ALS medicalized intensive care ambulances and in some places nurse vehicles (39). In the intricate ballet of extra-hospital medical interventions, each movement is gracefully orchestrated under the vigilant and discerning eye of the regulating physician, ensuring a harmonious symphony of care (40).
English-speaking actual system
Pre-hospital systems in English-speaking countries exhibit decentralization and fragmentation, with various EMS providers operating at the local level (41). Response times vary depending on the area and type of EMS service, aiming for an arrival time of 8 min to 12 min in urban areas. Personnel and training levels differ among English-speaking countries, with EMS teams consisting of paramedics, emergency medical technicians, and physicians, each requiring different levels of training. The equipment and services provided by EMS providers may vary based on location and business models.
The EMS hierarchy comprises basic life support (BLS) and advanced life support (ALS) stages, with state-specific utilization rates. BLS involves simple measures that can be performed by emergency medical personnel during transportation, while ALS includes invasive procedures such as endotracheal intubation and intravenous catheterization for managing complicated patients and delivering medications and fluids (41). However, EMTs could actually perform defibrillation, intramuscular injection of epinephrine and naloxone, and placement of supraglottic airways. Availability of specialist ALS services may vary, especially in rural areas, leading to potential delays and coordination challenges (42).
Israeli actual system
The Magen David Adom (MDA) is the sole EMS provider in the national-level Israeli pre-hospital system. With a single national phone number (101) for medical emergencies, the system is centralized. MDA intends to reach the scene of an emergency in urban regions within 8 min to 12 min and in rural areas within 20 min. Emergency medical technicians and paramedics make up the MDA EMS team. Between 250 h and a 2-year training program and a national certification test are requirements for all EMS providers. Paramedics have a 1-year course or a 3-year Bachelor's degree. Modern life support technology and transport trucks are available at MDA EMS. For patients with unique needs, such as newborn and pediatric patients, the system also offers pre-hospital care and transportation.
Systems differences
Systems evolution
Technology developments have also had an influence on the “scoop and run” vs. “stay and play” argument. Indeed, the “scoop and run” strategy was helped by French inventions and “stay and play” was helped by English-speaking ones.
Significant advancements in favor of “advanced field care” emerged during different historical periods. In World War I, the “petites Curies” mobile radiology unit was introduced, while the US Army Medical Service developed accessible transportation strategies during World War II (13, 43). Portable respirators led to the establishment of the corps of anesthesiologists-reanimators, and in 1956, the first inter-hospital transfer of patients on mechanical ventilation took place during the polio outbreak (44). Lyophilized plasma transfusion was initiated in 1994 through regional and national agreements (45, 46). The MORPHEE ICU unit was introduced in 2006, and in the 2010s, pre-hospital teams started utilizing Point of Care Ultrasound (POCUS) for assessments and diagnoses, redirecting patients to appropriate services (47, 48). New technologies like extracorporeal CPR and the Mobile Brain Stroke Unit with an onboard CT scanner were developed, while electrocardiogram became crucial for diagnosing acute coronary syndrome and Point-of-Care Troponin (POCT) or ionogram system useful in several pre-hospital situations (49–52).
Conversely, a number of developments have made the “scoop and run” more popular. Félix Hippolyte Larrey (1808–1895) continued his father's legacy by using mobile medical units to treat injured civilians during the French Revolution in 1830. Lucien Baudens (1804–1857) introduced the “Baudens' box” for stabilizing fractures during transportation (53). Charles Chrétien Henri Marc (1771–1845) published recommendations for immediate treatment of drowned and asphyxiated individuals in 1835. In the Russo-Japanese War of 1904, injured soldiers were transported using geophysical adaptation and sled evacuation, with Red Cross workers skiing over the snow (54). The medicalization of transportation and prompt resuscitation in the 1950s led to a decrease in the number of patients sent to advanced medical facilities. Lt. Alexis Santini (1914–1997) conducted the first helicopter transportation during the Indochina war (16). Olivier board (1950) provided stabilization during transportation, and Sauveur Piguillem (1930–2018) developed the Piguillem stretcher for airlifting in 1954. The VSAB (Emergency Vehicles for Asphyxiated and Injured) used to be called VSAV and underwent a name change in 2012. It is also worth highlighting the many changes that have contributed to the upscaling of rescue teams such as ECGs teletransmitted to medical regulation, new gestures (administration by aerosol, oral, intranasal or spraying of medicinal products, carrying out of electrocardiograms, etc.) authorized by the law of November 25, 2021, known as the Matras law.
Advancements in technology by 2030, including unmanned helicopters, pilotless flying ambulances, defibrillator-equipped support drones, and connected patient devices, will shape the concept of “EMS without eyes and without hands” (55–57). While these innovations offer promising possibilities, challenges like false positives and resource overuse must be addressed (58). Centralization and resource fusion will be crucial solutions. Telemedicine and mobile health technology enable remote patient monitoring and consultation, enhancing on-site treatment quality. Rapid point-of-care testing aids emergency physicians in making informed decisions. With these advancements, emergency physicians can effectively implement a kind of “stay and play” strategy, providing excellent on-site treatment for several medical situations.
Aspect of various approaches
In the “scoop and run” vs. “stay and play” argument, cost-effectiveness of various strategies is another aspect to take into account. It can be costly to convey patients to the finest hospital, especially when many cars or air transportation are required. A rescue helicopter, for example, costs 1.7 million euros a year in France, according to the French government (IGAS) (59). Further raising costs is the possibility that patients who are taken to the top hospital would need longer hospital stays or more intense care. On the other hand, providing on-site treatment may be more cost-effective in some cases, particularly for patients who do not require immediate transport to the hospital. For example, while costs of either prehospital advanced life support (ALS) and/or critical care per patient with out-of-hospital cardiac arrest (OHCA) are relatively low, significant costs are incurred during hospital treatment and after discharge in patients who survive with after effects (60). However, there is actually no cost-effectiveness study to compare “stay and play” and “scoop and run” on the financial side, but several concerning effectiveness according to indications for each model.
Both the French “field medicalization” and English-speaking “Scoop and Run” approaches have their merits and drawbacks. The French approach has been criticized for potential transfer delays in time-sensitive situations like severe trauma with uncontrolled bleeding. On the other hand, the English-speaking approach has faced criticism for inadequate on-site medical treatment and potential preventable death during transportation. Choosing between the two approaches depends on individual patient needs, prehospital and hospital resources and each specific emergency situation. The French approach could be preferable when advanced medical treatment is necessary, while the English-speaking approach excels in situations where swift transportation is crucial, especially in metropolitan areas with short travel times if all hospital resources are immediately available. The ongoing debate surrounding the “stay and play” vs. “scoop and run” EMS techniques continues, with differing opinions on which strategy is superior. The French approach prioritizes thorough on-site medical care over prompt patient transfer, based on the belief that immediate attention can improve outcomes, reduce after effects and sometimes the need for hospitalization. For instance, in the context of cardiac resuscitation, “stay and treat” must be used in order to maximize the likelihood of recovery and minimize the phenomenon of prolonged ischemia (61, 62). In contrast, the English-speaking “scoop and run” strategy places a higher priority on swift hospital transfer since it is thought that fast medical assistance at a hospital is the key to lifesaving (35, 36). With many American EMS systems switching to this method of first on-scene medical care of patients in cardiac arrest, international cardiac arrest literature has demonstrated a benefit from remaining and treating on site. Indeed, among patients experiencing out-of-hospital cardiac arrest, intra-arrest transport to hospital compared with continued on-scene resuscitation was associated with lower probability of survival to hospital discharge (63).
However, we have to add a caveat to that, as a study examining secondary carrying and transportation (to the adapted hospital/trauma center) found a correlation between increased mortality and sending badly injured patients to facilities that cannot provide definitive care (36). Moreover, despite the fact that the terms “over- and under-sorting of trauma patients” are frequently used in literature to allude to it, a randomized clinical trial compared ALS to BLS for penetrating trauma with no survival rate gain (64, 65). When it comes to specific, targeted scenarios like advanced airway care and cardiac arrest, ALS shines (63). The American approach to trauma includes quick off-scene transfer, basic airway treatment, and bleeding control (61). Medical expertise, technicality, patient care, and promptness all play a role in the nature of medical crises. While treating trauma (64, 66) or more difficult situations, time is invested in the patient's best interests by being decreased as far as is practicable by taking the time to stabilize the patient.
The practices of prehospital care in France and English-speaking countries, though nuanced in their system characteristics and outcomes, are not rigidly bifurcated. This landscape of emergency medical services shows a spectrum of approaches rather than a clear-cut division, underscoring a shared commitment to lifesaving care across different linguistic and geographic landscapes (67). This sweeping generalization fails to capture the rich tapestry of variation that characterizes the practices among English-speaking nations. It's a landscape where diversity in approach is not just common, but the norm, rendering any broad-brush characterization woefully inadequate in grasping the nuances of their medical methodologies (68). For instance, the acute trauma care systems in the US and Canada differ (69): Canada's more unified system ensures that about 80% of its populace is within an hour of a level I or II center, while the U.S., with its state-specific verification of trauma centers, presents a tapestry of variability across the country. In both Canada and the United States, efficient prehospital care is coupled with the recognition of post-discharge care as a financial challenge; while population-dense areas benefit from rapid access to well-developed trauma centers, those in remote regions face access hurdles, and with trauma centers ranging from level I (highest capability) to level IV, both systems, despite having room for improvement, effectively provide quality care to the vast majority of their injured patients.
Emergency staff training
In the “scoop and run” vs. “stay and play” argument, prehospital staff (paramedic or emergency physicians) training is a crucial consideration. Skilled and experienced caregivers will be able to initiate appropriate lifesaving interventions without losing any time.
Many countries are choosing to train their prehospital teams better and better, both for paramedics and for medical teams.
Since its founding 40 years ago (70), the French centers for emergency healthcare education (CESU) have helped to train more than 200,000 healthcare professionals each year. Since 2017 (71, 72), in France, Emergency Medicine has become a medical specialty with emergency medicine schools in the faculties of medicine in each university in France: 4-year training which will increase to 5 years to harmonize with Europe (73).
Moreover, in France, a new job concerning the EMS has appeared “Infirmier en Pratiques Avancées.” Initially, this job has been designed in order to delegate the follow-up of chronic diseases, then the mention “emergencies” on their diploma allows them to specialize in regulation, pre-hospital and in-hospital emergency medicine. Unfortunately, in terms of duration, their training (2 years into the emergency domain in addition to their initial 3 years nurse course) and lower than the English-speaking paramedics (6 months to 3 years according to the State).
In the front line of the emergency medical systems, first responders and non-medical individuals with medical expertise and flexibility are crucial and there are no “golden skills” (74).
The synthesis of information reveals the existence of diverse models within the Anglo-American (the US, Canada, and Australia…) paramedic system, where metaphorical models grounded in philosophical underpinnings delineate two novel subsystems: the professionally autonomous and the directive paramedic systems, with the latter further divided into rescue and hospital-managed submodels (75). In spite of this relative homogenous subdivision into the English-speaking world, inside the same system, the training could be different leading to various skills (76).
Physician default and medical demographics
Physician shortages play a significant role in shaping the “scoop and run” vs. “stay and play” debate. Different countries have pioneered approaches to address this issue, with Israel influencing the English-speaking model and France contributing innovations even to the “scoop and run” approach.
Emergency physicians specialize in acute care and patient stabilization, and the choice of strategy depends on factors such as the patient population demographics and the distance between the incident location and referral hospital. Utilizing helicopters for transportation to specialized reference hospitals, like trauma centers or cardiac catheterization facilities, can be efficient in certain situations. This type of transport triage has been in existence for trauma patients since at least the mid-1980s and for myocardial infarction and stroke patients for at least two decades (77).
However, resource scarcity must be considered. The effectiveness of the “stay and play” approach varies between rural and urban areas. In rural regions, helicopter transport between smaller hospitals and major medical centers is feasible, providing access to appropriate treatments. In contrast, rural areas may lack adequate technical infrastructure in some hospitals, leading to secondary transfers that can increase morbidity and mortality. These challenges emphasize the need for diverse approaches and innovative thinking in pre-hospital emergency medicine.
Organization and management
In 1927, Dr. Côt introduced medical prehospital care doctrine to the Parisian military Firefighters brigade, bringing battlefield principles to civilian emergency care (14). The doctrine emphasized: (a) Bringing the hospital to the victim, (b) Ensuring rigorous conditioning before transporting asphyxiated patients, (c) Implementing proven hospital-based therapeutic processes, (d) Recognizing the importance of “prompt help” before a doctor's arrival, (e) Restoring major physiological functions before departure, (f) Providing symptomatic treatment, and (g) Using appropriate vehicles for the mission.
In 2023, these principles remain completely relevant. In the 80s/90s, to save time, the firefighter VSAB would often depart with the victims and meet the SMUR team along the way. Currently in France, due to medical recruitment challenges, there is an evolving approach that includes the deployment of “Nurse precursor emergency teams” with graduated departures, inter-hospital nursing transfers in constant communication with a regulating doctor, and the development of paramedical regulation with specialized nurses or “Infirmier en Pratiques Avancées” (IPA) to provide varying levels of response.
However, the deployment of pre-hospital medical teams has the advantage of guaranteeing quality care from the first minutes, including far from the hospital or when the emergency department is already overloaded. Moreover, It seems important to maintain the attractiveness of emergency medicine careers among young students by preserving the medical aspect of pre-hospital treatment (78, 79).
The optimal level of prehospital care is also debated internationally for disaster medicine. In 1978, the red plan—a forerunner of NOVI (Nombreuses Victimes) national plan—was unveiled, and deployed during the 1995 attacks and hundreds of situations in France. At the same time, the Advanced Medical Post (AMP) was described as a place of categorization and care to assure early life saving interventions and prioritize the most urgent evacuations (80). Unfortunately, the Parisian attacks in 2015 have led to deploy “the Alpha Red plan” (anticipated since the 2000s to prepare a damage control response for large multi-site terrorist attacks), in order to combine rapid evacuation and prehospital lifesaving interventions (81). Speed and pre-hospital death avoidance are the cornerstones of the French alpha red plan. Contrast that with the “scoop and run,” which has drawbacks in emergency care (82). The goal of priority surgical hemostasis, which can only be achieved by sophisticated field care and efficient dispatching, must not be confused with a means, such as speedy transport. Therefore, a medical system should be adaptable depending on each unique, local circumstance (74). Recently, France has witnessed a subtle yet significant shift in its health policy landscape, marked by the introduction of new legislative measures like the decree on ORSAN, unveiled in early January 2024. This pivotal document ushers in an era of regionalized crisis management, moving away from the traditional reliance on zonal recourse, signaling a nuanced evolution in the country's approach to healthcare administration (83).
Worldwide, systems have changed, frequently in reaction to other developments in their local communities and healthcare systems. For instance, the US's trauma and emergency medical services systems have adjusted to the country's high rate of non-accidental penetrating trauma.
Perspectives
In the nuanced realm of emergency medical services (EMS), the juxtaposition of “field medicalization” and the “scoop and run” methodologies (74) offers a rich study in contrast. Each approach, with its distinctive set of pros and cons, is tailored to fit specific emergency scenarios, hinging significantly on variables like hospital resources and organizational frameworks. In crafting this manuscript, we delved into the historical intricacies of three systems—the Anglo-Saxon, French, and Israeli—territories of our expertise. Yet, as the tapestry of literature on English-speaking countries reveals (75), the broader landscape of pre-hospital systems is increasingly becoming a complex interweaving of the two models we introduced, each adapting and morphing in response to the unique demands of varying circumstances.
Notably, there's an evolving trend among organizations traditionally inclined toward the “scoop and run” model. These groups are increasingly emphasizing the enhancement of prehospital care quality. On the other hand, nations advocating for prehospital medicalization are intensifying efforts to reduce dispatch and transport durations, reflecting the dynamic evolution of EMS strategies. Irrespective of the specific EMS approach, the overarching priority remains the provision of prompt and appropriate medical care to patients (74).
Collaboration allows for efficient resource pooling, better patient preparation, and improved care. Real-time data sharing and technological advancements benefit from this collaboration (84). To maintain and advance this collaborative framework, it is crucial to encourage ongoing interactions between EMS and EDs. This goal can be realized through collaborative projects, specialized training programs, and robust communication channels. Additionally, the continual evolution of emergency medicine requires sustained research and investment. Comparative analyses of various EMS strategies and the establishment of shared data registries are vital for this advancement (84). Hence, international collaboration emerges as a key component in the enhancement of global healthcare systems, striving to uphold and elevate the quality of emergency medical care worldwide.
Author contributions
EL: Conceptualization, Investigation, Methodology, Writing—original draft, Writing—review & editing. NC: Validation, Writing—review & editing. OW: Validation, Writing—review & editing. ST: Validation, Writing—review & editing. ED: Conceptualization, Supervision, Validation, Writing—original draft, Writing—review & editing. EW: Validation, Writing—review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
Sarah Salvis (MSc-EMT) and General René Noto (MD).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
3. Barnes B, Bloor D, Henry J. Scientific knowledge. A sociological analysis. J Gen Philos Sci Z Für Allg Wiss. (1999) 30:173–6.
4. Barnes B, Edge DO. Science in Context: Readings in the Sociology of Science. Cambridge, MA: MIT Press (1982).
5. Pestre D. Pour une histoire sociale et culturelle des sciences. Nouvelles définitions, nouveaux objets, nouvelles pratiques. Annales. (1995) 50:487–522. doi: 10.3406/ahess.1995.279379
6. Pestré D. L'analyse de controverses dans l'étude des sciences depuis trente ans. Entre outil méthodologique, garantie de neutralité axiologique et politique. Mil Neuf Cent Rev Hist Intellect. (2007) 25:29–43. doi: 10.3917/mnc.025.0029
7. De Sahagun FB. Florentine Codex (1558). Available online at: https://www.google.fr/books/edition/Histoire_g%C3%A9n%C3%A9rale_des_choses_de_la_Nou/pK-4oOZVD6QC?hl=fr&gbpv=1&printsec=frontcover
8. Paré A. La Méthode de traiter les plaies faites par les arquebuts et autres bastons à feu, et celles qui sont faites par la poudre à canon (1545). Available online at: https://gallica.bnf.fr/ark:/12148/btv1b8609572j
9. Baker D, Cazalaà JB, Carli P. Resuscitation great. Larrey and Percy–a tale of two barons. Resuscitation. (2005) 66:259–62. doi: 10.1016/j.resuscitation.2005.03.009
11. Natchel H. L'organisation à Paris d'ambulances urbaines analogues à celles des grandes villes d'Amérique (1884).
12. Hallopeau H. Fonctionnement Complet d'un Service Chirurgical Transportable et Déplaçable Destiné à opérer, à panser les blessés du front. Paris: Presse Médicale (1915), 2
13. Riaud X. Médecine, Femmes et Première Guerre Mondiale. (2021). Available online at: https://www.quatrea.com/files/2021-05-medecine-femmes-et-premiere-guerre-mondiale.pdf (accessed May 21, 2021).
15. Drouet N. Mobile medical emergency units in France-part I. Br Med J Clin Res Ed. (1982) 284:1924–6. doi: 10.1136/bmj.284.6333.1924
18. Van Winsen N. Rétrospective et prospective du phénomène guerre. Mil Law Law War Rev. (1975) 14:191–2. doi: 10.4337/mllwr.1975.01-02.93
19. CirculaireDGS/650/MS 4 du 19 juillet 1972 Relative aux Directives Générales en ce qui Concerne les Secours Médicaux D'urgence (aide de l'Etat). - Programme Finalisé de Sécurité Routière (Sous-Programme ≪secours routier≫). - APHP DAJDP. (2023). Available online at: https://affairesjuridiques.aphp.fr/textes/circulaire-dgs650ms-4-du-19-juillet-1972-relative-aux-directives-generales-en-ce-qui-concerne-les-secours-medicaux-durgence-aide-de-letat-programme-finalise-de-securite-routiere-sous-prog/ (accessed November 10, 2023).
20. Loi n° 86-11 du 6 Janvier 1986 relative à l'aide Médicale Urgente et aux Transports Sanitaires. Available online at: https://www.legifrance.gouv.fr/loda/id/JORFTEXT000000512206
21. Bradwell S. Helps for Sudden Accidents (1663). Available online at: https://books.google.fr/books?id=BfhmAAAAcAAJ&printsec=frontcover&hl=fr&source=gbs_atb#v=onepage&q&f=false
22. Willard de F. Ambulance Service in Philadelphia. Philadelphia 188AD. Available online at: https://wellcomecollection.org/works/gmzkmw87/items
23. Hart HW. The conveyance of patients to and from hospital, 1720−1850. Med Hist. (1978) 22:397–407. doi: 10.1017/S002572730003341X
24. Pollock A. Historical Perspectives in the Ambulance Service. (2015). p. 17–28. doi: 10.1007/978-3-319-18642-9_2
25. Haller JS. The beginnings of urban ambulance service in the United States and England. J Emerg Med. (1990) 8:743–55. doi: 10.1016/0736-4679(90)90289-8
27. National Academy of Sciences (US) and National Research Council (US) Committee on Trauma, National Academy of Sciences (US) and National Research Council (US) Committee on Shock. Accidental Death and Disability: The Neglected Disease of Modern Society. Washington (DC): National Academies Press (US) (1966).
28. Carlson CL, Athelstan GT. The physician's assistant: versions and diversions of a promising concept. JAMA. (1970) 214:1855–61. doi: 10.1001/jama.214.10.1855
29. Baskett P, Safar P. The resuscitation greats. Nancy Caroline–from mobile intensive care to hospice. Resuscitation. (2003) 57:119–22. doi: 10.1016/S0300-9572(03)00127-8
30. Wacht O. International Paramedic Practice. The Development and History of the Paramedic Profession in Israel. (2023). Available online at: https://www.internationaljpp.com/features/article/the-development-and-history-of-the-paramedic-profession-in-israel (accessed November 10, 2023).
31. Hadas E, Eisenberg M, Nagel E. Emergency medical services in Israel. Am J Emerg Med. (1984) 2:366–7. doi: 10.1016/0735-6757(84)90172-4
32. Ellis DY, Sorene E. Magen David Adom–the EMS in Israel. Resuscitation. (2008) 76:5–10. doi: 10.1016/j.resuscitation.2007.07.014
33. Yafe E, Feingenberg Z, Miller R, Strugo R. Determination of death in mobile intensive care units operating without a physician. Harefuah. (2011) 150:918–34.
34. Hooker RS. Paramedics and physician assistants in Israel. Isr J Health Policy Res. (2020) 9:358. doi: 10.1186/s13584-019-0358-9
35. Haas B, Nathens AB. Pro/con debate: Is the scoop and run approach the best approach to trauma services organization? Crit Care. (2008) 12:224. doi: 10.1186/cc6980
36. Nirula R, Maier R, Moore E, Sperry J, Gentilello L. Scoop and run to the trauma center or stay and play at the local hospital: hospital transfer's effect on mortality. J Trauma. (2010) 69:595–9. doi: 10.1097/TA.0b013e3181ee6e32
37. Bagou G, Rebreyend-Colin M. Place du Personnel Infirmier à la Régulation du SAMU : Impact de la Transmission Systématique d'un bilan Secouriste par les Sapeurs-Pompiers. Paris (2004). Available online at: https://sofia.medicalistes.fr/spip/IMG/pdf/Place_du_personnel_infirmier_a_la_regulation_du_SAMU_impact_de_la_transmission_systematique_d_un_bilan_secouriste_par_les_sapeurs_pompiers.pdf (accessed November 9, 2023).
38. Cour des comptes. Rapport Annuel 2023 sur L'application des LFSS, Chapitre V (2023). Available online at: https://www.ccomptes.fr/sites/default/files/2023-10/20230524-RALFSS-2023_0.pdf
39. Revue E. Emergency Physicians International. Field Report: France. (2018). Available online at: https://www.epijournal.com/home/2018/5/17/field-report-france (accessed November 10, 2023).
40. Décret n° 2023-1376 du 29 Décembre 2023 Relatif Aux Conditions Techniques de Fonctionnement de L'activité Autorisée de Médecine d'urgence. 2023-1376 (2023). Available online at: https://www.legifrance.gouv.fr/jorf/id/JORFTEXT000048730410
41. McHugh DF, Driscoll PA. Accident and emergency medicine in the United Kingdom. Ann Emerg Med. (1999) 33:702–9. doi: 10.1016/S0196-0644(99)70201-5
42. Kornelsen J, Hobbs B, Buhler H, Kaus R, Grant K, Lamont SC, et al. High acuity rural transport: findings from a qualitative investigation. Rural Remote Health. (2018) 18:4316. doi: 10.22605/RRH4316
43. Douglas B. Kendrick. Blood Program in World War II - Digital Collections - National Library of Medicine. Medical Department, United States Army, in World War II and Clinical series (United States. Department of the Army. Office of the Surgeon General). Washington, DC: Office of the Surgeon General, Dept. of the Army : For sale by the Supt. of Docs., U.S. G.P.O. (1964).
44. Morris MJ. Acute respiratory distress syndrome in combat casualties: military medicine and advances in mechanical ventilation, military medicine, oxford academic. Mil Med. (2006) 171:1039–44. doi: 10.7205/MILMED.171.11.1039
45. Lemée G. Évaluation du plasma lyophilisé dans un trauma center de niveau 1, perspectives en médecine de l'avant (2017). Available online at: https://dumas.ccsd.cnrs.fr/dumas-01827853/document
46. Jost D, Lemoine S, Lemoine F, Derkenne C, Beaume S, Lanoë V, et al. Prehospital lyophilized plasma transfusion for trauma-induced coagulopathy in patients at risk for hemorrhagic shock: a randomized clinical trial. JAMA Netw Open. (2022) 5:e2223619. doi: 10.1001/jamanetworkopen.2022.23619
47. Beaussac M, Distinguin B, Turc J, Boutonnet M. Retour d'expérience des six évacuations sanitaires aériennes collectives MoRPHEE durant la pandémie de Covid-19. Ann Fr Médecine D'urgence. (2020) 10:272–7. doi: 10.3166/afmu-2020-0258
48. Ketelaars R, Reijnders G, van Geffen GJ, Scheffer GJ, Hoogerwerf N, ABCDE. of prehospital ultrasonography: a narrative review. Crit Ultrasound J. (2018) 10:17. doi: 10.1186/s13089-018-0099-y
49. Suverein MM, Delnoij TSR, Lorusso R, Brandon Bravo Bruinsma GJ, Otterspoor L, Elzo Kraemer CV, et al. Early extracorporeal CPR for refractory out-of-hospital cardiac arrest. N Engl J Med. (2023) 388:299–309. doi: 10.1056/NEJMoa2204511
50. Calderon VJ, Kasturiarachi BM, Lin E, Bansal V, Zaidat OO. Review of the mobile stroke unit experience worldwide. Interv Neurol. (2018) 7:347–58. doi: 10.1159/000487334
51. Alghamdi A, Cook E, Carlton E, Siriwardena A, Hann M, Thompson A, et al. Pre-hospital evaluation of sensitive TrOponin (PRESTO) study: multicentre prospective diagnostic accuracy study protocol. BMJ Open. (2019) 9:e032834. doi: 10.1136/bmjopen-2019-032834
52. Kevin Husson, Nicolas Pauchet, Barbara Decoulx, Patrick Goldstein. Apport de la biologie embarquée dans la gestion des urgences cardiorespiratoires en préhospitalier en 2018. Sang Thromb Vaiss. (2018) 30:21–5. doi: 10.1684/stv.2018.1011
53. Baudens L. On Military and Camp Hospitals: And the Health of the Troops in the Field. Being the Results of a Commission to Inspect the Sanitary Arrangements of the French Army, and Incidentally of Other Armies in the Crimean War. Amsterdam: Baillière Brothers (1862), 276.
55. Cheskes S, McLeod SL, Nolan M, Snobelen P, Vaillancourt C, Brooks SC, et al. Improving access to automated external defibrillators in rural and remote settings: a drone delivery feasibility study. J Am Heart Assoc. (2020) 9:e016687. doi: 10.1161/JAHA.120.016687
56. Schierbeck S, Svensson L, Claesson A. Use of a drone-delivered automated external defibrillator in an out-of-hospital cardiac arrest. N Engl J Med. (2022) 386:1953–4. doi: 10.1056/NEJMc2200833
57. Sedig K, Seaton MB, Drennan IR, Cheskes S, Dainty KN. “Drones are a great idea! What is an AED?” Novel insights from a qualitative study on public perception of using drones to deliver automatic external defibrillators. Resusc Plus. (2020) 4:100033. doi: 10.1016/j.resplu.2020.100033
58. Crampton NH. Ambient virtual scribes: Mutuo health's autoscribe as a case study of artificial intelligence-based technology - PubMed. Heal Manage Forum. (2020) 33:34–8. doi: 10.1177/0840470419872775
59. Fily J, du Mesnil d Buisson M, Laffont J, Guerin J, Mondoulet P, Marjoulet T. Les Hélicoptères de Service Public. Rev Dépenses (2016). Available online at: https://www.igas.gouv.fr/IMG/pdf/RD2016_helicopteres.pdf
60. Von Vopelius-Feldt J, Powell J, Benger JR. Cost-effectiveness of advanced life support and prehospital critical care for out-of-hospital cardiac arrest in England: a decision analysis model. BMJ Open. (2019) 9:e028574. doi: 10.1136/bmjopen-2018-028574
61. Timmermann A, Russo SG, Hollmann MW. Paramedic versus emergency physician emergency medical service: role of the anaesthesiologist and the European versus the Anglo-American concept. Curr Opin Anaesthesiol. (2008) 21:222–7. doi: 10.1097/ACO.0b013e3282f5f4f7
62. Pakkanen T, Virkkunen I, Kämäräinen A, Huhtala H, Silfvast T, Virta J, et al. Pre-hospital severe traumatic brain injury - comparison of outcome in paramedic versus physician staffed emergency medical services. Scand J Trauma Resusc Emerg Med. (2016) 24:62. doi: 10.1186/s13049-016-0256-x
63. Grunau B, Kime N, Leroux B, Rea T, Van Belle G, Menegazzi JJ, et al. Association of intra-arrest transport vs continued on-scene resuscitation with survival to hospital discharge among patients with out-of-hospital cardiac arrest. JAMA. (2020) 324:1058–67. doi: 10.1001/jama.2020.14185
64. Gauss T, Ageron FX, Devaud ML, Debaty G, Travers S, Garrigue D, et al. Association of prehospital time to in-hospital trauma mortality in a physician-staffed emergency medicine system. JAMA Surg. (2019) 154:1117–24. doi: 10.1001/jamasurg.2019.3475
65. Smith RM, Conn AKT. Prehospital care - scoop and run or stay and play? Injury. (2009) 40:S23–26. doi: 10.1016/j.injury.2009.10.033
66. Smith MEB, Chiovaro J, O'Neil M, Kansagara D, Quinones A, Freeman M, et al. Early Warning System Scores: A Systematic Review. Washington, DC: Department of Veterans Affairs (US) (2014).
67. Dick WF. Anglo-American vs. Franco-German emergency medical services system. Prehospital Disaster Med. (2003) 18:29–35. doi: 10.1017/S1049023X00000650
68. Makrides T, Smith F, Ross L, Gosling CM, Acker J, O'Meara P. No two systems are the same: paramedic perceptions of contemporary system performance using prehospital quality indicators. Cureus. (2021) 15:e35859. doi: 10.7759/cureus.35859
69. Lundy DW, Harvey EJ, Jahangir AA, Leighton RK. Trauma systems in North America. OTA Int. (20231) 2:e013. doi: 10.1097/OI9.0000000000000013
70. Arrêté du 12 avril 2018 fixant la liste des recherches mentionnées au 2° de l'article L. 1121-1 du code de la santé publique. Available online at: https://www.legifrance.gouv.fr/loda/id/JORFTEXT000036805796
71. Arrêté du 13 novembre 2015 fixant la liste des diplômes d'études spécialisées de médecine. Available online at: https://www.legifrance.gouv.fr/loda/id/JORFTEXT000031560595
72. Riou B. 2017 : l'an 1 du diplôme d'études spécialisées de médecine d'urgence. Ann Fr Médecine D'urgence. (2017) 7:1–4. doi: 10.1007/s13341-017-0710-z
73. Machard P. Les Médecins Urgentistes Veulent Porter leur Internat à 5 ans | egora.fr. (2023). Available online at: https://www.egora.fr/etudiants/internat/80750-les-medecins-urgentistes-veulent-porter-leur-internat-a-5-ans (accessed November 10, 2023).
74. Hoejenbos MJJ, McManus J, Hodgetts T. Is there one optimal medical treatment and evacuation chain for all situations: “scoop-and-run” or “stay-and-play”. Prehospital Disaster Med. (2008) 23:s74–8. doi: 10.1017/S1049023X00021294
75. Makrides T, Ross L, Gosling C, Acker J, O'Meara P. Exploring the structure and characteristics of the Anglo-American paramedic system in developed countries: a scoping review. Int J Emerg Serv. (2021) 11:248–62. doi: 10.1108/IJES-05-2021-0025
76. Bollinger M, Mathee C, Shapeton AD, Thal SC, Russo SG. Differences in training among prehospital emergency physicians in Germany. Notf Rettungsmedizin. (2022) 25:23–30. doi: 10.1007/s10049-022-01021-z
77. Liberman M, Branas CC, Mulder DS, Lavoie A, Sampalis JS. Advanced versus basic life support in the pre-hospital setting – the controversy between the ‘scoop and run' and the ‘stay and play' approach to the care of the injured patient. Int J Disaster Med. (2004) 2:9–17. doi: 10.1080/15031430410025515
78. Pelaccia T, Roy PM, Douillet D, Bilbault P, Abbiati M. Qu'est-ce qui motive [ou non] les étudiants en médecine à choisir comme spécialité la médecine d'urgence? Ann Fr Médecine Urgence. (2019) 9:221. doi: 10.3166/afmu-2019-0166
79. Douillet D, Ammirati C, Amsallem C, Hausfater P, Fonsegrive J, Annweiler C, et al. Quelle est la motivation des internes de la première promotion du DES de médecine d'urgence ? Ann Fr Médecine D'urgence. (2019) 9:213–20. doi: 10.3166/afmu-2019-0165
80. Travers S. Advanced Medical Posts (AMP). Disaster Medicine Pocket Guide: 50 Essential Questions: Work of the French Society of Disaster Medicine. Cham: Springer International Publishing (2022). p. 55–8.
81. Lesaffre X, Tourtier JP, Violin Y, Frattini B, Rivet C, Stibbe O, et al. Remote damage control during the attacks on Paris: lessons learned by the Paris Fire Brigade and evolutions in the rescue system. J Trauma Acute Care Surg. (2017) 82:S107. doi: 10.1097/TA.0000000000001438
82. Carli P, Puidupin A, Braun F. Le damage control pré-hospitalier n'est pas le scoop and run. J Eur Urgences Réanimation. (2017) 29:3–7. doi: 10.1016/j.jeurea.2017.02.003
83. Décret n° 2024-8 du 3 janvier 2024 relatif à la préparation et à la réponse du système de santé pour faire face aux situations sanitaires exceptionnelles. 2024-8 (2024). Available online at: https://www.legifrance.gouv.fr/jorf/id/JORFTEXT000048851655
Keywords: EMS, scoop and run, stay and play, pre-hospital emergency care, history, controversy
Citation: Lansiaux E, Cozzi N, Wacht O, Travers S, Drouin E and Wiel E (2024) Scoop and treat: from an historical controversy to the emergency future. Front. Disaster Emerg. Med. 2:1340348. doi: 10.3389/femer.2024.1340348
Received: 17 November 2023; Accepted: 29 January 2024;
Published: 14 February 2024.
Edited by:
Robert Ehrman, Wayne State University, United StatesReviewed by:
Robert Dunne, Wayne State University, United StatesIsabelle Piazza, Papa Giovanni XXIII Hospital, Italy
Copyright © 2024 Lansiaux, Cozzi, Wacht, Travers, Drouin and Wiel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Edouard Lansiaux, edouard.lansiaux.etu@univ-lille.fr
†ORCID: Edouard Lansiaux orcid.org/0000-0002-4342-8707
 Edouard Lansiaux
Edouard Lansiaux Nicholas Cozzi
Nicholas Cozzi Oren Wacht3
Oren Wacht3  Emmanuel Drouin
Emmanuel Drouin