Patterns, Outcomes and Predictors of Pediatric Medical Admissions at Gadarif Hospital in Eastern Sudan
- 1Faculty of Medicine, Gadarif University, Gadarif, Sudan
- 2Department of Medicine, Royal Commission Hospital in Al Jubail Industrial City, Al Jubail, Saudi Arabia
- 3Department of Pediatrics, Unaizah College of Medicine and Medical Sciences, Qassim University, Unaizah, Saudi Arabia
- 4Department of Family and Community Medicine, Unaizah College of Medicine and Medical Sciences, Qassim University, Unaizah, Saudi Arabia
- 5Department of Obstetrics and Gynecology, Unaizah College of Medicine and Medical Sciences, Qassim University, Unaizah, Saudi Arabia
Background: The reduction of childhood mortality is a reliable indicator of a national health system's progress and improvement. Sudan's population is still suffering from communicable diseases, with a considerably higher mortality rate among children. Efforts are therefore needed to reduce mortality and achieve the Millennium Development Goals and Sustainable Development Goals. This study was conducted to determine the morbidity, mortality and outcomes of children admitted to Gadarif Hospital in eastern Sudan.
Method: A retrospective study was conducted by reviewing the medical files of pediatric patients who were admitted to Gadarif Hospital between March 1, 2019 and March 31, 2020.
Result: A total of 740 medical files were reviewed. Most, 453 (61.2%) of the admissions were males. The median (interquartile range) age was 3.0 (8.0) years and 433 (58.8%) of the admissions were under 5 years of age. The median (interquartile range) of the length of hospital stay was 9.0 (12.0) days. Visceral leishmaniasis, malnutrition, severe malaria, sickle cell disease, acute watery diarrhea, severe anemia (regardless of its cause), septicemia and acute respiratory infection were the most common causes of admission. The mortality rate was 5.7%, and it was significantly higher in females than males [24/287 (8.4%) vs. 18/453 (4.0%), P = 0.01] and in children under 5 years [36/433 (8.3%) vs. 6/307 (2.0%), P < 0.001]. Malnutrition, visceral leishmaniasis, septicemia and meningitis/encephalitis were the main diseases causing death in the study population. The case fatality rate was not significantly different in malnutrition than in visceral leishmaniasis [9/93 (9.7%) vs. 7/178 (3.9%), P = 0.05].
Conclusion: The main causes of morbidity and mortality for children admitted to Gadarif Pediatric Hospital were communicable diseases. The mortality rate was 5.7%. Females and children under 5 years were the most vulnerable groups for fatality.
Introduction
Childhood mortality is an essential indicator to monitor child health. Mortality indicators are still considered a starting point for health status evaluation even after marked declines in mortality rates (1). Child morbidity and hospital admission are considered financial burdens to governments, health systems, and parents (2). In Africa, infections and communicable diseases are the leading causes of childhood morbidity and mortality (3). Despite the shift in the causes of mortality toward non-communicable diseases, communicable diseases remain the major causes of mortality and morbidity in middle- and low-income countries (4). Unlike the developed countries, where mortality from non-communicable diseases is escalating (5), in Sub-Saharan Africa, childhood mortality is mainly due to preventable communicable diseases (6, 7). Moreover, pediatric sepsis is a leading cause of hospital admission, with an increased risk of fatality in the African countries, including Sudan (8–10). Therefore, more research is needed to address mortality in children aged 5–9 years and in young adolescents. The World Health Organization (WHO) has reported that preventable diseases, such as respiratory tract infections, diarrheal diseases, and meningitis are responsible for about one million deaths in older children and young adolescents (11). Hence, further efforts are required to evaluate morbidities and mortalities in these age groups in order to improve outcomes. Previous studies have reported a significant variation in the leading causes of mortality between regions, gender, and age groups (4, 12). Most countries have very little information on mortality and general health conditions and, hence, it is of paramount importance to study the mortality conditions in these poor countries. There is a high rate (58.4 deaths per 1,000 live births) of childhood mortality in Sudan (13), which is one of the “least developed” countries in Africa. This study aimed to determine the patterns of morbidity and mortality and their predictors among children admitted to Gadarif Hospital in eastern Sudan.
Materials and Methods
Medical files (paper-based) of the children admitted to Gadarif Pediatric Hospital between March 1, 2019 and March 31, 2020 were retrospectively reviewed. The hospital is a tertiary care facility that serves as a referral center in Gadarif State and is staffed with eight consultants, 10 specialists, and 25 medical doctors (registrars and residents).
Inclusion and Exclusion Criteria
All children (aged between 1 month and 18 years) admitted to the hospital during the study period and with complete medical records were included. We excluded patients with missing information on diagnosis, age, or gender. If the patient was admitted more than once during the period of the study, the last admission was considered.
We followed the systematic random sampling technique to select the medical files to review. According to the hospital records, there were 2,273 medical files during the study period. The sampling interval (≈ 3) was assumed in dividing the all-medical files (2,273) by the calculated sample size (2,273/740 ≈ 3). Thus, the medical files were reviewed every three intervals to arrive at the required sample size (740). The subsequent medical file was taken if the selected file had incomplete data.
A seven-part questionnaire was used to collect the data, as follows: (1) socio-demographic information about the child and their family, their vaccine status, and their ward admission, (2) clinical diagnosis, (3) symptoms and signs, (4) relative investigations, (5) treatment, (6) outcome, and (7) cause of death.
Sample Size
A sample size of 740 medical files of children was calculated based on the reported rate of death (5.6%) in a previous study in Nigeria of children admitted to hospital (3). We assumed that 55 vs. 35% and 85 vs. 65% were the rates of the females and under-fives in children who died and children who survived, respectively. The gender and the rate of under-five children were chosen because the possible difference in these variables might serve as guidance for future interventions. This sample size had an 80% power, with a precision of 5%, assuming that 10% of the files would have incomplete data.
Statistics
The data were analyzed with the SPSS (Statistical Package for the Social Sciences) software, version 22.0. Frequency tables and percentages were generated for all the major variables of interest. The categorical variables were presented as percentages in tables, while comparisons between the variables were done using the Chi Square test. A p-value of <0.05 was considered statistically significant.
Results
A total of 740 children were admitted during the study period. Of these, 287 (38.8%) were female and 453 (61.2%) were male, with a male: female ratio of 1.57:1.
The median (interquartile range) age was 3.0 (8.0) years, and 433 (58.8) were aged <5 years. The median (interquartile range) of the length of hospital stay was 9.0 (12.0) days.
Visceral leishmaniasis, acute severe malnutrition, severe malaria, sickle cell disease, acute watery diarrhea, severe anemia (regardless to its cause), septicaemia and acute respiratory infection were the most common causes of admission (Figure 1).
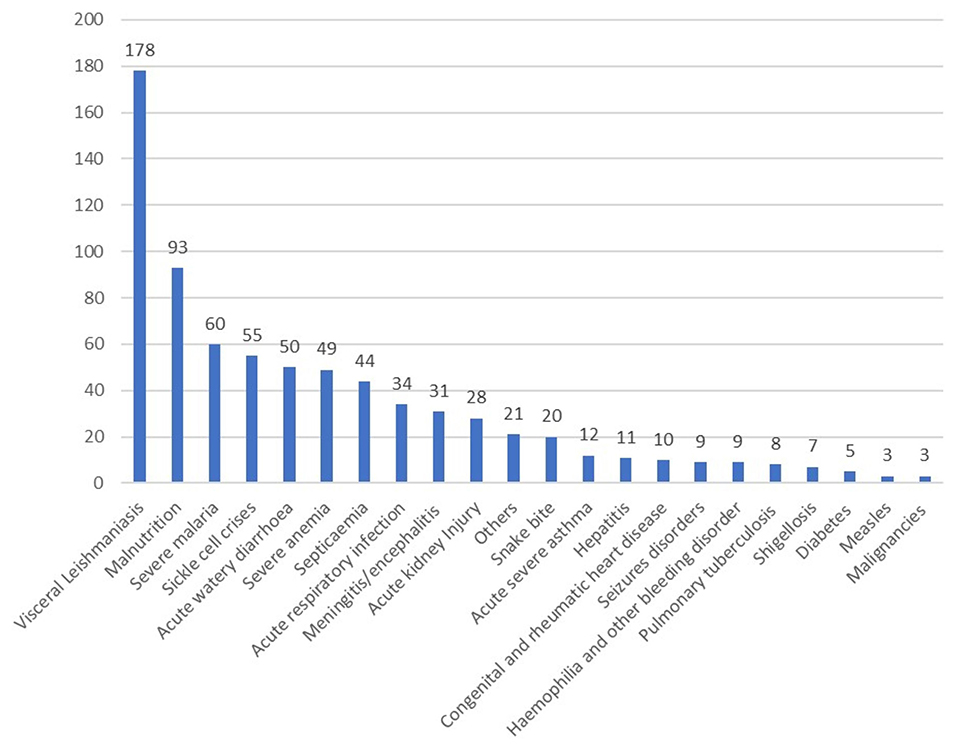
Figure 1. Diagnosis on pediatrics admission in Gadarif Hospital in eastern Sudan in 2020 (number = 740).
Forty-two patients died, resulting in a mortality rate of 5.7%. Forty-three children (5.8%) were discharged against medical advice, 638 (86.2%) were deemed well and discharged and 17 (2.3%) were referred elsewhere. The death rate was significantly higher in females than males [24/287 (8.4%) vs. 18/453 (4.0%), P = 0.01] and in children under five compared to children over five [36/433 (8.3%) vs. 6/307 (2.0%), P < 0.001]. Acute severe malnutrition or its complications, visceral leishmaniasis, septicemia and meningitis/encephalitis were the major diseases causing death in the study population.
The case fatality rate was not significantly different for malnutrition than for visceral leishmaniasis [9/93 (9.7%) vs. 7/178 (3.9%), P = 0.05].
Discussion
The main findings of the current study are that around three-fifths (61.2%) of the admissions were males, visceral leishmaniasis was the leading cause of admissions, and 5.7% of these children died. A similar finding of a higher proportion of male admissions than female admissions has been reported in neighboring Ethiopia (14). This may be explained by the underlying social factors affecting the care-seeking behaviors of family members (15). Moreover, some factors related to pediatrics admission, such as breastfeeding, have been reported to be higher in female infants (20% more likely) than in males (16).
In the current study, visceral leishmaniasis, malnutrition, severe malaria and sickle cell disease were the most common causes of admission. Previous studies have shown that severe anemia, sickle cell disease, malaria and visceral leishmaniasis were the main causes of pediatric morbidity and mortality in eastern Sudan (17, 18) and in other African countries, e.g., Nigeria, Tanzania, and Uganda (3, 19, 20).
The current study documented a mortality rate of 5.7%, similar to what has been observed previously in Sudan (5.8%) (13), as well as in Nigeria (5.7%) (3) and in Liberia (5.4%) (21). The mortality rate of children in the current study was lower than that reported in Ghana (7.12%) (22) but higher than in other African countries, e.g., Ethiopia (0.042%) (14), Malawi (3.3%.) (23), and Nigeria (4.9%) (24). The lower mortality rate in these countries may reflect a marked improvement in pediatric health facilities (14, 23). The mortality rate (8.3%) in children under five in this study was higher than the mortality (7.0%) of children under 5 years of age in Sudan (25). In contrast to this finding, a higher mortality rate (12.5%) was documented in Ethiopia in children under 5 years of age (26). It is worth mentioning that the results of our study should be cautiously compared with the results of the later ones because of the difference in socioeconomic status and other factors.
In the current study, despite the higher rate of admission for males, the death rate was significantly higher in females than in males and in children under five compared to over five, (8.4%) vs. (4.0%) and (8.3%) vs. (2.0%), respectively. This is in line with the results obtained in Tanzania (19) and in Ethiopia (15). Conversely, other studies have reported significantly higher mortality among males than females (3, 27). Although this discrepancy in gender mortality is fully explained, some have proposed a difference in immune response that is influenced by sex hormones (28). In addition, it has been previously reported that the tradition in Africa is to take care of male children first before female children (29).
In this study, malnutrition was the leading cause of mortality, with a case fatality rate of 9.7%, which was lower than the case fatality rate (12.5%) of malnutrition in Omdurman (part of the capital of Sudan) (30). However, a lower rate (3.7%) of case fatality of malnutrition has been reported in central Sudan (31) and in eastern Sudan (32). Visceral leishmaniasis was the second leading cause of morbidity and mortality in this study. Gadarif is an endemic area for this particular disease, which represents a high pediatric health burden (17, 18). Visceral leishmaniasis is also endemic in some areas of Sudan in general (33) and is frequently associated with severe anemia requiring blood transfusion (17). Severe anemia, another major cause of mortality in this study, can result from secondary causes, such as sickle cell disease, malaria, visceral leishmaniasis, severe acute malnutrition, snake bites, and sepsis (17). Severe-to- moderate anemia was also reported to be the main cause of admission to hospital among Ghanaian children (34).
Our study documented a considerably higher morbidity and mortality rate related to malaria infection. Malaria is an endemic disease that is associated with a significant mortality rate (5.3%) (35). Children are the most vulnerable age group for this disease, with a high mortality rate in Burundi (36) and Kenya (37, 38).
Diarrhea was a further cause of morbidity and mortality in this study. It is considered a major childhood medical problem in other areas in Sudan (39, 40) and in some African countries (41). Despite tremendous efforts, through a global initiative, to modify diarrheal-related fatalities in the last two decades, it is still one of the top two deadly diseases (72%) in children under the age of two in Sub-Saharan Africa in particular (42, 43). The common causes for diarrheal infection in this vulnerable group are enteric pathogenic rotavirus (44) and bacterial infections (40, 45).
In Sudan, the mortality rate may be explained by the poor distribution of health facilities in rural areas, family poverty, and the lack of hygienic and safe environments for children (46). Other reasons include low socioeconomic status and low educational levels of mothers (47, 48). Violence and war are additional risk factors that increase mortality in this vulnerable group of children (48). Similar risk factors affecting mortality have been demonstrated in several African countries, such as the preceding birth interval, family size, birth type, breastfeeding status, source of drinking water, maternal and child health services, mother's educational level, herbal medication use, sex of the child, and socioeconomic status (42, 49, 50). On the other hand, improvements in socio-demographic status, maternal health, governance, and financial status are likely to be associated with a reduction in the mortality rate (50). Furthermore, there is a growing body of evidence demonstrating that a sufficient density of distributed healthcare workers and health services can have a rapid and positive impact on neonatal and young child mortality and ultimately improve the child survival rate dramatically (51).
It is worth mentioning that human immunodeficiency virus (HIV) was reported as the top cause of death in other African countries (5), but a low incidence rate (0.4%) of HIV was reported in the hospital under study (52).
The limitations of this study are its cross-sectional design and that the data were collected only from major regional hospitals. The use of the incidence rate, a more precise measure, would be ideal to estimate the true at-risk population in etiological research. The study had some challenges, including incomplete reporting, as the hospital was unable to report cases in some years due to the lack of a computer-based system. Due to the retrospective nature of the study, some important factors, such as intubation or the use of respiratory support, were missing. In addition, some patients might have been seen in other health facilities or discharged against medical advice, and death may have occurred within the first month afterdischarge.
Conclusion
Sudan, similar to other developing countries where communicable diseases are the most prevalent causes for morbidity and mortality among children, has a high pediatric mortality rate. Hence, many more efforts are required to achieve the Millennium Development Goals and Sustainable Development Goals in this region.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without unduereservation.
Ethics Statement
The study received ethical approval from the Research Board at the Faculty of Medicine, University of Gadarif, Sudan (the reference number is 2018/11).
Author Contributions
MA and IM made a significant contribution to the data collection and data analysis. OA-W and IA conceived the study and made substantial contributions to the study design and data interpretation. HM contributed to the data collection and drafting of the manuscript. AA-N conceived the study and played a major rule in the study design, data collection, and drafting of the manuscript. All authors read and approved the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank the Deanship of Scientific Research, Qassim University, Kingdom of Saudi Arabia for funding the publication of this manuscript.
Abbreviations
WHO, The World Health Organization; SPSS, Statistical Package for the Social Sciences; SD, Standard Deviation; HIV, human immunodeficiency virus.
References
1. Park K. Park's Textbook of Preventive and Social Medicine. 23rd ed. Mumbai: Bhanot Publishers (2015).
2. Yu H, Wier LM, Elixhauser A. Hospital stays for children, 2009. (2011): Statistical Brief #118 (2011). In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD: Agency for Healthcare Research and Quality (US). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK65134/ (accessed November 21, 2021).
3. Okoronkwo NC, Onyearugha CN, Ohanenye CA. Pattern and outcomes of paediatric medical admissions at the Living Word Mission Hospital, Aba, South East Nigeria. Pan Afr Med J. (2018) 30:202. doi: 10.11604/pamj.2018.30.202.15966
4. Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. (2012) 380:2095–128. doi: 10.1016/S0140-6736(12)61728-0
5. Phillips-Howard PA, Odhiambo FO, Hamel M, Adazu K, Ackers M, van Eijk AM, et al. Mortality trends from 2003 to 2009 among adolescents and young adults in rural western Kenya using a health and demographic surveillance system. PLoS ONE. (2012) 7:e47017. doi: 10.1371/journal.pone.0047017
6. Sawyer SM, Afifi RA, Bearinger LH, Blakemore SJ, Dick B, Ezeh AC, et al. Adolescence: a foundation for future health. Lancet. (2012) 379:1630–40. doi: 10.1016/S0140-6736(12)60072-5
7. Einterz EM, Bates M. Causes and circumstances of death in a district hospital in northern Cameroon, 1993-2009. Rural Remote Heal. (2011) 11:1623. doi: 10.22605/RRH1623
8. Nwankwor OC, McKelvie B, Frizzola M, Hunter K, Kabara HS, Oduwole A, et al. A national survey of resources to address sepsis in children in tertiary care centers in Nigeria. Front Pediatr. (2019) 7:234. doi: 10.3389/fped.2019.00234
9. Geyesus T, Moges F, Eshetie S, Yeshitela B, Abate E. Bacterial etiologic agents causing neonatal sepsis and associated risk factors in Gondar, Northwest Ethiopia. BMC Pediatr. (2017) 17:137. doi: 10.1186/s12887-017-0892-y
10. Vekaria-Hirani V, Kumar R, Musoke RN, Wafula EM, Chipkophe IN. Prevalence and management of septic shock among children admitted at the Kenyatta national hospital, longitudinal survey. Int J Pediatr. (2019) 2019:1502963. doi: 10.1155/2019/1502963
11. WHO. Disease Burden and Mortality Estimates. WHO (2019). Available online at: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates, (accessed November 25, 2021).
12. Patton GC, Coffey C, Sawyer SM, Viner RM, Haller DM, Bose K, et al. Global patterns of mortality in young people: a systematic analysis of population health data. Lancet. (2009) 374:881–92. doi: 10.1016/S0140-6736(09)60741-8
13. SUDAN, WDA,. Our Data - Knoema. Available online at: https://knoema.com/atlas/sources/Central-Bureau-of-Statistics-Sudan (accessed Jan 12, 2022).
14. Bohn JA, Kassaye BM, Record D, Chou BC, Kraft IL, Purdy JC, et al. Demographic and mortality analysis of hospitalized children at a referral hospital in Addis Ababa, Ethiopia. BMC Pediatr. (2016) 16:168. doi: 10.1186/s12887-016-0709-4
15. Misganaw A, Mariam DH, Araya T, Ayele K. Patterns of mortality in public and private hospitals of Addis Ababa, Ethiopia. BMC Public Health. (2012) 12:1007. doi: 10.1186/1471-2458-12-1007
16. Lakew Y, Tabar L, Haile D. Socio-medical determinants of timely breastfeeding initiation in Ethiopia : evidence from the 2011 nation wide demographic and health survey. Int Breastfeed J. (2015) 10:24. doi: 10.1186/s13006-015-0050-9
17. Ahmed MAA, Al-nafeesah A, Al-wutayd O, Mahgoub M, Id IA. Severe childhood anemia and emergency blood transfusion in Gadarif Hospital, eastern Sudan. PLoS One. (2019) 14:e0225731. doi: 10.1371/journal.pone.0225731
18. Ahmed MAA, Ahmed AA, Omar SM, Adam GK, Abdallah TM, Ali AA. Epidemiology of visceral leishmaniasis among children in Gadarif hospital, eastern Sudan. BMC Public Health. (2016) 16:1234. doi: 10.1186/s12889-016-3875-2
19. Lugangira K, Kazaura M, Kalokola F. Morbidity and mortality of children aged 2-59 months admitted in the Tanzania Lake Zone's public hospitals: a cross-sectional study. BMC Res Notes. (2017) 10:502. doi: 10.1186/s13104-017-2818-z
20. Sanyang Y. Prevalence of under-five years of age mortality by infectious diseases in West African region. Int J Africa Nurs Sci. (2019) 11:100175. doi: 10.1016/j.ijans.2019.100175
21. Tsai C, Walters C, Sampson J, Kateh F, Chang M. Pediatric mortality in a rural tertiary care center in Liberia. Children. (2017) 4:8. doi: 10.3390/children4020008
22. Tette EMA, Neizer ML, Nyarko MY, Sifah EK, Sagoe-Moses IA, Nartey ET. Observations from mortality trends at the children's hospital, accra, 2003-2013. PLoS ONE. (2016) 11:e0167947. doi: 10.1371/journal.pone.0167947
23. Fitzgerald E, Mlotha-Mitole R, Ciccone EJ, Tilly AE, Montijo JM, Lang HJ, et al. A pediatric death audit in a large referral hospital in Malawi. BMC Pediatr. (2018) 18:75. doi: 10.1186/s12887-018-1051-9
24. Amin M, Lamidi A, Amsa M. Review of paediatric mortality in a tertiary hospital in Nigeria. Int J Sci Res. (2020) 9:1350–54. doi: 10.21275/ART20197970
25. Abdeldafie SY. Under 5 children mortality in Sudan: situation analysis. Int J Innov Res Med Sci. (2018) 3:1669–71. doi: 10.23958/ijirms/vol03-i01/16
26. Wagnew F, Tesgera D, Mekonnen M, Abajobir AA. Predictors of mortality among under-five children with severe acute malnutrition, Northwest Ethiopia: an institution based retrospective cohort study. Arch Public Heal. (2018) 76:64. doi: 10.1186/s13690-018-0309-x
27. Mouneke UV, Ibekwe RC, Eke CB, Ibekwe MU, Chinawa JM. Mortality among paediatric inpatients in Mile 4 Mission hospital Abakaliki, south-eastern Nigeria: a retrospective study. Niger J Paediatr. (2013) 40:259–63. doi: 10.4314/njp.v40i3,11
28. Piccini P, Montagnani C, De Martino M. Gender disparity in pediatrics: a review of the current literature. Ital J Pediatr. (2018) 44:1. doi: 10.1186/s13052-017-0437-x
29. Kam-lun EH, Nelson A. Gender disparity in paediatric hospital admissions. Ann Acad Med Singap. (2006) 35:882–8.
30. Kanan SOH, Swar MO. Prevalence and outcome of severe malnutrition in children less than five-year-old in Omdurman Paediatric Hospital, Sudan. Sudan J Paediatr. (2016) 16:23–30.
31. Bilal JA, Eltahir HG, Al-Nafeesah A, Al-Wutayd O, Adam I. Acute severe malnutrition treatment outcomes in children ages 6–59 months admitted to Singa Hospital, Sudan. Trans R Soc Trop Med Hyg. (2020) 114:612–7. doi: 10.1093/trstmh/traa033
32. Mahgoub HM, Adam I. Morbidity and mortality of severe malnutrition among Sudanese children in New Halfa Hospital, Eastern Sudan. Trans R Soc Trop Med Hyg. (2012) 106:66–8. doi: 10.1016/j.trstmh.2011.09.003
33. Mahamoud A, Osman HA, Abass EM, el Agib A, Madi RR, Semiao-Santos SJ, et al. Identification of an area predominantly endemic for childhood and adolescent visceral leishmaniasis in central Sudan. Acta Trop. (2018) 178:142–7. doi: 10.1016/j.actatropica.2017.11.010
34. Shenton LM, Jones AD, Wilson ML. Factors associated with anemia status among children aged 6–59 months in Ghana, 2003–2014. Matern Child Health J. (2020) 24:483–502. doi: 10.1007/s10995-019-02865-7
35. Hashim H, Ali E. Pattern of malaria in hospitalized children in Khartoum state. Sudan J Paediatr. (2017) 17:35–41. doi: 10.24911/SJP.2017.2.4
36. Moise I. Causes of morbidity and mortality among neonates and children in post-conflict Burundi: a cross-sectional retrospective study. Children. (2018) 5:125. doi: 10.3390/children5090125
37. Amek NO, Van Eijk A, Lindblade KA, Hamel M, Bayoh N, Gimnig J, et al. Infant and child mortality in relation to malaria transmission in KEMRI/CDC HDSS, Western Kenya: validation of verbal autopsy. Malar J. (2018) 17:37. doi: 10.1186/s12936-018-2184-x
38. Obonyo CO, Vulule J, Akhwale WS, Grobbee DE. In-hospital morbidity and mortality due to severe malarial anemia in western Kenya. Am J Trop Med Hyg. (2007) 77:23–8. doi: 10.4269/ajtmh.77.6.suppl.23
39. Siziya S, Muula AS, Rudatsikira E. Correlates of diarrhoea among children below the age of 5 years in Sudan. Afr Health Sci. (2013) 13:376–83. doi: 10.4314/ahs.v13i2.26
40. Saeed A, Abd H, Sandstrom G. Microbial aetiology of acute diarrhoea in children under five years of age in Khartoum, Sudan. J Med Microbiol. (2015) 64:432–7. doi: 10.1099/jmm.0.000043
41. Reiner RC, Graetz N, Casey DC, Troeger C, Garcia GM, Mosser JF, et al. Variation in childhood diarrheal morbidity and mortality in Africa, 2000-2015. N Engl J Med. (2018) 379:1128–38. doi: 10.1056/NEJMoa1716766
42. Gavhi F, Kuonza L, Musekiwa A, Villyen Motaze N. Factors associated with mortality in children under five years old hospitalized for severe acute malnutrition in Limpopo province, South Africa, 2014-2018: a cross-sectional analytic study. PLoS ONE. (2020) 15:e0232838. doi: 10.1371/journal.pone.0232838
43. Bado AR, Susuman AS, Nebie EI. Trends and risk factors for childhood diarrhea in sub-Saharan countries (1990-2013): assessing the neighborhood inequalities. Glob Health Action. (2016) 9:30166. doi: 10.3402/gha.v9.30166
44. Shaheen MNF. Rotavirus gastroenteritis among hospitalized children under 5 years of age in the eastern mediterranean region: a review. East Mediterr Heal J. (2019) 25:422–30. doi: 10.26719/emhj.18.054
45. Mbuthia OW. Diarrheal correlates associated with enteric bacterial infections among children below five years in Murang'a County, Kenya. Pan Afr Med J. (2019) 34:170. doi: 10.11604/pamj.2019.34.170.17403
46. Albasheer O. Basic human needs and child mortality, in Wad-Madani paediatric teaching hospital, Gezira, Sudan. Int J Community Med Public Heal. (2016) 3:893–6. doi: 10.18203/2394-6040.ijcmph20160924
47. Gritly SMO, Osman Elamin M, Rahimtullah H, Ali AYH, Hassan A, Yabarow D, et al. Risk factors of pneumonia among children under 5 years at a pediatric hospital in Sudan. Int J Med Res Heal Sci. (2018) 7:60–8.
48. Mugo NS, Agho KE, Zwi AB, Damundu EY, Dibley MJ. Determinants of neonatal, infant and under-five mortality in a war-affected country: analysis of the 2010 Household Health Survey in South Sudan. BMJ Glob Heal. (2018) 3:e000510. doi: 10.1136/bmjgh-2017-000510
49. Van Malderen C, Amouzou A, Barros AJD, Masquelier B, Van Oyen H, Speybroeck N. Socioeconomic factors contributing to under-five mortality in sub-Saharan Africa: a decomposition analysis. BMC Public Health. (2019) 19:760. doi: 10.1186/s12889-019-7111-8
50. Kipp AM, Blevins M, Haley CA, Mwinga K, Habimana P, Shepherd BE, et al. Factors associated with declining under-five mortality rates from 2000 to 2013: an ecological analysis of 46 African countries. BMJ Open. (2016) 6:e007675. doi: 10.1136/bmjopen-2015-007675
51. Doherty T, Kroon M, Rhoda N, Sanders D. Ending preventable child deaths in South Africa: what role can ward-based outreach teams play? South African Med J. (2016) 106:672–4. doi: 10.7196/SAMJ.2016.v106i7.10790
Keywords: morbidity, mortality, under 5 years, predictors, children
Citation: Ahmed MAA, Musa IR, Mahgoub HM, Al-Nafeesah A, Al-Wutayd O and Adam I (2022) Patterns, Outcomes and Predictors of Pediatric Medical Admissions at Gadarif Hospital in Eastern Sudan. Front. Pediatr. 10:764028. doi: 10.3389/fped.2022.764028
Received: 24 August 2021; Accepted: 06 January 2022;
Published: 27 January 2022.
Edited by:
Judie Arulappan, Sultan Qaboos University, OmanReviewed by:
Kulnipa Kittisakmontri, Chiang Mai University, ThailandCihad Dundar, Ondokuz Mayis University, Turkey
Copyright © 2022 Ahmed, Musa, Mahgoub, Al-Nafeesah, Al-Wutayd and Adam. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abdullah Al-Nafeesah, a.alnafeesah@qu.edu.sa
 Mohammed Ahmed A. Ahmed1
Mohammed Ahmed A. Ahmed1  Abdullah Al-Nafeesah
Abdullah Al-Nafeesah Ishag Adam
Ishag Adam