- 1Department of Pediatrics, Willem-Alexander Children's Hospital, Leiden University Medical Centre, Leiden, Netherlands
- 2Department of Medical Ethics and Health Law, Leiden University Medical Centre, Leiden, Netherlands
- 3Department of Obstetrics, Leiden University Medical Center, Leiden, Netherlands
Hematopoietic stem cell transplantation decision-making for hemoglobinopathy patients is a complex process, and it remains difficult for health care professionals to decide whether and when a hematopoietic stem cell transplantation should be offered. Gaining insight into health care professionals' considerations is required to understand and optimize this decision-making process. A qualitative interview study using semi-structured interviews with eighteen health care professionals. Data were thematically analyzed. Two main themes emerged from the data: (1) Experiencing the influence of a frame of reference and (2) Feeling responsible for a guided decision-making. The frame of reference, meaning the health care professionals' knowledge and experiences regarding hematopoietic stem cell transplantation, influenced the guided decision-making process. Subsequently, three subthemes evolved from the second theme: (a) weighing up disease severity against possible complications, (b) making an effort to inform, and (c) supporting the best fitting decision for the individual patient. The health care professionals' frame of reference determined the hematopoietic stem cell transplantation decision-making process. This demands reflection on the health care professionals' own frame of reference and its influence on decision-making. Furthermore, reflection on the frame of reference is needed by exchange of knowledge and experiences between referring and referred-to healthcare professionals in an open and two-way direction. The transplantation teams have a responsibility of keeping the frame of reference of their referring colleagues up to date and referring health care professionals should share their feelings regarding hematopoietic stem cell transplantation. To guide patients, a shared decision-making approach is supportive, in which eliciting the patients' preferences is highly important. Health care professionals can refine the decision-making process by guiding patients in eliciting their preferences and including these in the decision.
Introduction
Hemoglobinopathies are one of the most common recessive diseases affecting humans worldwide. At least 5.2% of the global population is a carrier of hemoglobinopathy (1). Annually, over 330.000 affected children are born, 17% have thalassemia, and 83% have Sickle Cell Disease (SCD) (1). Despite improvements in supportive care for both diseases, life expectancy and quality of life remain severely hampered (2–4). Allogeneic hematopoietic stem cell transplantation (HSCT) offers an established curative option (5–9) but is associated with significant risks (6, 10). Gene therapy is a promising alternative treatment modality, but long-term outcome data are currently lacking (11). The process to decide for HSCT, gene therapy, or remaining on supportive care is complex (12, 13).
In current practice, it remains difficult for healthcare professionals (HCPs) to decide when HSCT should be offered as an option in hemoglobinopathy patients (10, 14–16). As there is no clear-cut general answer to what the best treatment would be, the patients' and/or families opinions are of high value to include in decision-making. In general two types of medical decisions can be distinguished, effective, and preference-sensitive decisions (17). Effective decisions refer to decisions in which a scientific certainty exists, and clearly more pros than cons are known. Preference-sensitive decisions point to decisions in which no clear-cut answers are available, and the pros and cons are dependent on individual values (17). Treatment decision-making in hemoglobinopathy patients can be approached as preference-sensitive (18). A shared decision-making (SDM) approach can facilitate preference sensitive decisions (19, 20). This approach based on autonomy principles, aims to involve the patient's preferences and values in a collaborative decision-making process. An SDM approach in pediatrics showed to decrease uncertainty, clarify the patient's future health status, and facilitate the making of high-quality decisions (21–23).
For SDM to start, at least one of the participants (patient, family, HCP) needs to bring up the subject. Currently, it is unclear how HCPs decide whether HSCT for a given patient should be offered or explored (24). From clinical practice, fear of the unknown or personal opinions seem important issues influencing the position of HCPs in the decision-making process. Gaining insight into HCPs' considerations and whether these promote or hamper SDM is important because HCPs are involved in starting the process of deciding. This study aims to identify the considerations used by HCPs in the HSCT decision-making process in patients with hemoglobinopathies and/or caregivers.
Methods
Study Design
A qualitative interview study to identify and describe HCP's perspectives was conducted. As this study aimed to make sense of the perspectives of HCPs and very little is known about these perspectives, a qualitative method was chosen. A qualitative approach provides the opportunity to be able to describe, understand, and interpret the perspectives of HCP's (25, 26).
Population and Recruitment
This study is part of a longitudinal, multi-center study, focusing on the HSCT decision-making process from the patients' perspectives (0–35 yr) with hemoglobinopathies, their caregivers, and the involved HCPs. The six largest expert centers on both (pediatric and adult) regular hemoglobinopathy care and HSCT in the Netherlands participated in this study. These six specialized centers collaborate in SCD research in the Netherlands as the so-called SCORE consortium. The results of the interviews with the involved HCPs are described in the present article. Using purposive sampling, hematologists, transplantation specialists, and nurse practitioners from the six involved expert centers and actively involved in the care of the included patients in the larger study were invited by mail to participate. Purposive sampling was chosen in order to select professionals with extensive experience in hemoglobinopathies and HSCT. We intended to achieve a maximum variation in years of experience in the field and experience as referring hematologist, nurse specialist, and HSCT specialist. In consistence with qualitative research standards, inclusion continued until thematic saturation was reached (26). Saturation was reached after 17 interviews since the analysis of the last interview (interview 18) did not add to the descriptions of the themes and no new themes emerged (27). This number of respondents is in agreement with qualitative research standards, where 14–20 subjects are seen sufficient in heterogeneous groups (26). All study procedures were in accordance with the declaration of Helsinki (28), and all subjects consented to participation in the study. The medical ethics committee of Leiden University Medical Center approved the study protocol (P17.084).
Data Collection
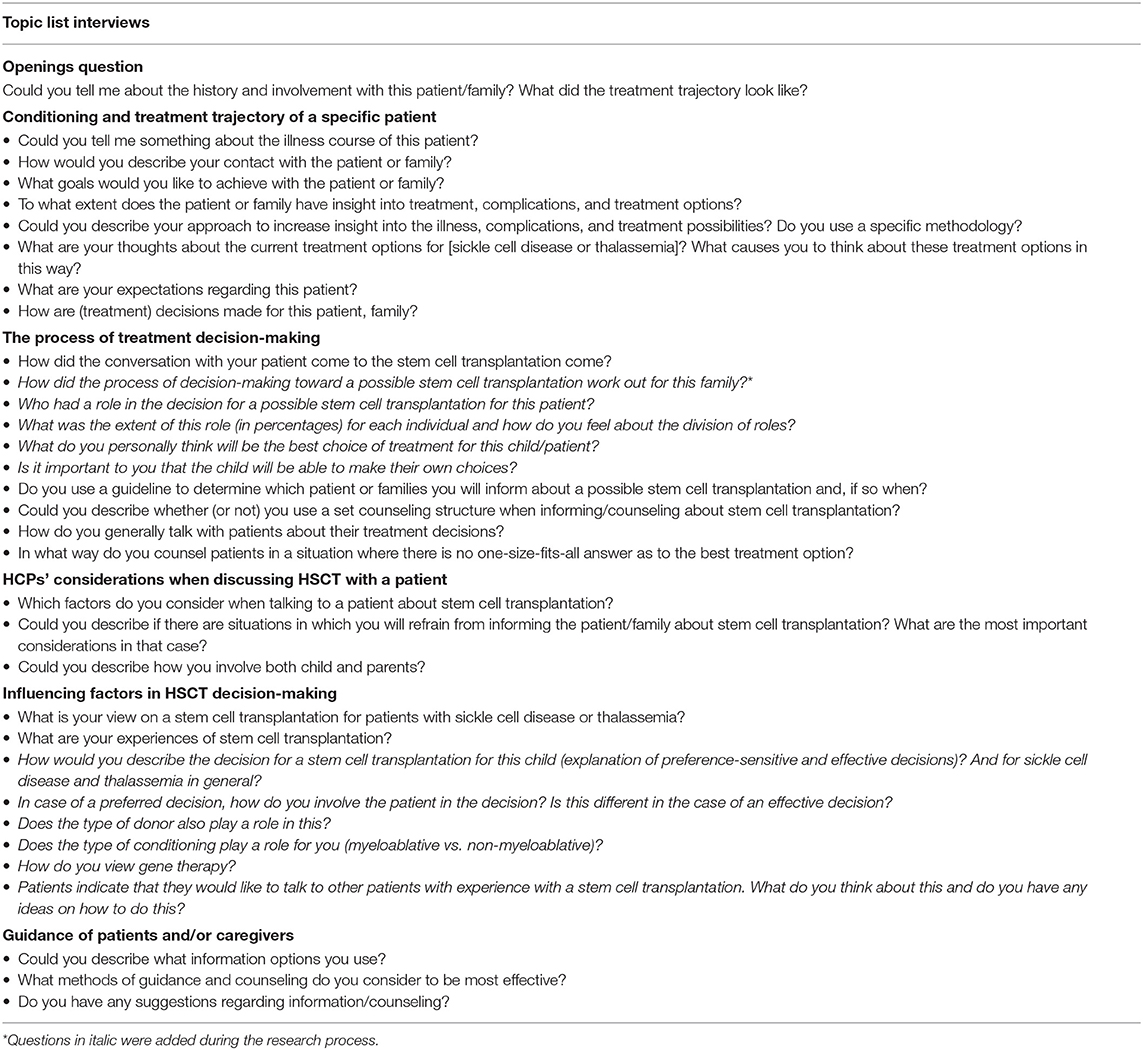
A nurse specialized in pediatric HSCT with experience in qualitative interviewing (HM) conducted the individual semi-structured interviews. Semi-structured interviews provide the opportunity to gain insight into the HCPs' considerations, whereas at the same time the focus of the interview can be controlled. A topic list was used to ensure whether all topics to answer the research question were covered (Table 1) (26, 27). This topic list was based on preliminary studies on HSCT decision-making and experts' experiences (23, 29–32). The topic list was evaluated and adjusted throughout the project twice, based on insights from the interviews and analyses, referring to an iterative process (26). The interviewed HCPs were involved in the decision-making process of specific patients (included in the larger study), either as (referring) pediatric hematologist, HSCT physician or nurse practitioner. The starting point for the interviews was this specific patient case. For examples of such patient cases, see Supplementary Table 1. Interviews consist of open-ended questions. The interviews were audio-recorded and transcribed verbatim. Observational memos were used to describe the setting, atmosphere, circumstances, and the researchers' reflections on the interview themes (26).
Data Analysis
Thematic analysis was used to identify patterns and themes that reflected the HCPs' perspectives (25–27, 33). Transcripts were read and reread for familiarization with the data and the generation of initial codes (HM,HZ). Open coding was conducted independently by two team members (HM,HZ). During this stage the transcripts were segmented into meaningful parts and labeled (coded) with a description of the essence of that part of the text. Subsequently, focused coding was used, comparing codes and categorizing these on a more conceptual level. Finally, categories were described into themes, interpreting the data and describing the meaning of the categories (33, 34). The themes were described in the results section and represent the considerations of the total group of HCPs. When differences did appear within the subgroups of HCPs, this is indicated. Discrepancies in coding, the developing of categories, and defining and refining of the themes were discussed until consensus was reached (HM,HZ,MV). The research team was involved in all phases of data collection and analysis to enhance validity and credibility (27). The COREQ checklist was used to enhance comprehensive reporting (Supplementary Table 2) (35). Coding was supported by qualitative data analysis software, ATLAS.ti (version 8) (36).
Results
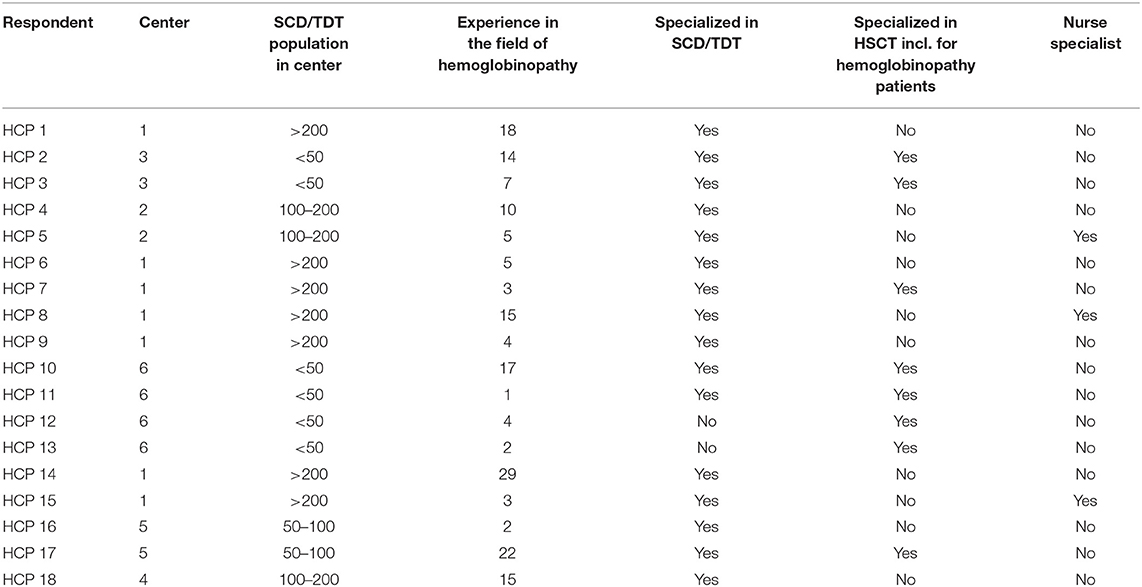
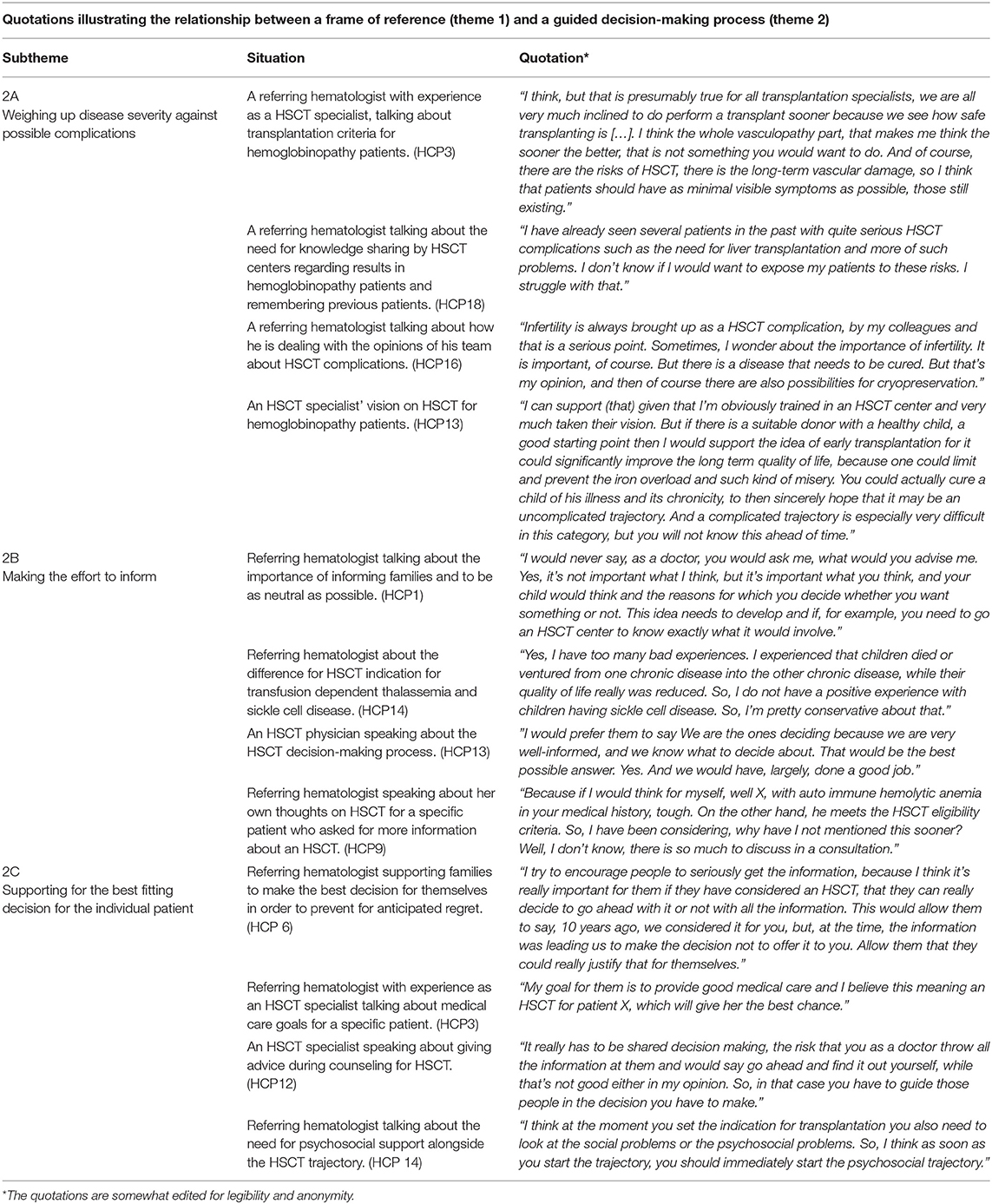
Between July 2017 and January 2020, 18 HCPs, including 10 (pediatric) referring hematologists, five transplantation specialists from HSCT centers, and three nurse specialists from referring centers, were approached and participated in the interviews (Table 2). The mean age of the professionals was 47 years (SD 9; range 33–64 years); the professional experience of the HCPs in the field of hemoglobinopathy was variable with a mean of 10 years (SD 8; range 1–29 years). Each HCP was interviewed once, and most interviews took place at the HCP's office and one by phone. The interviews lasted on average 38 min (SD 9; range 27–57 min). Two main themes emerged from the qualitative analysis of the interviews: (1) experiencing the influence of a frame of reference and (2) feeling responsible for a guided decision-making process. The first theme appeared to be an overarching theme, and the way how this frame of reference influenced HCPs in their decision-making is described within the second theme. This second theme is split in three subthemes. For illustrative quotations (37), see Table 3.
Theme 1: Experiencing the Influence of a Frame of Reference
From the interviews, it became clear that their frames of reference influenced HCPs' considerations about HSCT decision-making for hemoglobinopathy patients. The frame of reference refers to knowledge and experiences of the HCPs, as mentioned in the interviews. Firstly, HCPs referred to knowledge on treatment and specifically curative treatment options. This knowledge can be the knowledge available to themselves, within their team, in the literature or from new emerging therapies. Furthermore, HCP's pointed to the lack of evidence about curative treatments such as RCTs. The HCPs' knowledge depends on their specialty and experience and therefore differs between referring specialists and HSCT specialists, but also juniors and seniors. Available knowledge on HSCT seems more difficult to translate into practice by referring HCPs without experience in HSCT, pointing to the influence of experiences on the HCPs' frame of reference. HCPs referred to either positive or negative (team) experiences with the disease or with HSCT. Most referring pediatric HCPs struggled with experiences of individual HSCT patients without having the overview on cohort level, as articulated by a referring HCP “I have already seen several patients in the past with quite serious HSCT complications such as the need for liver transplantation and more of such problems. I don't know if I would want to expose my patients to these risks.” At the same time, HCPs of adult patients struggled with the experiences of non-transplanted SCD patients with serious organ damage and impaired QoL. Experiences furthermore are different among junior or senior members. Junior team members explained that if solid evidence is lacking and they do not have extensive experience themselves, they rely even more on a shared decision-making approach in which they valued the voice of the patient or family crucial. Although, senior professionals also stated the importance of including the patients perspective into the decision, they rely on their experiences in feeling comfortable to offer (HSCT physicians) or being reluctant in discussing a HSCT (referring HCP). Besides, (junior) HCPs experienced the influence of opinions of other (senior) team members in the difficulty of weighing chances vs. risks when considering to refer a patient for HSCT. This influence was illustrated by examples HCPs gave during the interviews about the negative experiences their colleagues had with specific patients with severe HSCT complications. HSCT for transfusion-dependent thalassemia (TDT) patients appeared to be a more broadly accepted approach based on experienced good outcomes in previously transplanted TDT patients, more available evidence in the literature, and a more predictable disease course with non-curative therapy.
Despite their knowledge and experiences, most HCPs stated that guiding the patients objectively in their decision-making is of high importance. Nevertheless, the HCPs' frame of reference influenced their considerations and consequently their decision-making. The influence of the HCPs' frame of reference on decision-making is demonstrated in how HCPs guide their patients during the decision-making process.
Theme 2: Feeling Responsible for a Guided Decision-Making Process
HCPs referred to treatment decision-making for patients with hemoglobinopathies as a process, starting with the first consultation where diagnosis, treatment, and curation possibilities are explained. During this phase, HCPs guide patients in coping with the disease, aiming for acceptance of the disease, and prevention and management of symptoms. In case of TDT, the possibility of HSCT is discussed with caregivers relatively early, at a young age of the child. For SCD, the option of an HSCT will usually be brought up in case of increased disease severity, for example, after an acute chest syndrome or in case of high risk of stroke. Increasingly, HCPs experience that pediatric and adult SCD patients or their caregivers themselves initiate the discussion on HSCT as a curative treatment option, often influenced by social media. Within the guided decision-making process, three subthemes emerged that describe the responsibility experienced by the HCPs in guiding patients and how their frame of reference promoted or hampered decision-making.
2A Weighing up Disease Severity Against Possible Complications
HCPs mentioned that, in general, they based the indication for HSCT on (inter)national criteria, and the HSCT teams made a final decision on the indication. In case caregivers have major doubts about an HSCT for their child with TDT and choose to continue with the transfusion scheme, most HCPs created time for parents to consider alternative options, or the HCPs accepted the caregiver's viewpoint. Most HCPs explained that transplanting TDT patients at a young age is important to prevent transfusions complications. Due to developments in transfusion and chelation therapy some HCPs reported a shift in their thinking, where the possibility of an HSCT should be explored, and the alternatives. When considering an HSCT for SCD patients, referring HCPs struggled with the dilemma between disease severity, the unpredictability of the disease process, the possible good responses on supportive care, and the significant risks of long-term HSCT complications. HCPs realized however, that non-curative treatments do not resolve the long-term disease burden sequelae, impacting the quality of life and life expectancy. Generally, all HCPs characterized the decision for HSCT as complex, weighing chances for cure vs. risks. HSCT physicians tend to offer HSCT more easily to patients meeting consensus-based criteria, whereas referring HCPs are more reluctant, both based on their formed frame of reference.
2B Making the Effort to Inform
To facilitate patients in decision-making, all HCPs emphasized their key role in providing the patient with objective information about all treatment options rather than giving advice. Most referring HCPs stated that they provided and discussed information about treatment possibilities regularly during the treatment over the years. HCPs explained that questions of patients or caregivers about curative therapy need to be respected and supported by providing all information. Therefore, patients were easily referred to an HSCT specialist to inform them with up-to-date knowledge about the currently used treatments and its outcomes. Nurse practitioners said they did not have a significant role in informing about HSCT, but patients regularly discussed their thoughts and questions about treatment possibilities with them. Their role appeared to be more supportive in decision-making rather than informative and decisive. In their counseling for a possible HSCT, HCPs included several aspects: the availability of a suitable donor, timing for a possible HSCT, future treatment possibilities and the perceived disease burden without HSCT, however hard to estimate and quantify. These latter aspects could have more or less impact depending on the disease severity, the families' wishes and circumstance, and were influenced by the HCPs' own frame of reference. As illustrated by a referring HCP: “Because if I would think for myself, well X, with autoimmune hemolytic anemia in your medical history, tough. On the other hand, he meets the HSCT eligibility criteria. So, I have been considering why have I not mentioned this sooner? Well, I don't know, there is so much to discuss in a consultation.” Although most HCPs stated that they have the task to inform, they based the timing of informing and discussing the option of HSCT on their frame of reference.
2C Supporting the Best-Fitting Decision for the Individual Patient
HCPs underlined their task in the SDM process in providing detailed information on an individual level. All HCPs stated that their role in the decision-making process is important, but most of them believed that neutrality is necessary to enable families to make their own decisions and to prevent for decisional regret. Since giving advice appeared to be influenced by personal experiences, some HCPs felt not experienced enough to fulfill this task. In contrast, other HCPs explained that they give some advice, mainly based on their experiences with HSCT, but also directed by the disease burden. In supporting patients in their decision-making, a trustful relationship with patients was mentioned as a vital condition; for patients to discuss their fears and for HCPs to understand patients' needs during the whole process. Furthermore, HCPs expressed the importance of paying attention to the patient's medical and psycho-social situation, treatment compliance, and the perceived burden of the disease. Providing support in such circumstances was considered essential by HCPs before proceeding in the HSCT decision-making process. This support seems essential for, but not limited to, patients with complex circumstances, such as a refugee background, adopted children or families with lower health literacy. Especially in adult patients' compliance was mentioned as of great importance for an intense treatment like HSCT, to increase the likelihood of a successful HSCT. HCPs mentioned that they consider the child's own wishes by not just speaking with the family but also, depending on his/her age, listening to the child's ideas and questions. The importance of team collaboration between the referring hematologists and the HSCT teams was mentioned in order to reach a consensus about the patient's disease progression, indication for HSCT, and proper support for the patient and/or family.
Discussion
Our study identified “the influence of a frame of reference” as the central theme in the HCPs' decision-making process when considering an HSCT for hemoglobinopathy patients. This frame of reference referred to the HCPs' knowledge and experiences and influenced the way HCPs guided their patients in the HSCT decision-making process and therefore demands awareness.
This study showed that HCPs considered SDM as an important approach in HSCT decision-making for hemoglobinopathy patients. We described that HSCT for TDT patients, based on successful experiences and available knowledge on outcomes, was considered an effective treatment and therefore, as a less complex decision. In contrast, the choice for HSCT in SCD patients was mainly experienced as a preference-sensitive decision, and hence the decision-making process was more multifaceted. The HCPs were aware that advances in HSCT care indications for transplantation for both diseases are changing, complicating the decision-making process, and urging the need for SDM. Furthermore, disease burden, expected disease course, and possible HSCT-related complications were important factors in weighing a possible HSCT for patients. The more broadly accepted approach for HSCT in TDT patients compared to SCD patients confirmed the results of a previous study investigating HCPs' referral policy for HSCT in hemoglobinopathy patients (32). We observed that HCPs used a more advising-directed approach in case of TDT or severe complications in SCD, which was observed in a previous study. This study reported a collaborative or proponent approach in the process of decision-making for SCD patients, influenced by disease severity, the intensity of treatment, and urgency of treatment (38). Our study added to this mechanism with the strong influence of the HCP's frame of reference in guiding the decision-making process. The influence of training was observed previously, showing that the period of specialty training influenced the referral of patients for HSCT evaluation (32). Our study provided in-depth insight into how experience and knowledge influenced the HSCT decision-making process.
An important finding in our study is the influence of the HCPs' frame of reference. This finding leads to a pertinent message for clinical practice. Although some HCPs expressed they want to use a neutral approach, the question arises if and to what extent it is possible to maintain a neutral position (39). In order to reflect on neutrality, some aspects can be taken into consideration. First of all, to be aware of your own frame of reference, to prevent framing of available treatment options (39). Subsequently, the frame of reference demands a reflection from HCPs on this phenomenon by exchanging knowledge and experiences of referring and referred-to HCPs in a two-way direction. The HSCT teams have a responsibility of keeping the frame of reference of their referring colleagues up-to-date, by providing them outcomes and experiences on the cohort level. Referring HCPs should share their feelings regarding HSCT and discuss their patients with HSCT centers regularly, in an open peer-review way. The HSCT decision-making process will benefit from such an open collaboration between centers. Furthermore, the non-neutral position of the information giver can be overcome by involving multiple information givers in the decision-making process with their own approach and vision. Finally, an SDM approach is a supportive and guiding methodology. SDM goes beyond providing information on which patients can base their decision. Deliberating options with patients, eliciting their preferences, and including these in the decision are of equal importance (19, 20). Research evaluating the SDM approach in conversations showed low or moderate levels of patient-involving behavior. (40, 41) These results shows the need for the implementation of SDM interventions and SDM training for HCP. In treatment decision-making, an advocating role of the HCP is necessary in which both the patient's health and respect for the patient's self-determination need to be thoughtfully balanced (39).
A strength of our study was the ability to provide a broad view of perspectives from HCPs from multiple centers and with different backgrounds. Maximum variation in the sample was achieved, increasing the likelihood of representing the population. We enhanced the objectivity of the data analysis by double, independent coding and the involvement of experts on the topic in the research team. We did not perform data validation by member check, although discussion of the study results with the study population (SCORE consortium) confirmed our observation of the importance of the frame of reference. We had a relatively long inclusion period combined with new developing therapies, such as gene therapy. With our description of the influence of the frame of reference, we showed that knowledge is an important factor in considering treatment options for hemoglobinopathy patients. Knowledge regarding new therapies is rapidly evolving, showing that knowledge in SDM constantly improves and easily changes.
In conclusion, our study shows the influence of the HCPs' frame of reference on how they guide their hemoglobinopathy patients in the HSCT decision-making process. This decision-making process will benefit from the HCPs' reflection on their frame of reference and exchange of knowledge and experiences. Finally, HCPs can refine the decision-making process by guiding patients in eliciting their preferences and including these in the decision.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by METC Leiden-Den Haag-Delft. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
HM, MdV, AL, and FS contributed to conception and design of the study. HM performed the interviews. HM and HvZ analyzed the data and wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank all the professionals who contributed to this study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2021.690309/full#supplementary-material
Abbreviations
SCD, Sickle Cell Disease; HSCT, Hematopoietic Stem Cell Transplantation; HCP, Health Care Professional; SDM, Shared Decision-making; TDT, Transfusions Dependent Thalassemia.
References
1. Modell B, Darlison M. Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ. (2008) 86:480–7. doi: 10.2471/BLT.06.036673
2. Badawy SM, Thompson AA, Lai J-S, Penedo FJ, Rychlik K, Liem RI. Adherence to hydroxyurea, health-related quality of life domains, and patients' perceptions of sickle cell disease and hydroxyurea: a cross-sectional study in adolescents and young adults. Health Qual Life Outcomes. (2017) 15:136. doi: 10.1186/s12955-017-0713-x
3. Porter J. Beyond transfusion therapy: new therapies in thalassemia including drugs, alternate donor transplant, and gene therapy. Hematol Am Soc Hematol Educ Program. (2018) 2018:361–70. doi: 10.1182/asheducation-2018.1.361
5. King A, Shenoy S. Evidence-based focused review of the status of hematopoietic stem cell transplantation as treatment of sickle cell disease and thalassemia. Blood. (2014) 123:3089–94. doi: 10.1182/blood-2013-01-435776
6. Smiers FJ, Krishnamurti L, Lucarelli G. Hematopoietic stem cell transplantation for hemoglobinopathies: current practice and emerging trends. Pediatr Clin North Am. (2010) 57:181–205. doi: 10.1016/j.pcl.2010.01.003
7. Guilcher GMT, Truong TH, Saraf SL, Joseph JJ, Rondelli D, Hsieh MM. Curative therapies: allogeneic hematopoietic cell transplantation from matched related donors using myeloablative, reduced intensity, and nonmyeloablative conditioning in sickle cell disease. Semin Hematol. (2018) 55:87–93. doi: 10.1053/j.seminhematol.2018.04.011
8. La Nasa G, Caocci G, Efficace F, Dessì C, Vacca A, Piras E, et al. Long-term health-related quality of life evaluated more than 20 years after hematopoietic stem cell transplantation for thalassemia. Blood. (2013) 122:2262–70. doi: 10.1182/blood-2013-05-502658
9. Badawy SM, Beg U, Liem RI, Chaudhury S, Thompson AA. A systematic review of quality of life in sickle cell disease and thalassemia after stem cell transplant or gene therapy. Blood Adv. (2021) 5:570–83. doi: 10.1182/bloodadvances.2020002948
10. Nickel RS, Hendrickson JE, Haight AE. The ethics of a proposed study of hematopoietic stem cell transplant for children with “less severe” sickle cell disease. Blood. (2014) 124:861–6. doi: 10.1182/blood-2014-05-575209
11. Thompson AA, Walters MC, Kwiatkowski J, Rasko JEJ, Ribeil JA, Hongeng S, et al. Gene therapy in patients with transfusion-dependent β-Thalassemia. N Engl J Med. (2018) 378:1479–93.
12. Krishnamurti L. Hematopoietic cell transplantation for sickle cell disease. Front Pediatrics. (2020) 8:551170. doi: 10.3389/fped.2020.551170
13. Sinha CB, Bakshi N, Ross D, Loewenstein G, Krishnamurti L. Primary caregiver decision-making in hematopoietic cell transplantation and gene therapy for sickle cell disease. Pediatr Blood Cancer. (2021) 68:e28749. doi: 10.1002/pbc.28749
14. Walters MC, Patience M, Leisenring W, Eckman JR, Scott JP, Mentzer WC, et al. Bone marrow transplantation for sickle cell disease. N Engl J Med. (1996) 335:369–76. doi: 10.1056/NEJM199608083350601
15. Angelucci E, Matthes-Martin S, Baronciani D, Bernaudin F, Bonanomi S, Cappellini MD, et al. Hematopoietic stem cell transplantation in thalassemia major and sickle cell disease: indications and management recommendations from an international expert panel. Haematologica. (2014) 99:811–20. doi: 10.3324/haematol.2013.099747
16. Nickel RS, Kamani NR. Ethical challenges in hematopoietic cell transplantation for sickle cell disease. Biol Blood Marrow Transplant. (2017) 24:219–27. doi: 10.1016/j.bbmt.2017.08.034
17. Wennberg JE. Dealing with medical practice variations: a proposal for action. Health Affairs. (1984) 3:6–32. doi: 10.1377/hlthaff.3.2.6
18. Brand PL, Stiggelbout AM. Effective follow-up consultations: the importance of patient-centered communication and shared decision making. Paediatr Respir Rev. (2013) 14:224–8. doi: 10.1016/j.prrv.2013.01.002
19. Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. (2012) 27:1361–7. doi: 10.1007/s11606-012-2077-6
20. Stiggelbout AM, Pieterse AH, De Haes JC. Shared decision making: concepts, evidence, and practice. Patient Educ Couns. (2015) 98:1172–9. doi: 10.1016/j.pec.2015.06.022
21. Kon AA, Morrison W. Shared decision-making in pediatric practice: a broad view. Pediatrics. (2018) 142(Suppl. 3):S129–32. doi: 10.1542/peds.2018-0516B
22. Boland L, Graham ID, Legare F, Lewis K, Jull J, Shephard A, et al. Barriers and facilitators of pediatric shared decision-making: a systematic review. Implement Sci. (2019) 14:7. doi: 10.1186/s13012-018-0851-5
23. Meier ER, Dioguardi JV, Kamani N. Current attitudes of parents and patients toward hematopoietic stem cell transplantation for sickle cell anemia. Pediatr Blood Cancer. (2015) 62:1277–84. doi: 10.1002/pbc.25446
24. Yawn BP, Buchanan GR, Afenyi-Annan AN, Ballas SK, Hassell KL, James AH, et al. Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. JAMA. (2014) 312:1033–48. doi: 10.1001/jama.2014.10517
25. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
26. Holloway I, Wheeler S. Qualitative Research in Nursing and Healthcare. 3rd ed. Oxford: Wiley-Blackwell (2010) 368 p.
28. World Medical Association World Medical Association Declaration of Helsinki: Ethical principles for medical reserach involving human subjects. JAMA. (2013) 310:2191–2194. doi: 10.1001/jama.2013.281053
29. Pelletier W, Hinds PS, Alderfer MA, Fairclough DL, Stegenga K, Pentz RD. Themes reported by families as important when proceeding with pediatric hematopoietic stem cell transplantation. Pediatr Blood Cancer. (2014) 61:1625–31. doi: 10.1002/pbc.25075
30. Hankins J, Hinds P, Day S, Carroll Y, Li CS, Garvie P, et al. Therapy preference and decision-making among patients with severe sickle cell anemia and their families. Pediatr Blood Cancer. (2007) 48:705–10. doi: 10.1002/pbc.20903
31. Hansbury EN, Schultz WH, Ware RE, Aygun B. Bone marrow transplant options and preferences in a sickle cell anemia cohort on chronic transfusions. Pediatr Blood Cancer. (2012) 58:611–5. doi: 10.1002/pbc.23304
32. Mikles B, Bhatia M, Oyeku SO, Jin Z, Green NS. Pediatric hematology providers on referral for transplant evaluation for sickle cell disease: a regional perspective. J Pediatr Hematol Oncol. (2014) 36:566–71. doi: 10.1097/MPH.0000000000000147
33. Charmaz K. Constructing Grounded Theory, a Practical Guide Through Qualitative Analysis. 1st ed. College DSG, editor. London, United Kingdom Sage Publications Ltd (2006). 224 p.
34. Dierckx de Casterle B, Gastmans C, Bryon E, Denier Y. QUAGOL: a guide for qualitative data analysis. Int J Nurs Stud. (2012) 49:360–71. doi: 10.1016/j.ijnurstu.2011.09.012
35. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
37. Eldh AC, Årestedt L, Berterö C. Quotations in qualitative studies: reflections on constituents, custom, and purpose. Int J Qual Methods. (2020). 19:1609406920969268. doi: 10.1177/1609406920969268
38. Bakshi N, Sinha CB, Ross D, Khemani K, Loewenstein G, Krishnamurti L. Proponent or collaborative: physician perspectives and approaches to disease modifying therapies in sickle cell disease. PLoS ONE. (2017) 12:e0178413. doi: 10.1371/journal.pone.0178413
39. Brock DW. The ideal of shared decision making between physicians and patients. Kennedy Inst Ethics J. (1991) 1:28–47. doi: 10.1353/ken.0.0084
40. Couët N, Desroches S, Robitaille H, Vaillancourt H, Leblanc A, Turcotte S, et al. Assessments of the extent to which health-care providers involve patients in decision making: a systematic review of studies using the OPTION instrument. Health Expect. (2015) 18:542–61. doi: 10.1111/hex.12054
Keywords: decision-making, hematopoietic stem cell transplantation, health care professional, hemoglobinopathy, sickle cell disease, Thalassemia
Citation: Mekelenkamp H, Zanten Hv, Vries Md, Lankester A and Smiers F (2021) How to Facilitate Decision-Making for Hematopoietic Stem Cell Transplantation in Patients With Hemoglobinopathies. The Perspectives of Healthcare Professionals. Front. Pediatr. 9:690309. doi: 10.3389/fped.2021.690309
Received: 02 April 2021; Accepted: 29 July 2021;
Published: 18 August 2021.
Edited by:
Maria Ester Bernardo, San Raffaele Hospital (IRCCS), ItalyReviewed by:
Massimo Berger, University Hospital of the City of Health and Science of Turin, ItalyJeffrey R. Andolina, University of Rochester, United States
Copyright © 2021 Mekelenkamp, Zanten, Vries, Lankester and Smiers. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hilda Mekelenkamp, aC5tZWtlbGVua2FtcEBsdW1jLm5s
 Hilda Mekelenkamp
Hilda Mekelenkamp Herma van Zanten
Herma van Zanten Martine de Vries1,2
Martine de Vries1,2 Arjan Lankester
Arjan Lankester