Pediatric Flatfeet—A Disease Entity That Demands Greater Attention and Treatment
- 1Indian Valley Podiatry Associates, PC, Souderton, PA, United States
- 2Hospital de Niños Victor J. Vilela, Rosario, Argentina
Background: Pediatric flatfoot is a common deformity. Unfortunately, the common opinion has been that most children with this faulty foot structure will simply out-grow it, despite no radiographic evidence to support this claim. Every step on a deformed foot leads to excessive tissue strain and further joint damage. Many forms of conservative and surgical treatments have been offered. This study was aimed at investigating the effectiveness of non-surgical and surgical treatment options.
Main Text: faulty-foot structure is the leading cause of many secondary orthopedic deformities. A wide range of treatments for pediatric flatfeet have been recommended from the “do-nothing” approach, observation, to irreversible reconstructive surgery. Most forms of conservative care lack evidence of osseous realignment and stability. A conservative surgical option of extra-osseous talotarsal joint stabilization provides patients an effective form of treatment without the complications associated with other irreversible surgical procedures.
Conclusion: Pediatric flatfeet should not be ignored or downplayed. The sooner effective treatment is prescribed, the less damage will occur to other parts of the body. When possible, a more conservative corrective procedure should be performed prior to irreversible, joint destructive options.
Pediatric flatfeet are a very common concern for parents and one of the most frequent presenting complaints to a pediatric practice (1). Unfortunately, parents are told that it isn't necessary to treat and to simply ignore this foot deformity. One author even concluded “the best treatment is simply taking enough time to convince the family that no treatment is necessary” (2). Other authors suggest that surgical intervention is rarely necessary, that there is very little evidence for the efficacy of non-surgical care but that non-surgical care should still be considered (2–4). While a child's foot shape and size change over the first several years of life, there is a recognizable difference between normal development and pathology at any age. Foot and ankle specialists know that sooner or later, flat and misaligned feet will slowly lead to other pathologies within the foot and ankle and proximal structures (5).
Walking is one of the most common unconscious functions of our body. We are told to take 10,000 steps a day, to keep healthy (6). The stability and alignment of the foot is very important because the foot is the foundation to the upright body. Failure to identify and treat foot and ankle instability and misalignment will lead to long-term tissue pathology. Foot misalignment has been shown to reduce propulsive phase push off muscle power by 35%, which seems to be an obvious gait inefficiency (7). Tissue strain leads to pain, increased deformity, and eventually decreased activity level. The body's metabolic rate decreases as a result which leads to other health risks such as obesity, diabetes, hypertension, and heart disease (8, 9).
The goal in treating any disease is early identification and intervention with a method proven to achieve the desired outcome that is measurable and makes sense. There is a long evolution in the internal correction of this faulty-foot alignment disease. The use of extra-articular realignment and stabilization techniques have stood the test of time. The medical necessity and evidence basis of extra-osseous talotarsal stabilization has been established (10). The time has come to embrace this minimally invasive, reversible solution as an early intervention to pediatric flatfeet.
Hindfoot Alignment and Biomechanics
The talus is an osseous extension of the leg that articulates distally with the hindfoot bones. The distal and plantar articular facets of the talus interact with the calcaneus and navicular to form the talotarsal joint (TTJ). The large posterior talocalcaneal joint is responsible to accept a vertical force as much as 80% at heel strike that reduces to slightly greater than 50% of the weightbearing forces at mid-stance (11, 12). These forces occur posterior to the posterior aspect of the sinus tarsi (Figure 1A). The remaining force acts distal to the anterior aspect of the sinus tarsi (Figure 1B). The balance of the forces acting within the TTJ is responsible for an efficient hindfoot machine by performing the essential function of converting vertical force into a horizontal force.
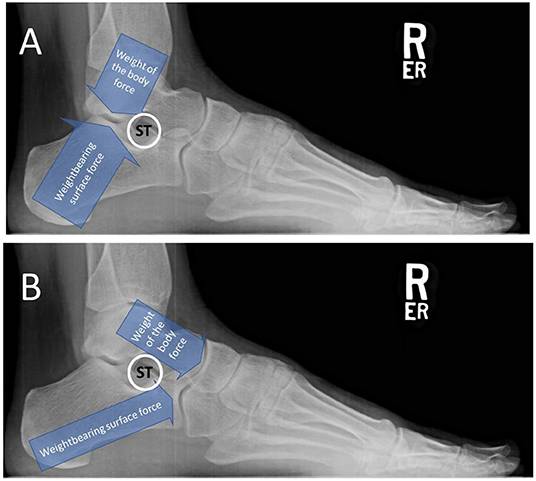
Figure 1. Weightbearing lateral foot radiograph of a foot in resting stance position showing normal talotarsal joint forces. (A) Forces acting posterior to the sinus tarsi at heel strike. The sinus tarsi is labeled as ST. (B) Forces acting anterior/distal to the sinus tarsi as the plantar surface of the foot makes contact with the weightbearing surface. Sinus tarsi should remain open.
The TTJ allows for the locking and unlocking of the joints within the medial column of the foot during weightbearing. TTJ pronation unlocks the joints which provides the adaptability of an uneven weightbearing surface at the beginning of the full, plantar foot contact portion of the gait cycle. The TTJ should resupinate at approximately 1/4th to 1/3rd of the full-foot contact (Figure 2). This strengthens the foot structure as it prepares for heel lift and forward foot propulsion.
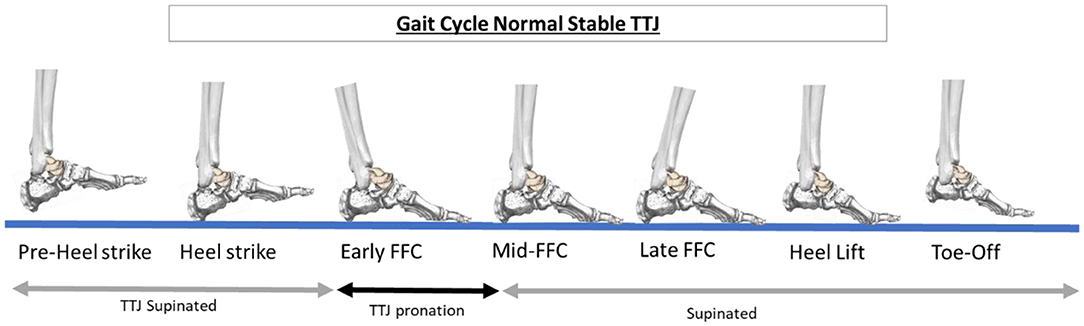
Figure 2. Schematic showing the portions of the gait cycle with a normal stable talotarsal joint (TTJ). It also shows when the TTJ should be in a supinated or pronated alignment. “FFC” is full plantar foot contact.
The primary component of a flexible “flatfoot” is the loss of stability and alignment of the TTJ (Figure 3) (13). A flatfoot cannot occur unless the talus and calcaneus are malaligned. Instability of the TTJ results in the pathologic redistribution of the weightbearing forces acting within the hind-, mid-, and forefoot. The forces are non-existent during the swing phase and excessive during the weightbearing stance phase of the gait cycle. TTJ displacement leads to osseous malalignment, increased strain to ligaments, and increased muscle-tendon contraction until the foot has left the weightbearing surface (14). This cascade of excessive tissue loading and unloading of forces occurs with every step taken.
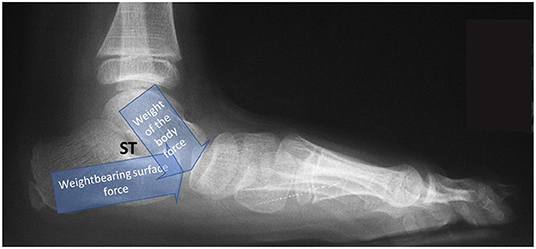
Figure 3. Weightbearing lateral foot radiograph of a foot in resting stance position showing partial dislocation of the talotarsal joint illustrating joint forces. Loss of TTJ alignment occurs at the initial stage of full plantar foot contact. Sinus tarsi is obliterated. Excessive forces are thrust on the mid-foot.
A visible sign of TTJ misalignment is the lowering of the medial arch of the foot, contributing to a flatfoot. That is because the joints of the medial arch are unlocked longer than they should during the weightbearing portion of the gait cycle leading to excessive pronation (Figure 4) (15). It is navicular drop/sag that leads to the lowering of the medial arch of the foot (16, 17). The navicular is forced plantar-medially because of subtalar joint (STJ) instability—specifically the talus partially dislocating on the calcaneus. Realignment of the STJ shows the restoration of the elevation of the navicular (Figure 5).
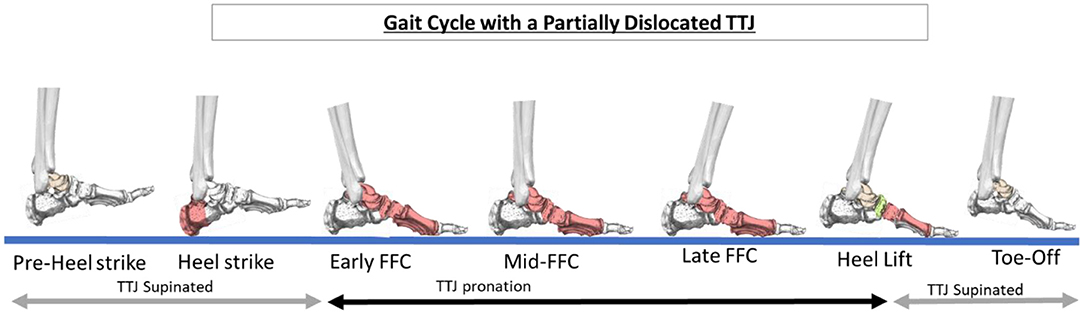
Figure 4. Schematic showing the portions of the gait cycle with an unstable, partially dislocated talotarsal joint (TTJ). The TTJ remains in a pronated, unlocked position longer than normal. “FFC” is full plantar foot contact. The joints and soft tissues will be forced to compensate for the excessive forces acting on the medial column of the foot.
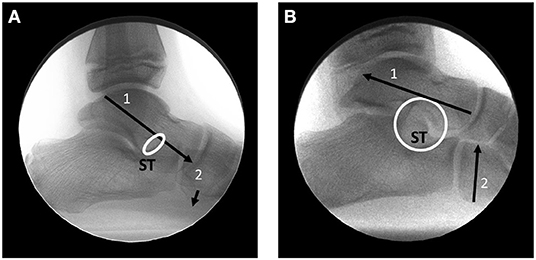
Figure 5. Lateral weight bearing fluoroscopic radiographs. (A) Relaxed stance position. The talus has partially dislocated on the calcaneus (1). The sinus tarsi (ST) is obliterated and the navicular has dropped (2). (B) The same foot with the articular facets of the talus repositioned on the calcaneus (1). Sinus tarsi (ST) is re-opened and the navicular is elevated (2).
Some feet may also exhibit a calcaneal valgus, but this is not always present with TTJ instability (18, 19). Heel valgus occurs as a form of compensation from excessive internal talar rotation and plantar flexion (Figure 6) (20). This is a very important consideration because surgeons may choose to cut and shift the heel bone to a more “aligned” position, but the excessive talar instability will still be present, unaffected by this form of treatment.
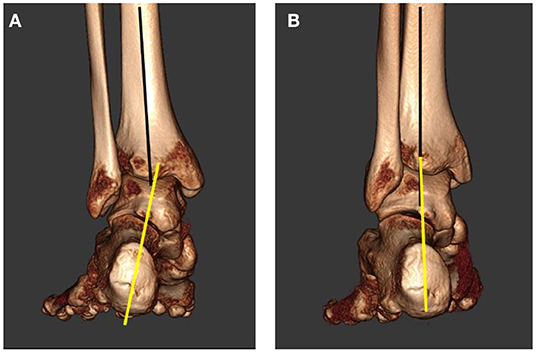
Figure 6. Posterior 3-dimensional weightbearing computed tomography of the hindfoot. (A) Hindfoot is in relaxed-stance position, notice the heel valgus (yellow line). (B) Same foot with the subtalar joint placed into neutral alignment, notice the rectus heel alignment.
Diagnosis of a Flatfoot
The diagnosis of a flatfoot has historically been determined by many different factors. This could be one of the many reasons why there is so much confusion in the diagnosis and subsequentially, the treatment of flatfeet. There are subjective, clinical observations that must be confirmed by objective, standardized, and validated radiographic angular measurements. A major issue with clinical observations, such as arch height, heel eversion, and plantar foot prints, is that they are subjective and poorly reproducible from examiner to examiner. These observations are unable to pin-point a specific anatomic consideration, such as internal osseous malalignment.
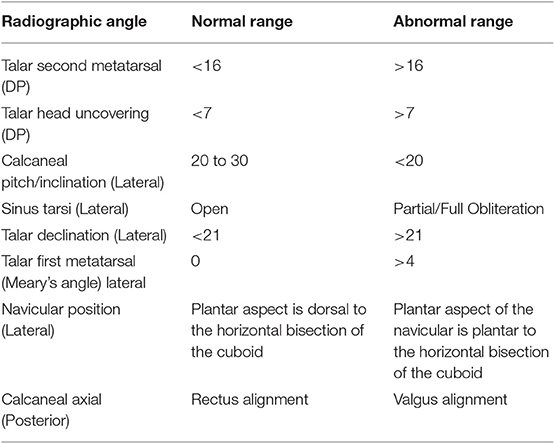
Resting- or relaxed-stance position weightbearing radiographs should be the gold standard in the diagnosis of a flatfoot. Osseous malalignment leads to faulty foot structure and the only way to visualize foot bone alignment is with radiographs taken while the individual is standing on their feet. There are specific validated radiographic angles that show normal or abnormal alignment of the osseous foot structures. The dorsoplantar (DP) view measurements include the talar second metatarsal along with the talar navicular head uncovering. Key features on the lateral radiograph include the opening or obliteration of the sinus tarsi, talar declination angle, talar first metatarsal angle, calcaneal inclination or pitch angle, and navicular position (Table 1).
The diagnosis of a “flatfoot” is too generic. It does not give an accurate indication of what is “broken.” The specific “broken” components leading to the overall less-than-aligned foot should be individually described to patients. A recurrent talotarsal joint dislocation (RTTJD) is the primary deformity of a flexible “flatfoot.” RTTJD indicates that there is a condition where the TTJ has lost its normal alignment during weightbearing throughout the gait cycle. RTTJD is a “flexible” verse rigid pathology and important in determining the best form of treatment. Realignment of the TTJ results in an increase in arch height, re-opening of the sinus tarsi, normalization of joint forces, increased navicular height, normalization of the cyma line, rectus calcaneus, and possibly normalization of the calcaneal inclination angle.
Some clinicians will assume a foot to be “normal” unless there is complete loss of the medial arch (21). RTTJD can exist with a “normal” appearing arch, due to a normal calcaneal inclination angle and a navicular that does not drop, but it is still considered a pathological phenomenon. A rigid, non-reducible flatfoot still leads to a prolonged degree of pronation during the gait cycle. All of these factors lead to further confusion in the diagnosis abnormal foot alignment. Other disease processes such as a tarsal coalition must also be ruled out.
The Myth of “Autocorrection”
One of the reasons why many pediatricians downplay the severity of this orthopedic deformity is that there are claims the flatfoot self-repairs. The evidence basis of these claims is based on a cross-sectional epidemiologic study by determining the heel-to-arch width ratio in two different age groups (22). This was not a longitudinal study over an 8-year period. The research showed that 97% of children 2 years or younger had a flatfoot according to the foot-print ratio and that the ratio decreased to 4% when measured at a separate group of children 10 years old. The assumption was that the majority of flatfeet would resolve by age 10. This data only evaluated the plantar fat pad of the medial arch, it did not take into consideration the osseous alignment. The results of the comparison lack the necessary data to conclude auto-correction of a faulty foot structure.
How could a misaligned, unstable foot become internally realigned and stabilized when excessive abnormal forces are acting on those structures with every step taken? Osseous malaligned structures do not realign. Juvenile hallux abductovalgus deformities, for example, become progressively worse, not better (23). There are no long-term follow up radiographic studies that document osseous realignment of a pediatric flatfoot (24). The non-surgical treatment of flatfeet has been studied and shown to be ineffective in addressing the osseous misaligned, so how could anyone expect the feet to auto-heal? There is documentation that adult flatfeet continue to progressively get worse (25, 26). Those asymptomatic pediatric flatfeet eventually lead to a symptomatic adult flatfoot.
Outcome if not Treated
If you don't fix what is broken, it remains broken. If forces continue to act excessively on tissues, those tissues will create a defense mechanism in an attempt to handle those excessive forces as described by Wolff and Davis (27, 28). Eventually, a critical threshold is reached when the tissues can no longer compensate, at that point tissue failure occurs. Subsequentially, joint and other tissues will be forced to compensate for the loss of the primary stabilizing tissues. Excessive force and pressure within the joint leads to an inflammatory reaction. If those repetitive excessive forces remain unchecked, chronic inflammation will result leading to arthritis and joint destruction.
Hindfoot joint displacement has been found to be the most common finding associated with the onset of symptoms (29). Hyperpronation is named at the leading etiologic factor to many chronic foot pathologies such as plantar fasciopathy (30–32), posterior tibial tendon insufficiency (33–37), first ray deformities (38–40), hallux limitus (41, 42), tarsal tunnel syndrome (43, 44), and posterior tibial tendon dysfunction (45, 46). Proximal manifestations attributed to hindfoot misalignment are ankle joint pathology (47, 48), growing pains, medial tibial stress syndrome/shin splints (49–51), knee pathology (52–57), hip pathology (58, 59), pelvic tilt (60), and even back misalignment (61, 62).
There are additional considerations that must be also factored into this disease process. Children are taken to a pediatrician or foot care specialist and are told they have a musculoskeletal deformity, they are deformed. The physician is tries to “convince the parent” that there is no need for treatment? This will create a psychological disturbance in the child's mind. There is also the issue of decreased physical activity in sports. Competitive sports are a big part of lower and upper school. Children who are less competitive are looked down upon against their more athletic classmates.
The health-related quality of life is significantly impaired in children with flexible flatfoot (63). Children with flexible flatfeet have an increased body mass index (BMI) compared to children with normal appearing feet (64). One of the primary treatments of obesity is to increase the metabolism to burn off those calories (65). Walking on misaligned feet is less-than-ideal as muscles will have to work harder to lift the inner arch and sooner rather than later, pain will ensue stopping the weightbearing activity (66, 67).
Primary Goals of Treatment
The successful treatment of flatfoot must take into account the underlying pathology to optimize outcomes. We must be mindful of the three principles of orthopedic treatment. That which is crooked, make straight. That which is unstable, make stable. Joint preservation should be attempted over joint-destructive measures, when possible. The primary deformity of a flatfoot is RTTJD so the goal of treatment should be aimed at realigning the articular facets of the TTJ and to maintain that alignment, while still allowing a natural range of motion. When considering the various treatment options for flatfeet, we must ask the question, does that treatment make sense? Is it capable of accomplishing the primary goals of treatment? If it doesn't meet the standards, then should it be considered below the standard of care to offer that form of treatment?
Treatment in the Absence of Pain
Much of the published literature on pediatric flatfoot advises that treatment is only necessary when pain is present. This goes against the principles of medical ethics. Should we wait until a diabetic patient falls into a hyperglycemic coma to begin care? Should we wait until someone has their first heart attack to begin treatment? Of course not. The same is true when considering the treatment of malaligned feet. Sooner or later certain tissues will no longer be able to handle the excessive forces and that tissue will partially rupture. If no intervention is provided to decrease the strain on the tissue it will eventually result in a complete rupture. If there is an imbalance of force acting within a joint, eventually those excessive forces will have a negative impact on the cartilage until the cartilage is damaged. If the forces aren't normalized, that damage becomes chronic eventually leading to irreversible changes. It makes sense therefore to eliminate the tissue strain to prevent the partial rupture, to balance the joint facets to prevent arthritis, and to improve the biomechanics of the foot.
It is also important to make a connection between pain elsewhere in the body and other symptoms related to a faulty foot structure. It is true that many pediatric patients, or even adult patients, with flat feet have no pain or symptoms within their feet. However, those symptoms can show up as pain to other parts of the body as previously discussed, i.e., growing pains, shin splints, knee pain, hip pain, back pain, and other functional symptoms. Ultimately, the decision on accepting a treatment has to be made by the parents or legal guardian.
Forms of Non-surgical Treatment
There have been many non-surgical forms of treatments prescribed for pediatric flatfeet including activity modification, orthopedic shoes, foot orthoses, stretching and strengthening exercises, and non-steroidal anti-inflammatory medications.
Observation
The most common form of treatment is simply to ignore this orthopedic disease as a normal variant. This “non-treatment” should be considered below the standard of care as multiple studies have identified flat/over-pronating feet are a significant contributing factor to the development and progression of pathologies within the foot, knee, hip, and back pain (47, 50, 53, 62, 68–70). Tens of millions of steps taken on malaligned feet will eventually take their toll.
Physical Therapy/Muscle Strengthening
Muscle strengthening exercises have been strongly recommended. There is very limited, if any, scientific basis for this form of treatment. Does it even make sense? The strong muscles of the lower extremity are over-powered by the collapse of the medial arch. It has been shown that the pronatory muscles are already contracting to lift the arch and assist in re-supinating the foot (37, 71). Another study found that the posterior tibial tendon is incapable of fully accommodating hindfoot misalignment (72). This is why there are no long-term studies showing a positive effect or correction to a flatfoot and that this is a less-than-ideal long-term solution.
Arch Supports/Foot Orthoses
Use of arch supports has long been advocated even though there is little to no evidence basis (73, 74). There are very short-term positive results in reduction of symptoms but longer follow up is lacking. Staheli concluded “Treatment of children with physiologic flatfoot with orthoses or shoe modifications not only is ineffective but is uncomfortable and embarrassing for the child and is associated with lowered self-esteem in adult life” (4). A prospective study was undertaken to determine whether flexible flatfoot in children can be influenced by corrective shoes and inserts (75). They concluded “that wearing corrective shoes or inserts for 3 years does not influence the course of flexible flatfoot in children.” Many other studies have discovered similar inability of custom foot orthotics or specialized shoes to be ineffective in the treatment of pediatric flatfoot (24, 76). Furthermore, other studies have shown that there is no radiologic improvement with the use of arch supports/custom foot orthotics (77). Arch supports/foot orthoses should be considered a subtherapeutic form of treatment.
Non-Conservative Surgical Treatment
There are advocated surgical procedures to realign and stabilize the hind- and mid-foot. These osseous procedures such as a lateral calcaneal lengthening, opening cuneiform osteotomy, navicular lifting procedures, can be associated with many risks and potential complications such as sural nerve injury, surgical wound dehiscence, under or over-correction, and graft subsidence (78). Due to the invasiveness of these surgical options, it was recommended to delay this form of treatment after failure of any other potential option that can accomplish the treatment goals.
Conservative Surgical Treatment
The insertion of a stent into the sinus tarsi has been advocated and performed by foot and ankle surgeons for many decades (79–82). This procedure was born out the necessity to achieve the desired results of foot realignment without sacrificing joint structures. Over the past many decades many different designs of implants and materials have evolved into three types of methods. Intra-osseous talotarsal stabilization (Figure 7A) involves the partial insertion of a screw type implant into either the floor of the sinus tarsi of the calcaneus (83, 84), or partially into the lateral process of the talus (85). This method is a true joint blocking—arthroereisis. Many surgeons simply use a rather inexpensive large orthopedic screw. This technique is limited to patients 12 to 18 years of age. Typically, the screw is removed within 18 months of insertion. Correction is achieved while the screw is in situ but the long-term results after screw removal are unknown.
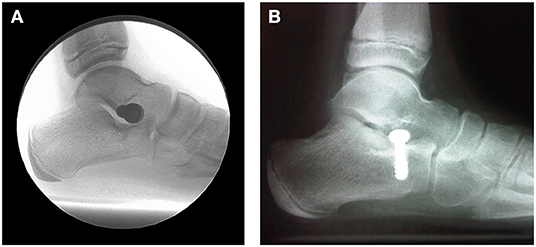
Figure 7. (A) Lateral weightbearing radiograph of an extra-osseous sinus tarsi implant. (B) Intra-osseous screw acting to stabilize the talotarsal joint.
Extra-osseous sinus tarsi stents (EOTTS) (Figure 7B) are the second type of devices inserted to maintain the alignment and stability of the TTJ. During weightbearing the anterior process of the talus pushes against the implant until the anterioplantar surface of the implant comes into contact with the posterior surface of the anterior floor of the sinus tarsi, formed by the calcaneus. These devices can correct in both the transverse and sagittal, and therefore frontal planes (Figure 8).
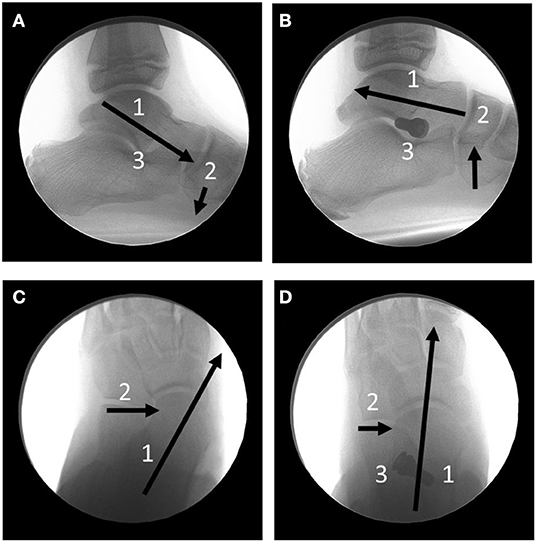
Figure 8. Full Weightbearing, relaxed stance position fluoroscopic radiographs. (A) Lateral image showing the anterioplantar parital dislocation of the talus (1) on the calcaneus. The navicular (2) is forced plantarly. The sinus tarsi (3) is obliterated. (B) The same foot post-extraosseous talotarsal stabilization. Notice the realignment of the talus on the calcaneus (1) and elevated navicular (2). (3) is the HyProCure (GraMedica, Michigan, USA) sinus tarsi implant. (C) Dorsoplantar view of the hindfoot. The talus (1) is medially and anteriorly displaced on the calcaneus (2). (D) The same foot post-extraosseous talotarsal stabilization. Notice the lateralization of the talus (1) and reduction of the anteriomedial displacement of the talus (2). (3) The HyProCure implant.
There are numerous studies that have provided the evidence basis, safety and effectiveness of this minimally invasive joint sparing procedure. There is evidence of radiographic normalization of osseous realignment (86, 87), restoration of navicular height/position (88), maintenance of arch height (89, 90), restoration of joint congruity (3), rebalancing of subtalar joint forces (91), decreased strain to the plantar fascia (92), posterior tibial nerve (93), and tendon (94), improved function and pain scores (95), improved ankle joint alignment (96), return to sports activity, and improved emotional status (97). Pediatric patients report a high degrees of satisfaction, and their quality of life was improved and not compromised by the procedure (98, 99).
Complication of extraosseous sinus tarsi implants include pain within the sinus tarsi area, device extrusion/displacement, and under/over-correction. These less-than-ideal situation are self-resolving once the procedure is revised or with permanent removal of the implant. There have been no long-term complications as a result of the stent being in the sinus tarsi. A benefit-risk analysis will show the benefits far exceeds any potential risks. Other less-conservative surgical procedures can still be performed.
Conclusion
Pediatric flatfoot is a progressive mechanical disease process that is linked to many other musculoskeletal, metabolic, and physiological pathologies. There is no supportive evidence that osseous misaligned structures will auto-correct. These misaligned feet do not get better, they progressively worsen. Failure to address this disease process will lead to deleterious effects to many parts of the body and to one's physical and mental health. Foot pain may not be present in most people with flatfeet however, the symptoms of flatfeet can appear as knee, hip, and back pain. The algorithm for the treatment of flatfeet must begin with measures proven to realign and stabilize the malaligned osseous structures, i.e., the talotarsal joint, while still allowing a natural range of motion, without compromising adjacent joint structures.
We must acknowledge that there is no evidence of auto-correction of pediatric flatfeet. That this orthopedic disease will lead to other orthopedic, metabolic, and even mental distress if not properly addressed. Conservative options are proven to be ineffective in the realignment of the osseous pathologies. Traditional osteotomies and arthrodesis procedures have many known complications and risks. EOTTS is superior option to external measures in realigning and stabilizing the TTJ. EOTTS should be considered as a minimally invasive, conservative surgical option prior to irreversible osseous surgery, when indicated. EOTTS can be used in combination with other treatment options.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest
PB has no financial interest in Gramedica, but has been reimbursed for travel expenses to speak at seminars (as all speakers are), but received no honoraria while discussing the type of procedure performed in the article. MJ is listed as a clinical instructor for the Graham International Implant Institute.
Reviewer MG is the founder and president of the Graham International Implant Institute, and the company GraMedica that produces the HyProCure® implant, which is used to treat bone misalignment in flat feet.
References
1. Luhmann SJ, Rich MM, Schoenecker PL. Painful idiopathic rigid flatfoot in children and adolescents. Foot Ankle Int. (2000) 21:59–66. doi: 10.1177/107110070002100111
2. Sullivan JA. Pediatric flatfoot: evaluation and management. J Am Acad Orthop Surg. (1999) 7:44–53. doi: 10.5435/00124635-199901000-00005
3. Cappello TMD, Song KMMD. Determining treatment of flatfeet in children. Curr Opin Pediatr. (1998) 10:77–81. doi: 10.1097/00008480-199802000-00016
4. Staheli L. Planovalgus foot deformity. Current Status. J Am Podiatr Med Assoc. (1999) 89:94–9. doi: 10.7547/87507315-89-2-94
5. Fabry G. Clinical practice. Static, axial, and rotational deformities of the lower extremity in children. Eur J Pediatr. (2010) 169:529–34. doi: 10.1007/s00431-009-1122-x
6. Igarashi Y, Akazawa N, Maeda S. The required step count for a reduction in blood pressure: a systematic review and meta-analysis. J Hum Hypertens. (2018) 32:814–24. doi: 10.1038/s41371-018-0100-z
7. Hösl M, Böhm H, Multerer C, Döderlein L. Does excessive flatfoot deformity affect function? A comparison between symptomatic and asymptomatic flatfeet using the Oxford Foot Model. Gait Posture. (2014) 39:23–8. doi: 10.1016/j.gaitpost.2013.05.017
8. Lavie CJ, Ozemek C, Carbone S, Katzmarzyk PT, Blair SN. Sedentary behavior, exercise, and cardiovascular health. Circ Res. (2019) 124:799–815. doi: 10.1161/CIRCRESAHA.118.312669
9. Bowden Davies KA, Sprung VS, Norman JA, Thompson A, Mitchell KL, Halford JCG, et al. Short-term decreased physical activity with increased sedentary behaviour causes metabolic derangements and altered body composition: effects in individuals with and without a first-degree relative with type 2 diabetes. Diabetologia. (2018) 61:1282–94. doi: 10.1007/s00125-018-4603-5
10. Graham ME. Medical necessity and evidence basis for extra-osseous talotarsal joint stabilization. Clin Surg. (2017) 2:1–8.
11. Hutton WC, Dehanendran M. The mechanics of normal and hallux valgus feet-A quantitative study. Clin Ortho. (1981) 157:7–13. doi: 10.1097/00003086-198106000-00004
12. Graham ME, Parikh R, Goel V, Mhatre D, Matyas A. Stabilization of joint forces of the subtalar complex via HyProCure sinus tarsi stent. J Am Podiatr Med Assoc. (2011) 101:390–9. doi: 10.7547/1010390
13. Graham ME. Congenital talotarsal joint displacement and pes planovalgus: evaluation, conservative management, and surgical management. Clin Podiatr Med Surg. (2013) 30:567–81. doi: 10.1016/j.cpm.2013.07.001
14. Resende RA, Pinheiro LSP, Ocarino JM. Effects of foot pronation on the lower limb sagittal plane biomechanics during gait. Gait Posture. (2019) 68:130–5. doi: 10.1016/j.gaitpost.2018.10.025
15. Prachgosin T, Chong DY, Leelasamran W, Smithmaitrie P, Chatpun S. Medial longitudinal arch biomechanics evaluation during gait in subjects with flexible flatfoot. Acta Bioeng Biomech. (2015) 17:121–30.
16. Snook AG. The relationship between excessive pronation as measured by navicular drop and isokinetic strength of the ankle musculature. Foot Ankle Int. (2001) 22:234–40. doi: 10.1177/107110070102200311
17. Moraleda L, Mubarak SJ. Flexible flatfoot: differences in the relative alignment of each segment of the foot between symptomatic and asymptomatic patients. J Pediatr Orthop. (2011) 31:421–8. doi: 10.1097/BPO.0b013e31821723ce
18. de Cesar Netto C, Kunas GC, Soukup D, Marinescu A, Ellis SJ. Correlation of clinical evaluation and radiographic hindfoot alignment in stage II adult-acquired flatfoot deformity. Foot Ankle Int. (2018) 39:771–79. doi: 10.1177/1071100718762113
19. Cody EA, Williamson ER, Burket JC, Deland JT, Ellis SJ. Correlation of talar anatomy and subtalar joint alignment on weightbearing computed tomography with radiographic flatfoot parameters. Foot Ankle Int. (2016) 37:874–81. doi: 10.1177/1071100716646629
20. Tarissi N, Vallée A, Dujardin F, Duparc F, Roussignol X. Reducible valgus flat-foot: assessment of posterior subtalar joint surface displacement by posterior arthroscopy during sinus tarsi expansion screwing. Orthop Traumatol Surg Res. (2014) 100(8 Suppl.):S395–9. doi: 10.1016/j.otsr.2014.09.004
21. Elmoatasem EM, Eid MA. Assessment of the medial longitudinal arch in children with flexible pes planus by plantar pressure mapping. Acta Orthop Belg. (2016) 82:737–44.
23. Kilmartin TE, Barrington RL, Wallace WA. A controlled prospective trial of a foot orthosis for juvenile hallux valgus. J Bone Joint Surg Br. (1994) 76:210–4. doi: 10.1302/0301-620X.76B2.8113278
24. Kanatli U, Aktas E, Yetkin H. Do corrective shoes improve the development of the medial longitudinal arch in children with flexible flat feet? J Orthop Sci. (2016) 21:662–6. doi: 10.1016/j.jos.2016.04.014
25. Wong DW, Wang Y, Leung AK, Yang M, Zhang M. Finite element simulation on posterior tibial tendinopathy: load transfer alteration and implications to the onset of pes planus. Clin Biomech. (2018) 51:10–6. doi: 10.1016/j.clinbiomech.2017.11.001
26. Ling SK, Lui TH. Posterior tibial tendon dysfunction: an overview. Open Orthop J. (2017) 31:714–23. doi: 10.2174/1874325001711010714
27. Wolff J. The classic: on the inner architecture of bones and its importance for bone growth. 1870. Clin Orthop Relat Res. (2010) 468:1056–65. doi: 10.1007/s11999-010-1239-2
29. Yan GS, Yang Z, Lu M, Zhang JL, Zhu ZH, Guo Y. Relationship between symptoms and weight-bearing radiographic parameters of idiopathic flexible flatfoot in children. Chin Med J. (2013) 126:2029–33.
30. Kwong PK, Kay D, Vorner RT, White MW. Plantar fasciitis. Mechanics and pathomechanics of treatment. Clin Sports Med. (1988) 7:119–26.
31. Prichasuk S, Subhadrabandhu T. The relationship of pes planus and calcaneal spur to plantar heel pain. Clin Orthop Relat Res. (1994) 306:192–6.
32. Wearing SC, Smeathers JE, Urry SR, Hennig EM, Hills AP. The pathomechanics of plantar fasciitis. Sports Med. (2006) 36:585–611. doi: 10.2165/00007256-200636070-00004
33. Zhang TJ, Wang Y, Lin SJ, Ma X. Correlation between hindfoot joint three-dimensional kinematics and the changes of the medial arch angle in stage II posterior tibial tendon dysfunction flatfoot. Clin Biomech. (2015) 30:153–8. doi: 10.1016/j.clinbiomech.2014.12.007
34. Zhang Y, Xu J, Wang X, Huand J, Zhang C, Chen L, et al. An in vivo study of hindfoot 3D kinetics in stage II posterior tibial tendon dysfunction (PTTD) flatfoot based on weight-bearing CT scan. Bone Joint Res. (2013) 2:255–63. doi: 10.1302/2046-3758.212.2000220
35. Rabbito M, Pohl MB, Humble N, Ferber R. Biomechanical and clinical factors related to stage I posterior tibial tendon dysfunction. J Orthop Sports Phys Ther. (2011) 41:776–84. doi: 10.2519/jospt.2011.3545
36. Arai K, Ringleb SJ, Zhao KD, Berglund LJ, Kitaoka HB, Kaufman KR. The effect of flatfoot deformity and tendon loading on the work of friction measured in the posterior tibial tendon. Clin Biomech. (2007) 22:592–8. doi: 10.1016/j.clinbiomech.2007.01.011
37. Kamiya T, Uchiyama E, Wantanabe K, Suzuki D, Fujimiua M, Yamashita T. Dynamic effect of the tibialis posterior muscle on the arch of the foot during cyclic axial loading. Clin Biomech. (2012) 27:962–6. doi: 10.1016/j.clinbiomech.2012.06.006
38. Kalen V, Brecher A. Relationship between adolescent bunions and flatfeet. Foot Ankle Int. (1988) 8:331–6. doi: 10.1177/107110078800800609
39. Eustace S, Byrne JO, Beausang O, Codd M, Stack J, Stephens MM. Hallux valgus, first metatarsal pronation and collapse of the medial longitudinal arch–a radiological correlation. Skeletal Radiol. (1994) 23:191–4. doi: 10.1007/BF00197458
40. Ross FD. The relationship of abnormal foot pronation to hallux abducto valgus—a pilot study. Prosthet Orthot Int. (1986) 10:72–8.
41. Vallotton J. Functional hallux limitus (Fhl): a new explanation for overuse pathologies. Rev Mew Suisse. (2014) 10:2333–7.
42. Gatt A, Mifsud T, Chockalingam N. Severity of pronation and classification of first metatarsophalangeal joint dorsiflexion increases the validity of the Hubscher Manoeuvere for the diagnosis of functional hallux limitus. Foot. (2014) 24:62–5. doi: 10.1016/j.foot.2014.03.001
43. Bracilovic A, Nihal A, Houston VL, Beattie AC, Rosenberg ZS, Trepman E. Effect of foot and ankle position on tarsal tunnel compartment volume. Foot Ankle Int. (2006) 27:431–7. doi: 10.1177/107110070602700608
44. Alshami AM, Babri AS, Souvlis T, Coppieters MW. Strain in the tibial and plantar nerves with foot and ankle movements and the influence of adjacent joint positions. J Appl Biomech. (2008) 24:368–76. doi: 10.1123/jab.24.4.368
45. Blackwood S, Gossett L. Hallux valgus/medial column instability and their relationship with posterior tibial tendon dysfunction. Foot Ankle Clin. (2018) 23:297–313. doi: 10.1016/j.fcl.2018.02.003
46. Guelfi M, Pantalone A, Mirapeix RM, Vanni D, Usuelli FG, Guelfi M, et al. Anatomy, pathophysiology and classification of posterior tibial tendon dysfunction. Eur Rev Med Pharmacol Sci. (2017) 21:13–9.
47. Friedman MA, Draganich LF, Toolan B, Brage ME. The effects of adult acquired flatfoot deformity on tibiotalar joint contact characteristics. Foot Ankle Int. (2001) 22:241–6. doi: 10.1177/107110070102200312
48. Tochigi Y. Effect of arch supports on ankle-subtalar complex instability: a biomechanical experimental study. Foot Ankle Int. (2003) 24:634–9. doi: 10.1177/107110070302400811
49. Plisky MS, Rauh MJ, Heiderscheit B, Underwood FB, Tank RT. Medial tibial stress syndrome in high school cross-country runners: incidence and risk factors. J Orthop Sports Phys Ther. (2007) 37:40–7. doi: 10.2519/jospt.2007.2343
50. Winkelmann ZK, Anderson D, Games KE, Eberman LE. Risk factors for medial tibial stress syndrome in active individuals: an evidence-based review. J Athl Train. (2016) 51:1049–52. doi: 10.4085/1062-6050-51.12.13
51. Tweed JL, Campbell JA, Avil SJ. Biomechanical risk factors in the development of medial tibial stress syndrome in distance runners. J Am Podiatr Med Assoc. (2008) 98:436–44. doi: 10.7547/0980436
52. Allen MK, Glasoe WM. Metrecom measurement of navicular drop in subjects with anterior cruciate ligament injury. J Athl Train. (2000) 35:403–6.
53. Rodriques P, Change R, TenBroek T, van Emmerik R, Hamill J. Evaluating the coupling between foot pronation and tibial internal rotation continuously using vector coding. J Appl Biomech. (2015) 31:88–94. doi: 10.1123/JAB.2014-0067
54. Levinger P, Menz HB, Morrow AD, Bartlett JR, Feller JA, Bergman NR. Relationship between foot function and medial knee joint loading in people with medial compartment knee osteoarthritis. J Foot Ankle Res. (2013) 6:33. doi: 10.1186/1757-1146-6-33
55. Levinger P, Menz HB, Fotoohabadi MR, Feller JA, Bartlett RJ, Bergman NR. Foot posture in people with medial compartment knee osteoarthritis. J Foot Ankle Res. (2010) 3:29. doi: 10.1186/1757-1146-3-29
56. Hintermann B, Nigg BM. Pronation from the viewpoint of the transfer of movement between the calcaneus and tibia. Schweiz Z Sportsmed. (1993) 41:151–6.
57. Mullaji A, Shetty GM. Persistent hindfoot valgus causes lateral deviation of weightbearing axis after total knee arthroplasty. Clin Orthop Relat Res. (2011) 469:1154–60. doi: 10.1007/s11999-010-1703-z
58. Hetsroni I, Funk S, Ben-Sira D, Nyska M, Palmanovich E, Avalon M. Femoracetabular impingement syndrome is associated with alteration in hindfoot mechanics: a three-dimensional gait analysis study. Clin Biomech. (2015) 30:1189–93. doi: 10.1016/j.clinbiomech.2015.08.005
59. Tiberio D. Relationship between foot pronation and rotation of the tibia and femur during walking. Foot Ankle Int. (2000) 21:1057–60. doi: 10.1177/107110070002101214
60. Khamis S, Dar G, Peretz C, Yizhar Z. The relationship between foot and pelvic alignment while standing. J Hum Kinet. (2015) 46:85–97. doi: 10.1515/hukin-2015-0037
61. Tateuchi H, Wada O, Ichihashi N. Effects of calcaneal eversion on three-dimensional kinematics of the hip, pelvis and thorax in unilateral weightbearing. Hum Mov Sci. (2011) 30:566–73. doi: 10.1016/j.humov.2010.11.011
62. Duval K, Lam T, Sanderson D. The mechanical relationship between the rearfoot, pelvis and low-back. Gait Posture. (2010) 32:637–40. doi: 10.1016/j.gaitpost.2010.09.007
63. Kothari A, Stebbins J, Zavatsky AB, Theologis T. Health-related quality of life in children with flexible flatfeet: a cross-sectional study. J Child Orthop. (2014) 8:489–96. doi: 10.1007/s11832-014-0621-0
64. Tenenbaum S, Hershkovich O, Gordon B, Bruck N, Thein R, Derazne E, et al. Flexible pes planus in adolescents: body mass index, body height, and gender–an epidemiological study. Foot Ankle Int. (2013) 34:811–7. doi: 10.1177/1071100712472327
65. Tsiros MD, Buckley JD, Olds T, Howe PR, Hills AP, Walkley J, et al. Impaired physical function associated with childhood obesity: how should we intervene? Child Obes. (2016) 12:126–34. doi: 10.1089/chi.2015.0123
66. Mesquita PR, Neri SGR, Lima RM, Carpes FP, de David AC. Childhood obesity is associated with altered plantar pressure distribution during running. Gait Posture. (2018) 62:202–5. doi: 10.1016/j.gaitpost.2018.03.025
67. Song-Hua Y, Lu W, Kuan Z. Effects of different movement modes on plantar pressure distribution patterns in obese and non-obese Chinese children. Gait Posture. (2017) 57:28–34. doi: 10.1016/j.gaitpost.2017.05.001
68. Rao S, Song J, Kraszewski A, Backus S, Ellis SJ, Deland JT, et al. The effect of foot structure on the 1st metatarsophalangeal joint flexibility and hallucal loading. Gait Posture. (2011) 34:131–7. doi: 10.1016/j.gaitpost.2011.02.028
69. Farahpour N, Jafanezhad A, Damavandi M, Bakhtiari A, Allard P. Gait ground reaction force characteristics of low back pain patients with pronated foot and able-bodied individuals with and without foot pronation. J Biomech. (2016) 49:1705–10. doi: 10.1016/j.jbiomech.2016.03.056
70. Barwick A, Smith J, Chuter V. The relationship between foot motion and lumbopelvic-hip function: a review of the literature. Foot. (2012) 22:224–31. doi: 10.1016/j.foot.2012.03.006
71. Dullaert K, Hagen J, Klos K, Gueorguiev B, Lenz M, Richards RG, et al. The influence of the Peroneus Longus muscle on the foot under axial loading: a CT evaluated dynamic cadaveric model study. Clin Biomech. (2016) 34:7–11. doi: 10.1016/j.clinbiomech.2016.03.001
72. Jennings MM, Christensen JC. The effects of sectioning the spring ligament on rearfoot stability and posterior tibial tendon efficiency. J Foot Ankle Surg. (2008) 47:219–24. doi: 10.1053/j.jfas.2008.02.002
73. Jane MacKenzie A, Rome K, Evans AM. The efficacy of nonsurgical interventions for pediatric flexible flat foot: a critical review. J Pediatr Orthop. (2012) 32:830–4. doi: 10.1097/BPO.0b013e3182648c95
74. Bauer K, Mosca VS, Zionts LE. What's new in pediatric flatfoot? J Pediatr Orthop. (2016) 36:865–9. doi: 10.1097/BPO.0000000000000582
75. Wenger DR, Mauldin D, Speck G, Morgan, Lieber RL. Corrective shoes and inserts as treatment for flexible flatfoot in infants and children. J Bone Joint Surg Am. (1989) 71:800–10. doi: 10.2106/00004623-198971060-00002
76. Whitford D, Esterman A. A randomized controlled trial of two types of in-shoe orthoses in children with flexible excess pronation of the feet. Foot Ankle Int. (2007) 28:715–23. doi: 10.3113/FAI.2007.0715
77. Steber S, Kolodziej L. Analysis of radiographic outcomes comparing foot orthosis to extra-osseous talotarsal stabilization in the treatment of recurrent talotarsal joint dislocation. J Min Inv Orthop. (2015) 1:1–11. doi: 10.15383/jmio.8
78. Jara ME. Evans osteotomy complications. Foot Ankle Clin. (2017) 22:573–85. doi: 10.1016/j.fcl.2017.04.006
79. Subotnick SI. The subtalar joint lateral extra-articular arthroereisis: a preliminary report. J Am Podiatry Assoc. (1974) 64:701–11. doi: 10.2105/AJPH.64.7.701
80. Lanham RH Jr. Indications and complications of arthroereisis in hypermobile flatfoot. J Am Podiatry Assoc. (1979) 69:178–85. doi: 10.7547/87507315-69-3-178
81. Smith RD, Rappaport MJ. Subtalar arthroereisis. A four-year follow-up study. J Am Podiatry Assoc. (1983) 73:356–61. doi: 10.7547/87507315-73-7-356
82. Peters PA, Sammarco GJ. Arthroereisis of the subtalar joint. Foot Ankle. (1989) 10:48–50. doi: 10.1177/107110078901000111
83. Pavone V, Costarella L, Testa G, Conte G, Riccioli M, Sessa G. Calcaneo-stop procedure in the treatment of the juvenile symptomatic flatfoot. J Foot Ankle Surg. (2013) 52:444–7. doi: 10.1053/j.jfas.2013.03.010
84. De Pellegrin M, Moharamzadeh D, Strobl WM, Biedermann R, Tschauner C, Wirth T. Subtalar extra-articular screw arthroereisis (SESA) for the treatment of flexible flatfoot in children. J Child Orthop. (2014) 8:479–87. doi: 10.1007/s11832-014-0619-7
85. Arbab D, Frank D, Bouillon B, Lüring C, Wingenfeld C, Abbara-Czardybon M. [Subtalare Screw Arthroereisis for the Treatment of Symptomatic, Flexible Pes Planovalgus]. Z Orthop Unfall. (2018) 156:93–9. doi: 10.1055/s-0043-120071
86. Graham ME, Jawrani NT, Chikka A, Rogers RJ. Surgical treatment of hyperpronation using an extra-osseous talotarsal stabilization device: radiographic outcomes in adult patients. J Foot Ankle Surg. (2012) 51:548–55. doi: 10.1053/j.jfas.2012.05.027
87. Graham ME, Jawrani NT, Chikka A. Radiographic evaluation of navicular position in the sagittal plane – Correction following an extra-osseous talotarsal stabilization procedure. J Foot Ankle Surg. (2011) 50:551–7. doi: 10.1053/j.jfas.2011.04.027
88. Dana C, Péjin Z, Cadilhac C, Wicart P, Glorion C, Aurégan JC. Long-term results of the “horseman” procedure for severe idiopathic flatfoot in children: a retrospective analysis of 41 consecutive cases with mean 8.9 year duration of follow-up. J Foot Ankle Surg. (2019) 58:10–6. doi: 10.1053/j.jfas.2018.05.008
89. Xu J, Ma X, Wang D, Lu W, Zhu W, Ouyang K, et al. Comparison of extraosseous talotarsal stabilization implants in a stage II adult-acquired flatfoot model: a finite element analysis. J Foot Ankle Surg. (2017) 56:1058–64. doi: 10.1053/j.jfas.2017.05.009
90. Chong DY, Macwilliams BA, Hennessey TA, Teske N, Stevens PM. Prospective comparison of subtalar arthroereisis with lateral column lengthening for painful flatfeet. J Pediatr Orthop B. (2015) 24345–53. doi: 10.1097/BPB.0000000000000179
91. Graham ME, Jawrani NT, Goel VK. Evaluating plantar fascia strain in hyperpronating cadaveric feet following an extra-osseous talotarsal stabilization procedure. J Foot Ankle Surg. (2011) 50:682–6. doi: 10.1053/j.jfas.2011.07.005
92. Graham ME. Jawrani NT, Goel VK. Effect of extra-osseous talotarsal stabilization on posterior tibial nerve strain in hyperpronating feet: a cadaveric evaluation. J Foot Ankle Surg. (2011) 50:672–5. doi: 10.1053/j.jfas.2011.07.004
93. Graham ME, Jawrani, NT, Goel VK. Effect of extra-osseous talotarsal stabilization on posterior tibial tendon strain in hyperpronating feet. J Foot Ankle Surg. (2011) 50:676–81. doi: 10.1053/j.jfas.2011.06.015
94. Caravaggi P, Lullini G, Berti L, Giannini S, Leardini A. Functional evaluation of bilateral subtalar arthroereisis for the correction of flexible flatfoot in children: 1-year follow-up. Gait Posture. (2018) 64:152–8. doi: 10.1016/j.gaitpost.2018.06.023
95. Martinelli N, Marinozzi A, Schulze M, Denaro V, Evers J, Bianchi A, Rosenbaum D. Effects of subtalar arthroereisis on the tibiotalar contact characteristics in a cadaver flatfoot model. J Biomech. (2012) 45:1745–8. doi: 10.1016/j.jbiomech.2011.11.009
96. Martinelli N, Bianchi A, Martinkevich P, Sartorelli E, Romeo G, Bonifacini C, et al. Return to sport activities after subtalar arthroereisis for correction of pediatric flexible flatfoot. J Pediatr Orthop B. (2018) 27:82–7. doi: 10.1097/BPB.0000000000000449
97. Nelson SC, Haycock DM, Little ER. Flexible flatfoot treatment with arthroereisis: radiographic improvement and child health survey analysis. J Foot Ankle Surg. (2004) 43:144–55. doi: 10.1053/j.jfas.2004.03.012
98. Faldini C, Mazzotti A, Panciera A, Persiani V, Pardo F, Perna F, et al. Patient-perceived outcomes after subtalar arthroereisis with bioabsorbable implants for flexible flatfoot in growing age: a 4-year follow-up study. Eur J Orthop Surg Traumatol. (2018) 28:707–12. doi: 10.1007/s00590-017-2119-1
Keywords: pediatric flatfeet, hyperpronation, pes planus, subtalar joint instability, extra-osseous talotarsal stabilization, flat feet
Citation: Bresnahan PJ and Juanto MA (2020) Pediatric Flatfeet—A Disease Entity That Demands Greater Attention and Treatment. Front. Pediatr. 8:19. doi: 10.3389/fped.2020.00019
Received: 17 September 2019; Accepted: 14 January 2020;
Published: 11 February 2020.
Edited by:
Ulf Kessler, Klinik Beau-Site, Hirslanden, SwitzerlandReviewed by:
Zorica Momcilo Zivkovic, University Hospital Center Dr. Dragiša Mišović, SerbiaMichael E. Graham, Graham International Implant Institute, United States
Copyright © 2020 Bresnahan and Juanto. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Philip J. Bresnahan, footdoc_99@yahoo.com
 Philip J. Bresnahan
Philip J. Bresnahan Mario A. Juanto2
Mario A. Juanto2