Risk factors for falls among community-dwelling older adults: A systematic review and meta-analysis
- 1School of Nursing, Weifang University of Science and Technology, Weifang, Shandong, China
- 2Nursing Department, Peking University Shenzhen Hospital, Shenzhen, China
- 3Wuxi Mental Health Center, Wuxi, Jiangsu, China
- 4Department of Neurology, Shandong Guoxin Senior Care Group Laiwu Central Hospital, Jinan, China
Background and objective: The prevalence of falls among older adults living in the community is ~30% each year. The impacts of falls are not only confined to the individual but also affect families and the community. Injury from a fall also imposes a heavy financial burden on patients and their families. Currently, there are different reports on the risk factors for falls among older adults in the community. A retrospective analysis was used in this study to identify risk factors for falls in community-dwelling older adults. This research aimed to collect published studies to find risk factors for falls in community-dwelling older adults.
Methods: We searched for literature from the founding of PubMed, EMBASE, the Cochrane Library, the Web of Science, the China National Knowledge Infrastructure (CNKI), the China Science and Technology Periodicals Database (VIP), and the Wanfang database until September 2022. The studies were selected using inclusion and exclusion criteria. We collected information from relevant studies to compare the impact of potential risk factors such as age, female gender, fear of falling, history of falls, unclear vision, depression, and balance disorder on falls among community-dwelling older adults.
Results: A total of 31 studies were included with 70,868 community seniors. A significant risk factor for falls in the community of older adults was dementia (2.01, 95% CI: 1.41–2.86), age (1.15, 95% CI: 1.09–1.22), female gender (1.52, 95% CI: 1.27–1.81), fear of falling (2.82, 95% CI: 1.68–4.74), history of falls (3.22, 95% CI: 1.98–5.23), vision unclear (1.56, 95% CI: 1.29–1.89), depression (1.23, 95% CI: 1.10–1.37), and balance disorder (3.00, 95% CI: 2.05–4.39).
Conclusion: This study provides preliminary evidence that falls among community-dwelling older adults are associated with factors such as age, female gender, fear of falling, history of falls, unclear vision, depression, and balance disorders. The results of this research may help improve clinician awareness, risk stratification, and fall prevention among community-dwelling older adults.
Systematic review registration: identifier INPLASY2022120080.
Introduction
With the advancement of society and medical and health standards, the older adults of the world (60 and older) now account for 12.3% of the total population. The average life expectancy has risen to 71 years (1). In 2018, China had 249 million people aged 60 and older, accounting for 17.9% of the total population, and approximately 167 million people aged 65 and older, accounting for 11.9% (2). The community serves as a place for older adults to live and participate in activities. According to the survey, roughly 84.5% of the older adults in the community choose a home or a combination of the community and the house for older adults.
Consequently, older adults are more inclined to fall inside the community and even at home (3). In community settings, the incidence of falls for men and women aged 65 and older ranges from 21 to 23% and from 43 to 44%, respectively (4). The community serves as a place for older adults to live and participate in activities. According to a survey, roughly 84.5% of the older adults in the community choose a home or a combination of the community and the house for older adults. Consequently, older adults are more inclined to fall inside the community and even at home (3). In Community Settings, the incidence of falls among men and women aged 65 and older was 21–23% and 43–44%, respectively (4). Falls are a leading cause of injury, related disability, and premature death among older adults (5). Injuries vary in severity, with 40–60% of falls resulting in severe lacerations, non-vertebral fractures, and traumatic head injuries (6). Prolonged lying after a fall can lead to dehydration, rhabdomyolysis, pressure sores, and pneumonia, all of which can increase hospital stays (7). Falls are also associated with successive radial, humerus, vertebral, and hip fractures (8). Approximately 95% of hip fractures are caused by falls (9). A previous study estimated that 10–20% of patients with hip fractures are admitted to nursing homes, and 20% die within 12 months (10, 11). In addition, falling can cause not only physical damage but also psychological damage (12). Falling can lead to a “fear” of falling. This “fear” can appear in 20–40% of people who fall, causing weakness and leading to a downward spiral in physical health that leads to functional decline, social isolation, and depression (12). The impacts of falls are not confined to the individual but affect families and the community. Injury from a fall also imposes a heavy financial burden on patients and their families. Fall injuries cost RMB ¥70 billion ($10 billion) in the United States and RMB ¥3.99 billion ($570 million) annually in the Netherlands, and per capita direct economic burden of China due to falls is 3,800 yuan (13–15). Falls in older adults can also result in disability, reduced quality of life, loss of independence, and hospitalization.
The risk of falls increases with the number of risk factors in each individual (16). According to the research, falls in older adults are multifactorial events involving internal (patient-related), external (environment-related), and behavioral (activity-related) aspects (17, 18). However, the sample size of each study was small, and the reported risk factors were inconsistent, so nursing professionals could not determine the risk factors for falls among older adults in the community. The meta-analysis reported pain, weakness, gait problems, dizziness, and age as risk factors for falls among older adults in the community (19–22). The reports on the relationship between poor vision and fall risk are inconsistent and controversial (23, 24). In recent years, some studies reported on the impact of risk factors such as dementia, bone and joint disease, and depression on falls of older adults in the community (25–29). However, it has yet to attract the attention of nursing professionals. To better prevent older adults from falling in the community, it is necessary to have a more comprehensive understanding of the risk factors leading to falls among older adults. This study aimed to systematically review the risk factors for falls among older adults in the community to comprehensively and systematically understand the risk factors among older adults and provide the basis for formulating relevant intervention measures.
Methods
A meta-analysis was conducted in adherence to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (30).
Data source collection
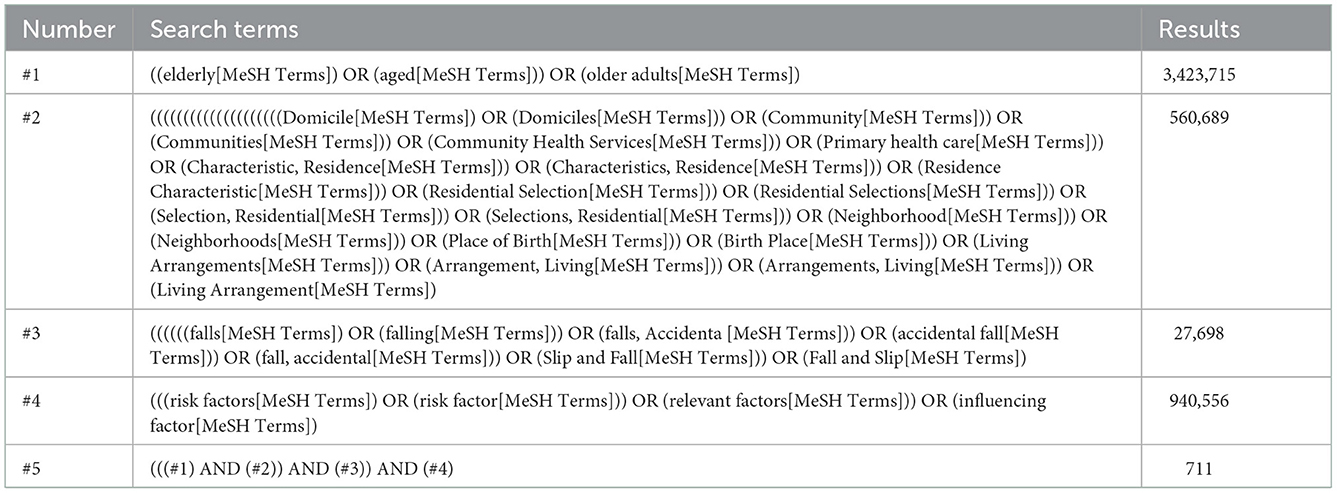
In PubMed, Web of Science, Embase, Cochrane Library, China National Knowledge Infrastructure (CNKI), Wanfang Data database, and Chinese Periodical database (VIP), a literature search was conducted to identify studies published as of September 2022 associated with risk factors for falls in older adults in the community. The search terms included “Elderly OR Aged or Older adults” and “Domicile OR Domiciles OR Community OR Communities OR Community Health Services OR Primary health care OR Characteristic, Residence OR Characteristics, Residence OR Residence Characteristic OR Residential Selection OR Residential Selections OR Selection, Residential OR Selections, Residential OR Neighborhood OR Neighborhoods OR Place of Birth OR Birth Place OR Living Arrangements OR Arrangement, Living OR Arrangements, Living OR Living Arrangement” and “Falls OR Falling OR Falls, Accidental OR Accidental fall OR fall, accidental OR Slip and Fall OR Fall and Slip” and “Risk factors OR Risk factor OR Relevant factors OR Influencing factor.” Table 1 shows the search strategy in the PubMed database. The complete search strategies for all databases are available in Supplementary material 1.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) the study was an observational study that could be a cross-sectional, cohort, or case-control study; (2) the older adults in the community were in fact the research participants; (3) data on fall risk factors in community-dwelling older adults with 95% confidence intervals (95% CI) or odds ratios were some of the outcome types (ORs); (4) the study which met the fall definition: an unexpected event in which the participant rests on the ground, floor, or lower level; and (5) types of comparison: comparisons of fall risk factors among community-dwelling older adults.
The following types of records were excluded: (1) replicated research data; (2) incomplete data; and (3) non-original studies (conference abstracts, editorials, letters, reviews, meta-analyses, commentaries, or case reports).
Data extraction
Two researchers independently screened the literature and extracted data according to the inclusion and exclusion criteria. In disagreements, the two parties discussed and resolved them or consulted experts. Data extraction contents included author, year, study type, number of cases and control groups, relevant risk factors, and so on.
Statistical analysis
Review Manager 5.3 was used for statistical analysis. I2> 50% or a P < 0.1 was considered significant for heterogeneity (31). For homogeneous data (I2 < 50% or P > 0.05), the fixed-effects model was used to calculate the 95% CI and pooled ORs. The random-effects model was used in all other cases. Sensitivity analysis was carried out by eliminating one study at a time. When at least three study samples examined the same outcome measure, data were pooled and analyzed in random-effects meta-analysis models (32).
Quality assessment
To evaluate the quality of case-control studies and cohort studies, we used Quality Assessment Scale for Non-Experimental Studies (33), based on prospective cohort studies and retrospective case-control studies, using an adapted Newcastle-Ottawa Scale (34) (the Newcastle-Ottawa Scale, NOS), including study population selection (comparability, exposure, or outcomes); cross-sectional studies were assessed using the AHRQ-recommended quality evaluation criteria (35).
Results
Study selection
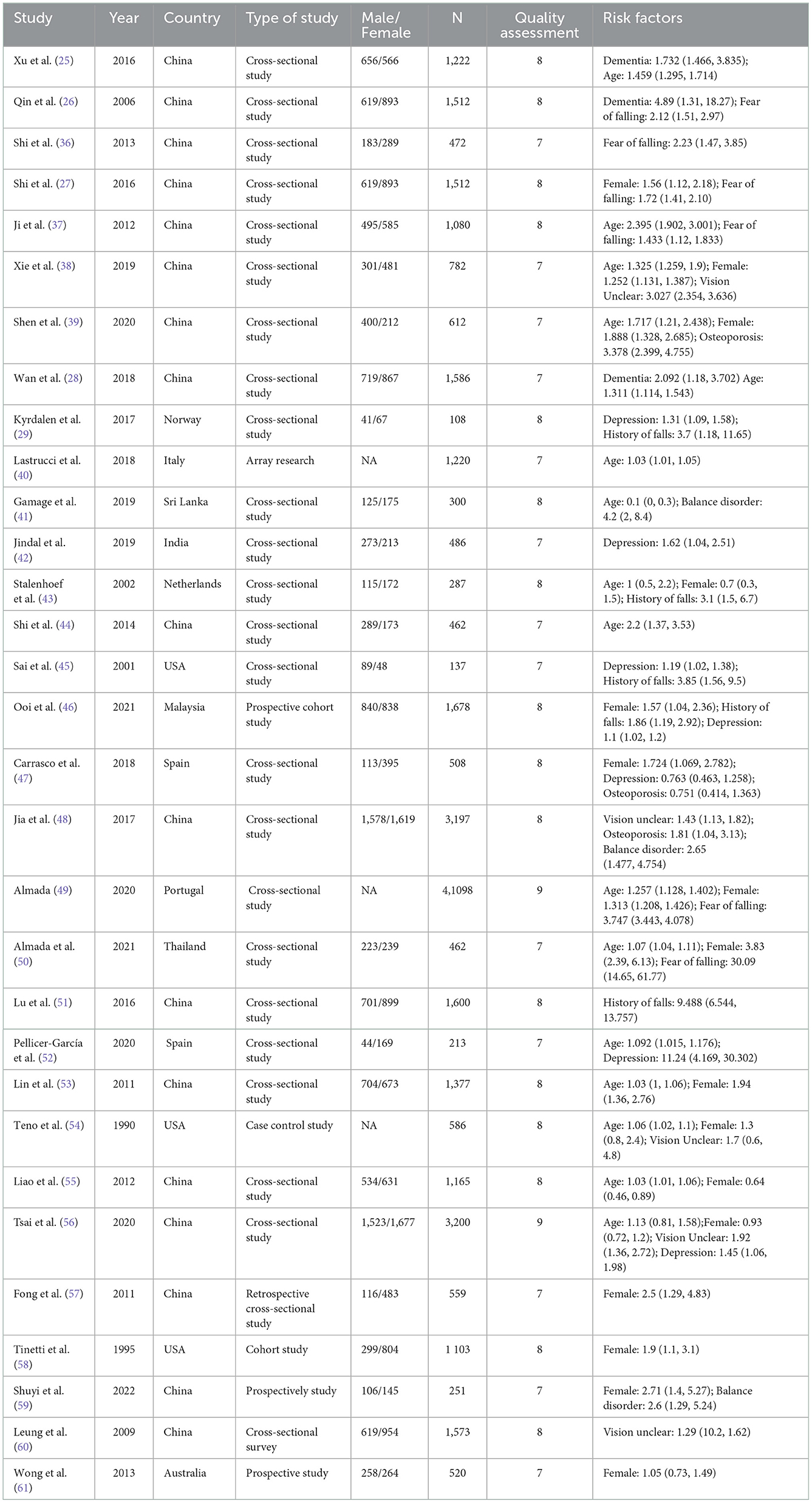
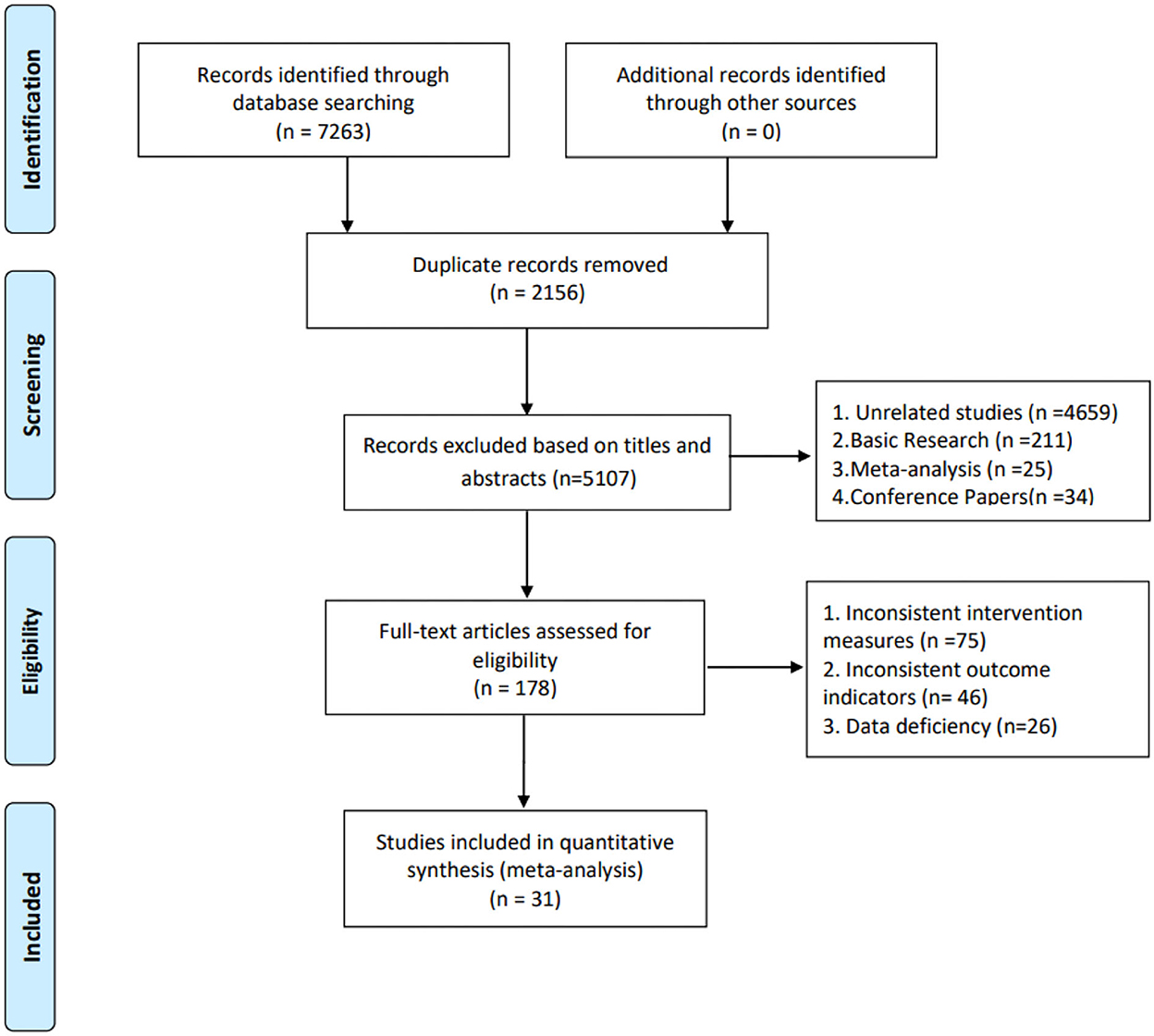
Through the database, a total of 7,263 related literature were retrieved and a total of 2,156 repeated literature were removed. After further reading the full-text, 5,076 pieces of literature were eliminated and 31 types were finally included (25–29, 36–61), totaling 70,868 study subjects. The study and characteristics of the participants are shown in Table 2.
Characteristics of the studies
The included studies were published from 1995 to 2022: one study in Norway, one in Italy, one in Sri Lanka, one in India, one in the Netherlands, three in the USA, two in Spain, one in Australia, one in Thailand, one in Portugal, one in Malaysia, and seventeen in China. The sample sizes included in the study ranged from 251 to 41,098. The flow diagram is shown in Figure 1.
Falls risk factors
Dementia
The relationship between dementia and the risk of falls in the community was reported in three studies. Dementia significantly impacts falls (2.01, 95% CI: 1.41–2.86, Z = 3.86, p = 0.0001), and heterogeneity is negligible (I2= 6%) (Figure 2A).
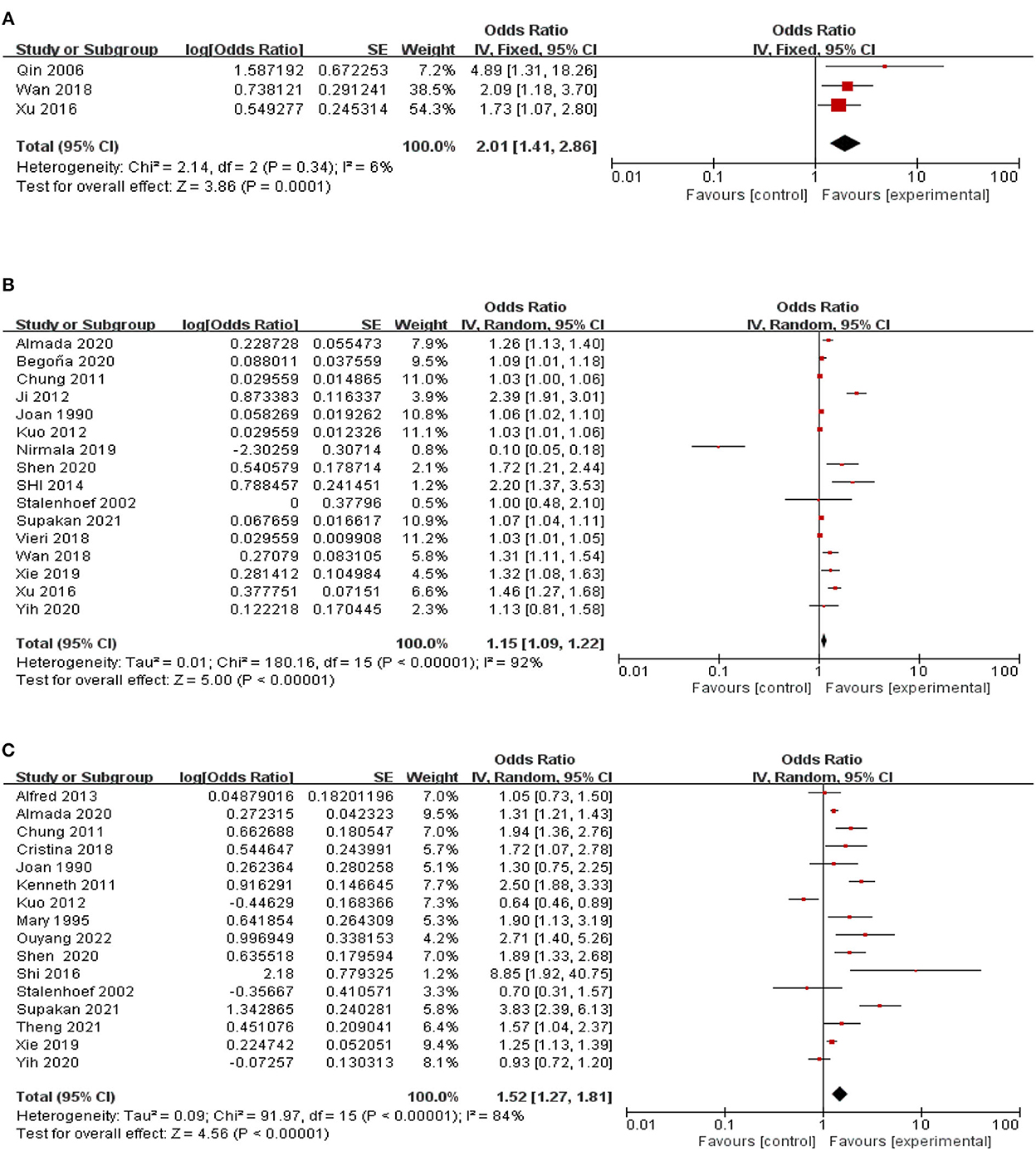
Figure 2. A forest plot for the association between falls among community-dwelling older adults. (A) Dementia. (B) Age. (C) Female.
Age
A link between age and the risk of falls in the community was reported in 16 studies. Age significantly affected falls (1.15, 95% CI: 1.09–1.22, Z = 5, p < 0.00001). There is a high degree of heterogeneity (I2= 92%) between studies. Therefore, these studies were grouped by region, type of study, and gender, but the results were still highly heterogeneous (Figure 2B).
Female gender
Associations between women and the risk of falls in their communities are reported in 16 studies. Older women had a significant impact on falls (1.52, 95% CI: 1.27–1.81, Z = 4.56, p < 0.00001), and heterogeneity was negligible (I2= 84%). There was a high degree of heterogeneity between studies. Therefore, these studies were grouped by region and type of study, but the results were still highly heterogeneous (Figure 2C).
Fear of falling
The relationship between fear of falling and the risk of falls in the community was reported in six studies. Fear of falling has a significant impact on falls of older adults in the community (2.82, 95% CI: 1.68–4.74, Z = 3.91, p < 0.0001), and there is a high degree of heterogeneity between studies (I2= 97%). Therefore, these studies are grouped by region, research type, and gender, but the results are still highly heterogeneous (Figure 3A).
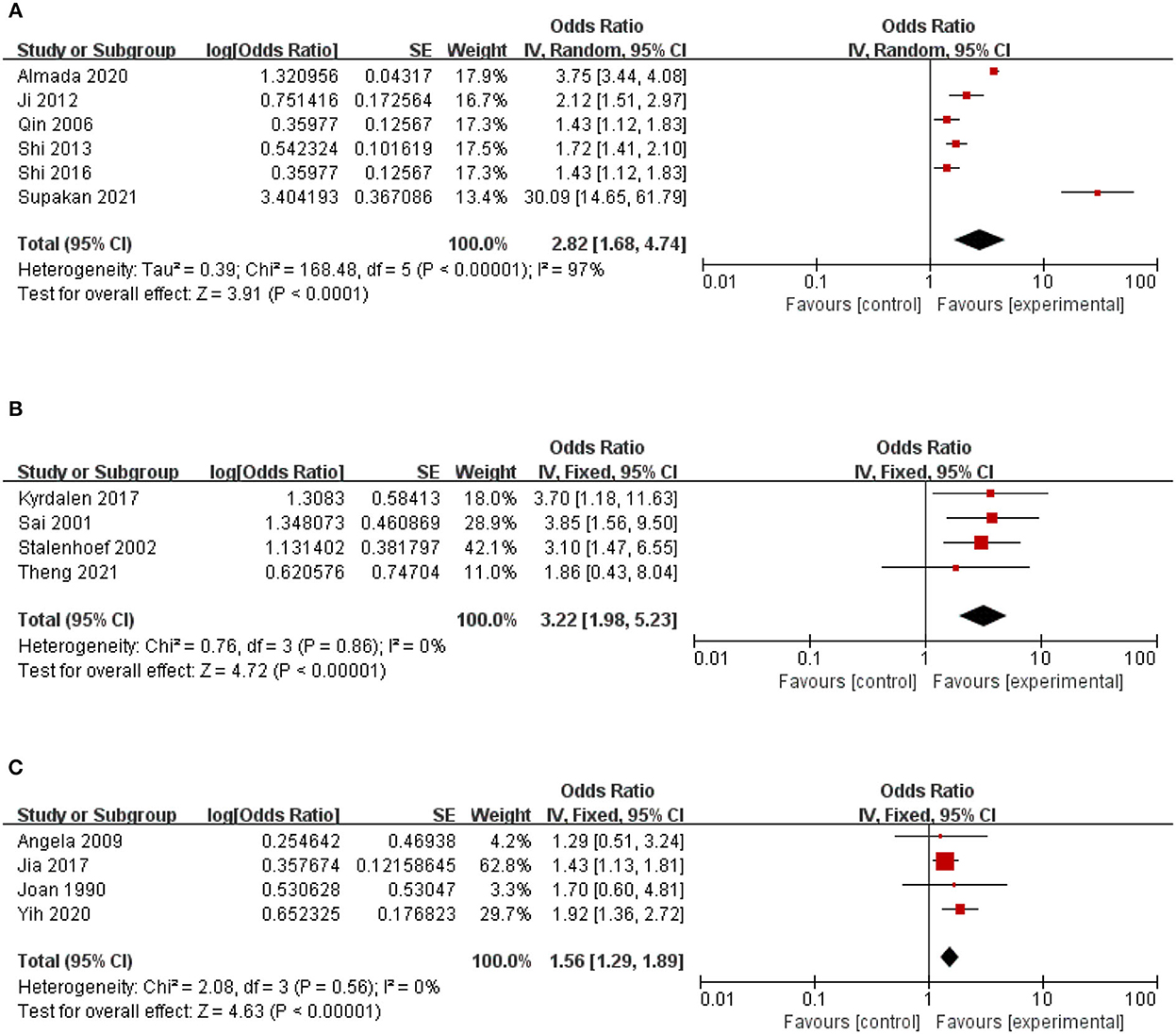
Figure 3. A forest plot for the association between falls among community-dwelling older adults. (A) Fear of falling. (B) History of falls. (C) Vision Unclear.
History of falls
The relationship between past falls and community fall risk was reported in five studies. The study had direct heterogeneity (I2= 68%). After sensitivity analysis, the study of Lu et al. (51) was excluded. History of falls significantly impacts the falls of older adults in the community (3.22, 95% CI: 1.98–5.23, Z = 4.72, p < 0.0001, I2= 0) (Figure 2B).
Vision unclear
The relationship between visual impairment and fall risk in the community was reported in five studies. The study had direct heterogeneity (I2= 68%). After sensitivity analysis, the study of Xie et al. (38) was excluded. The study found that visual impairment significantly impacted falls of older adults in the community (1.56, 95% CI: 1.29–1.89, Z = 4.63, p < 0.00001, I2= 0) (Figure 2C).
Depression
The relationship between depression and community fall risk was reported in seven studies. The study had heterogeneity (I2=70%). After sensitivity analysis, the study of Begoña et al. (52) was excluded. The study found that visual impairment significantly impacted falls of older adults in the community (1.23, 95% CI: 1.10–1.37, Z = 3.66, p = 0.0003, I2= 12%) (Figure 4A).
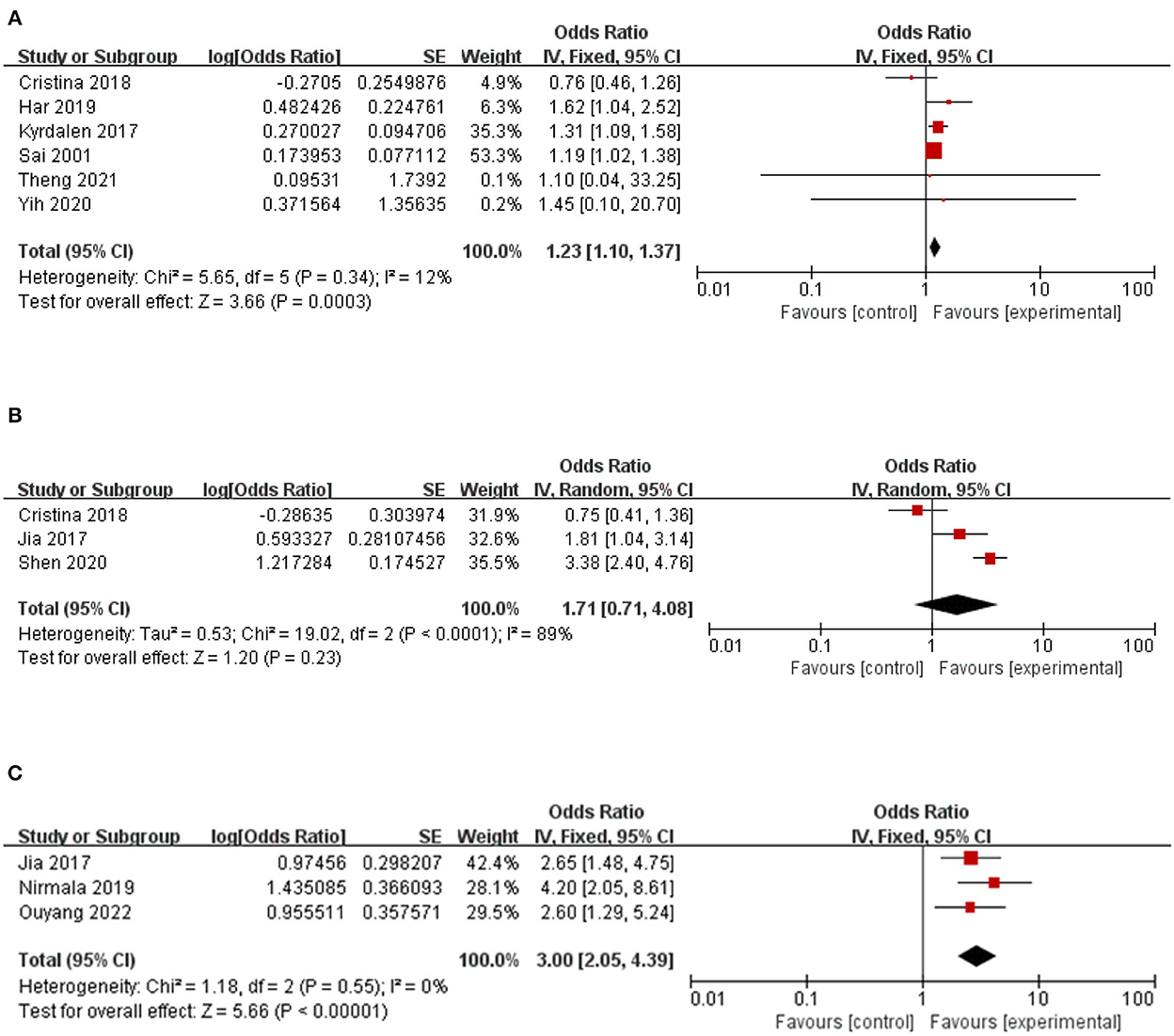
Figure 4. A forest plot for the association between falls among community-dwelling older adults. (A) Depression. (B) Osteoporosis. (C) Balance disorder.
Osteoporosis
The association between osteoporosis and the risk of falls among older people in the community was reported in three studies. Osteoporosis has no significant impact on the fall risk of middle-aged and older adults in the community (1.71, 95% CI: 0.71–4.08, Z = 1.20, p = 0.23), with high heterogeneity (I2= 89%) (Figure 4B).
Balance disorder
The relationship between balance disorders and the risk of falls in the community was reported in three studies. Balance significantly impacts falls (3.00, 95% CI: 2.05–4.39, Z = 5.66, p < 0.00001, I2= 0) (Figure 4C).
Sensitivity analysis
In the analysis of visual impairment, history of falls, and depression, we conducted a sensitivity analysis by excluding each study one by one to explore whether a study significantly affected the results or contributed to heterogeneity. We found that the results were not affected by any research, and our meta-analysis was relatively robust. However, after excluding the studies of Xie et al. (38), Lu et al. (51), and Begoña et al. (52) the heterogeneity was significantly reduced, indicating that these two studies were the primary sources of the heterogeneity of visual impairment and depression.
Bias assessment
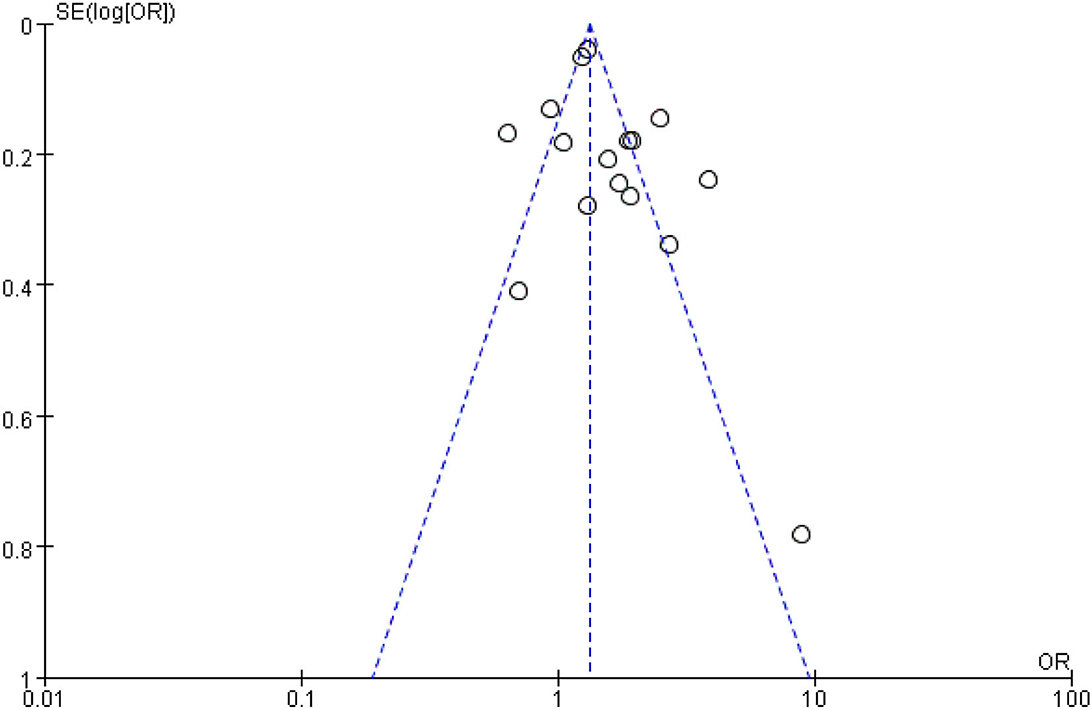
Finally, funnel plots were constructed to qualitatively analyze the publication bias among the included studies. Fall risk factors for women and older people in the community were used as examples. The funnel diagram shows a symmetrical distribution without apparent publishing deviation (Figure 5).
Discussion
An analysis of the included studies found that the risk factors for falls among older adults in the community are fear of falling, age, female gender, balance disorder, dementia, depression, previous falls, and unclear vision. This study found that fear of falling was closely related to falls among older adults in the community, which was consistent with the results of Sousa et al. (62). Studies showed that fear of falling and other fall-related psychological problems are common among older adults in the community and nursing homes after falls (63). The fear of falling often reduces activities in older adults, which weakens muscle strength and increases the risk of falling, increasing the fear of losing and forming a vicious circle (64). A research report pointed out that the fear of falling among older adults in the Chinese community is 41–5%, and the incidence of fear of loss among older adults in older adult care institutions is 79.4% (65, 66). According to this study, older adults should receive proper psychological intervention following a fall to reduce the psychological fear of losing and avoid falling again. This study identified age as a risk factor for falls in older people. The higher the age, the greater the risk of falling. This result is consistent with Sousa et al. (62) and Deandrea et al. (19). Because of the potential for the age-related decline, position senses, hearing, visual, and physical functions of older adults will all deteriorate. Moreover, older adults are frequently accompanied by a variety of chronic diseases. The presence of chronic diseases will impair the cognitive and balance abilities of older adults, increasing the risk of falls in older adults. Therefore, it is reasonable to believe that aging and falls among more senior adults in the community are mutually causal.
This study found balance disorders to be a risk factor for falls in community-dwelling older adults. This result was not reported in the studies of Sousa et al. (62), Deandrea et al. (19), and Chantanachai et al. (32). According to King et al., the age of 60 is a watershed in balance ability. After 60 years, the balance ability of older adults declines by 16% every 10 years, and the risk of falls also increases (67). With the increase in age, the aging of the bodies of older adults leads to weakened muscle strength and decreased joint flexibility, resulting in damage to the balance function, which will directly affect the mobility of older adults. Older adults with good balance ability have strong lower extremity muscles, high physical sensitivity, quick responses, and a low probability of falling.
In contrast, older adults with poor balance experience lower extremity weakness and reduced physical sensitivity, which increases the risk of falls (68). In addition, this study found that depression is a risk factor for falls in older adults in the community. Considering that it may be related to unstable emotions, depression weakens the attention of older adults, resulting in a decline in their ability to respond to and perceive environmental risk factors, increasing the risk of falling.
In addition, this study identified a history of falls, visual impairment, and dementia as risk factors for falls among older adults in the community. A history of falls is a risk factor among older adults in the community, and this result has not been reported in Chantanachai et al. (32) study. When comparing the older adult patients who fell in the past 6 months with the matched group who did not fall, 57% of the falls were unable to walk at the fastest speed, with short steps and small lateral swings (69). Compared with non-falling people, the variability of kinematic measurement in falling people increases (69). The changes in these actions reflect the limitation of mobility and increase the risk of falls in older adults. Older adults with a history of falls are also associated with higher symptoms of depression and anxiety (70), thus increasing the risk of falls in older adults. This study confirms that older adults with a visual impairment are 1.56 times more likely to fall than those without a visual impairment. This result is not reported in Jehu et al. (22) and Stubbs et al. (21). In the case of insufficient visual input, the ability to balance control and obstacle avoidance will be impaired due to misjudgment of distance and misunderstanding of spatial information. It has been found that impaired depth perception is one of the essential visual risk factors for older adults living in communities to fall repeatedly (71). Postural stability is a complex skill that depends on the coordination of the motor and sensory systems to perceive environmental stimuli and respond to disturbances to control body movements (72, 73). Dementia can reduce cognitive ability and gait stability, affect the ability of older adults to cope with the external environment, and increase the risk of falls in older adults.
Our findings found no association between osteoporosis and falls in older adults in the community. However, older adult patients with osteoporosis should be watched with alertness as it has been proven to be an essential risk factor for falls among older adults in the community (47). In older adult patients, calcium loss is high, and the decline of muscle content, strength, and function can significantly increase the risk of falls and fractures. Some countries, such as the United States, recommend screening for osteoporosis for all women ≥ 65 years of age (74). Therefore, we need to be more alert to osteoporosis. Similarly, the results of this meta-analysis showed that osteoporosis is not a risk factor for falls among older adults in the community, which may be because only a small sample study was included.
In conclusion, this systematic review and meta-analysis study provides strong evidence for the risk factors for falls among older adults in the community. We further confirmed that age, female gender, fear of falling, depression, visual impairment, dementia, and balance disorder increase the risk of falls for older adults in the community. In addition, the results of this study will help formulate the best practice guide for preventing falls among older adults in the community and provide a basis for establishing a prediction model.
Limitations
There were some limitations in the present study. First, the articles included in this study were meta-integrated, but some results included only 2–3 pieces, which may have resulted in selection bias. Second, individual heterogeneity exists in the populations included in the literature of this study regarding regions, races, and socioeconomic levels. Third, because few studies involve some risk factors, meta-analysis cannot be performed, and more large-scale studies are required. Therefore, it is necessary to conduct more carefully designed studies on the potential fall risk factors in community-dwelling older adults.
Conclusion
In conclusion, this meta-analysis identified some risk factors for community-dwelling older adults and provided a reference for preventing falls. However, more strictly designed studies are needed to substantiate our findings and identify practical measures for preventing falls.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
YL and LH designed the study. RX and YY acquired, analyzed, and interpreted the data. XD, YL, YY, and HZ revised the manuscript. HZ plays the role of inspection, assistance and drafting the work or revising it critically for important intellectual content in the modification phase of the article. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Sanming Project of Medicine in Shenzhen (No. SZSM202111013).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.1019094/full#supplementary-material
References
2. National Health Commission. Healthy China Action (2019-2030) [EB/OL(2019-07-15)]. (2020). Available online at: http://www.gov.cn/xinwen/2019-07/15/content_5409694.htm
3. Li F, Qin K, Zhang P, Yuan J, Luo Yh. An empirical study on the demand and influencing factors of health care services for the elderly. Health Econ Res. (2019) 36:42–6.
5. Tinetti ME, Williams CS. The effect of falls and fall injuries on functioning in community-dwelling older persons. J Gerontol A Biol Sci Med Sci. (1998) 53:M112–9. doi: 10.1093/gerona/53A.2.M112
6. Masud T, Morris RO. Epidemiology of falls. Age Ageing. (2001) 30:3–7. doi: 10.1093/ageing/30.suppl_4.3
7. Fleming J, Brayne C. Inability to get up after falling, subsequent time on floor, and summoning help: prospective cohort study in people over 90. BMJ. (2008) 337:a2227. doi: 10.1136/bmj.a2227
8. Melton LJ 3rd, Amin S. Is there a specific fracture ‘cascade'? Bonekey Rep. (2012) 2:367. doi: 10.1038/bonekey.2013.101
9. Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. (2002) 359:1761–7. doi: 10.1016/S0140-6736(02)08657-9
10. Sattui SE, Saag KG. Fracture mortality: associations with epidemiology and osteoporosis treatment. Nat Rev Endocrinol. (2014) 10:592–602. doi: 10.1038/nrendo.2014.125
11. Vochteloo AJH, van Vliet-Koppert ST, Maier AB, Tuinebreijer WE, Röling ML, de Vries MR, et al. Risk factors for failure to return to the pre-fracture place of residence after hip fracture: a prospective longitudinal study of 444 patients. Arch Orthop Trauma Surg. (2012) 132:823–30. doi: 10.1007/s00402-012-1469-8
12. Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing. (2008) 37:19–24. doi: 10.1093/ageing/afm169
13. Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical costs of fatal and non- fatal falls in older adults. J Am Geriatr Soc. (2018) 66:693–8. doi: 10.1111/jgs.15304
14. Hartholt KA, van Beeck EF, Polinder S, van der Velde N, van Lieshout EMM, Panneman MJM, et al. Societal consequences of falls in the older population: injuries, healthcare costs, and long-term reduced quality of life. J Trauma. (2011) 71:748–53. doi: 10.1097/TA.0b013e3181f6f5e5
15. Peng K, Lei l, Feng Np, Zeng Nb, Li H, Zhou Hb. The prevalence of falls and direct diseases among the elderly in Shenzhen burden research chronic disease prevention and control in China. Prevention and control of chronic diseases in China. (2016) 24:122–4. doi: 10.16386/j.cjpccd.issn.1004-6194.2016.02.011
16. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. (2013) 75:51–61. doi: 10.1016/j.maturitas.2013.02.009
17. Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. (1988) 319:1701–7. doi: 10.1056/NEJM198812293192604
18. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
19. Deandrea S, Lucenteforte E, Bravi F, Foschi R, Vecchia CL, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. (2010) 21:658–68. doi: 10.1097/EDE.0b013e3181e89905
20. Cheng MH, Chang SF. Frailty as a risk factor for falls among community dwelling people: evidence from a meta-analysis. J Nurs Scholarsh. (2017) 49:529–36. doi: 10.1111/jnu.12322
21. Stubbs B, Binnekade T, Eggermont L, Sepehry AA, Patchay S, Schofield P. Pain and the risk for falls in community-dwelling older adults: systematic review and meta-analysis. Arch Phys Med Rehabil. (2014) 95:175–87.e9. doi: 10.1016/j.apmr.2013.08.241
22. Jehu DA, Davis JC, Falck RS, Bennett KJ, Tai D, Souza MF, et al. Risk factors for recurrent falls in older adults: a systematic review with meta-analysis. Maturitas. (2021) 144:23–8. doi: 10.1016/j.maturitas.2020.10.021
23. de Boer MR, Pluijm SM, Lips P, Moll AC, Völker-Dieben HJ, Deeg DJ, et al. Different aspects of visual impairment as risk factors for falls and fractures in older men and women. J Bone Miner Res. (2004) 19:1539–47. doi: 10.1359/JBMR.040504
24. Lord SR, Ward JA, Williams P, Anstey KJ. Physiological factors associated with falls in older community-dwelling women. J Am Geriatr Soc. (1994) 42:1110–7. doi: 10.1111/j.1532-5415.1994.tb06218.x
25. Xu W, Lv ZP, Hu Cy, Yang C, Fu M. Analysis of risk factors for falls in the elderly in the community. Guangxi Med. (2016) 38:1568–70+7.
26. Zhou B-Y, Shi J, Yu P-L. Analysis of risk factors for falls among 1512 older people in urban communities in Beijing. Chin J Epidemiol. (2006) 7:579–82.
27. Shi J, Tao Yk, Zhou BY, Duan CB, Zhang CF, Qin ZH. A follow-up study on the incidence and related factors of falls among the elderly in the Beijing community China. Geriatrics J. (2016) 35:551–5.
28. Wan YL, Xia P. Analysis of factors related to falls in the elderly in the community and research on the effect of the intervention China. Public Health Admin. (2018) 34:694–7. doi: 10.19568/j.cnki.23-1318.2018.05.033
29. Kyrdalen IL, Thingstad P, Sandvik L, Ormstad H. Associations between gait speed and well-known fall risk factors among community-dwelling older adults. Physiother Res Int. (2019) 24:e1743. doi: 10.1002/pri.1743
30. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
31. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
32. Chantanachai T, Sturnieks DL, Lord SR, Payne N, Webster L, Taylor ME. Risk factors for falls in older people with cognitive impairment living in the community: systematic review and meta-analysis. Ageing Res Rev. (2021) 71:101452. doi: 10.1016/j.arr.2021.101452
33. Kawatani Y, Nakamura Y, Hayashi Y, Taneichi T, Ito Y, Kurobe H, et al. Development of delirium in the intensive care unit in patients after endovascular aortic repair: a retrospective evaluation of the prevalence and risk factors. Crit Care Res Pract. (2015) 2015:405817. doi: 10.1155/2015/405817
34. Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA. Healthcare infection control practices advisory committee. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. (2010) 31:319–26. doi: 10.1086/651091
35. Zeng XL, Liu X, Chen X, Leng XT. Meta-analysis series four: quality assessment tools for observational studies. Chin J Evid Based Cardiovasc Med. (2012) 4:297–9.
36. Shi Jing TZhou B, et al. A follow-up study on the incidence of multiple falls and related factors among the elderly in a community in Beijing. Chin J Epidemiol. (2013) 34:967–9.
37. Ji Y, Li L, Chen W. Status and risk factors of falls among the elderly in the community in Beijing. Chin J Dis Control. (2012) 16:22–4.
38. Xie N, Yang Y, Wei Q. Analysis of the status and influencing factors of falls among the elderly aged 60 and over in Chengdu. Pract Preven Med. (2019) 26:42–5+58.
39. Shen Xiaojun CXun X, et al. Analysis of the status and risk factors of falls in the elderly over 60 in Laoximen Street Community, Shanghai China. J Clin Health. (2020) 23:770–3.
40. Lastrucci V, Lorini C, Rinaldi G, Bonaccorsi G. Identification of fall predictors in the active elderly population from the routine medical records of general practitioners. Prim Health Care Res Dev. (2018) 19:131–9. doi: 10.1017/S146342361700055X
41. Gamage N, Rathnayake N, Alwis G. Prevalence and associated risk factors of falls among rural community-dwelling older people: a cross-sectional study from Southern Sri Lanka. Curr Gerontol Geriatr Res. (2019) 2019:2370796. doi: 10.1155/2019/2370796
42. Jindal HA, Duggal M, Jamir L, Sharma D, Kankaria A, Rohilla L, et al. Mental health and environmental factors associated with falls in the elderly in North India: a naturalistic community study. Asian J Psychiatr. (2019) 39:17–21. doi: 10.1016/j.ajp.2018.11.013
43. Stalenhoef PA, Diederiks JPM, Knottnerus JA, Kester ADM, Crebolder HFJM. A risk model for predicting recurrent falls in community-dwelling elderly: a prospective cohort study. J Clin Epidemiol. (2002) 55:1088–94. doi: 10.1016/S0895-4356(02)00502-4
44. Shi J, Zhou BY, Tao YK, Yu PL, Zhang CF, Qin ZH, et al. Incidence and associated factors for single and recurrent falls among the elderly in an urban community of Beijing. Biomed Environ Sci. (2014) 27:939–49.
45. Sai AJ, Gallagher JC, Smith LM, Logsdon S. Fall predictors in the community dwelling elderly: a cross sectional and prospective cohort study. J Musculoskelet Neuronal Interact. (2010) 10:142–50.
46. Ooi TC, Singh DKA, Shahar S, Rajab NF, Vanoh D, Sharif R, et al. Incidence and multidimensional predictors of occasional and recurrent falls among Malaysian community-dwelling older persons. BMC Geriatr. (2021) 21:154. doi: 10.1186/s12877-021-02103-2
47. Carrasco C, Tomas-Carus P, Bravo J, Pereira C, Mendes F. Understanding fall risk factors in community-dwelling older adults: a cross-sectional study. Int J Older People Nurs. (2020) 15:e12294. doi: 10.1111/opn.12294
48. Butler J, Jayson GG, Swallow AJ. The reaction between the superoxide anion radical and cytochrome c. Biochim Biophys Acta. (1975) 408:215–22. doi: 10.1016/0005-2728(75)90124-3
49. Jia Chunyuan ZDuan L, et al. Analysis of risk factors of falls among the elderly in northern China Chinese. J Geriat Healthcare Med. (2017) 15:21–5.
50. Almada M, Brochado P, Portela D, Midão L, Costa E. Prevalence of falls and associated factors among community-dwelling older adults: a cross-sectional study. J Frailty Aging. (2021) 10:10–6. doi: 10.14283/jfa.2020.44
51. Lu Q, Lou DH, Zheng XS, Wang H, Liu XL. Risk factors of falls among older adults in Qinhuangdao City. Chin J Gerontol. (2016) 36:5140–1.
52. Pellicer-García B, Antón-Solanas I, Ramón-Arbués E, García-Moyano L, Gea-Caballero V, Juárez-Vela R. Risk of falling and associated factors in older adults with a previous history of falls. Int J Environ Res Public Health. (2020) 17:4085. doi: 10.3390/ijerph17114085
53. Lin C-H, Liao K-C, Pu S-J, Chen Y-C, Liu M-S. Associated factors for falls among the community-dwelling older people assessed by annual geriatric health examinations. PLoS ONE. (2011) 6:e18976. doi: 10.1371/journal.pone.0018976
54. Teno J, Kiel DP, Mor V. Multiple stumbles: a risk factor for falls in community-dwelling elderly. A prospective study. J Am Geriatr Soc. (1990) 38:1321–5. doi: 10.1111/j.1532-5415.1990.tb03455.x
55. Liao K-C, Pu S-J, Lin C-H, Chang H-J, Chen Y-J, Liu M-S. Association between the metabolic syndrome and its components with falls in community-dwelling older adults. Metab Syndr Relat Disord. (2012) 10:447–51. doi: 10.1089/met.2012.0046
56. Tsai Y-J, Yang P-Y, Yang Y-C, Lin M-R, Wang Y-W. Prevalence and risk factors of falls among community-dwelling older people: results from three consecutive waves of the national health interview survey in Taiwan. BMC Geriatr. (2020) 20:529. doi: 10.1186/s12877-020-01922-z
57. Fong KNK, Siu AMH, Yeung KA, et al. Falls among the community-living elderly people in Hong Kong: a retrospective study. Hong Kong J Occup Ther. (2011) 21:33–40. doi: 10.1016/j.hkjot.2011.05.005
58. Tinetti ME, Doucette J, Claus E, Marottoli R. Risk factors for serious injury during falls by older persons in the community. J Am Geriatr Soc. (1995) 43:1214–21. doi: 10.1111/j.1532-5415.1995.tb07396.x
59. Shuyi O, Zheng C, Lin Z, Zhang X, Li H, Fang Y, et al. Risk factors of falls in elderly patients with visual impairment. Front Public Health. (2022) 10:984199. doi: 10.3389/fpubh.2022.984199
60. Leung A, Chi I, Lou VWQ, Chan KS. Psychosocial risk factors associated with falls among Chinese community-dwelling older adults in Hong Kong. Health Soc Care Community. (2010) 18:272–81. doi: 10.1111/j.1365-2524.2009.00900.x
61. Wong AKW, Lord SR, Sturnieks DL, Delbaere K, Trollor JN, Close JCT. Angiotensin system-blocking medications are associated with fewer falls over 12 months in community-dwelling older people. J Am Geriatr Soc. (2013) 61:776–81. doi: 10.1111/jgs.12205
62. Sousa LMM, Marques-Vieira CMA, de Caldevilla MNGN, Henriques CMAD, Severino SSP, Caldeira SMA. Risk for falls among community-dwelling older people: systematic literature review. Rev Gaucha Enferm. (2017) 37:e55030. doi: 10.1590/1983-1447.2016.04.55030
63. Liu JY. Fear of falling in robust community-dwelling older people: results of a cross-sectional study. J Clin Nurs. (2015) 24:393–405. doi: 10.1111/jocn.12613
64. Zheng Jing C, Cui Y. Research on the current situation and influencing factors of fear of falling among the elderly in nursing homes. Nurs Res. (2019) 33:14–7.
65. Yue B. Research the Psychology and Influencing Factors of Fear of Falling Among the Elderly in Elderly Apartments. Shenyang: China Medical University (2009).
66. Chang HT, Chen HC, Chou P. Factors associated with fear of falling among community-dwelling older adults in the Shih-Pai study in Taiwan. PLoS ONE. (2016) 11:e0150612. doi: 10.1371/journal.pone.0150612
67. King MB, Judge JO, Wolfson L. Functional base of support decreases with age. J Gerontol. (1994) 49:M258–63. doi: 10.1093/geronj/49.6.M258
68. Yang H, Lu Q. The latest research on the balance function of the elderly. Chin Med Innov. (2016) 13:145–8.
69. Barak Y, Wagenaar RC, Holt KG. Gait characteristics of elderly people with a history of falls: a dynamic approach. Phys Ther. (2006) 86:1501–10. doi: 10.2522/ptj.20050387
70. Srygley JM, Herman T, Giladi N, Hausdorff JM. Self-report of missteps in older adults: a valid proxy of fall risk? Arch Phys Med Rehabil. (2009) 90:786–92. doi: 10.1016/j.apmr.2008.11.007
71. Salonen L, Kivelä SL. Eye diseases and impaired vision as possible risk factors for recurrent falls in the aged: a systematic review. Curr Gerontol Geriatr Res. (2012) 2012:271481. doi: 10.1155/2012/271481
72. Yogev-Seligmann G, Hausdorff JM, Giladi N. The role of executive function and attention in gait. Mov Disord. (2008) 23:329–42. doi: 10.1002/mds.21720
73. Brauer SG, Woollacott M, Shumway-Cook A. The interacting effects of cognitive demand and recovery of postural stability in balance-impaired elderly persons. J Gerontol A Biol Sci Med Sci. (2001) 56:M489–96. doi: 10.1093/gerona/56.8.M489
Keywords: community, older adults, risk factors, meta-analysis, systematic review
Citation: Li Y, Hou L, Zhao H, Xie R, Yi Y and Ding X (2023) Risk factors for falls among community-dwelling older adults: A systematic review and meta-analysis. Front. Med. 9:1019094. doi: 10.3389/fmed.2022.1019094
Received: 14 August 2022; Accepted: 02 December 2022;
Published: 06 January 2023.
Edited by:
Tzvi Dwolatzky, Technion Israel Institute of Technology, IsraelReviewed by:
Vahid Rashedi, University of Social Welfare and Rehabilitation Sciences, IranJaquelini Betta Canever, Federal University of Santa Catarina, Brazil
Copyright © 2023 Li, Hou, Zhao, Xie, Yi and Ding. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaorong Ding,  1442935193@qq.com
1442935193@qq.com
†These authors have contributed equally to this work and share first authorship
 Ying Li
Ying Li Lingyu Hou2†
Lingyu Hou2†