Staphylococcus aureus endocarditis: Identifying prognostic factors using a method derived from morbidity and mortality conferences
- 1Université de Lorraine, CHRU-Nancy, Service des Maladies Infectieuses et Tropicales, Nancy, France
- 2Université de Lorraine, APEMAC, Nancy, France
- 3CH Andrée Rosemon, Unité de Maladies Infectieuses et Tropicales, Cayenne, France
- 4CHRU-Nancy, Service des Maladies Infectieuses et Tropicales, Nancy, France
- 5CHRU-Nancy, Institut National de la Sante et de la Recherche Medicale (INSERM), Université de Lorraine, CIC, Epidémiologie Clinique, Nancy, France
- 6UMR 6249 CNRS-UFC Chrono-environnement, Service de Maladies Infectieuses, CHRU Besançon, Besançon, France
- 7Infectious Diseases and Intensive Care Unit, Pontchaillou University Hospital, Rennes, France
- 8CIC-Institut National de la Sante et de la Recherche Medicale (INSERM) 1414, Pontchaillou University Hospital, Rennes, France
- 9University of Rennes, Institut National de la Sante et de la Recherche Medicale (INSERM), Bacterial Regulatory RNAs and Medicine, UMR 1230, Rennes, France
- 10UFR Médecine, CHU Robert Debré, Reims, France
- 11Institut National de la Sante et de la Recherche Medicale (INSERM) CIC 1425, Bichat–Claude Bernard Hospital, Assistance Publique-Hôpitaux de Paris, Paris, France
- 12Institut National de la Sante et de la Recherche Medicale (INSERM), UMR-1137, IAME, Paris University, Paris, France
- 13Université de Paris, IAME, Institut National de la Sante et de la Recherche Medicale (INSERM), Paris, France
- 14Centre for Clinical Investigation, Assistance Publique-Hôpitaux de Paris, Bichat-Claude Bernard University Hospital, Paris, France
- 15Louis Pradel Hospital, Department of Cardiology, Lyon, France
- 16Montpellier University Hospital, Department of Infectious and Tropical Diseases, Montpellier, France
- 17CHU Nancy-Brabois, Department of Cardiology, Nancy, France
Objectives: Lethality of Staphylococcus aureus (Sa) infective endocarditis (IE) is high and might be due to yet unidentified prognostic factors. The aim of this study was to search for new potential prognostic factors and assess their prognostic value in SaIE.
Materials and methods: We used a two-step exploratory approach. First, using a qualitative approach derived from mortality and morbidity conferences, we conducted a review of the medical records of 30 patients with SaIE (15 deceased and 15 survivors), randomly extracted from an IE cohort database (NCT03295045), to detect new factors of possible prognostic interest. Second, we collected quantitative data for these factors in the entire set of SaIE patients and used multivariate Cox models to estimate their prognostic value.
Results: A total of 134 patients with modified Duke definite SaIE were included, 64 of whom died during follow-up. Of the 56 candidate prognostic factors identified at the first step, 3 had a significant prognostic value in multivariate analysis: the prior use of non-steroidal anti-inflammatory drugs [aHR 3.60, 95% CI (1.59–8.15), p = 0.002]; the non-performance of valve surgery when indicated [aHR 1.85, 95% CI (1.01–3.39), p = 0.046]; and the decrease of vegetation size on antibiotic treatment [aHR 0.34, 95% CI (0.12–0.97), p = 0.044].
Conclusion: We identified three potential SaIE prognostic factors. These results, if externally validated, might eventually help improve the management of patients with SaIE.
Introduction
Infective endocarditis (IE) is a rare but serious disease associated with high morbidity and mortality (1, 2). Staphylococcus aureus (Sa) became the most frequent pathogen responsible for IE during the past decades (3, 4). In comparison with other pathogens, lethality of SaIE is higher (4, 5). Its morbidity is also of concern, with 20–60% of embolic events (4, 5), 20–25% of sepsis (6, 7), and 26–38% of cardiac surgery during the initial management (4, 5).
To improve the outcomes of SaIE, identifying new prognostic factors may help tailor IE management to patients’ risk and improve patients’ management accordingly. Prognostic factors have already been identified in IE and SaIE. Among these, patients’ characteristics such as age (4, 8) and comorbidities (1, 8), have a major prognostic impact. Many SaIE clinical characteristics are associated with lethality, including prosthetic valve infection (8, 9), disease severity (septic shock and SOFA score) (9, 10), and heart, valve, or organ failures (1, 11). Higher mortality is also associated with left-sided IE (12), intracardiac abscess (1, 8), and larger vegetations (1, 13). Embolic events (2, 13), neurological complications (1, 10), and cardiac conduction abnormalities (14) are associated with poorer outcome. Methicillin-resistance of Sa (9) and persistent bacteremia are also associated with poorer outcome (4). Finally, deviations from optimal management such as inadequate antibiotic therapy (15) and delayed surgical treatment (8, 16) may also worsen the prognosis of SaIE. The plateauing high mortality observed in SaIE over the last decades (4, 5, 17, 18) suggests that specific prognostic factors may have not yet been identified. Moreover, most of the already identified prognostic factors are not modifiable. Searching for new prognostic factors might lead to identify modifiable factors and help design interventions that could improve SaIE outcome.
Prognostic factors are best identified using longitudinal studies and collecting candidate prognostic factors at baseline and outcomes during the follow-up, and then using Cox models to estimate the prognostic value of each factor. However, such methods require having candidate factors before initiating data collection. Once major factors, such as age and comorbidities, have been tested, identification of newer candidate factors becomes harder. Morbidity and mortality conferences (MMC) are designed to improve the quality of healthcare by addressing errors in patient’s management. In these conferences, healthcare professionals review and discuss, collegially, confidentially, and critically, the charts of patients who developed severe adverse events, to identify healthcare related factors that contributed to their occurrence (19). We thought that this approach could be helpful to identify candidate prognostic factors in SaIE. The aim of this study was to search for new potential prognostic factors and assess their prognostic value in SaIE.
Materials and methods
Study design
We used an exploratory two-step approach that included: (1) a qualitative approach derived from MMC to identify candidate prognostic factors in SaIE, and (2) a conventional quantitative approach to estimate the prognostic value of the factors identified at the end of step 1, using the source data that had been collected for the EI2008 study (NCT03295045) (3).
Setting
The EI2008 study has been extensively described elsewhere (3). Briefly, EI2008 is a longitudinal cohort study conducted in France in 2008, which aimed to describe IE incidence and prognosis, and enrolled 602 patients aged ≥ 18 years with definite (n = 497) or possible (n = 105) IE according to modified Duke criteria. Data collection consisted of demographic characteristics, medical history, medications, IE mode of acquisition, and clinical, biological, and therapeutic characteristics (see Supplementary material). Patients were followed up for 1-year all-cause mortality (3). The identification of all Sa strains had been confirmed by the national reference center for staphylococci (Centre National de Référence des Staphylocoques, Institut des Agents Infectieux, Hospices Civils de Lyon, Lyon, France).
Participants
For the first-step qualitative approach, among 134 patients with modified Duke definite SaIE included in EI2008, we used computer-generated random numbers to sample 15 patients with definite SaIE who had died and 15 patients with definite SaIE who had survived at the end of the 1-year follow-up.
For the quantitative approach, we selected from the EI2008 study database all the 134 patients with modified Duke definite SaIE, of whom 70 survived and 64 died during follow-up (Figure 1).
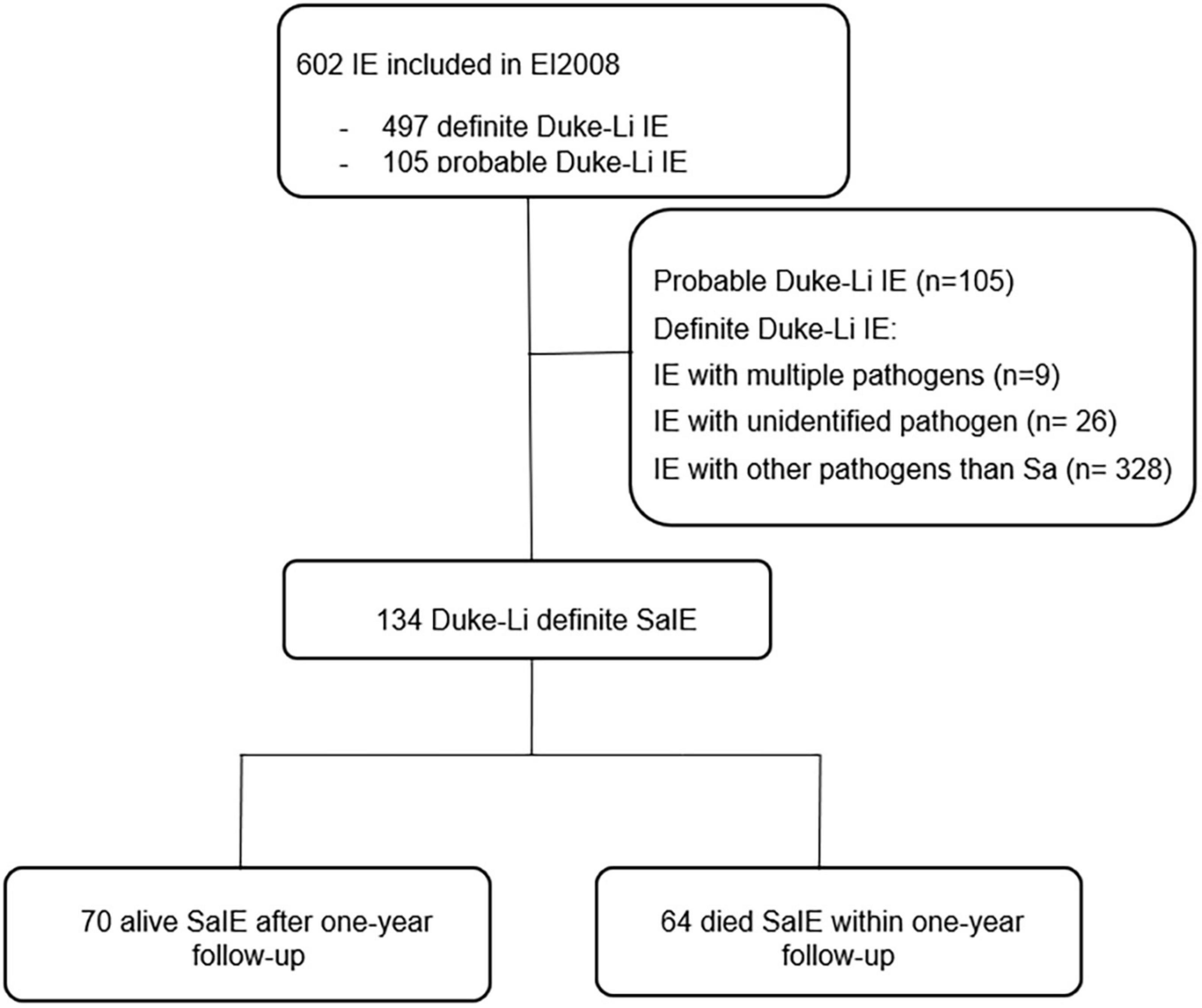
Figure 1. Flow chart of patients with Staphylococcus aureus infective endocarditis (SaIE) selected from EI2008. IE, infective endocarditis, Sa, Staphylococcus aureus.
Data collection
For the qualitative approach, we used a method inspired by MMC (19, 20) and conducted an in-depth review of the whole patients’ charts (MB, AL, and BL) to identify factors that were not already collected in the EI2008 case report form (CRF) but could be associated with the outcome (defined as “candidate prognostic factors”). We searched the charts of the 15 patients who died during follow-up for factors deemed unfavorable candidate prognostic factors, and the charts of the 15 patients who survived for factors deemed favorable candidate prognostic factors. Following the guidelines of the French National Authority for Health on MMC (20), each candidate prognostic factor was then collegially and critically reviewed (by MB, AL, BL, NA, and BH) to drop duplicates (i.e., variables that were already collected as part of EI2008 CRF) and to select those that were deemed relevant on a clinical and pathophysiological perspective. All the candidate prognostic factors that were retained at the end of the first step were collected from the medical charts of all the 134 patients included in the quantitative approach and were implemented into an enriched EI2008 database.
For the quantitative approach, we re-used the data that were prospectively collected as part of the EI2008 cohort study protocol and additional data (concerning the candidate prognostic factors identified by the qualitative approach) that were specifically collected from patients’ medical charts for the purpose of the present study.
Statistical analyses
We first described patients’ characteristics and the distribution of candidate factors, using frequencies and percentages for categorical variables, or median and interquartile range for quantitative variables. Second, we used Cox models to identify potential prognostic factors among candidates using bivariate analyses. We retained candidate prognostic factors with a p-value < 0.2 as eligible for multivariate analyses. Third, for each eligible candidate prognostic factor, we conducted a multivariate Cox model, using the given factor as an independent variable and adjusting for confounding factors that were identified among baseline characteristics and candidate prognostic factors by their bivariate association (p-value < 0.2) with both survival and the candidate prognostic factor under scrutiny. P-values were two-sided, and statistical significance level was set at 0.05. All statistical analyses were performed using SAS 9.4 (SAS Institute, Inc., Cary, NC, USA) software.
Ethics
This study complies with the principles outlined in the Declaration of Helsinki. EI2008 was approved by the French Commission Nationale Informatique et des Libertés (CNIL-DR-2010-219). Patients received complete information about the study, and their right to refuse to participate. EI2008 being an observational study, in accordance with the French law, patient written consent was waived (NCT03295045).
Results
Staphylococcus aureus infective endocarditis patients’ characteristics and follow-up
The characteristics of the 134 patients are described in Table 1. Their median age was 62.5 years (IQR 31 years) and there was a majority of men (n = 98, 73.1%). A heart disease at risk of IE was present in 54 (40.3%) patients. Most IE cases were community-acquired (n = 72, 53.7%). Most frequent complications included septic shock (n = 49, 36.6%), cerebral embolisms (n = 48, 35.8%), and heart failure (n = 13, 9.7%).
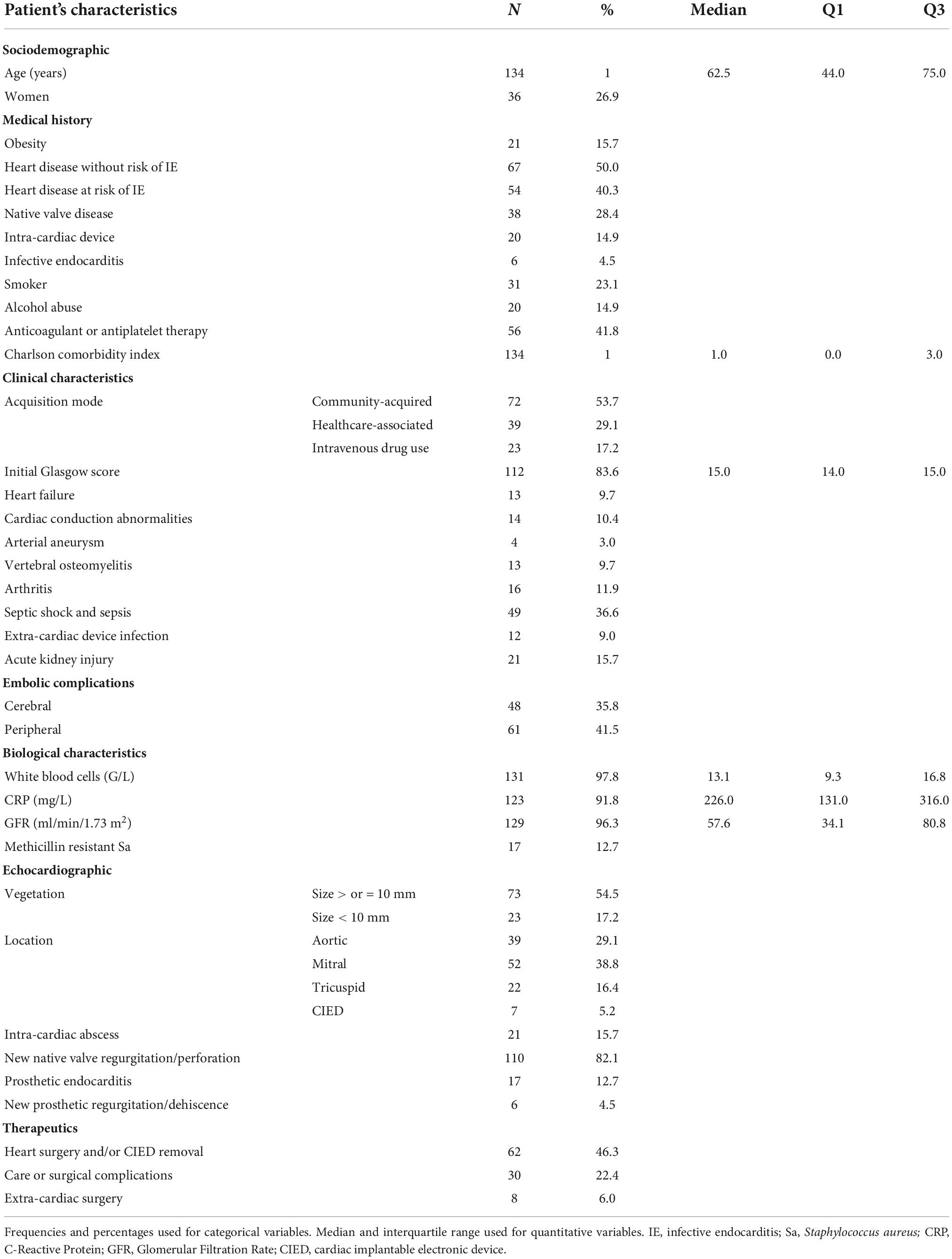
Table 1. Main characteristics of the 134 patients with Staphylococcus aureus infective endocarditis.
Identification of candidate prognostic factors in Staphylococcus aureus infective endocarditis: Results of the qualitative approach
In the charts of the 15 surviving patients, we identified 22 candidate prognostic factors that could be associated with higher survival (Table 2). In the charts of the 15 deceased patients, we identified 34 candidate prognostic factors that could be associated with higher mortality (Table 3). All these candidate prognostic factors were then collected in the medical charts of all the 134 patients included in the quantitative approach (the frequency of each factor was presented in Tables 2, 3).
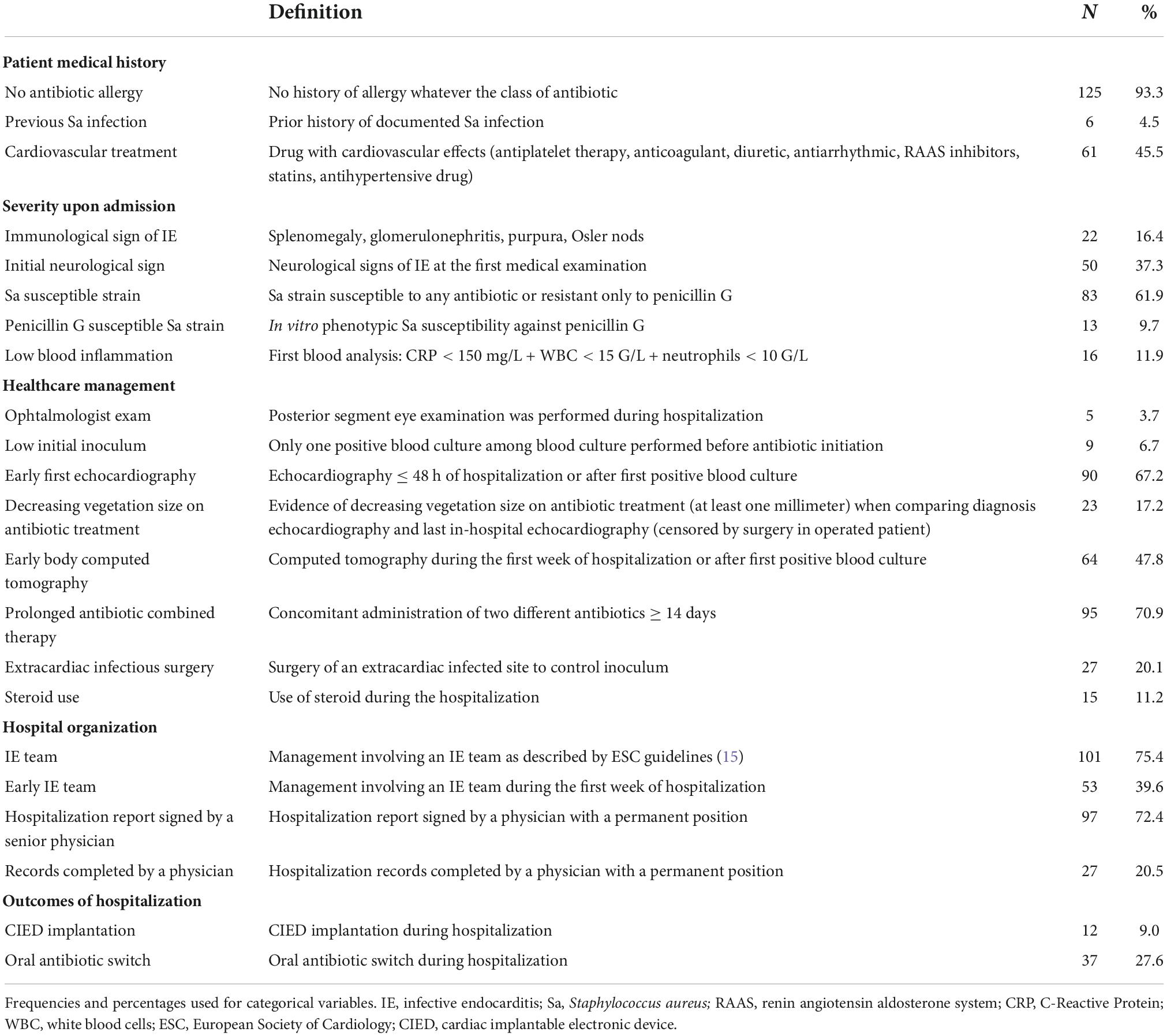
Table 2. Description of candidate prognostic factors that could be associated with survival in the 134 Staphylococcus aureus infective endocarditis patients.
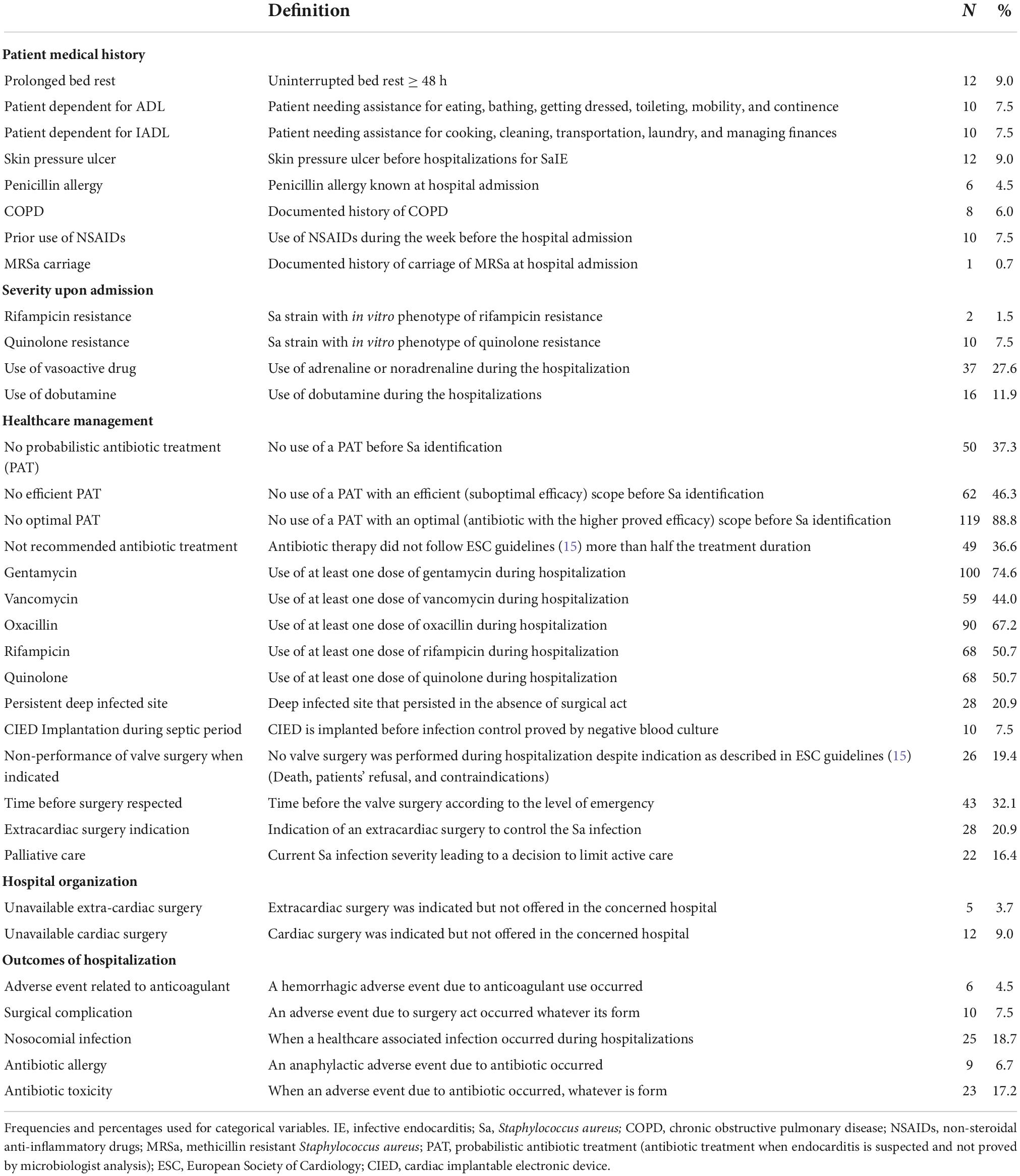
Table 3. Description of factors that could be associated with death in the 134 Staphylococcus aureus infective endocarditis patients.
Candidate prognostic factors were sorted out into five categories: patient medical history (3 potentially associated with higher survival vs. 8 potentially associated with higher mortality), severity upon admission (5 vs. 4), healthcare management (8 vs. 15), hospital organization (4 vs. 2), and outcomes of hospitalization (2 vs. 5).
Prognostic value of candidate prognostic factors in Staphylococcus aureus infective endocarditis: Results from the quantitative approach
Eligible factors associated with outcome are presented in Table 4. After adjustment for potential confounders, two eligible candidate prognostic factors remained significantly associated with higher mortality during the 1-year follow-up: the prior use of non-steroidal anti-inflammatory drugs (NSAIDs) [aHR 3.60, 95% confidence interval (95% CI) (1.59–8.15), p = 0.002] and the non-performance of valve surgery when indicated [aHR 1.85, 95% CI (1.01–3.39), p = 0.046]. One eligible candidate prognostic factor was associated with lower mortality: the decrease of vegetation size on antibiotic treatment [aHR 0.34 95% CI (0.12–0.97), p = 0.044].
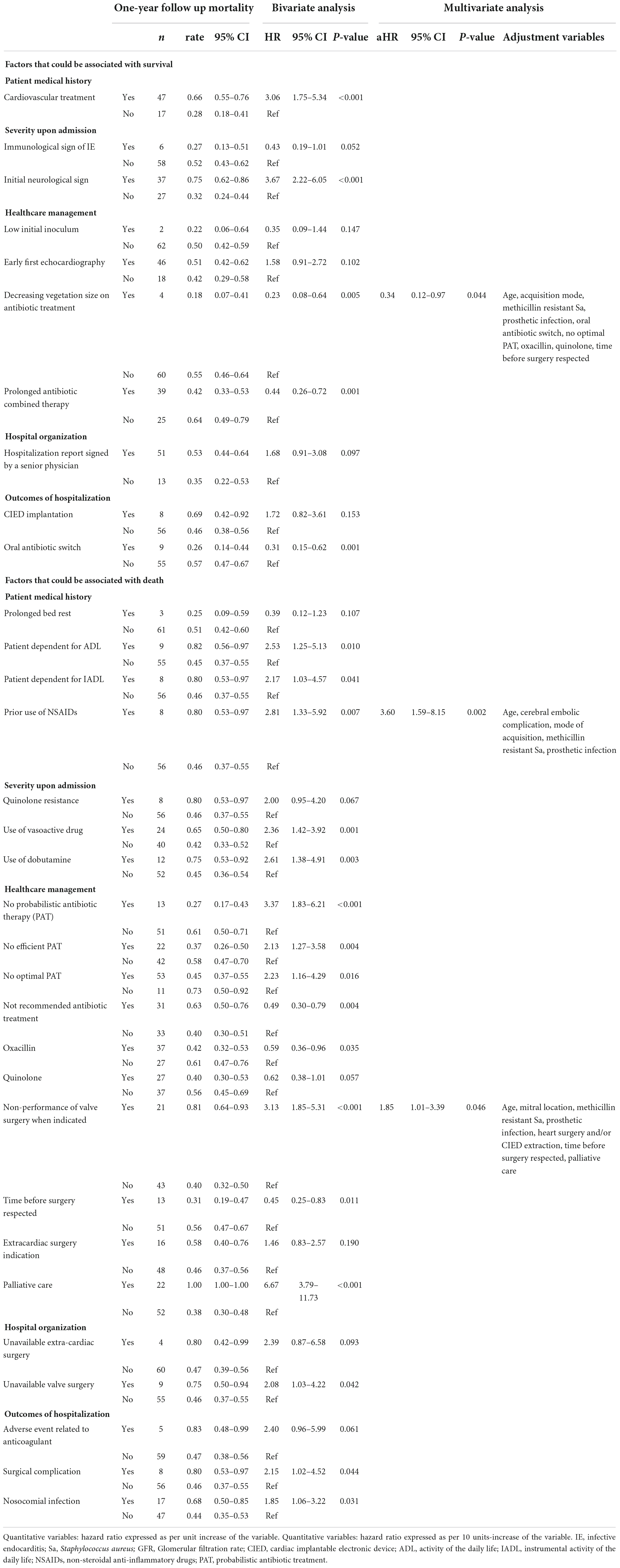
Table 4. Prognostic value of factors that could be associated with Staphylococcus aureus infective endocarditis outcome.
Discussion
In this study, relying on a method derived from MMC, we identified three potential prognostic factors, two that were associated with higher mortality, i.e., the prior use of NSAIDs and the non-performance of valve surgery when indicated, and one that was associated with lower mortality, i.e., the decrease of vegetation size on antibiotic treatment.
To the best of our knowledge, no published study used a method derived from MMC to identify potential prognostic factors in SaIE. In most instances, it takes the form of a meeting of members of different medical teams who collectively try to retrospectively identify factors that may have contributed to a patient’s unfavorable outcome. The patient’s management is described and analyzed in an attempt to identify the causal factors of complications with the aim to improve the quality and safety of care, without judging individuals or looking for a culprit (21). In an attempt to standardize the course of MMC, Gregor and Taylor recommended that it be based on five essential components: (1) an adverse event (the case presented must include an adverse event that resulted from clinical decisions and/or care provided); (2) anonymity (individuals involved in the case must be afforded anonymity to allow for free and objective discussion); (3) critical analysis (based on reliable, objective data and careful attention to sources of bias in clinical decision making); (4) reframing understanding of errors to prevent their repetition; and (5) projection to practice change (19). Here, in an attempt to suggest practice changes to improve SaIE patients’ outcome, we organized a meeting of members of different medical backgrounds, i.e., infectious disease (MB, BH, AL, and BL), epidemiology (NA), and public health (NA), to collectively reframe the understanding of favorable or unfavorable prognosis relying on a critical analysis of all the data collected in the anonymized medical charts of some patients who died or survived from SaIE. And then, relying on a more classic quantitative approach, we raised hypotheses about factors that could be considered as prognostic factors.
We are aware that an association may not be causal. To establish epidemiologic evidence of a causal relationship between a presumed cause and an observed effect, Hill proposed to examine a set of nine criteria (22). We therefore examined our three potential prognostic factors versus these criteria (Table 5). NSAIDs were strongly associated with death, with a threefold higher risk of death in SaIE patients who had vs. those who had not received NSAIDs. To date, no study assessed the prognostic value of the use of NSAIDs in IE. However, NSAIDs are known to have multiple effects on innate and adaptive immunity (prostaglandin and leukotriene pathways) (23). Several studies showed that NSAID use could worsen the prognosis of infectious conditions, especially respiratory tract, osteoarticular and skin and soft tissue bacterial infection (24–26). The non-performance of valve surgery when indicated was associated with impaired prognosis in SaIE patients. This result was consistent with what was previously reported in other studies focusing on prognostic factors in IE and SaIE (1, 27, 28). In our study, as in previous studies (1, 27, 28), patients who did not undergo cardiac surgery despite indication were old, had many comorbidities, and presented with cardiac, infectious or embolic complications resulting in an unfavorable benefit-risk ratio for undergoing surgery. The decrease of vegetation size on antibiotic treatment was associated with a lower mortality. Decreasing vegetation size on antibiotic treatment was obtained by comparing diagnostic and last in-hospital echocardiography (which was censored by surgery in operated patient). The strength of this association was high, with a threefold decreased risk of death in SaIE patients in whom the vegetation size decreased. Regarding plausibility, our finding is consistent with prior results that showed a correlation between the size of the vegetation, the risk of embolism, and the risk of death in IE (13, 29–31). For this variable, as for the others, it seems essential to confirm our results in other studies. However, before that, it seems essential to find a standardized definition of a significant reduction in the size of the vegetation: how many millimeters? By what echocardiographic method? After what period of antibiotic treatment? An intervention to improve SaIE outcomes could be multidisciplinary meeting to adapt treatment when the vegetation size does not decrease during antibiotic treatment. For example, some authors believe that antibiotics other than those recommended should be tested in Sa infections, including IE, as they may have a better tolerability profile or even greater efficacy (32–38). However, these data are based on meta-analyses from biased observational studies and deserve to be confirmed in a large randomized controlled trial (39, 40). We have therefore identified three potential prognostic factors, two of which have never been identified before in endocarditis. In the future, it would seem interesting to confirm our results in an independent cohort. Ideally, a precise definition of each factor will have to be decided and the prognostic influence of each of them will be studied prospectively. Finally, if these results are confirmed, interventional projects could be developed to change the management of SaIE and improve its poor prognosis.
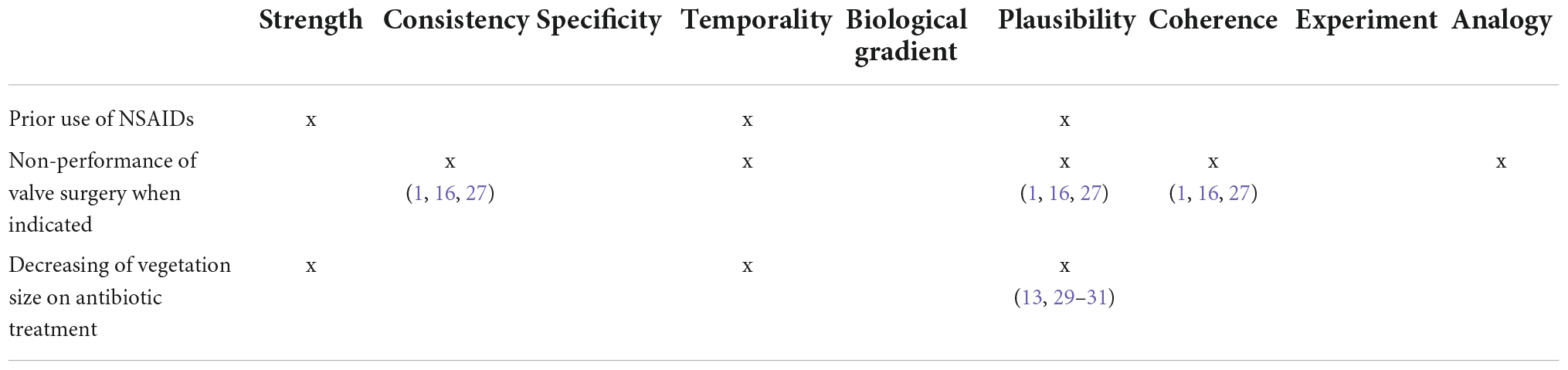
Table 5. The potential prognostic factors relevance in Staphylococcus aureus endocarditis assessed by the Hill criteria.
We acknowledge that our work may have some limitations. First, the patients’ medical charts may not include key prognostic information that was therefore missed by our qualitative approach. Second, due to the observational design, residual unmeasured confounding might still threaten the validity of our multivariate analyses. Third, due to the relatively low number of IE cases that were included in this study, we may not have been able to identify factors that had a genuine prognostic value. Fourth, the wording and definition of our candidate prognostic factors may be questioned and our results need now to undergo external validation in an independent dataset with standardized definitions to ensure reproducibility and therefore confirm the possible causality of the factors we identified.
Conclusion
Our results suggest that the management of patients with SaIE could be improved by considering new prognostic factors. Although they need to be confirmed by additional studies, our findings indicate that the outcome of SaIE would be enhanced by limiting the use of NSAIDs, considering valve surgery when indicated even if the likelihood of postoperative death is high, and reconsidering the treatment strategy when the size of the vegetation does not decrease during the antibiotic treatment.
Data availability statement
This raw data supporting the conclusions of this article are protected by the French law. Requests to access the datasets should be directed to the corresponding author.
Ethics statement
This studies involving human participants were reviewed and approved by the French Commission Nationale de l’Informatique et des Libertés (CNIL-DR-2010-219). The patients/participants provided their written informed consent to participate in this study.
Author contributions
BL, AL, MB, BH, and NA: conception and design of the study. BL, AL, MB, WN-S, BH, and NA: analysis and interpretation of data. All authors acquired of data, drafted the article or revised it critically for important intellectual content, and final approval of the version to be submitted.
Acknowledgments
We would like to acknowledge the AEPEI study group and the whole French National Observatory on Infective Endocarditis team.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.1053278/full#supplementary-material
Abbreviations
ADL, activity of the daily life; AEPEI, Association pour l’Etude et la Prévention de l’Endocardite Infectieuse; CIED, cardiac implantable electronic device; COPD, chronic obstructive pulmonary disease; CRF, case report form; ESC, European Society of Cardiology; GFR, Glomerular Filtration Rate; HAS, Haute Autorité de Santé; IADL, instrumental activity of the daily life; IE, infective endocarditis; MMC, morbidity and mortality conferences; MRSa, methicillin resistant Staphylococcus aureus; NSAIDs, non-steroidal anti-inflammatory drugs; PAT, probabilistic antibiotic treatment; Sa, Staphylococcus aureus; SaIE, Staphylococcus aureus infective endocarditis.
References
1. Habib G, Erba PA, Iung B, Donal E, Cosyns B, Laroche C, et al. Clinical presentation, aetiology and outcome of infective endocarditis. Results of the ESC-EORP EURO-ENDO (European infective endocarditis) registry: a prospective cohort study. Eur Heart J. (2019) 40:3222–32. doi: 10.1093/eurheartj/ehz620
2. Olmos C, Vilacosta I, Fernández-Pérez C, Bernal JL, Ferrera C, García-Arribas D, et al. The evolving nature of infective endocarditis in Spain. J Am Coll Cardiol. (2017) 70:2795–804. doi: 10.1016/j.jacc.2017.10.005
3. Selton-Suty C, Célard M, Le Moing V, Doco-Lecompte T, Chirouze C, Iung B, et al. Preeminence of Staphylococcus aureus in infective endocarditis: a 1-year population-based survey. Clin Infect Dis. (2012) 54:1230–9. doi: 10.1093/cid/cis199
4. Fowler VG, Miro JM, Hoen B, Cabell CH, Abrutyn E, Rubinstein E, et al. Staphylococcus aureus endocarditis: a consequence of medical progress. JAMA. (2005) 293:3012. doi: 10.1001/jama.293.24.3012
5. Miro JM, Anguera I, Cabell CH, Chen AY, Stafford JA, Corey GR, et al. Staphylococcus aureus native valve infective endocarditis: report of 566 episodes from the international collaboration on endocarditis merged database. Clin Infect Dis. (2005) 41:507–14. doi: 10.1086/431979
6. Nadji G, Rémadi JP, Coviaux F, Mirode AA, Brahim A, Enriquez-Sarano M, et al. Comparison of clinical and morphological characteristics of Staphylococcus aureus endocarditis with endocarditis caused by other pathogens. Heart Br Card Soc. (2005) 91:932–7. doi: 10.1136/hrt.2004.042648
7. Abdallah L, Habib G, Remadi J-P, Salaun E, Casalta J-P, Tribouilloy C. Comparison of prognoses of Staphylococcus aureus left-sided prosthetic endocarditis and prosthetic endocarditis caused by other pathogens. Arch Cardiovasc Dis. (2016) 109:542–9. doi: 10.1016/j.acvd.2016.02.010
8. Murdoch DR, Corey GR, Hoen B, Miró JM, Fowler VG, Bayer AS, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the international collaboration on endocarditis-prospective cohort study. Arch Intern Med. (2009) 169:463–73. doi: 10.1001/archinternmed.2008.603
9. Leroy O, Georges H, Devos P, Bitton S, De Sa N, Dedrie C, et al. Infective endocarditis requiring ICU admission: epidemiology and prognosis. Ann Intensive Care. (2015) 5:45. doi: 10.1186/s13613-015-0091-7
10. Muñoz P, Kestler M, De Alarcon A, Miro JM, Bermejo J, Rodríguez-Abella H, et al. Current epidemiology and outcome of infective endocarditis: a multicenter, prospective, cohort study. Medicine. (2015) 94:e1816. doi: 10.1097/MD.0000000000001816
11. Olmos C, Vilacosta I, Fernandez C, Lopez J, Sarria C, Ferrera C, et al. Contemporary epidemiology and prognosis of septic shock in infective endocarditis. Eur Heart J. (2013) 34:1999–2006. doi: 10.1093/eurheartj/ehs336
12. Tagliari AP, Steckert GV, Silveira LMV, Kochi AN, Wender OCB. Infective endocarditis profile, prognostic factors and in-hospital mortality: 6-year trends from a tertiary university center in South America. J Card Surg. (2020) 35:1905–11. doi: 10.1111/jocs.14787
13. Nunes MCP, Guimarães-Júnior MH, Murta Pinto PHO, Coelho RMP, Souza Barros TL, Faleiro Maia N, et al. Outcomes of infective endocarditis in the current era: early predictors of a poor prognosis. Int J Infect Dis. (2018) 68:102–7. doi: 10.1016/j.ijid.2018.01.016
14. DiNubile MJ, Calderwood SB, Steinhaus DM, Karchmer AW. Cardiac conduction abnormalities complicating native valve active infective endocarditis. Am J Cardiol. (1986) 58:1213–7. doi: 10.1016/0002-9149(86)90384-X
15. Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta J-P, Del Zotti F, et al. 2015 ESC guidelines for the management of infective endocarditis: the task force for the management of infective endocarditis of the European society of cardiology (ESC)endorsed by: European association for cardio-thoracic surgery (EACTS), the European association of nuclear medicine (EANM). Eur Heart J. (2015) 36:3075–128. doi: 10.1093/eurheartj/ehv319
16. Chirouze C, Alla F, Fowler VG, Sexton DJ, Corey GR, Chu VH, et al. Impact of early valve surgery on outcome of Staphylococcus aureus prosthetic valve infective endocarditis: analysis in the international collaboration of endocarditis–prospective cohort study. Clin Infect Dis. (2015) 60:741–9. doi: 10.1093/cid/ciu871
17. Hill EE, Herijgers P, Claus P, Vanderschueren S, Herregods M-C, Peetermans WE. Infective endocarditis: changing epidemiology and predictors of 6-month mortality: a prospective cohort study. Eur Heart J. (2006) 28:196–203. doi: 10.1093/eurheartj/ehl427
18. Chu VH, Cabell CH, Benjamin DK, Kuniholm EF, Fowler VG, Engemann J, et al. Early predictors of in-hospital death in infective endocarditis. Circulation. (2004) 109:1745–9. doi: 10.1161/01.CIR.0000124719.61827.7F
19. Gregor A, Taylor D. Morbidity and mortality conference: its purpose reclaimed and grounded in theory. Teach Learn Med. (2016) 28:439–47. doi: 10.1080/10401334.2016.1189335
20. Haute autorité de Santé H France. Revue de Mortalité et de Morbidité (RMM) Outil D’amélioration Des Pratiques Professionnelles. (2015). Available online at: has-sante.fr/jcms/c_434817/fr/revue-de-mortalite-et-de-morbidite-rmm (accessed August 21, 2020).
21. Orlander JD, Barber TW, Fincke BG. The morbidity and mortality conference: the delicate nature of learning from error. Acad Med. (2002) 77:1001–6. doi: 10.1097/00001888-200210000-00011
22. Hill AB. The environment and disease: association or causation? J R Soc Med. (2015) 108:32–7. doi: 10.1177/0141076814562718
23. Bacchi S, Palumbo P, Sponta A, Coppolino MF. Clinical pharmacology of non-steroidal anti-inflammatory drugs: a review. Anti Inflamm Anti Allergy Agents Med Chem. (2012) 11:52–64. doi: 10.2174/187152312803476255
24. Le Turnier P, Boutoille D, Joyau C, Veyrac G, Asseray N. Bacterial infections and NSAIDs exposure? Seek septic complications. Eur J Intern Med. (2017) 41:e33–4. doi: 10.1016/j.ejim.2017.03.004
25. Basille D, Plouvier N, Trouve C, Duhaut P, Andrejak C, Jounieaux V. Non-steroidal anti-inflammatory drugs may worsen the course of community-acquired pneumonia: a cohort study. Lung. (2017) 195:201–8. doi: 10.1007/s00408-016-9973-1
26. Leroy S, Marc E, Bavoux F, Tréluyer J-M, Gendrel D, Bréart G, et al. Hospitalization for severe bacterial infections in children after exposure to NSAIDs: a prospective adverse drug reaction reporting study. Clin Drug Investig. (2010) 30:179–85. doi: 10.2165/11532890-000000000-00000
27. Fernández Guerrero ML, González López JJ, Goyenechea A, Fraile J, de Górgolas M. Endocarditis caused by Staphylococcus aureus: a reappraisal of the epidemiologic, clinical, and pathologic manifestations with analysis of factors determining outcome. Medicine. (2009) 88:1–22. doi: 10.1097/MD.0b013e318194da65
28. Hill EE, Herregods M-C, Vanderschueren S, Claus P, Peetermans WE, Herijgers P. Management of prosthetic valve infective endocarditis. Am J Cardiol. (2008) 101:1174–8. doi: 10.1016/j.amjcard.2007.12.015
29. Rohmann S, Erbel R, Darius H, Görge G, Makowski T, Zotz R, et al. Prediction of rapid versus prolonged healing of infective endocarditis by monitoring vegetation size. J Am Soc Echocardiogr. (1991) 4:465–74. doi: 10.1016/S0894-7317(14)80380-5
30. Scheggi V, Alterini B, Olivotto I, Del Pace S, Zoppetti N, Tomberli B, et al. Embolic risk stratification and prognostic impact of early surgery in left-sided infective endocarditis. Eur J Intern Med. (2020) 78:82–7. doi: 10.1016/j.ejim.2020.04.017
31. Mohananey D, Mohadjer A, Pettersson G, Navia J, Gordon S, Shrestha N, et al. Association of vegetation size with embolic risk in patients with infective endocarditis: a systematic review and meta-analysis. JAMA Intern Med. (2018) 178:502. doi: 10.1001/jamainternmed.2017.8653
32. Maraolo AE, Giaccone A, Gentile I, Saracino A, Bavaro DF. Daptomycin versus vancomycin for the treatment of methicillin-resistant Staphylococcus aureus bloodstream infection with or without endocarditis: a systematic review and meta-analysis. Antibiotics. (2021) 10:1014. doi: 10.3390/antibiotics10081014
33. Lee S, Song K-H, Jung S-I, Park WB, Lee SH, Kim Y-S, et al. Comparative outcomes of cefazolin versus nafcillin for methicillin-susceptible Staphylococcus aureus bacteraemia: a prospective multicentre cohort study in Korea. Clin Microbiol Infect. (2018) 24:152–8. doi: 10.1016/j.cmi.2017.07.001
34. Shi C, Xiao Y, Zhang Q, Li Q, Wang F, Wu J, et al. Efficacy and safety of cefazolin versus antistaphylococcal penicillins for the treatment of methicillin-susceptible Staphylococcus aureus bacteremia: a systematic review and meta-analysis. BMC Infect Dis. (2018) 18:508. doi: 10.1186/s12879-018-3418-9
35. Rindone JP, Mellen CK. Meta-analysis of trials comparing cefazolin to antistaphylococcal penicillins in the treatment of methicillin-sensitive Staphylococcus aureus bacteraemia: meta-analysis: cefazolin vs. antistaphylococcal penicillin. Br J Clin Pharmacol. (2018) 84:1258–66. doi: 10.1111/bcp.13554
36. Eljaaly K, Alshehri S, Erstad BL. Systematic review and meta-analysis of the safety of antistaphylococcal penicillins compared to cefazolin. Antimicrob Agents Chemother. (2018) 62:e1816–7. doi: 10.1128/AAC.01816-17
37. Bidell MR, Patel N, O’Donnell JN. Optimal treatment of MSSA bacteraemias: a meta-analysis of cefazolin versus antistaphylococcal penicillins. J Antimicrob Chemother. (2018) 73:2643–51. doi: 10.1093/jac/dky259
38. Samura M, Kitahiro Y, Tashiro S, Moriyama H, Hamamura Y, Takahata I, et al. Efficacy and safety of daptomycin versus vancomycin for bacteremia caused by methicillin-resistant Staphylococcus aureus with vancomycin minimum inhibitory concentration > 1 μg/mL: a systematic review and meta-analysis. Pharmaceutics. (2022) 14:714. doi: 10.3390/pharmaceutics14040714
39. Lecomte R, Bourreau A, Deschanvres C, Issa N, Le Turnier P, Gaborit B, et al. Comparative outcomes of cefazolin versus anti-staphylococcal penicillins in methicillin-susceptible Staphylococcus aureus infective endocarditis: a post-hoc analysis of a prospective multicentre French cohort study. Clin Microbiol Infect. (2020) 27:1015–21. doi: 10.1016/j.cmi.2020.08.044
40. Lefèvre B, Hoen B, Goehringer F, Sime WN, Aissa N, Alauzet C, et al. Antistaphylococcal penicillins vs. cefazolin in the treatment of methicillin-susceptible Staphylococcus aureus infective endocarditis: a quasi-experimental monocentre study. Eur J Clin Microbiol Infect Dis. (2021) 40:2605–16. doi: 10.1007/s10096-021-04313-3
Keywords: Staphylococcus aureus, infective endocarditis, prognostic factors, survival, morbidity and mortality conference method
Citation: Lefèvre B, Legoff A, Boutrou M, Goehringer F, Ngueyon-Sime W, Chirouze C, Revest M, Vernet Garnier V, Duval X, Delahaye F, Le Moing V, Selton-Suty C, Filippetti L, Hoen B and Agrinier N (2022) Staphylococcus aureus endocarditis: Identifying prognostic factors using a method derived from morbidity and mortality conferences. Front. Med. 9:1053278. doi: 10.3389/fmed.2022.1053278
Received: 25 September 2022; Accepted: 17 November 2022;
Published: 06 December 2022.
Edited by:
Carlo Tascini, University of Udine, ItalyReviewed by:
Davide Fiore Bavaro, University of Bari Medical School, ItalyKatarina Westling, Karolinska Institutet (KI), Sweden
Copyright © 2022 Lefèvre, Legoff, Boutrou, Goehringer, Ngueyon-Sime, Chirouze, Revest, Vernet Garnier, Duval, Delahaye, Le Moing, Selton-Suty, Filippetti, Hoen and Agrinier. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Benjamin Lefèvre, b.lefevre@chru-nancy.fr
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share last authorship
 Benjamin Lefèvre
Benjamin Lefèvre Antoine Legoff1†
Antoine Legoff1†  Véronique Vernet Garnier
Véronique Vernet Garnier Laura Filippetti
Laura Filippetti