Oxygen-enriched oleic matrix (NovoX) for wound healing in pediatric patients undergoing open surgical treatment for pilonidal disease: Preliminary experience
- 1Division of Pediatric Surgery, Department of Women’s and Children’s Health, University of Padua, Padua, Italy
- 2Municipal Non-Profit Enterprise “Lviv Territorial Medical Union”, Multidisciplinary Clinical Hospital of Emergency and Intensive Care - Separated Division “Hospital of Saint Nicolaus”, Danylo Halytsky Lviv National Medical University, Lviv, Ukraine
- 3Department of Pediatric Surgery and Urology, Institute of Maternal and Child Health - IRCCS “Burlo Garofolo”, Trieste, Italy
- 4Chief of Surgical Department, Institute for Maternal and Child Health - IRCCS “Burlo Garofolo”, Trieste, Italy
Introduction: Pilonidal disease (PD) is a common infectious and inflammatory condition affecting the gluteal cleft and sacrococcygeal region. The optimal treatment for PD remains controversial. While the open technique reduces the number of relapses compared to minimally invasive approaches, it is associated with a longer healing time. Reactive oxygen species are a key part of the normal wound-healing process. Herein, we reported our preliminary experience using a new oxygen-enriched oil-based product called NovoX for wound healing after open surgery for PD.
Materials and methods: We used a new oxygen-enriched product for wound healing in three pediatric patients undergoing open surgical repair for PD between December 2021 and April 2022. During postoperative follow-up, healing time and the aesthetic result were evaluated.
Results: Our preliminary study included three patients with chronic PD. The average follow-up time was 5 weeks, corresponding to the end of the healing process and the resumption of normal daily activities. Only one mild complication occurred during the study period. No short-term side effects were reported. The cosmetic result was reported as satisfactory.
Conclusion: NovoX is easy to apply, safe, and effective for treating pediatric patients undergoing open surgical treatment for PD, leading to slightly faster wound healing with good aesthetic outcomes.
Introduction
Pilonidal disease (PD) is a condition that typically affects the gluteal cleft and sacrococcygeal region in adolescents and young adults. While the pilonidal condition spectrum in children includes pilonidal cysts, abscesses, pits, and sinuses, PD is commonly characterized by sacrococcygeal abscesses that form due to a chronic inflammatory response to hair follicle retention in the intergluteal subcutaneous tissue. PD occurs more frequently in male patients. Pain, bleeding, and recurrent secretions are the most representative symptoms of acute disease, often requiring several interventions and negatively impacting patients’ quality of life. PD treatment remains controversial, with many surgical techniques having different success rates and no agreed-upon gold standard approach (1–3).
Innovative medical devices have been developed for use in postoperative wound healing management. Numerous lines of evidence show that wound healing is impaired in hypoxic conditions and that reactive oxygen species (ROS) are a key component of the normal wound-healing response. Recently, a new oxygen-enriched oil-based product called NovoX (Moss SpA; Lesa, Novara, Italy) was shown to create a local microenvironment unfavorable to pathogen growth and to promote the healing of deep and narrow wounds, including those secondary to surgical procedures. NovoX is an approved class IIb Medical Device in the European Union, which is on the market since 2011 and is currently CE marked according to the EU Regulation 2017/745 (MDR) (4–6).
Herein, we describe our preliminary experience using NovoX for wound healing in pediatric patients undergoing open surgery for PD.
Materials and methods
Patients referred to our Pediatric Surgical Center between December 2021 and April 2022 for PD were evaluated for inclusion in this study. Surgical procedures were performed by three different experienced surgeons as follows. Under general anesthesia and prone position, routine skin preparation was performed, and sterile drapes were placed after a few minutes according to our safe surgery guidelines. Methylene blue was initially injected in the fistulous orifices to define disease spread. Therefore, the pathologic tissue is removed en bloc with a diamond-shaped incision downward to the fascia underneath. The wound is partially closed with interrupted resorbable sutures or kept completely open and medicated. All patients enrolled were medicated with NovoX directly applied to the wound and covered with a hyaluronic acid gauze. Follow-up evaluations were scheduled with the surgeon who performed the procedure. Our follow-up protocol included a weekly outpatient evaluation for the first 2 months. During each visit, the surgeon accurately examined the wound, evaluating the healing process and documenting possible complications and cosmetic results with photographs.
Results
Three patients with chronic PD were enrolled in this preliminary study. They comprised two males and one female with a median age at surgery of 16.3 years. Two patients suffered from severe obesity with an average weight and body mass index of 107.3 and 35.3, respectively. One patient presented with a history of suppurative hidradenitis and Hashimoto's thyroiditis. Another patient suffered from IperIgD disease, insipid diabetes, and mevalonate kinase deficiency. In all cases, a recurrent pilonidal sinus disease was described. One patient required a pilonidal abscess incision 3 months before surgical treatment, while the other two patients were treated with antibiotic therapy before surgery.
All patients underwent definitive surgical excision of a pilonidal cyst using the open surgical technique. Surgery length ranged from 30 to 85 min. The wound was partially closed in one patient with interrupted stitches in resorbable material. The wound was kept totally open in the other two cases. No intraoperative complications were described. Two cases were medicated with NovoX gel and hyaluronic acid gauze. In the last patient, NovoX roll and hyaluronic acid gauze were used immediately after the operation and then replaced with NovoX gel (Figure 1). Their median hospitalization period was 1.6 days.

Figure 1. Close-up views of our three patients’ surgical wounds immediately after open midline treatment of chronic PD. NovoX was applied directly inside the wounds.
No patients were lost during follow-up at our Outpatient Clinic. No adverse skin reactions or allergies to the product occurred. One case experienced postoperative hyperemia of the skin close to the surgical wound, which was treated with topical ointments. The median time of follow-up was 5 weeks post-surgery (Figure 2). No patients had any physical limitations postoperatively. Six months after the surgery, no recurrence occurred, and all patients reported high satisfaction regarding the cosmetic result (Figure 3).
Discussion
PD is a common condition affecting adolescents and young adults. Its pathogenesis involves skin injury by the hair follicles, causing a foreign body reaction leading to the formation of an abscess or edema. Its known risk factors include familiarity, repeated local traumatism, sedentary life, and obesity (1, 7). Data on best practices for managing PD without surgery are severely lacking. The only near-universal consensus about PD management is the necessity of incision and drainage of pilonidal abscess as primary treatment. However, recurrence rates after incision and drainage remain high (2, 8). Notably, hygiene and hair removal from the natal cleft and surrounding area plays a crucial role in managing patients with PD and form the cornerstone of almost all care approaches (1, 2, 9).
PD treatment options include phenol or fibrin glue instillation into pits (2, 10), using laser probes to induce tract obliteration (11), subcutaneous tissue radiofrequency ablation (12), classical or minimally invasive sinusectomy (2, 13), endoscopic pilonidal sinus treatment or video-assisted pilonidal sinus ablation (2, 4, 14), and en bloc removal of affected tissue followed by primary closure or healing by secondary intention or flap coverage in cases of chronic or multiply recurrent PD (2, 15–18). Removal of affected tissue with en bloc resection followed either by primary closure or healing by secondary intention has been the most common definitive surgical PD treatment for decades. However, it is associated with longer healing times and greater pain and disability than less radical procedures.
Several studies reported that minimally invasive techniques might represent the optimal choice for treating PD in the pediatric setting, mainly due to their lower impact on daily activities in the postoperative period compared to open approaches (2, 15). Open surgery remains the treatment preferred in patients with recurrent or chronic PD. However, open healing has a higher recurrence risk (∼26%) and wound healing time (38–92 days) than off-midline primary closure, minimally invasive approaches, or other surgical techniques. No clear advantage has been shown for open healing over primary closure. In addition, when primary closure is the desired surgical option, off-midline closure should be recommended (3, 19). At our institution, we opt for a midline or off-midline wide excision of the pathologic tissue (depending on the singular case) and totally or partially open healing by secondary intention.
ROS play a key role in wound healing. They are secondary messenger-signaling molecules promoting immunocyte recruitment to the wound site and effective tissue repair. They also have a bacteriostatic effect by inhibiting the growth of adjacent contaminating bacteria and play a major role in angiogenesis by stimulating endothelial cell and keratinocyte proliferation and migration. Finally, they accelerate wound healing by promoting collagen synthesis and fibroblast division and migration (20, 21).
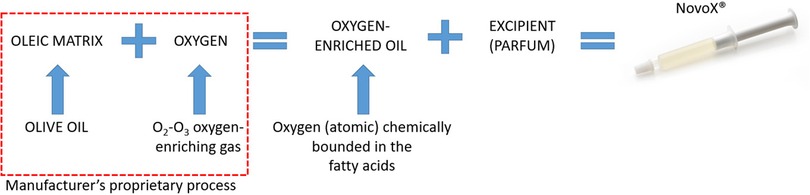
NovoX is a new oxygen-enriched oil-based product claimed to create a local wound microenvironment unfavorable to pathogen growth. In particular, NovoX's oxygen-enriched oleic matrix (organic extra virgin olive oil) enables the stable and prolonged release of limited ROS amounts and has filmogenic, protective, and barrier actions (Figure 4) (22–24). Notably, it has recently shown encouraging results in treating ulcers, skin lesions, wound dehiscences, and surgical wounds. Interestingly, since the device's effectiveness is prolonged, it only needs to be changed 2–3 times per week (4, 6, 25). Therefore, we tested this new oxygen-enriched oil-based product in a preliminary study on pediatric patients undergoing wound healing by secondary intention after midline open surgery for PD.
Conclusion
Our experience suggests that this new oxygen-enriched oil-based product (NovoX) is easy to apply, safe, and effective for treating pediatric patients undergoing surgical treatment for chronic PD. In particular, it appears to confer slightly faster wound healing with good aesthetic outcomes in patients treated via open surgery followed by healing by secondary intention. Further studies with larger sample sizes are highly encouraged to confirm our preliminary results.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
Conceptualization: M-GS, EG, JS, and AB. Methodology: M-GS, EG, and AB. Investigation: MB and ST. Data curation: MB, ST, CP, and AB. Formal analysis: CP, DC, and AB. Validation: DO, DC, and JS. Writing—original draft preparation: MB, ST, CP, and DO. Writing—review and editing: EG, DC, and AB. Supervision: JS. This work has not been published previously and is not under consideration for publication elsewhere. All the authors approved the final version of the manuscript and attest that they meet the ICMJE criteria for authorship.
Funding
This work was supported by the Ministry of Health, Rome - Italy, in collaboration with the Institute for Maternal and Child Health IRCCS Burlo Garofolo, Trieste - Italy.
Acknowledgments
We thank Moss SpA (Lesa, Novara, Italy) for their kind permission to use the figure representing components and manufacturing process of NovoX Medical Device in this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
PD, pilonidal disease; ROS, reactive oxygen species.
References
1. Collings AT, Rymeski B. Updates on the management of pilonidal disease. Adv Pediatr. (2022) 69(1):231–41. doi: 10.1016/j.yapd.2022.03.001
2. Grabowski J, Oyetunji TA, Goldin AB, Baird R, Gosain A, Lal DR, et al. The management of pilonidal disease: a systematic review. J Pediatr Surg. (2019) 54(11):2210–21. doi: 10.1016/j.jpedsurg.2019.02.055
3. Hardy EJO, Herrod PJ, Doleman B, Phillips HG, Ranat R, Lund JN. Surgical interventions for the treatment of sacrococcygeal pilonidal sinus disease in children: a systematic review and meta-analysis. J Pediatr Surg. (2019) 54(11):2222–33. doi: 10.1016/j.jpedsurg.2019.02.058
4. Esposito C, Mendoza-Sagaon M, Del Conte F, Cerulo M, Coppola V, Esposito G, et al. Pediatric endoscopic pilonidal sinus treatment (PEPSiT) in children with pilonidal sinus disease: tips and tricks and new structurated protocol. Front Pediatr. (2020) 8:345. doi: 10.3389/fped.2020.00345
5. Cipriani F, Lucattelli E, De Rosa M, Di Lonardo A. Effectiveness of reactive oxygen species in an oil-based medication for healing burn wounds: a case series. Ann Burns Fire Disasters. (2021) 34(2):170–4. PMID: 34584506
6. Santorelli A, Bernini M, Orzalesi L, Avvedimento S, Palumbo P, Kothari A, et al. Treatment with oxygen-enriched olive oil improves healing parameters following augmentation-mastopexy. Aesthet Surg J Open Forum. (2021) 3(3):ojab016. doi: 10.1093/asjof/ojab016
7. Harlak A, Mentes O, Kilic S, Coskun K, Duman K, Yilmaz F. Sacrococcygeal pilonidal disease: analysis of previously proposed risk factors. Clinics. (2010) 65(2):125–31. doi: 10.1590/S1807-59322010000200002
8. Vahedian J, Nabavizadeh F, Nakhaee N, Vahedian M, Sadeghpour A. Comparison between drainage and curettage in the treatment of acute pilonidal abscess. Saudi Med J. (2005) 26(4):553–5. PMID: 15900358
9. Lukish JR, Kindelan T, Marmon LM, Pennington M, Norwood C. Laser epilation is a safe and effective therapy for teenagers with pilonidal disease. J Pediatr Surg. (2009) 44(1):282–5. doi: 10.1016/j.jpedsurg.2008.10.057
10. Yuksel ME. Pilonidal sinus disease can be treated with crystallized phenol using a simple three-step technique. Acta Dermatovenerol Alp Pannonica Adriat. (2017) 26(1):15–7. doi: 10.15570/actaapa.2017.4
11. Dessily M, Charara F, Ralea S, Allé JL. Pilonidal sinus destruction with a radial laser probe: technique and first Belgian experience. Acta Chir Belg. (2017) 117(3):164–8. doi: 10.1080/00015458.2016.1272285
12. Gupta PJ. A randomized study between excision and marsupialization and radiofrequency sinus excision in sacro-coccygeal pilonidal disease. Curr Surg. (2004) 61(3):307–12. doi: 10.1016/j.cursur.2003.11.015
13. Kallis MP, Maloney C, Lipskar AM. Management of pilonidal disease. Curr Opin Pediatr. (2018) 30(3):411–6. doi: 10.1097/MOP.0000000000000628
14. Milone M, Fernandez LM, Musella M, Milone F. Safety and efficacy of minimally invasive video-assisted ablation of pilonidal sinus: a randomized clinical trial. JAMA Surg. (2016) 151(6):547–53. doi: 10.1001/jamasurg.2015.5233
15. Iesalnieks I, Ommer A, Petersen S, Doll D, Herold A. German national guideline on the management of pilonidal disease. Langenbecks Arch Surg. (2016) 401(5):599–609. doi: 10.1007/s00423-016-1463-7
16. Sit M, Aktas G, Yilmaz EE. Comparison of the three surgical flap techniques in pilonidal sinus surgery. Am Surg. (2013) 79(12):1263–8. doi: 10.1177/000313481307901217
17. Ersoy E, Devay AO, Aktimur R, Doganay B, Ozdoğan M, Gündoğdu RH. Comparison of the short-term results after limberg and karydakis procedures for pilonidal disease: randomized prospective analysis of 100 patients. Colorectal Dis. (2009) 11(7):705–10. doi: 10.1111/j.1463-1318.2008.01646.x
18. Guner A, Boz A, Ozkan OF, Ileli O, Kece C, Reis E. Limberg flap versus bascom cleft lift techniques for sacrococcygeal pilonidal sinus: prospective, randomized trial. World J Surg. (2013) 37(9):2074–80. doi: 10.1007/s00268-013-2111-9
19. Al-Khamis A, McCallum I, King PM, Bruce J. Healing by primary versus secondary intention after surgical treatment for pilonidal sinus. Cochrane Database Syst Rev. (2010) 2010(1):CD006213. doi: 10.1002/14651858.CD006213.pub3
20. Schreml S, Szeimies RM, Prantl L, Karrer S, Landthaler M, Babilas P. Oxygen in acute and chronic wound healing. Br J Dermatol. (2010) 163(2):257–68. doi: 10.1111/j.1365-2133.2010.09804.x
21. Dunnill C, Patton T, Brennan J, Barrett J, Dryden M, Cooke J, et al. Reactive oxygen species (ROS) and wound healing: the functional role of ROS and emerging ROS-modulating technologies for augmentation of the healing process. Int Wound J. (2017) 14(1):89–96. doi: 10.1111/iwj.12557
22. Bennison LR, Miller CN, Summers RJ, Minnis AMB, Sussman G, McGuiness W. The pH of wounds during healing and infection: a descriptive literature review. Wound Pract Res. (2017) 25(2):63–9.
23. Milne SD, Connolly P. The influence of different dressings on the pH of the wound environment. J Wound Care. (2014) 23(2):53–4; 56–7. doi: 10.12968/jowc.2014.23.2.53
24. Jones EM, Cochrane CA, Percival SL. The effect of pH on the extracellular matrix and biofilms. Adv Wound Care. (2015) 4(7):431–9. doi: 10.1089/wound.2014.0538
Keywords: sinus pilonidalis, children, post operative treatment, oxygen enrichment therapy, wound healing
Citation: Bisol M, Tykhomyrova S, Pagliara C, Scarpa M, Guida E, Olenik D, Codrich D, Schleef J and Boscarelli A (2022) Oxygen-enriched oleic matrix (NovoX) for wound healing in pediatric patients undergoing open surgical treatment for pilonidal disease: Preliminary experience. Front. Pediatr. 10:1068280. doi: 10.3389/fped.2022.1068280
Received: 12 October 2022; Accepted: 14 November 2022;
Published: 25 November 2022.
Edited by:
Satoshi Ieiri, Kagoshima University, JapanReviewed by:
Sherif Mohamed Shehata, Tanta University, EgyptAntonino Morabito, University of Florence, Italy
© 2022 Bisol, Tykhomyrova, Pagliara, Scarpa, Guida, Olenik, Codrich, Schleef and Boscarelli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alessandro Boscarelli tboscar@hotmail.it
†ORCID Edoardo Guida orcid.org/0000-0003-4901-2515 Damiana Olenik orcid.org/0000-0003-4901-2515 Daniela Codrich orcid.org/0000-0003-2925-8876 Jürgen Schleef orcid.org/0000-0001-9754-2479 Alessandro Boscarelli orcid.org/0000-0003-1934-1764
Specialty Section: This article was submitted to Pediatric Surgery, a section of the journal Frontiers in Pediatrics
 Marta Bisol1
Marta Bisol1  Sophia Tykhomyrova
Sophia Tykhomyrova Maria-Grazia Scarpa
Maria-Grazia Scarpa Daniela Codrich
Daniela Codrich Alessandro Boscarelli
Alessandro Boscarelli