Spontaneous pregnancy after thread-embedding therapy treatment with premature ovarian insufficiency after unilateral oophorectomy: a case report
- Department of Acupuncture, Dongzhimen Hospital, Beijing University of Chinese Medicine, Beijing, China
Premature ovarian insufficiency (POI) is a condition characterized by menstrual disturbance, subfertility, and estrogen deficiency symptoms. Women with POI have a small chance of natural conception, which may be even smaller when complicated with unilateral ovarian due to reduction of the ovarian follicular reserve. In China, acupuncture has been widely used to treat POI and POI-induced infertility, and studies have shown that acupuncture is helpful for improving ovarian function. Thread-embedding therapy is a method of acupuncture treatment development and extension, which can make the acupuncture effect last. In this article, we report a patient diagnosed with POI after unilateral oophorectomy (UO) who spontaneously conceived after thread-embedding therapy. Thread-embedding therapy may improve ovarian function in patients with POI, thereby providing a treatment strategy for infertility in patients with POI. This case report was written in accordance with the CARE guidelines.
1 Introduction
Premature ovarian insufficiency (POI) is a clinical syndrome defined by loss of ovarian activity that occurs in individuals less than 40 years old. It usually presents with menstrual disturbance (secondary amenorrhea or oligomenorrhea), subfertility, and estrogen deficiency symptoms (1, 2). The diagnostic criteria for POI are amenorrhea or oligomenorrhea (≥4 months) and two FSH levels higher than 25 IU/L (>4 weeks apart) according to the European Society of Human Reproduction and Embryology guidelines (1). The aetiologies of POI are still not fully determined, and its occurrence may be related to the following causes: chromosomal abnormalities, genetics, iatrogenic factors, autoimmunity, metabolism, infection, and environmental pollutants (3, 4). The global overall prevalence of POI was calculated as 3.7% (5). It has a significant negative impact on physical health, psychological well-being and the quality of life of patients (1, 6).
POI is one of the main factors affecting female fertility (7). Women with POI have a small chance of spontaneous pregnancy (1). Hormone replacement therapy is a main treatment for POI and can ameliorate the clinical complications caused by low estrogen levels (4). However, it has little or no benefit for improving the fertility rate and may increase the risk of ovarian cancer, breast cancer, endometrial cancer, thrombotic disease, meningioma, and other diseases (8, 9). Acupuncture therapy is a method of preventing and treating diseases that originated in ancient China. Due to its simple operation, satisfactory effect and low cost, acupuncture has been used increasingly frequently in clinical treatment (10). Thread-embedding therapy, as a type of acupuncture method, is widely used in the clinic. We will present a patient with POI after UO who conceived after thread-embedding therapy, which is rarely reported to our knowledge. The patient only retained her left ovary, which made pregnancy more difficult while experiencing POI. This study was approved by the ethics committee of Dongzhimen Hospital, Beijing University of Chinese Medicine (Approval no. 2022DZMEC-257–01). Signed written informed consents were obtained from the patient.
2 Case presentation
2.1 Medical history
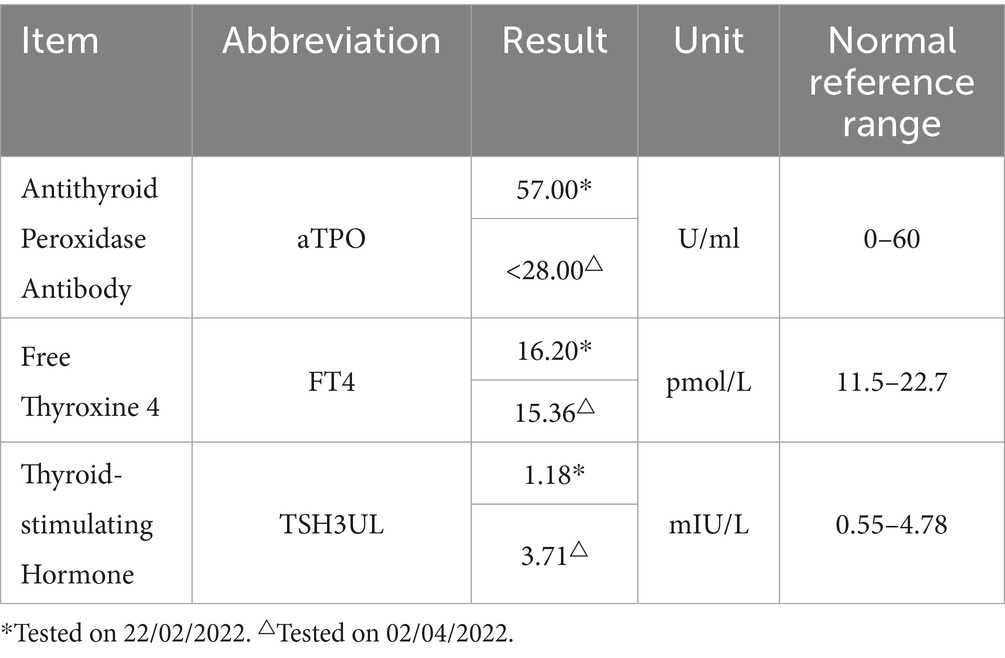
A 35-year-old woman presented to Department of Acupuncture, Dongzhimen Hospital, Beijing University of Chinese Medicine complaining of oligomenorrhea for more than 4 months (weighed 60 kg and was 162 cm tall, body mass index [BMI] 23 kg/m2). She denied any thyroid (related blood tests listed in Table 1) and adrenal cortex function-related medical history, any related family history or any exposure to radioactive materials or anticancer drugs. The patient had regular cycles and a relatively large blood flow after menarche at 12 years of age, accompanied by dysmenorrhea and blood clots. She married at the age of 23 with no contraception all the time. In 2017, she received right oophorectomy due to the torsion of a right ovarian cyst. She reported that she began experiencing menstrual disorder after that operation. Unfortunately, relevant records and evidence were not available, and she did not receive any treatment. She conceived in the same year, but an inevitable abortion occurred in March 2018 because of a low lying placenta and preterm premature rupture of membranes. She took traditional Chinese medicine herbs intermittently for 6 months after the abortion, and the symptoms seemed to be relieved.
However, the effect did not last long. She had not conceived for 2 years, so she tested her hormonal blood on August 4, 2020, which showed a high level of follicle-stimulating hormone (FSH) at 25.80 IU/L (normal reference range: follicular phase 3.85–8.78 IU/L), together with luteinizing hormone (LH) at 19.81 IU/L (normal reference range: follicular phase 2.12–10.89 IU/L) and estradiol (E2) at 78 pg./mL (normal reference range: follicular phase 27–122 pg./mL). A repeat test on September 12, 2020, at the same hospital confirmed POI (FSH: 37.80 IU/L, LH: 15.34 IU/L, E2: 25 pg./mL). Transvaginal sonography conducted on August 28, 2020 showed that the left ovary was 3.3 cm*1.8 cm in length and width, and the antral follicle count (AFC) was only 1. The left ovarian arterial blood flow was so low that the peak systolic velocity (PSV), end-diastolic velocity (EDV), resistance index (RI) and pulsatility index (PI) were all undetectable by Doppler blood flow measurements.
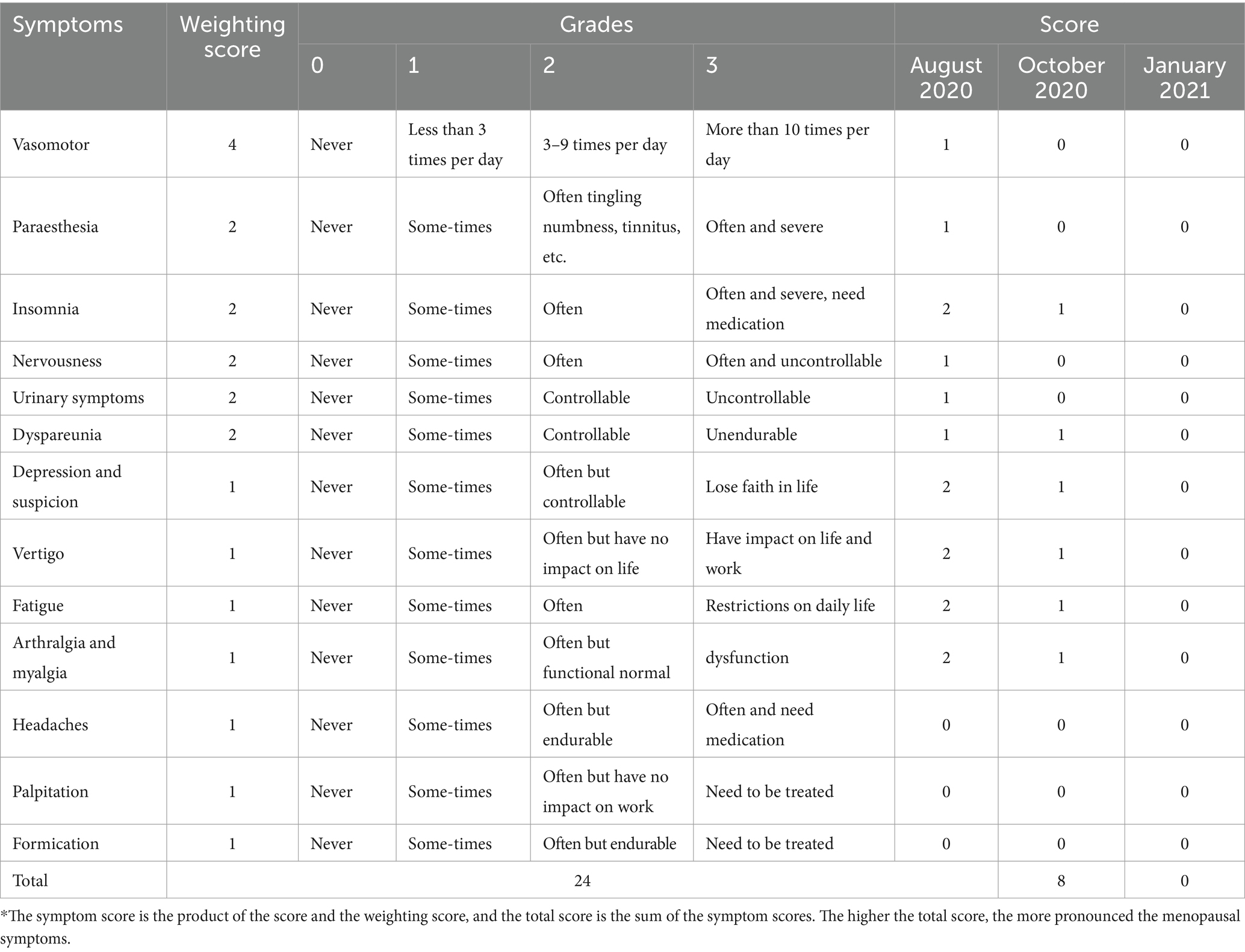
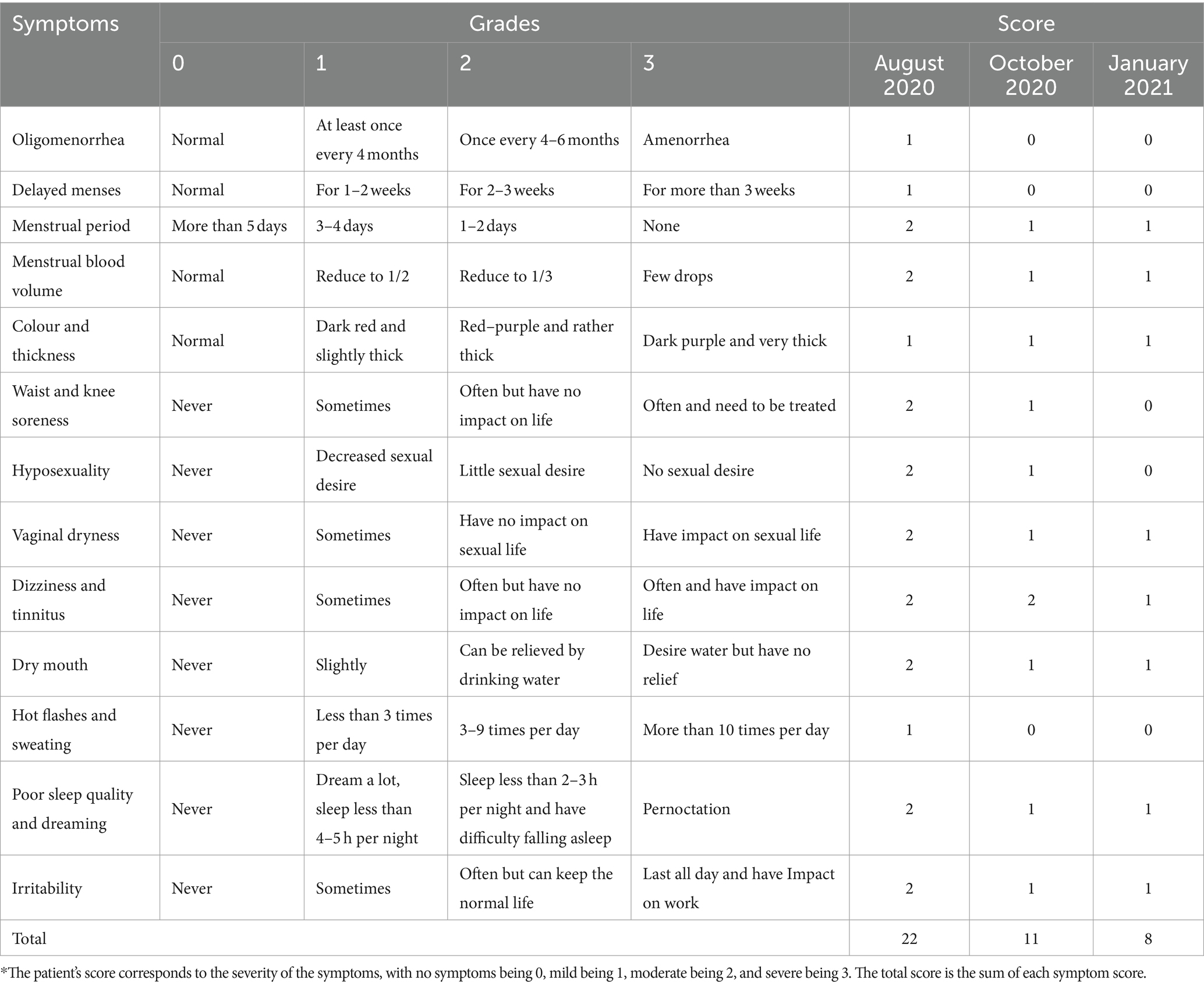
POI symptoms also exist. In August 2020, her modified Kupperman index (mKMI) (11) was 24, with moderate symptoms of insomnia, depression and suspicion, vertigo, fatigue, arthralgia and myalgia as well as mild symptoms of vasomotor, paraesthesia, nervousness, urinary symptoms and dyspareunia. Her score of TCM syndrome [developed referring to Guidance Principle of Clinical Study on New Drug of Traditional Chinese Medicine (12) and Gynaecology of Traditional Chinese Medicine (13)] was 22 with the following symptoms: menses occurred at least once every 4 months and lasted 1–2 days, and the period was delayed for 1–2 weeks; menstrual blood had a 2/3 reduction in volume from the original, which was slightly thick and dark red in colour; moderate symptoms of waist and knee soreness, hyposexuality, vaginal dryness, dizziness, tinnitus, dry mouth, poor sleep quality, dreaming and irritability; and a mild symptom of hot flashes and sweating. Physical examination was normal.
2.2 Treatment process
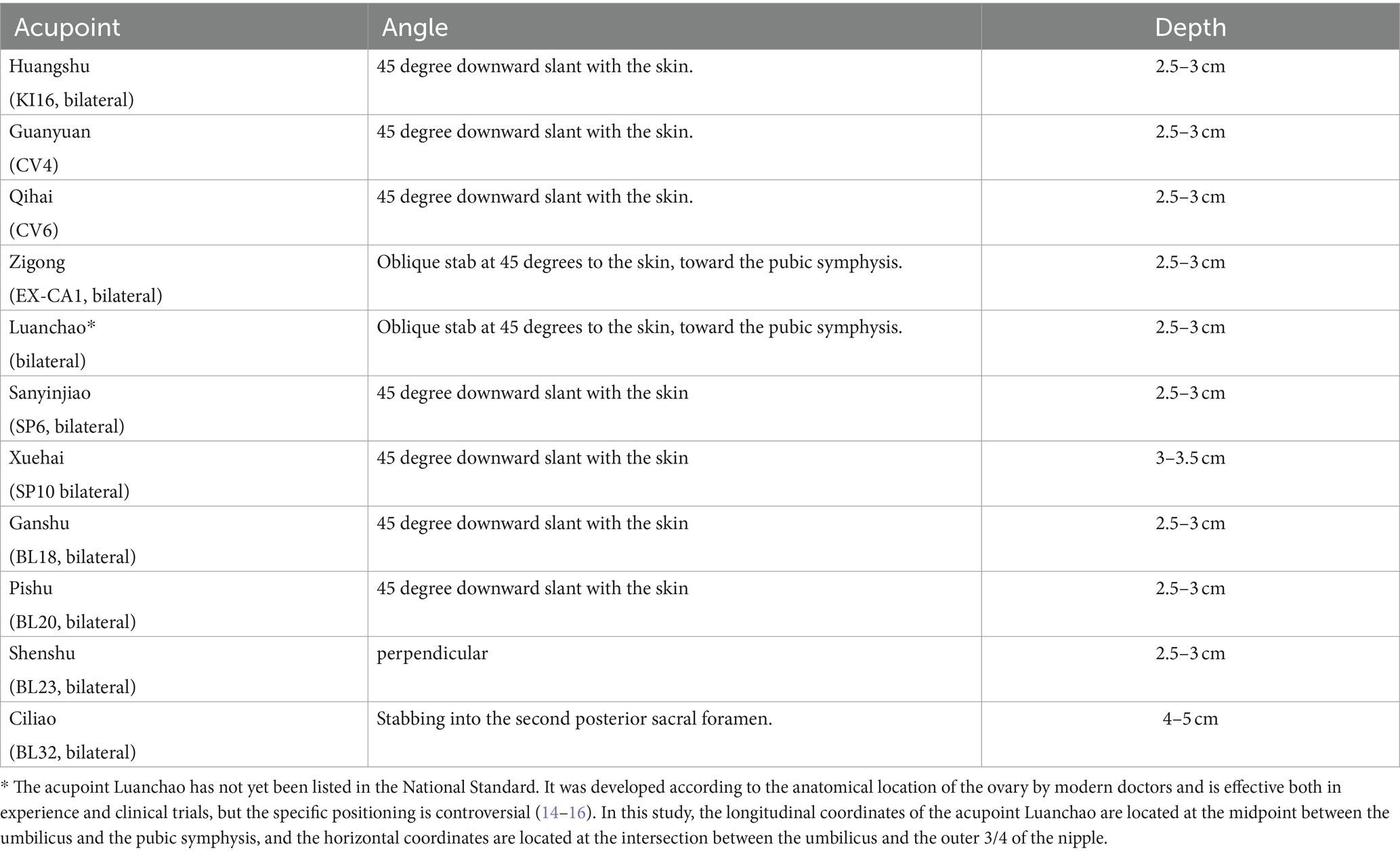
We prescribed thread-embedding therapy once every 2 weeks for the patient. The following acupoints were chosen: Huangshu (KI16 bilateral), Qihai (CV6), Guanyuan (CV4), Zigong (EX-CA1 bilateral), Luanchao (bilateral), Xuehai (SP10 bilateral), Sanyinjiao (SP6 bilateral), Ganshu (BL18 bilateral), Pishu (BL20 bilateral), Shenshu (BL23 bilateral), and Ciliao (BL32 bilateral). Their location are based on the National Standards of P. R GB∕T 12346–2021 Nomenclature and location of meridian points and National Standards of P. R GB∕T 40997–2021 nomenclature and location of extra points in common use. Figure 1 illustrates their location on the human body. Through the thread-embedding needle, a short segment of absorbable collagen thread will be embedded into acupoints, together with the adjustment of the needling angle, to evoke a “de qi” sensation (manifesting as soreness, numbness, heaviness, and distention). The operating method follows the National Standards of P.R GB/T 21709.10–2008 Standard manipulations of acupuncture and moxibustion—Part 10 Thread-embedding therapy. In short, the patient were placed in the supine position first and then in the prone position, and the acpoints was fully exposed and disinfected. The operator cleaned and disinfected his or her hands, opened the embedding bag, wore sterile gloves, and took a 4–0 absorbable surgical suture with a length of 2 cm (Shandong Boda Medical Products CO., LTD, BD150301, Figure 2A) with sterile tweezers. It was placed in the front of the tube of a 0.7 mm × 60 mm disposable thread-embedding needle (Zhenjiang Gaoguan Medical Equipment Co., LTD, YZB/Su 0480–2007, Figures 2B,C), and the thread was loaded into the needle body from the tip (the needle core was slightly back so that the thread was flush with the inner edge of the needle tip). The angles and depths of needling at each acupuncture point are listed in Table 2, which is appropriate to feel acid and swelling at the acupoints specifically. Then, push the needle core while withdrawing the needle tube at the same time (Figure 2D). After the needle is out, press the acupoint with a sterilized cotton swab for a moment to prevent bleeding. The patient described her experience of thread-embedding therapy as “feeling good physically.”

Figure 1. Location of acupoints on the human body. By Figdraw. (A) Abdominal acupoints. (B) Dorsal acupoints. (C) Femoral acupoints. (D) Crural acupoints.

Figure 2. Process of thread-embedding therapy. (A) Absorbable surgical suture. (B) Disposable thread-embedding needle. (C) Place the thread in the front of the tube of the needle. (D) Puncture the needle into the acupoint. Then, push the needle core while withdrawing the needle tube at the same time.
2.3 Follow up and outcomes
After 4 rounds of thread-embedding, the patient conceived in October 2020 and thus suspended the therapy. At that time, her mKMI was reduced sharply to 8, and the score of TCM syndrome was reduced to 11. Unfortunately, curettage was performed in December 2020 because of embryo arrest. One month later, she continued to receive the therapy once every 2 weeks for 8 months, which was sustained until August 2021. The follow-up in January 2021 showed an even better outcome in mKMI and TCM syndrome scores of 0 and 8, respectively. A hormonal blood test conducted on January 26, 2021, also showed that all three indices had returned to normal (FSH: 5.53 IU/L, LH: 2.24 IU/L, E2: 89.53 pg./mL). Each of the patient’s sex hormones was measured during the second to the fourth day of menstruation. The details of her mKMI and score of TCM syndrome are shown in Tables 3, 4. The changes in her hormone level and the treatment timeline are demonstrated, respectively, in Figures 3, 4.
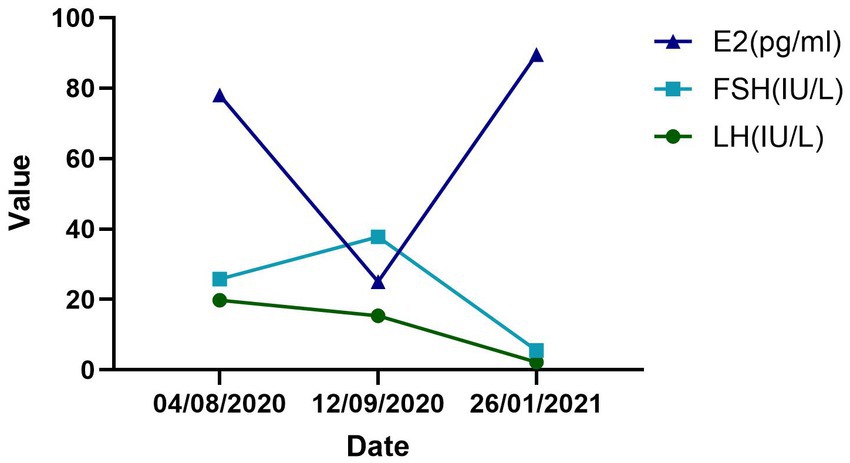
Figure 3. Female hormonal change values. August 4, 2020 and September 12, 2020 were the times before treatment. January 26, 2021 was the time during the treatment period.
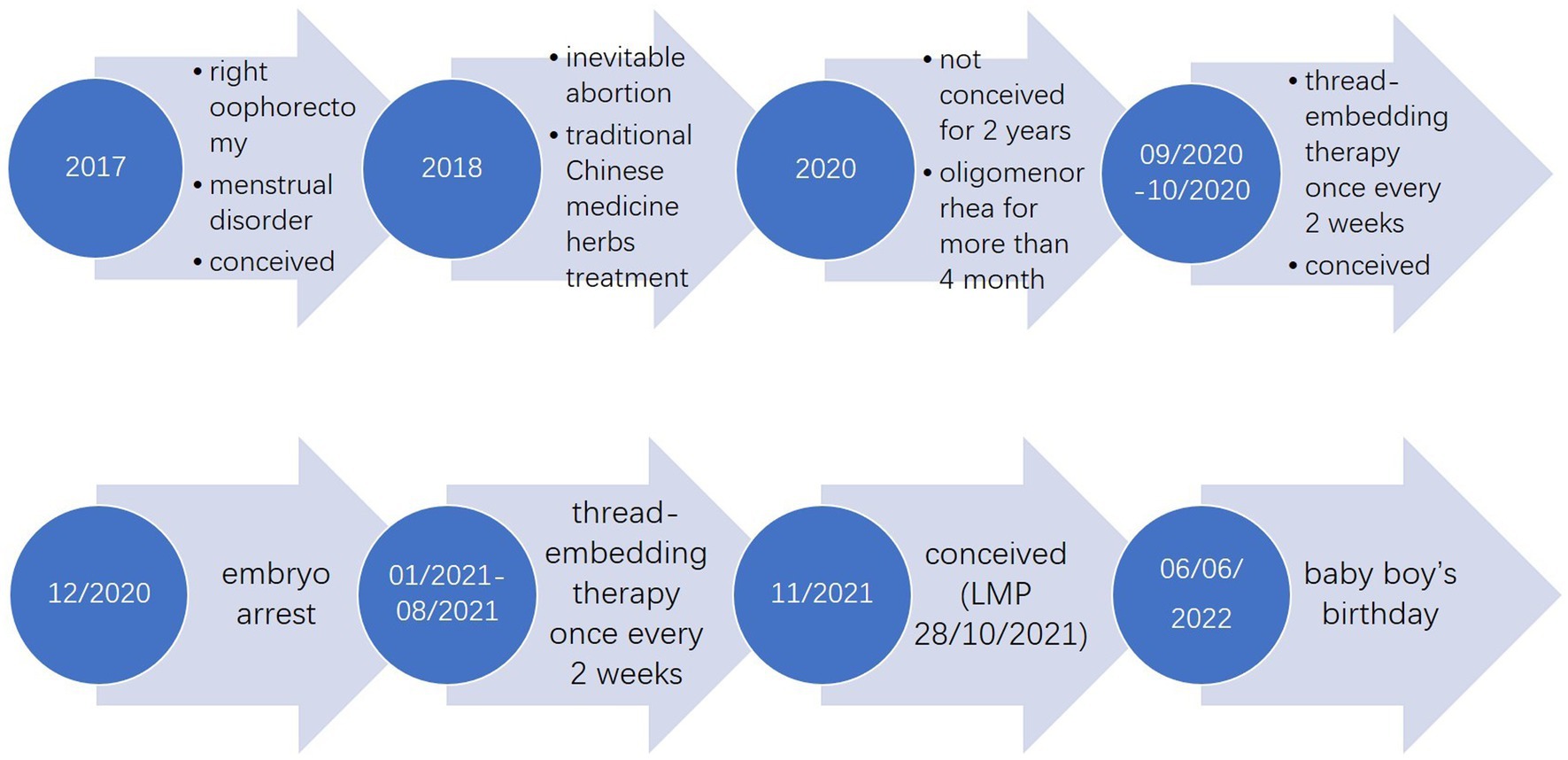
Figure 4. Treatment timeline. Contents in the arrow lists the main events in treatment and the development and outcome of the disease at the time labelled in the circle at the bottom of the arrow.
In November 2021, the patient celebrated her third pregnancy. Her last menstrual period (LMP) was October 28, 2021, and she gave birth to a baby boy by spontaneous labour on June 6, 2022. The baby is in good health.
3 Discussion
As a patient with only one ovary, of which arterial blood flow was too low to detect, the function of her ovary was low. The increase in FSH and dramatic decrease in E2 between August 4, 2020, and September 12, 2020, may also suggest that her ovarian function was declining sharply at the beginning, adding challenges to our treatment. In this circumstance, the two pregnancies after treatment were truly inspiring, and the three main serum sex hormones we tested (FSH, LH, and E2, January 26, 2021) had all returned to normal. The former conception did not turn out well, indicating that management in pregnancy still requires attention among patients with POI. Second, the significant decreases in mKMI and TCM syndrome scores were notable. The menopausal symptoms disappeared completely, and her menstrual cycle was regular. She claimed to take proprietary Chinese medicine such as Baotai Cuyun Pill and Xianlingpi capsule for a short period of time during her thread-embedding therapy, but we tend to consider it only a supporting role due to the small dosage and short duration. In addition, the patient did not receive any treatment other than four thread-embedding therapies between August and October 2020. At that time, she also conceived and showed progress for mKMI and TCM syndrome scores, indicating promotion of ovarian function and an independent therapeutic effect of thread-embedding therapy.
POI is a condition in which there is a decline in ovarian function in women who are younger than 40 years resulting in a hypo-oestrogenic state with elevated gonadotrophins and oligomenorrhoea/amenorrhoea. This leads to short term complications of menopausal symptoms and long-term effects on bone and cardiovascular health, cognition as well as the impact of reduced fertility and sexual function associated with this condition (17). A study reported that the prevalence of infertility is approximately 9%, with more than half of couples seeking medical care (18). POI is one of the main causes of infertility in women (1). The impact of UO to fertility is controversial. Some supposed that the removal of one ovary does not significantly reduce the pregnancy or fertility outcome respect to other abdominal or pelvic procedures (19, 20), while others showed a significant detrimental effect of UO on the rates of live birth and pregnancy (21), or have less IVF capacity but the same pregnancy rate (22). When excluded assisted reproductive technology, the spontaneous pregnancy after UO is rarely reported. Yet UO can still be considered as a limitation on account of the reduction of ovarian follicular reserve (23).
Acupuncture therapy is an external treatment of traditional Chinese medicine and has been applied for POI. A prospective consecutive case series study suggested that acupuncture may decrease serum FSH and LH levels, raise serum E2 levels, improve menopausal symptoms, and reduce mental stress in patients with no serious side effects (24). Similarly, in another prospective observational study, the authors noted that electroacupuncture may modulate reproductive hormone levels with no significant side effects (25). A meta-analysis of acupuncture for POI showed that acupuncture could decrease FSH levels and improve menstruation (26). Modern medicine shows that the effectiveness of acupuncture in treating POI is mainly attributed to the improvement of ovarian function by regulating the neuroendocrine system and increasing blood supply to the reproductive organs (25, 27).
Thread-embedding therapy belongs to the range of acupuncture therapy. It is a kind of prevention and treatment technology that exerts long-lasting stimulatory effects on acupoints by incorporating absorbable surgical sutures into the acupoints (18). Thread-embedding therapy may combine the acupuncture effect, the absorption effect of the thread and the repair effect after the injury, integrating the needle and buried needle effect into one. It is the development of “needle retention” in traditional acupuncture by modern technology. Through the liquefaction and absorption process of absorbable protein lines, the acupoints are stimulated continuously and stably. The Internal Classic is the earliest classical work of TCM, and it says if the needle is not retained long enough then the persistent disease cannot be removed, which is the most significant difference and innovation from traditional acupuncture. In addition, it has the advantage of a lower treatment frequency, which can save time and improve the compliance among patients. This treatment method is widely used in our clinic and has advantages for POI. The adverse effects of thread-embedding therapy generally include subcutaneous bleeding, hard nodules, itching, redness, swelling, and heat pain, which may be related to the material of the thread and different personal physical conditions. The absorbable collagen threads used in this study had low antigenicity and good histocompatibility. In our report, the patient only experienced bleeding during treatment, which is a predictable event usually caused by a puncture on a vessel and can be stopped by applying pressure to the puncture site with a cotton swab. There were no other serious adverse events.
In this article, we report a patient with POI after UO who became pregnant spontaneously after thread-embedding therapy. We infer that thread-embedding therapy might be effective for POI in ameliorating serum sex hormone levels, improving ovarian function, and helping pregnancy in clinical treatment. The cause of POI is unknown in 85–90% of cases, and the proportion of different causes was also not determined overall (17, 28). In addition to the iatrogenic POI involved in this study, it can also be spontaneous. Based on the theory of traditional Chinese medicine, the mechanism of modern medicine and our clinical experience, we believe that other types of POI can also have a try to refer to this method. Possible mechanism of thread-embedding instead of traditional acupuncture in the treatment of POI still needs to be further explored.
One of the important factors influencing the clinical effectiveness of thread-embedding therapy is the selection of acupoints. In addition to the localized acupoints to be selected, some other acupoints were also vital and worthy of being chosen. In TCM theory, the kidney collects essence-qi and is closely related to female pregnancy. The liver is the master of drainage, which helps the kidney to collect and discharge essence-qi and influences the opening and closure of the uterus. The spleen is the foundation of the acquirement, which transports and transforms water and grain essence and can replenish the kidney essence. Furthermore, these three organs also have connections to the ovaries in meridians. Thus, the majority of selected acupoints in our treatment were located at the Liver Meridian of Foot-Jueyin, Kidney Meridian of Foot-Shaoyin, and Spleen Meridian of Foot-Taiyin. Additionally, the back-shu of the liver, kidney, and spleen were also indispensable.
There are also limitations to our report. The article was a retrospective report in which we gathered relevant information depending on the patient’s narrative. Patients may experience recall bias, which would not facilitate our collection and analysis of complete treatment information. In addition, based on the study design, the grade of evidence is low. Hence, the effectiveness and safety of thread-embedding therapy for POI need to be confirmed by more high-quality evidence.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Dongzhimen Hospital Affiliated to Beijing University of Chinese Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ZZ: Data curation, Writing – original draft. JY: Writing – original draft, Writing – review & editing. JZ: Data curation, Writing – original draft. YS: Investigation, Writing – original draft. JN: Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. ENN award fund in Beijing University of Chinese Medicine (2019-XAJLJ J-014).
Acknowledgments
The authors would like to thank the patients who allowed sharing their cases.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Eshre Guideline Group on POIWebber, L, Davies, M, Anderson, R, Bartlett, J, Braat, D, et al. ESHRE guideline: management of women with premature ovarian insufficiency. Hum Reprod. (2016) 31:926–37. doi: 10.1093/humrep/dew027
2. Panay, N, Anderson, RA, Nappi, RE, Vincent, AJ, Vujovic, S, Webber, L, et al. Premature ovarian insufficiency: an international menopause society white paper. Climacteric. (2020) 23:426–46. doi: 10.1080/13697137.2020.1804547
3. Vabre, P, Gatimel, N, Moreau, J, Gayrard, V, Picard-Hagen, N, Parinaud, J, et al. Environmental pollutants, a possible etiology for premature ovarian insufficiency: a narrative review of animal and human data. Environ Health. (2017) 16:37. doi: 10.1186/s12940-017-0242-4
4. Ishizuka, B . Current understanding of the etiology, symptomatology, and treatment options in premature ovarian insufficiency (POI). Front Endocrinol. (2021) 12:626924. doi: 10.3389/fendo.2021.626924
5. Golezar, S, Ramezani Tehrani, F, Khazaei, S, Ebadi, A, and Keshavarz, Z. The global prevalence of primary ovarian insufficiency and early menopause: a meta-analysis. Climacteric. (2019) 22:403–11. doi: 10.1080/13697137.2019.1574738
6. Li, XT, Li, PY, Liu, Y, Yang, HS, He, LY, Fang, YG, et al. Health-related quality-of-life among patients with premature ovarian insufficiency: a systematic review and meta-analysis. Qual Life Res. (2020) 29:19–36. doi: 10.1007/s11136-019-02326-2
7. Vander Borght, M, and Wyns, C. Fertility and infertility: definition and epidemiology. Clin Biochem. (2018) 62:2–10. doi: 10.1016/j.clinbiochem.2018.03.012
8. Sullivan, SD, Sarrel, PM, and Nelson, LM. Hormone replacement therapy in young women with primary ovarian insufficiency and early menopause. Fertil Steril. (2016) 106:1588–99. doi: 10.1016/j.fertnstert.2016.09.046
9. Lin, J, Wu, D, Jia, L, Liang, M, Liu, S, Qin, Z, et al. The treatment of complementary and alternative medicine on premature ovarian failure. Shabbir a, editor. Evid Based Complement Alternat Med. (2021) 2021:1–14. doi: 10.1155/2021/6677767
10. Fu, Y, Ding, DN, Shen, Y, Jia, LY, Yan, MY, Wei, W, et al. Complementary and alternative medicine for premature ovarian insufficiency: a review of utilization and mechanisms. Liu TB, editor. Evid Based Complement Alternat Med. (2022) 2022:1–15. doi: 10.1155/2022/9053930
12. Zheng, X . Guidance principle of clinical study on new drug of traditional Chinese medicine. Beijing: Chinese Medical and Pharmaceutical Science Press (2002).
13. Tan, Y . Gynecology of traditional Chinese medicine. Beijing: China Press of Traditional Chinese Medicine (2016).
14. Yan, L, and Zuo, F. Clinical observation on 38 cases of ovum stagnation syndrome treated by acupuncture of Luanchao point (MA). Zhongguo Zhen Jiu. (1998) 10:9–10.
15. Jiang, DS, and Ding, D. Clinical observation on acupuncture combined with medication for treatment of continuing unovulation infertility. Zhongguo Zhen Jiu. (2009) 29:21–4.
16. Li, X, Xu, H, Fang, Y, Shang, J, Yang, H, Zhou, X, et al. Acupuncture with regulating menstruation to promote pregnancy for diminished ovarian reverse: a prospective case series study. Zhongguo Zhen Jiu. (2017) 37:1061–5. doi: 10.13703/j.0255-2930.2017.10.009
17. Hamoda, H, and Sharma, A. Premature ovarian insufficiency, early menopause, and induced menopause. Best Pract Res Clin Endocrinol Metab. (2024) 38:101823. doi: 10.1016/j.beem.2023.101823
18. Boivin, J, Bunting, L, Collins, JA, and Nygren, KG. International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Hum Reprod. (2007) 22:1506–12. doi: 10.1093/humrep/dem046
19. Wang, P, and Fang, L. Salpingo-oophorectomy versus cystectomy in patients with borderline ovarian tumors: a systemic review and meta-analysis on postoperative recurrence and fertility. World J Surg Onc. (2021) 19:132. doi: 10.1186/s12957-021-02241-2
20. Bellati, F, Ruscito, I, Gasparri, ML, Antonilli, M, Pernice, M, Vallone, C, et al. Effects of unilateral ovariectomy on female fertility outcome. Arch Gynecol Obstet. (2014) 290:349–53. doi: 10.1007/s00404-014-3194-8
21. Rodriguez-Wallberg, KA, Nilsson, HP, and Lind, T. Live birth and pregnancy rates after in vitro fertilization/intracytoplasmic sperm injection in women with previous unilateral oophorectomy: a systematic review and meta-analysis. Fertil Steril. (2022) 117:992–1002. doi: 10.1016/j.fertnstert.2022.01.033
22. Younis, J, Naoum, I, Salem, N, Perlitz, Y, and Izhaki, I. The impact of unilateral oophorectomy on ovarian reserve in assisted reproduction: a systematic review and meta-analysis. BJOG. (2018) 125:26–35. doi: 10.1111/1471-0528.14913
23. Bjelland, EK, Wilkosz, P, Tanbo, TG, and Eskild, A. Is unilateral oophorectomy associated with age at menopause? A population study (the HUNT2 survey). Hum Reprod. (2014) 29:835–41. doi: 10.1093/humrep/deu026
24. Chen, Y, Fang, Y, Yang, J, Wang, F, Wang, Y, and Yang, L. Effect of acupuncture on premature ovarian failure: a pilot study. Evid Based Complement Alternat Med. (2014) 2014:1–6. doi: 10.1155/2014/718675
25. Wang, Y, Li, Y, Chen, R, Cui, X, Yu, J, and Liu, Z. Electroacupuncture for reproductive hormone levels in patients with diminished ovarian reserve: a prospective observational study. Acupunct Med. (2016) 34:386–91. doi: 10.1136/acupmed-2015-011014
26. Jo, J, Lee, YJ, and Lee, H. Effectiveness of acupuncture for primary ovarian insufficiency: a systematic review and Meta-analysis. Evid Based Complement Alternat Med. (2015) 2015:1–12. doi: 10.1155/2015/842180
27. Qu, F, Li, R, Sun, W, Lin, G, Zhang, R, Yang, J, et al. Use of electroacupuncture and transcutaneous electrical acupoint stimulation in reproductive medicine: a group consensus. J Zhejiang Univ Sci B. (2017) 18:186–93. doi: 10.1631/jzus.B1600437
Keywords: thread-embedding therapy, premature ovarian insufficiency, unilateral oophorectomy, pregnancy, acupuncture, case report
Citation: Zhang Z, Yuan J, Zhao J, Song Y and Ni J (2024) Spontaneous pregnancy after thread-embedding therapy treatment with premature ovarian insufficiency after unilateral oophorectomy: a case report. Front. Med. 11:1357824. doi: 10.3389/fmed.2024.1357824
Edited by:
A. Seval Ozgu-Erdinc, Ankara City Hospital, TürkiyeReviewed by:
Huri Güvey, Private Parkhayat Hospital, TürkiyeXiaoyan Zheng, Chengdu University of Traditional Chinese Medicine, China
Soobin Jang, Daegu Haany University, Republic of Korea
Copyright © 2024 Zhang, Yuan, Zhao, Song and Ni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jinxia Ni, nijinxia118@126.com
†These authors have contributed equally to this work and share first authorship
 Ziniu Zhang
Ziniu Zhang Jingxue Yuan
Jingxue Yuan Jingjing Zhao†
Jingjing Zhao†