The Effective Cognitive Assessment and Training Methods for COVID-19 Patients With Cognitive Impairment
- 1Brain Computer Intelligence and Intelligent Health Institution, Institute of Artificial Intelligence, University of Science and Technology Beijing, Beijing, China
- 2The Key Laboratory for Computer Virtual Technology and System Integration of Hebei Province, School of Information Science and Engineering, Yanshan University, Qinhuangdao, China
- 3Department of Statistics, School of Science, Yanshan University, Qinhuangdao, China
- 4Department of Computer Science and Technology, School of Mathematics and Information Science and Technology, Hebei Normal University of Science and Technology, Qinhuangdao, China
- 5Department of Biomedical Engineering, Chengde Medical University, Chengde, China
- 6Department of Computer and Communication Systems Engineering, Faculty of Engineering, Universiti Putra Malaysia, Serdang, Malaysia
- 7Department of Neurology, Xuanwu Hospital of Capital Medical University, Beijing, China
Introduction
Since late 2019, COVID-19 has been raging worldwide. Related studies have reported that many COVID-19 patients present cognitive sequelae (Ahmad and Rathore, 2020; Baschi et al., 2020; Gunasekaran et al., 2020; Heneka et al., 2020; Kieron et al., 2020; Koralnik and Tyler, 2020; Pinna et al., 2020; Vespignani et al., 2020; Woo et al., 2020; Taquet et al., 2021). However, the implementation of isolation measures greatly limits the traditional cognitive impairment assessment and treatment methods (Lara et al., 2020). Therefore, we need to explore better ways to assess and train cognitive impairment in patients with COVID-19.
The rapid development of a brain-computer interface (BCI), virtual reality (VR), and artificial intelligence has promoted the diagnosis and treatment of cognitive impairment in the direction of intellectual development. Studies have shown that BCI-VR technology can compensate for the limitations of BCI alone and provide new rehabilitation and assessment methods for patients with cognitive impairment, which has attracted increasing attention (Wen et al., 2018, 2020; Bauer and Andringa, 2020; Mancuso et al., 2020; Pinter et al., 2021).
This paper first discussed current cognitive impairment assessment and rehabilitation methods for patients with cognitive impairment. On this basis, we proposed a new comprehensive strategy for cognitive impairment assessment and rehabilitation based on BCI-VR. It will be a new approach for cognitive rehabilitation that fully integrates the accurate detection of BCI technology and the effective training of VR technology. Further, we discussed the advantages and challenges of BCI-VR in cognitive impairment assessment and rehabilitation training for COVID-19 patients in this current pandemic.
Current Cognitive Impairment of COVID-19 Patients
Since the start of the COVID-19 pandemic, a growing number of studies have reported neurological impairment in COVID-19 patients (Ahmad and Rathore, 2020; Gunasekaran et al., 2020; Heneka et al., 2020; Kieron et al., 2020; Koralnik and Tyler, 2020; Pinna et al., 2020; Vespignani et al., 2020; Taquet et al., 2021). We found that stroke and cognitive impairment are the most common manifestations of neurological impairment in COVID-19 patients (Belani et al., 2020; Fara et al., 2020; Fatima et al., 2020; Haji Akhoundi et al., 2020; Heneka et al., 2020; Jain et al., 2020; Mahboob et al., 2020; Merkler et al., 2020; Rajdev et al., 2020; Sezgin et al., 2020; Taquet et al., 2021). Studies showed that the incidence of stroke in confirmed hospitalized COVID-19 patients ranged from 2.8 to 5.4%, the incidence of cognitive impairment was 26%, and patients with stroke often cause concurrent manifestations of cognitive impairment (Haji Akhoundi et al., 2020; Majidi et al., 2020; Oxley et al., 2020; Sun et al., 2020; Taquet et al., 2021). Other studies showed that patients with neurological impairment caused by COVID-19 tended to be younger (Ahmad and Rathore, 2020; Cavallieri et al., 2020; Oxley et al., 2020; Woo et al., 2020; Harrison et al., 2021).
In the current pandemic, both hospitals and patients are facing huge and severe challenges in the assessment and rehabilitation training of patients with cognitive impairment (Coetzer, 2020; Richardson et al., 2020). Studies showed, as the COVID-19 pandemic intensified, patients with cognitive impairment were limited in going out for rehabilitation training, which had many negative effects on the mental state of patients and his mental condition was deteriorating (Lara et al., 2020; Manca et al., 2020; Devita et al., 2021). Therefore, we need to explore better ways to assess and train cognitive impairment in patients with COVID-19.
Current Evaluation Methods of Cognitive Impairment
Currently, common cognitive impairment methods include cognitive scale, neuroimaging technology and new wearable devices. In clinical practice, the most classic method of objective evaluation is the cognitive scale. The cognitive scale test achieves the evaluation effect by comparing the patient's test results with the scale indicators, include: Mini-Mental State Examination (MMSE) (Pangman et al., 2000), Montreal Cognitive Assessment (MoCA) (Nasreddine et al., 2019) and Activities of Daily Living (ADL) (Lopez Mongil, 2017), Auditory Verbal Learning Test (AVLT) (Stricker et al., 2021), Trail Marking Test (TMT) (Lunardini et al., 2020), etc. Recently, Burns et al. proposed a new hybrid scale—Free-COG, which could also be used to assess subjects' cognitive and executive functions (Burns et al., 2021). However, subjective factors of the testers reduced the accuracy of the results in the cognitive scale test.
The degree of cognitive impairment of patients is evaluated by observing the changes of brain structure through imaging (Knopman and Petersen, 2014). Among them, the commonly used neuroimaging techniques include: structural neuroimaging techniques (Zhang et al., 2019), functional neuroimaging techniques, positron emission tomography (PET), molecular imaging, and functional magnetic resonance imaging (fMRI) (Zhang et al., 2019; Xu et al., 2020). However, neuroimaging technology equipment is larger, and detection costs are higher, which significantly limits its application (Narayanan and Murray, 2016).
Relevant studies have introduced wearable devices into the assessment of cognitive impairment (Narayanan and Murray, 2016). Related study showed that wearable biosensor devices might be a viable tool to assess physiological changes in patients with AD, enabling remote and continuous monitoring of neurocognitive function in patients (Saif et al., 2019; Stavropoulos et al., 2020; Eggenberger et al., 2021). However, the evaluation indicators of the new wearable devices are uncertain, and there is no unified standard in use.
Current Rehabilitation Methods of Cognitive Impairment
Currently, commonly used cognitive rehabilitation methods include medication-assisted, cognitive rehabilitation training, and home rehabilitation.
Medication-assisted therapy can inhibit the induction of cognitive impairment or other diseases (Rejdak and Grieb, 2020; Zhaojun and Miaser, 2020). The implementation of medication-assisted therapy is costly, and it also only serves as an adjustment role in the rehabilitation of cognitive impairment and may be accompanied by other side effects (Jin-xuan et al., 2020).
General cognitive rehabilitation training usually refers to systematic and targeted training depending on the patient's cognitive function under face-to-face guidance by the rehabilitation therapist. Studies showed it can improve or maintain patients' cognitive abilities related to daily task performance, so as to prevent or delay cognitive decline (Irazoki et al., 2020). But it requires the participation of both the therapist and the patient. And there are many limitations in the rehabilitation plan, such as time, personnel, and cost.
During the COVID-19 pandemic, traditional rehabilitation training is limited, researchers have suggested remote home rehabilitation for patients with cognitive impairment (Chang and Boudier-Revéret, 2020) and adopting some remote home rehabilitation measures (Richardson et al., 2020). Through literature analysis and comparison, it is found that home rehabilitation provides great convenience for both the therapists and patients, which can meet the needs of patients with cognitive impairment (Natta et al., 2015; Gately et al., 2019). However, long-term home rehabilitation reduces contact between patients with cognitive impairment and the outside world and has a certain impact on the patient's psychological state.
BCI-VR Strategy for Evaluating and Rehabilitating COVID-19 Patients With Cognitive Impairment
It can be seen that there are many limitations in traditional cognitive impairment assessment and cognitive rehabilitation training during the COVID-19 pandemic. There is an urgent need for a novel and comprehensive strategy to overcome the shortcomings of traditional approaches. Thus, we propose a comprehensive rehabilitation strategy of BCI-VR, which combines the characteristics of accurate detection of BCI technology with the characteristics of effective training of VR technology and provide one-stop service for cognitive impairment assessment and cognitive rehabilitation training for COVID-19 patients. This strategy is described in detail below.
In BCI technology, EEG signals can be used to objectively and accurately detect the brain specificity of patients with cognitive impairment, which could be performed in the community or even at home (PoŽar et al., 2020; San-Juan et al., 2020; Pinter et al., 2021). VR technology provides an immersive environment for patients with cognitive impairment, improves patient participation and training effect (Snider et al., 2013; Appel et al., 2020; Bauer and Andringa, 2020; Mancuso et al., 2020; Thielbar et al., 2020). This makes the new rehabilitation strategy of BCI-VR proposed in this research more feasible.
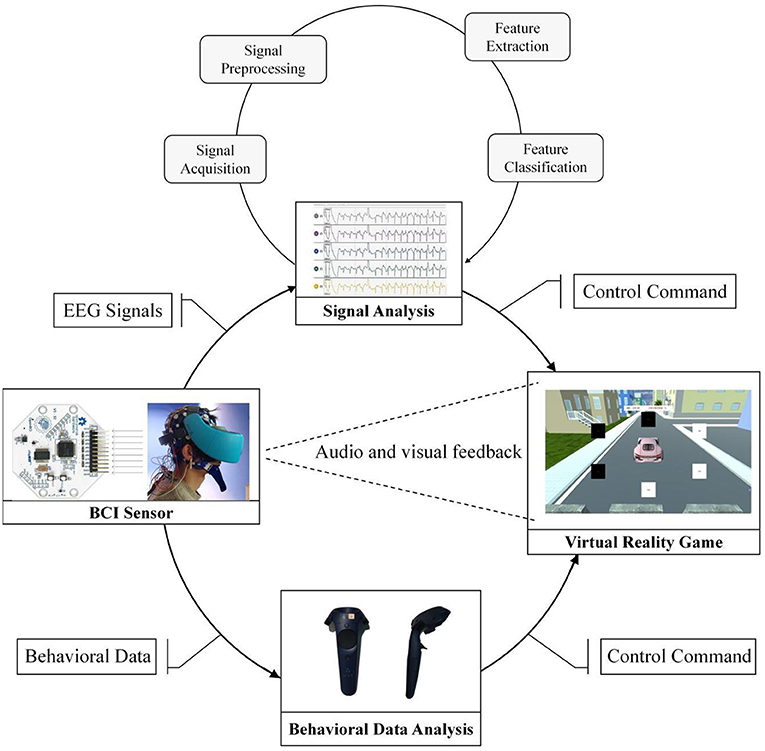
The BCI-VR rehabilitation strategy proposed in this study provides guarantee for cognitive impairment assessment and cognitive rehabilitation training during the COVID-19 pandemic, which can meet the cognitive rehabilitation needs of patients at home. Moreover, the application of VR technology would greatly alleviate the negative psychological state and mental state of patients with cognitive impairment caused by blocking (Gao et al., 2020). In the implementation process (as shown in Figure 1), BCI-VR requires computers, EEG acquisition instruments and VR wearable devices, which are relatively light and common compared with medical devices in hospitals.
The BCI-VR strategy is specifically divided into a behavioral data analysis module and an EEG analysis module. During cognitive rehabilitation training in a VR environment, the EEG signals of patients with cognitive impairment are collected synchronously for offline or real-time online analysis (Taquet et al., 2021). Rehabilitation training data of patients with cognitive impairment in the VR environment will be recorded in the behavioral data analysis module. With the advancement of the rehabilitation training process, behavior data analysis can be intuitive to see its effect. For example, after a month of spatial navigation ability training, the first day of the spatial navigation ability will compare the 30 days of spatial navigation ability to test the result of rehabilitation training (Vespignani et al., 2020).
The EEG signals of cognitive impairment patients during rehabilitation training will be recorded and processed in the EEG analysis module. Continuous rehabilitation training will gradually show the characteristics of brain regions that constantly change. In patients, these changes can play an evaluation role.
Compared with traditional methods, BCI-VR has the following advantages: It reduces the need for patients with cognitive impairment to go out, and they can receive effective cognitive impairment assessment and rehabilitation at home; long-term home rehabilitation can relieve the mental state of patients with cognitive impairment, such as impatience and depression; it provides a low-cost cognitive rehabilitation strategy that uses relatively light and common equipment, which can be used in a wide range of applications.
Discussion
More and more studies have been reported on the symptoms of cognitive impairment in COVID-19 patients (Baschi et al., 2020; Haji Akhoundi et al., 2020; Heneka et al., 2020; Jain et al., 2020). These patients need to undergo necessary cognitive impairment assessment and rehabilitation training after they are cured from COVID-19. Traditional cognitive impairment assessment and rehabilitation training have been greatly limited during the pandemic. BCI-VR provides a feasible method for patients in this situation. Recent studies have shown that the EEG signals of COVID-19 patients have certain characteristics (Sethi, 2020; Kubota et al., 2021). More and more researchers suggested that more attention should be paid to the EEG signals of patients during the epidemic (Haines et al., 2020). Perhaps BCI-VR may also monitor whether SARS-COV-2 virus reactivation occur while conducting cognitive rehabilitation training for COVID-19 patients after they are cured.
The application scenarios and implementation forms of the BCI-VR strategy are relatively flexible. It can be applied in rehabilitating various cognitive functions, such as memory, spatial cognition, or language perception, and multi-person interactive rehabilitation training, cross-scene interactive rehabilitation training, or cross-age rehabilitation training. Moreover, studies have shown that cognitive rehabilitation training with multi-person interaction in a VR environment has a better effect (Thielbar et al., 2020). Therefore, BCI-VR is better developed and applied in cognitive impairment rehabilitation.
BCI-VR in the assessment and rehabilitation of cognitive impairment is still in its early stages. In future research, BCI-VR will make great progress in integrating medical and industrial intelligence, which is not limited to cognitive impairment rehabilitation. However, the current optimized data fusion algorithm and feature extraction of high-dimensional data are still a bottleneck for BCI-VR development. In the following work, we will continue to solve the key BCI and VR technologies in monitoring, evaluating, and rehabilitating cognitive impairment.
Conclusion
Through literature analysis and summary, we will find that more and more patients, including young people with COVID-19, exhibit signs of cognitive impairment. We analyze some popular traditional cognitive impairment assessment and rehabilitation methods and summarize their limitations during the current pandemic. Moreover, the proposed new comprehensive rehabilitation BCI-VR strategy and the cognitive impairment assessment and rehabilitation process of BCI-VR are expounded. The advantages of BCI-VR in cognitive impairment assessment and rehabilitation are discussed, and the development trend of this technology in the future is evaluated. However, the optimized data fusion algorithm and feature extraction of high-dimensional data are still the bottlenecks of BCI-VR development. Nevertheless, we expect that BCI-VR will soon play an important role in many fields, such as medical rehabilitation, providing more service support for humans.
Author Contributions
DW, YZ, and HS contributed to conception and design of the study. JX, ZW, and YL searched the database. DW, JX, and JL performed the analysis of literature. JX, DW, and ZW wrote the first draft of the manuscript. YL and SW wrote sections of the manuscript. XD and MS revised this paper and analyzed the literature. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This work was supported in part by National Natural Science Foundation of China (Nos. 61876165 and 61503326) and National Key Research and Development Program of China (No. 2021YFF1200603).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ahmad, I., and Rathore, F. A. (2020). Neurological manifestations and complications of COVID-19: a literature review. J. Clin. Neurosci. 77, 8–12. doi: 10.1016/j.jocn.2020.05.017
Appel, L., Appel, E., Bogler, O., Wiseman, M., Cohen, L., Ein, N., et al. (2020). Older adults with cognitive and/or physical impairments can benefit from immersive virtual reality experiences: a feasibility study. Front. Med. 6:329. doi: 10.3389/fmed.2019.00329
Baschi, R., Luca, A., Nicoletti, A., Caccamo, M., Cicero, C. E., D'Agate, C., et al. (2020). Changes in motor, cognitive, and behavioral symptoms in parkinson's disease and mild cognitive impairment during the COVID-19 lockdown. Front. Psychiatry. 11:590134. doi: 10.3389/fpsyt.2020.590134
Bauer, A. C. M., and Andringa, G. (2020). The potential of immersive virtual reality for cognitive training in elderly. Gerontology. 66, 614–623. doi: 10.1159/000509830
Belani, P., Schefflein, J., Kihira, S., Rigney, B., Delman, B. N., Mahmoudi, K., et al. (2020). COVID-19 is an independent risk factor for acute ischemic stroke. Am. J. Neuroradiol. 41, 1361–1364. doi: 10.3174/ajnr.A6650
Burns, A., Harrison, J. R., Symonds, C., and Morris, J. (2021). A novel hybrid scale for the assessment of cognitive and executive function: the Free-Cog. Int. J. Geriatr. Psych. 36, 566–572. doi: 10.1002/gps.5454
Cavallieri, F., Marti, A., Fasano, A., Dalla Salda, A., Ghirarduzzi, A., Moratti, C., et al. (2020). Prothrombotic state induced by COVID-19 infection as trigger for stroke in young patients: a dangerous association. eNeurologicalSci. 20:100247. doi: 10.1016/j.ensci.2020.100247
Chang, M. C., and Boudier-Revéret, M. (2020). Usefulness of telerehabilitation for stroke patients during the COVID-19 pandemic. Am. J. Phys. Med. Rehab. 99:582. doi: 10.1097/PHM.0000000000001468
Coetzer, R.. (2020). First impressions of performing bedside cognitive assessment of COVID-19 inpatients. J. Am. Geriatr. Soc. 68, 1389–1390. doi: 10.1111/jgs.16561
Devita, M., Bordignon, A., Sergi, G., and Coin, A. (2021). The psychological and cognitive impact of Covid-19 on individuals with neurocognitive impairments: Research topics and remote intervention proposals. Aging Clin. Exp. Res. 33, 733–736. doi: 10.1007/s40520-020-01637-6
Eggenberger, P., Bürgisser, M., Rossi, R. M., and Annaheim, S. (2021). Body temperature is associated with cognitive performance in older adults with and without mild cognitive impairment: a cross-sectional analysis. Front. Aging Neurosci. 13:585904. doi: 10.3389/fnagi.2021.585904
Fara, M. G., Stein, L. K., Skliut, M., Morgello, S., Fifi, J. T., and Dhamoon, M. S. (2020). Macrothrombosis and stroke in patients with mild Covid-19 infection. J. Thromb. Haemost. 18, 2031–2033. doi: 10.1111/jth.14938
Fatima, N., Saqqur, M., Qamar, F., Shaukat, S., and Shuaib, A. (2020). Impact of COVID-19 on neurological manifestations: an overview of stroke presentation in pandemic. Neurol. Sci. 41, 2675–2679. doi: 10.1007/s10072-020-04637-6
Gao, Z., Lee, J. E., McDonough, D. J., and Albers, C. (2020). Virtual reality exercise as a coping strategy for health and wellness promotion in older adults during the COVID-19 pandemic. J. Clin. Med. 9:1986. doi: 10.3390/jcm9061986
Gately, M. E., Trudeau, S. A., and Moo, L. R. (2019). In-home video telehealth for dementia management: implications for rehabilitation. Curr. Geriatr. Rep. 8, 239–249. doi: 10.1007/s13670-019-00297-3
Gunasekaran, K., Amoah, K., Rajasurya, V., and Buscher, M. G. (2020). Stroke in a young COVID-19 patient. QJM 113, 573–574. doi: 10.1093/qjmed/hcaa177
Haines, S., Caccamo, A., Chan, F., Galaso, G., Catinchi, A., and Gupta, P. K. (2020). Practical considerations when performing neurodiagnostic studies on patients with COVID-19 and other highly virulent diseases. Neurodiagn. J. 60, 78–95. doi: 10.1080/21646821.2020.1756132
Haji Akhoundi, F., Sahraian, M. A., and Naser Moghadasi, A. (2020). Neuropsychiatric and cognitive effects of the COVID-19 outbreak on multiple sclerosis patients. Multiple Scler. Relat. Disord. 41:102164. doi: 10.1016/j.msard.2020.102164
Harrison, S. L., Fazio-Eynullayeva, E., Lane, D. A., Underhill, P., and Lip, G. Y. H. (2021). Higher mortality of ischaemic stroke patients hospitalized with COVID-19 compared to historical controls. Cerebrovasc. Dis. 50, 326–331. doi: 10.1159/000514137
Heneka, M. T., Golenbock, D., Latz, E., Morgan, D., and Brown, R. (2020). Immediate and long-term consequences of COVID-19 infections for the development of neurological disease. Alzheimer's Res. Ther. 12:69. doi: 10.1186/s13195-020-00640-3
Irazoki, E., Contreras-Somoza, L. M., Toribio-Guzmán, J. M., Jenaro-Río, C., van der Roest, H., and Franco-Martín, M. A. (2020). Technologies for cognitive training and cognitive rehabilitation for people with mild cognitive impairment and dementia. A systematic review. Front. Psychol. 11:648. doi: 10.3389/fpsyg.2020.00648
Jain, R., Young, M., Dogra, S., Kennedy, H., Nguyen, V., Jones, S., et al. (2020). COVID-19 related neuroimaging findings: a signal of thromboembolic complications and a strong prognostic marker of poor patient outcome. J. Neurol. Sci. 414:116923. doi: 10.1016/j.jns.2020.116923
Jin-xuan, Z., Rui, S., Tian-hao, M., and Hong, W. (2020). Progress in rehabilitation treatment of mild cognitive impairment. Chinese J. Alzheimer's Dis. Relat. Disord. 3, 147–153. doi: 10.3969/j.issn.2096-5516.2020.02.011
Kieron, S., Laura, M., McColl, B. W., Elkind, M. S., Allan, S. M., and Smith, C. J. (2020). Preceding infection and risk of stroke: an old concept revived by the COVID-19 pandemic. Int. J. Stroke. 15, 722–732. doi: 10.1177/1747493020943815
Knopman, D. S., and Petersen, R. C. (2014). Mild cognitive impairment and mild dementia: a clinical perspective. Mayo Clin. Proc. 89, 1452–1459. doi: 10.1016/j.mayocp.2014.06.019
Koralnik, I. J., and Tyler, K. L. (2020). COVID-19: a global threat to the nervous system. Ann. Neurol. 88, 1–11. doi: 10.1002/ana.25807
Kubota, T., Gajera, P. K., and Kuroda, N. (2021). Meta-analysis of EEG findings in patients with COVID-19. Epilepsy Behav. 115:107682. doi: 10.1016/j.yebeh.2020.107682
Lara, B., Carnes, A., Dakterzada, F., Benitez, I., and Pinol-Ripoll, G. (2020). Neuropsychiatric symptoms and quality of life in Spanish patients with Alzheimer's disease during the COVID-19 lockdown. Eur. J. Neurol. 27, 1744–1747. doi: 10.1111/ene.14339
Lopez Mongil, R.. (2017). [Cognitive impairment/dementia: Assessment and follow-up. Functional aspects]. Deterioro cognitivo/demencia: Valoracion y seguimiento. Aspectos funcionales. Revista espanola de geriatria y gerontologia. 52, 28–33. doi: 10.1016/S0211-139X(18)30077-5
Lunardini, F., Luperto, M., Romeo, M., Basilico, N., Daniele, K., Azzolino, D., et al. (2020). Supervised digital neuropsychological tests for cognitive decline in older adults: usability and clinical validity study. JMIR mHealth uHealth 8:e17963. doi: 10.2196/17963
Mahboob, S., Boppana, S. H., Rose, N. B., Beutler, B. D., and Tabaac, B. J. (2020). Large vessel stroke and COVID-19: case report and literature review. eNeurologicalSci 20:100250. doi: 10.1016/j.ensci.2020.100250
Majidi, S., Fifi, J. T., Ladner, T. R., Lara-Reyna, J., Yaeger, K. A., Yim, B., et al. (2020). Emergent large vessel occlusion stroke during new york city's COVID-19 outbreak clinical characteristics and paraclinical findings. Stroke. 51, 2656–2663. doi: 10.1161/STROKEAHA.120.030397
Manca, R., De Marco, M., and Venneri, A. (2020). The impact of COVID-19 infection and enforced prolonged social isolation on neuropsychiatric symptoms in older adults with and without dementia: a review. Front. Psychiatry. 11:585540. doi: 10.3389/fpsyt.2020.585540
Mancuso, V., Stramba-Badiale, C., Cavedoni, S., Pedroli, E., Cipresso, P., and Riva, G. (2020). Virtual reality meets non-invasive brain stimulation: integrating two methods for cognitive rehabilitation of mild cognitive impairment. Front. Neurol. 11:566731. doi: 10.3389/fneur.2020.566731
Merkler, A. E., Parikh, N. S., Mir, S., Gupta, A., Kamel, H., Lin, E., et al. (2020). Risk of ischemic stroke in patients with Coronavirus Disease 2019 (COVID-19) vs patients with influenza. JAMA Neurol. 77, 1366–1372. doi: 10.1001/jamaneurol.2020.2730
Narayanan, L., and Murray, A. D. (2016). What can imaging tell us about cognitive impairment and dementia? World J. Radiol. 8:240. doi: 10.4329/wjr.v8.i3.240
Nasreddine, Z. S., Phillips, N. A., Bedirian, V., Charbonneau, S., Whitehead, V., Collin, I., et al. (2019). The montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment (vol 53, pg 695, 2005). J. Am. Geriatr. Soc. 67:1991. doi: 10.1111/j.1532-5415.2005.53221.x
Natta, D. D. N., Alagnide, E., Kpadonou, G. T., Stoquart, G. G., Detrembleur, C., and Lejeune, T. M. (2015). Feasibility of a self-rehabilitation program for the upper limb for stroke patients in Benin. Ann. Phys. Rehabil. Med. 58, 322–325. doi: 10.1016/j.rehab.2015.08.003
Oxley, T. J., Mocco, J., Majidi, S., Kellner, C. P., Shoirah, H., Singh, I. P., et al. (2020). Large-Vessel stroke as a presenting feature of covid-19 in the young. [Case Reports; Letter]. New Engl. J. Med. 382:e60. doi: 10.1056/NEJMc2009787
Pangman, V. C., Sloan, J., and Guse, L. (2000). An examination of psychometric properties of the mini-mental state examination and the standardized mini-mental state examination: Implications for clinical practice. Appl. Nurs. Res. 13, 209–213. doi: 10.1053/apnr.2000.9231
Pinna, P., Grewal, P., Hall, J. P., Tavarez, T., Dafer, R. M., Garg, R., et al. (2020). Neurological manifestations and COVID-19: experiences from a tertiary care center at the Frontline. J. Neurol. Sci. 415:116969. doi: 10.1016/j.jns.2020.116969
Pinter, D., Kober, S. E., Fruhwirth, V., Berger, L., Damulina, A., Khalil, M., et al. (2021). MRI correlates of cognitive improvement after home-based EEG neurofeedback training in patients with multiple sclerosis: a pilot study. J. Neurol. 268, 3808–3816. doi: 10.1007/s00415-021-10530-9
PoŽar, R., Giordani, B., and Kavcic, V. (2020). Effective differentiation of mild cognitive impairment by functional brain graph analysis and computerized testing. PLoS ONE. 15:e230099. doi: 10.1371/journal.pone.0230099
Rajdev, K., Lahan, S., Klein, K., Piquette, C. A., and Thi, M. (2020). Acute ischemic and hemorrhagic stroke in COVID-19: mounting evidence. Cureus 12:e10157. doi: 10.7759/cureus.10157
Rejdak, K., and Grieb, P. (2020). Adamantanes might be protective from COVID-19 in patients with neurological diseases: multiple sclerosis, parkinsonism and cognitive impairment. Multiple Scler. Relat. Disord. 42:102163. doi: 10.1016/j.msard.2020.102163
Richardson, S. J., Carroll, C. B., Close, J., Gordon, A. L., O'Brien, J., Quinn, T. J., et al. (2020). Research with older people in a world with COVID-19: identification of current and future priorities, challenges and opportunities. Age Ageing. 49, 901–906. doi: 10.1093/ageing/afaa149
Saif, N., Yan, P., Niotis, K., Scheyer, O., Rahman, A., Berkowitz, M., et al. (2019). Feasibility of using a wearable biosensor device in patients at risk for Alzheimer's disease dementia. J. Prevent. Alzheimer's Dis. 7, 104–111. doi: 10.14283/jpad.2019.39
San-Juan, D., Jiménez, C. R., Camilli, C. X., de la Cruz Reyes, L. A., Galindo, E. G. A., Burbano, G. E. R., et al. (2020). Guidance for clinical neurophysiology examination throughout the COVID-19 pandemic. Latin American chapter of the IFCN task force –COVID-19. Clin. Neurophysiol. 131, 1589–1598. doi: 10.1016/j.clinph.2020.04.011
Sethi, N. K.. (2020). EEG during the COVID-19 pandemic: what remains the same and what is different. Clin. Neurophysiol. 131:1462. doi: 10.1016/j.clinph.2020.04.007
Sezgin, M., Ekizoglu, E., Yesilot, N., and Coban, O. (2020). Stroke during covid-19 pandemic. Arch. Neuropsychiatry. 57, 83–84. doi: 10.29399/npa.27196
Snider, J., Plank, M., Lee, D., and Poizner, H. (2013). Simultaneous neural and movement recording in large-scale immersive virtual environments. IEEE T. Biomed. Circ. S. 7, 713–721. doi: 10.1109/TBCAS.2012.2236089
Stavropoulos, T. G., Papastergiou, A., Mpaltadoros, L., Nikolopoulos, S., and Kompatsiaris, I. (2020). IoT wearable sensors and devices in elderly care: a literature review. Sensors Basel. 20:2826. doi: 10.3390/s20102826
Stricker, N. H., Christianson, T. J., Lundt, E. S., Alden, E. C., Machulda, M. M., Fields, J. A., et al. (2021). Mayo normative studies: regression-based normative data for the auditory verbal learning test for ages 30–91 years and the importance of adjusting for sex. J. Int. Neuropsych. Soc. 27, 211–226. doi: 10.1017/S1355617720000752
Sun, J., Lv, X., Gao, X., Chen, Z., Wei, D., Ling, Y., et al. (2020). The association between serum uric acid level and the risk of cognitive impairment after ischemic stroke. Neurosci. Lett. 734:135098. doi: 10.1016/j.neulet.2020.135098
Taquet, M., Geddes, J. R., Husain, M., Luciano, S., and Harrison, P. J. (2021). 6-Month neurological and psychiatric outcomes in 236379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry 8, 416–427. doi: 10.1016/S2215-0366(21)00084-5
Thielbar, K., Spencer, N., Tsoupikova, D., Ghassemi, M., and Kamper, D. (2020). Utilizing multi-user virtual reality to bring clinical therapy into stroke survivors' homes. J. Hand Ther. 33, 246–253. doi: 10.1016/j.jht.2020.01.006
Vespignani, H., Colas, D., Lavin, B. S., Soufflet, C., Maillard, L., Pourcher, V., et al. (2020). Report on electroencephalographic findings in critically ill patients with COVID-19. Ann. Neurol. 88, 626–630. doi: 10.1002/ana.25814
Wen, D., Fan, Y., Hsu, S., Xu, J., Zhou, Y., Tao, J., et al. (2020). Combining brain-computer interface and virtual reality for rehabilitation in neurological diseases: a narrative review. Ann. Phys. Rehabil. Med. 64:101404. doi: 10.1016/j.rehab.2020.03.015
Wen, D., Lan, X., Zhou, Y., Li, G., Hsu, S., and Jung, T. (2018). The study of evaluation and rehabilitation of patients with different cognitive impairment phases based on virtual reality and EEG. Front. Aging Neurosci. 10:88. doi: 10.3389/fnagi.2018.00088
Woo, M. S., Malsy, J., Pöttgen, J., Seddiq Zai, S., Ufer, F., Hadjilaou, A., et al. (2020). Frequent neurocognitive deficits after recovery from mild COVID-19. Brain Commun. 2:fcaa205. doi: 10.1093/braincomms/fcaa205
Xu, M., Wang, Z., Zhang, H., Pantazis, D., Wang, H., and Li, Q. (2020). A new graph Gaussian embedding method for analyzing the effects of cognitive training. PLoS Comput. Biol. 16:e1008186. doi: 10.1371/journal.pcbi.1008186
Zhang, X., Su, J., Gao, C., Ni, W., Gao, X., Li, Y., et al. (2019). Progression in vascular cognitive impairment: pathogenesis, neuroimaging evaluation, and treatment. Cell Transplant. 28, 18–25. doi: 10.1177/0963689718815820
Keywords: cognitive assessment and training, COVID-19 patients, cognitive impairment, brain-computer interface, virtual reality
Citation: Wen D, Xu J, Wu Z, Liu Y, Zhou Y, Li J, Wang S, Dong X, Saripan MI and Song H (2022) The Effective Cognitive Assessment and Training Methods for COVID-19 Patients With Cognitive Impairment. Front. Aging Neurosci. 13:827273. doi: 10.3389/fnagi.2021.827273
Received: 01 December 2021; Accepted: 16 December 2021;
Published: 11 January 2022.
Edited by:
Peng Xu, University of Electronic Science and Technology of China, ChinaReviewed by:
Chao Chen, Tianjin University of Technology, ChinaYuliang Ma, Hangzhou Dianzi University, China
Copyright © 2022 Wen, Xu, Wu, Liu, Zhou, Li, Wang, Dong, Saripan and Song. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yanhong Zhou, yhzhou168@163.com; Haiqing Song, songhq@xwhosp.org
 Dong Wen
Dong Wen Jian Xu
Jian Xu Zhonglin Wu2
Zhonglin Wu2  Yanhong Zhou
Yanhong Zhou Xianlin Dong
Xianlin Dong M. Iqbal Saripan
M. Iqbal Saripan Haiqing Song
Haiqing Song