The non-clinical burden of febrile seizures: a systematic review
- 1Department of Clinical Science and Community Health, University of Milan, Milan, Italy
- 2Struttura Complessa Pediatria, Presidio Ospedaliero Magenta, ASST Ovest Milanese, Milan, Italy
- 3Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Pediatric Unit, Milan, Italy
- 4Department of Pediatrics, AOUP Santa Chiara Hospital, Pisa, Italy
- 5Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health, University of Genoa, Genoa, Italy
- 6Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Neuropathophysiology Unit, Milan, Italy
Febrile seizures (FS) can be frightening for parents, even though they are usually harmless. Various questionnaires have been used to assess parental reactions and awareness about FS, revealing insufficient knowledge. Studies have shown that educational interventions significantly reduce parental concerns, improve knowledge, and promote better first-aid measures. Providing clear information and emotional support to parents is important to reduce their concerns and improve FS management. Healthcare providers should give comprehensive information about FS, including the risk of recurrence, and provide clear instructions on their management. The economic impact of FS includes direct and indirect costs. Studies have shown a decrease of hospitalizations and associated costs due to improved clinical adherence to guidelines, which also reduces the inappropriate use of healthcare resources. This systematic review provides a comprehensive overview of the existing literature on parental anxiety and education about FS, as well as their economic impact, aiming at identifying areas for improvement in the management of FS and providing valuable insights for healthcare providers and policymakers to better address the non-clinical burden of this condition.
1 Introduction
Febrile seizures (FS) represent the most common type of childhood convulsions, typically occurring between 6 months and 5 years of age without any underlying neurological disorder (1). FS are characterized by a sudden onset of seizures associated with fever, usually triggered by respiratory or gastrointestinal infections (2). While the exact pathogenesis of FS is not fully understood, they might occur as a result of several causes, including genes encoding for ion channels, inflammatory pathways (3), environmental factors and family history (4, 5).
Although FS are generally benign, they can represent a major cause of distress in caregivers. Nevertheless, the non-clinical burden of this condition is still underestimated (6, 7). Parental anxiety and education, as well as the direct and indirect costs associated with FS, are important factors that affect the clinical management and need for a specific focus (8). The subjective burden experienced by caregivers whose child experiences FS encompasses various dimensions, including concerns about the child's health, family dynamics, and the broader implications for public health. Parental education is critical in reducing anxiety and improving management of FS, resulting in a better allocation of healthcare resources (9, 10). Interestingly, the lack of knowledge about FS, including their causes and potential complications, could enhance anxiety-related parental symptoms (11). Therefore, effective communication between healthcare providers and caregivers could be pivotal in addressing these concerns and improving parental education about FS. This review aims to analyze the multifaceted impact of FS on caregivers, exploring the subjective burden they face and its implications. Specifically, we seek to evaluate current evidence on parental stress and anxiety, factors influencing the management of FS in case of relapses, and the potential consequences of inappropriate healthcare service utilization.
In addition to the psychological toll, FS also have a financial impact on public health and family finances (7, 12–14). The direct costs associated with FS include medical expenses, such as emergency department (ED) visits, hospitalizations, exams and follow-up care (12–14). Indirect costs, such as lost wages related to time off work, can also be significant, even in cases of a self-limited and benign condition (15).
Despite an estimated prevalence of FS between 2% and 5% in Western countries and their well-known impact on families, there is a significant gap in literature concerning the non-clinical burden of the condition (1). Understanding the subjective burden experienced by caregivers is important for healthcare providers and policymakers to develop targeted interventions that address the specific needs of these individuals. Our purpose is to identify areas for improvement in the management of FS and provide insights for healthcare providers and policymakers to better address the non-clinical burden of this condition.
2 Methods
In this systematic review we conducted a comprehensive literature research using three databases: PubMed/Medline, Web of Science, and Cochrane. The research was conducted using the following terms: (“febrile seizures” OR “febrile convulsions”) AND (“parents” OR “survey” OR “questionnaire” OR “parental anxiety” OR “parental education” OR “costs” OR “public health” OR “economic burden”). We limited our research to articles published in English and involving pediatric patients. Our inclusion criteria included questionnaire-based studies, as well as studies that delved into different aspects of FS, including their management, their impact on parental anxiety, and their economic implications. Conversely, we excluded studies that exclusively focused on clinical aspects of FS or those that did not directly address our primary research question. Following data were extracted from each study included: first author, year, country, population, type of questionnaire, and conclusions.
Studies were screened and eligible studies were selected according to the PRISMA statement and specific inclusion criteria. To ensure a systematic review process, two independent reviewers conducted an initial screening by evaluating titles and abstracts of the identified studies. This screening was performed to caliber the relevance of each study to our research question. Subsequently, full-text articles of potentially relevant studies were subjected to a more detailed review for inclusion in our review. In cases where discrepancies or uncertainties arose during the review process, a third reviewer was consulted to facilitate discussion and reach a consensus.
3 Results
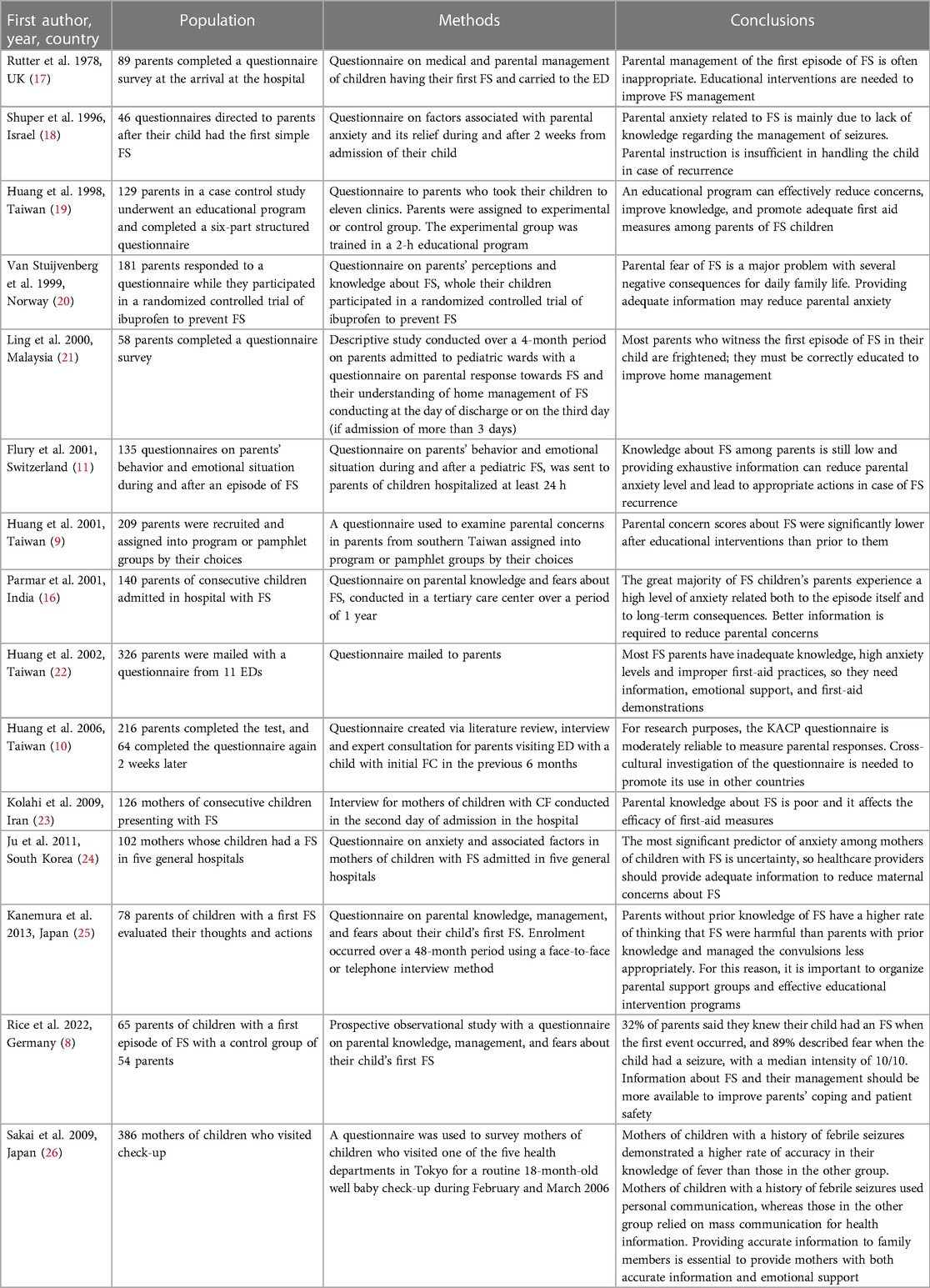
A total of 15 studies were included in this review (8–11, 16–26). The literature search process is reported in the Supplementary Material Figure S1. Seven surveys (46.7%) reported an insufficient parental knowledge, suggesting the need for educational interventions (8, 16, 17, 21–23, 25). Huang et al. conducted a survey about parental knowledge and concerns regarding FS in Taiwan and showed that the majority of involved caregivers had high concerns and inadequate knowledge on first-aid practices (22). For this reason, the Authors concluded that parents with FS children should be provided with more information, emotional support, and first-aid training. Educational interventions significantly reduce parental concerns about FS, improve knowledge and first-aid efficacy (9, 20). Two-hundred and nine caregivers were recruited and assigned to either an educational program or a pamphlet receiving group, and a questionnaire was used to examine parental concerns prior to and after the interventions (9). Results showed that caregivers had higher levels of concern before interventions, mainly of their children's risk of being more vulnerable in case of fever episodes, and therefore more prone to further seizures. Moreover, they were also concerned of the eventual sequelae of FS, such as brain damage, or even death. Notably, concern scores were significantly lower after educational interventions for the training group than for the pamphlet group (9).
The study conducted by Sakai et al. in 2009 compared maternal knowledge and perception of fever, fever management and information sources of mothers of children with and without a history of FS (26). The authors administered a questionnaire to mothers of children who visited health departments for a routine 18-month-old well baby check-up, collecting a total of 386 responses. They found out that mothers of children with a history of febrile seizures demonstrated a higher rate of accuracy in their knowledge of fever than those in the other group. Mothers of children with a history of febrile seizures used personal communication, whereas those in the other group relied on mass communication for health information. Providing accurate information to family members is essential to provide mothers with both accurate information and emotional support.
Another Swiss study examined parental behavior and emotional response during and after a FS episode in their children (11). Authors highlighted that FS were unknown to 44% of parents; 91% of parents reported severe anxiety on witnessing the first episode; 60% of parents thought their child would have died. Interestingly, severe anxiety was more frequently experienced by parents with lack of knowledge about the overmentioned condition and lower educational level. Moreover, 72% of parents did not know how to handle the first FS of their child, thus often leading to inappropriate measures.
A survey conducted in South Korea assessed the level of anxiety in mothers of children with FS and aimed at identifying factors associated with higher levels of concern (24). The study showed that major factors associated with maternal anxiety were uncertainty, frequency of FS, income, and information about FS. Another study confirmed that the major factor directly associated with parental anxiety is lack of knowledge regarding the management of seizures (18).
A Japanese study investigated parental thoughts and actions when their child experienced the first FS and medical management before reaching the hospital (25). The study found that parents without prior knowledge were more likely to think that FS were life-threatening; they also managed the convulsion less appropriately than parents with prior knowledge. A similar study investigated awareness, concerns, attitudes of mothers of children presenting a first episode of FS and found out that the majority of mothers did not recognize the seizure, and notably 39% of them interpreted the seizures as death; the main concern among parents was the state of their child's health in the future, followed by the fear of recurrence (23). While 76% of mothers lacked awareness regarding preventive measures, 68% demonstrated an acceptable understanding of the necessary steps in the event of a recurrence. Mothers with a higher educational level exhibited greater awareness of preventive measures (23). Analogue conclusions were reached by Rice et al., who found how only one-third of parents realized that their child had a FS when the event occurred, and most of them expressed extremely high levels of anxiety during the first episode (8).
A recent consensus involving child neurologists and pediatricians from five European countries was used to establish a consensus on the key messages to share with parents following a FS (27). Although there were some differences in emphasis between the two groups of experts, both converged on the main key messages to share with parents. This included reassurance based on epidemiology, underlying mechanisms, and emergency management, as well as information about risk factors and differential diagnoses. Importantly, both groups of experts highlighted the risks associated with medication overuse. They stated that parental information would be effective if it improved understanding, decreased parental anxiety and post-traumatic stress disorder, and prevented the modification of usual parenting behaviors.
Table 1 presents the findings from the included studies, encompassing surveys on various aspects of parental education. The data highlights a general lack of knowledge regarding FS among parents of children and toddlers.
4 Discussion
Although the occurrence of FS in children is frequent and mostly benign, it can be frightening and perceived as life-threatening by parents who witness them (7). Main immediate fears are about death and cerebral damage, although they are extremely rare events (28). Few cases of death following FS have been described in literature in past years, mainly attributed to neuronal necrosis due to systemic anoxia (29, 30). At the current state of knowledge, studies demonstrated that simple FS do not cause neurological damage, whereas complex ones may be associated with cerebral lesions at neuroimaging (31). When a child experiences a first episode of FS, parents may experience a range of reactions, encompassing both physical and psychological responses (7). Physically, they may grapple with symptoms such as a loss of appetite, sleep disturbances, including insomnia, and gastrointestinal discomfort, which can, in some instances, even lead to weight loss (16, 32).
The studies included into this review suggest that providing clear information and emotional support to parents is important to reduce their concerns, improve FS management and adopt appropriate measures in case of recurrence. Since uncertainty is often reported as the main predictor factor of parental anxiety, doctors should give exhaustive information about FS to reduce it. Parents should be informed about the features of FS and the risk of recurrence, which is estimated around 30%–50% (4, 33), varying based on the number of risk factors. They should also receive clear indications on their management, possibly with adequate information leaflets that may be delivered directly to caregivers by health care providers (Figure 1).

Figure 1. A sample of the information leaflet that should be given to caregivers by health care providers.
Psychological reactions, on the other hand, can manifest immediately or persist as delayed concerns. Immediate responses include a visceral fear of their child's mortality and apprehension about potential brain damage. In the long term, parents may wrestle with anxieties regarding the development of epilepsy, which in turn carries an inherent risk of developing disorders such as post-traumatic stress disorder, an excessive anxiety with even minor fevers, and haunting apprehensions about seizure recurrence (34). Remarkably, this emotional turmoil persists even among parents who have previously witnessed FS episodes, affecting their mental well-being (7). Following a FS episode, many parents tend to perceive their child as more fragile than their peers, a phenomenon often referred to as the “vulnerable child syndrome”. This theory, developed by Green and Solnit, implies that after a child has recovered from a potentially fatal medical condition, there is a marked difference between his normal health and parents' perception of his vulnerability; this mismatch not only heightens parental anxiety during their child's feverish episodes, but may also cast a shadow over the overall quality of family life (35).
Furthermore, this perceived vulnerability sometimes compels parents to seek medical attention more frequently, potentially increasing healthcare costs, although this connection has yet to be conclusively demonstrated.
The economic burden of FS is constituted by direct and indirect costs. Direct charges are related to visits in the ED and days of hospitalization, while indirect costs are mainly related to missed school days by children and missed days of work by parents (12, 14). Gabutti et al. estimated that 70,610 children were hospitalized for FS in the years 2006–2010 in Italy, equal to 171 cases per 100,000 inhabitants (14). As far as the economic impact of FS on public health is concerned, we distinguish two main aspects. The first issue are costs directly related to parenteral management of FS, such as the inappropriate access to the ER, the increased level of medical attention seeking supposed to follow a first FS episode (often referred to as “the vulnerable child syndrome”) and the increased level of care due to delayed treatment out of hospital. The second aspect is exclusively related to the healthcare personnel, especially to his adherence to international guidelines. In conclusion, charges of FS may be reduced by improving their management according to existing guidelines and, on the other hand, by providing parents with correct and exhaustive information on how to handle these episodes (36).
Up to date, few data are available regarding healthcare services utilization and treatment costs of children experiencing FS (7). Most studies analyzing such aspects have been in children already diagnosed with epilepsy (37, 38). A single-center study conducted in the USA evaluated the direct costs of seizures exclusively managed in the emergency room, that did not need hospitalization (12). Authors enlightened that rescue medications, administered before medical intervention by parents could effectively manage recurrent or prolonged seizures in patients who had already been diagnosed with FS or epilepsy. This evidence requires caregivers to be properly educated in assessing when medications are necessary and when medical examination is needed. The use of rescue medications, such as diazepam rectal gel or other medications (intranasal/intramuscular diazepam, and intranasal/buccal midazolam, more recently) has proven to be cost-saving and to reduce the access to emergency services (12, 39).
Huang et al. calculated the rate and the costs of hospitalization due to simple FS in patients aged less than 6 years from 2003 to 2012 in the USA (40). Authors noticed that simple FS-associated hospitalizations and the related economic costs decreased throughout the years, probably due to improved clinical adherence to guidelines set forth by AAP in 2011 (36). The use of diagnostic procedures such as neuroimaging (except for MRI), EEG and lumbar puncture decreased as well from 2003 to 2012, showing a satisfying adherence to AAP Guidelines. These guidelines emphasize the importance of finding the etiology of the febrile episode, rather than investigating the seizure itself; they do not recommend routine use of EEG and neuroimaging in neurologically healthy children. Furthermore, in most cases no intervention is needed since FS are usually brief and self-limited events. These data are consistent with the hypothesis that AAP guidelines published in 2011 reduced the improper use of healthcare resources in the management of FS.
To strengthen this theory, Chin et al. retrospectively analyzed hospital discharge records in Scotland for a first febrile or afebrile seizure in children aged 1 month to 4 years, and the subsequent prescription of rescue anti-seizure medications (ASMs). Interestingly, the study showed that adherence to UK Guidelines reduced the inappropriate use of healthcare resources (13). Authors also enlightened that there was not an over-prescription of ASMs, as recommended by the overmentioned guidelines (13). Notably, the UK Guidelines, differently from the current clinical practice in most centers in Italy, do not recommend prescribing rescue ASMs after the first episodes of FS or for single afebrile episodes (41).
According to a case-control study, children with FS do not consume excessive healthcare resources, since they have nearly identical rates of hospitalization and physician visits as the control group (42). This study observed that children who presented to the ED with a first FS did not have more medical contacts or hospitalizations during the next 6 to 7.5 years, compared with age-matched controls who had visited the same ED at the same time. Interestingly, a significant reduction in the use of pediatricians' services following the first FS episode was observed. Authors supposed that families may require consultative and emergency care services less often after going through a perceived life-threatening event.
Surprisingly, according to this study the experience of a FS had very little effect on subsequent healthcare utilization, in contrast to the “vulnerable child syndrome” theory mentioned above. According to this theory, after a child has recovered from a potentially fatal medical event, there is a mismatch between his normal health and parents' perception of his vulnerability, which can lead to increased use of health care resources. In this study, even if children with FS were initially perceived as vulnerable, their families did not seek excessive medical attention after the acute event (42). The habits encountered in family with FS could depend greatly on the specific features of the population studies and probably need to be replicated in different settings around the world. A secondary analysis of the same data was conducted to determine which children with an initial FS required excessive subsequent physician visits (43). Authors discovered that children with a known family history of febrile or afebrile seizures had fewer medical visits than those with negative family history.
A retrospective study evaluated the adherence of ED physicians to AAP Guidelines on FS in the USA in the period 2002–2003, with the objective of minimizing invasive interventions, assuming that FS are in most cases a benign event with an excellent prognosis (44). This review noted that the use of lumbar puncture in the differential diagnosis of FS is uncommon, and most patients are discharged at home instead. However, the relatively frequent use of brain CT is inconsistent with these practice guidelines, and we then probably assume an excessive consumption of healthcare resources for this practice. This study does not specifically address direct and indirect costs of FS, but it is likely that a strict adherence to AAP recommendations reduces treatment costs and service utilization.
This review emphasizes the importance of healthcare providers and policymakers addressing the non-clinical burden of FS, which are one of the most common reasons for medical seeking in pediatric EDs. Recent studies indicate that economic impact of FS is notable, although it is decreasing due to the better adherence to published guidelines. Despite recent guidelines, there is still heterogeneity in clinical management and inadequate support for parental concerns. Parents can experience different reactions to their child's FS (both physical and psychological) and are likely to consider their child more vulnerable than the peers, thus potentially increasing the use of medical resources. Nevertheless, the impact of these aspects seems extremely heterogeneous among the different studied populations. Nonetheless, effective communication and information provision to caregivers seems to be effective in mitigating the burden associated with FS. While various approaches exist, the optimal method for disseminating information to caregivers warrants careful consideration. A comprehensive approach that combines written materials, such as informative brochures, with personalized discharge interviews may enhance caregiver understanding and confidence in managing FS. Providing caregivers with written materials allows them to reference essential information at their convenience, while personalized discharge interviews offer an opportunity for healthcare providers to address specific concerns and reinforce key messages, in order to alleviate stress and anxiety.
Our findings show a significant knowledge gap about FS among parents, highlighting the need for educational interventions. Such interventions have demonstrated the potential to relieve parental anxiety, enhance knowledge and improve first-aid measures. A comprehensive parental education approach should encompass information about FS features, risk of recurrence, and proper management of future episodes. Addressing these issues can improve overall management of FS, alleviate parental anxiety, and optimize healthcare resource utilization.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
MM: Conceptualization, Data curation, Formal Analysis, Investigation, Writing – original draft, Writing – review & editing. AC: Data curation, Formal Analysis, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing. LC: Data curation, Investigation, Methodology, Writing – review & editing. CA: Funding acquisition, Supervision, Visualization, Writing – review & editing. AS: Data curation, Investigation, Writing – review & editing. GM: Funding acquisition, Investigation, Methodology, Supervision, Validation, Visualization, Writing – review & editing. RD: Conceptualization, Data curation, Supervision, Validation, Visualization, Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This study was partially funded by Italian Ministry of Health—Current research IRCCS.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2024.1377939/full#supplementary-material
References
1. Leung AK, Hon KL, Leung TN. Febrile seizures: an overview. Drugs Context. (2018) 7:212536. doi: 10.7573/dic.212536
2. Patterson JL, Carapetian SA, Hageman JR, Kelley KR. Febrile seizures. Pediatr Ann. (2013) 42:249–54. doi: 10.3928/00904481-20131122-09
3. Mosili P, Maikoo S, Mabandla MV, Qulu L. The pathogenesis of fever-induced febrile seizures and its current state. Neurosci Insights. (2020) 15:2633105520956973. doi: 10.1177/2633105520956973
4. Sawires R, Buttery J, Fahey M. A review of febrile seizures: recent advances in understanding of febrile seizure pathophysiology and commonly implicated viral triggers. Front Pediatr. (2022) 9:801321. doi: 10.3389/fped.2021.801321
5. Gallentine WB, Shinnar S, Hesdorffer DC, Epstein L, Nordli DR, Lewis DV, et al. Plasma cytokines associated with febrile status epilepticus in children: a potential biomarker for acute hippocampal injury. Epilepsia. (2017) 58:1102–11. doi: 10.1111/epi.13750
6. Østergaard JR. Febrile seizures. Acta Paediatr. (2009) 98:771–3. doi: 10.1111/j.1651-2227.2009.01200.x
7. Jones T, Jacobsen SJ. Childhood febrile seizures: overview and implications. Int J Med Sci. (2007) 4:110–4. doi: 10.7150/ijms.4.110
8. Rice SA, Müller RM, Jeschke S, Herziger B, Bertsche T, Neininger MP, et al. Febrile seizures: perceptions and knowledge of parents of affected and unaffected children. Eur J Pediatr. (2022) 181:1487–95. doi: 10.1007/s00431-021-04335-1
9. Huang MC, Liu CC, Chi YC, Huang CC, Cain K. Parental concerns for the child with febrile convulsion: long-term effects of educational interventions. Acta Neurol Scand. (2001) 103:288–93. doi: 10.1034/j.1600-0404.2001.103005288.x
10. Huang M-C, Huang C-C, Thomas K. Febrile convulsions: development and validation of a questionnaire to measure parental knowledge, attitudes, concerns and practices. J Formos Med Assoc. (2006) 105:38–48. doi: 10.1016/S0929-6646(09)60107-8
11. Flury T, Aebi C, Donati F. Febrile seizures and parental anxiety: does information help? Swiss Med Wkly. (2001) 131:556–60. doi: 10.4414/smw.2001.09790
12. Caron E, Wheless CE, Patters AB, Wheless JW. The charges for seizures in the pediatric emergency room: a single center study. Pediatr Neurol. (2015) 52:517–20. doi: 10.1016/j.pediatrneurol.2015.02.010
13. Chin RF, Ajetunmobi O, Weir CJ, Wood R. Prescription of emergency antiepileptic medication after a first childhood seizure: analysis of routine administrative data. Epileptic Disord. (2015) 17:172–6. doi: 10.1684/epd.2015.0745
14. Gabutti G, Kuhdari P, Ferioli S, Trucchi C. Hospital admissions for seizure in Italy: a decennial retrospective analysis with a special focus on the burden in the pediatric age. Neurol Sci. (2015) 36:1667–73. doi: 10.1007/s10072-015-2230-1
15. Wirrell E, Turner T. Parental anxiety and family disruption following a first febrile seizure in childhood. Paediatr Child Health. (2001) 6:139–43. doi: 10.1093/pch/6.3.139
16. Parmar RC, Sahu DR, Bavdekar SB. Knowledge, attitude and practices of parents of children with febrile convulsion. J Postgrad Med. (2001) 47:19–23.11590285
17. Rutter N, Metcalfe DH. Febrile convulsions–what do parents do? Br Med J. (1978) 2:1345–6. doi: 10.1136/bmj.2.6148.1345
18. Shuper A, Gabbay U, Mimouni M. Parental anxiety in febrile convulsions. Isr J Med Sci. (1996) 32:1282–5.9007172
19. Huang MC, Liu CC, Huang CC. Effects of an educational program on parents with febrile convulsive children. Pediatr Neurol. (1998) 18:150–5. doi: 10.1016/s0887-8994(97)00171-9
20. van Stuijvenberg M, de Vos S, Tjiang GC, Steyerberg EW, Derksen-Lubsen G, Moll HA. Parents’ fear regarding fever and febrile seizures. Acta Paediatr. (1999) 88:618–22. doi: 10.1080/08035259950169260
21. Ling SG. Parental response and understanding towards febrile convulsion. Med J Malaysia. (2000) 55:419–23.11221152
22. Huang M-C, Liu C-C, Huang C-C, Thomas K. Parental responses to first and recurrent febrile convulsions. Acta Neurol Scand. (2002) 105:293–9. doi: 10.1034/j.1600-0404.2002.1o200.x
23. Kolahi A-A, Tahmooreszadeh S. First febrile convulsions: inquiry about the knowledge, attitudes and concerns of the patients’ mothers. Eur J Pediatr. (2009) 168:167–71. doi: 10.1007/s00431-008-0724-z
24. Ju HO, McElmurry BJ, Park CG, McCreary L, Kim M, Kim EJ. Anxiety and uncertainty in Korean mothers of children with febrile convulsion: cross-sectional survey. J Clin Nurs. (2011) 20:1490–7. doi: 10.1111/j.1365-2702.2010.03496.x
25. Kanemura H, Sano F, Mizorogi S, Tando T, Sugita K, Aihara M. Parental thoughts and actions regarding their child’s first febrile seizure. Pediatr Int. (2013) 55:315–9. doi: 10.1111/ped.12058
26. Sakai R, Niijima S, Marui E. Parental knowledge and perceptions of fever in children and fever management practices: differences between parents of children with and without a history of febrile seizures. Pediatr Emerg Care. (2009) 25:231–7. doi: 10.1097/pec.0b013e31819e353a
27. Loussouarn A, Devlin A, Bast T, Benoist G, Corrard F, Cross H, et al. Consensus statements on the information to deliver after a febrile seizure. Eur J Pediatr. (2021) 180:2993–9. doi: 10.1007/s00431-021-04067-2
28. Verity CM. Do seizures damage the brain? The epidemiological evidence. Arch Dis Child. (1998) 78:78–84. doi: 10.1136/adc.78.1.78
29. Chungath M, Shorvon S. The mortality and morbidity of febrile seizures. Nat Clin Pract Neurol. (2008) 4:610–21. doi: 10.1038/ncpneuro0922
30. Vestergaard M, Pedersen MG, Ostergaard JR, Pedersen CB, Olsen J, Christensen J. Death in children with febrile seizures: a population-based cohort study. Lancet. (2008) 372:457–63. doi: 10.1016/S0140-6736(08)61198-8
31. Das R, Swain B, Sahoo CK, Jena PK, Sahu BR, Soren NN, et al. MRI abnormalities of the brain after complex febrile seizures in children. Cureus. (2022) 14:e33084. doi: 10.7759/cureus.33084
32. Kürügöl NZ, Tütüncüoglu S, Tekgül H. The family attitudes towards febrile convulsions. Indian J Pediatr. (1995) 62:69–75. doi: 10.1007/BF02752187
33. Offringa M, Bossuyt PM, Lubsen J, Ellenberg JH, Nelson KB, Knudsen FU, et al. Risk factors for seizure recurrence in children with febrile seizures: a pooled analysis of individual patient data from five studies. J Pediatr. (1994) 124:574–84. doi: 10.1016/s0022-3476(05)83136-1
34. Corsi M, Orsini A, Pedrinelli V, Santangelo A, Bertelloni CA, Carli N, et al. PTSD in parents of children with severe diseases: a systematic review to face COVID-19 impact. Ital J Pediatr. (2021) 47:8. doi: 10.1186/s13052-021-00957-1
35. Gordon KE, Dooley JM, Camfield PR, Camfield CS, MacSween J. Treatment of febrile seizures: the influence of treatment efficacy and side-effect profile on value to parents. Pediatrics. (2001) 108:1080–8. doi: 10.1542/peds.108.5.1080
36. Subcommittee on Febrile Seizures. Febrile seizures: guideline for the neurodiagnostic evaluation of the child with a simple febrile seizure. Pediatrics. (2011) 127:389–94. doi: 10.1542/peds.2010-3318
37. Begley CE, Beghi E. The economic cost of epilepsy: a review of the literature. Epilepsia. (2002) 43(Suppl 4):3–9. doi: 10.1046/j.1528-1157.43.s.4.2.x
38. Annegers JF, Beghi E, Begley CE. Cost of epilepsy: contrast of methodologies in United States and European studies. Epilepsia. (1999) 40(Suppl 8):14–8. doi: 10.1111/j.1528-1157.1999.tb00942.x
39. Bhattacharyya M, Kalra V, Gulati S. Intranasal midazolam vs rectal diazepam in acute childhood seizures. Pediatr Neurol. (2006) 34:355–9. doi: 10.1016/j.pediatrneurol.2005.09.006
40. Huang YY, Li G, Sun LS. Epidemiology and resource utilization of simple febrile seizure-associated hospitalizations in the United States, 2003–2012. J Neurosurg Anesthesiol. (2019) 31:144–50. doi: 10.1097/ANA.0000000000000546
41. Gonzalez-Viana E, Sen A, Bonnon A, Cross JH, Guideline Committee. Epilepsies in children, young people, and adults: summary of updated NICE guidance. Br Med J. (2022) 378:o1446. doi: 10.1136/bmj.o1446
42. Gordon KE, Camfield PR, Camfield CS, Dooley JM, Bethune P. Children with febrile seizures do not consume excess health care resources. Arch Pediatr Adolesc Med. (2000) 154:594–7. doi: 10.1001/archpedi.154.6.594
43. Gordon KE, Dooley JM, Wood E, Brna P, Bethune P. Which characteristics of children with a febrile seizure are associated with subsequent physician visits? Pediatrics. (2004) 114:962–4. doi: 10.1542/peds.2003-0650-F
Keywords: febrile seizures, burden, parental anxiety management, public health, caregiver education, healthcare resources
Citation: Marangoni MB, Corsello A, Cozzi L, Agostoni C, Santangelo A, Milani GP and Dilena R (2024) The non-clinical burden of febrile seizures: a systematic review. Front. Pediatr. 12:1377939. doi: 10.3389/fped.2024.1377939
Received: 28 January 2024; Accepted: 10 April 2024;
Published: 22 April 2024.
Edited by:
Jo Madeleine Wilmshurst, University of Cape Town, South AfricaReviewed by:
Irene Toldo, University of Padua, ItalyMartina P. Neininger, Leipzig University, Germany
© 2024 Marangoni, Corsello, Cozzi, Agostoni, Santangelo, Milani and Dilena. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Robertino Dilena robertino.dilena@policlinico.mi.it
†These authors have contributed equally to this work and share first authorship
 Maria Beatrice Marangoni1,†
Maria Beatrice Marangoni1,†  Antonio Corsello
Antonio Corsello Laura Cozzi
Laura Cozzi Carlo Agostoni
Carlo Agostoni Andrea Santangelo
Andrea Santangelo Gregorio Paolo Milani
Gregorio Paolo Milani Robertino Dilena
Robertino Dilena