Khat use and associated factors during pregnancy in eastern Ethiopia: A community-based cross-sectional study
- 1Department of Psychiatry, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 2School of Public Health, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 3Department of Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 4School of Nursing and Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
Introduction: Women of reproductive age are increasingly using khat. The use of khat is associated with prelabor rupture of membranes, anemia among pregnant women, and other problems related to motherhood and infanthood. Most of the previous studies performed at the facility level revealed that different factors were associated with khat use among pregnant women. Lower educational status, low wealth index, and the age of the mother were the factors significantly associated with maternal khat use. Partner substance use also has a significant association with maternal khat use. However, there is limited information about khat use and its associated factors among pregnant women in the study area.
Objective: This study aims at assessing the prevalence of khat use and associated factors among pregnant women in Kersa and Haramaya Health and Demographic Surveillance System Sites, eastern Ethiopia.
Methods: A community-based cross-sectional study design was employed among randomly selected 1,015 pregnant women from an open cohort from Kersa and Haramaya Health and Demographic Surveillance System Sites in Ethiopia. Data were collected through face-to-face interviews from January 30 to April 30, 2021, using Open Data Kit (ODK) software and analyzed using SPSS v-26. Descriptive statistics were used to summarize the characteristics of pregnant women. Factors associated with khat use were identified by bivariate and multivariable logistic regression analyses; an adjusted odds ratio (AOR) with a 95% confidence interval (CI) was estimated. Statistical significance was declared at p < 0.05.
Results: The prevalence of khat use among pregnant women was 15.5% (95% CI, 13.3–17.7). Age of the pregnant women; being in the age group between 25 and 35 years (AOR = 2.27, 95% CI, 1.33–4.89) and 35 years and greater (AOR = 2.33, 95% CI, 1.29–4.20); having a chronic medical illness (AOR = 3.28, 95% CI, 1.27–8.48); and having a history of abortion (AOR = 2.87 95% CI, 1.73–4.76) significantly increased the likelihood of khat use among pregnant women.
Conclusion: The current study revealed a relatively high magnitude of khat use in pregnant women as compared with previous studies. The age of the pregnant women, history of medical illness, and history of abortion were significantly associated with khat use during pregnancy.
Introduction
Khat (Catha edulis) is an evergreen plant that is widely used in the Middle East, Somalia, East Africa, and Ethiopia (1, 2). Cathinone is the most important chemical found in young leaves and shoots of khat. It also contains cathine, nor-ephedrine, and other chemicals (3). Khat is believed to have the same effect as amphetamine, a stimulant of the central nervous system (4). Acute oral administration of khat offers a sense of euphoria, cheerfulness, relief from fatigue, increased energy levels, the ability to communicate easily, the capacity to associate ideas, and improved self-confidence (5). However, these symptoms are typically followed by discomforts including depression, anxiety, and insomnia (1).
Khat chewing poses many health-related problems. Khat chewing among reproductive-age women is on the rise, and it is a risk factor for serious reproductive health problems among pregnant women. These problems include intrauterine growth retardation, low birth weight (LBW), and increased infant mortality (2). It also is a risk factor for lower lipoid level, sexual impotence, and inhibition of uteroplacental blood flow, which can lead to a teratogenic effect and the impairment of fetal growth (6). Hence, among pregnant women, consumption of khat affects the growth of the fetus by inhibiting uteroplacental blood flow and, consequently, impairs fetal growth (2).
Complex physiological changes occur during pregnancy and result in the impairment of sleep and memory. The adverse effects of khat on memory and sleep may further aggravate those impairments (7). Problematic khat use is a possible risk factor for harmful use of other psychoactive substances such as alcohol, and it was observed that one of the risk factors for engaging in risky sexual behavior was pushed by the effect of khat after chewing (8).
A national longitudinal survey conducted in the United States showed that women with a history of abortion were reported to use different types of substances (9, 10). In another national population survey carried out in Yemen, about 40.7% of women surveyed reported chewing khat while pregnant during the previous 5 years before the survey. This study also revealed that old age, no education, rural residence, living in mountainous regions, and low wealth were significant risk factors for chewing khat (5). A study designed to determine the psychosocial correlates of substance use among women attending antenatal services at a tertiary hospital in southwestern Nigeria revealed that the presence of medical conditions was associated with substance use among pregnant women (11).
A study conducted in eastern Ethiopia revealed that khat chewing is associated with prelabor rupture of membranes among pregnant women (12). Another study performed in rural communities in eastern Ethiopia indicated that khat chewing was associated with anemia among pregnant women (13). Cross-sectional studies conducted at primary healthcare centers in Ethiopia revealed that the prevalence of khat chewing ranged from 9.9% to 35.8% of pregnant women chewing khat during the current pregnancy (14, 15).
Khat use increased with increasing age, remaining constant after age 35, having a child, having a lower educational level, and not pertaining to the lowest wealth index category. Not being in a marital relationship with the most recent sex partner and protestant religion were protective factors (16). The outcome of the multivariable analysis showed that partner khat use, alcohol use, and mental distress were factors significantly associated with current khat use (15).
Despite the high prevalence of khat use during pregnancy, the focus of most studies has been to assess the magnitude of khat use among the general population and college students, but the magnitude of khat use among pregnant women and its determinant factors are not well addressed in Ethiopia. As per the authors’ knowledge, there is no empirical evidence reporting on the magnitude, pattern, and associated factors of khat use during pregnancy in the study area. Therefore, this study aims at filling this gap by assessing the magnitude and associating factors of khat use among pregnant women in eastern Ethiopia. The findings of this study can also help planners and decision-makers by showing the magnitude and pattern of khat chewing during pregnancy. Furthermore, the findings of this study will be used as baseline information for further studies.
Methods and materials
Study setting, period, and study design
This study has employed a community-based cross-sectional study design with the quantitative method. It was conducted in Kersa and Haramaya Health and Demographic Surveillance Sites (HDSS) from January 30 to April 30, 2021. Kersa HDSS is in Kersa District, Oromia Regional State, and eastern Ethiopia. There are 35 rural subdistricts (called kebeles) and three small-town kebeles. According to the 2007 national census, the district has a total population of 172,626 of whom 6.9% are urban dwellers. The Kersa HDSS covers 24 of the 38 kebeles, with 4 health centers and 10 health posts. There are 18 elementary, 2 secondary, 1 preparatory, and 2 religious schools in the HDSS area, as well as 134 mosques, 8 churches, and 6 farmers’ training stations. Most of the inhabitants are farmers, with a minority working in small trade, government posts, or casual laborers (17). Haramaya HDSS is a new site, which was established in 2018. It covers 12 rural kebeles. At baseline, the total number of households in the HDSS was 17,461, and the total population was 99,898 (51,259 males and 48,639 females), of whom 23.86% were women of reproductive age (18).
Characteristics of the population
All pregnant women who were living in Kersa and Haramaya HDSS sites were the source population, and all pregnant women who were in the selected kebeles from January 30 to April 30, 2021, were included in the study. Pregnant women who were not able to communicate due to serious medical illnesses during the study period were excluded from the study.
Data collection measurements
Semistructured and structured questionnaires were deployed to gather data on participants’ khat use during the current pregnancy, sociodemographic variables such as age, marital status, religion, ethnicity, educational status, occupation, and wealth index. Other factors include reproductive, obstetric, and gynecological characteristics such as gravidity, parity, gestational age, history of abortion, antenatal care follow-up, interval between last delivery and last normal menstrual period, history of gynecological problem, history of gynecological operation; and psychosocial and other substance use characteristics, such as intimate partner violence (IPV), alcohol use (ever and current), tobacco (ever and current), and other substances.
Current khat use was assessed based on questions developed from different pieces of literature (15, 19). A study participant who reported chewing khat during the current pregnancy was considered a current khat chewer. Ever-use of substances was assessed based on the questions developed from various kinds of literature too (15, 19). A study participant who answered “yes” to a question that asked about lifetime use of khat was considered an ever-user of khat. Common mental disorder (CMD) was assessed by using the self-reporting questionnaire (SRQ-20). The SRQ-20 is composed of 20 yes/no items asking about the experience of depression, anxiety, panic, and somatic symptoms in the preceding 30 days. For this study, the total score was dichotomized (SRQ-20 < 6 vs. SRQ ≥ 6), and those who scored SRQ ≥ 6 indicated having CMD (20). Household economic status was assessed by using questions adapted and modified from the Ethiopian Demographic and Health Survey (EDHS) of 2016 (21). The experience of IPV was assessed using the World Health Organization (WHO) multicountry study questionnaire constituting psychological, physical, and sexually violent acts often accompanied by controlling behavior where a single positive answer indicated the presence of violence (22).
Sample techniques/procedures
The sample size was estimated using a single population proportion formula, with the assumptions that, the corresponding standard value (Zα/2) at 95% confidence level = 1.96, 4% of margin of error, =4%, design effect (deff) = 1.5, the proportion of khat chewing (p) among pregnant women from the previous study conducted in Butajira (14), southern Ethiopia = 35.8%. Then, the result gave a sample size of 828. By considering a 10%, nonresponse rate the final sample size gave 911.
For the factors associated with current khat use, sample size was estimated using the double population proportion formula using OpenEpi online software, and the minimum sample size was far below the 911 obtained single population proportion formula and then 911 was considered as the so-called “minimum required sample size.” However, this study was part of a larger project on the impact of maternal common mental disorder on the obstetric outcome, birth outcomes, infant nutritional status and maternal functioning in Kersa and Haramaya Health and Demographic Surveillance Site, eastern Ethiopia, with a sample size of 1,160. Therefore, a total of 1,160 were considered as a total sample size.
There were 24 kebeles in Kersa and 12 kebeles in Haramaya HDSS sites. From the total kebeles on each site, sample kebeles were selected using lottery methods. Finally, the total sample size was proportionally allocated to the total population of pregnant women in sampled kebeles, and they were selected using lottery methods (Figure 1).
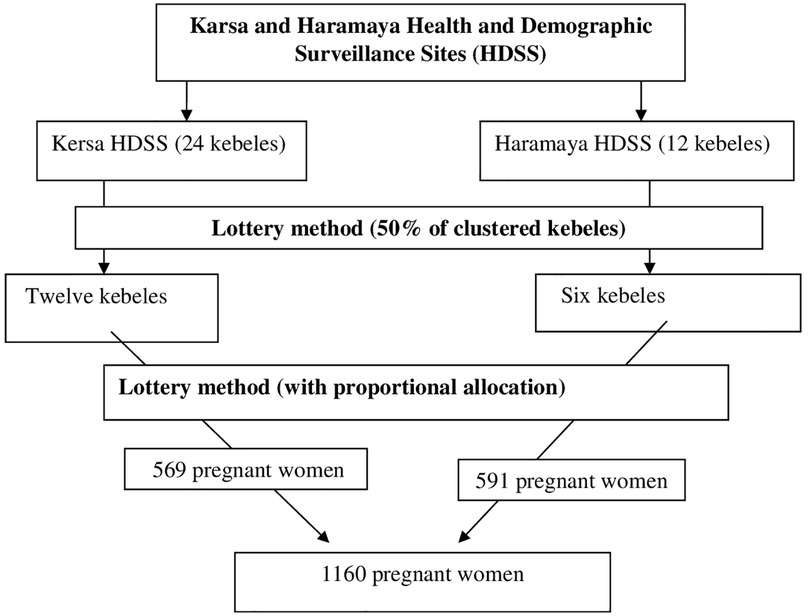
Figure 1. Schematic presentation of the sampling procedure for assessing khat use and associated factors among pregnant women.
Data collection procedure
Twenty data collectors who have been working in Kersa and Haramaya HDSS sites collected the data for this study. In addition, six MSc holders were supervising the data collection process. An intensive 3-day training was provided for data collectors and supervisors. The data were collected by face-to-face interviews using structured and semistructured questionnaires prepared in an Open Data Kit collect form, and completed data were sent directly to the server. Pregnant women were interviewed in separate rooms in their home environment or inside their compounds during all working hours of seven days a week. During the interviews, all the WHO recommendations/precautions for the prevention of COVID-19 infection were implemented.
Data quality assurance
To maintain consistency of the data collection tool, the questionnaire was prepared first in the English language and translated to Afan Oromo and back to the English language by professional translators. Data collectors and supervisors took training. To evaluate the acceptability and applicability of the procedures and tools, a pretesting was carried out on 5% of the sample size in Harar town 1 week before the actual data collection. To maintain the completeness and consistency of the questionnaire, supervisors and investigators closely supervised the data collectors during the data collection process.
Statistical analysis
After collection, the data clerk checked and cleaned the data; each questionnaire was checked for completeness and then coded. The data clerk entered the data into the computer using EpiData (Version 3.1, EpiData Association, Denmark) and then exported and analyzed the data using SPSS (Version 26; IBM Corp., Armonk, NY, United States). Categorical variables were described using frequencies and percentages.
In this study, bivariate and multivariate logistic regression was used. All variables with a p-value of ≤0.25 in bivariate logistic regression were taken to multivariable logistic regression. The strength of the association was described by odds ratio and 95% confidence interval (CI), and a p-value less than 0.05 was considered statistically significant. Multicollinearity of independent variables was tested using the variance inflation factor (VIF). In addition, model goodness of fit was checked by using Hosmer–Lemeshow test and the p-value was 0.834.
Results
Sociodemographic characteristics
From a total of 1,160 participants selected for the study, 1,015 consented to participate in the study yielding a response rate of 87.5%. Those participants who refused to participate in this study complained multiple reasons without any regard to the sociodemographic, clinical, and reproductive conditions. The mean age of the participants was 30.1 years (SD = 8.5). The majority of the study participants [982 (96.75%)] were married in their current relationship; 1,012 (99.7%) were Muslim followers and 1,010 (99.51%) were Oromo in ethnicity. About 772 (76.06%) of the participants neither read nor write and 900 (88.67) were housewives. About 388 (38.2%) participants were on the first quantile of the wealth index (Table 1).
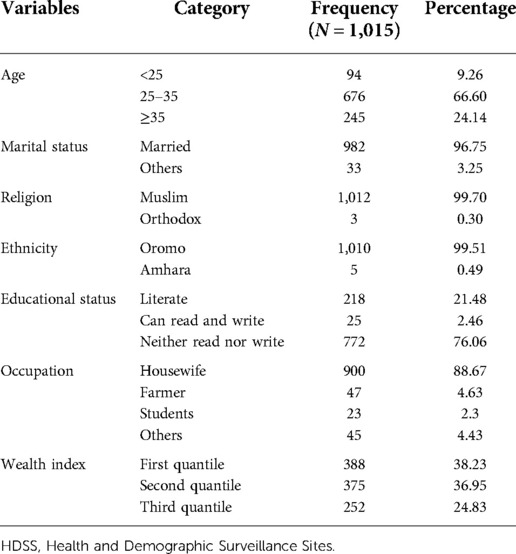
Table 1. Sociodemographic and economic characteristics of pregnant women at Kersa and Haramaya HDSS sites, 2021
Clinical characteristics
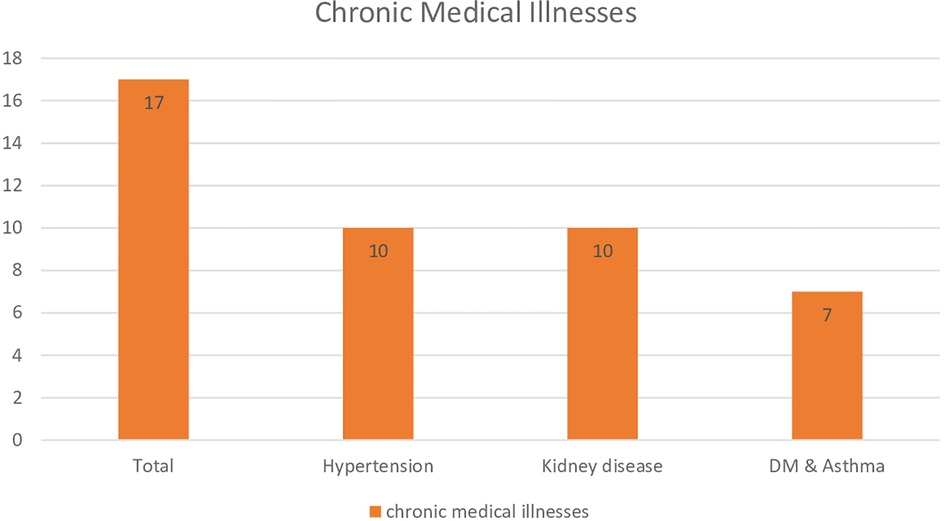
The study showed that 26 (2.56%) of the participants included in this study had a history of mental illness with a mean duration of 2.7 years (SD = 1.37). Of them, 10 (38.46%) were on treatment during the study period. On the other hand, 23 (2.27%) of the participants had chronic medical illnesses and 17 (73.91%) were on treatment. Hypertension [10 (43.48%)], kidney disease [10 (43.48%)], and other chronic illnesses such as diabetes and asthma [7 (30.34%)] were the medical conditions reported by the women (Figure 2).
Reproductive, obstetric, and gynecological characteristics
The majority of the study participants were multigravida of 4 and above [542 (53.40%)]. About 472 (46.50%) of the participants were multipara of 4 and above. Over half (52.12%) of the participants were in the third trimester and the median gestational age of the pregnant women was 32 weeks (IQR = 8). Ninety-eight (9.66%) of the participants had a history of abortion, while 488 (48.08%) have antenatal care (ANC) follow-up. About 70 (6.9%) of the participants had a history of gynecological problems, where tumor (41.43%) was the most prevalent one. The mean pregnancy interval and age at first marriage were 1.7 years (SD = 0.56) and 17.7 years (SD = 2.12), respectively (Table 2).
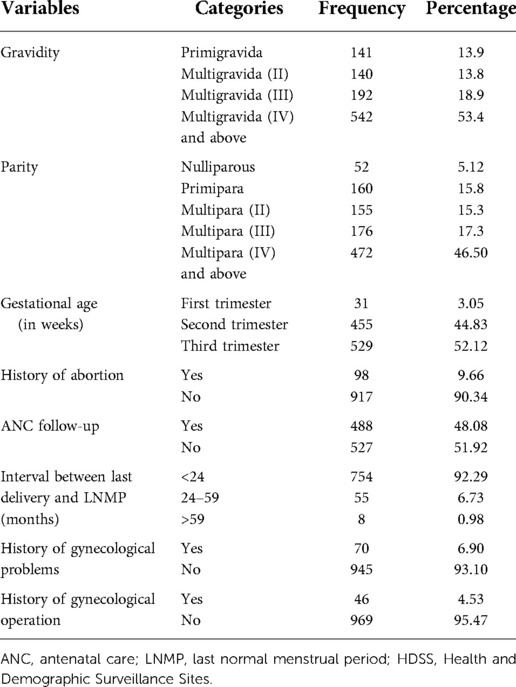
Table 2. Reproductive, obstetric, and gynecological characteristics of pregnant women at Kersa and Haramaya HDSS sites, 2021 (n = 1015)
Psychosocial and other substance use characteristics
A significant proportion of the pregnant women had experienced IPV during the current pregnancy. About 493 (48.6%) had reported that they had experienced the violence. Very few, four and nine, of the participants ever used alcohol and tobacco, respectively. Two (0.2%) and six (0.6%) of the pregnant women were current users of alcohol and tobacco, respectively (Table 3).

Table 3. Psychosocial and other substance use behavioral characteristics of pregnant women at Kersa and Haramaya HDSS sites, 2021 (n = 1,015).
Prevalence of khat use
The result of this study showed that the prevalence of current khat use among pregnant women was 15.5% (95% CI, 13.3–17.7). The prevalence of ever khat use was 20.1% (95% CI, 17.8–22.5).
Description of the outcome variable with some selected independent variable
About 154 of the married pregnant women use khat and 143 of the pregnant housewives were using khat. Sixty-four pregnant women from the second quartile of the wealth index use khat; 70 pregnant women who have experienced intimate partner violence use khat while 87 pregnant women who have not experienced intimate partner violence use khat. All (6) of the current tobacco user pregnant women were also using khat. About 114 pregnant women who have four or more pregnancies were using khat, about 98 pregnant women who have delivered four or more times use khat, and 5 pregnant women who had gynecological operations use khat (Table 4).
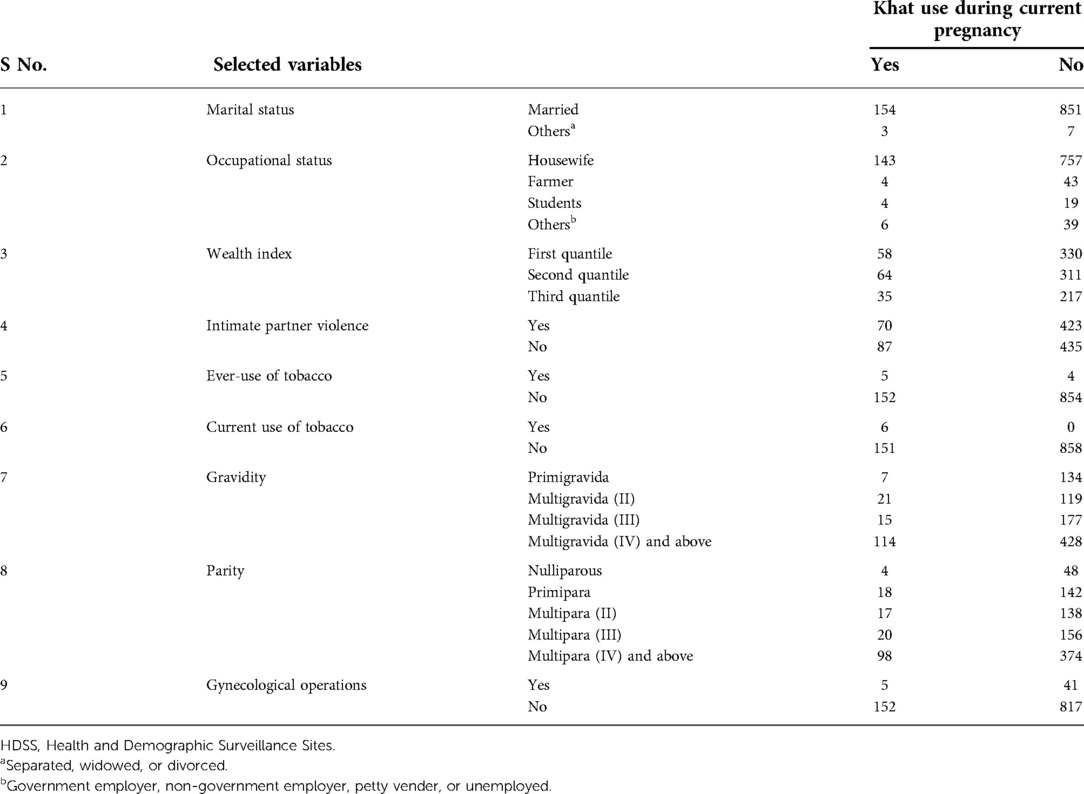
Table 4. Selected variables and the magnitude of khat use during pregnancy at Kersa and Haramaya HDSS sites, 2021 (n = 1,015).
Factors associated with khat use during pregnancy
To identify different factors associated with khat use bivariate and multivariable logistic regressions were performed. In the bivariate logistic model age, educational status, presence of common mental disorder, presence of chronic medical illnesses, number of deliveries, history of abortion, ANC follow-ups, and gynecological problems were associated with khat use with a p-value of ≤0.25. However, after controlling the potential confounders by using multivariable logistic regression, only age, presence of medical illness, and history of abortion were significantly associated with khat use among pregnant women with a p-value of <0.05.
Those pregnant women aged 25–35 were 2.27 times more likely to use khat during the current pregnancy than those pregnant women aged less than 25 years old [adjusted odds ratio (AOR) 2.27, 95% CI, 1.33–4.89]. Likewise, those pregnant women aged 35 or more years were 2.33 times more likely to use khat as compared with those aged less than 25 years old (AOR: 2.33, 95% CI, 1.29–4.20). Additionally, those pregnant women with chronic medical illnesses were 3.28 times more likely to be khat users as compared with those pregnant women without chronic medical illnesses (AOR: 3.28, 95% CI, 1.27–8.48). Finally, those pregnant women with a history of abortion were 2.87 times more likely to be khat users during the current pregnancy than those without a history of abortion (AOR: 2.87, 95% CI, 1.73–4.76) (Table 5).
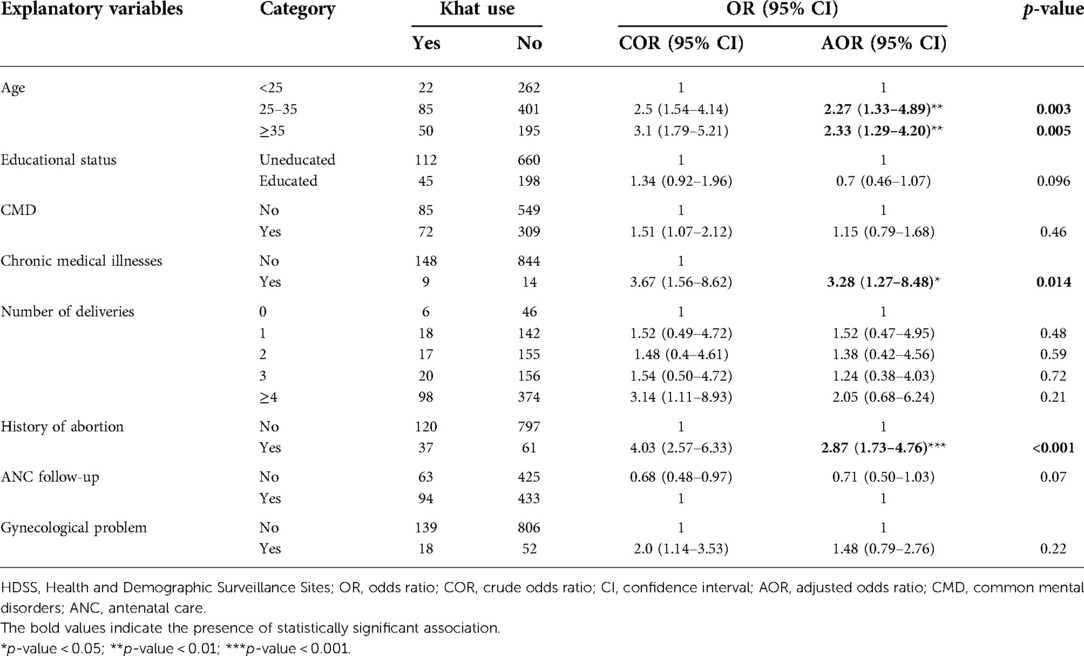
Table 5. Factors associated with khat use among pregnant women in Kersa and Haramaya HDSS sites, 2021.
Discussion
The prevalence of khat use among pregnant women in this study was 15.5% (95% CI, 13.3–17.7). The finding of this study is higher than studies conducted in other parts of the country. According to the Ethiopian Demographic and Health Survey 2016, the current prevalence of khat chewing among women was 8.4% (16) and a study conducted in the Gedeo zone among pregnant women in primary healthcare revealed that the prevalence was 9.9% (15). The discrepancy might be attributable to variations in the characteristics of the sample, cultural differences in attitudes toward chewing a khat, and methodological differences between the studies. For instance, the study conducted in the Gedeo zone is a facility-based survey compared with our study which is a community-based study that involved a sample of mothers from rural areas, which is known to have variation from urban areas in both substances use patterns and access to healthcare (23, 24).
On other hand, this finding was lower than studies conducted in other parts of Ethiopia and other countries: in eastern Ethiopia (19.6%) (25), Butajira (35.8%) (14), Jimma (24.9%) (26), and Yemen (40.7%) (5). These variations might be due to the low concurrence use of other substances such as cigarettes and alcohol in the study samples. This pattern was different from other countries such as Yemen where simultaneous use of khat and tobacco is common, particularly among men (27). As evidenced by another study (28), social desirability of response bias, self-reporting about substance use could be the other reason for the lower prevalence of khat use.
The result of this study revealed that the age of the mothers, history of medical illness, and history of abortion were significantly associated with current khat use among pregnant women.
The odds of pregnant women aged 25–35 years were 2.39 times more likely to use khat when compared with those aged less than 25 years. The odds of those pregnant women aged greater than or equal to 35 years or more were 2.52 times more likely to use khat currently than those aged less than 25 years old. This indicates that as the age increased, the odds of khat use during pregnancy also increased. This result was congruent with a community-based study conducted in Ethiopia (16), and a national population survey conducted in Yemen where older women were shown to be khat chewers (5). The possible reason may be that as age increases, women are more likely to have changes in life situations such as bereavement, loneliness, poor social support, and financial difficulties, all of which have been found to increase the risk of substance use (29, 30).
The result of this study revealed another associated factor, and that those pregnant women who had a history of chronic medical illness were 3.18 times more likely to use khat during pregnancy than those who have had no history of medical illness. In a cross-sectional study of psychoactive substance use among pregnant women attending antenatal clinics at a federal government-owned tertiary hospital in Ogun state, southwestern Nigeria, there was an association between the presence of the medical conditions and lifetime use of other drugs (11). Also, it has been shown that in a study of 1,141 consecutive deliveries at delivery centers in the Yemen Arab Republic, significantly more khat chewers had concomitant diseases (31). The most likely explanation for this association is that khat has an identified wide range of adverse effects on the cardiovascular, gastrointestinal, and other peripheral systems (32–35).
Furthermore, in our study, pregnant women with a history of abortion had a higher odd of khat use. Those pregnant women who had a history of abortion were 2.79 times more likely to use khat during pregnancy than those who had no history of abortion. A study conducted in southern Ethiopia (36) revealed that there is a significant association between the history of abortion and substance use. Similarly, different studies conducted in the United States (9, 10, 37) and Norway (38) have shown a significant association between the history of abortion and substance use. There are several possible explanations for this significant finding. Women with a history of abortion reported five times more subsequent abuse of substance following abortion. Abortion can be considered one of life's stressful events, which leads women to use substances as a coping mechanism. On the other hand, pregnancy can also be considered stressful and may lead women to begin abusing substances (39). Abortion was found to be associated with an increased risk of substance abuse disorders (40). Women with a history of abortion may have a greater need to use emotion-altering substances during pregnancy, because the subsequent pregnancy may arouse unresolved feelings related to the abortion. Women with a history of abortion, compared with their peers who opt for delivery, also may be more liberal, inclined to take risks, and/or tend to be involved in difficult partner relationships more often (41, 42).
Limitations of the study
This study has some limitations. Due to the nature of a cross-sectional study design, we could not explore the cause-and-effect relationships of the khat use and the independent variables. In addition to this, the study did not include the quantity and frequency of khat use. Furthermore, the laboratory screening for khat use was not performed, and this makes it difficult to corroborate the findings. Finally, a face-to-face interview method might induce recall bias and social desirability responses bias.
Conclusions
The current study revealed that the use of khat was relatively high among pregnant women as compared with the previous studies. Special emphasis is paramount for pregnant women of increased age, those with medical illnesses, and those with a history of abortion, which were the factors significantly associated with khat chewing during pregnancy.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Health Research Ethics Review Committee of College of Health and Medical Sciences of Haramaya University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
All authors contributed to the inception of the study, organized the data collection process, equally contributed to data analysis, drafted or revised the article, and agreed to be accountable for all aspects of the work. All authors contributed to the article and approved the submitted version.
Funding
This research has been funded by Haramaya University (HURG_2020_02_02_80). The university has no influence on the design, research methodology, result presentation and others.
Acknowledgments
We would like to thank Kersa and Haramaya Health and Demographic Surveillance Sites staff, supervisors, data collectors, and all study participants for the valuable effort they made with the provision of quality data during the study period.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio; CMD, common mental disorder; EDHS, Ethiopian Demographic and Health Survey; LBW, low birth weight; WHO, World Health Organization
References
1. Nakajima M, Jebena MG, Taha M, Tesfaye M, Gudina E, Lemieux A, et al. Correlates of khat use during pregnancy: a cross-sectional study. Addict Behav. (2017) 73:178–84. doi: 10.1016/j.addbeh.2017.05.008
2. Mwenda JM, Arimi MM, Kyama MC, Langat DK. Effects of khat (Catha edulis) consumption on reproductive functions: a review. East Afr Med J. (2003) 80(6):318–23. doi: 10.4314/eamj.v80i6.8709
3. Al-Hebshi N, Skaug N. Khat (Catha edulis)—an updated review. Addict Biol. (2005) 10(4):299–307. doi: 10.1080/13556210500353020
4. World Health Organization. Assessment of khat (Catha edulis Forsk). Proceedings of the 34th Meeting of the Expert Committee on Drug Dependence (March 28 to 31, 2006). Switzerland, Geneva: WHO Press (2006).
5. Khawaja M, Al-Nsour M, Saad G. Khat (Catha edulis) chewing during pregnancy in Yemen: findings from a national population survey. Matern Child Health J. (2008) 12(3):308–12. doi: 10.1007/s10995-007-0231-2
6. Abdel-Aleem MA. Khat chewing during pregnancy: an insight on an ancient problem. Impact of chewing Khat on maternal and fetal outcome among Yemeni pregnant women. J Gynecol Neonatal Biol. (2015) 1(2):28–31. doi: 10.15436/2380-5595.15.004
7. Manzar MD, Salahuddin M, Sony P, Maru TT, Pandi-Perumal SR, Moscovitch A, et al. Sleep disturbances and memory impairment among pregnant women consuming khat: an under-recognized problem. Ann Thorac Med. (2017) 12(4):247. doi: 10.4103/atm.ATM_24_17
8. Mihretu A, Teferra S, Fekadu A. Problematic khat use as a possible risk factor for harmful use of other psychoactive substances: a mixed method study in Ethiopia. Subst Abuse Treat Prev Policy. (2017) 12(1):1–7. doi: 10.1186/s13011-016-0086-x
9. Reardon DC, Coleman PK, Cougle JR. Substance use associated with unintended pregnancy outcomes in the national longitudinal survey of youth. Am J Drug Alcohol Abuse. (2004) 30(2):369–83. doi: 10.1081/ADA-120037383
10. Steinberg JR, Finer LB. Examining the association of abortion history and current mental health: a reanalysis of the National Comorbidity Survey using a common-risk-factors model. Soc Sci Med. (2011) 72(1):72–82. doi: 10.1016/j.socscimed.2010.10.006
11. Daniel A, Emmanuel B, Timothy A. Psychosocial correlates of psychoactive substance use among pregnant women. Int Neuropsychiatr Dis J. (2018) 11(1):1–12. doi: 10.9734/INDJ/2018/39639
12. Yadeta TA, Egata G, Seyoum B, Marami D. Khat chewing in pregnant women associated with prelabor rupture of membranes, evidence from eastern Ethiopia. Pan Afr Med J. (2020) 36:1. doi: 10.11604/pamj.2020.36.1.22528
13. Kedir H, Berhane Y, Worku A. Khat chewing and restrictive dietary behaviors are associated with anemia among pregnant women in high prevalence rural communities in eastern Ethiopia. PLoS One. (2013) 8(11):e78601. doi: 10.1371/journal.pone.0078601
14. Alamneh AA, Endris BS, Gebreyesus SH. Caffeine, alcohol, khat, and tobacco use during pregnancy in Butajira, South Central Ethiopia. PLoS One. (2020) 15(5):e0232712. doi: 10.1371/journal.pone.0232712
15. Mekuriaw B, Belayneh Z, Yitayih Y. Magnitude of Khat use and associated factors among women attending antenatal care in Gedeo zone health centers, southern Ethiopia: a facility based cross sectional study. BMC Public Health. (2020) 20(1):1–8. doi: 10.1186/s12889-019-8026-0
16. Yitayih Y, van Os J. Prevalence and determinants of chewing khat among women in Ethiopia: data from Ethiopian demographic and health survey 2016. BMC Psychiatry. (2021) 21(1):1–8. doi: 10.1186/s12888-021-03136-y
17. Assefa N, Oljira L, Baraki N, Demena M, Zelalem D, Ashenafi W, et al. HDSS profile: the Kersa health and demographic surveillance system. Int J Epidemiol. (2016) 45(1):94–101. doi: 10.1093/ije/dyv284
18. Gudata ZG, Dheresa M, Mengesha G, Roba KT, Yusuf J, Daraje G, et al. Cohort profile: the Haramaya health and demographic surveillance system (Haramaya HDSS). Int J Epidemiol. (2021) 51(2):e46–54. doi: 10.1093/ije/dyab232
19. Alem A, Kebede D, Kullgren G. The prevalence and socio-demographic correlates of khat chewing in Butajira, Ethiopia. Acta Psychiatr Scand. (1999) 100:84–91. doi: 10.1111/j.1600-0447.1999.tb10699.x
20. Beusenberg M, Orley JH, World Health Organization. A user's guide to the self reporting questionnaire (SRQ No. WHO/MNH/PSF/94.8). Geneva: World Health Organization (1994).
21. CSA, ICF. Ethiopia demographic and health survey 2016. Addis Ababa: Central Statistical Agency of Ethiopia (2017).
22. García-Moreno CJH, Ellsberg M, Heise L, Watts C. WHO multi-country study on women's health and domestic violence against women: initial results on prevalence, health outcomes and women's responses. Geneva: World Health Organization (2005).
23. Haile D, Lakew Y. Khat chewing practice and associated factors among adults in Ethiopia: further analysis using the 2011 demographic and health survey. PLoS One. (2015) 10(6):e0130460. doi: 10.1371/journal.pone.013046
24. Kenea D, Jisha H. Urban-rural disparity and determinants of delivery care utilization in Oromia region, Ethiopia: community-based cross-sectional study. Int J Nurs Pract. (2017) 23(1):1–10. doi: 10.1111/ijn.12510
25. Fetene MT, Teji K, Assefa N, Bayih WA, Tsehaye G, Hailemeskel HS. Magnitude and associated factors of substance use among pregnant women attending antenatal care in public hospitals of eastern Ethiopia. BMC Psychiatry. (2021) 21(1):1–12. doi: 10.1186/s12888-021-03078-5
26. Tesso FY, Woldesemayat L, Kebede DB. Magnitude of substance use and associated factors among pregnant women attending Jimma town public health facilities, Jimma Zone, Oromia Regional State Southwest Ethiopia. Clinics Mother Child Health. (2017) 14(275):2. doi: 10.4172/2090-7214.1000275
27. Nakajima M, al’Absi M, Dokam A, Alsoofi M, Khalil NS, Al Habori M, et al. Gender differences in patterns and correlates of khat and tobacco use. Nicotine Tob Res. (2013) 15(6):1130–5. doi: 10.1093/ntr/nts257
28. Latkin CA, Edwards C, Davey-Rothwell MA, Tobin KE. The relationship between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in Baltimore, Maryland. Addict Behav. (2017) 73:133–6. doi: 10.1016/j.addbeh.2017.05.005
29. Simoni-Wastila L, Yang HK. Psychoactive drug abuse in older adults. Am J Geriatr Pharmacother. (2006) 4(4):380–94. doi: 10.1016/j.amjopharm.2006.10.002
30. Ziegler PP. Addiction in older women: American health care's best-kept secret. J Calif Dent Assoc. (2008) 36(2):115–8. Available at: https://pubmed.ncbi.nlm.nih.gov/18411973/ accessed date (April 20, 2022)18411973
31. Eriksson M, Ghani NA, Kristiansson B. Khat-chewing during pregnancy-effect upon the off-spring and some characteristics of the chewers. East Afr Med J. (1991) 68(2):106–11. https://pubmed.ncbi.nlm.nih.gov/2040229/ accessed date (April 24, 2022)2040229
32. Al-Hadrani AM. Khat induced hemorrhoidal disease in Yemen. Saudi Med J. (2000) 21(5):475–7. Available at: https://pubmed.ncbi.nlm.nih.gov/11500685/ accessed date (April 22, 2022)11500685
33. Vanwalleghem IE, Vanwalleghem PW, De Bleecker JL. Khat chewing can cause stroke. Cerebrovasc Dis. (2006) 22(2–3):198. doi: 10.1159/000093807
34. Al-Motarreb A, Al-Habori M, Broadley KJ. Khat chewing, cardiovascular diseases and other internal medical problems: the current situation and directions for future research. J Ethnopharmacol. (2010) 132(3):540–8. doi: 10.1016/j.jep.2010.07.001
35. Tesfaye F, Byass P, Wall S, Berhane Y, Bonita RJ. Peer reviewed: association of smoking and khat (Catha edulis Forsk) use with high blood pressure among adults in Addis Ababa, Ethiopia, 2006. Prev Chronic Dis. (2008) 5(3):A89. Available at: https://pubmed.ncbi.nlm.nih.gov/18558039/ accessed date (May 2, 2022)18558039
36. Mekuriaw B, Belayneh Z, Shemelise T, Hussen R. Alcohol use and associated factors among women attending antenatal care in Southern Ethiopia: a facility based cross sectional study. BMC Res Notes. (2019) 12(1):1–7. doi: 10.1186/s13104-019-4703-4
37. Steinberg JR, McCulloch CE, Adler NE. Abortion and mental health: findings from the national comorbidity survey-replication. Obstet Gynecol. (2014) 123(2 pt 1):263. doi: 10.1097/AOG.0000000000000092
38. Pedersen W. Childbirth, abortion and subsequent substance use in young women: a population-based longitudinal study. Addiction. (2007) 102(12):1971–8. doi: 10.1111/j.1360-0443.2007.02040.x
39. Reardon DC, Ney PG. Abortion and subsequent substance abuse. Am J Drug Alcohol Abuse. (2000) 26(1):61–75. doi: 10.1081/ADA-100100591
40. Coleman PK, Coyle CT, Shuping M, Rue VM. Induced abortion and anxiety, mood, and substance abuse disorders: isolating the effects of abortion in the national comorbidity survey. J Psychiatr Res. (2009) 43(8):770–6. doi: 10.1016/j.jpsychires.2008.10.009
41. Amaro H, Fried LE, Cabral H, Zuckerman B. Violence during pregnancy and substance use. Am J Public Health. (1990) 80(5):575–9. doi: 10.2105/ajph.80.5.575
Keywords: khat use, pregnant women, substance use, associated factors, eastern Ethiopia
Citation: Misgana T, Tesfaye D, Alemu D, Gebremichael B, Tamiru D, Tariku M, Weldesenbet AB and Dheresa M (2022) Khat use and associated factors during pregnancy in eastern Ethiopia: A community-based cross-sectional study. Front. Glob. Womens Health 3:941300. doi: 10.3389/fgwh.2022.941300
Received: 11 May 2022; Accepted: 7 November 2022;
Published: 2 December 2022.
Edited by:
Ephrem Engidawork, Addis Ababa University, EthiopiaReviewed by:
Triphonie Nkurunziza, World Health Organization—Regional Office for Africa, Republic of CongoMarkos Tesfaye, St. Paul's Hospital Millennium Medical College, Ethiopia
© 2022 Misgana, Tesfaye, Alemu, Gebremichael, Tamiru, Tariku, Weldesenbet and Dheresa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dejene Tesfaye dejudeme01@gmail.com
Specialty Section: This article was submitted to Maternal Health, a section of the journal Frontiers in Global Women's Health
 Tadesse Misgana
Tadesse Misgana Dejene Tesfaye
Dejene Tesfaye Daniel Alemu
Daniel Alemu Berhe Gebremichael
Berhe Gebremichael Dawit Tamiru
Dawit Tamiru Mandaras Tariku
Mandaras Tariku Adisu Birhanu Weldesenbet
Adisu Birhanu Weldesenbet Merga Dheresa
Merga Dheresa