The unseen patient: competing priorities between patients and providers when cannabis is used in pregnancy, a qualitative study
- Department of Population and Public Health Sciences, Keck School of Medicine, University of Southern California, Los Angeles, CA, United States
Objectives: This study aimed to explore competing priorities when cannabis is used during pregnancy from the perspective of providers and Black and Latina people. Maternal cannabis use is increasingly common, but patients and providers alike struggle to navigate it.
Methods: This pilot used qualitative, constructivist ground theory methods to conduct semi-structured, remote interviews between 16 November 2021, and 7 February 2022 with 7 Black and Latina people who used cannabis during pregnancy, and 10 providers between 15 March 2022, and 6 April 2022, all of who were in Southern California, U.S.
Results: We identified three main findings: (1) Providers reported barriers to caregiving and relationship building with patients due to maternal cannabis use stigma, (2) Providers prioritized the fetus despite patients’ current health system challenges that drove cannabis use, and (3) Both patients and providers engaged in personal research beyond the healthcare system to better understand maternal cannabis use.
Discussion: Our findings indicate that challenges exist between people who use cannabis during pregnancy and providers. Both groups need accurate, sociocultural sensitive information about maternal cannabis use via a harm reduction lens.
Introduction
Cannabis is the most common substance used in pregnancy (1). As early as the 7th century BCE, cannabis has been used as a medicinal treatment for ailments specific to reproductive and gynecological events (2), and people today continue to use it for pregnancy-related symptoms such as nausea, pain, and mood changes (3–6). Pregnant and postpartum individuals are increasingly using cannabis, especially in states where it is legalized (7–9). In recent years, estimated rates of use are up to 8% in this group and may even be higher due to lack of self-report data caused by fear of stigma and legal consequences (10–12, 5, 6, 13, 14).
The American College of Obstetricians and Gynecologists (ACOG) and the American Academy of Pediatrics (AAP) (15) advise against cannabis use during pregnancy because there is convincing evidence from observational studies that people who use cannabis during pregnancy are more likely to give birth to babies that are small for their gestational age and have a low birth weight (16). Specific cannabinoids present in cannabis can be effective for multiple sclerosis and chronic pain treatment (16) but it is likely that in utero exposure to cannabis may produce negative health effects (17, 18). However, there are limitations to the conclusiveness of the current body of evidence (19). Limitations of current evidence include sample size and generalizability, self-reported data, lack of data on timing and dosing of cannabis ingestion, as well as a lack of focus on social environmental contexts influencing use of cannabis during pregnancy (20, 21). The extant data has identified that more research is needed on maternal cannabis use to optimize public health promotion and intervention development (22–24).
Pregnant individuals who are considering using cannabis report perceptions of insufficient data as well as not seeing providers as sources of information or care on this topic (24, 25). On the other hand, providers often describe a lack of confidence in their own knowledge of cannabis and the available medical protocol regarding maternal cannabis use, leading to issues with screening and counselling (5, 26–29). ACOG and other groups recommend universal screening practices for substance use in pregnancy, but screening is often non-standardized and is fraught with racial disparities (30). Patients of color are also the most likely to face punitive consequences for disclosures of maternal cannabis use such as Child Protective Services (CPS) involvement or stigmatized care, prompting criticism of screening practices (31, 32).
The paucity of reliable, high-quality data on the long-term effects of maternal cannabis use coupled with conflicting stances in healthcare settings can lead to potential confusion among both patients and practitioners (20, 25, 29). While more data is emerging, little is understood about how individuals navigate care settings while using cannabis during pregnancy or discussing maternal cannabis usage with their providers. Patients and providers alike often do not know what information to consult, apply, or trust when making an informed decision about cannabis use during pregnancy. This study aimed to explore competing priorities when cannabis is used during pregnancy from the perspective of providers and Black and Latina people who use or used cannabis during pregnancy. We explore the potential for ensuing inequities, such as selective substance use screening practices, that lead to disparities in care among Black and Latina pregnant people who use cannabis.
Methods
Study design—constructivist grounded theory
We conducted qualitative interviews with maternal healthcare providers as well as people who use cannabis during pregnancy, an approach that has been documented in our other studies (29, 33). The research team consisted of advanced public health students (RMN, SSG), research staff (EEG), faculty co-investigators (GFD, CVB, TMB), and a faculty member (RCC) acting as the Principal Investigator of the study. We reviewed COREQ (consolidated criteria for reporting qualitative research), a validated 32-item checklist for qualitative reporting throughout the study to document important aspects of our research team, methodology, findings, and analysis (Supplementary Table S7: COREQ checklist) (34, 35).
We conducted a phenomenological study using constructivist grounded theory that aimed to understand the perspectives of two groups who have experienced a shared phenomenon, respectively: maternal health providers who care for patients who use cannabis during pregnancy and non-Hispanic Black and Latina people who used cannabis during pregnancy (36, 37).
Selection of participants—sampling and recruitment strategies
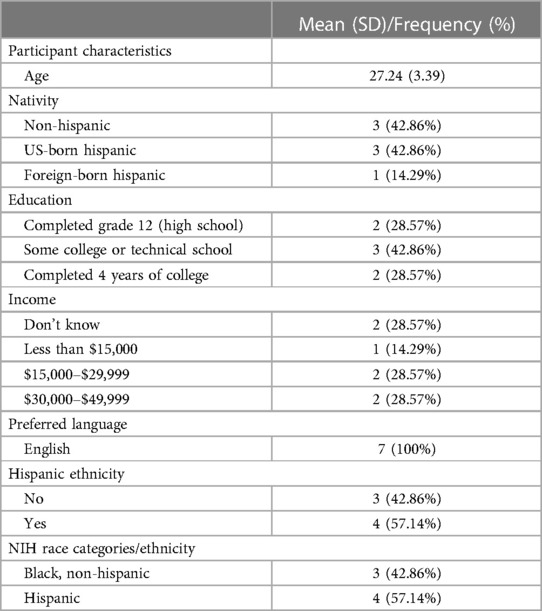
We used theoretical sampling based on grounded theory methodology (38, 39). This study is part of a larger project focused on patient and provider experiences regarding maternal cannabis use (40). We recruited patients from the Maternal and Developmental Risks from Environmental and Social Stressors (MADRES) cohort study who enrolled pregnant persons from three locations that predominantly serve patients with Medi-Cal, a California Medicaid health program that directly pays for medical services for people with limited income through federal and state taxes (40, 41). The study coordinator contacted patients from the larger MADRES cohort who were identified as using cannabis during pregnancy through medical record abstraction; had given birth in the last 0–2 years; were 21 years or older; and fluent in English or Spanish (Table 1). We recruited maternal health providers (e.g., physicians, doulas, midwives) via selective sampling using a convenience sample and snowball approach to reach practitioners in safety net health settings in Southern California who had experience caring for people who use cannabis during pregnancy within the past year (Table 2). This type of non-random sampling was based on team discussions about selecting participants that would provide insightful information regarding the research question (42, 43). Potential participants completed a HIPAA-compliant REDCap survey to confirm eligibility, sign an e-consent form, and schedule an interview.
Data collection—semi-structured interviews
The semi-structured interview guides drew upon existing qualitative and quantitative literature (Supplementary Table S1: Interview guide 1, Supplementary Table S2: Interview guide 2) (27, 44–46). We piloted and adapted the questions within the research team. We revised the interview guides as the interviews progressed to refine questions and pursue areas identified as theoretically relevant. This was part of an iterative process aimed at generating richer responses from participants (39, 47).
The 60-min interviews occurred remotely via HIPAA-compliant Zoom™ video calls from 16 November 2021 to 7 February 2022 (patients, n = 7) or from 15 March 2022 to 6 April 2022 (providers, n = 10). Each interview was conducted by 1–3 research team members, with one individual leading the discussion and the others co-leading and taking analytical notes to inform analysis. We followed up on questions with open-ended inquiries about topics introduced by the participants. This non-directive, open-ended approach of qualitative interviewing encouraged participants to elaborate beyond the original scope of the interview guide and allowed for unanticipated perspectives (48). Further, the interview guide was iteratively revised based on topics introduced by participants to generate better insights in subsequent interviews (39). Throughout data collection, the theoretical sampling strategy guided responsiveness to emerging theory to identify important concepts and guide decisions about when data collection was complete (38, 39).
We sent audio recordings of interviews to an external transcriptionist who de-identified transcripts and then uploaded the files to a HIPAA-compliant One Drive for team analysis. The team made summaries of emerging ideas in transcripts after each interview was completed as part of the initial analysis. As data collection continued, emerging ideas aligned with previously observed phenomena, meaning that theoretical saturation was achieved (38, 47).
Data analysis—grounded theory
We used grounded theory methodology to generate a conceptual framework (theory or explanation) by analyzing and comparing data on experiences and discussion around an area of interest (maternal cannabis use) across the data (38). This method is best used to learn about social processes when little is known about a phenomenon (39). Once the final interview was completed, the team reviewed and categorized the summarized emerging subject areas in each transcript to develop codebooks for patient and provider datasets. The codebooks consisted of thematic categories with definitions and examples discussed and revised as a team. We then uploaded the transcripts into ATLAS.ti™ data software program, Mac Version 22.1.0, and inputted the codebooks, which were tested on one transcript from each dataset as a team and revised as needed, resulting in 16 thematic codes for each patient and provider dataset (Supplementary Table S3: Codebook 1, Supplementary Table S4: Codebook 2) for analysis (49). Then, two team members independently analyzed each transcript and assessed consistent code application to ensure intercoder reliability. Final memos were made to capture themes resulting from code overlap and to facilitate deeper discussions of the data. Final insights from this process developed into the three results as they pertain to codes and final memos related to patient-provider relationships, priorities, and access to information.
This was a phenomenological study which used constructivist grounded theory to generate results. Constructivist grounded theory is a methodology where themes are inductively generated from the data and we develop specific theories and constructs as they relate to each other, co-occur, and build upon each other to add contextual richness to our data. As such, this methodology does not necessitate results with equal numbers of each group of participants, comparison within groups, or quotes from all participants and is instead focused on demonstrating results that best represent our themes. We did not include quotes from certain providers (i.e., doulas and midwives) because the quotes chosen were the best representation of the themes presented in results. While using theoretical sampling, we reached theoretical saturation for both patient and provider cohorts indicating that our results rigorously reflect and evaluate both perspectives (38, 47).
Results
Result 1: providers reported barriers to caregiving and relationship building with patients due to stigma around maternal cannabis use
Most providers described the prevalence of judgement towards cannabis in medicine today. One provider recounted their appraisal of patient disclosures, noting that most patients won't disclose cannabis use to their provider in fear of judgement:
“[T]here's still a decent amount of judgment… medicine is historically and traditionally patriarchal and … dismissive … the remnants of that circulate still … [patients are] not going to tell their doctor they’re using cannabis … because we can occasionally be judgmental, or we have a history of being judgmental.” (Dakota, Physician—OB/GYN)
Providers further explained this judgmental history via discussion of enacted screening practices that cause patients who disclose cannabis use to face negative repercussions. They explained that provider views of cannabis use leading to other substances (i.e., the gateway theory) meant patients attempting to communicate openly with providers are not only judged but subjected to punitive treatment as well:
“[C]annabis is seen … as a gateway drug in our particular specialty [inpatient maternity nursing] … we see that as a risky behavior … it does feel a little punitive … because … the person who's not saying anything [disclosing cannabis use] gets a different treatment [lack of drug screening] … than somebody who's trying to be honest about what is actually occurring.” (Cameron, Women's Health Nurse)
One provider recounted socioeconomic differences in screening and care: at different care sites, lower-income patients were monitored for substances without any evidence of use, but higher-income ones were spared this surveillance. They detailed provider assumptions about patients' behavior and how that impacted which ones received more oversight:
“[I]n the private practice, it's definitely a bias among the other providers that women with money don't have these issues … when I was at the low-income clinic … they would just run a drug panel on everybody in every pregnancy. And people would get dinged for using weed. We wouldn't call social services or anything because it wasn't a reportable drug use, but then they would get tested in labor at the hospital … in private practice, the doctors just figure that ‘Oh, women with money know better [than to use cannabis in pregnancy], so they don't do it.’” (Avery, Nurse Midwife)
They detailed the judgement and lack of understanding exhibited by many providers towards pregnant patients who are using cannabis. They called for divesting from this thinking via examination of patient motivations for using cannabis:
“[A]mongst the nurses, they … thought that the patient was just a shitty person for exposing their baby to drugs, and not looking at it as this whole entire problem … ‘Well it's really not that bad, but you should know better. It's not a huge addiction, like methamphetamine or heroin is. Why can't you just stop?’… [providers] looked down on the women for using it, not asking why they were using it. ‘Cause that's how I use it. If you're using cannabis, why? Is it because you have anxiety, is it because you have stress, is it because you have nausea?” (Avery, Nurse Midwife)
Another participant described the patient stereotypes many providers hold and emphasized the importance of exposure to patients who use cannabis to combat them. Without the opportunity to directly challenge preconceived notions regarding patients' views on pregnancy and their baby, they anticipated that the judgement towards cannabis use in pregnancy would continue:
“[I]f you practice in a population where you're not exposed to patients who are using cannabis, it can be a lot easier to maintain stereotypes about what kind of patient uses cannabis. And that only a patient who doesn't care about themselves, or doesn't care about their pregnancy, would use drugs during pregnancy.” (Riley, Physician—OB/GYN)
Result 2: providers felt the need to prioritize the fetus and potential risks to it despite patients' current challenges within the health system that drove cannabis use
Patients and providers described a dissonance between their priorities as well as perceptions of risks and benefits of cannabis use. While patients wanted inclusion of their reasons for turning to cannabis in care conversations, providers expressed interest in following science that tends to focus on fetal outcomes rather than maternal ones. One provider detailed concern about the long-term impacts of prenatal cannabis use on fetal well-being and thus saw their role as using patient education to protect only the baby:
“[W]e have our unseen patient, which is our baby, that we're responsible for. The mom can be responsible for herself, but we [as inpatient maternity nurses] are responsible for that baby … It's not really for me to judge. It's really for me to educate [the mother]. And I follow the science. The science tells us that these babies can have problems [if they are exposed to cannabis prenatally].” (Cameron, Women's Health Nurse)
Yet, from the patient perspective, they felt “misjudged” by providers who prioritized potential risk of cannabis exposure to their fetus over the challenges they currently faced during pregnancy. One individual, who was using cannabis to deal with symptoms such as nausea and lack of appetite, shared difficulties with managing not only their pregnancy but also the perceptions of their providers as they explored the nuance of caring for self and baby in a health system with limited resources:
“They did give me the nausea pills, but they would make me throw up. So I didn't take those … they said they didn't have anything other than the pills … [People who use cannabis during pregnancy] get misjudged because they are … carrying another life. But you have to realize [what happens] … if they can't give to that life … [because] not all of the things [to manage pregnancy symptoms] that the doctor's office gives you works.” (Valeria, Patient)
Another participant expanded on what was lacking in their communication with providers as they trusted their own reasons for cannabis use. While their conversations were oriented towards the baby, this mother expressed a need to shift some focus to her own care and how to navigate that via harm reduction-based symptom management strategies:
“[Providers should] listen to their patients about why they use it while they're pregnant. I know they're concerned about the baby … but if it helps them in the first weeks of their pregnancy, as to morning sickness or they can't sleep … they should be allowed to use it at a certain point … give them a time limit or give them a deadline. Okay, when your morning sickness stops, don't use it.” (Emma, Patient)
Another provider described how mothers face punitive measures because of their cannabis use in pregnancy rather than being offered support. As providers decide from an individual standpoint to conduct precautionary screening and reporting of patients for using cannabis in pregnancy, they tie care to agencies that can potentially perpetuate harm. As a result, the relationship between patient and provider can be damaged:
“[Providers] will order drug screens, or will call DCFS, Department of Child and Family Services, if they're worried about somebody … cannabis use alone shouldn't trigger that. But it is kind of provider-dependent, whether they decide to order those tests or referrals. You're in this vulnerable situation … as a pregnant woman, where you're coming to a healthcare center, you're looking for care, and then some of the care, in this case, ordering additional drug screens, or calling in Child and Family Services (CPS) [due to cannabis use], isn't really aimed at helping the mom. It's potentially used against the mom, in terms of losing custody of the child. [I]t's … a betrayal of the provider/patient relationship.” (Riley, Physician—OB/GYN)
One provider similarly emphasized the support needed by patients and their role in this. Knowing why patients are turning to cannabis and counseling or providing resources specific to this shifts the focus to encompass both maternal and fetal needs:
“I think that recommendations … [are] less inclusive of the range of patient experiences. I find most recommendations … advise us to counsel patients to … stop all substances immediately. And there's not a lot of room for us to support patients in where they are in their life, and what that would mean to them if they stopped substance use, and how we could support them … I feel like definitely knowing and caring about patients who have some form of substance use really makes the difference in terms of how you look at it.” (Riley, Physician—OB/GYN)
Result 3: both patients and providers felt the need to seek out information to better understand maternal cannabis use
Both patients and providers detailed seeking out information about cannabis use during pregnancy on their own. Patients described feeling compelled to do their own research amidst acknowledgment that healthcare providers were not open to their cannabis use. Reliance on peer knowledge and social media were commonly described among participants seeking information:
“My home girls told me, ‘Hey, I used it. Don't trip, it's fine. I know the doctor will try to scare you, but my mom's done it.’ … It's mostly just [learning from] word of mouth from friends. I know a couple [of canna] doulas on IG. She shares a lot of info.” (Mia, Patient)
Another participant recounted turning to their social networks to discuss maternal cannabis use and how these conversations were centered around the mother's experience:
“[A] few of my friends have had kids, and they smoked throughout their pregnancy … they were like, ‘Yeah, I think everything in moderation, do it because of your pain, not to get high.’” (Ava, Patient)
Providers acknowledged seeking out information on maternal cannabis use because they felt there was limited data on the subject but did not trust the knowledge patients shared about cannabis. One healthcare provider noted the challenge of navigating conflicting information when discussing patients doing their own research on maternal cannabis use:
“I've definitely learned things from patients in other areas, but with cannabis use, I would say probably not as much, just because there's not a ton of data out there that's on strictly cannabis use … somebody will quote a study … so I've gone and searched for that. But then at the same time, there's another study that says [the opposite] … point me into directions and I'll look it up, but it hasn't really changed anything.” (Avery, Nurse Midwife)
Another provider acknowledged that healthcare settings could take advantage of patients' drive to educate themselves and their social circles via peer-to-peer education programs, harnessing the positives of patients' desires and improving collective well-being:
“[T]hat'd be a big opportunity for our hospital as a whole to better connect with our community, is to empower them more to be leaders in the community and relay information that we give them to their peers and help them feel empowered that by improving their own health, they're also improving the health of their community as a whole.” (Taylor, Physician—OB/GYN)
Discussion
Our findings showcase consequences related to cannabis use disclosure perpetuated by providers such as institutionalized stigma and structural violence (50), dissociation between prioritizing baby vs. pregnant patient when cannabis use is disclosed, and patient and provider perceptions of lacking information.
Structural violence, a conceptualization of social injustice, refers to the position of potential harm that individuals are put in due to inequities within large-scale forces; Social structures within economic, cultural, medical, and legal domains are embedded with inequities (i.e., race or class-based discrimination) which prevent the fulfillment of optimal health and well-being (50–54). This is a structural issue as these experiences are situated within social structures and it is violent because it causes harm. While healthcare providers often lack training and education on these structural forces, there is a need for providers to have a broader understanding of how health behaviors and outcomes are situated within the social context of the patient's lived experience (19, 45, 54). Our findings reinforce this need as providers in our sample lacked awareness of structural consequences that pregnant patients who use cannabis may face. Our data demonstrated that severe medicolegal consequences, ranging from drug screenings to CPS involvement, awaited patients who disclosed their cannabis use to their providers. Open and honest communication within the provider-patient relationship was disincentivized, whereas defensive communication was protective for the patient. These findings call attention to institutionalized stigma in medicine by subjecting patients seeking care at low-income clinics to increased surveillance via procedures such as drug screenings (55–58). This data demonstrates manifestations of structural violence as these structural inequities can result in relational tension between patients and providers as well as drastic consequences for patients such as family separation (50).
In our study, providers described prioritizing empirical data over patient lived experience when it comes to maternal cannabis use. Our findings indicate that providers rely on maternal cannabis use data which focuses largely or exclusively on fetal outcomes. Participants reported how patient-centered care practices including shared decision-making by factoring the needs of pregnant people and their reasons cannabis use were absent. We observed a chasm in the provision of patient-centered care when it comes to maternal cannabis use due to a transition to the fetus being the patient and a dissociation from the pregnant person as a patient as well. Providers saw themselves as protectors of fetal health, rather than both maternal and fetal health, with the underlying assumption that pregnant individuals were incapable of this role due to their cannabis use. This led to individuals feeling deprioritized in their provider-patient relationship. In response, pregnant patients who are protecting themselves against ambiguous and far-reaching structural consequences (e.g., CPS involvement) often will not disclose cannabis use to providers and face consequences when they do (33). Future perinatal cannabis research and educational interventions should expand the focus to encompass maternal needs as well as social and environmental experiences to keep pregnant individuals engaged.
Both patients and providers reported seeking out information on maternal cannabis use due to their lack of personal knowledge on the topic. Our findings are consistent with prior research, which shows that providers often do not adequately counsel patients following disclosure of maternal cannabis use (59). When providers do acknowledge use, it is often a punitive approach due to perceptions of unclear evidence (32, 60). While the body of research is growing and there may be fetal impacts due to use, there appears to be no benefits to surveillance measures such as drug testing (61). Further, data showing little to no fetal harm from cannabis exposure may counter provider concerns (32).
Future empirical studies must consider social and structural determinants of health when looking at neonatal outcomes from maternal cannabis use, as higher screening occurs among pregnant patients with lower socioeconomic resources.
Our research echoes previous findings that pregnant patients are using cannabis medicinally to manage pregnancy symptoms such as nausea (59). In the absence of satisfactory provider counseling, patients relied on peers for information and advice, which reiterates previous findings that individuals value information online to learn about cannabis use during pregnancy (62, 63). Patients perceived that the maternal experience of using cannabis was pushed to the margins of the general research body, with their questions and drivers of use ignored by providers. This, in turn, led to them to conduct their own personal research. As patients pursue their own research, they can frame questions around the maternal experience, highlighting ways they may not be able to in the provider's office. However, when providers lack information on the maternal experience and utilize punitive care following cannabis disclosure, it may disincentivize disclosure and pave the way for dismissal of the research or overemphasis of peer knowledge (3, 44, 64).
There is an urgent need for multi-level harm reduction-based interventions as evidence in this area is generated. This includes: (1) provider-based interventions to highlight how harm reduction can be implemented in one-on-one patient-provider appointments, education around why patients are using cannabis, and how providers can reduce structural inequities such as increased screening among low-income patients; (2) institutional interventions, such as clear guidelines for how to approach pregnant patients who disclose cannabis use, and pathways that prioritize the patient rather than punish; and (3) peer-to-peer programming with an emphasis on health literacy, media literacy, and social media literacy to enable better navigation and comprehension of cannabis content in and outside of healthcare settings (65–70).
Providers described a missed intervention point for maternal cannabis use caregiving training in their education. Providers' maternal cannabis use assumptions can be intervened upon with direct patient care during didactic and experiential learning by working with patients using cannabis to understand their lived and living experiences. This harm reduction training via an educational praxis is vital to reducing stigma, implicit bias, and moralistic judgement. Prior studies similarly show stigma towards substance use disorders and demonstrate efficacy of stigma-reducing interventions via direct exposure or didactic training (71).
Additionally, providing clear guidelines around mandatory reporting is imperative. ACOG states that, “[s]eeking obstetric–gynecologic care should not expose a woman to criminal or civil penalties for marijuana use,” which requires clear guidelines for how to handle cannabis disclosure during prenatal care (72). The current ambiguity in guidelines leaves room for provider stigma, knowledge gaps, and individual case-by-case evaluations of cannabis screening which works against structurally vulnerable pregnant patients (29). Patients must know that when they disclose their cannabis use, they have structural protection from medicolegal consequences.
Providers face difficulties as they must remain the ultimate authority in care amidst conflicting information, but including community programming could help to ease that burden. Providers typically hold a position of power in caregiving settings as they counsel patients and set their care plan including protocols for drug screening and CPS involvement. Despite this, they are not patients' only source of information and must educate within the context of social media and peer discussions (73, 74). Engaging patients and providers via structured peer-to-peer programming initiatives can educate both groups and potentially mitigate the likelihood of providers perpetrating harm by creating a negative care atmosphere or reporting to CPS resulting in loss of parental custody. Both groups need accurate, sociocultural sensitive information using a harm reduction lens to acknowledge the realities of drivers for maternal cannabis use and avoid perpetuating further damage.
Limitations
This research has limitations. First, our findings may not be generalizable as we interviewed patients and providers who are based in California where cannabis is medically and recreationally legal. Second, maternal health stakeholders were not randomly selected and may not be representative of all providers, especially because of the limited maternal health roles they held. Third, though providers all cared for BIPOC patients, they had limited insights specific to this group as well as the role of their own identities outside of it, content we wish to explore in future projects focusing more on race and racism (75, 76). Fourth, despite patients giving informed consent to information from their medical records, some potential participants were surprised to be contacted for a cannabis study and refuted any use. Because younger, less educated, publicly insured, patients of color are more likely to be screened for substance use during prenatal care visits and face ensuing sociolegal ramifications, future studies would benefit from using self-reporting of cannabis use, despite greater identification of cannabis use via urine toxicology testing vs. self-report (30, 77). Fifth, this study may overrepresent people confident in their cannabis decision making and disclosure to providers about using during pregnancy.
Despite these limitations, this study includes a qualitative exploratory approach to understand perspectives, behaviors, motivations, and challenges on a taboo public health subject for both pregnant patients and maternal health providers. This supports ongoing research to better understand the stigma and barriers faced by those using cannabis while engaging in perinatal care. Further, our preliminary findings support future interventions that aim to inform providers and patients, protect patients from discrimination and criminalization during pregnancy, and preserve continuity of care.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by University of Southern California Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
EG: Data curation, Formal Analysis, Investigation, Project administration, Software, Writing – original draft, Writing – review & editing. SG: Writing – review & editing. RN: Writing – review & editing. CB: Writing – review & editing. TB: Writing – review & editing. GD: Writing – review & editing. RC: Conceptualization, Funding acquisition, Investigation, Methodology, Supervision, Writing – review & editing.
Funding
The authors declare financial support was received for the research, authorship, and/or publication of this article.
This study was funded by the University of Southern California (USC) Maternal and Developmental Risks from Environmental and Social Stressors (MADRES) Center for Environmental Health Disparities' Pilot Projects Program (2021), which is funded by the U.S. National Institute of Health, National Institute on Minority Health and Health Disparities (grant no. NIH-NIMHD P50MD015705). RC Ceasar is supported by USC Institute of Preventive Research, USC Institute of Addiction Science, and University of Arizona PRIDE pilot grant (grant no. R25-HL 126140).
Conflict of interest
RC Ceasar conducted research analysis and report writing for the Women in Cannabis. Study in 2020 as a research consultant for Culture of Health & Tech Consulting.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2024.1355375/full#supplementary-material
Supplementary Table 1
Study participant characteristics - pregnant patients.
Supplementary Table 2
Study participant characteristics - maternal healthcare providers.
Supplementary Data Sheet 1
COREQ checklist.
Supplementary Data Sheet 2
Interview guide - pregnant patients.
Supplementary Data Sheet 3
Interview guide - maternal healthcare stakeholders.
Supplementary Data Sheet 4
Codebook - people who use cannabis during pregnancy.
Supplementary Data Sheet 5
Codebook - maternal healthcare stakeholder.
References
1. SAMHSA. Marijuana During Pregnancy—Know the Risks | SAMHSA [WWW Document]. (2019). Available online at: https://www.samhsa.gov/marijuana/marijuana-pregnancy (Accessed February 13, 2024).
2. Russo E. Cannabis treatments in obstetrics and gynecology: a historical review. J Cannabis Ther. (2002) 2(3–4):5–35. doi: 10.1300/J175v02n03_02
3. Chang JC, Tarr JA, Holland CL, De Genna NM, Richardson GA, Rodriguez KL, et al. Beliefs and attitudes regarding prenatal marijuana use: perspectives of pregnant women who report use. Drug Alcohol Depend. (2019) 196:14–20. doi: 10.1016/j.drugalcdep.2018.11.028
4. Young-Wolff KC, Sarovar V, Tucker L-Y, Avalos LA, Conway A, Armstrong MA, et al. Association of nausea and vomiting in pregnancy with prenatal marijuana use. JAMA Intern Med. (2018) 178:1423. doi: 10.1001/jamainternmed.2018.3581
5. Young-Wolff KC, Gali K, Sarovar V, Rutledge GW, Prochaska JJ. Women’s questions about perinatal cannabis use and health care providers’ responses. J Womens Health. (2020a) 29:919–26. doi: 10.1089/jwh.2019.8112
6. Young-Wolff KC, Sarovar V, Tucker L-Y, Goler N, Conway A, Weisner C, et al. Validity of self-reported cannabis use among pregnant females in Northern California. J Addict Med. (2020b) 14:287. doi: 10.1097/ADM.0000000000000581
7. Gnofam M, Allshouse AA, Stickrath EH, Metz TD. Impact of marijuana legalization on prevalence of maternal marijuana use and perinatal outcomes. Am J Perinatol. (2020) 37:59–65. doi: 10.1055/s-0039-1696719
8. Skelton KR, Hecht AA, Benjamin-Neelon SE. Recreational cannabis legalization in the US and maternal use during the preconception, prenatal, and postpartum periods. Int J Environ Res Public Health. (2020) 17:909. doi: 10.3390/ijerph17030909
9. Skelton KR, Hecht AA, Benjamin-Neelon SE. Association of recreational cannabis legalization with maternal cannabis use in the preconception, prenatal, and postpartum periods. JAMA Netw Open. (2021) 4:e210138. doi: 10.1001/jamanetworkopen.2021.0138
10. Keyhani S, Steigerwald S, Ishida J, Vali M, Cerdá M, Hasin D, et al. Risks and benefits of marijuana use: a national survey of U. S. adults. Ann Intern Med. (2018) 169:282–90. doi: 10.7326/M18-0810
11. Volkow ND, Han B, Compton WM, McCance-Katz EF. Self-reported medical and nonmedical cannabis use among pregnant women in the United States. JAMA. (2019) 322:167. doi: 10.1001/jama.2019.7982
12. Roncero C, Valriberas-Herrero I, Mezzatesta-Gava M, Villegas JL, Aguilar L, Grau-López L. Cannabis use during pregnancy and its relationship with fetal developmental outcomes and psychiatric disorders. A systematic review. Reprod Health. (2020) 17:25. doi: 10.1186/s12978-020-0880-9
13. Young-Wolff KC, Ray GT, Alexeeff SE, Adams SR, Does MB, Ansley D, et al. Rates of prenatal cannabis use among pregnant women before and during the COVID-19 pandemic. JAMA. (2021) 326:1745. doi: 10.1001/jama.2021.16328
14. Young-Wolff KC, Sarovar V, Tucker L-Y, Ansley D, Goler N, Conway A, et al. Trends in cannabis polysubstance use during early pregnancy among patients in a large health care system in northern California. JAMA Netw Open. (2022) 5:e2215418. doi: 10.1001/jamanetworkopen.2022.15418
15. Ryan SA, Ammerman SD, O’Connor ME, Committee On Substance Use And Prevention, Section On Breastfeeding, Gonzalez L, Patrick SW, et al. Marijuana use during pregnancy and breastfeeding: implications for neonatal and childhood outcomes. Pediatrics. (2018) 142:e20181889. doi: 10.1542/peds.2018-1889
16. Solmi M, De Toffol M, Kim JY, Choi MJ, Stubbs B, Thompson T, et al. Balancing risks and benefits of cannabis use: umbrella review of meta-analyses of randomised controlled trials and observational studies. Br Med J. (2023) 382:e072348. doi: 10.1136/bmj-2022-072348
17. Metz TD, Allshouse AA, Hogue CJ, Goldenberg RL, Dudley DJ, Varner MW, et al. Maternal marijuana use, adverse pregnancy outcomes, and neonatal morbidity. Am J Obstet Gynecol. (2017) 217(4):478.e1–e8. doi: 10.1016/j.ajog.2017.05.050
18. Metz TD, Allshouse AA, McMillin GA, Greene T, Chung JH, Grobman WA, et al. Cannabis exposure and adverse pregnancy outcomes related to placental function. JAMA. (2023) 330:2191. doi: 10.1001/jama.2023.21146
19. Sujan AC, Pal A, Avalos LA, Young-Wolff KC. A systematic review of in utero cannabis exposure and risk for structural birth defects. Front Pediatr. (2023) 11:1–11. doi: 10.3389/fped.2023.1149401
20. Sujan AC, Young-Wolff KC, Avalos LA. In-utero cannabis exposure and long-term psychiatric and neurodevelopmental outcomes: the limitations of existing literature and recommendations for future research. Birth Defects Research. (2022a) 114:689–713. doi: 10.1002/bdr2.2060
21. Ceasar RC, Terplan M, Rewegan A. Cannabis use and perinatal health. JAMA. (2024) 331:256–7. doi: 10.1001/jama.2023.23236
22. Silverstein M, Howell EA, Zuckerman B. Cannabis use in pregnancy: a tale of 2 concerns. JAMA. (2019) 322(2):121–2. doi: 10.1001/jama.2019.8860
23. Pike CK, Sofis MJ, Budney AJ. Correlates of continued cannabis use during pregnancy. Drug Alcohol Depend. (2021) 227:108939. doi: 10.1016/j.drugalcdep.2021.108939
24. Taneja S, Panday J, Popoola A, Greyson D, McDonald SD, Patel T, et al. Making informed choices about cannabis use during pregnancy and lactation: a qualitative study of information use. Birth. (2023) 50:504–12. doi: 10.1111/birt.12668
25. Foti TR, Green A, Altschuler A, Iturralde E, Does MB, Jackson-Morris M, et al. Patient perceptions of prenatal cannabis use and implications for clinicians. Obstet Gynecol. (2023) 142:1153. doi: 10.1097/AOG.0000000000005295
26. McKenzie LB, Keim SA, Klebanoff MA. Risk perceptions about cannabis use and receipt of health-related information during pregnancy. Am J Health Promot. (2022) 36:1316–25. doi: 10.1177/08901171221099496
27. Panday J, Taneja S, Popoola A, Pack R, Greyson D, McDonald SD, et al. Clinician responses to cannabis use during pregnancy and lactation: a systematic review and integrative mixed-methods research synthesis. Fam Pract. (2022) 39:504–14. doi: 10.1093/fampra/cmab146
28. Kitsantas P, Pursell SR. Are health care providers caring for pregnant and postpartum women ready to confront the perinatal cannabis use challenge? Am J Perinatol. (2023) 11. doi: 10.1055/s-0043-1777669
29. Ceasar RC, Gould E, Stal J, Laughter J, Tran M, Wang SD, et al. Legislation has changed but issues remain: provider perceptions of caring for people who use cannabis during pregnancy in safety net health settings, a qualitative pilot study. Womens Health Rep. (2023b) 4:400–8. doi: 10.1089/whr.2023.0057
30. Patel E, Bandara S, Saloner B, Stuart EA, Goodman D, Terplan M, et al. Heterogeneity in prenatal substance use screening despite universal screening recommendations: findings from the pregnancy risk assessment monitoring system, 2016–2018. Am J Obstet Gynecol MFM. (2021) 3:100419. doi: 10.1016/j.ajogmf.2021.100419
31. Stadterman JM, Hart CL. Screening women for marijuana use does more harm than good. Am J Obstet Gynecol. (2015) 213:598–9. doi: 10.1016/j.ajog.2015.06.024
32. Mark K, Terplan M. Cannabis and pregnancy: maternal child health implications during a period of drug policy liberalization. Prev Med. (2017) 104:46–9. doi: 10.1016/j.ypmed.2017.05.012
33. Ceasar RC, Gould E, Laughter J, Granacki J, Kirsch K, Chauca E, et al. “They might take my baby away:” black and Latina peoples’ experiences of using cannabis during pregnancy in California while engaged in perinatal care. J Perinatol. (2023) 43:1497–9. doi: 10.1038/s41372-023-01781-7
34. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
35. Dossett LA, Kaji AH, Cochran A. SRQR and COREQ reporting guidelines for qualitative studies. JAMA Surg. (2021) 156:875. doi: 10.1001/jamasurg.2021.0525
36. Starks H, Brown Trinidad S. Choose your method: a comparison of phenomenology, discourse analysis, and grounded theory. Qual Health Res. (2007) 17:1372–80. doi: 10.1177/1049732307307031
37. Fornaro CJ, Sterin K, Struloeff KL. Qualitative data collection tools: design, development, and applications by Felice D. Billups. CICE. (2021) 23. doi: 10.52214/cice.v23i1.8144
39. Ligita T, Harvey N, Wicking K, Nurjannah I, Francis K. A practical example of using theoretical sampling throughout a grounded theory study: a methodological paper. Qual Res J. (2019) 20:116–26. doi: 10.1108/QRJ-07-2019-0059
40. Bastain TM, Chavez T, Habre R, Girguis MS, Grubbs B, Toledo-Corral C, et al. Study design, protocol and profile of the maternal and developmental risks from environmental and social stressors (MADRES) pregnancy cohort: a prospective cohort study in predominantly low-income hispanic women in urban Los Angeles. BMC Pregnancy Childbirth. (2019) 19:189. doi: 10.1186/s12884-019-2330-7
41. Department of Health Care Services. What is medi-cal? [WWW Document]. Washington, D.C.: Department of Health Care Services (2024). Available online at: https://www.dhcs.ca.gov/services/medi-cal/pages/whatismedi-cal.aspx
42. Coyne IT. Sampling in qualitative research. Purposeful and theoretical sampling; merging or clear boundaries? J Adv Nurs. (1997) 26:623–30. doi: 10.1046/j.1365-2648.1997.t01-25-00999.x
43. Burnard P. Writing a qualitative research report. Accid Emerg Nurs. (2004) 12:176–81. doi: 10.1016/j.aaen.2003.11.006
44. Jarlenski M, Tarr JA, Holland CL, Farrell D, Chang JC. Pregnant women’s access to information about perinatal marijuana use: a qualitative study. Women’s Health Issues. (2016) 26:452–9. doi: 10.1016/j.whi.2016.03.010
45. Latuskie KA, Andrews NCZ, Motz M, Leibson T, Austin Z, Ito S, et al. Reasons for substance use continuation and discontinuation during pregnancy: a qualitative study. Women Birth. (2019) 32:e57–64. doi: 10.1016/j.wombi.2018.04.001
46. Vanstone M, Taneja S, Popoola A, Panday J, Greyson D, Lennox R, et al. Reasons for cannabis use during pregnancy and lactation: a qualitative study. CMAJ. (2021) 193:E1906–14. doi: 10.1503/cmaj.211236
47. Charmaz K, Thornberg R. The pursuit of quality in grounded theory. Qual Res Psychol. (2021) 18:305–27. doi: 10.1080/14780887.2020.1780357
48. Sangaramoorthy T, Kroeger KA. Rapid Ethnographic Assessments: A Practical Approach and Toolkit for Collaborative Community Research. 1st ed. Oakland: Routledge (2020). doi: 10.4324/9780429286650
50. Farmer PE, Nizeye B, Stulac S, Keshavjee S. Structural violence and clinical medicine. PLoS Med. (2006) 3:e449. doi: 10.1371/journal.pmed.0030449
51. Galtung J. Violence, peace, and peace research. J Peace Res. (1969) 6:167–91. doi: 10.1177/002234336900600301
52. Farmer P. An anthropology of structural violence. Curr Anthropol. (2004) 45:305–25. doi: 10.1086/382250
53. Metzl JM, Hansen H. Structural competency: theorizing a new medical engagement with stigma and inequality. Soc Sci Med. (2014) 103:126–33. doi: 10.1016/j.socscimed.2013.06.032
54. Farmer P, Nizeye B, Stulac S, Keshavjee S. Structural violence and clinical medicine. In: Brown PJ, Closser S, editors. Understanding and Applying Medical Anthropology. New York: Routledge (2016). p. 336–43.
56. van Boekel LC, Brouwers EPM, van Weeghel J, Garretsen HFL. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. (2013) 131:23–35. doi: 10.1016/j.drugalcdep.2013.02.018
57. Hatzenbuehler ML. Structural stigma: research evidence and implications for psychological science. Am Psycho. (2016) 71:742–51. doi: 10.1037/amp0000068
58. Nyblade L, Stockton MA, Giger K, Bond V, Ekstrand ML, Lean RM, et al. Stigma in health facilities: why it matters and how we can change it. BMC Med. (2019) 17:25. doi: 10.1186/s12916-019-1256-2
59. Barbosa-Leiker C, Brooks O, Smith CL, Burduli E, Gartstein MA. Healthcare professionals’ and budtenders’ perceptions of perinatal cannabis use. Am J Drug Alcohol Abuse. (2022) 48:186–94. doi: 10.1080/00952990.2021.1988091
60. Holland CL, Rubio D, Rodriguez KL, Kraemer KL, Day N, Arnold RM, et al. Obstetric health care providers’ counseling responses to pregnant patient disclosures of marijuana use. Obstet Gynecol. (2016) 127:681–7. doi: 10.1097/AOG.0000000000001343
61. Mark K, Crimmins S. Maternal and infant cannabis testing and associated birth outcomes. Arch Gynecol Obstet. (2023) 55. doi: 10.1007/s00404-023-07009-5
62. Lebron CN, Morales V, Saenz S, Vidot DC. “Ganja mamas”: online discussions about cannabis use in pregnancy. Drug Alcohol Depend. (2022) 241:109689. doi: 10.1016/j.drugalcdep.2022.109689
63. Khademi S, Hallinan CM, Conway M, Bonomo Y. Using social media data to investigate public perceptions of cannabis as a medicine: narrative review. J Med Internet Res. (2023) 25:e36667. doi: 10.2196/36667
64. Barbosa-Leiker C, Burduli E, Smith CL, Brooks O, Orr M, Gartstein M. Daily cannabis use during pregnancy and postpartum in a state with legalized recreational cannabis. J Addict Med. (2020) 14:467–74. doi: 10.1097/ADM.0000000000000625
65. Norman CD, Skinner HA. eHEALS: the eHealth literacy scale. J Med Internet Res. (2006) 8:e27. doi: 10.2196/jmir.8.4.e27
66. Woodruff K, Scott KA, Roberts SCM. Pregnant people’s experiences discussing their cannabis use with prenatal care providers in a state with legalized cannabis. Drug Alcohol Depend. (2021) 227:108998. doi: 10.1016/j.drugalcdep.2021.108998
67. Parandeh Afshar P, Keshavarz F, Salehi M, Fakhri Moghadam R, Khajoui E, Nazari F, et al. Health literacy and media literacy: is there any relation? Community Health Equity Res Policy. (2022) 42:195–201. doi: 10.1177/0272684X20972642
68. Polanco-Levicán K, Salvo-Garrido S. Understanding social media literacy: a systematic review of the concept and its competences. Int J Environ Res Public Health. (2022) 19:8807. doi: 10.3390/ijerph19148807
69. Centers for Disease Control and Prevention. Develop & test materials. [WWW Document]. (2023a). Available online at: https://www.cdc.gov/healthliteracy/developmaterials/index.htm (Accessed October 19, 2023).
70. Centers for Disease Control and Prevention. Simply put: a guide for creating easy-to-understand materials [WWW Document]. (2023b). Available online at: https://www.cdc.gov/healthliteracy/pdf/simply_put.pdf (Accessed June 2022).
71. Magnan E, Weyrich M, Miller M, Melnikow J, Moulin A, Servis M, et al. Stigma against patients with substance use disorders among health care professionals and trainees and stigma-reducing interventions: a systematic review. Acad Med. (2023) 6:1–5. doi: 10.1097/ACM.0000000000005467
72. American College of Obstetricians and Gynecologists. Marijuana use during pregnancy and lactation [WWW Document]. (2021). Available online at: https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/10/marijuana-use-during-pregnancy-and-lactation
73. Chen J, Wang Y. Social media use for health purposes: systematic review. J Med Internet Res. (2021) 23:e17917. doi: 10.2196/17917
74. Petkovic J, Duench S, Trawin J, Dewidar O, Pardo Pardo J, Simeon R, et al. Behavioural interventions delivered through interactive social media for health behaviour change, health outcomes, and health equity in the adult population. Cochrane Database Syst Rev. (2021) 99:1–238. doi: 10.1002/14651858.CD012932.pub2
75. Sim W, Lim WH, Ng CH, Chin YH, Yaow CYL, Cheong CWZ, et al. The perspectives of health professionals and patients on racism in healthcare: a qualitative systematic review. PLoS One. (2021) 16:e0255936. doi: 10.1371/journal.pone.0255936
76. Hamed S, Bradby H, Ahlberg BM, Thapar-Björkert S. Racism in healthcare: a scoping review. BMC Public Health. (2022) 22:988. doi: 10.1186/s12889-022-13122-y
Keywords: pregnancy, prenatal cannabis use, healthcare provider knowledge, maternal health, substance use
Citation: Gould EE, Ganesh SS, Nguyen RM, Breton CV, Bastain TM, Dunton GF and Ceasar RC (2024) The unseen patient: competing priorities between patients and providers when cannabis is used in pregnancy, a qualitative study. Front. Glob. Womens Health 5:1355375. doi: 10.3389/fgwh.2024.1355375
Received: 13 December 2023; Accepted: 25 March 2024;
Published: 18 April 2024.
Edited by:
Tabassum Firoz, Yale New Haven Health System, United StatesReviewed by:
Audrey Merriam, Yale University, United StatesJean Tornatore, Yale New Haven Health System, United States
© 2024 Gould, Ganesh, Nguyen, Breton, Bastain, Dunton and Ceasar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Erin E. Gould ering@usc.edu
 Erin E. Gould
Erin E. Gould Siddhi S. Ganesh
Siddhi S. Ganesh Ryan Mikeala Nguyen
Ryan Mikeala Nguyen  Theresa M. Bastain
Theresa M. Bastain Genevieve F. Dunton
Genevieve F. Dunton Rachel Carmen Ceasar
Rachel Carmen Ceasar