- 1School of Public Health and Family Medicine, Kamuzu University of Health Sciences, Blantyre, Malawi
- 2 Institute for Medical Information Processing, Biometry and Epidemiology, LMU Munich, Munich, Germany
- 3Pettenkofer School of Public Health, Munich, Germany
- 4Chronic Disease Initiative for Africa, University of Cape Town, Cape Town, South Africa
- 5Department of Public Health, Vrije Universiteit Brussel, Brussels, Belgium
- 6Department of Disease Control and Environmental Health, School of Public Health, College of Health Sciences, Makerere University, Kampala, Uganda
- 7College of Medicine and Health Sciences, University of Rwanda, Kigali, Rwanda
- 8Non-Communicable Diseases Directorate, Armauer Hansen Research Institute, Addis Ababa, Ethiopia
- 9Centre for Evidence-based Health Care, Division of Epidemiology and Biostatistics, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
- 10Department of International Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States
Background: Low- and middle-income countries (LMICs) are currently experiencing an increasing prevalence of non-communicable diseases (NCDs). To address this as well as other health challenges, Integrated Knowledge Translation (IKT) approaches to build mutually beneficial relationships between researchers and decision-makers can concurrently inform research as well as enhance evidence use in policy and practice. The Collaboration for Evidence-Based Healthcare and Public Health in Africa (CEBHA+) is a research consortium which conducts research on NCDs and uses an IKT approach to facilitate the uptake of this research in five African countries: Ethiopia, Uganda, Rwanda, Malawi, and South Africa. Tailored IKT strategies were designed and implemented to plan and guide stakeholder engagement. This systematic approach contrasts with more commonly used ad hoc approaches to stakeholder engagement.
Methods: In this article, we explore the experiences of researchers engaged in the CEBHA+ IKT approach across the five African countries. Data sources included: 1) an informal document review of CEBHA+ country-specific IKT strategies, IKT team meeting minutes and activity reports, and 2) a semi-structured survey of IKT implementers to elicit country-specific experiences on actual implementation and adaptation of the IKT strategies. Results were collated and contrasted across all CEBHA+ countries with a focus on systematic versus ad hoc approaches to engagement.
Results: South Africa, Malawi and Ethiopia country teams indicated that their engagements benefited from a systematic IKT strategy. This was especially the case in the early stages of the project as it allowed focused and intentional engagement. However, ad hoc engagement was still required as new professional relationships developed, and contextual circumstances - including the SARS-CoV-2 pandemic - required responsive engagement with decision-makers and other stakeholders. In Rwanda and Uganda, continuous systematic engagement was found to bolster ownership of the research at both community and national levels.
Conclusion: Political and health climates are constantly shifting with a need to maintain flexibility in how IKT strategies are implemented. While strategic IKT can benefit from deliberate planning and stakeholder engagement, there is value in remaining flexible to respond to the needs of stakeholders and contextual circumstances. This paper highlights how IKT implementers in the five African CEBHA+ countries responded to this challenge.
Introduction
Non-Communicable Disease Burden
Globally, non-communicable diseases (NCDs) account for 71% of deaths with 41 million people dying each year (1). Cardiovascular diseases, cancers, respiratory diseases, and diabetes are amongst the top four killers. In sub-Saharan Africa (SSA) the burden of disease from NCDs increased from 18.6% in 1990 to 29.8% in 2017 (2). This increase can be attributed to an increase in population size and an ageing population. The age standardized rate of disability-adjusted life years (DALYs) due to NCDs (21,757.7 DALYs/100,000 population) was almost equivalent to that for communicable, maternal, neonatal, and nutritional diseases (26,491.6 DALYs/100,000 population) (2).
These challenges call for public health and healthcare decision-making that is informed by the best available, context-specific evidence for the prevention, diagnosis, and care of NCDs in SSA (3, 4). It has long been recognized, however, that research evidence does not easily translate into health policy and change practice for a number of reasons (5). Amongst other factors, research translation is a complex, dynamic and non-linear process that is dependent on timeliness and relevance of research as well as relationship-building and collaborations with policymakers (6). This has sometimes been referred to as the “know-do gap” and has subsequently sparked deliberate practices and global efforts to address this challenge and link research to action, in both healthcare and public health (7–10).
Integrated Knowledge Translation
There exists a diversity of terms referring to activities that aim to close the “know-do” gap. Knowledge translation represents one such term, which has gained particular traction in public health and has been described as “a dynamic and iterative process that includes synthesis, dissemination, exchange and ethically-sound application of knowledge to improve [health], provide more effective health services and products and strengthen the healthcare system” by the Canadian Institutes of Health Research (11). Knowledge translation (KT), along with other approaches to address the “know-do” gap, have been subsumed under the umbrella term knowledge to action (KTA), a framework delineating the processes of knowledge creation and action, e.g. policy or practice action (12). The KTA framework emphasizes that the knowledge cycle and action cycle can be distinct but may also be closely intertwined, requiring an exchange between knowledge producers and users (12).
Recently, there has been an increasing interest in approaches to strengthen the collaboration between knowledge producers and knowledge users, representing this ‘exchange’ model (13). This is because knowledge users have expertise in the topic and context while researchers bring methodological and content competences (14). These efforts are referred to under a range of different terminologies including but not limited to research co-production, engaged scholarship, participatory action research, and integrated knowledge translation (IKT) (13, 15). IKT seeks to ensure that research focuses on the needs of knowledge users, such as decision-makers in healthcare and public health (13, 16). IKT comprises a process of ongoing, collaborative research with knowledge users “who identify a problem and have the authority to implement the research recommendations” (14). In this process, researchers and knowledge users aspire to work as equals for their mutual benefit and learning (13) and may collaborate on one of the following: information exchange; formulating the research question; data collection, analysis, and/or interpretation; formulating policy recommendations; or developing implementation strategies (17, 18). IKT approaches thus flow from the premise that knowledge co-produced with decision-makers is more likely to i) increase the availability of contextually relevant research evidence, ii) enhance its usefulness for knowledge users, and iii) improve decision-maker access to and application of relevant evidence, in order to ultimately influence practice, policy, and health systems at large (14, 16, 19).
In recent years, interest in IKT has increased, in particular among funders (20) and researchers (13). Evidence details the promises and potential benefits of employing an IKT approach (21, 22) as well as some of its unintended effects or risks (23). Furthermore, some of the key barriers to undertaking IKT include: differing needs and priorities of researchers and decision-makers, lack of funding, staff turnover, and a lack of clarity about the IKT concept and respective roles; whilst multiple avenues for interaction, leadership commitment, formalized structures, partner openness, and pre-existing relationships constitute commonly identified enablers (19). With respect to knowledge translation in LMICs further particularities have been described, including the “tension between ‘global’ and ‘local’ evidence; complexities in accessing and creating evidence; contextualizing strategies for KT in LMICs; and the unique role of non-governmental organizations (NGOs) in the KT process” (24), as well as a lack of institutional incentives and insufficient networks for KT (25). There have been a number of efforts in LMICs to investigate the barriers and facilitators to knowledge translation. A systematic review described the lessons learnt from descriptions and evaluations of KT platforms in LMICs (26) and more specifically, a study focusing on global health research projects in Tunisia and Cote D’Ivoire (27) outlined barriers and facilitators of stakeholder engagement. Both Kalbarczyk et al. (25) and Jessani et al. (28) recognize that academic institutions are strategically placed to conduct IKT activities. The authors assessed barriers and facilitators in academic institutions in LMICs and described strategies for engagement at public health faculty and policymakers in Kenya respectively (25, 28). Thus, whilst barriers and facilitators to knowledge translation have received some research attention, in-depth studies of the processes and implementation of KT and IKT activities, including rigorous evaluation, remain scarce (19, 21, 26). And although the usefulness of IKT in healthcare has been shown, there is a need for more research to ascertain amongst other issues, the most effective means of partnership formation and collaboration (19).
Integrated Knowledge Translation as a Key Concept in CEBHA+
The Collaboration for Evidence Based Healthcare and Public Health in Africa (CEBHA+) is a research consortium which employs a systematic IKT approach to engage with decision-makers and ultimately facilitate uptake of NCD research in five African countries: Ethiopia, Malawi, Rwanda, South Africa, and Uganda (see Figure 1).
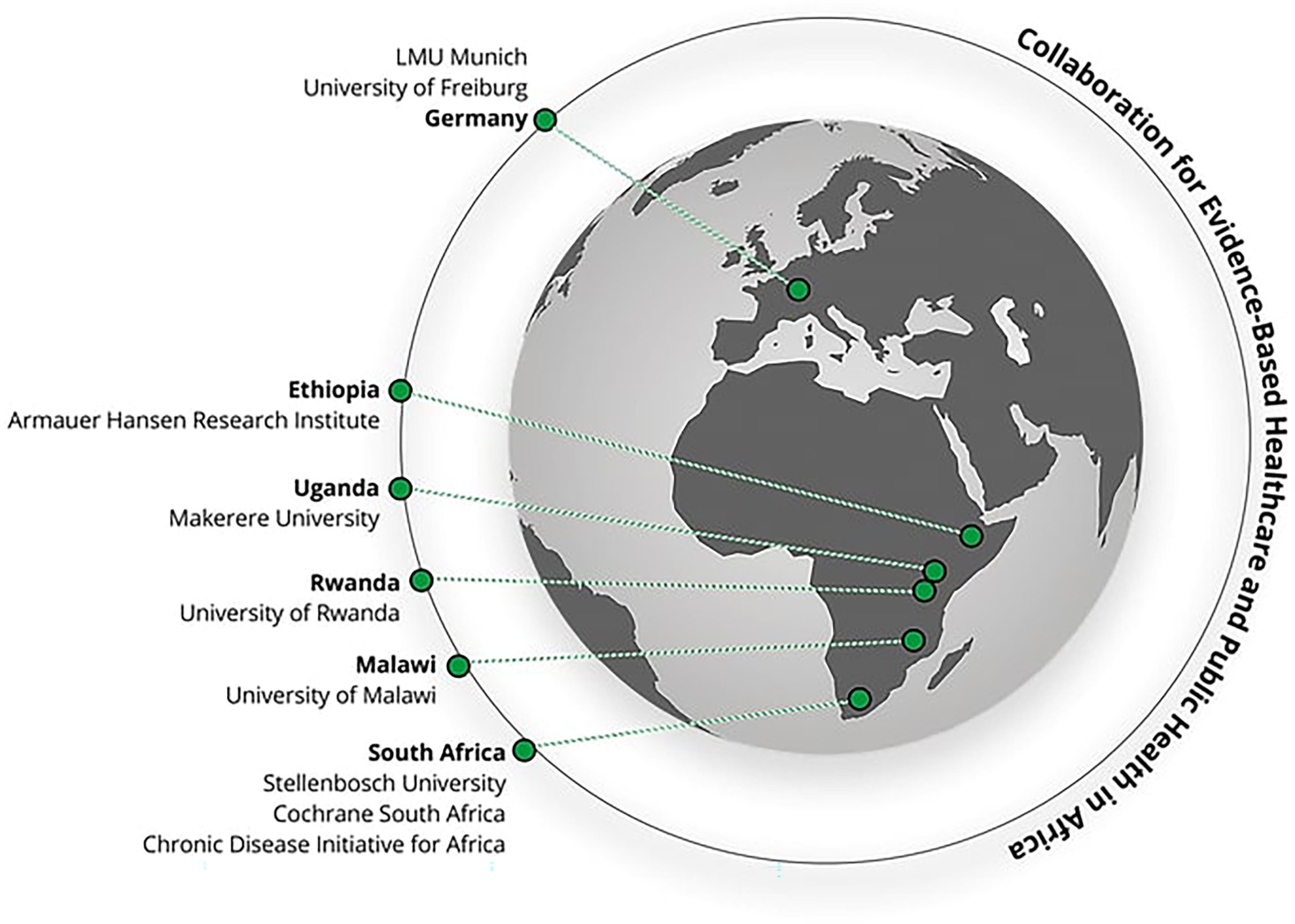
Figure 1 Overview of partner countries and institutions in CEBHA+ (29).
In order to address policy-relevant questions and fill priority research gaps, the scope of CEBHA+ was defined in consultation with decision-makers from SSA and based on evidence (gap) maps (30). As a result, CEBHA+ focused on rigorous primary and secondary research in the field of screening, prevention and integrated care for diabetes and hypertension (Ethiopia, Malawi, Rwanda, Uganda, South Africa), as well as the prevention of road traffic injuries (Rwanda, Uganda). Its ultimate goal is building long-term capacity and infrastructure for evidence-based healthcare and public health in SSA.
The CEBHA+ consortium developed a general IKT framework and process (29). All five country teams in SSA subsequently developed a site-specific stakeholder engagement strategy that first evolved as part of a joint CEBHA+ partner workshop in 2018 (31). During this workshop, each country team plotted stakeholders on a power/interest grid to determine how stakeholders would be prioritized. They subsequently produced detailed engagement strategies for these priority stakeholders including specification of the main message/topic of the engagement, the messenger, the appropriate medium and forum, as well as uptake indicators (32). Each team then implemented their strategies locally, refined them where appropriate, and monitored them for adaptation and learning. One or two researchers at each site acted as IKT focal points and participated in regular update meetings with the CEBHA+ IKT team to discuss implementation and experiences. This process as well as the context that influenced the implementation has been described in detail for the case of South Africa (33).
This systematic approach contrasts with an ‘ad hoc’ mode of stakeholder engagement, which is akin to a more reactive or responsive approach to stakeholder engagement as part of a traditionally protracted process of new evidence moving into policy and practice (12). For the purpose of this paper, we understand ad hoc engagement as interactions with stakeholders that were not deliberately planned in the IKT strategy or that covered topics beyond the CEBHA+ project focus.
In this article, we thus aim to share five years of experience (from 2017 to 2021) from the perspective of researchers from the five CEBHA+ partner countries in SSA who have engaged in deliberate, planned, and systematic as well as ad hoc IKT. Through this analysis of experiences, we aim to shed light on the IKT process and implementation aspects, focusing in particular on the systematic nature of the IKT approach as well as instances of more ad hoc modes of stakeholder engagement. Additionally, we seek to describe some intermediate outcomes of incorporating IKT into a multinational consortium seeking to advance NCD policy and practice. The paper, however, does not purport to determine what is best practice and does not constitute a formal evaluation of IKT in CEBHA+ which will be reported elsewhere (29).
Methods
This is a qualitative analysis which focuses on the reflections from IKT country teams. We used a cross-sectional study design using a self-administered semi-structured questionnaire and a document review of project minutes and reports. Our approach entailed the following steps: TM and NJ spearheaded the development of a semi-structured survey to explore CEBHA+ researchers’ experiences of both undertaking systematic IKT activities as well as their ad hoc engagement with stakeholders at each site. The survey was refined by IKT focal points from each partner country. The survey requested details of the stakeholder engagement strategies, aspects which had been successfully implemented instances of ad hoc or responsive stakeholder engagement and benefits and disadvantages of both approaches (see online Supplementary Material). In June 2021, the survey was sent electronically as a Microsoft Word document to the IKT focal points of each country, filled in, and submitted to the corresponding first author (TM). Country teams drew on their stakeholder engagement strategies, meeting minutes, and in-group reflections to respond to the questions. These inputs were read, examined, and analyzed by the first author using key questions from the survey as guiding themes for the analysis of responses and the organization of this article. Data related to individual countries was analyzed first before making comparisons across countries. Common themes and results that emerged from the analysis were discussed and verified by the country representatives who co-authored this paper and subsequently compiled.
Results
Country Summaries
Country summaries were available for all five CEBHA+ partner countries in SSA. To establish the background, we prompted countries to describe the characteristics of their initial IKT strategies, which are detailed below.
Ethiopia
CEBHA+ in Ethiopia is situated at the Armauer Hansen Research Institute (AHRI). The aims of stakeholder engagement were as follows: to establish a relationship that would allow sharing of project and research updates and to increase awareness of evidence-based healthcare through capacity-building activities such as trainings and workshops. A total of 18 stakeholders were identified, including policymakers [NCD Directorate of the Ethiopian Ministry of Health (MOH)], NGOs actively involved in NCD healthcare delivery, and advocacy organizations such as the Diabetes Association of Ethiopia. In-person meetings, telephone calls, and emails were the chosen forms of engagement. Initially, the principal investigator was responsible for engagement, but the responsibilities were delegated to other team members as the team grew.
Malawi
In Malawi, CEBHA+ research is conducted at the Kamuzu University of Health Sciences (KUHES, formerly known as College of Medicine, University of Malawi). The research team, together with officials from the MOH refined the stakeholder engagement strategy drafted in an earlier IKT stakeholder workshop in Cape Town. The team identified 14 priority stakeholders including policymakers (MOH NCD unit, MOH research unit), NCD advocacy groups (Diabetes Association of Malawi, Communities against Diabetes and Hypertension), academia (KUHES faculty members), and NGOs addressing NCDs. The research team planned to carry out engagement through in-person meetings, capacity-building workshops, emails, and phone calls. Initially, engagement was carried out by the project coordinator and principal investigator but later some duties were assigned to an IKT research fellow. The IKT strategy was intended to inform and update stakeholders on research findings and project progress, to build capacity in evidence-based healthcare and to lobby for uptake of research findings into decision-making processes.
Rwanda
In Rwanda, CEBHA+ consists of a research team from the University of Rwanda. Amongst the 68 stakeholders who were identified in the initial IKT stakeholder mapping, 18 were deemed to be priority stakeholders. They consisted of policymakers from relevant ministries (Ministry of Health, Ministry of Sports, Ministry of Infrastructure and Ministry of labor and public services), health practitioners (Rwanda Biomedical Centre, University teaching Hospital of Kigali, Rwanda Military Hospital), law enforcement (Rwanda Traffic Police, Rwanda utilities and regulatory authority), and civil society organizations (National Council of Persons with Disabilities, Rwanda Diabetes Association, Rwanda Insurers Association, NCDs alliance). Planned communication channels varied, and both formal and informal means were used including in-person and online meetings, emails, phone calls, social media, interaction during workshops and an annual stakeholder meeting. The project coordinator was responsible for driving engagement, but researchers had the task of interacting with stakeholders relevant to their specific research tasks. The IKT strategy was instrumental for the initiation of specific research activities and played a vital role in the uptake of these research findings. In Rwanda, the IKT approach was coupled with a community citizen science approach in one of the implemented research projects as described by Niyibizi et al. (34).
South Africa
The South African country team consists of partners across three organizations: Stellenbosch University, Cochrane South Africa, and the Chronic Diseases Initiative for Africa (CDIA). A dedicated IKT focal person was identified at each of these institutions. All three organizations are based in Cape Town in the Western Cape Province which permitted ease of communication and coordination but also limited relationships to decision-makers at the Western Cape Department of Health (WCDoH) and the National Department of Health (NDoH). Altogether, 20 stakeholders were identified, eight of which were prioritized. Besides the WCDoH and NDoH, the list also included research institutions (South African Medical Research Council) and civil society organizations (South African NCD Alliance). The main goal of the IKT strategy in South Africa was to establish and enhance partnerships, promote research collaboration, increase NCD research awareness, contribute to priority setting, and influence NCD policy and practice.
Uganda
CEBHA+ in Uganda consists of researchers from Makerere University. Prior to the development of a stakeholder engagement strategy, interactions had occurred organically since the inception of the project. The process was however formalized through the development of the IKT strategy and priority stakeholders identified, including policymakers (Ministry of Health, Ministry of Works and Transport), law enforcement (Uganda Traffic Police), and Kampala Capital City Authority. The main purpose of the IKT strategy was research collaboration (some stakeholders provided key data for research); to engage in agenda setting with respect to road traffic issues; and to increase the awareness of research for better use in policy and practice. Like Rwanda, the project coordinator and principal investigator in Uganda were responsible for implementing the strategy.
Development of IKT Strategies
There was consensus among CEBHA+ team members that pre-existing professional relationships were important for stakeholder engagement and in some cases, determined who would be the messenger as defined in the IKT strategy, i.e., the most appropriate person to interact with the research user or stakeholder of interest. Both the Malawi and South African partners noted that their stakeholder engagement strategy reflected stakeholder needs and was tailored to suit them with respect to timing and mode of communication.
Enabling Factors for Systematic Stakeholder Engagement
Each country context gave rise to a different set of enablers for IKT. In Uganda, stakeholder commitment to addressing road safety motivated their interaction with researchers. In South Africa, the political climate prioritized NCDs which permitted traction of the CEBHA+ research. Having similar goals across the research team and research-users enhanced stakeholder engagement. Ethiopia described a rising need for NGOs in the country to include evidence when submitting grant applications, thereby making CEBHA+’s planned capacity-building activities a worthwhile venture as NGOs were able to upgrade their skills in this area. Affiliation to well established and respected academic institutions assisted with credibility of the research and research team when engaging with stakeholders in the five countries. Relationships were also invaluable for stakeholder engagement. In Rwanda, Uganda, and South Africa, the CEBHA+ team consisted of individuals from different institutions who had prior relationships with key stakeholders, thereby providing an entry point for engagement. In South Africa, dedicated resources, both financial and human, were also considered enablers for coordinating stakeholder engagement. In Malawi, the CEBHA+ team highlighted that being part of a network of evidence brokers called EvIDeNt (Evidence-Informed Decision-Making Network for Health Policy and Practice in Malawi) and involvement in its activities resulted in familiarity of the project for key health policy and research stakeholders.
Challenges Encountered During Systematic Stakeholder Engagement
Natural to all efforts with stakeholder engagement, the various sites experienced some challenges. Staff turnover within the stakeholder institutions proved to be disruptive in Ethiopia, Uganda, and Rwanda. This was especially the case in government institutions where political changes led to personnel changes. The CEBHA+ Ethiopian, Ugandan and Rwandan partners were however able to mitigate disruption by identifying multiple contacts within an organization during the development and implementation of the strategy instead of reliance on one key contact.
As the stakeholder engagement strategy was rolled out, it became apparent at some sites that the level of stakeholder interest had been misjudged or incorrectly assumed. In Malawi, the timing and frequency of some engagements was also misjudged; some stakeholders would only need to be engaged for the purpose of information sharing as research results became available. In South Africa, despite efforts to tweak the mode of communication, engagement in some cases was still unsuccessful. In Ethiopia, this was determined to be due to the lack of awareness by some key stakeholders of the importance of evidence-based healthcare. Furthermore, the Ethiopian site encountered similar initiatives in the country addressing the same research questions as CEBHA+. Rather than duplicate efforts, the Ethiopian team was able to modify its approach so that both research and capacity-building activities would add to existing programs in the country.
A veritable challenge that was more external to the project was the impact of the global COVID-19 pandemic. All five sites had included face-to-face meetings as a key mode of engagement in their stakeholder strategy which was inevitably disrupted by COVID-19. This required a shift from physical to virtual meetings and caused overall delays in some planned meetings. For some aspects of the project, such as primary research in South Africa, the entire research was put on hold as access to clinics was restricted during the pandemic.
Scheduling of meetings with high profile individuals also required some flexibility due to full schedules. Both the South African and Malawian sites creatively and opportunistically leveraged forums where groups of stakeholders were present to share information as opposed to focusing on individual interactions. This was especially relevant for stakeholders within government ministries and departments.
Whilst acknowledging the merits of a systematic planned approach, the Ethiopian and South African sites maintained the need for flexibility while implementing the strategy to avoid missing out on opportunities.
Instances of Ad Hoc Stakeholder Engagement
While the country sites were all able to implement some aspects of their planned stakeholder engagement strategies, they were also involved in some activities which had not initially been anticipated. In particular, when the COVID-19 pandemic warranted an urgent need for evidence, decision-makers and practitioners turned to the research community for rapid responses. For instance, the Malawi CEBHA+ team was involved in building the capacity of researchers to develop issue briefs communicating COVID-19 research results to better inform public health responses to the pandemic. This activity was facilitated by the Ministry of Health Research Unit, and more specifically the Knowledge Translation Platform (KTP) Malawi, one of CEBHA+ Malawi’s key stakeholders. The KTP Malawi coordinator had previously benefited from an issue briefs training facilitated by South African CEBHA+ partners at Stellenbosch University. Similarly, in South Africa, the CEBHA+ team in collaboration with other researchers in the country provided rapid reviews and evidence syntheses to guide the government on COVID-19 related lockdown and infection mitigation measures. South African CEBHA+ researchers also engaged in new emerging research questions, for instance, “The impact of COVID-19 on the delivery and uptake of NCD services at local level”. These ad hoc engagements as a result of knowledge user demand instigated by COVID-19 led to amendments and adaptations of the local stakeholder engagement strategies.
In 2019, the Malawi CEBHA+ team partnered with the NCD Unit of the MoH at its request to conduct further evidence synthesis on one of its priority areas: screening of hypertension and diabetes in Malawi. A series of prioritization, communities of practice and writing meetings took place to develop the aforementioned policy brief. Similarly, in South Africa, opportunities arose to interact with local and national government officials in matters related to NCD agenda setting in 2020.
In Ethiopia, a significant proportion of engagement occurred responsively due to several factors; first, the AHRI team observed that other stakeholders in the country including the Knowledge Management Directorate under AHRI, the Fenot initiative, and the Ethiopian Public Health Institute (EPHI) had also planned capacity-building activities similar to those planned by CEBHA+.
The Ethiopian team modified their planned capacity-building activities to make them collaborative ventures with the three aforementioned stakeholders. Together, they planned a long-term course on systematic reviews. This adaptation highlighted that the initial stakeholder mapping had been incomplete, supporting the assertion highlighted in the initial workshop (31) that it needed to be an iterative process. A second issue was linked to a change in the approach to research, specifically on community healthcare worker screening of CVD risk. The AHRI researchers became aware that the Ethiopian MoH had previously initiated a similar program in Addis Ababa. The researchers therefore refocused research efforts to regions and clinics which had not yet implemented this approach and partnered with the MOH NCD directorate to rollout training on basic NCD care in addition to the previously planned research work on a new CVD risk screening tool.
Advantages and Disadvantages of Ad Hoc Engagement
In all cases, ad hoc engagements were described as complementary to the existing strategy. In Rwanda, ad hoc engagements enabled the research team to access data crucial to their research, which was previously unattainable through a government official who was initially included in the strategy. Both Malawi and Uganda CEBHA+ teams noted that ad hoc engagement increased project buy-in from its main stakeholders (MoH NCD unit and road safety institutions). Bearing this in mind, the Malawi CEBHA+ team indicated that unlike in systematic and planned IKT engagement, resources were not earmarked for such ad hoc activities resulting in potential budgeting challenges. They also highlighted the need to ensure that ad hoc activities done in collaboration with other stakeholders did not distract from overall project goals.
IKT teams in both Rwanda and Ethiopia were able to strengthen relationships with key stakeholders and generate knowledge which was relevant to the local context through ad hoc engagement. South Africa emphasized that successful stakeholder engagement, both systematic and ad hoc depended on the quality of personal relationships, a key factor in achieving implementation results.
Outcomes of Stakeholder Engagement
All country IKT teams agreed that developing a systematic IKT and stakeholder engagement strategy was valuable as it provided a strategic starting point for IKT activities. Identification of key stakeholders was not left to chance and efforts were focused, systematic and deliberate. CEBHA+ researchers reported some intermediate outcomes of the IKT intervention that were seen as enablers of the project’s ultimate aim which was to increase uptake and consideration of relevant research evidence in policy and practice. Whilst the latter was not investigated in this study, relevant intermediate outcomes included improved relationships, joint identification of research and capacity-building gaps, and creation of an enabling environment for research uptake into policy and practice. We elaborate on these further below.
Relationships
Although several country sites drew on pre-existing professional relationships to facilitate engagement, a thorough stakeholder mapping helped to draw in new actors and the stakeholder analysis helped to identify priority actors to engage with. For instance, in South Africa, the CEBHA+ team was able to compile a comprehensive list of guests to invite to the NCD Research Symposium that it jointly hosted with the NDoH in March 2020. This symposium permitted exchange of new knowledge on NCDs across multiple stakeholders and provided a networking opportunity for researchers, policymakers and practitioners. Ethiopia pointed out that embedding a strategic IKT approach into the CEBHA+ project required them to forge new relationships which proved very useful in the eventual demand, acceptance and uptake of CEBHA+ NCD research results.
Gap Identification: Capacity and Research
The IKT approach also assisted the CEBHA+ team in Ethiopia to identify capacity gaps amongst its stakeholders, particularly around evidence-based policymaking. Of note, while NGOs were aware of the need to support international funding applications with strong evidence, they lacked the skills. NGOs were therefore attracted to CEBHA+’s capacity building activities. Both the Rwandan and Ethiopian sites reflected on how a systematic strategy encouraged co-creation of knowledge, identification of relevant research questions, and potential future collaborations. For instance, in Rwanda, during the dissemination of results on screening for hypertension, diabetes, and CVD risk, a feedback session from stakeholders resulted in the addition of a new research question and an important amendment of the study protocol.
Enabling Environment for Research Uptake Into Policy and Practice
The embedded IKT approach into the CEBHA+ project produced synergies between the researchers and the research users resulting in better science, enhancing the ultimate production of more relevant and actionable research findings, and increasing the likelihood of findings being used in policy and practice. For example, it led to the development of an electronic data system to replace paper-based record keeping for road traffic crashes in Uganda. Additionally, in Uganda and Malawi, systematic stakeholder engagement was reported to create a receptive and conducive environment for collaboration, research and uptake of research findings. In Malawi in particular, the research team disseminated results for one of its research tasks (a situational analysis of population-level interventions targeting risk factors for diabetes and hypertension) to a diverse pool of stakeholders who were eager to offer feedback and suggestions to improve the study.
In Rwanda, stakeholders joined the CEBHA+ team and actively provided support in the implementation of research activities such as protocol writing, data collection, analysis, and feedback sessions. Across all research foci, preliminary results for some studies were shared with various stakeholders at national and community level, and their inputs or suggestions were leveraged during the writing up of the papers for publication in peer reviewed journals.
As mentioned above, South African colleagues were requested by the NDoH to provide rapid evidence syntheses and appraisals on new and emerging NCD related issues during the COVID-19 pandemic, e.g. the impact of COVID-19 on the delivery and uptake of NCD services at local level, which was shared with policymakers at the appropriate fora.
Discussion
This article summarizes five country teams’ reflections on their experience with a systematic approach to IKT, including stakeholder mapping, analysis and subsequent development of a country-specific stakeholder engagement strategy that was implemented alongside NCD-focused research activities in the CEBHA+ collaboration in SSA. The teams’ reflections and deliberations showcase the value and challenges of a systematic IKT approach whilst delineating occasions that call for unplanned, ad hoc engagement with decision-makers to enhance the interaction with these stakeholders.
This article complements the ongoing, semi-external mixed methods evaluation of IKT in CEBHA+ (29) by providing a snapshot of how implementing researchers perceive the value of a systematic IKT approach and reflect on stakeholder engagement beyond the planned activities outlined in this approach. The country summaries illustrate that researchers perceived a systematic approach to engaging with decision-makers to be beneficial to their project goals, whilst encountering common challenges to IKT, including decision-maker staff turnover, funding challenges, time constraints, as well as failure to establish some of the intended relationships (19). Importantly, CEBHA+ researchers developed strategies to overcome these barriers, for example by engaging with multiple individuals within a single organization to address institutional staff turnover. Ad hoc engagement presented another avenue of enhancing relationships with decision-makers as it allowed for flexibility and openness to interact with, and respond to decision-makers’ ad hoc demands, which has been identified as an important factor facilitating IKT and collaborative research (19, 27). The COVID-19 pandemic, despite its enormous toll on societies across the globe, was identified as an opportunity to strengthen researcher-decision-maker collaboration, which has been documented for KTPs as well (35).
One important lesson from the CEBHA+ project with respect to developing a systematic IKT approach was the need for comprehensive consultation in the project conceptualization phase, as illustrated by the Ethiopian case. A longer project conceptualization phase, including consultation with diverse stakeholders, can allow for a better overview of the stakeholder landscape, thus helping to identify similar projects and alliances, and subsequently preventing the duplication of work and enabling further collaboration beyond individual research projects or institutions. This observation is in line with a study by Zych et al. (36) in which authors recognized initiation as an important phase of IKT ensuring functional partnerships. Aside from allowing for enough time for this stakeholder mapping and consultation process, the CEBHA+ experience shows that it can be helpful to identify an individual as a guide to the local policy-making or decision-making scene for researchers to enhance their understanding of this sphere. This may be achieved by involving a person who works in both research and health policy sectors and acts as a knowledge broker, spanning boundaries between these two spheres (37).
Overall, even though research teams in all country sites seemed to have been guided by the systematic IKT approach to stakeholder engagement, different needs arose that necessitated a detour from the original plan. These needs were influenced by contextual factors, such as the political climate, needs of stakeholders, and emergence of the COVID-19 pandemic. Another important lesson from this work therefore is the necessity to anticipate flexible, ad hoc engagement at the research proposal and grant writing stage, and for researchers to budget a flexible IKT budget. This should be encouraged by funders, as suggested by our reflections, which showcase that ad hoc engagement can substantially enhance relationships with decision-makers and can subsequently inform updates of the IKT strategy, thus strengthening the systematic approach to decision-maker engagement.
Whilst our work points to the benefits of a systematic IKT approach complemented by more flexible, ad hoc engagement with decision-makers, it also showcases some challenges. Furthermore, to date, the outcomes of IKT in CEBHA+ are limited to improved access to information, enhanced relationships with decision-makers, and some collaborative work on defining research questions, whilst the impact on decision-making is still unclear and may be delineated in the evaluation study (29). It remains to be discussed whether researchers and their IKT partners from policy and practice truly act as equals, as theorized for IKT engagements (18, 22). Overall, it is noteworthy that IKT does not constitute a panacea but comes with its own opportunities and challenges, requiring careful deliberation of whether the project circumstances and scope lend themselves to a systematic IKT approach (23, 32, 38).
Implications
This analysis highlights the need for an initial wide and thorough scoping review of the stakeholder landscape to inform IKT strategies. Additionally, a detailed understanding of IKT approaches and models is needed so that they can be linked to outcomes. Further, a balance between systematic planned IKT and responsive ad hoc efforts is necessary for a more comprehensive and tailored IKT approach. Funders should encourage and support research applications that include IKT and dedicate some non-earmarked funding for both types of IKT approaches to strengthen engagement with decision-makers and increase opportunities for evidence-informed decision-making.
Strengths and Limitations
This work draws mostly on in-team reflections and is therefore inherently shaped by our perspectives. Due to the unique experiences documented in this paper, it might not be possible to generalize the findings. Nevertheless, we felt that the structured country-specific reflections provide valuable insights into the practicalities of doing IKT and that the cross-country comparison allows for lessons learned. These reflections go beyond the individual implementation site and would be interesting for others implementing IKT or considering similar approaches to the co-production of research in other settings.
Conclusion
This paper examined the nuances of the IKT stakeholder engagement process from the researchers’ perspectives and supports existing literature in that contextual factors play a big role in how engagement is carried out. The importance of developing a stakeholder engagement strategy at the initiation of research activities cannot be overemphasized, as was reflected in the experiences of researchers from all CEBHA+ country sites. In fact, consultation with stakeholders should commence while research is still being conceptualized to ensure relevance. This paper highlights that organizational, political and health system factors are constantly shifting and therefore stakeholder engagement plans cannot remain static but rather need to embrace being dynamic in nature. As NCDs become a more prominent issue in SSA and research activities grow, this paper offers insights into the complexities of conducting IKT activities in different contexts. Besides the area of NCDs, there is opportunity for lessons from this paper to guide researchers in other disease areas where progress has been slow. These insights are especially relevant as IKT processes will enhance research uptake to inform public health responses to the current COVID-19 pandemic. Overall, we aim to support the research community in making strides towards evidence-based healthcare.
Data Availability Statement
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding author.
Author Contributions
All authors contributed to conception and design of the study. TM, PD, JO, JN, SN, and NJ contributed insights for the country summaries. TM organized data collection and analyzed country summary templates. TM, KS, and NJ wrote the first draft of the manuscript. TM, KS, NJ, and PD revised the manuscript. All authors contributed to aspects of manuscript revision, and approved the submitted version.
Funding
The authors declare that this study received funding from the German Federal Ministry of Education and Research [BundesministeriumfürBildung und Forschung (BMBF)] (01KA1608) as part of the “Research Networks for Health Innovation in Sub-Saharan Africa” funding initiative. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors wish to extend their gratitude to all those who provided feedback, thoughts, and comments at various points to strengthen this paper: Ann R Akiteng,Bonny EnocBalugaba, Gertrude Chapotera, Hailemichael Getachew, Rawleigh Howe, Kiya Kedir, Tamara Kredo, Lisa Pfadenhauer and Anke Rohwer.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fitd.2021.753192/full#supplementary-material
Abbreviations
AHRI, Armauer Hansen Research Institute; CDIA, Chronic Disease Initiative for Africa; CEBHA+, Collaboration for Evidence-based Healthcare and Public Health in Africa; CVD, Cardiovascular disease; DALYs, Disability-adjusted life years; DoH, Department of Health; EPHI, Ethiopian Public Health Institute; EVIPnet, The Evidence-informed Policy Network; KT, Knowledge Translation; KTA, Knowledge to action; KTP, Knowledge Translation Platform; KUHES, Kamuzu University of Health Sciences; LMICs, Low- and middle-income countries; MOH, Ministry of Health; NCDs, Non-communicable diseases; SSA, Sub Saharan Africa; SURE, Supporting the Use of Research Evidence.
References
1. Forouzanfar MH, Afshin A, Alexander LT, Biryukov S, Brauer M, Cercy K, et al. Global, Regional, and National Comparative Risk Assessment of 79 Behavioural, Environmental and Occupational, and Metabolic Risks or Clusters of Risks, 1990–2015: A Systematic Analysis for the Global Burden of Disease Study 2015. Lancet (2016) 388(10053):1659–724. doi: 10.1016/S0140-6736(16)31679-8
2. Gouda HN, Charlson F, Sorsdahl K, Ahmadzada S, Ferrari AJ, Erskine H, et al. Burden of non-Communicable Diseases in Sub-Saharan Africa, 1990–2017: Results From the Global Burden of Disease Study 2017. Lancet Glob Heal (2019) 7(10):e1375–87. doi: 10.1016/S2214-109X(19)30374-2
3. Forland F, Rehfuess E, Klatser P, Kyamanywa P, Mayanja-Kizza H. Why Evidence Based Approaches are Urgently Needed in Africa. Z Evid Fortbild Qual Gesundhwes (2014) 108(10):606–8. doi: 10.1016/j.zefq.2014.10.025
4. Forland F, Rohwer AC, Klatser P, Boer K, Mayanja-Kizza H. Strengthening Evidence-Based Healthcare in Africa. Evid Based Med (2013) 18(6):204–6. doi: 10.1136/eb-2012-101143
5. Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of Innovations in Service Organizations: Systematic Review and Recommendations. Milbank Q (2004) 82(4):581–629. doi: 10.1111/j.0887-378X.2004.00325.x
6. Oliver K, Innvar S, Lorenc T, Woodman J, Thomas J. A Systematic Review of Barriers to and Facilitators of the Use of Evidence by Policymakers. BMC Health Serv Res (2014) 14(1):2. doi: 10.1186/1472-6963-14-2
7. Lavis J, Lomas J, Hamid M, Sewankambo N. Assessing Country-Level Efforts to Link Research to Action. Bull World Health Organ (2006) 84(8):620–8. doi: 10.2471/BLT.06.030312
8. Greenhalgh T, Sietsewieringa S. Is it Time to Drop the “Knowledge Translation” Metaphor? A Critical Literature Review. J R Soc Med (2011) 104(12):501–9. doi: 10.1258/jrsm.2011.110285
9. Organization WH. The Mexico Statement on Health Research (2004). Available at: http://www.who.int/rpc/summit/agenda/Mexico_Statement-English.pdf.
10. Bucknall T. Bridging the Know-do Gap in Health Care Through Integrated Knowledge Translation. In: Worldviews on Evidence-Based Nursing, vol. 9. United States: Worldviews on Evidence-Based Nursing (2012). p. 193–4.
11. CIHR. Knowledge Translation (2016). Available at: https://cihr-irsc.gc.ca/e/29418.html#2.
12. Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, et al. Lost in Knowledge Translation: Time for a Map? J Contin Educ Health Prof (2006) 26(1):13–24. doi: 10.1002/chp.47
13. Graham ID, Mccutcheon C, Kothari A. Exploring the Frontiers of Research Co-Production: The Integrated Knowledge Translation Research Network Concept Papers. Heal Res Policy Syst (2019) 7:1–4. doi: 10.1186/s12961-019-0501-7
14. Kothari A, McCutcheon C, Graham ID. Defining Integrated Knowledge Translation and Moving Forward: A Response to Recent Commentaries. Int J Heal Policy Manag (2017) 6(5):299–300. doi: 10.15171/ijhpm.2017.15
15. Hoekstra F, Mrklas KJ, Khan M, McKay RC, Vis-Dunbar M, Sibley KM, et al. A Review of Reviews on Principles, Strategies, Outcomes and Impacts of Research Partnerships Approaches: A First Step in Synthesising the Research Partnership Literature. Heal Res Policy Syst (2020) 18(1):1–23. doi: 10.1186/s12961-020-0544-9
16. Nguyen T, Graham ID, Mrklas KJ, Bowen S, Cargo M, Estabrooks CA, et al. How Does Integrated Knowledge Translation (IKT) Compare to Other Collaborative Research Approaches to Generating and Translating Knowledge? Learning From Experts in the Field. Heal Res Policy Syst (2020) 6:1–20. doi: 10.1186/s12961-020-0539-6
17. Kothari A, Wathen CN. A Critical Second Look at Integrated Knowledge Translation A Critical Second Look at Integrated Knowledge Translation. Health Policy (New York) (2012) 109(2):187–91. doi: 10.1016/j.healthpol.2012.11.004
18. Andrews D, Fong G, Hackam D, Li L, Lynam M, Mathews M, et al. Guide to Knowledge Translation Planning at CIHR: Integrated and End-of-Grant Approaches (2012). Available at: http://www.cihr-irsc.gc.ca/e/45321.html.
19. Gagliardi AR, Berta W, Kothari A, Boyko J, Urquhart R. Integrated Knowledge Translation (IKT) in Health Care: A Scoping Review. Implement Sci (2016) 11(1):1–12. doi: 10.1186/s13012-016-0399-1
20. McLean RKD, Graham ID, Tetroe JM, Volmink JA. Translating Research Into Action: An International Study of the Role of Research Funders. Heal Res Policy Syst (2018) 16(1):1–15. doi: 10.1186/s12961-018-0316-y
21. Lawrence L. Integrated Knowledge Translation With Public Health Policy Makers: A Scoping Review Application Des Connaissances Intégrée Auprès Des Décideurs En Santé Publique : Un Examen De La Portée De La Littérature. Healthcare Policy 14(3):55–77. doi: 10.12927/hcpol.2019.25792
22. Kothari A, Wathen CN. A Critical Second Look at Integrated Knowledge Translation. Health Policy (2013) 109(2):187–91. doi: 10.1016/j.healthpol.2012.11.004
23. Oliver K, Kothari A, Mays N. The Dark Side of Coproduction: Do the Costs Outweigh the Benefits for Health Research? Heal Res Policy Syst (2019) 17(1):1–10. doi: 10.1186/s12961-019-0432-3
24. Malla C, Aylward P, Ward P. Knowledge Translation for Public Health in Low- and Middle- Income Countries: A Critical Interpretive Synthesis. Glob Heal Res Policy (2018) 3(1):1–12. doi: 10.1186/s41256-018-0084-9
25. Kalbarczyk A, Rodriguez DC, Mahendradhata Y, Sarker M, Seme A, Majumdar P, et al. Barriers and Facilitators to Knowledge Translation Activities Within Academic Institutions in Low- And Middle-Income Countries. Health Policy Plan (2021) 36(5):728–39. doi: 10.1093/heapol/czaa188
26. Partridge ACR, Mansilla C, Randhawa H, Lavis JN, El-Jardali F, Sewankambo NK. Lessons Learned From Descriptions and Evaluations of Knowledge Translation Platforms Supporting Evidence-Informed Policy-Making in Low- and Middle-Income Countries: A Systematic Review. Heal Res Policy Syst (2020) 18(1):1–22. doi: 10.1186/s12961-020-00626-5
27. Kothari A, Maclean L, Edwards N, Hobbs A. Indicators at the Interface: Managing Policymaker-Researcher Collaboration. Knowl Manag Res Pract (2011) 9(3):203–14. doi: 10.1057/kmrp.2011.16
28. Jessani N, Kennedy C, Bennett S. Enhancing Evidence-Informed Decision Making: Strategies for Engagement Between Public Health Faculty and Policymakers in Kenya. Evid Policy (2017) 13(2):225–53. doi: 10.1332/174426416X14595114153349
29. Pfadenhauer LM, Grath T, Delobelle P, Jessani N, Meerpohl JJ, Rohwer A, et al. Mixed Method Evaluation of the CEBHA+ Integrated Knowledge Translation Approach: A Protocol. Heal Res Policy Syst (2021) 19(1):1–12. doi: 10.1186/s12961-020-00675-w
30. Rehfuess EA, Durão S, Kyamanywa P, Meerpohl JJ, Young T, Rohwer A. Démarche Pour Définir Les Priorités De Recherche À Partir D’éléments Factuels Et Avec L’apport Des Parties Prenantes Dans Les Pays À Revenu Faible Et Intermédiaire. Bull World Health Organ (2016) 94(4):297–305. doi: 10.2471/BLT.15.162966
31. Jessani NS, Hendricks L, Nicol L, Young T. University Curricula in Evidence-Informed Decision Making and Knowledge Translation: Integrating Best Practice, Innovation, and Experience for Effective Teaching and Learning. Front Public Heal (2019) 7(December):1–13. doi: 10.3389/fpubh.2019.00313
32. Kreindler SA. When Coproduction is Unproductive Comment on “Experience of Health Leadership in Partnering With University-Based Researchers in Canada: A Call to ‘Re-Imagine’ Research”. Int J Heal Policy Manag (2020) 9(9):406–8. doi: 10.15171/ijhpm.2019.140
33. Jessani NS, Rohwer A, Schmidt BM, Delobelle P. Integrated Knowledge Translation to Advance Noncommunicable Disease Policy and Practice in South Africa: Application of the Exploration, Preparation, Implementation, and Sustainment (EPIS) Framework. Heal Res Policy Syst (2021) 19(82):1–15. doi: 10.1186/s12961-021-00733-x
34. Niyibizi JB, Nganabashaka JP, Ntawuyirushintege S, Tumusiime D, Umwali G, Rulisa S, et al. Using Citizen Science Within an Integrated Knowledge Translation (IKT) Approach to Explore Cardiovascular Disease Risk Perception in Rwanda. Front Trop Dis (2021) 2: (October):1–11. doi: 10.3389/fitd.2021.752357
35. El-Jardali F, El-Jardali F, El-Jardali F, Bou-Karroum L, Bou-Karroum L, Fadlallah R, et al. Amplifying the Role of Knowledge Translation Platforms in the COVID-19 Pandemic Response. Heal Res Policy Syst (2020) 18(1):1–7. doi: 10.1186/s12961-020-00576-y
36. Zych MM, Berta WB, Gagliardi AR. Initiation is Recognized as a Fundamental Early Phase of Integrated Knowledge Translation (IKT): Qualitative Interviews With Researchers and Research Users in IKT Partnerships. BMC Health Serv Res (2019) 19(1):772. doi: 10.1186/s12913-019-4573-4
37. Langeveld K, Stronks K, Harting J. Use of a Knowledge Broker to Establish Healthy Public Policies in a City District: A Developmental Evaluation. BMC Public Health (2016) 16(1):1–13. doi: 10.1186/s12889-016-2832-4
Keywords: Integrated knowledge translation (IKT), non-communicable diseases (NCD), sub-Saharan Africa (SSA), public health, research co-production, evidence-informed decision-making, road traffic injuries, prevention
Citation: Mpando TL, Sell K, Delobelle P, Osuret J, Niyibizi JB, Ntawuyirushintege S, Geremew B and Jessani NS (2021) Integrated Knowledge Translation in Non-Communicable Disease Research in Sub-Saharan Africa: A Comparison of Systematic and Ad Hoc Stakeholder Engagement. Front. Trop. Dis 2:753192. doi: 10.3389/fitd.2021.753192
Received: 04 August 2021; Accepted: 15 November 2021;
Published: 07 December 2021.
Edited by:
Yodi Mahendradhata, Gadjah Mada University, IndonesiaReviewed by:
Temmy Sunyoto, Médecins Sans Frontières, BelgiumFekri Dureab, Akkon College of Human Sciences, Germany
Copyright © 2021 Mpando, Sell, Delobelle, Osuret, Niyibizi, Ntawuyirushintege, Geremew and Jessani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Talitha L. Mpando, talithampando@gmail.com
†These authors share first authorship
 Talitha L. Mpando
Talitha L. Mpando Kerstin Sell
Kerstin Sell Peter Delobelle
Peter Delobelle Jimmy Osuret
Jimmy Osuret Jean Berchmans Niyibizi
Jean Berchmans Niyibizi Seleman Ntawuyirushintege
Seleman Ntawuyirushintege Bezinash Geremew
Bezinash Geremew Nasreen S. Jessani
Nasreen S. Jessani