Blood Pressure Circadian Variation, Cognition and Brain Imaging in 90+ Year-Olds
- 1Department of Neurology, School of Medicine, University of California, Irvine, Irvine, CA, United States
- 2Institute for Memory Impairments and Neurological Disorders, University of California, Irvine, Irvine, CA, United States
- 3Department of Epidemiology, School of Medicine, University of California, Irvine, Irvine, CA, United States
- 4Department of Neurology, Center for Neuroscience, University of California, Davis, Davis, CA, United States
- 5Department of Radiological Sciences, School of Medicince, University of California, Irvine, Irvine, CA, United States
- 6Department of Neurobiology & Behavior, School of Biological Sciences, University of California, Irvine, Irvine, CA, United States
Purpose: To analyze the relationship between blood pressure (BP) variables, including circadian pattern, and cognition in 90+ year-olds.
Methods: Twenty-four hour ambulatory BP monitoring was completed on 121 participants drawn from a longitudinal study of aging and dementia in the oldest-old. Various measures of BP and its variability, including nocturnal dipping, were calculated. Each person was given both a neuropsychological test battery covering different cognitive domains and a neurological examination to determine cognitive status. Seventy-one participants had a brain magnetic resonance imaging (MRI) scan.
Results: Participants ranged in age from 90 to 102 years (mean = 93), about two-thirds were female, and nearly 80% had at least some college education. Mean nocturnal dips differed significantly between cognitively normal (n = 97) and impaired individuals (n = 24), with cognitively normal participants having on average greater nocturnal dips [6.6% vs. 1.3%, p = 0.006 for systolic BP (SBP); 11% vs. 4.4%, p = 0.002 for diastolic BP (DBP)]. Nocturnal dips were also related to performance on select cognitive test scores (especially those related to language, recent memory and visual-spatial ability), with individuals who performed below previously established median norms having significantly smaller nocturnal dips (both SBP and DBP) than those above the median. DBP reverse dippers had larger mean white matter hyperintensities (WMH as percent of total brain volume; 1.7% vs. 1.2%, 1.1% and 1.0% in extreme dippers, dippers, non-dippers) and a greater proportion had lobar cerebral microbleeds (CMBs; 44% vs. 0%, 7%, 16%, p < 0.05). Impaired participants had higher mean WMH than those with normal cognition (1.6% vs. 1.0% p = 0.03) and more tended to have CMB (31% vs. 20%, p = n.s.).
Conclusion: These findings suggest that cognitive dysfunction is associated with dysregulation in the normal circadian BP pattern. Further study is warranted of the potential role of WHM and CMB as mediators of this association.
Introduction
Several studies have found that blood pressure (BP) levels and other BP-related features such as variability, daytime and nighttime measures, and nocturnal dipping are associated with mortality, cardiovascular events, cerebrovascular disease, and subclinical damage to the heart, kidney and vessels (Boggia et al., 2007; Sörös et al., 2013; Diaz et al., 2014; Douma and Gumz, 2018). Although studies show that high BP in middle-age and late-life is associated with increased risk of cognitive decline and dementia (Launer et al., 2000; Kivipelto et al., 2001; Yamada et al., 2003; Whitmer et al., 2005; Arvanitakis et al., 2018), other work suggests that developing hypertension at older ages may protect against dementia (Corrada et al., 2017).
Twenty-four hour ambulatory BP monitoring (ABPM) offers greater precision in estimating average BP than one-time readings and provides information on variability and circadian pattern of BP (O’Brien et al., 2013). While several studies have analyzed the association of BP variability and cognition in the elderly (van Boxtel et al., 1998, 2006; Kanemaru et al., 2001; Axelsson et al., 2008; Nagai et al., 2008; Guo et al., 2010; Conway et al., 2015), none, to our knowledge, have investigated this in the oldest-old (aged 90+ years). Considering the aging of the population with an increasing proportion of those aged 90+ (United Nations Department of Economic and Social Affairs Population Division, 2017) and the increasing risk of cognitive decline and dementia with age (Corrada et al., 2010), elucidating associations with cognitive function, especially of variables which are modifiable, remains vital. Therefore, using data from 24-h ABPM of 90+ year-olds, we analyzed the relationships between various BP measurements, their variability, and circadian pattern of BP and cognition with the aim of finding the variable most closely associated with cognitive function, hypothesizing that BP circadian variation impacts cognitive function.
Materials and Methods
Participants
Study subjects were participants in The 90+ Study, a study of aging and dementia in individuals aged 90 years and older from the Laguna Woods Village (California) retirement community and its surroundings (Paganini-Hill et al., 2016). Subjects are seen in-person and longitudinally followed every 6 months. At each visit, their medical history is updated and they are given a neuropsychological test battery and a neurological examination as previously described (Whittle et al., 2007). Data from the visit closest in date to the date of ABPM were selected. The study was approved by the Institutional Review Board of the University of California Irvine and 149 participants agreed to and gave written informed consent for 24-h ABPM.
Ambulatory Blood Pressure Monitoring
Subjects underwent ABPM with a fully automatic device (Sun Tech—Oscar 2 with AccuWi n 3.4.4.0 software). The instrument was worn 24-h (during daytime and sleep) with sampling every 1 h. Systolic BP (SBP) readings greater than 260 mmHg or lower than 70 mmHg as well as diastolic BP (DBP) readings greater than 150 mmHg or lower than 40 mmHg were discarded. Participants were told to follow their normal daily activities during measurements. Daytime measures were considered those between 07:00 and 21:59 and nighttime as those between 22:00 and 06:59.
We represented BP by several indices. Separately for 24-h, daytime and nighttime and for SBP and DBP, we calculated mean, minimum, maximum, standard deviation (SD), coefficient of variation (CV), average real variability (ARV), proportion of high values (SBP ≥140 mmHg, DBP ≥90 mmHg), and proportion of low values (SBP <90 mmHg, DBP <60 mmHg). We also calculated proportion of high BP measurements (either SBP ≥140 mmHg or DBP ≥90 mmHg) and proportion of low BP measurements (either SBP <90 mmHg or DBP <60 mmHg). Separately for SBP and DBP, we calculated nocturnal dip (%) as (1-mean nighttime BP/mean daytime BP) × 100. Subjects were further classified by nocturnal dipping category: extreme dipper (≥20%), dipper (10%–19%), non-dipper (0%–9%), reverse dipper (<0%).
Neuropsychological Tests
Trained psychometrists administered the neuropsychological test battery. The 10 tests represent different cognitive domains such as language (Verbal Fluency Tests (Animal and Letter F) and Boston Naming Test, BNT), recent memory (California Verbal Learning Tests, CVLT), executive function (Trail Making Tests), visual-spatial ability (Clock Drawing and CERAD Construction), attention/working memory (Digit Span Tests), as well as global cognition [the mini-mental state examination (MMSE) and modified MMSE (3MS)]. Details of the use of these tests and age-adjusted cognitive norms in this population group have been previously presented (Whittle et al., 2007).
Neurological Examination
Neurological examiners (trained physicians or nurse practitioners) administered the Clinical Dementia Rating scale (Morris, 1993) and assessed functional abilities using the Functional Activities Questionnaire (Pfeffer et al., 1982). Using MMSE and 3MS results and information from their examination they determined the presence or absence of dementia, applying Diagnostic and Statistical Manual of Mental Disorders, 4th edition criteria (American Psychiatric Association, 1994), classifying individuals as normal, cognitively impaired not demented (CIND), or demented.
Brain Imaging
Some participants underwent brain magnetic resonance imaging (MRI) using a GE Signa HD 3.0 Tesla MRI system as previously described (Bennett et al., 2017). A high-resolution T1-weighted fast-spoiled gradient recalled echo (TR/TE/IT = 7/3/400ms, FOV = 256 × 256 mm, 166 sagittal slices, and 1.0 mm3 spatial resolution), fluid attenuation inversion recovery (FLAIR) sequence and susceptibility-weighted imaging (SWI) were acquired. We calculated T1-weighted image tissue volumes using in-house methods described previously (Fletcher et al., 2018). Briefly, brain masks to separate brain from whole head were generated using an atlas-based method (Aljabar et al., 2009) followed by human quality control as needed. Stripped brains were further segmented into four tissue types: gray matter (GM), white matter (WM), cerebrospinal fluid (CSF) and WM hyperintensities (WMH), using a segmentation algorithm designed to enhance accuracy at tissue boundaries (Fletcher et al., 2012) in combination with FLAIR imaging to estimate WMH. Volumes of CSF, GM, WM and WMH were calculated as percent of total brain volume.
MRI were also reviewed by a neuroradiologist (DF), who rated definite cerebral microbleeds (CMBs) presence, number and distribution on SWI using the microbleed anatomical rating scale (MARS; Gregoire et al., 2009). In MARS, definite CMB were defined as small, rounded or circular, well-defined hypodense lesions within brain parenchyma with clear margins ranging from 2 to 10 mm in size on T2*-weighted images, and locations of CMB were classified into deep, lobar, and infratentorial categories.
Covariates
Age, sex, education, smoking and medical histories of cardiovascular and cerebral vascular diseases [high BP, heart attack, coronary artery disease, congestive heart failure, heart valve disease, stroke, transient ischemic attack (TIA), diabetes] were asked. Consumption of wine, beer and hard liquor (0, <1, 1, 2, 3, 4+ drinks) and participation in physical and other activities (0, 1/4, 1/2, 1, 2, 3–4, 5–6, 7–8, 9+ h) were asked for an average weekday.
Statistical Analyses
Univariate analyses (calculation of means, standard errors, proportions) were conducted to assess BP metrics and subject characteristics. Mean daytime and nighttime values for each BP metric were compared using paired t-tests. To study the association between BP and cognition, we used chi-square and Fisher exact-tests for categorical variables and t-tests and analysis of variance (ANOVA) with contrasts for specific group comparisons for continuous variables. All analyses were conducted using SAS statistical software version 9.4 (SAS Institute, Cary, NC, USA). A two-sided p < 0.05 was considered statistically significant.
Results
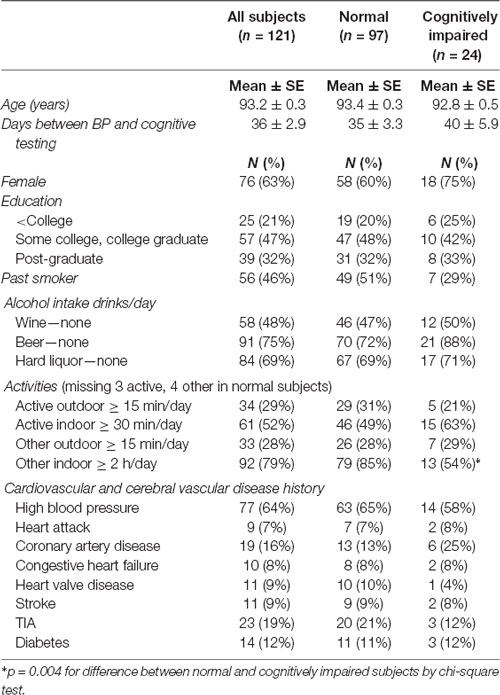
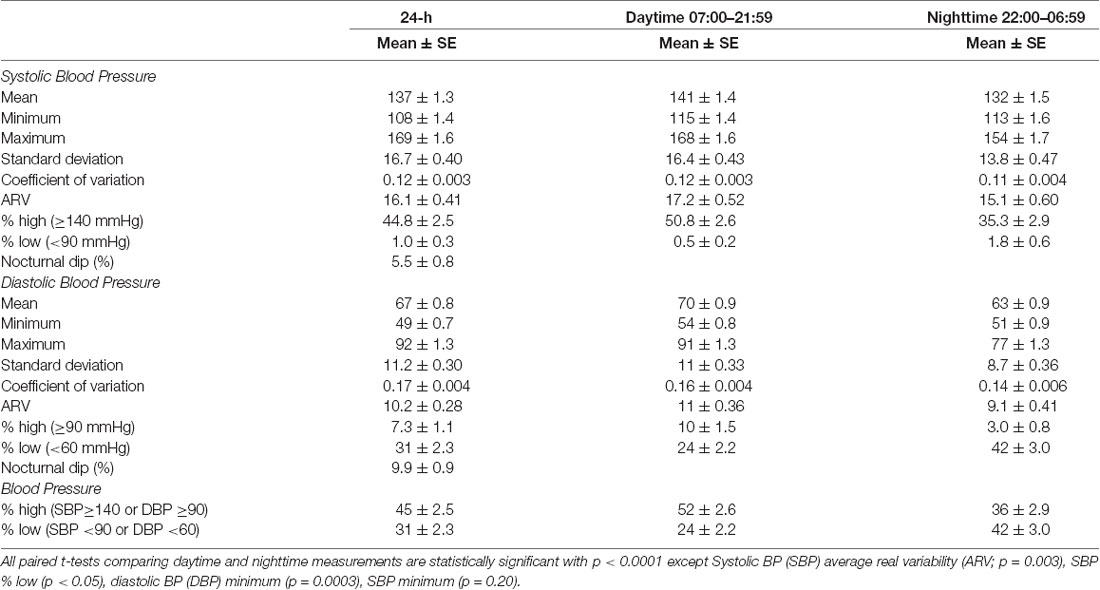
From the 149 participants agreeing to 24-h ABPM, we eliminated 28 persons who had less than six valid observations during the daytime or the nighttime periods. The characteristics of the remaining 121 subjects with sufficient ABPM readings (ranging from 12 to 24) are shown in Table 1. The age of participants ranged from 90 to 102 (mean ± SE = 93.2 ± 0.3). All participants were Caucasian, except one Asian. Nearly two-thirds (63%) were women and 79% had at least some college education. No subject currently smoked although 46% had smoked in the past. About two-thirds (64%) of participants reported having had high BP. Other cardiovascular and cerebral vascular diseases ranged from 7% for heart attack to 19% for TIA. The number of days between BP monitoring and the cognitive testing visit ranged from 0 to 182 (mean ± SE = 36 ± 2.9). By neurological examination most (80%) participants were classified as normal (n = 97), the others as cognitively impaired with CIND (n = 21) or dementia (n = 3). Normal and cognitively impaired subjects did not differ significantly on baseline characteristics except time spent in other indoor activities (85% vs. 54% for 2 + h/day, p = 0.004; Table 1). Table 2 shows the BP metrics for 24-h, daytime and nighttime periods for the 121 subjects. Paired t-tests verified significant differences between daytime and nighttime BP variables signifying a circadian pattern.
Nocturnal Dips and Association With Cognitive Status
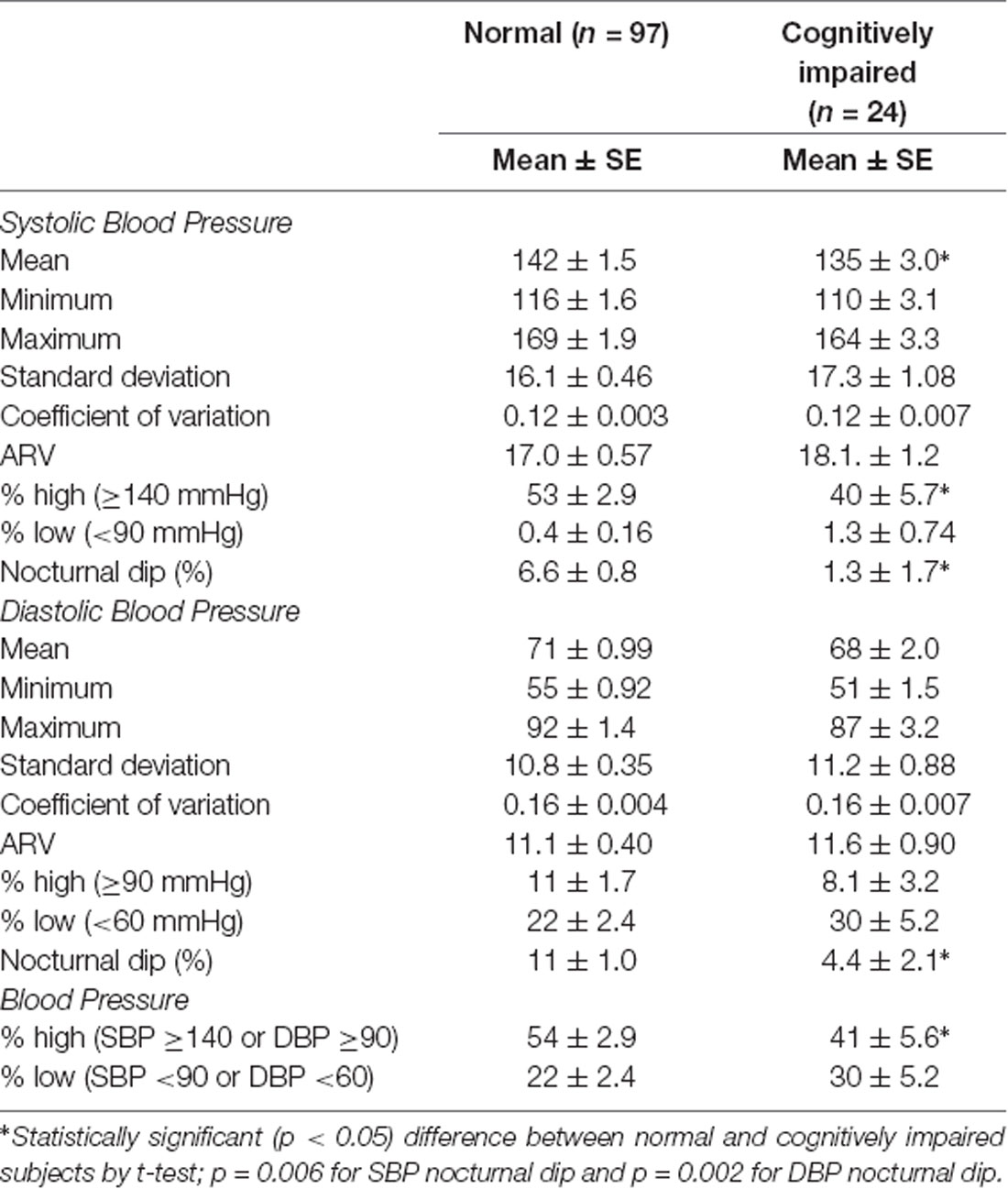
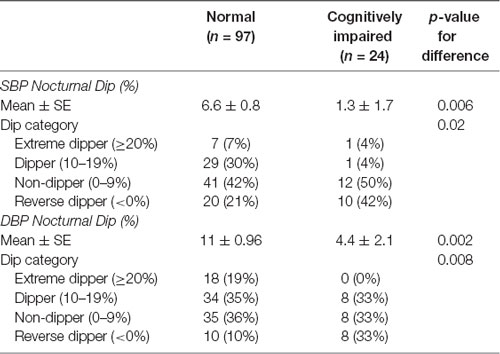
Normal individuals did not differ from cognitively impaired individuals on most BP metrics. Impaired persons had lower means of daytime SBP, % high SBP (≥140 mmHg) and % high BP (SBP ≥140 or DBP ≥90; Table 3). The most significant differences between the two groups were mean nocturnal dips with cognitively normal participants having on average greater nocturnal dips (6.6% vs. 1.3%, p = 0.006 for SBP; 11% vs. 4.4%, p = 0.002 for DBP). Likewise, cognitively normal individuals were more likely than impaired individuals to be nocturnal dippers (37% vs. 8% for SBP; 54% vs. 33% for DBP) while impaired individuals were more likely to be reverse dippers (42% vs. 21% for SBP, p = 0.03; 33% vs. 10% for DBP, p = 0.01; Table 4).
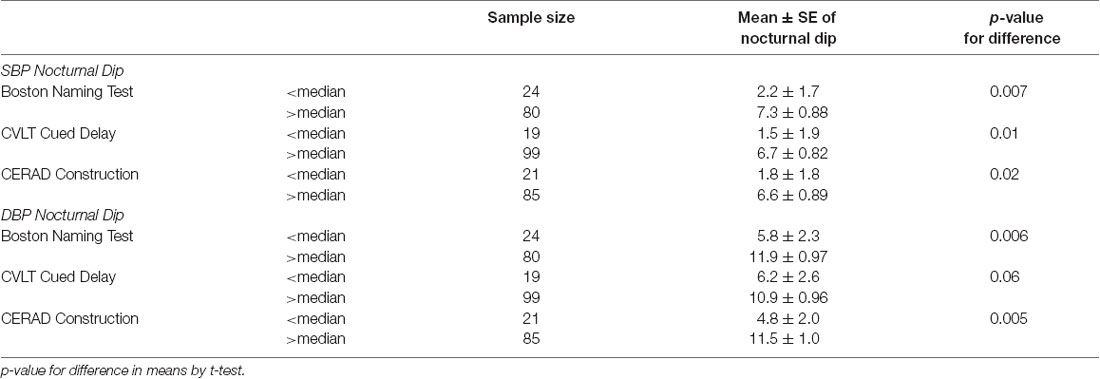
Nocturnal Dips and Association With Cognitive Measures
Over three-quarters of participants surpassed the median norm previously established for their age group on most cognitive tests. Performance was poorer on tests of executive function or attention/working memory (60%–70% above median norm; data not shown). Nocturnal dips were related to performance on cognitive test scores related to language (BNT), recent memory (CVLT), and visual-spatial ability (CERAD Construction; Table 5). Individuals who performed below the median norm had significantly smaller nocturnal dips (both SBP and DBP) than those above the median. Table 6 cross-classifies individuals on these same cognitive tests as below/above the median norm and the four dipping categories. Similar results were observed; reverse dippers performed the worst on these three tests. Cognitively impaired individuals by neurological examination were also more likely to be reverse dippers.
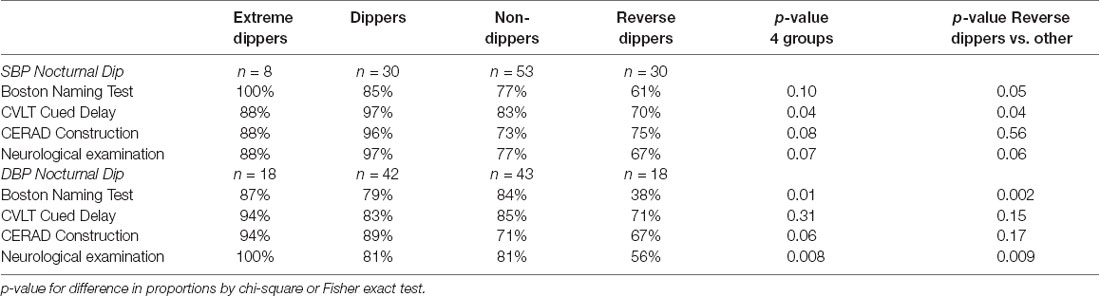
Table 6. Percent normal (above median norm) on cognitive tests and on neurological examination by nocturnal BP dipping category.
Nocturnal Dips and Association With Structural Brain Measures
Brain MRI was available for 71 participants. Reasons for missing MRI data were bodily presence of hardware (e.g., pacemaker, metal implant; n = 21), other condition (e.g., too weak, could not tolerate time in scanner; n = 4), refused (n = 1), bad imaging (n = 1), not part of imaging study (n = 23).
Both mean WMH volume and presence of CMB were related to DBP nocturnal dip and to cognitive status (Table 7). Mean WMH was highest in DBP reverse dippers (1.7% vs. 1.2%, 1.1% and 1.0% in extreme dippers, dippers, non-dippers) and was significantly different between reverse dippers and non-dippers (p < 0.05). Mean WMH was also higher in those with impaired cognition (1.6%, vs. 1.0% p = 0.03). Impaired participants were also more likely than those with normal cognition to have CMB (31% vs. 20%), although the difference was not significant. A greater proportion of DBP reverse dippers had lobar CMB than the others (44% vs. 0%, 7%, 16% in extreme dippers, dippers, non-dippers, p < 0.05). In contrast, a greater proportion of DBP extreme dippers had deep CMB than the others (30% vs. 4%, 0%, 0% in dippers, non-dippers, reverse dippers, p < 0.05).
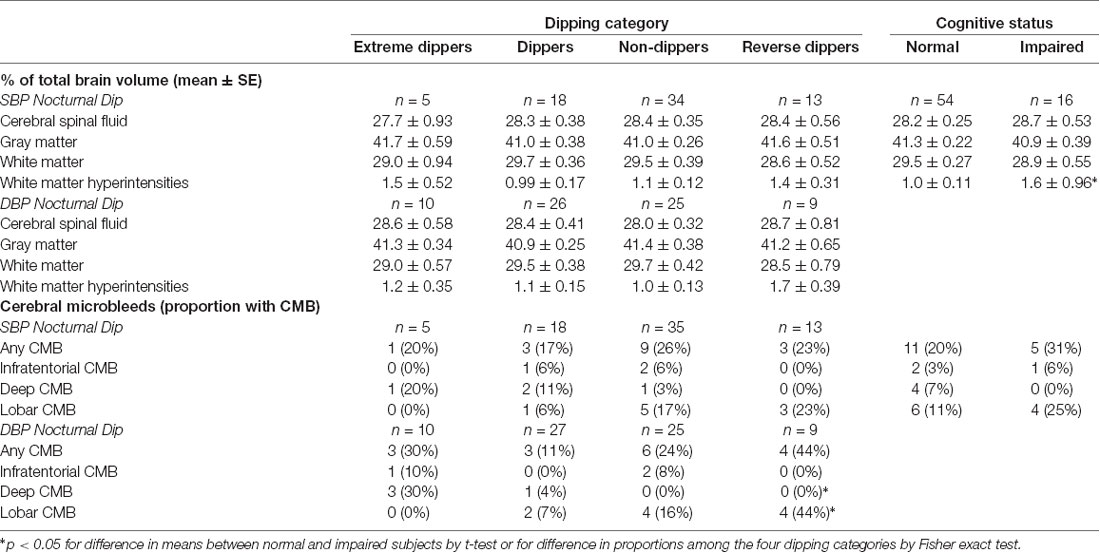
Table 7. Brain magnetic resonance imaging (MRI) findings by nocturnal BP dipping category and cognitive status.
Discussion
To our knowledge, our study is the first to evaluate 24-h BP measures, including circadian BP pattern, and their association with cognition in individuals aged 90 years and older. In this oldest-old sample, mean nocturnal dip (% difference in mean daytime and mean nighttime BP measures) differed between cognitively normal and impaired individuals for both SBP and DBP. Classification of individuals by dipping categories showed that impaired individuals compared with cognitively normal individuals were less likely to be dippers (SBP 8% vs. 37%, DBP 33% vs. 54%) and more likely to be reverse dippers (SBP 42% vs. 21%, DBP 33% vs. 10%).
Studies examining nocturnal dipping and cognition in the elderly are limited and those using community-dwelling samples even more so. Three studies included only hypertensive patients (Kanemaru et al., 2001; van Boxtel et al., 2006; Nagai et al., 2008). Classifying 88 Japanese patients from a hypertension clinic (mean age = 71, range = 37–90) into three cognitive groups, Kanemaru et al. (2001) found the severely affected group had smaller differences of day-night BP (i.e., less nocturnal dipping), which was significant for DBP. In another Japanese study, Nagai et al. reported a positive association between nocturnal SBP dipping and MMSE score in 55 untreated hospitalized hypertensives (aged ≥ 70, mean = 73; Nagai et al., 2008). However, an investigation of 86 patients aged 40–80 years from a hypertension clinic in the Netherlands reported no association between nocturnal dipping and cognitive measures (van Boxtel et al., 2006). Two additional non-community based studies showed a positive association between nocturnal dipping and cognitive function based on MMSE; the first utilized 99 nursing home/geriatric hospital subjects (mean age 80 years; Ohya et al., 2001) and the second 224 patients hospitalized for lacunar infarctions (Yamamoto et al., 2011). In a sample of 115 community residents aged 28–82 years from the Maastricht Aging Study, non-dippers showed lower levels of both memory and sensorimotor speed scores, but extreme dippers were not analyzed separately (van Boxtel et al., 1998). In a study of 79 81-year-old men in a Swedish community, nocturnal SBP dipping was associated with lower cognitive performance (Axelsson et al., 2008). In a study of 144 Japanese community dwelling persons (aged ≥ 50 years, mean = 68), MCI had a J-shaped relationship with dipping category with frequency of MCI being about 32%, 13%, 30%, and 50% (from extreme dipper to reverse dipper) subjects (Guo et al., 2010). In our study of the oldest-old, we also found that reverse dippers had the highest frequency of cognitive impairment (SBP 12%, 3%, 23%, and 33%; DBP 0%, 19%, 17%, 44%). Another community-based study of 319 older (≥60 years, mean = 72) adults from the San Diego Population Study found greater nighttime SBP dipping significantly associated in a linear manner across quartile groups (cutoffs not given) with better cognitive function (Montreal Cognitive Assessment; Conway et al., 2015). Greater nighttime dipping was modestly associated with better performance on the immediate recall portion of the Hopkins Verbal Learning Test–Revised, which measures memory, and on the Trail-Making Test Part A, which measures a number of domains including cognitive flexibility, visuospatial processing, and executive function. We also found that mean nocturnal dips differed between participants above and below the median performance on select cognitive tests including BNT, CVLT cued delay and CERAD construction, tests related to the domains of naming, recent memory and construction. Dippers were also more likely than non-dippers to perform better on these three cognitive tests. Although we found no association with global measures of cognition, previous studies have underscored the necessity of more robust assessment of memory function—especially delayed recall—in cognitive screening (Lacy et al., 2015).
These findings suggest that cognitive dysfunction may be associated with dysregulation in BP pattern. If confirmed, and if nocturnal dipping patterns are shown to precede cognitive impairment in longitudinal studies, the addition of ABPM to clinic-based BP may allow identification of older persons at higher risk for cognitive impairment beyond other known risk factors. However, analyses of future BP intervention studies will need to examine whether manipulation of dipping pattern would improve the trajectory of cognitive function in older persons.
Although current guidelines recommend the use of ABPM for diagnosis of hypertension, its role as a guide to prescribing the appropriate drug and dosage over time is lacking (O’Brien and Dolan, 2016). Studies in recent years on the use of chronotherapy in hypertension suggest that nighttime administration of antihypertensives improves the 24-h BP profiles of patients (Smolensky et al., 2016; Bowles et al., 2018). However, only the American Diabetic Association has made such a recommendation (American Diabetes Association, 2014).
Whether these events are regulated by a common central mechanism of BP variability needs further study. Dipping patterns can be explained by physiological changes in circadian rhythm, though its underlying mechanisms are not fully understood. Suggested factors include sympathetic nervous system overactivation (perhaps due to obesity, diabetes, metabolic syndrome), obstructive sleep apnea, dysfunction in activity of renin-angiotensin-aldosterone axis, sodium intake, and chronic kidney disease (Dubielski et al., 2016; Douma and Gumz, 2018). Some studies have found associations with cerebral WM lesions, as we did (Sander et al., 2000), asymptomatic lacunar infarction (Kario et al., 1996), reduced total brain matter (Nagai et al., 2008), and small vessel disease (Yamaguchi et al., 2014). Both ischemic (microinfarctions) and hemorrhagic (CMB) small vessel disease have been linked to dysfunctional cerebral blood flow as a consequence of altered BP regulation (Fisher, 2016). We also found that lobar microbleeds were associated with reverse dipping, while deep microbleeds were associated with extreme dipping. These intriguing findings, which raise the possibility of different hemodynamic mechanisms for these two kinds of microbleeds, warrant further study. Note that lobar and deep microbleeds are thought to be driven by cerebral amyloid angiopathy and hypertension, respectively (Greenberg et al., 2009). Overall, these results suggest that cerebrovascular disease may mediate the link between cognitive dysfunction and BP dysregulation.
Several strengths and limitations of this study warrant mention. Our major strength is the well-characterized participants who are part of a longitudinal epidemiologic study of aging and dementia. These community-dwelling older adults include women and men as well as hypertensives and non-hypertensives. Additionally, we used a neuropsychological test battery covering numerous cognitive domains and a structured neurological examination. One limitation is that ABPM, although noninvasive, was unsuccessful in nearly 20% of subjects; some participants found the cuff inflation or sleep disturbance intolerable. Additionally, we used the fixed-time method (hourly) of measuring ABPM, which would not detect differences in short-term BP variability. Also, we selected daytime and nighttime measures by time of day and not by sleep/wake pattern. Nonetheless, ABPM provides information on BP variability, the day and night BP profile, and nocturnal dipping pattern not available from one-time clinical measurement (O’Brien et al., 2013). Our sample was recruited from a highly educated, moderately affluent population, which may limit the generalizability of our findings to populations with less education. Our cross-sectional design does not allow us to determine the temporal direction of the associations or causal inferences. Analysis of MRI imaging as well as longitudinal follow-up for cognitive decline in these participants may help answer remaining questions.
In conclusion, we observed associations of nocturnal BP dipping with cognitive status, performance on select cognitive tests and MRI evidence of cerebral microvascular disease in a group of apparently healthy oldest-old individuals. This suggests that cognitive dysfunction is associated with dysregulation in the normal circadian BP pattern and that microvascular disease may play a role as a mediator of this phenomenon. Further studies incorporating longitudinal observations with brain imaging are warranted to fully evaluate these findings.
Author Contributions
AP-H, MC, CK and MF made substantial contributions to the conception or design of the work. NB, DG, EF, BS and DF contributed to the acquisition of the data. AP-H and NB contributed to the analysis. AP-H and MF contributed to the interpretation of data. AP-H and MF drafted the work and the other authors revised it critically for important intellectual content. All authors approved the final version to be published and agreed to be accountable for all aspects of their work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
This work was supported by NIH grants R01AG021055 from NIA and R01NS20989 from NINDS.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Aljabar, P., Heckemann, R. A., Hammers, A., Hajnal, J. V., and Rueckert, D. (2009). Multi-atlas based segmentation of brain images: atlas selection and its effect on accuracy. Neuroimage 46, 726–738. doi: 10.1016/j.neuroimage.2009.02.018
American Diabetes Association. (2014). Standards of medical care in diabetes—2014. Diabetes Care 37, S14–S80. doi: 10.2337/dc14-s014
American Psychiatric Association. (1994). Diagnostic and Statistical Manual of Mental Disorders. 4th Edn. Washington, DC: American Psychiatric Association.
Arvanitakis, Z., Capuano, A. W., Lamar, M., Shah, R. C., Barnes, L. L., Bennett, D. A., et al. (2018). Late-life blood pressure association with cerebrovascular and Alzheimer disease pathology. Neurology 91, e517–e525. doi: 10.1212/wnl.0000000000005951
Axelsson, J., Reinprecht, F., Siennicki-Lantz, A., and Elmståhl, S. (2008). Lower cognitive performance in 81-year-old men with greater nocturnal blood pressure dipping. Int. J. Gen. Med. 1, 69–75. doi: 10.2147/ijgm.s4287
Bennett, I. J., Greenia, D. E., Maillard, P., Sajjadi, S. A., DeCarli, C., Corrada, M. M., et al. (2017). Age-related white matter integrity differences in oldest-old without dementia. Neurobiol. Aging 56, 108–114. doi: 10.1016/j.neurobiolaging.2017.04.013
Boggia, J., Li, Y., Thijs, L., Hansen, T. W., Kikuya, M., Björklund-Bodegård, K., et al. (2007). Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet 370, 1219–1229. doi: 10.1016/S0140-6736(07)61538-4
Bowles, N. P., Thosar, S. S., Herzig, M. X., and Shea, S. A. (2018). Chronotherapy for hypertension. Curr. Hypertens. Rep. 20:97. doi: 10.1007/s11906-018-0897-4
Conway, K. S., Forbang, N., Beben, T., Criqui, M. H., Ix, J. H., and Rifkin, D. E. (2015). Relationship between 24-hour ambulatory blood pressure and cognitive function in community-living older adults: the ucsd ambulatory blood pressure study. Am. J. Hypertens. 28, 1444–1452. doi: 10.1093/ajh/hpv042
Corrada, M. M., Brookmeyer, R., Paganini-Hill, A., Berlau, D., and Kawas, C. H. (2010). Dementia incidence continues to increase with age in the oldest old: the 90+ study. Ann. Neurol. 67, 114–121. doi: 10.1002/ana.21915
Corrada, M. M., Hayden, K. M., Paganini-Hill, A., Bullain, S. S., DeMoss, J., Aguirre, C., et al. (2017). Age of onset of hypertension and risk of dementia in the oldest-old: the 90+ study. Alzheimers Dement. 13, 103–110. doi: 10.1016/j.jalz.2016.09.007
Diaz, K. M., Tanner, R. M., Falzon, L., Levitan, E. B., Reynolds, K., Shimbo, D., et al. (2014). Visit-to-visit variability of blood pressure and cardiovascular disease and all-cause mortality: a systematic review and meta-analysis. Hypertension 64, 965–982. doi: 10.1161/HYPERTENSIONAHA.114.03903.
Douma, L. G., and Gumz, M. L. (2018). Circadian clock-mediated regulation of blood pressure. Free Radic. Biol. Med. 119, 108–114. doi: 10.1016/j.freeradbiomed.2017.11.024
Dubielski, Z., Zamojski, M., Wiechecki, B., Możeńska, O., Petelczyc, M., Kosior, D., et al. (2016). The current state of knowledge about the dipping and non-dipping hypertension. Arter. Hypertens. 20, 33–43. doi: 10.5603/ah.2016.0007
Fisher, M. (2016). Cerebral microbleeds and thrombolysis: clinical consequences and mechanistic implications. JAMA Neurol. 73, 632–635. doi: 10.1001/jamaneurol.2016.0576
Fletcher, E., Gavett, B., Harvey, D., Farias, S. T., Olichney, J., Beckett, L., et al. (2018). Brain volume change and cognitive trajectories in aging. Neuropsychology 32, 436–449. doi: 10.1037/neu0000447
Fletcher, E., Singh, B., Harvey, D., Carmichael, O., and DeCarli, C. (2012). Adaptive image segmentation for robust measurement of longitudinal brain tissue change. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2012, 5319–5322. doi: 10.1109/embc.2012.6347195
Greenberg, S. M., Vernooij, M. W., Cordonnier, C., Viswanathan, A., Al-Shahi Salman, R., Warach, S., et al. (2009). Cerebral microbleeds: a guide to detection and interpretation. Lancet Neurol. 8, 165–174. doi: 10.1016/S1474-4422(09)70013-4
Gregoire, S. M., Chaudhary, U. J., Brown, M. M., Yousry, T. A., Kallis, C., Jäger, H. R., et al. (2009). The microbleed anatomical rating scale (MARS): reliability of a tool to map brain microbleeds. Neurology 73, 1759–1766. doi: 10.1212/wnl.0b013e3181c34a7d
Guo, H., Tabara, Y., Igase, M., Yamamoto, M., Ochi, N., Kido, T., et al. (2010). Abnormal nocturnal blood pressure profile is associated with mild cognitive impairment in the elderly: the J-SHIPP study. Hypertens. Res. 33, 32–36. doi: 10.1038/hr.2009.172
Kanemaru, A., Kanemaru, K., and Kuwajima, I. (2001). The effects of short-term blood pressure variability and nighttime blood pressure levels on cognitive function. Hypertens. Res. 24, 19–24. doi: 10.1291/hypres.24.19
Kario, K., Matsuo, T., Kobayashi, H., Imiya, M., Matsuo, M., and Shimada, K. (1996). Nocturnal fall of blood pressure and silent cerebrovascular damage in elderly hypertensive patients. Advanced silent cerebrovascular damage in extreme dippers. Hypertension 27, 130–135. doi: 10.1161/01.hyp.27.1.130
Kivipelto, M., Helkala, E. L., Laakso, M. P., Hanninen, T., Hallikainen, M., Alhainen, K., et al. (2001). Midlife vascular risk factors and alzheimer’s disease in later life: longitudinal, population based study. BMJ 322, 1447–1451. doi: 10.1136/bmj.322.7300.1447
Lacy, M., Kaemmerer, T., and Czipri, S. (2015). Standardized mini-mental state examination scores and verbal memory performance at a memory center: implications for cognitive screening. Am. J. Alzheimers Dis. Other Demen. 30, 145–152. doi: 10.1177/1533317514539378
Launer, L. J., Ross, G. W., Petrovitch, H., Masaki, K., Foley, D., White, L. R., et al. (2000). Midlife blood pressure and dementia: the honolulu-asia aging study. Neurobiol. Aging 21, 49–55. doi: 10.1016/S0197-4580(00)00096-8
Morris, J. C. (1993). The clinical dementia rating (CDR): current version and scoring rules. Neurology 43, 2412–2414. doi: 10.1212/wnl.43.11.2412-a
Nagai, M., Hoshide, S., Ishikawa, J., Shimada, K., and Kario, K. (2008). Ambulatory blood pressure as an independent determinant of brain atrophy and cognitive function in elderly hypertension. J. Hypertens. 26, 1636–1641. doi: 10.1097/hjh.0b013e3283018333
O’Brien, E., and Dolan, E. (2016). Ambulatory blood pressure monitoring for the effective management of antihypertensive drug treatment. Clin. Ther. 38, 2142–2151. doi: 10.1016/j.clinthera.2016.08.006
O’Brien, E., Parati, G., Stergiou, G., Asmar, R., Beilin, L., Bilo, G., et al. (2013). European society of hypertension position paper on ambulatory blood pressure monitoring. J. Hypertens. 31, 1731–1768. doi: 10.1097/HJH.0b013e328363e964
Ohya, Y., Ohtsubo, T., Tsuchihashi, T., Eto, K., Sadanaga, T., Nagao, T., et al. (2001). Altered diurnal variation of blood pressure in elderly subjects with decreased activity of daily living and impaired cognitive function. Hypertens. Res. 24, 655–661. doi: 10.1291/hypres.24.655
Paganini-Hill, A., Kawas, C. H., and Corrada, M. M. (2016). Lifestyle factors and dementia in the oldest-old: the 90+ study. Alzheimer Dis. Assoc. Disord. 30, 21–26. doi: 10.1097/wad.0000000000000087
Pfeffer, R. I., Kurosaki, T. T., Harrah, C. H. Jr., Chance, J. M., and Filos, S. (1982). Measurement of functional activities in older adults in the community. J. Gerontol. 37, 323–329. doi: 10.1093/geronj/37.3.323
Sander, D., Winbeck, K., Klingelhofer, J., and Conrad, B. (2000). Extent of cerebral white matter lesions is related to changes of circadian blood pressure rhythmicity. Arch. Neurol. 57, 1302–1307. doi: 10.1001/archneur.57.9.1302
Smolensky, M. H., Hermida, R. C., Reinberg, A., Sackett-Lundeen, L., and Portaluppi, F. (2016). Circadian disruption: new clinical perspective of disease pathology and basis for chronotherapeutic intervention. Chronobiol. Int. 33, 1101–1119. doi: 10.1080/07420528.2016.1184678
Sörös, P., Whitehead, S., Spence, J. D., and Hachinski, V. (2013). Antihypertensive treatment can prevent stroke and cognitive decline. Nat. Rev. Neurol. 9, 174–178. doi: 10.1038/nrneurol.2012.255
United Nations Department of Economic and Social Affairs Population Division. (2017). World population prospects: The 2017 Revision, Key Findings and Advance Tables. Working Paper No. ESA/P/WP/248. New York, NY: United Nations.
van Boxtel, M. P., Gaillard, C., Houx, P. J., Buntinx, F., de Leeuw, P. W., and Jolles, J. (1998). Is nondipping in 24 h ambulatory blood pressure related to cognitive dysfunction? J. Hypertens. 16, 1425–1432. doi: 10.1097/00004872-199816100-00005
van Boxtel, M. P., Henskens, L. H., Kroon, A. A., Hofman, P. A., Gronenschild, E. H., Jolles, J., et al. (2006). Ambulatory blood pressure, asymptomatic cerebrovascular damage and cognitive function in essential hypertension. J. Hum. Hypertens. 20, 5–13. doi: 10.1038/sj.jhh.1001934
Whitmer, R. A., Sidney, S., Selby, J., Johnston, S. C., and Yaffe, K. (2005). Midlife cardiovascular risk factors and risk of dementia in late life. Neurology 64, 277–281. doi: 10.1212/01.wnl.0000149519.47454.f2
Whittle, C., Corrada, M. M., Dick, M., Ziegler, R., Kahle-Wrobleski, K., Paganini-Hill, A., et al. (2007). Neuropsychological data in nondemented oldest old: the 90+ study. J. Clin. Exp. Neuropsychol. 29, 290–299. doi: 10.1080/13803390600678038
Yamada, M., Kasagi, F., Sasaki, H., Masunari, N., Mimori, Y., and Suzuki, G. (2003). Association between dementia and midlife risk factors: the radiation effects research foundation adult health study. J. Am. Geriatr. Soc. 51, 410–414. doi: 10.1046/j.1532-5415.2003.51117.x
Yamaguchi, Y., Wada, M., Sato, H., Nagasawa, H., Koyama, S., Takahashi, Y., et al. (2014). Impact of ambulatory blood pressure variability on cerebral small vessel disease progression and cognitive decline in community-based elderly Japanese. Am. J. Hypertens. 27, 1257–1267. doi: 10.1093/ajh/hpu045
Keywords: ambulatory blood pressure monitoring, cognition, cognitive neurological examination, neuropsychological tests, magnetic resonance imaging
Citation: Paganini-Hill A, Bryant N, Corrada MM, Greenia DE, Fletcher E, Singh B, Floriolli D, Kawas CH and Fisher MJ (2019) Blood Pressure Circadian Variation, Cognition and Brain Imaging in 90+ Year-Olds. Front. Aging Neurosci. 11:54. doi: 10.3389/fnagi.2019.00054
Received: 14 September 2018; Accepted: 22 February 2019;
Published: 17 April 2019.
Edited by:
Patrizia Mecocci, University of Perugia, ItalyReviewed by:
Xiao-Min Zhao, Taishan Medical University, ChinaJ. David Spence, University of Western Ontario, Canada
Copyright © 2019 Paganini-Hill, Bryant, Corrada, Greenia, Fletcher, Singh, Floriolli, Kawas and Fisher. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Annlia Paganini-Hill, apaganin@uci.edu
 Annlia Paganini-Hill
Annlia Paganini-Hill Natalie Bryant2
Natalie Bryant2  David Floriolli
David Floriolli Mark J. Fisher
Mark J. Fisher