Association Between Hair Diseases and COVID-19 Pandemic-Related Stress: A Cross-Sectional Study Analysis
- 1Central Medical College, Cumilla, Bangladesh
- 2Public Health Foundation, Dhaka, Bangladesh
- 3Rajshahi Medical College, Rajshahi, Bangladesh
- 4Khulna Medical College, Khulna, Bangladesh
- 5M Abdur Rahim Medical College, Dinajpur, Bangladesh
- 6International Center for Diarrhoeal Disease Research, Dhaka, Bangladesh
- 7Delta Medical College, Dhaka, Bangladesh
- 8Department of Public Health, State University of Bangladesh, Dhaka, Bangladesh
- 9Department of Primary Care & Mental Health, University of Liverpool, Liverpool, United Kingdom
Introduction: Psychological stress from the ongoing coronavirus disease 2019 (COVID-19) pandemic can potentially aggravate the course of several stress-sensitive skin and hair diseases. This study aimed to determine the potential association of COVID-19 stress with hair diseases, such as telogen effluvium (TE), alopecia areata (AA), and seborrheic dermatitis (SD), among medical students in Bangladesh.
Methods: This online-based cross-sectional study was conducted among 404 medical students of Bangladesh using a self-administered questionnaire, including sociodemographic information, status of hair diseases (i.e., TE, AA, and SD), COVID-19 fear scale, impact of event scale specific for COVID-19 (IES-COVID-19), and COVID-19 student stress questionnaire (CSSQ) scale, to determine pandemic-related stress. The logistic regression model was used to analyze the association.
Results: Overall prevalence of TE, AA, and SD was 61.1, 24.7, and 57.7%, respectively, with female predominance in case of TE and male predominance in case of AA and SD. More than half of the participants had COVID-19-related fear and traumatic stress symptoms. In the multiple logistic regression model, smoking [adjusted odds ratio (aOR) 2.93, 95% CI 1.29–6.65 for AA and aOR 4.19, 95% CI 1.83–9.56 for TE], COVID-19-related fear (aOR 1.70, 95% CI 1.01–2.89 for AA and aOR 2.620, 95% CI 1.25–5.48 for TE), and COVID-19-related traumatic stress symptoms (aOR 1.84, 95% CI 1.08–3.13 for AA, aOR 2.61, 95% CI 1.19–5.68 for TE, and aOR 1.92, 95% CI 1.14–3.25 for SD) were the risk factors of hair fall disorders.
Conclusion: Our study showed that a large number of medical students experienced TE, AA, and SD during the pandemic era. COVID-19-related stress and fear potentially have an association with these diseases.
Introduction
Psychological stresses have been associated with the development of a variety of skin and hair loss problems globally. Increased psychosocial stress can impact the course of many common “stress-sensitive” skin conditions that lead to actual or perceived exacerbation of the disease (1, 2). Psychological distress, including stress, post-traumatic stress disorder, depression, and anxiety disorders, have all been linked to the emergence or exacerbation of a variety of dermatologic diseases [e.g., psoriasis, atopic eczema, urticaria, alopecia areata (AA), and hair-related problems] (3). The process is mediated by complicated neuroendocrine regulation of inflammatory and related systems. The hypothalamic–pituitary–adrenocortical (HPA) axis plays a crucial role during stressful events and potentially triggers the skin-related disorders (3–5).
Patients with hair diseases, such as telogen effluvium (TE), AA, and scalp seborrheic dermatitis, often reported a low quality of life and increased levels of psychological stress, depression, and anxiety (6–8). The treatment challenges are centered on the role of stress in hair loss and place a premium on the development of appropriate coping mechanisms and the enhancement of patients' quality of life (9). The connection between a stressor and subsequent alterations in the hair growth cycle has resulted in the designation of the brain-hair follicle axis. By promoting the transition of anagen hairs into the telogen process, certain neuropeptides, neurotransmitters, and hormones produced along this brain-hair follicle axis can induce significant alterations in the hair development cycle (7).
Current pandemic, uncertainties, and lockdown circumstances are challenging for the majority of people and contribute to increase psychological suffering worldwide (10, 11). In Bangladesh, university students are considered a vulnerable group for psychological distress as a consequence of coronavirus disease 2019 (COVID-19), and they are experiencing mild to extremely severe psychological stresses during this pandemic (12, 13). In a developing country, such as Bangladesh, where the job market is already scanty after graduation, the uncertainty of academic progress during this pandemic is deteriorating the condition (14). Moreover, medical students have considerably higher rates of psychiatric depression, anxiety, suicidal ideation, and mood disturbances compared with other post-secondary graduate students. Medical students are suffering from severe mental disorders during the COVID-19 pandemic. COVID-19 has caused a variety of negative consequences, including a harmful effect on the mental health of medical students in Bangladesh. A considerable percentage of Bangladeshi medical students is experiencing adverse psychological stresses as a result of the pandemic (15–17).
Different hair-related problems, such as TE, AA, and SD levels, were shown to have increased to some extent during the pandemic (18). A study reported that the patient density for these diseases was substantially greater during the COVID-19 pandemic phase than a year before (19). There is a limited number of literature reviews on this issue. However, TE was reported as a common post-COVID manifestation in infected patients (20). In addition, with these results, it was hypothesized that the psychosocial stress caused by the ongoing pandemic situation may result in exacerbations or the initiation of these hair loss problems. To the best of our knowledge, this is the first study focused on hair diseases associated with COVID-19-related stress in the Southeast Asian region, especially among the Bangladeshi medical students. Hence, this study aimed to report the prevalence and examine the possible association between hair loss problems, especially TE, AA, scalp SD, and COVID-19-related stress among the medical students of Bangladesh. Our research hypothesis was COVID-related stress associated with TE, AA, and SD.
Materials and Methods
Study Design and Participants
This was a cross-sectional study that used an online data collection method. All the undergraduate medical students of Bangladesh were the study population. The sample size for the study was calculated by the following formula: , where z = 1.96 (for 95% confidence level), p is the estimated prevalence of hair loss problem, and d is the precision of error. A previous study has reported that the prevalence of hair loss problems during pandemic among Turkish participants was 53.1% (18). Considering this information, the calculated sample size was 404, assuming a 20% non-response rate.
All the undergraduate medical students studying in different government and private medical colleges were our study population. Due to COVID-19 pandemic and lockdown enforced by the government, all the medical colleges were continuing their academic activities online. Hence, we chose the online survey which is already used in a similar study (18). Our inclusion criteria were undergraduate students of both public and private medical colleges of Bangladesh of either sex aged > 18 years and who had access to social media where the survey was circulated. The students who did not use social media (Facebook) and were not attending online classes during the data collection period were excluded from the study. We used a private and common Facebook group for Bangladeshi medical students “Platform” (https://www.facebook.com/groups/platform.organization) where more than 40,000 medical students were joined. We posted the Google Forms link in the group and requested the students to fill it up. The link was active until we reached the targeted number of students.
Study Instrument
The questionnaire was developed after an extensive literature search in the English language as the medium of learning is English in medical colleges of Bangladesh. The first draft of the questionnaire was reviewed by a consultant psychiatrist and a consultant dermatologist for necessary modification. The questionnaire was pretested among 5% of the study sample (n = 20) for content validity and linguistic modification. Internal consistency was assessed by using Cronbach's α. The internal reliability of this study was found to be 0.910, indicating high internal consistency for our scale for this specific sample. The questionnaire has three parts, namely, (i) sociodemographic information, (ii) questions about pre- and post-pandemic TE, AA, and scalp SD, and (iii) information about COVID-19-related stress, and the three separate stress scales were employed to determine the level of stress.
The first dimension of the questionnaire includes demographic features (9 questions), such as name, age, sex, study year, family income, residence, relationship status, body mass index (BMI), and smoking status.
The second dimension includes hair loss problems about pre- and during the pandemic hair loss problems (6 questions), such as TE, AA, and scalp SD. TE is a term that refers to transient hair loss that frequently happens as a result of stress, shock, or a traumatic event. Individuals with this condition lose far more hair than the average 50–100 hairs each day (21).
The AA is a chronic inflammatory complex and widespread autoimmune skin disease that causes sudden non-scarring hair loss on the scalp, face, and sometimes other body parts (22). Acute or chronic psycho-emotional stress or psychological distress may be causing the initiation and progress of AA (23, 24).
The SD is an itchy rash covered in flaky scales condition referred to as dandruff, oily eczema, and seborrheic eczema (25). There is strong evidence of a possible link between stressful life events and episodes of scalp SD (8, 18).
The participants were asked about their scalp hair loss of more than 100 strands a day before and during the pandemic for TE, about focal hair loss-related questions (focal hair loss; also known as ringworm, oval or round para-shaped or wider, sharply circumscribed complete hair loss) for AA, and about the redness of the scalp, dandruff, itching, and oily eczema that caused the complaints before and during the pandemic period for scalp SD.
The third dimension included 3 validated stress scales to determine the level of stress of individuals.
COVID-19 Fear Scale
This scale was used to find out the effects of coronavirus on mental health, such as fear, anxiety, and stress (26). This scale is also validated for the Bangladeshi population (27). Using a five-item Likert-type scale, the participants rated their degree of agreement with the claims. Answers included “strongly disagree” to “strongly agree.” The lowest possible score for each question is 1 and the highest possible score is 5. The sum of each item's scores yields a cumulative ranking (ranging from 7 to 35). The higher the ranking, the more concerned and stressed about COVID-19. A score of 20 or higher is considered a fear of COVID-19. The scale demonstrated acceptable internal consistency (Cronbach's α 0.89).
Impact of Event Scale Specific for COVID-19
The IES-COVID-19 is a reliable indicator of traumatic stress symptoms due to the COVID-19 epidemic. It is an extension of the commonly used IES (28). This scale has 15 items. Every item is rated on a 4-point scale ranging from “not at all”−0 over “seldom”−1 and “sometimes”−3 to “often”−5. In terms of COVID-19, higher scores suggest a more significant psychological effect of the situation. A score of 26 or higher is considered as developing post-traumatic stress disorder (29). This scale is also previously used among the Bangladeshi population (12). The scale demonstrated acceptable internal consistency (Cronbach's α 0.86).
COVID-19 Student Stress Questionnaire
This is a recently created measuring instrument for evaluating the sources of stress associated with the COVID-19 pandemic lockdown among university students (30). There are 7 questions included in the scale related to personal and academic life's stresses during COVID-19 pandemic. It consists of 7 items on a 5-point Likert-type scale ranging from zero (“Not at all stressful”) to four (“Extremely stressful”). The scale provides a Global stress score ranging from 0 to 28. Scores of 6 or below indicate low levels of perceived COVID-19-related Global stress, scores of 7–15 indicate average levels of perceived COVID-19-related Global stress, and scores of 16 or more indicate high levels of perceived COVID-19-related Global stress among university students. The scale demonstrated acceptable internal consistency (Cronbach's α 0.88).
Ethical Consideration
Ethical approval was obtained from the Ethical Review Committee of the Public Health Foundation, Bangladesh (PHF, BD) (ref. no. 03/2021). Informed written consent was obtained via email from participants before inclusion.
Statistical Analysis
All the statistical analyses were carried out using SPSS version 25.0. For continuous variables, a mean with standard deviation was used, and for nominal variables, a frequency distribution was used. The chi-square test and logistic regression models are used to find out the association between hair diseases and COVID-19-related stress with sociodemographic variables. The variables achieving p <0.2 in the bivariate analysis were included in the multiple logistic regression model (Nagelkerke's R2 = 0.314). Significant results were interpreted as p <0.05 with 95% CI.
Results
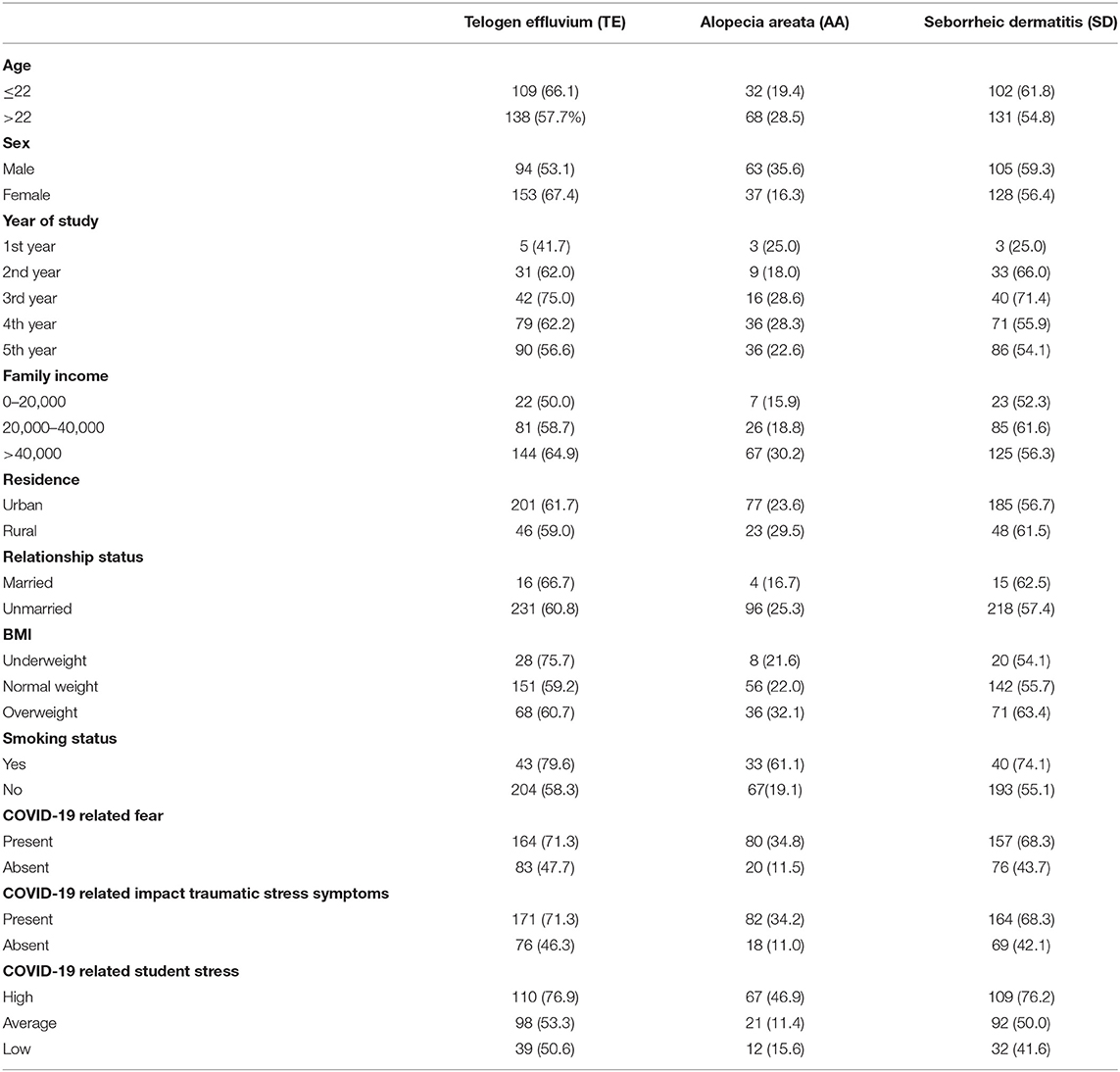
Among 404 participants included in our study, female participants were predominant (56%) and most of them (81%) hailed from urban areas. The majority of the participants belonged to the middle (34%) or higher (55%) income families (Table 1).
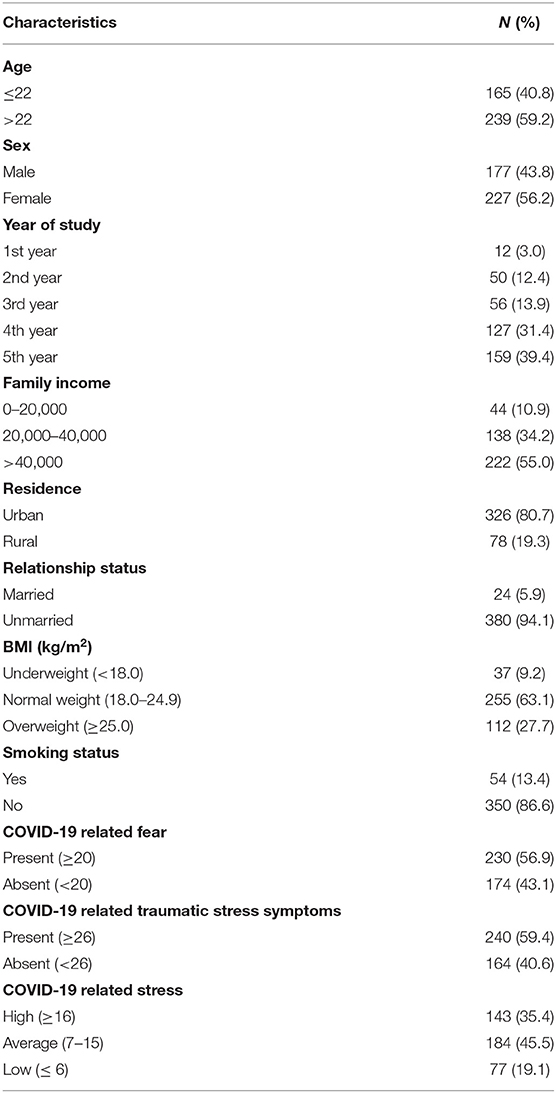
Table 1. Sociodemographic characteristics and COVID-19 pandemic-related stresses of the participants (n = 404).
It was found that more than half of the participants had COVID-19-related fear and COVID-19-related impact traumatic stress symptoms (56.9 and 59.4% consecutively). In addition, 35.4% of participants had high COVID-19-related student stress.
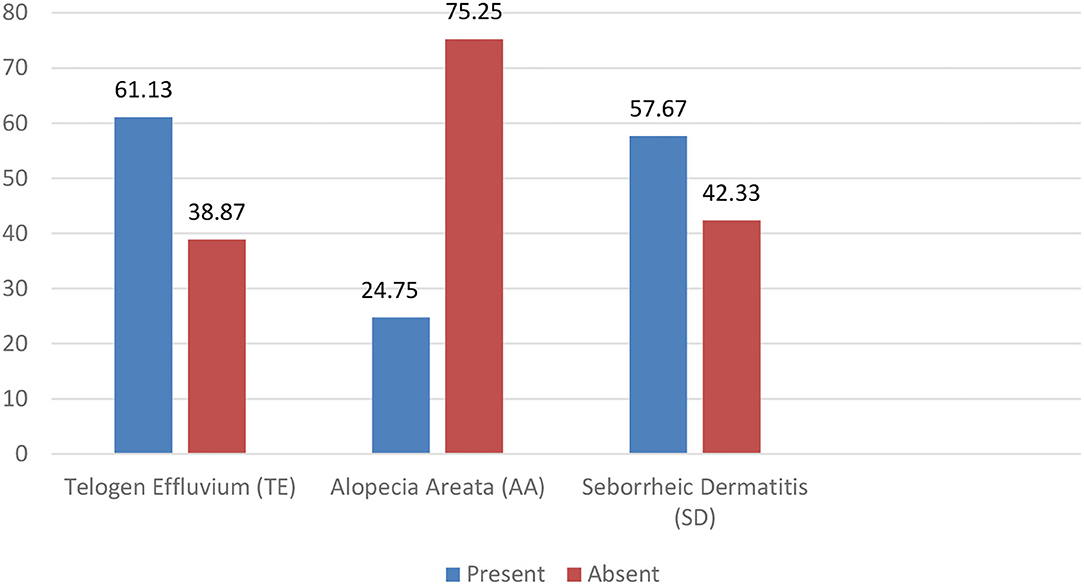
In our study, the prevalence of TE, AA, and SD was revealed consequently 61.13% (n = 247), 24.75% (n = 100), and 57.67% (n = 233) (Figure 1).
In our study, female medical students had more prevalence of TE (67.4%); in contrast, SD was more common among male students (59.3%). In addition, TE was more common among first- and third-year students, and AA was more common among fourth-year students. Urban people have more TE than rural people, but, in contrast, rural people have more SD. Persons who smoke have more prevalence in all three conditions (i.e., TE, AA, and SD). Similarly, persons having COVID-19-related fear, COVID-19-related traumatic stress symptoms, and high COVID-19-related student stress have a higher prevalence in all three conditions (i.e., TE, AA, and SD) too. Other prevalence of different groups is shown in Table 2.
In the multiple logistic regression model, it was revealed that male participants had two times more tendency to have AA than female participants (aOR 2.12, 95% CI 1.15–3.93, p= 0.016) and smoker participants had four and three times higher risk for developing TE (aOR 4.194, 95% CI 1.839–9.567, p = 0.001) and AA (aOR 2.930, 95% CI 1.290–6.658, p = 0.010) consequently than nonsmoker participants (Table 3).
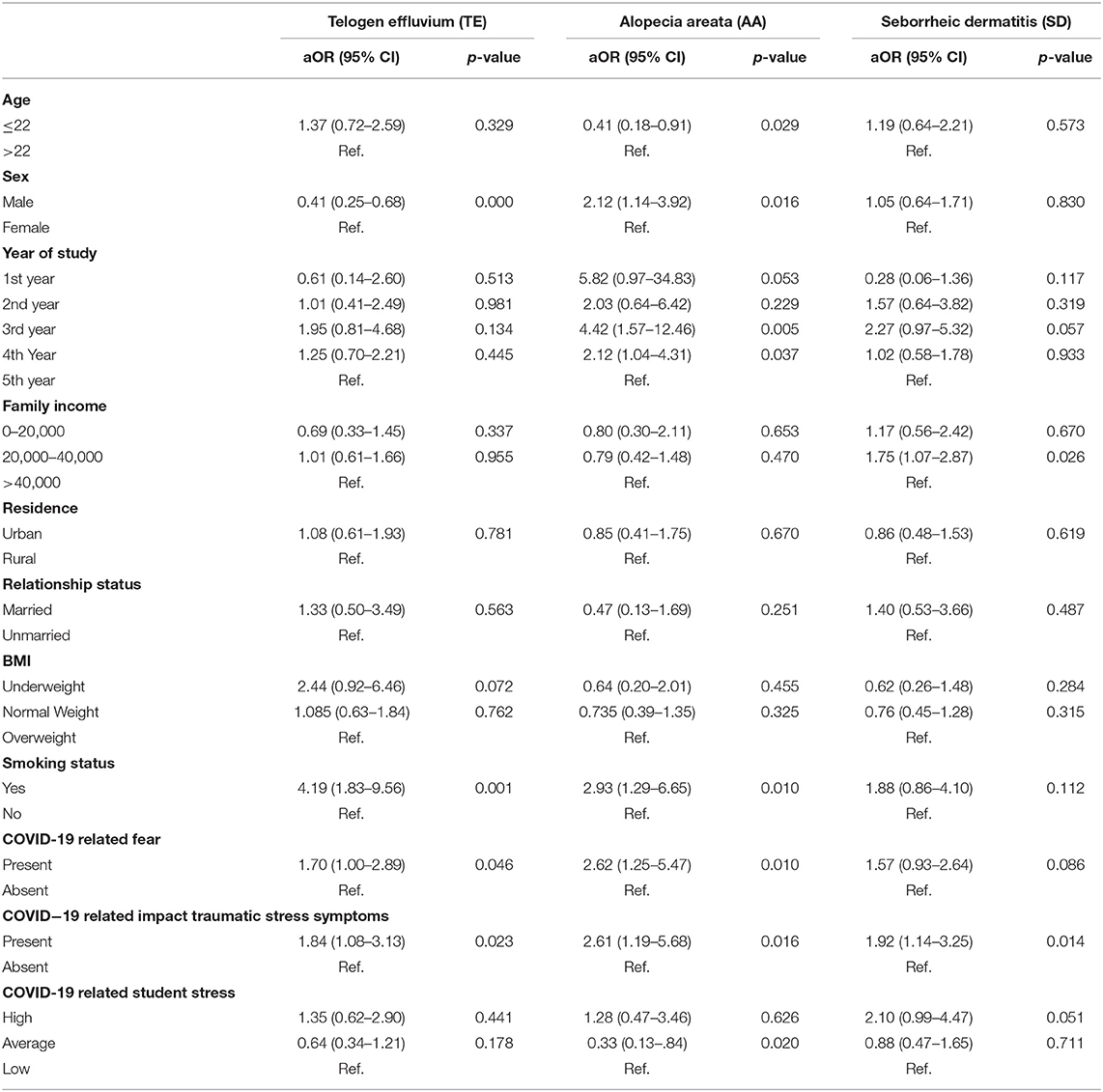
Table 3. Multiple logistic regression model for the variables associated with TE, AA, and SD (n = 404).
Discussion
Psychological stress can have an effect on the course of several stress-sensitive skin diseases, such as SD, urticaria, acne vulgaris, TE, AA, and pruritus, causing actual or perceived aggravation of the disease (5, 6, 31). The importance of the brain-skin axis has been repeatedly underlined in cases when there is a complicated link between the brain and the skin (3). Psychological stress influences hypothalamic–pituitary–adrenocortical (HPA) axis hormones as well as stress mediators, such as neuropeptides and cytokine profiles, affecting the immune response which impairs the skin's capacity to adapt to stressful situations. These stress-induced skin alterations might contribute to the worsening of skin disease (32, 33). Furthermore, the link between a stressful situation and any subsequent alterations in the hair development cycle has resulted in the identification of the brain-hair follicle axis. Specific neuropeptides, neurotransmitters, and hormones released along this axis, in particular, can induce substantial alterations in the hair development cycle (1, 7).
The recent outbreak of COVID-19 has exerted tremendous psychological pressure on people of all classes globally (34). These psychological alterations are triggered by fear, stress, anxiety, or uncertainty (35). It has altered the functioning of educational institutions globally, causing significant changes in the everyday lives of students. Due to this unexpected stressful situation, this group has experienced psychological stresses as a result of a dramatic shift in their daily routine (36). Such data suggest that the ongoing psychosocial stress caused by the present pandemic can contribute to the aggravation or onset of prevalent skin and hair diseases at the population level. All of these stressors may enhance the likelihood of developing psychiatric-related dermatologic diseases linked with the COVID-19 pandemic. According to few studies, current pandemic circumstances have already started to alter the course of a variety of skin and scalp diseases, such as TE, AA, and SD in scalp, and other skin diseases (18, 19).
In our study, we selected medical students as a vulnerable group to evaluate pandemic stress associated with hair diseases. Medical students are frequently seen as having a greater level of psychological stress and due to the closure of educational institutions, mental health has been hampered to students all over the country (17). Apart from the general population, medical students are at a higher risk of psychological distress as a result of confronting the new threat of pandemic (16). In addition, in Bangladesh, there is a report of a higher prevalence of depression among medical students, as well as a higher suicidal tendency (15). A large percentage of Bangladeshi medical students are experiencing adverse psychological effects as a result of the pandemic (17). The purpose of this study was to determine the potential association of COVID-19-related stress with hair diseases among medical students in Bangladesh.
In our study, the prevalence of TE, AA, and SD was 61, 25, and 58%, respectively. To the best of our knowledge, there is hardly any previous study on this issue from our country to compare with. However, during this virus outbreak, a number of studies conducted in different countries to explore the pandemic's stress-related hair diseases demonstrate a significant prevalence of hair diseases during this pandemic (18, 37–39).
According to a study conducted in Turkey, the prevalence of TE, AA, and SD was 28, 2.8, and 20%, respectively, in the participants which is comparatively lower than our findings (18). Another Turkish finding revealed that the frequency of AA increased considerably during the COVID-19 pandemic which was hypothesized to be associated with short-term stress (19). Another study from Italy reported that 12.5% of participants experienced relapses of AA during this pandemic (39).
With the global spread of COVID-19 starting in March 2020, physicians and patients have started to report an increase in hair loss (40). Emotional stress associated with COVID-19 pandemic can be associated with TE and SD which usually appear following a stressful incident (18). However, we found that COVID-19-related post-traumatic symptoms and COVID-19-related stress or fear were also associated with all three diseases (i.e., TE, AA, and SD). A previous study has reported that the AA (1.48%) and TE (2.17%) significantly increased during the COVID-19 pandemic along with other skin diseases' dermatological outpatient department. As a result of this investigation, it has been demonstrated that the COVID-19 pandemic sheds fresh light on the emotional stress period associated with hair diseases that may have been induced by psychological imbalances. When compared to the previous year, the percentages of AA and TE increased by 2.83 and 5.51 times, respectively (37). Another study reported that within the first 10 days following the COVID-19 outbreak, SD increased by 4.5% in the dermatology clinic of a tertiary care hospital (37). Some other studies, before the pandemic, identified hair loss and SD as the most common stress-related skin disorders among young adults (41, 42).
In contrast, we have found that smokers had a higher risk for developing TE and AA There is a hypothesis that exogenous nicotine might promote overstimulation of the cellular nicotinic acetylcholine receptors, resulting in receptor desensitization which, in turn, contributes to hair follicle loss by activating keratinocyte-specific programmed cell death pathways (43, 44). Further studies are needed with different subsets of Bangladeshi adult smokers to investigate this particular finding in detail.
Stress has been recognized as an exacerbating element in stress-related skin and hair disorders on several occasions. Such data suggest that the present pandemic's long-term psychological stress may cause exacerbations or the development of skin and hair diseases. However, there is a limitation of data on the interplay of pandemic-related stress and psychological risk factors among people with skin and hair disorders during the COVID-19 pandemic.
As the study's findings indicated a significant degree of stress connected with hair diseases among medical students, we have recommended that the student support system assists and cares for this group. However, this study will benefit a subset of the population that has been exposed to stress for an extended period of time and has developed skin and hair disorders. It is critical to target stress-reduction tactics and treatment facilities in low-resource settings to individuals who are experiencing any level of psychological stress in order to avoid the development of more serious skin disorders associated with stress. Another longitudinal research might be conducted with a cohort of students to determine the degree of stress experienced by students during their undergraduate medical years and the factors that contribute to it.
Nonetheless, these cases suggest that COVID-19 infection, as well as the associated psychological and physiological stress, is capable of causing hair disease. Further research will be required as the pandemic progresses to determine the long-term prevalence and prognosis of hair diseases linked with COVID-19 infection.
This study has several limitations. The major flaw was being a self-reported online survey clinical diagnosis of the hair loss problems was not possible. We can potentially interpret the results largely based on disease symptoms without an exact clinical diagnosis by registered physicians. Moreover, recall bias could not be escaped. Besides, because of its cross-sectional design, causal effect of COVID-19 stress on hair diseases could not be established. Finally, the findings cannot be inferential at the population level as only a specific group of people were included.
Conclusion
Our study reported that a large number of medical students were experiencing TE, AA, and SD during the pandemic era. COVID-19-related stress and fear potentially have had an effect on these conditions. Further longitudinal and exploratory studies among different subsets of population are needed to enhance our understanding of short- and long-term direct psychological effects on skin and hair disease and to identify effective interventions to address such unique issues. This research opens several doors for psychodermatology to discuss this complex dynamic in the context of low resource settings, such as Bangladesh.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethical Review Committee of the Public Health Foundation, Bangladesh (PHF, BD) (ref. no. 03/2021). Informed written consent was obtained via email from participants before inclusion. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AM: conceptualization and study design, data collection, and writing—draft preparation. MAR: supervision, reviewing, and editing. TS and SS: data analysis and helping-draft preparation. MGR and MA: data collection and data formatting. MM and MH: reviewing of the draft manuscript for potential intellectual content. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would want to express our gratitude to all of the participants who voluntarily offered their time, illustrated their situations attentively, and provided honest and significant responses during this unexpected COVID-19 situation. In addition, we appreciate the research assistants (volunteers) who supported the online data collection for this research.
References
1. Jafferany M, King BH. Psychodermatology: a guide to understanding common psychocutaneous disorders. Prim Care Companion J Clin Psychiatry. (2007) 9:203–13. doi: 10.4088/PCC.v09n0306
2. Jafferany M, Franca K. Psychodermatology: basics concepts. Acta Derm Venereol. (2016) 96:35–7. doi: 10.2340/00015555-2378
3. Alexopoulos A, Chrousos GP. Stress-related skin disorders. Rev Endocr Metab Disord. (2016) 17:295–304. doi: 10.1007/s11154-016-9367-y
4. Gupta MA, Jarosz P, Gupta AK. Posttraumatic stress disorder (PTSD) and the dermatology patient. Clin Dermatol. (2017) 35:260–6. doi: 10.1016/j.clindermatol.2017.01.005
5. Poot F, Sampogna F, Onnis L. Basic knowledge in psychodermatology. J Eur Acad Dermatol Venereol. (2007) 21:227–34. doi: 10.1111/j.1468-3083.2006.01910.x
6. Garcovich S, Bersani FS, Chiricozzi A, De Simone C. Mass quarantine measures in the time of COVID-19 pandemic: psychosocial implications for chronic skin conditions and a call for qualitative studies. J Eur Acad Dermatology Venereol. (2020) 34:e293–4. doi: 10.1111/jdv.16535
7. Jafferany M, Patel A. Trichopsychodermatology: the psychiatric and psychosocial aspects of hair disorders. Dermatol Ther. (2020) 33:e13168. doi: 10.1111/dth.13168
8. Misery L, Touboul S, Vinçot C, Dutray S, Rolland-Jacob G, Consoli S-G, et al. [Stress and seborrheic dermatitis]. Ann Dermatol Venereol. (2007) 134:833–7. doi: 10.1016/S0151-9638(07)92826-4
9. Anwar S, Jafferany M. Trichotillomania: a psychopathological perspective and the psychiatric comorbidity of hair pulling. Acta Dermatovenerologica Alpina, Pannonica Adriat. (2019) 28:33–6. doi: 10.15570/actaapa.2019.7
10. Montano RLT, Acebes KML. Covid stress predicts depression, anxiety and stress symptoms of filipino respondents. Int J Res Bus Soc Sci. (2020) 9:78–103. doi: 10.20525/ijrbs.v9i4.773
11. WHO. Mental Health and COVID-19. WHO (2020). Available online at: https://www.who.int/teams/mental-health-andsubstance-use/covid-19
12. Khan AH, Sultana MS, Hossain S, Hasan MT, Ahmed HU, Sikder MT. The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: a cross-sectional pilot study. J Affect Disord. (2020) 277:121–8. doi: 10.1016/j.jad.2020.07.135
13. Faisal RA, Jobe MC, Ahmed O, Sharker T. Mental health status, anxiety, and depression levels of bangladeshi university students during the COVID-19 pandemic. Int J Ment Health Addict. (2021) 4:1–16. doi: 10.1007/s11469-020-00458-y
14. Akhtarul Islam M, Barna SD, Raihan H, Nafiul Alam Khan M, Tanvir Hossain M. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: a web-based cross-sectional survey. PLoS ONE. (2020) 15:e0238162. doi: 10.1371/journal.pone.0238162
15. Hasan MT, Hossain S, Das GR, Podder V, Mowri NA, Ghosh A, et al. Depression, sleeping pattern, and suicidal ideation among medical students in Bangladesh: a cross-sectional pilot study. J Public Heal. (2020) 1–9. doi: 10.30682/nm2003f Available online at: https://link.springer.com/article/10.1007/s10389-020-01304-0
16. SeetanID K, Al-Zubi M, Rubbai Y, Athamneh M, KhameesID atasim, Radaideh T. Impact of COVID-19 on medical students' mental wellbeing in Jordan. PLoS ONE. (2021) 16:e0253295doi: 10.1371/journal.pone.0253295
17. Safa F, Anjum A, Hossain S, Trisa TI, Alam SF, Abdur Rafi M, et al. Immediate psychological responses during the initial period of the COVID-19 pandemic among Bangladeshi medical students. Child Youth Serv Rev. (2021) 122:105912. doi: 10.1016/j.childyouth.2020.105912
18. Turkmen D, Altunisik N, Sener S, Colak C. Evaluation of the effects of COVID-19 pandemic on hair diseases through a web-based questionnaire. Dermatol Ther. (2020) 33:e13923. doi: 10.1111/dth.13923
19. Kutlu Ö, Aktaş H, Imren IG, Metin A. Short-term stress-related increasing cases of alopecia areata during the COVID-19 pandemic. J Dermatolog Treat. (2020) 33:1177. doi: 10.1080/09546634.2020.1782820
20. Hussain N, Agarwala P, Iqbal K, Omar HMS, Jangid G, Patel V, et al. A systematic review of acute telogen effluvium, a harrowing post-COVID-19 manifestation. J Med Virol. (2022) 94:1391–401. doi: 10.1002/jmv.27534
21. Rivetti N, Barruscotti S. Management of telogen effluvium during the COVID-19 emergency: psychological implications. Dermatol. Ther. (2020) 33:e13648. doi: 10.1111/dth.13648
22. Gilhar A, Kalish RS. Alopecia areata: a tissue specific autoimmune disease of the hair follicle. Autoimmunity Rev. (2006) 5:64–9. doi: 10.1016/j.autrev.2005.07.001
23. Willemsen R, Roseeuw D, Vanderlinden J. Alexithymia and dermatology: the state of the art. Int J Dermatol. (2008) 47:903–10. doi: 10.1111/j.1365-4632.2008.03726.x
24. Ari B, Cenesizoglu E, Denli Y. Alopesi areata hastalarinda psikiyatrik belirtiler/psychiatric symptoms in patients with alopecia areata. Turkderm. (2011) 45:203. doi: 10.4274/turkderm.31549
25. Naldi L, Diphoorn J. Seborrhoeic dermatitis of the scalp. BMJ Clin Evid. (2015) 2015. Available online at: https://www.researchgate.net/publication/50592346_Seborrhoeic_dermatitis
26. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. (2020) 27:1–9. doi: 10.1007/s11469-020-00270-8
27. Sakib N, Bhuiyan AKMI, Hossain S, Al Mamun F, Hosen I, Abdullah AH, et al. Psychometric validation of the bangla fear of COVID-19 scale: confirmatory factor analysis and rasch analysis. Int J Ment Health Addict. (2020) 11:1–12. doi: 10.1007/s11469-020-00289-x
28. Vanaken L, Scheveneels S, Belmans E, Hermans D. Validation of the impact of event scale with modifications for COVID-19 (IES-COVID19). Front Psychiatry. (2020) 11:738. doi: 10.3389/fpsyt.2020.00738
29. Horowitz M, Wilner N, Alvarez W. Impact of event scale: a measure of subjective stress : psychosomatic medicine. Psychosom Med. (1979) 41:209–18. doi: 10.1097/00006842-197905000-00004
30. Zurlo MC, Cattaneo Della Volta MF, Vallone F. COVID-19 student stress questionnaire: development and validation of a questionnaire to evaluate students' stressors related to the coronavirus pandemic lockdown Front Psychol. (2020) 11:576758. doi: 10.3389/fpsyg.2020.576758
31. Basavaraj KH, Navya MA, Rashmi R. Relevance of psychiatry in dermatology: present concepts. Indian J Psychiatry. (2010) 52:270. doi: 10.4103/0019-5545.70992
32. Kim JE, Cho BK, Cho DH, Park HJ. Expression of hypothalamic-pituitary-adrenal axis in common skin diseases: evidence of its association with stress-related disease activity. Acta Derm Venereol. (2013) 93:387–93. doi: 10.2340/00015555-1557
33. Peters EM. Stressed skin?–a molecular psychosomatic update on stress-causes and effects in dermatologic diseases. J Dtsch Dermatol Ges. (2016) 14:233–52. doi: 10.1111/ddg.12957
34. Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob Health BioMed Central. (2020) 16:57. doi: 10.1186/s12992-020-00589-w
35. Zhang J, Lu H, Zeng H, Zhang S, Du Q, Jiang T, et al. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav Immun. (2020) 87:49–50. doi: 10.1016/j.bbi.2020.04.031
36. Browning Id MHEM, Larson Id LR, Sharaievska I, Rigolon A, Mcanirlin O, Mullenbachid L, et al. Psychological impacts from COVID-19 among university students: risk factors across seven states in the United States. PLoS ONE. (2021) 16:e0245327. doi: 10.1371/journal.pone.0245327
37. Kutlu Ö, Güneş R, Coerdt K, Metin A, Khachemoune A. The effect of the “stay-at-home” policy on requests for dermatology outpatient clinic visits after the COVID-19 outbreak. Dermatol Ther. (2020) 33:e13581. doi: 10.1111/dth.13581
38. Olds H, Liu J, Luk K, Lim HW, Ozog D, Rambhatla P V. Telogen effluvium associated with COVID-19 infection. Dermatol Ther. (2021) 34:e14761. doi: 10.1111/dth.14761
39. Rinaldi F, Trink A, Giuliani G, Pinto D. Italian survey for the evaluation of the effects of coronavirus disease 2019 (COVID-19) pandemic on alopecia areata recurrence. Dermatol Ther. (2021) 11:339–45. doi: 10.1007/s13555-021-00498-9
40. Kutlu Ö, Metin A. Relative changes in the pattern of diseases presenting in dermatology outpatient clinic in the era of the COVID-19 pandemic. Dermatol Ther. (2020) 33:e14096. doi: 10.1111/dth.14096
41. Saif GA Bin, Alotaibi HM, Alzolibani AA, Almodihesh NA, Albraidi HF, Alotaibi NM, et al. Association of psychological stress with skin symptoms among medical students. Saudi Med J. (2018) 39:59. doi: 10.15537/smj.2018.1.21231
42. Schut C, Mollanazar NK, Sethi M, Nattkemper LA, Valdes-Rodriguez R, Lovell MM, et al. Psychological stress and skin symptoms in college students: results of a cross-sectional web-based questionnaire study. Acta Derm Venereol. (2016) 96:550–1. doi: 10.2340/00015555-2291
43. Salem AS, Ibrahim HS, Abdelaziz HH, Elsaie ML. Implications of cigarette smoking on early-onset androgenetic alopecia: a cross-sectional study. J Cosmet Dermatol. (2021) 20:1318–24. doi: 10.1111/jocd.13727
Keywords: hair fall diseases, telogen effluvium, alopecia areata, seborrheic dermatitis, COVID-19 stress
Citation: Mahadi AR, Rafi MA, Shahriar T, Seemanta S, Rabbani MG, Akter M, Majumder MI and Hasan MT (2022) Association Between Hair Diseases and COVID-19 Pandemic-Related Stress: A Cross-Sectional Study Analysis. Front. Med. 9:876561. doi: 10.3389/fmed.2022.876561
Received: 15 February 2022; Accepted: 05 April 2022;
Published: 12 May 2022.
Edited by:
Giovanni Damiani, University of Milan, ItalyReviewed by:
Martina Burlando, San Martino Hospital (IRCCS), ItalyBijaya Kumar Padhi, Post Graduate Institute of Medical Education and Research (PGIMER), India
Copyright © 2022 Mahadi, Rafi, Shahriar, Seemanta, Rabbani, Akter, Majumder and Hasan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ashrafur Rahaman Mahadi, ashrafmahadi123mahadi@gmail.com
 Ashrafur Rahaman Mahadi
Ashrafur Rahaman Mahadi Md. Abdur Rafi
Md. Abdur Rafi Tasnim Shahriar
Tasnim Shahriar Senjuti Seemanta5
Senjuti Seemanta5  Md. Golam Rabbani
Md. Golam Rabbani Munjarin Akter
Munjarin Akter Mahabubul Islam Majumder
Mahabubul Islam Majumder M. Tasdik Hasan
M. Tasdik Hasan