- 1Department of Internal Medicine, Center for Value-Based Care Research, Medicine Institute, Cleveland Clinic, Cleveland, OH, USA
- 2Department of Quantitative Health Sciences, Lerner Research Institute, Cleveland Clinic, Cleveland, OH, USA
The Problem
Conflicting results of two major randomized trials on prostate cancer mortality (1, 2) have led to evolving guidelines for clinicians regarding prostate cancer screening (3–6). While the European Randomised Study of Screening for Prostate Cancer (ERSPC) showed that one prostate cancer death could be prevented per 781 men screened, the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial showed no mortality benefit at 13 years of follow-up (1, 2). Because of the question of mortality benefit and the possible harms of screening, the United States Preventive Services Task Force (USPSTF) initially recommended in 2008 against screening men over age 75 for prostate cancer (3) then in 2012 against screening for prostate cancer at any age (4). However, it is most recently recommended in 2013 by both the American College of Physicians (ACP) and the American Urologic Association (AUA) that screening for prostate cancer occurs through a process of shared decision making (5, 6). While it is not recommended to screen men for prostate cancer at age 70 or above, or men with a life expectancy of less than 10–15 years, for men with average risk of developing prostate cancer, these shared decisions should occur between physicians and patients for men starting at age 50. For those men with high risk of developing prostate cancer, including men with a family history of prostate cancer or African-American men, these conversations could start as early as age 40 (5, 6).
Most of these shared discussions will initially occur between men and their primary care physician. Previous reports of decision aids for prostate cancer screening have shown improvement in patient knowledge and in decisional conflict as well as satisfaction with the decision (7). However, it is also known that patients may be more likely to be aware of the benefits of screening decisions and not the harms, and may ultimately rely on the physician’s recommendation, and it is not clear if the use of decision support alters prostate-specific antigen (PSA) testing behavior (8). Indeed, the rates of PSA testing were reduced in older men after the initial USPSTF recommendations (9–11) and in men over age 50 after the 2012 recommendations (12). However, is it not known to what extent shared decision making contributed to the decreased screening rates observed, whether shared decision making is occurring more frequently since the ACP and AUA recommendations were released, or to what degree patient or provider factors have contributed to the decline in screening rates.
Barriers to shared decision making regarding prostate cancer screening include lack of time for discussions as well as physician and patient factors (13–18). Patients may address an average of 25 problems during some chronic care and primary care visits (19), and cancer screening discussions may not be prioritized when management of multiple chronic diseases is also needed during the same office visit. More importantly, primary care physicians do not readily have access to tools that can promote shared decision making for prostate cancer screening. Elwyn et al. have proposed a model of “choice, option, and decision talk” to be used for shared decision making conversations in the clinical encounter (20). For a complex decision, such as prostate cancer screening, we propose the use of a simple tool in a routine outpatient encounter to begin this discussion, to accomplish the first two steps of this model: (1) make the patient aware that he has a choice and (2) begin to consider the options. We suggest that the decision is discussed after the patient has had appropriate time to consider the choice and options. This step may occur within the same visit or at a later time.
Explanation of Constructs
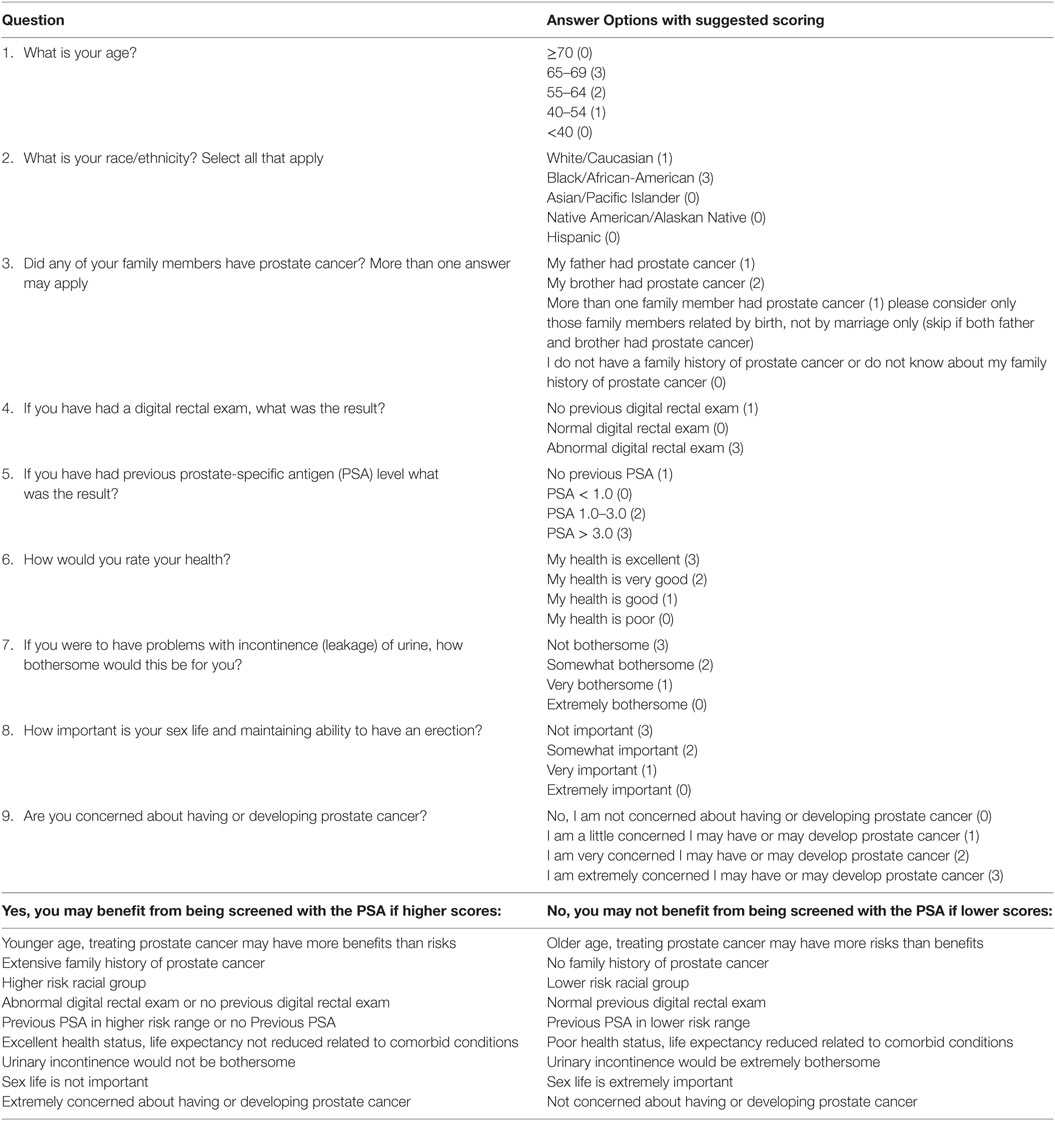
We propose shared decision making for prostate cancer in a primary care encounter is based upon nine constructs incorporating risk for prostate cancer and patient preferences.
These constructs can provide a framework for the physician–patient discussion of choice and options regarding prostate cancer screening and help the patient to understand the relative contribution of each of these constructs to the ultimate choice of “Yes, you may benefit from being screened with the PSA” vs. “No, you may not benefit from being screened with the PSA.”
Constructs 1–5: Risk for Developing Prostate Cancer
Age
The risk for developing prostate cancer increases with age. The median age at diagnosis is 66 (21). However, screening at age 70 or above is not recommended (5, 6), based upon life expectancy (22).
Family History of Prostate Cancer
A family history of prostate cancer increases the relative risk of prostate cancer in a man with a first-degree relative with prostate cancer to 2.48, with a higher risk in men younger than age 65, or if the man’s brother had prostate cancer, and greater risk if more than one first-degree relative was affected (23, 24).
High vs. Low Risk Racial/Ethnic Group
African-American men have an increased risk of developing prostate cancer compared to Caucasian men, while men from Asian and Native American or Alaskan native backgrounds have a lower risk. Hispanic ethnicity is also associated with a lower risk of developing prostate cancer (21).
History of Previous Digital Rectal Exam
Data from the Prostate Cancer Prevention Trial suggest that the odds ratio for having prostate cancer is 2.47 if a man has an abnormal digital rectal exam (DRE) (25) but the sensitivity of the DRE is low. It is possible that primary physicians will not routinely have performed a DRE for risk stratification.
History of Previous Prostate-Specific Antigen Test
Risk of prostate cancer is predicted by PSA level (25) with recent recommendations suggesting different approaches to men using PSA cut off levels of <1, 1–3, and >3 ng/ml (26).
Constructs 6–9: Patient Self-Reported Health Status/Preferences
Health Status/Comorbidities
We propose that a patient’s self-reported rating of quality of life is incorporated into the decision to offer screening for prostate cancer. While this initial tool does not quantitatively address comorbidities, we propose that clinicians will make an assessment of comorbidities with patients during the screening discussion after reviewing the patient’s answer to this question on the tool.
Importance of Urinary Symptoms
Urinary symptoms are a known side effect of prostate cancer treatment. Up to 14% of men can experience urinary incontinence 5 years after radical prostatectomy for treatment of prostate cancer (27–29). Assessment of the importance of maintaining urinary function should be performed as part of the prostate cancer screening discussion.
Importance of Maintaining Sexual Function
Erectile dysfunction is also a known side effect of radical prostatectomy (27–29) and can affect 50% of men undergoing treatment, with slightly lower rates after radiotherapy (30, 31).
Anxiety about Developing Prostate Cancer
Anxiety regarding prostate cancer may be a major driver in the screening decision (32, 33), and this issue should be addressed prior to making a choice to proceed with screening.
A Brief Tool
While we understand that the decision for prostate cancer screening is complex, we also appreciate the limited time available to discuss this topic in a routine clinical encounter and the proposed tool is meant to begin a discussion that incorporates patient preferences and is not meant to be comprehensive. We propose a tool that can be given to patient within the clinical encounter (Table 1). Questions 1–5 address demographic or past medical history indicators of prostate cancer risk, while Questions 6–9 focus on patient preference. While we do not propose a specific “cut off” score to prompt a decision to screen for prostate cancer, we have suggested assigned points to answer options based upon our available data for each of our constructs.
Discussion
It is extraordinarily difficult to use a tool like this precisely to make a screening decision due to the enormous complexity of the decision. However, we think this tool could be useful as a guide for physicians to identify men who may benefit from further discussion vs. those who may not. Extreme values on this tool may indicate decisions on whether to screen. Scores toward the center values may indicate those who will need further thought and discussion, and possibly extensive shared decision making. Ideally, a physician would introduce this tool during an office visit with a phrase, such as “I would like to make you aware of the option you have to choose to have a screening test to look for prostate cancer. Some men may choose this test while others may not based upon their preferences. I have a few questions you can answer to help think about this option. I can then provide more information for you and we can discuss this at your next visit.” An alternative would be to have a patient fill out the tool prior to an office visit with a plan to discuss the results at the time of the visit. Testing of this tool in busy primary care clinical settings is underway, and the tool will be refined with continued feedback from clinicians and patients.
Author Contributions
AM-H and MK contributed equally to the concept and design of this opinion piece. Both the authors have reviewed the final version of the manuscript being submitted.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Andriole GL, Crawford ED, Grubb RL, Buys SS, Chia D, Church TR, et al. Prostate cancer screening in the randomized prostate, lung, colorectal, and ovarian cancer screening trial: mortality results after 13 years of follow-up. J Natl Cancer Inst (2012) 104(2):125–32. doi:10.1093/jnci/djr500
2. Schröder FH, Hugosson J, Roobol MJ, Tammela TLJ, Zappa M, Nelen V, et al. Screening and prostate cancer mortality: results of the European Randomised Study of Screening for Prostate Cancer (ERSPC) at 13 years of follow-up. Lancet (2014) 384(9959):2027–35. doi:10.1016/S0140-6736(14)60525-0
3. U.S. Preventive Services Task Force. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med (2008) 149(3):185–91. doi:10.7326/0003-4819-149-3-200808050-00008
4. Moyer VA, U.S. Preventive Services Task Force. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med (2012) 157(2):120–34. doi:10.7326/0003-4819-157-2-201207170-00459
5. Qaseem A, Barry MJ, Denberg TD, Owens DK, Shekelle P, Clinical Guidelines Committee of the American College of Physicians. Screening for prostate cancer: a guidance statement from the Clinical Guidelines Committee of the American College of Physicians. Ann Intern Med (2013) 158(10):761–9. doi:10.7326/0003-4819-158-10-201305210-00633
6. Carter HB, Albertsen PC, Barry MJ, Etzioni R, Freedland SJ, Greene KL, et al. Early detection of prostate cancer: AUA guideline. J Urol (2013) 190(2):419–26. doi:10.1016/j.juro.2013.04.119
7. Ilic D, Jammal W, Chiarelli P, Gardiner RA, Hughes S, Stefanovic D, et al. Assessing the effectiveness of decision aids for decision making in prostate cancer testing: a systematic review. Psychooncology (2015) 24:1303–15. doi:10.1002/pon.3815
8. Lewis CL, Adams J, Tai-Seale M, Huang Q, Knowles SB, Nielsen ME, et al. A randomized controlled effectiveness trial for PSA screening decision support interventions in two primary care settings. J Gen Intern Med (2015) 30(6):810–6. doi:10.1007/s11606-015-3214-9
9. Zeliadt SB, Hoffman RM, Etzioni R, Gore JL, Kessler LG, Lin DW. Influence of publication of US and European prostate cancer screening trials on PSA testing practices. J Natl Cancer Inst (2011) 103(6):520–3. doi:10.1093/jnci/djr007
10. Ross JS, Wang R, Long JB, Gross CP, Ma X. Impact of the 2008 US Preventive Services Task Force recommendation to discontinue prostate cancer screening among male Medicare beneficiaries. Arch Intern Med (2012) 172(20):1601–3. doi:10.1001/archinternmed.2012.3726
11. Lee SY, Friderici J, Stefan MS, Rothberg MB. Impact of the 2008 U.S. Preventative Services Task Force recommendation on frequency of prostate-specific antigen screening in older men. J Am Geriatr Soc (2014) 62(10):1912–5. doi:10.1111/jgs.13061
12. Drazer MW, Huo D, Eggener SE. National prostate cancer screening rates after the 2012 US Preventive Services Task Force recommendation discouraging prostate-specific antigen–based screening. J Clin Oncol (2015) 33:2416–23. doi:10.1200/JCO.2015.61.6532
13. Guerra CE, Jacobs SE, Holmes JH, Shea JA. Are physicians discussing prostate cancer screening with their patients and why or why not? A Pilot Study. J Gen Intern Med (2007) 22(7):901–7. doi:10.1007/s11606-007-0142-3
14. Philips GK, Reinier K, Ashikaga T, Luebbers RA. Attitudes and beliefs of primary care physicians regarding prostate and colorectal cancer screening in a rural state. J Cancer Educ (2005) 20(3):167–72. doi:10.1207/s15430154jce2003_11
15. Tang VL, Shi Y, Fung K, Tan J, Espaldon R, Sudore R, et al. Clinician factors associated with prostate-specific antigen screening in older veterans with limited life expectancy. JAMA Intern Med (2016) 176(5):654–61. doi:10.1001/jamainternmed.2016.0695
16. Elstad EA, Sutkowi-Hemstreet A, Sheridan SL, Vu M, Harris R, Reyna VF, et al. Clinicians’ perceptions of the benefits and harms of prostate and colorectal cancer screening. Med Decis Making (2015) 35(4):467–76. doi:10.1177/0272989X15569780
17. Pickles K, Carter SM, Rychetnik L. Doctors’ approaches to PSA testing and overdiagnosis in primary healthcare: a qualitative study. BMJ Open (2015) 5(3):e006367. doi:10.1136/bmjopen-2014-006367
18. Hayat Roshanai A, Nordin K, Berglund G. Factors influencing primary care physicians’ decision to order prostate-specific antigen (PSA) test for men without prostate cancer. Acta Oncol (2013) 52(8):1602–8. doi:10.3109/0284186X.2012.762998
19. Bolen SD, Sage P, Perzynski AT, Stange KC. No moment wasted: the primary-care visit for adults with diabetes and low socio-economic status. Prim Health Care Res Dev (2016) 17(1):18–32. doi:10.1017/S1463423615000134
20. Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med (2012) 27(10):1361–7. doi:10.1007/s11606-012-2077-6
21. Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Altekruse SF, et al. editors. SEER Cancer Statistics Review, 1975–2013. Bethesda, MD: National Cancer Institute (2016). Available from: http://seer.cancer.gov/csr/1975_2013/
22. Social Security Actuarial Life Table. (2013). Available from: https://www.ssa.gov/oact/STATS/table4c6.html
23. Cuzick J, Thorat MA, Andriole G, Brawley OW, Brown PH, Culig Z, et al. Prevention and early detection of prostate cancer. Lancet Oncol (2014) 15(11):e484–92. doi:10.1016/S1470-2045(14)70211-6
24. Kiciński M, Vangronsveld J, Nawrot TS. An epidemiological reappraisal of the familial aggregation of prostate cancer: a meta-analysis. PLoS One (2011) 6(10):e27130. doi:10.1371/journal.pone.0027130
25. Thompson IM, Ankerst DP, Chi C, Goodman PJ, Tangen CM, Lucia MS, et al. Assessing prostate cancer risk: results from the prostate cancer prevention trial. J Natl Cancer Inst (2006) 98(8):529–34. doi:10.1093/jnci/djj131
26. Vickers AJ, Eastham JA, Scardino PT, Lilja H. The memorial Sloan Kettering cancer center recommendations for prostate cancer screening. Urology (2016) 91:12–8. doi:10.1016/j.urology.2015.12.054
27. Stanford JL, Feng Z, Hamilton AS, Gilliland FD, Stephenson RA, Eley JW, et al. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: the Prostate Cancer Outcomes Study. JAMA (2000) 283(3):354–60. doi:10.1001/jama.283.3.354
28. Hoffman RM, Barry MJ, Stanford JL, Hamilton AS, Hunt WC, Collins MM. Health outcomes in older men with localized prostate cancer: results from the Prostate Cancer Outcomes Study. Am J Med (2006) 119(5):418–25. doi:10.1016/j.amjmed.2005.06.072
29. Penson DF, McLerran D, Feng Z, Li L, Albertsen PC, Gilliland FD, et al. 5-year urinary and sexual outcomes after radical prostatectomy: results from the prostate cancer outcomes study. J Urol (2005) 173(5):1701–5. doi:10.1097/01.ju.0000154637.38262.3a
30. Potosky AL, Legler J, Albertsen PC, Stanford JL, Gilliland FD, Hamilton AS, et al. Health outcomes after prostatectomy or radiotherapy for prostate cancer: results from the Prostate Cancer Outcomes Study. J Natl Cancer Inst (2000) 92(19):1582–92. doi:10.1093/jnci/92.19.1582
31. Hamilton AS, Stanford JL, Gilliland FD, Albertsen PC, Stephenson RA, Hoffman RM, et al. Health outcomes after external-beam radiation therapy for clinically localized prostate cancer: results from the Prostate Cancer Outcomes Study. J Clin Oncol (2001) 19(9):2517–26. doi:10.1200/jco.2001.19.9.2517
32. Dale W, Bilir P, Han M, Meltzer D. The role of anxiety in prostate carcinoma. Cancer (2005) 104(3):467–78. doi:10.1002/cncr.21198
Keywords: shared decision making, cancer screening, prostate cancer diagnosis, primary health care, screening tools
Citation: Misra-Hebert AD and Kattan MW (2016) Prostate Cancer Screening: A Brief Tool to Incorporate Patient Preferences in a Clinical Encounter. Front. Oncol. 6:235. doi: 10.3389/fonc.2016.00235
Received: 12 July 2016; Accepted: 21 October 2016;
Published: 04 November 2016
Edited by:
Scott T. Tagawa, Weill Cornell Medical College, USAReviewed by:
Albert James Chang, University of California San Francisco, USAWon Kim, University of California San Francisco, USA
Copyright: © 2016 Misra-Hebert and Kattan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anita D. Misra-Hebert, misraa@ccf.org
 Anita D. Misra-Hebert
Anita D. Misra-Hebert Michael W. Kattan
Michael W. Kattan