Role of Extracorporeal Membrane Oxygenation in Adults and Children With Refractory Septic Shock: A Systematic Review and Meta-Analysis
- Department of Intensive Care Unit of Hunan Children's Hospital, Changsha, China
Background: The benefits of extracorporeal membrane oxygenation in patients with refractory septic shock remain controversial. Current guidelines on the management of refractory septic shock recommend the consideration of extracorporeal membrane oxygenation as a salvage therapy. The difference between adults and children with septic refractory shock treated with extracorporeal membrane oxygenation has not been previously analyzed. We aimed to review peer-reviewed publications on the role of extracorporeal membrane oxygenation in adults and children with refractory septic shock.
Methods: Studies reporting on mortality in both adults and children with refractory septic shock supported with extracorporeal membrane oxygenation published in PubMed, Cochrane Library, and Embase databases were included in the meta-analysis. Study eligibility was independently assessed by two authors, and disagreements were resolved by a third author. The outcome measure was survival at discharge. Subgroup analysis included the adult and pediatric groups.
Results: Of the 293 articles screened, 14 original articles were identified for systematic review and meta-analysis. The cumulative estimate of survival (14 studies, 535 patients) in the cohort was 39% (95% confidence interval [CI]: 27–51%). During the subgroup analysis, the cumulative estimate of survival at discharge in the adult group (6 studies, 276 patients) in the cohort was 18% (95% CI: 10–27%), and that in the pediatric group (8 studies, 259 patients) was 53% (95% CI: 47–59%).
Conclusions: The survival rate of adults with refractory septic shock requiring extracorporeal membrane oxygenation was 18%, and children with refractory septic shock requiring extracorporeal membrane oxygenation had a higher survival rate (53%) than adults.
Introduction
In recent years, the use of extracorporeal membrane oxygenation (ECMO) in both adult and pediatric patients has increased significantly (1). Refractory septic shock is a clinical condition caused by a dysregulated host response to infection and is characterized by the presence of refractory hypotension and a high serum lactate level (2). The American College of Critical Care Medicine has suggested that ECMO is a viable therapy for refractory septic shock that is unresponsive to all other conservative treatments (3). However, although successful use of ECMO in adults with refractory septic shock has been reported in a few cases (4–6), reports of ECMO in adults and children with refractory septic shock remain limited. In addition, no study has explored the difference in the use of ECMO in refractory septic shock between adults and children. As a result, the outcome benefits of ECMO in refractory septic shock remain controversial. We aimed to systematically review the literature to examine the survival rates of adult and pediatric patients with refractory septic shock requiring ECMO and to discuss the differences between them.
Methods
This study adhered to the ethical guidelines of the Declaration of Helsinki following the Preferred Reporting Items for Systematic Review and Meta-Analysis statement (7). Publications were reviewed for quality using the Joanna Briggs Institute (JBI) checklist for prevalence studies (8) and the Grading of Recommendations Assessment Development and Evaluation (GRADE) system to determine the overall rating confidence in the body of evidence (9).
Study Selection
Inclusion criteria: (1) study design: the study was original research from prospective or retrospective studies; (2) participants: adults and children; (3) exposure: refractory septic shock treated with ECMO; (4) comparator: survival at discharge; and (5) outcome: death or survival. Exclusion criteria: the review, commentaries, opinions, guidelines, pathological studies. Two investigators independently searched PubMed, Embase, and Cochrane Library databases for studies that enrolled patients with refractory septic shock treated with ECMO, which were published before July 9, 2021 and restricted to English. The search phrases for the three databases included Boolean terms “AND” and “OR” with the following keywords in various possible combinations: “ECMO,” “extracorporeal membrane oxygenation,” “Infant,” “newborn,” “neonatal,” “pediatric,” “adults,” and “refractory septic shock” (details of the search strategy are included in the Supplementary Material). Two authors screened titles, abstracts, or full texts and determined their eligibility. In addition, a manual search of all relevant studies and their citation lists was performed to identify additional articles for inclusion. And no restrictions were placed on study type (prospective or retrospective) because we have used the Joanna Briggs Institute Checklist to assess all the studies and put it in the Supplementary Data.
Study Analysis
Meta-analysis was performed using R software. Data including study design, outcomes, patient characteristics, and interventions were extracted independently. Survival to discharge was the outcome measure in our meta-analysis. Subgroup analysis was also performed to analyze the differences between the adult and pediatric groups. Briefly, for the meta-analysis of proportions, the exact confidence interval (CI) for each proportion was computed using the Clopper-Pearson method (10). I2-tests were performed to assess the heterogeneity of the summary rates. Statistical heterogeneity between studies was identified using I2 statistics, where I2 ≤ 40%, between 30 and 60%, between 50 and 75%, and ≥75% indicated low, moderate, substantial, and considerable heterogeneity, respectively. P-values for I2 statistics were derived from the chi-square distribution of Cochran's Q-test.
Results
Study Characteristics
The results of the study selection process are presented in Figure 1. A total of 293 records were found in PubMed, Embase, and the Cochrane Library databases. And we excluded 36 records and 243 irrelevant records (review, commentaries, opinions, guidelines, pathological) in this meta-analysis. After excluding duplicates, irrelevant studies, and studies without corresponding data, we eventually identified 14 studies that met the inclusion criteria.
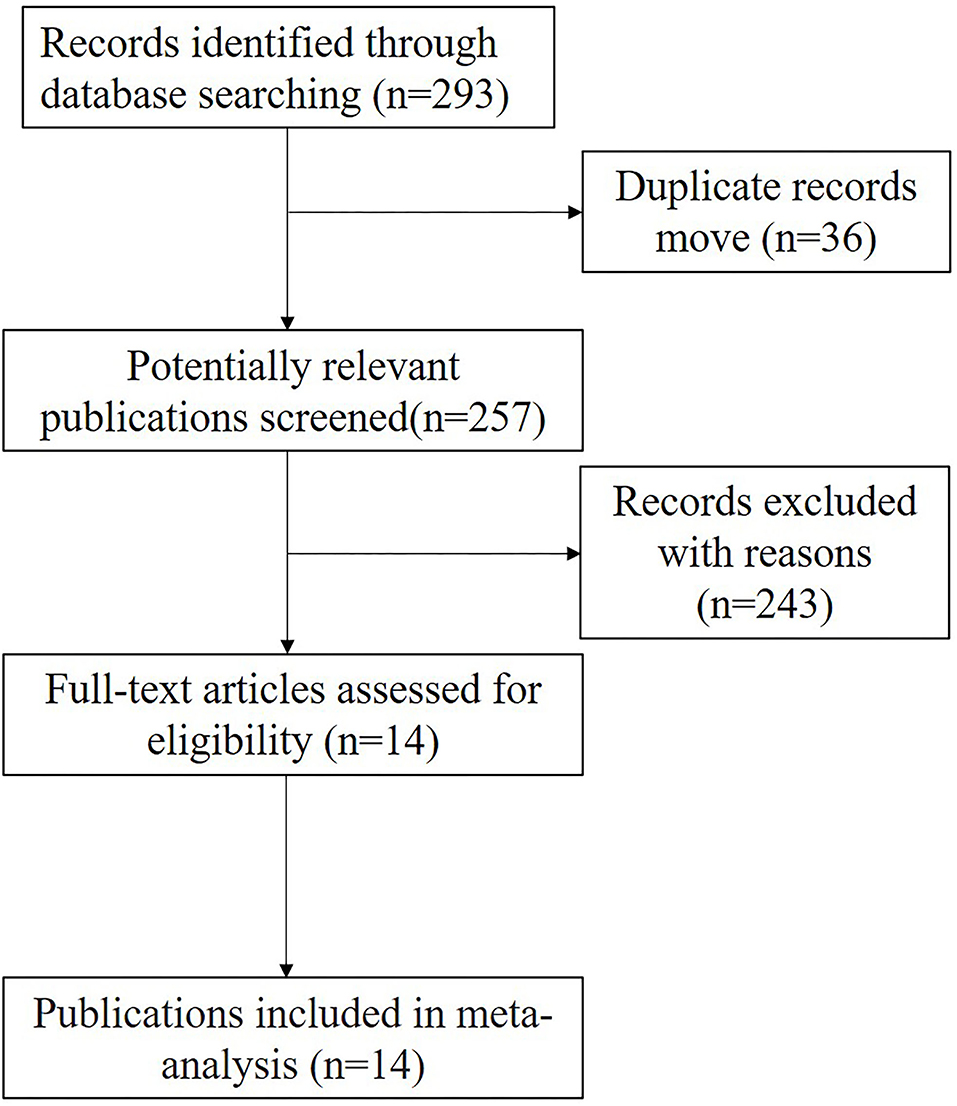
Figure 1. Flow chart showing the process of study selection and numbers of studies included. A total of 293 studies were found in PubMed, Embase, and the Cochrane Library databases. And there were 14 studies included in this meta-analysis.
Clinical Outcomes
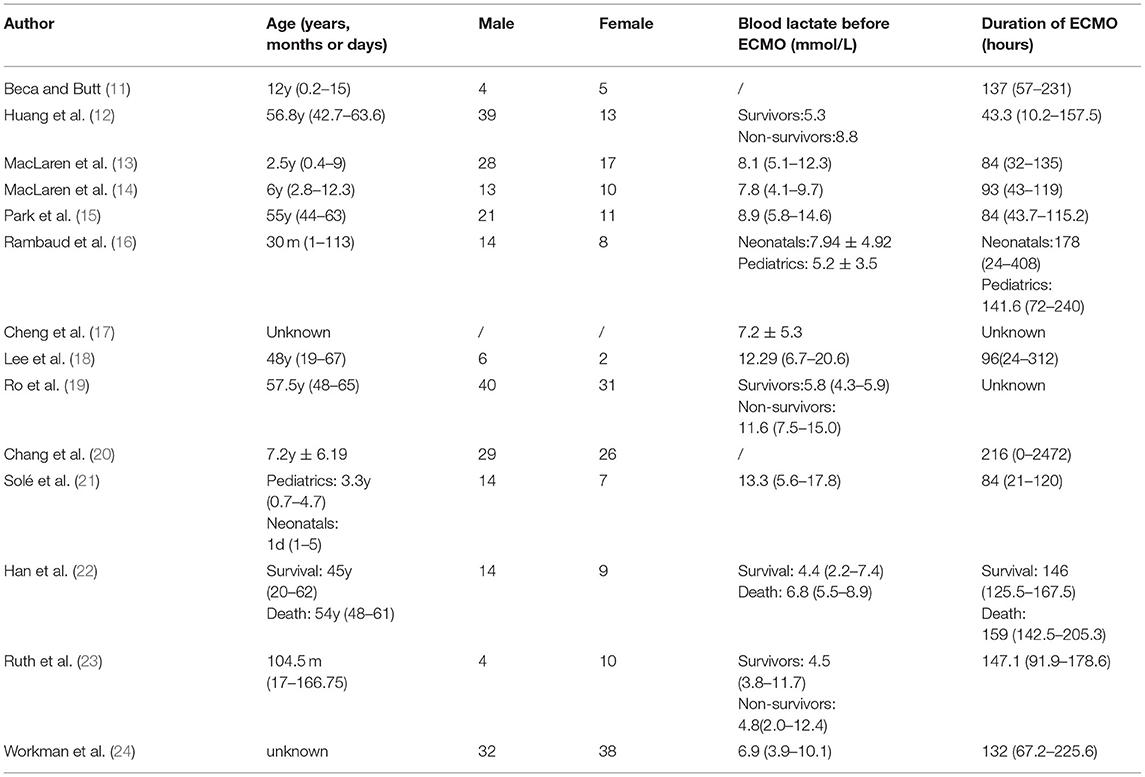
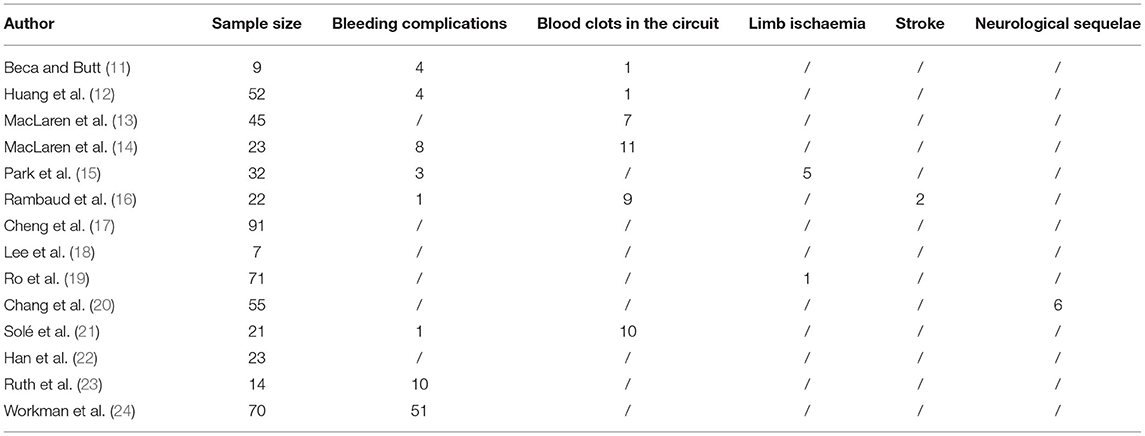
Of the 293 articles screened, 14 were identified for systematic review and meta-analysis. The cumulative estimate of survival (14 studies, 535 patients) in the cohort was 39% (95% CI: 27–51%) (Figure 2). An assessment of the funnel plots of all the patients is shown in Figure 3. The 14 studies included in the systemic review and meta-analysis that reported on children with refractory septic shock requiring ECMO are shown in Table 1 (11–24). And the details of the cohort studies are summarized in Table 2. Furthermore, the compilation of adverse events associated with the use of ECMO are provided in Table 3.
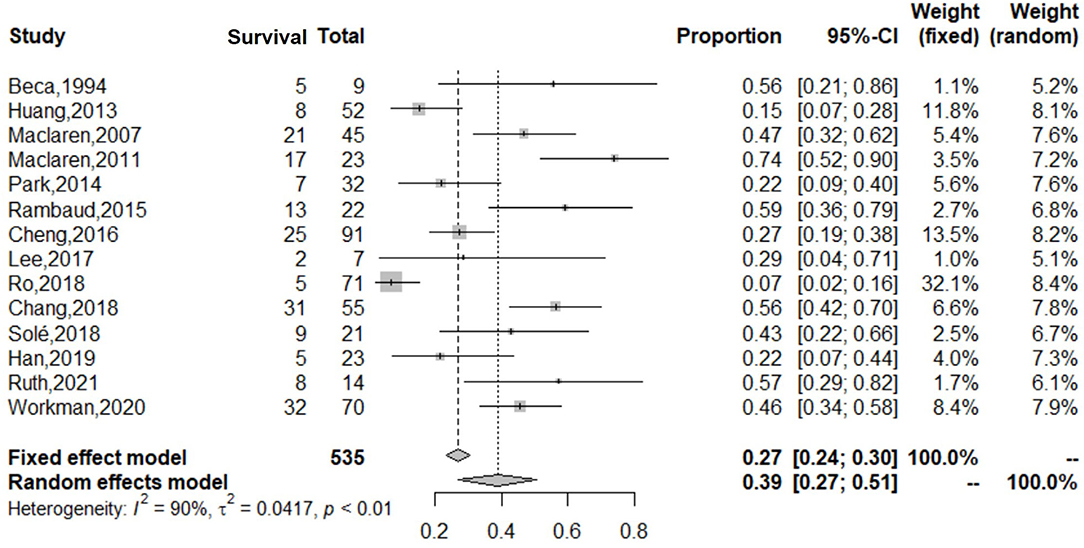
Figure 2. Forest plot of studies reporting on use of ECMO in both adults and children with refractory septic shock. The cumulative estimate of survival (14 studies, 535 patients) in the cohort was 39% (95% CI: 27–51%). CI, confidence interval.
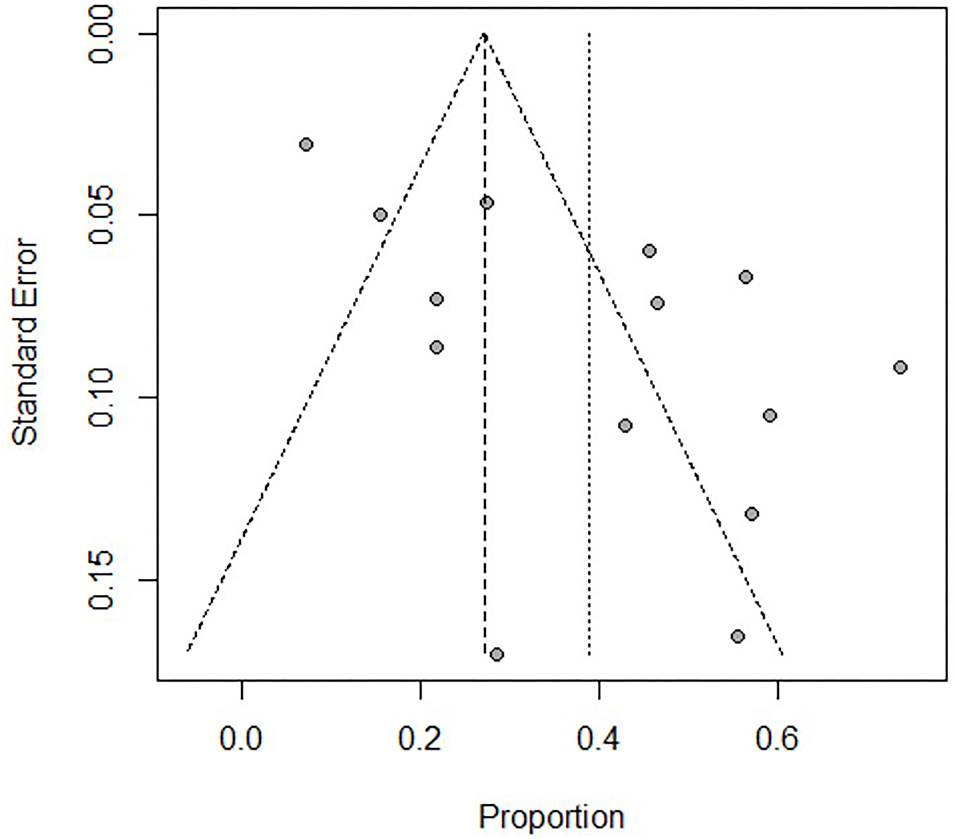
Figure 3. Assessment of the funnel plot of both adults and children with refractory septic shock treated with ECMO. It shows that the heterogeneity is great before dividing into subgroups.
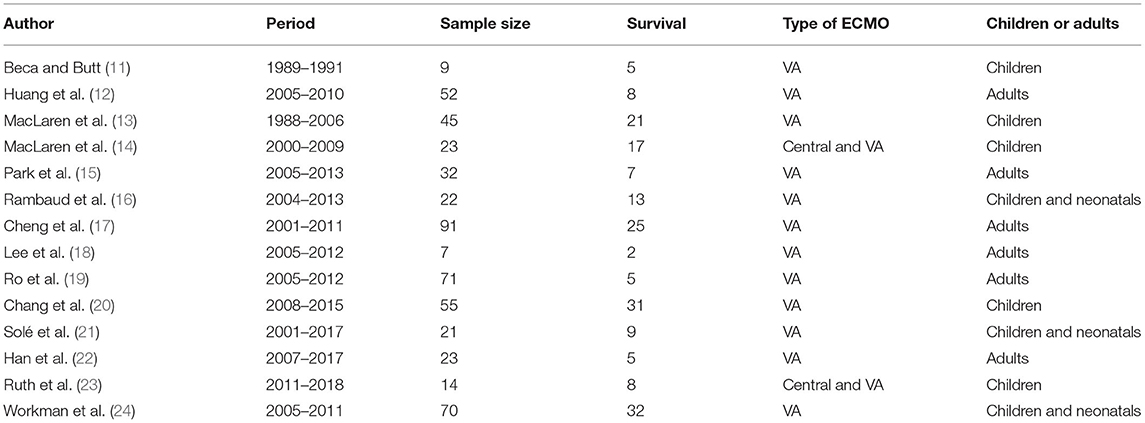
Table 1. List of 13 articles included in systemic review and meta-analysis that reported on patients with refractory septic shock needing ECMO.
Subgroup Analysis
During the subgroup analysis, the cumulative estimate of survival in the adult group (6 studies, 276 patients) in the cohort was 18% (95% CI: 10–27%) (Figure 4), and an assessment of the funnel plot of adults is shown in Figure 5. The cumulative estimate of survival in the pediatric group (8 studies, 259 patients) in the cohort was 53% (95% CI: 47–59%) (Figure 6), and the assessment of the funnel plot of children is shown in Figure 7.
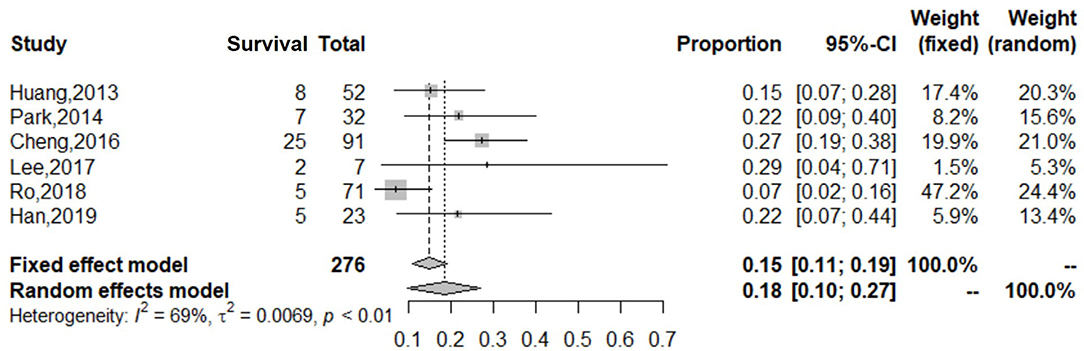
Figure 4. Forest plot of studies reporting on use of ECMO in adults with refractory septic shock. The cumulative estimate of survival in the adult group (6 studies, 276 patients) in the cohort was 18% (95% CI: 10–27%). CI, confidence interval.
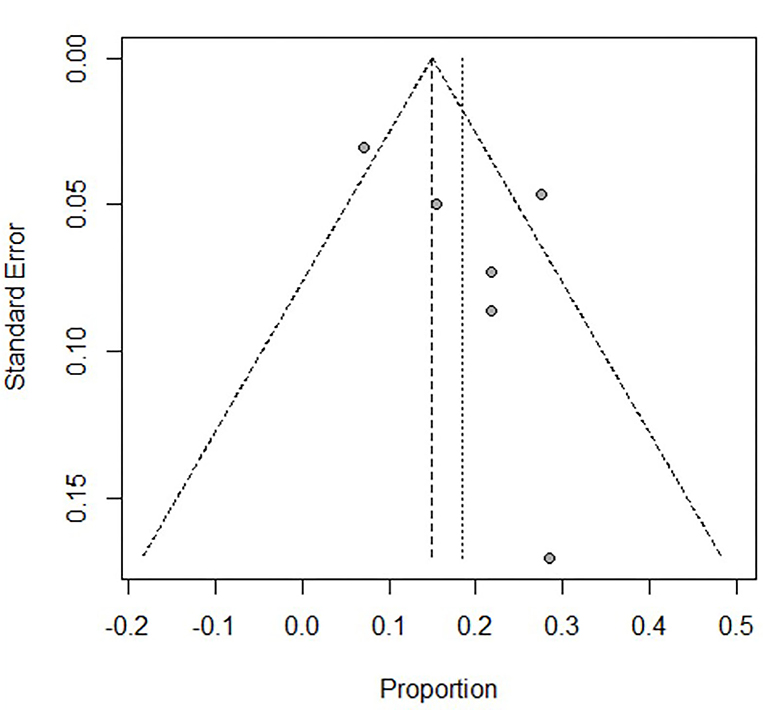
Figure 5. Assessment of the funnel plot of adults with refractory septic shock treated with ECMO. The heterogeneity in the funnel plots of adults was lower than after dividing into subgroups.
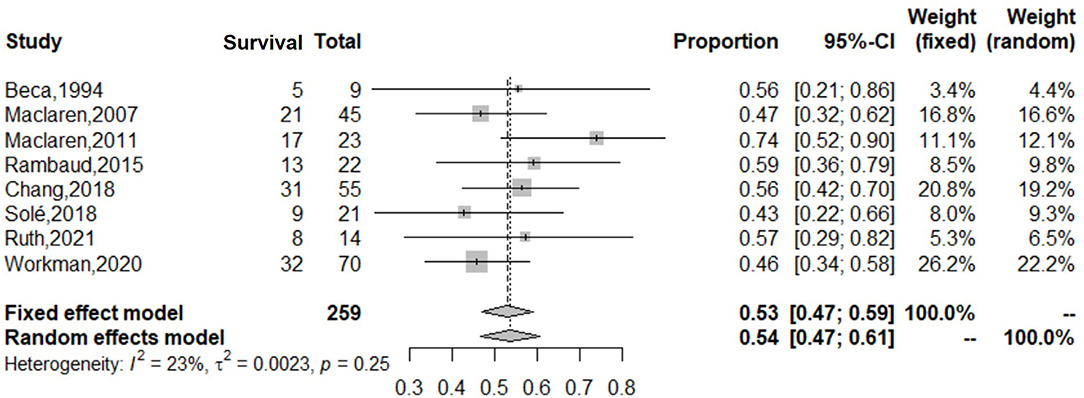
Figure 6. Forest plot of studies reporting on use of ECMO in children with refractory septic shock. The cumulative estimate of survival in the pediatric group (8 studies, 259 patients) in the cohort was 53% (95% CI: 47–59%). CI, confidence interval.
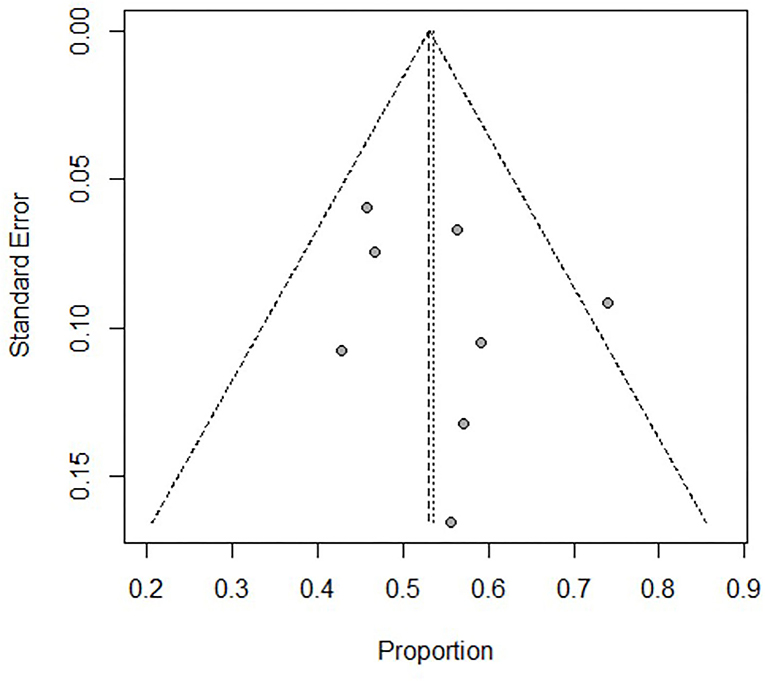
Figure 7. Assessment of the funnel plot of children with refractory septic shock treated with ECMO. The heterogeneity in the funnel plots of children was lower than after dividing into subgroups.
Quality Assessment
There was no evidence of publication bias, and the methodological quality of all the studies included in our analysis scored high using the JBI critical appraisal tool (Supplementary Table 1). The GRADE analysis demonstrated moderate to high certainty in the evidence presented in this paper.
Discussion
The application of ECMO in patients with refractory septic shock has increased over the past decade, with variable survival rates (25, 26). Our meta-analysis of observational studies showed that the overall survival rate of patients (adults and children) with refractory septic shock treated with ECMO was 39%, while in the subgroup analysis, the cumulative estimate of survival in the adult group (6 studies, 276 patients) in the cohort was 18% (95% CI: 11–19%), and that in the pediatric group (8 studies, 259 patients) in the cohort was 53% (95% CI: 47–59%). The benefits of extracorporeal support include improved global oxygen delivery, reduced intrathoracic pressures from reduced mechanical ventilatory requirements, improved carbon dioxide clearance and acid-base management, and improved myocardial performance (27).
Subgroup Analysis
There was great heterogeneity in the forest and funnels plots of all patients (Figures 2, 3). Consequently, we selected the random-effects model to assess the overall survival rate of patients treated with ECMO, which was 39%. We divided the patients into two subgroups: adults, and children and neonates.
The adult group with refractory septic shock treated with ECMO had significantly lower survival rates (18%) than pediatric group. In addition, the heterogeneity in the forest and funnel plots of adults was lower than that of the overall patients (Figures 4, 5). The pediatric and neonate group with refractory septic shock treated with ECMO had significantly higher survival rates than the adult groups. In addition, the heterogeneity in the forest and funnel plots of pediatrics was lower than that of the overall patients (Figures 6, 7). This indicates that our subgroup analysis is of great significance in reducing heterogeneity.
Huang et al. have concluded that for patients with refractory septic shock treated with ECMO, the older the adult, the worse the prognosis. All 20 adults aged over 60 years died despite the use of ECMO, which indicates that the outcomes of these patients remain unsatisfactory. There are three possible explanations for this phenomenon: First, refractory septic shock has a variety of hemodynamic presentations. Left ventricular dysfunction with reduced cardiac output is commonly seen in infants and children; however, distributive shock, a hyperdynamic state with high cardiac output, usually manifests in adults (28). ECMO is used primarily for cardiac or cardiopulmonary support and is intuitively more beneficial for patients with ventricular dysfunction than for those with profound vasodilation. Thus, the performance of ECMO is better in pediatric than adult refractory septic shock. Second, among adults, older patients have more comorbid diseases (such as diabetes and hypertension), which are more difficult to recover from after ECMO for life support. Thus, the adult survival rates declined at discharge. According to our experience, although some children with refractory septic shock who need ECMO in PICU also have chronic comorbidity such as type 1 diabetes, congenital heart disease, chronic lung disease, the incidence rate is lower than that of adults, and the exposed time to chronic diseases is shorter than adults. Third, cardiovascular diseases increase dramatically with age in human. While it is clear that advanced age allows more time for individuals to be exposed to risk factors in general, there is strong evidence that age itself is a major independent risk factor for death (29). These three points may be the cause of the significant differences between the adult and pediatric groups.
Shock-to-Extracorporeal Membrane Oxygenation Interval
Han et al. (22) have reported that the shock-to-ECMO interval for adults at 12, 18, and 24 h during ECMO between the survival and death groups was significantly different. They found that shock-to-ECMO interval before ECMO placement in the survival group were significantly lower than those in the death group (23.5 vs. 42.2 h, P = 0.037). Cheng et al. (17) have found that better outcomes were associated with in ECMO patients with door-to-ECMO times of 96 h or less. Solé et al. (21) have reported 21 refractory septic shock patients treated with ECMO, 9 were pediatric and 12 were newborns. And they were diagnosed with septic shock for a median duration of 29.5 h before ECMO was started (IQR, 20–46), with significant differences between the survival and non-survival groups (P = 0.009). These three studies indicate that the shorter the time from refractory septic shock to ECMO, the higher the survival rate at discharge.
Study Limitations
First, this study lacked long-term survival rate for patients with refractory septic shock treated with ECMO; however, ECMO is a supportive method, not a treatment. The most important points in patient management are the control of the focus of infection and the early initiation of adequate antibiotics. Second, the number of the cases in some studies included in this meta-analysis are small. Thus, further multicenter studies conducted with larger sample sizes are needed to confirm our findings.
Conclusions
The survival rate of adults with refractory septic shock requiring ECMO was 18%, and children with refractory septic shock requiring ECMO had a higher survival rate (53%) than adults.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
XL: conception and design. ZX: administrative support. YY and JH: provision of study materials or patients. YY and LG: collection and assembly of data and data analysis and interpretation. All authors manuscript writing and final approval of manuscript.
Funding
This work was funded by the Hunan Provincial Science and Technology Department Project (No. 2018SK2135, 2020SK1014-3), the Hunan Provincial Key Laboratory of Emergency Medicine for Children (No. 2018TP1028), and the Hunan Provincial Key Laboratory of Metabolomics in Critical Care Medicine (No. 2017TP1034). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2021.791781/full#supplementary-material
Abbreviations
ECMO, Extracorporeal membrane oxygenation; JBI, Joanna Briggs Institute; GRADE, the Grading of Recommendations Assessment Development and Evaluation; CI, Confidence interval.
References
1. Bréchot N, Hajage D, Kimmoun A, Demiselle J, Agerstrand C, Montero S, et al. Extracorporeal membrane oxygenation use has increased by 433% in adults in the United States from 2006 to 2011. Lancet. (2020) 396:545–52. doi: 10.1016/S0140-6736(20)30733-9
2. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. (2016) 315:801–10. doi: 10.1001/jama.2016.0287
3. Brierley J, Carcillo JA, Choong K, Cornell T, Decaen A, Deymann A, et al. Clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock: 2007 update from the American College of Critical Care Medicine. Crit Care Med. (2009) 37:666–88. doi: 10.1097/CCM.0b013e31819323c6
4. MacLaren G, Pellegrino V, Butt W, Preovolos A, Salamonsen R. Successful use of ECMO in adults with life-threatening infections. Anaesthesia Intensive Care. (2004) 32:707–10. doi: 10.1177/0310057X0403200519
5. Vohra HA, Adamson L, Weeden DF, Haw MP. Use of extracorporeal membrane oxygenation in the management of septic shock with severe cardiac dysfunction after Ravitch procedure. Ann Thorac Surg. (2009) 87:e4–5. doi: 10.1016/j.athoracsur.2008.07.077
6. MacLaren G, Cove M, Kofidis T. Central extracorporeal membrane oxygenation for septic shock in an adult with H1N1 influenza. Ann Thorac Surg. (2010) 90:e34–5. doi: 10.1016/j.athoracsur.2010.06.019
7. Liberati A, Altman DG, Tetzlaf J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. (2009) 339:b2700. doi: 10.1136/bmj.b2700
8. Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manag. (2014) 3:123–8. doi: 10.15171/ijhpm.2014.71
9. Guyatt GH, Oxman AD, Schunemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. (2011) 64:380–2. doi: 10.1016/j.jclinepi.2010.09.011
10. Freeman MF, Tukey JW. Transformations related to the angular and the square root. Ann Math Stat. (1950) 1:607–11. doi: 10.1214/aoms/1177729756
11. Beca J, Butt W. Extracorporeal membrane oxygenation for refractory septic shock in children. Pediatrics. (1994) 93:726–9. doi: 10.1542/peds.93.5.726
12. Huang CT, Tsai YJ, Tsai PR, Ko WJ. Extracorporeal membrane oxygenation resuscitation in adult patients with refractory septic shock. J Thorac Cardiovasc Surg. (2013) 146:1041–6. doi: 10.1016/j.jtcvs.2012.08.022
13. Maclaren G, Butt W, Best D, Donath S, Taylor A. Extracorporeal membrane oxygenation for refractory septic shock in children: one institution's experience. Pediatr Crit Care Med. (2007) 8:447–51. doi: 10.1097/01.PCC.0000282155.25974.8F
14. MacLaren G, Butt W, Best D, Donath S. Central extracorporeal membrane oxygenation for refractory pediatric septic shock. Pediatr Crit Care Med. (2011) 12:133–6. doi: 10.1097/PCC.0b013e3181e2a4a1
15. Park TK, Yang JH, Jeon K, Choi SH, Choi JH, Gwon HC, et al. Extracorporeal membrane oxygenation for refractory septic shock in adults. Eur J Cardio Thorac Surg. (2015) 47:e68–74. doi: 10.1093/ejcts/ezu462
16. Rambaud J, Guellec I, Léger PL, Renolleau S, Guilbert J. Venoarterial extracorporeal membrane oxygenation support for neonatal and pediatric refractory septic shock. Indian J Crit Care Med. (2015) 19:600–5. doi: 10.4103/0972-5229.167038
17. Cheng A, Sun HY, Tsai MS, Ko WJ, Tsai PR, Hu FC, et al. Predictors of survival in adults undergoing extracorporeal membrane oxygenation with severe infections. J Thorac Cardiovasc Surg. (2016) 152:1526–36.e1. doi: 10.1016/j.jtcvs.2016.08.038
18. Lee KW, Cho CW, Lee N, Choi GS, Cho YH, Kim JM, et al. Extracorporeal membrane oxygenation support for refractory septic shock in liver transplantation recipients. Ann Surg Treat Res. (2017) 93:152–8. doi: 10.4174/astr.2017.93.3.152
19. Ro SK, Kim WK, Lim JY, Yoo JS, Hong SB, Kim JB. Extracorporeal life support for adults with refractory septic shock. J Thorac Cardiovasc Surg. (2018) 156:1104–9.e1. doi: 10.1016/j.jtcvs.2018.03.123
20. Chang TH, Wu ET, Lu CY, Huang SC, Yang TI, Wang CC, et al. Pathogens and outcomes in pediatric septic shock patients supported by extracorporeal membrane oxygenation. J Microbiol Immunol Infect. (2018) 51:385–91. doi: 10.1016/j.jmii.2017.07.012
21. Solé A, Jordan I, Bobillo A, Moreno J, Balaguer M, Hernández-Platero L, et al. Venoarterial extracorporeal membrane oxygenation support for neonatal and pediatric refractory septic shock: more than 15 years of learning. Eur J Pediatr. (2018) 177:1191–200. doi: 10.1007/s00431-018-3174-2
22. Han L, Zhang Y, Zhang Y, Wu W, He P. Risk factors for refractory septic shock treated with VA ECMO. Ann Transl Med. (2019) 7:476. doi: 10.21037/atm.2019.08.07
23. Ruth A, Vogel AM, Adachi I, Shekerdemian LS, Bastero P, Thomas JA. Central venoarterial extracorporeal life support in pediatric refractory septic shock: a single center experience. Perfusion. (2021). doi: 10.1177/02676591211001782. [Epub ahead of print].
24. Workman JK, Bailly DK, Reeder RW, Dalton HJ, Berg RA, Shanley TP, et al. Risk factors for mortality in refractory pediatric septic shock supported with extracorporeal life support. ASAIO J. (2020) 66:1152–60. doi: 10.1097/MAT.0000000000001147
25. Ramanathan K, Yeo N, Alexander P, Raman L, Barbaro R, Tan CS, et al. Role of extracorporeal membrane oxygenation in children with sepsis: a systematic review and meta-analysis. Crit Care. (2020) 24:684. doi: 10.1186/s13054-020-03418-z
26. Barbaro RP, Paden ML, Guner YS, Raman L, Ryerson LM, Alexander P, et al. Pediatric extracorporeal life support organization registry international report 2016. ASAIO J. (2017) 63:456–63. doi: 10.1097/MAT.0000000000000603
27. Vogel DJ, Murray J, Czapran AZ, Camporota L, Ioannou N, Meadows CIS, et al. Veno-arerio-venous ECMO for septic cardiomyopathy: a single-centre experience. Perfusion. (2018) 33:57–64. doi: 10.1177/0267659118766833
28. Maclaren G, Butt W. Extracorporeal membrane oxygenation and sepsis. Crit Care Resusc. (2007) 9:76–80.
Keywords: children, refractory septic shock, extracorporeal membrane oxygenation, adults, survival
Citation: Yang Y, Xiao Z, Huang J, Gong L and Lu X (2022) Role of Extracorporeal Membrane Oxygenation in Adults and Children With Refractory Septic Shock: A Systematic Review and Meta-Analysis. Front. Pediatr. 9:791781. doi: 10.3389/fped.2021.791781
Received: 09 October 2021; Accepted: 10 December 2021;
Published: 21 January 2022.
Edited by:
Praveen Khilnani, Rainbow Children's Hospital, IndiaReviewed by:
Michael Hermon, Medical University of Vienna, AustriaJerry John Zimmerman, Seattle Children's Hospital, United States
Thomas Vincent Brogan, Seattle Children's Hospital, United States
Copyright © 2022 Yang, Xiao, Huang, Gong and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiulan Lu, 13787252674@163.com
†These authors have contributed equally to this work and share first authorship
 Yufan Yang
Yufan Yang Zhenghui Xiao†
Zhenghui Xiao†