Immigration and C-sections incidence: Maternal care and perinatal outcomes in the context of the pandemic in Chile
- 1Programa de Doctorado en Salud Pública, Escuela de Salud Pública, Facultad de Medicina, Universidad de Chile, Santiago, Chile
- 2Departamento de Promoción de la Salud de la Mujer y el Recién Nacido, Facultad de Medicina, Universidad de Chile, Santiago, Chile
- 3Servicio de Ginecología y Obstetricia, Complejo Hospitalario San José, Servicio de Salud Metropolitano Norte, Santiago, Chile
- 4Programa de Bioestadística, Escuela de Salud Pública, Facultad de Medicina, Universidad de Chile, Santiago, Chile
- 5Programa de Microbiología, Instituto de Ciencias Biomédicas, Facultad de Medicina, Universidad de Chile, Santiago, Chile
- 6Programa de MBA con Especialización en Salud, Instituto de Salud Pública, Universidad Andrés Bello, Santiago, Chile
Introduction: Immigration has increased significantly in Chile. Despite that all pregnant women, regardless of nationality and immigration status, have the right to access to all healthcare services during pregnancy, childbirth, and postpartum, inequities in health care outcomes and health provision have been reported. During COVID-19 pandemic, these inequities are completely unknown.
Objective: The aim of this study was to compare the incidence of c-sections according to mother's migration status, as well as other maternal care and perinatal outcomes in women giving birth at San José Hospital in Santiago, Chile, during the COVID-19 pandemic.
Methods: A retrospective cohort study was designed including 10,166 registered single births at the San José Hospital between March 2020 and August 2021. To compare between groups, statistical tests such as Chi-square and Fisher's exact were used. Log Binomial regression models were performed adjusted for potential confounding variables. To estimate the strength of association the relative risk was used.
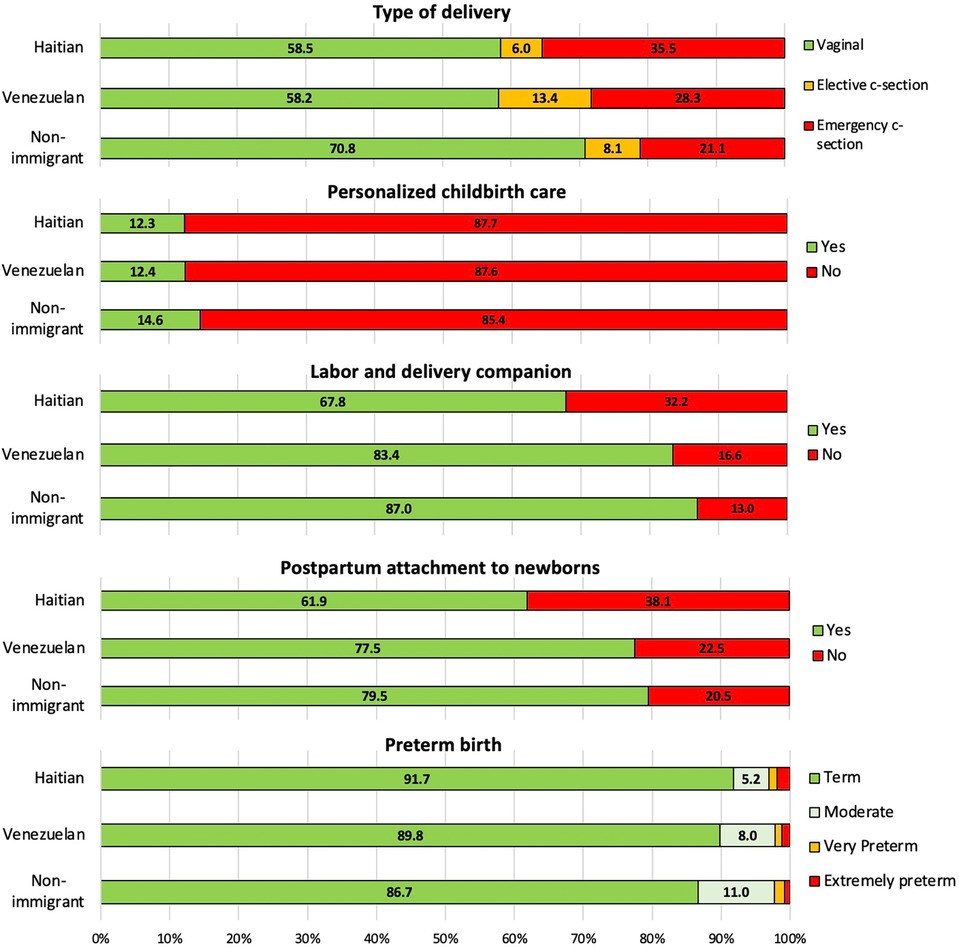
Results: Immigrant mothers account for 48.1% of the registered births. Compared to non-immigrant women, immigrants exhibit a higher proportion of c-section, specifically, emergency c-section (28.64% vs. 21.10%; p-value < 0.001) but a lower proportion of and having a preterm birth (8.24% vs. 13.45%; p < 0.05), receiving personalized childbirth care (13.02% vs. 14.60%; p-value < 0.05), companion during labor and childbirth (77.1% vs. 86.95%; p-value < 0.001), And postpartum attachment to newborn (73% vs. 79.50%; p-value < 0.001). The proportion of COVID exposure was not significant between groups, not the severity also. Haitians had a highest risk of undergoing emergency c-section (aRR = 1.61) and Venezuelans had a highest risk of elective c-section (aRR = 2.18) compared to non-immigrants.
Conclusion: This study reports high rates of c-sections in the entire population, but in immigrant populations it is even higher. Additionally, it found gaps in maternal care and perinatal outcomes between immigrants and non-immigrants. More studies are needed to elucidate the possible causes of these differences and establish new regulations to protect the reproductive rights of the immigrant population.
1. Introduction
Immigration has increased significantly in Chile. In 20 years, it went from being 0.8% in 1992, to 7.5% in 2021 (1), however, due to their demographic characteristics, immigrants' mothers account for the 16.4% of live births, with the top five maternal nationalities being Haiti (21.6%), Venezuela (17.1%), Peru (12.5%), Bolivia (7.9%), and Colombia (6.8%) (2). Some international studies have reported higher C-section rates among the immigrant population compared to the local population (3, 4). While the causes for these higher rates remain unknown, certain risk factors have been identified, such as language or communication barriers, inadequate prenatal care even after a shorter stay in the host country, socioeconomic status, and lack of health insurance (5, 6).
Chile is one of the few countries in Latin America and the Caribbean that has reached the advanced stage of the obstetric transition (7). One of the major challenges at this stage is the excessive obstetric interventionism and medicalization of childbirth, as a consequence, Chile has one of the highest rates of c-sections in the region, reaching 43.1% of total births in the public system in 2020 (8). Moreover, an increasing rate of obesity in women of childbearing age (9, 10), delayed pregnancy, and barriers to access to healthcare for the immigrant population (11–13), are urgent priorities to be addressed.
COVID-19 has been associated with an increase in adverse maternal and perinatal health conditions, such as preterm birth and maternal hospitalization (14, 15). According to Haye et al., during the pandemic, there was an observed increase in C-section rates (16). However, it remains unclear whether this increase is due to the perinatal consequences of COVID-19 or changes in medical decision-making regarding C-section practice, or the impact of other factors such as immigration (17).
In Chile, pregnant women, regardless of nationality and immigration status, have access to all healthcare services during their pregnancy, childbirth, and up to 12 months postpartum within the public system (18). Despite immigrants having the same rights as the non-immigrant population, the inequities in health care and health outcomes are unknown.
At the beginning of the pandemic period, hospitals modified protocols to reduce the spread of the virus, so the maternal care provision changed, visitors were prohibited, companionship during labor and childbirth was reduced and the attachment to the baby was restricted in mothers with COVID-19. Due to the concern of hospital collapse because of the excess of COVID-19 cases and high levels of stress or depression observed in mothers giving birth (19), providing a positive birth experience was a challenge.
The aim of this study was to compare the incidence of C-sections, obstetric and neonatal outcomes according to the mother's migration status when giving birth at San José Hospital in Santiago, Chile, during the COVID-19 pandemic.
2. Methods
2.1. Study design and population
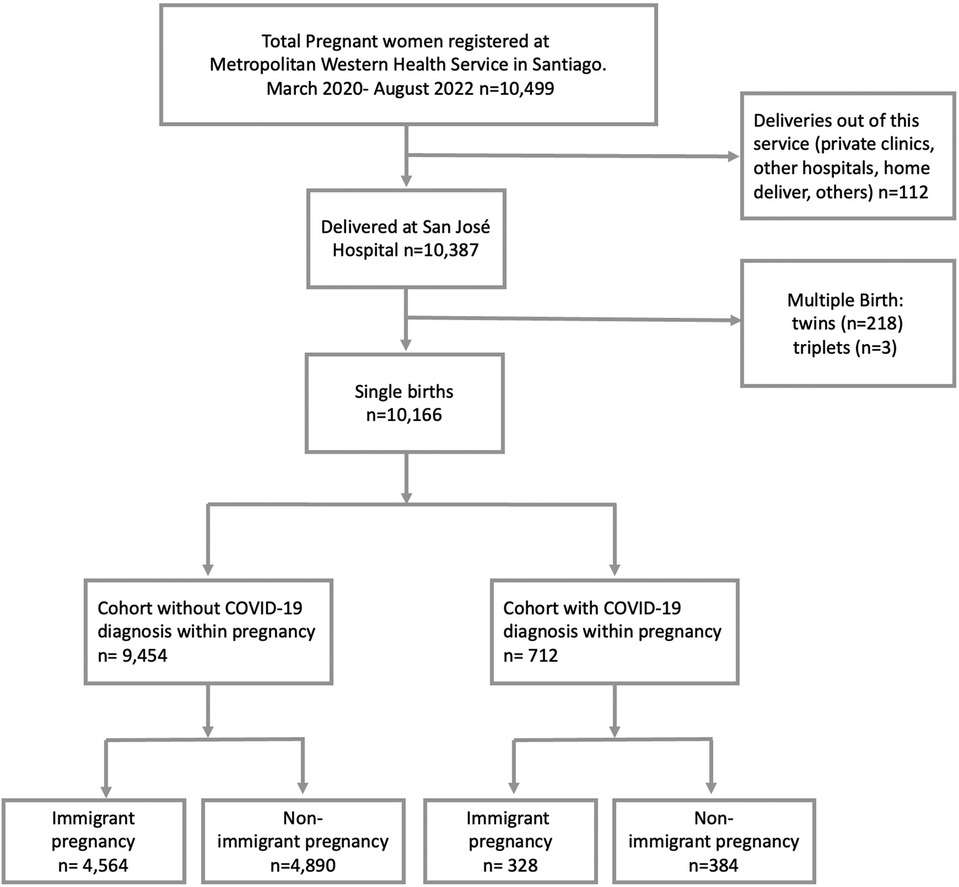
A retrospective cohort study was designed including 10,166 registered single births at the San José Hospital between March 2020 (pandemic's starting date in Chile) and August 2021 (before the vaccination of pregnant women began) (Figure 1). The San José Hospital is a high complexity public's health provider, serving a population of approximately 1.2 million. Nearly 50% of pregnant women are immigrants according to previous reports, with the most common nationalities being Haiti, Venezuela, and Peru. The data was obtained from the systematized clinical records. The diagnosis of COVID-19 was made using Polymerase Chain Reaction (PCR). At the beginning of the pandemic, the PCR test was performed as screening on patients with clinical symptoms. Subsequently, from May 2020 the PCR was taken preventively to all hospitalized patients admitted to the hospital. That means that asymptomatic patients could be undiagnosed, in consequence, a slight underestimation of the parameter within the first two months is expected.
2.2. Instrument and variables
The data was gathered from the hospital's clinical record and the women's health agenda, which includes historical records of pregnancy check-ups.
2.2.1. Exposure variables
The data was analyzed in terms of non-immigrant and immigrant status (non-immigrant = 0, immigrant = 1). Then, specific analyses were conducted considering the most prevalent nationalities, pair comparison such as Haitians with non-immigrants, Venezuelan with non-immigrants, and finally, immigrants from other nationalities were included in comparison to non-immigrants.
2.2.2. Outcome variables
The main outcome variable of this study was the type of delivery, categorized as vaginal birth, forceps-assisted vaginal birth, elective c-section, and emergency c-section. For a separate analysis of elective c-section and emergency c-section categories, vaginal birth (including forceps-assisted births) was used as the reference.
Maternal care variables are personalized childbirth care, labor and childbirth companion, postpartum attachment to newborns (defined as the immediate connection that occurs once the baby is born, involving skin-to-skin contact with the mother and the promotion of the first breastfeeding within the first 30 min and a maximum of one hour) (20). Finally, neonatal variables include newborn sex (female, male, undefined), Apgar score, gestational weeks at birth, and newborn weight and height.
2.2.3. Covariables
Clinical variables related to COVID-19 include severity of exposure illness (non-COVID, mild illness, moderate illness, and severe illness) (Figure 2), critical patient unit (CPT), pneumonia, mechanical ventilation, prone position, pulmonary embolism (TEP), and hospitalization based on disease severity. Other maternal covariables are maternal obesity and labor induction.
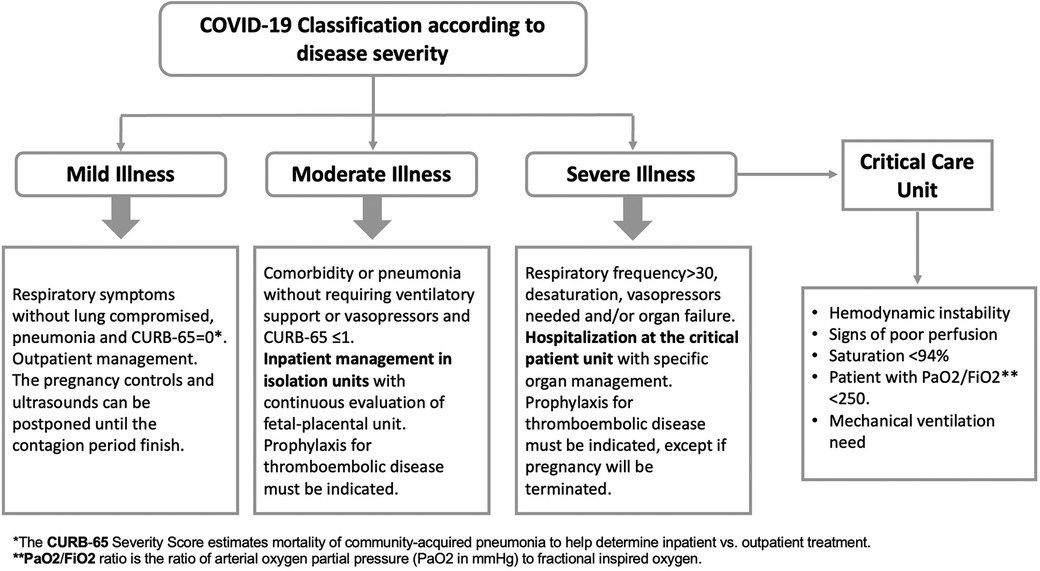
Figure 2. Case management protocol of SARS-CoV-2 virus (COVID-19) during pregnancy, puerperium, and mother-baby dyad care at the San José hospital, in Santiago of Chile.
Sociodemographic variables include age (in years) and type of health insurance (FONASA is the State-run health service founded by public taxes and the 7% of the income deduction; private insurance is funded using the contributions of their members).
2.3. Statistical analysis
Categorical variables were presented as frequency and percentage, while quantitative variables were categorized. To compare between groups, statistical tests such as Chi-square and Fisher's exact test (with less than 5 observations) were used, considering a p-value <0.05 as significant. Log Binomial multivariable regression models were used to calculate risk ratios (RRs) crude and adjusted for potential confounding variables to estimate the strength of association between nationality variable and types of c-section (elective and emergency). The data were analyzed using Stata software version 18.
3. Results
10,166 births were registered at the San José Hospital within the study period. The immigrant population was 48.12% (n = 4,892), the most prevalent countries of origin were Haiti 36.41% (n = 1,781), Peru 24.9% (n = 1,218), and Venezuela 19.91% (n = 974).
Immigrants have a lower percentage of women under 19 years-old compared to non-immigrant group (4.03% vs. 8.76% respectively; p < 0.05) and a higher proportion of women aged 35 years-old and more, although this difference was not statistically significant.
A significant difference was found in the type of health insurance between the two groups. Immigrants register a higher percentage of enrollment to FONASA A compared to non-immigrants (80.09% vs. 55.46%, respectively), but a lower proportion of enrollment to FONASA B and C compared to non-immigrant women. Non-significant differences were found in private health insurance (ISAPRE) between the groups.
Regarding parity, a higher percentage of immigrant women were primiparous compared to non-immigrants (38.88% vs. 30.24% respectively; p < 0.05). A significant difference was found in body mass index (BMI) between the two groups. Immigrants has a lower percentage of obesity (BMI 30 or more), compared to non-immigrant women (53.85% vs. 70.05%, respectively; p-value <0.001). No significant differences were found in the prevalence of COVID-19 between both groups (Table 1).
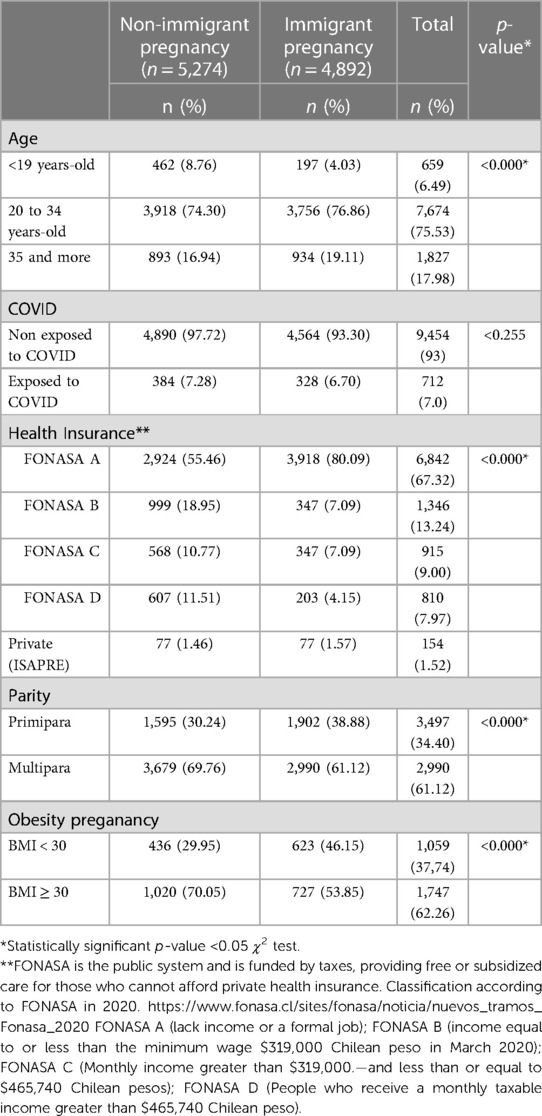
Table 1. Sample characterization. Cohort of 10,166 single births at the hospital San José in Santiago of Chile between March 2020 to August 2022.
Immigrant women had a higher proportion of c-sections compared to non-immigrant women, specifically emergency c-sections (28.64% vs. 21.10%; p-value <0.001). In contrast, vaginal births were more frequent in non-immigrant women (69.6%).
Regarding maternal care provision, immigrant women registered a significantly smaller percentage of receiving personalized care or having a companion compared to non-immigrant women, and had less postpartum attachment with their babies, compared to immigrant women. Furthermore, immigrants have a lower proportion of preterm births compared with non-immigrants (p-value <0.001) (Table 2).
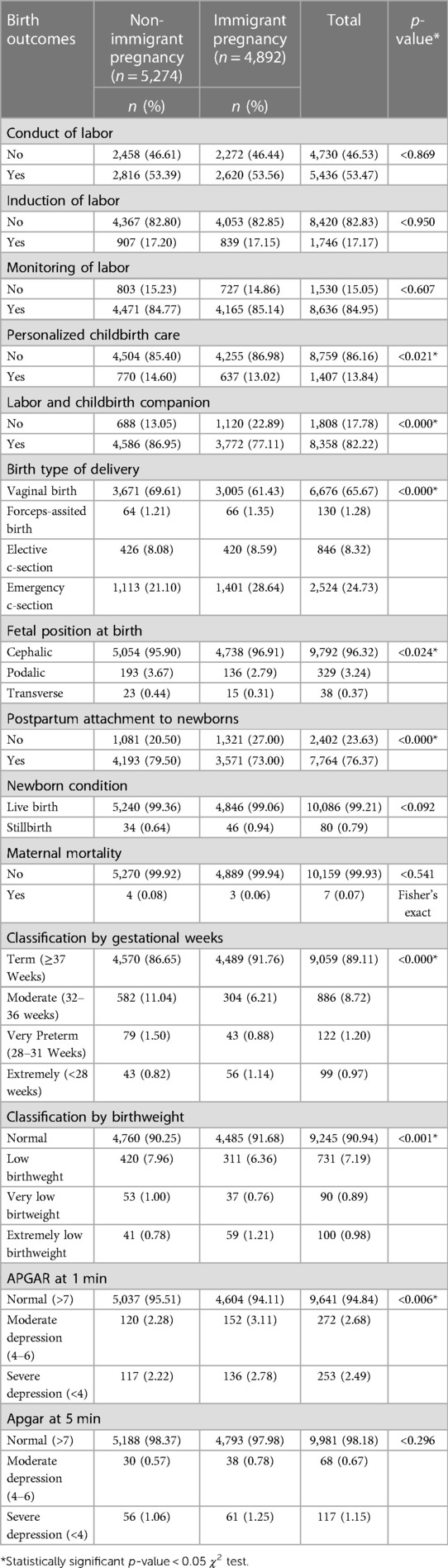
Table 2. Comparison of obstetric and perinatal outcomes between non-immigrant and immigrant pregnant women in the context of a COVID-19 pandemic. Hospital San José, Santiago of Chile. March 2020 to August 2022.
Regarding the COVID-19 no differences were found in the severity of illness, need for admission to the Intensive Care Unit (ICU), the presence of pneumonia, the use of mechanical ventilation, prognosis complications, pulmonary embolism (PE), between the two groups (Table 3).
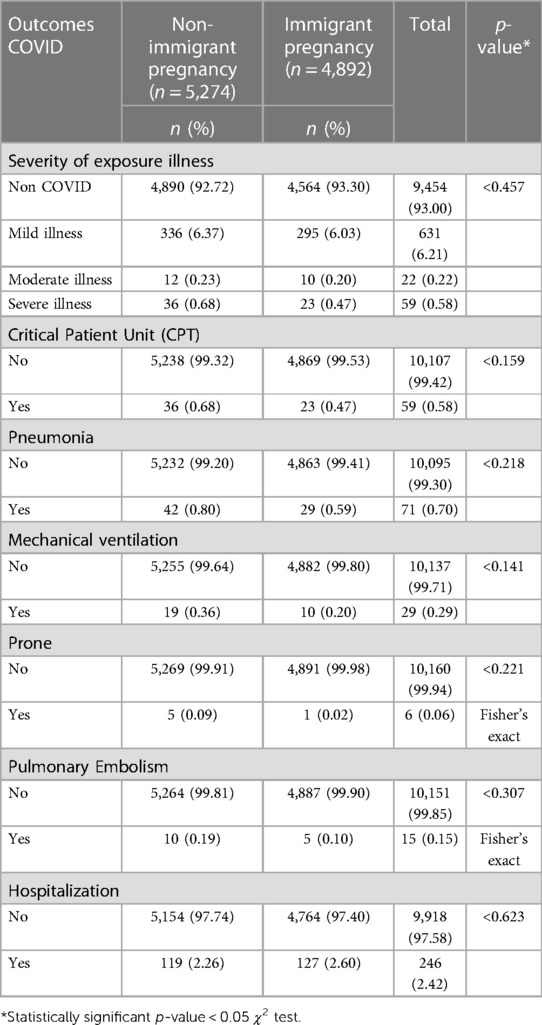
Table 3. Comparison of COVID clinical severity between non-immigrant and immigrant pregnant women. Hospital San José, Santiago of Chile. March 2020 to August 2022.
As shown in Figure 3, Haitians had the highest proportion of emergency c-section and preterm birth, but the lowest proportion of labor and delivery companion, postpartum attachment to newborn. On the other hand Venezuelans had the highest proportion of elective c-sections and less proportion of maternal care provision variables compared with non-immigrants (Figure 3).
In the pair comparison analysis shown in Table 4, Haitians had a higher risk of undergoing emergency c-section compared to non-immigrants (aRR = 1.61; 95% CI: 1.48–1.75). Venezuelans, had a higher risk of both planned/elective c-section and emergency c-section compared to non-immigrants (aRR = 2.18; 95% CI: 1.81–2.63 and aRR = 1.50; 95% CI: 1.33–1.68, respectively). Women from other nationalities, exhibited a slightly higher risk of emergency c-section was reported but after adjusting by age and health insurance, the risk of emergency c-section disappeared (aRR = 1.09; 95% CI: 0.99–1.19). Both Haitians and Venezuelans had a significant higher risk of not having maternal care provision, however, Haitians had a higher risk of not receiving personalized childbirth care (aRR = 1.03; 95% CI: 1.00–1.05), not having a companion during labor and childbirth (aRR = 2.48; 95% CI: 2.24–2.75), not having postpartum attachment to newborns (aRR = 1.88; 95% CI: 1.73–2.05). Also Haitians has the highest risk of extreme preterm birth (<28 weeks, aRR = 2.09; 95% CI: 1.30–3.36) compared to non-immigrants. (Table 4).
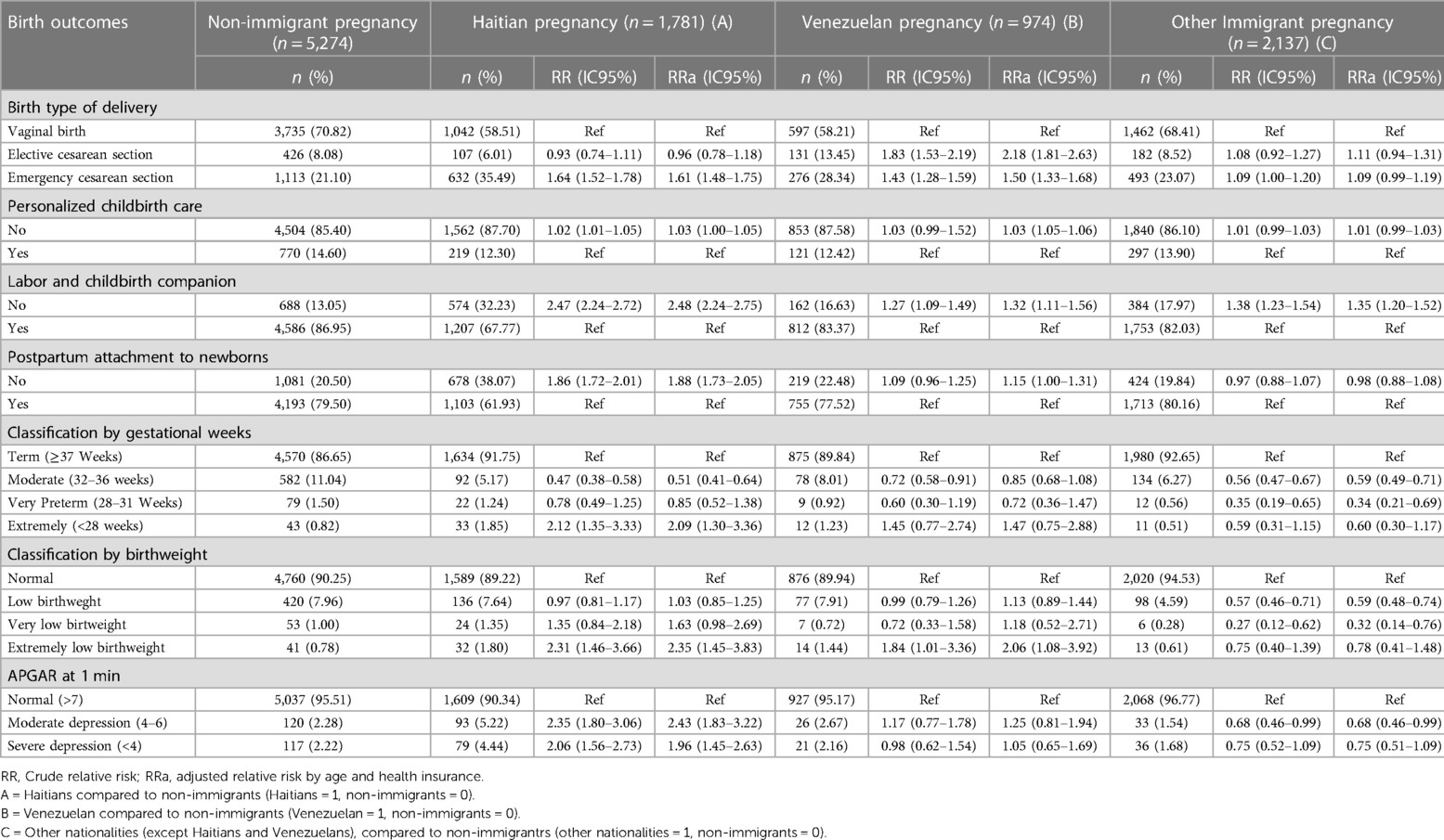
Table 4. Risk of c-section and other obstetric and perinatal outcomes in Haitian, Venezuelan, and other nationalities, compared to non-immigrant women. Log Binomial multivariable regression models.
4. Discussion
The present study reported significant differences in perinatal outcomes between immigrant and non-immigrant women. The main finding of this study is related to high rates of c-section in the entire population, that in immigrants it exceeds 40% of the total births, which is one of the highest rates reported in the world. Haitian women had the highest risk of emergency c-section and Venezuelan women the highest rate of elective c-section. Additionally, it found a higher risk of not having a companion during labor and not postpartum attachment with the newborn among mothers from Haiti.
Regarding biosociodemographic data, the results demonstrate that approximately half of the pregnant women attended at the San José Hospital were immigrants, most prevalent countries of origin were Haiti, Peru, and Venezuela. Significant differences were observed in various demographic and health variables between immigrant and non-immigrant women. These findings are consistent with previous studies that have examined the composition of the immigrant population in Chile (11–13). A study conducted by Veliz et al. supports the presence of a significant proportion of immigrants from the same countries mentioned. This validates and enhances the representativeness of the current study's sample (21).
We found that immigrant women received less personalized attention during labor and had a lower presence of companion at birth compared to non-immigrant women. Additionally, significant differences were observed in postpartum attachment with newborns, prematurity and birth weight. These findings are consistent with previous research that has addressed the unequal impact of the pandemic on the health of migrants and the exercising of their reproductive rights. International studies have reported challenges in establishing the mother-newborn emotional connection in immigrant women, which may be related to factors such as social support, communication barriers, and cultural adaptation. A publication from Fabi and Ludmir (17), suggests that immigrant women, in particular, have experienced difficulties asserting their reproductive rights due to the pandemic. Although the pandemic could have accentuated the differences between the immigrant and non-immigrant population, more studies are required to determine the effect of migration as a social determinant of inequities in childbirth care, independent of the health crisis.
Significant differences were found in the c-section rate. Although other studies have shown higher rates of c-section in immigrant women in different countries (10, 22, 23), Chile has been recognized for its high rates of c-section. Nevertheless, the disparity in cesarean section rates between immigrant and non-immigrant populations was not known. Although it is known that there are determining factors such as access to prenatal care, communication barriers and other social determinants of health, it is urgent to design more studies to elucidate the possible causes and establish new regulations that protect the reproductive rights of the immigrant population.
Significant differences were observed in the distribution of preterm births. Although immigrant women have a higher proportion of full-term births, they also have a higher proportion of extremely premature births. Haitians are the ones who exhibit the highest proportion of extreme prematurity. International studies have shown differences in the duration of pregnancy and prematurity in immigrant women, which may be influenced by socioeconomic, health and access to prenatal care factors (10, 17).
Although immigration has been associated with a higher risk of having COVID-19, in this study no differences were found regarding the prevalence of COVID-19 during pregnancy, or in the severity of the disease, admission to Intensive Care Unit, pneumonia, use of mechanical ventilation, prognosis, pulmonary thromboembolism, and hospitalization, between the immigrant and non-immigrant groups. However, these divergent results could be explained by the specific migratory conditions of the country since in Chile migration is a recent phenomenon and better perinatal maternal health indicators have been reported compared to the local population (12, 13). Furthermore, the importance of considering other contextual and sociocultural factors that could influence the observed outcomes is highlighted (7, 24–28).
The main limitations of this study includes a limited ability to extrapolate the results to other populations. Also, it should be noted that there might be a slight subestimation of the parameters, because as asymptomatic pregnant women were not tested within the first two months of the pandemic. Another limitation of the study is the used of secondary data, some relevant variables were not measured, such as maternal education, length of residence in the country, and the presence of pathologies that could influence the results. More studies should be conducted to address the effect of preeclampsia, and gestational diabetes and its impact on obstetric and perinatal outcomes.
5. Conclusion
These findings have significant implications for the perinatal care of the immigrant population, indicating that immigrant women may encounter additional barriers in terms of personalized care during childbirth, access to a companion, type of delivery, and establishing an emotional bond with their newborns. These differences could influence perinatal outcomes and underscore the need to address disparities in perinatal care between non-immigrant and immigrant pregnancy groups.
Furthermore, it is essential to consider other contextual and sociocultural factors that may be influencing the observed outcomes. These results should encourage additional investigation into the causes for these disparities in care and the development of targeted programs to enhance maternal health and obstetric care for immigrant women, not just in Chile but also in other nations, considering the specific stage of obstetric transition they are in.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
This study was approved by the Comité de ética del Servicio de Salud Metropolitano Norte and conducted in accordance with local legislation and institutional requirements. Written informed consent was not required from participants or their legal guardians/next of kin because the study used information from clinical records without sensitive data (secondary data).
Author contributions
MC: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Software, Visualization, Writing – original draft, Writing – review & editing. NS: Conceptualization, Data curation, Investigation, Visualization, Writing – review & editing. JO: Conceptualization, Writing – review & editing. RV: Data curation, Formal Analysis, Methodology, Software, Supervision, Writing – review & editing. SV: Supervision, Visualization, Writing – review & editing. CN: Conceptualization, Visualization, Writing – review & editing. LV: Visualization, Writing – review & editing. LV: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
The realization of this project was funded by the Health Research Projects of the Faculty of Medicine at the University of Chile, number CE: 400286.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Instituto Nacional de Estadísticas de Chile (INE). Demografía. INE (2021). Available at: https://serviciomigraciones.cl/estudios-migratorios/estimaciones-de-extranjeros/ (Accessed July 20, 2023).
2. Instituto Nacional de Estadísticas de Chile (INE). Anuario de estadísticas Vitales: Período de información: 2019. Santiago, Chile: INE (2019). Available at: https://www.ine.cl/docs/default-source/nacimientos-matrimonios-y-defunciones/publicaciones-y-anuarios/anuarios-de-estadísticas-vitales/anuario-de-estadísticas-vitales-2019.pdf?sfvrsn=97729b7b_5 (Accessed July 20, 2023).
3. Poncet L, Panjo H, Andro A, Ringa V. Caesarean delivery in a migration context: the role of prior delivery in the host country. Sex Reprod Heal Matters. (2020) 28(1):373–83. doi: 10.1080/26410397.2020.1763576
4. Gagnon AJ, Merry L, Haase K. Predictors of emergency cesarean delivery among international migrant women in Canada. Int J Gynecol Obstet. (2013) 121(3):270–4. doi: 10.1016/j.ijgo.2012.12.017
5. Boerma T, Ronsmans C, Melesse DY, Barros AJD, Barros FC, Juan L, et al. Global epidemiology of use of and disparities in caesarean sections. Lancet. (2018) 392(10155):1341–8.doi: 10.1016/S0140-6736(18)31928-7
6. Abdulla F, Hossain MM, Rahman MM, Rahman MS, Rahman A. Risk factors of caesarean deliveries in urban–rural areas of Bangladesh. Front Reprod Heal. (2023) 5:1–12. doi: 10.3389/frph.2023.1101400
7. Souza J, Tunçalp Ö, Vogel J, Bohren M, Widmer M, Oladapo O, et al. Obstetric transition: the pathway towards ending preventable maternal deaths. BJOG An Int J Obstet Gynaecol. (2014) 121(1):1–4. doi: 10.1111/1471-0528.12735
8. Departamento de Estadística e Información de Salud (DEIS). Natalidad. Ministerio de Salud de Chile (2023). Available at: https://deis.minsal.cl/wp-content/uploads/2020/07/Reporteria_Programa_Mujer.html (Accessed July 24, 2023).
9. Araya Bannout MA, Padilla O, Garmendia ML, Atalah E, Uauy R. Obesidad en mujeres chilenas en edad fértil. Rev Med Chil. (2014) 142(11):1440–8. doi: 10.4067/S0034-98872014001100011
10. Carroza Escobar MB, Ortiz Contreras J, Bertoglia MP, Araya Bannout M. Pregestational obesity, maternal morbidity and risk of caesarean delivery in a country in an advanced stage of obstetric transition. Obes Res Clin Pract. (2020) 15:73–7. doi: 10.1016/j.orcp.2020.12.006
11. Ortiz Contreras J, Carroza Escobar MB, Quiroz-Carreño J, Díaz Navarrete M, Araya Bannout M. Resultados materno-perinatales de gestantes peruanas en Chile: exploración del efecto del migrante sano. Rev Peru Med Exp Salud Publica. (2020) 37(4):654–61. doi: 10.17843/rpmesp.2020.374.6098
12. Ortiz J, Quiroz J, Carroza MB, Díaz M. Condición migratoria y salud materno-perinatal en mujeres inmigrantes en Chile. Salud, Bienestar y Soc. (2021) 7(1):16–28. doi: 10.18848/2474-5219/CGP/v07i01/17-27
13. Ortiz J, Diaz M, Araya BM, Quiroz J, Carroza B, Pavez J, et al. Comparison of bio-sociodemographic, obstetric and perinatal characteristics among immigrant and native women in the metropolitan region in Chile. Midwifery. (2019) 75:72–9. doi: 10.1016/j.midw.2019.04.008
14. Wei SQ, Bilodeau-Bertrand M, Liu S, Auger N. The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. Can Med Assoc J. (2021) 193(16):E540–8. doi: 10.1503/cmaj.202604
15. Twanow J-DE, McCabe C, Ream MA. The COVID-19 pandemic and pregnancy: impact on mothers and newborns. Semin Pediatr Neurol. (2022) 42:100977. doi: 10.1016/j.spen.2022.100977
16. Haye MT, Cartes G, Gutiérrez J, Ahumada P, Krause B, Merialdi M, et al. Maternal and perinatal outcomes in pregnant women with confirmed severe and mild COVID-19 at one large maternity hospital in Chile. J Matern Neonatal Med. (2021) 35:1–6. doi: 10.1080/14767058.2021.1902498
17. Fabi RE, Ludmir J. Pregnancy, pandemics, and public health policy: the disparate impact of COVID-19 on pregnant immigrants. Women’s Heal Issues. (2021) 31(3):195–7. doi: 10.1016/j.whi.2020.12.001
18. MINSAL. Política de salud de migrantes internacionales. (2018). Available at: https://www.minsal.cl/wp-content/uploads/2015/09/2018.01.22.POLITICA-DE-SALUD-DE-MIGRANTES.pdf (Accessed August 18, 2023).
19. Eri TS, Blix E, Downe S, Vedeler C, Nilsen ABV. Giving birth and becoming a parent during the COVID-19 pandemic: a qualitative analysis of 806 women’s responses to three open-ended questions in an online survey. Midwifery. (2022) 109:103321. doi: 10.1016/j.midw.2022.103321
20. Hospital San José. Servicio de Salud Metropolitano Norte. Protocolo de contacto piel a piel. Santiago, Chile (2016). p. 7.
21. Veliz F, Ponce MJ, Flores J, Haye MT, Rubio G, Gutiérrez J, et al. Nacimientos en Chile: ¿cuál ha sido el impacto de la última ola de madres migrantes? Rev Médica Clínica Las Condes. (2023) 34(1):64–70. doi: 10.1016/j.rmclc.2023.01.008
22. Ferrazzi E, Frigerio L, Savasi V, Vergani P, Prefumo F, Barresi S, et al. Vaginal delivery in SARS-CoV-2 infected pregnant women in northern Italy: a retrospective analysis. BJOG An Int J Obstet Gynaecol. (2020) 24:1–6. doi: 10.1111/1471-0528.16278
23. Belizan JM, Althabe F, Barros FC, Alexander S. Rates and implications of caesarean sections in Latin America: ecological study. Br Med J. (1999) 319(7222):1397–400. doi: 10.1136/bmj.319.7222.1397
24. Chaves SdC, Cecatti JG, Carroli G, Lumbiganon P, Hogue CJ, Mori R, et al. Obstetric transition in the world health organization multicountry survey on maternal and newborn health: exploring pathways for maternal mortality reduction. Rev Panam Salud Publica. (2015) 37(4–5):203–10. Available at: https://www.ncbi.nlm.nih.gov/pubmed/2620818626208186
25. Timircan M, Bratosin F, Vidican I, Suciu O, Tirnea L, Avram V, et al. Exploring pregnancy outcomes associated with SARS-CoV-2 infection. Medicina (B Aires). (2021) 57(8):796. doi: 10.3390/medicina57080796
26. Roberton T, Carter ED, Chou VB, Stegmuller AR, Jackson BD, Tam Y, et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Heal. (2020) 8(7):e901–8. doi: 10.1016/S2214-109X(20)30229-1
27. Karasek D, Baer RJ, McLemore MR, Bell AJ, Blebu BE, Casey JA, et al. The association of COVID-19 infection in pregnancy with preterm birth: a retrospective cohort study in California. Lancet Reg Heal Am. (2021) 2:100027. doi: 10.1016/j.lana.2021.100027
Keywords: COVID, immigrant women, cesarean sections, maternal care, pregnancy, perinatal outcomes
Citation: Carroza Escobar MB, Silva N, Ortíz-Contreras J, Villegas R, Vargas SL, Núñez C, Vergara Maldonado LF and Villanueva LP (2023) Immigration and C-sections incidence: Maternal care and perinatal outcomes in the context of the pandemic in Chile. Front. Glob. Womens Health 4:1267156. doi: 10.3389/fgwh.2023.1267156
Received: 26 July 2023; Accepted: 9 October 2023;
Published: 22 November 2023.
Edited by:
Ramon Escuriet, Blanquerna Ramon Llull University, SpainReviewed by:
Laura Rodellar Merino, University General Hospital of Catalonia, SpainFrancesca Palestra, World Health Organization, Switzerland
© 2023 Carroza Escobar, Silva, Ortíz-Contreras, Villegas, Vargas, Núñez, Vergara Maldonado and Villanueva. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Loreto Paola Villanueva loreto.villanueva@uchile.cl
 María Begoña Carroza Escobar
María Begoña Carroza Escobar Nicole Silva3
Nicole Silva3  Sergio L. Vargas
Sergio L. Vargas Loreto Paola Villanueva
Loreto Paola Villanueva