Early stress during NICU stay and parent-reported health-related quality of life after extremely preterm birth: an exploratory study with possible targets for early intervention
- 1Divison of Neonatology, Department of Pediatrics, Beatrix Children’s Hospital, University Medical Center Groningen, University of Groningen, Groningen, Netherlands
- 2Department of Health Sciences, University Medical Center Groningen, University of Groningen, Groningen, Netherlands
- 3Department of Epidemiology, University Medical Center Groningen, University of Groningen, Groningen, Netherlands
- 4Environment and Health, Youth Health Care, University of Leuven, KU Leuven, Leuven, Belgium
Introduction: The association between neonatal intensive care unit (NICU) related stress in preterm infants and their health-related quality of life (HRQoL) in the first year following preterm birth remains unexplored. Understanding this association is crucial for enhancing preventive and supportive measures for infants and parents within and beyond the NICU.
Methods: From a single center observational cohort study, we included infants with gestational ages below 30 weeks and/or birth weights under 1,000 grams. HRQoL was quantified using the Infant Quality of Life Instrument (IQI) at 3-, 6-, 9- and 12-months corrected age, covering seven domains. NICU stress was quantified using the Neonatal Infant Stressor Scale (NISS) for the first week of life. We performed Spearman's correlation analyses to test this association.
Results: Of the 45 included infants, the IQI was completed for 27 (60%) at 3, 15 (33%) at 6, 14 (31%) at 9 and 15 (33%) at 12 months. The HRQoL sum scores were related to neonatal stress at 9 and 12 months (ρ = 0.643 and 0.591, p = 0.013 and p = 0.019, respectively) but not at 3 and 6 months (ρ = −0.001 and −0.077 respectively, p > 0.05). Higher NICU stress tended to be associated with more respiratory and mood problems throughout the first year.
Discussion: From a parental perspective on infant HRQoL, extremely preterm infants with higher stress exposure show more problems in the second half-year of life, mainly breathing and possibly mood-related problems. This knowledge may help improve our neonatal care, both during NICU stay and in follow-up clinics, by implementing targeted interventions.
Introduction
Prematurity is a global health concern that poses a significant challenge. Approximately every one in ten children born worldwide is born preterm, i.e., before 37 weeks of gestation (1, 2). While medical advancements have improved the survival rates of preterm infants, the long-term adverse effects on health and neurodevelopment remain (3–7). For example, these infants are at higher risk of cognitive and motor delays, as well as behavioral and emotional problems. A part of these adverse effects is attributed to exposure to neonatal stress (8), which refers to physiological and psychological stress experiences undergone by preterm neonates during their period in the Neonatal Intensive Care Unit (NICU).
While the developmental consequences of preterm birth have been well established, less is known about health-related quality of life (HRQoL) during the first year of life. Amongst HRQoL domains are regulatory problems, i.e., encompassing feeding, sleeping, and crying. Particularly these three domains have been subject of study and estimates are that approximately one in five preterm children have at least a single regulatory problem (9). The prevalence of combined regulatory problems in crying and sleeping among preterm children is debated, while for feeding a consistently higher prevalence is reported (9). Regulatory problems have consequences in later life, including a higher risk of obesity at pre-school age (10), and childhood attention problems (11). In addition to feeding, sleeping, and crying, parents and experts in the field also consider breathing, stooling, skin, interaction, and mood important domains in the first year after birth (12).
Whether problems in these HRQoL domains are associated with neonatal stress exposure is unknown, but this seems plausible, especially for the regulatory domains (13). Proposed mechanisms include a triggered and exaggerated stress system and a possible impact on parent–child bonding. Understanding the relationship between neonatal stress and HRQoL is crucial for developing more effective preventive and supportive measures for parents and infants both during NICU stay and beyond. Therefore, we aimed to determine the association between early NICU-related stress and outcomes in HRQoL domains during the first year after birth in an exploratory study.
Methods
Setting and participants
We included 45 infants as part of the Stress and Outcomes in NICU Graduates (STRONG) study, a single center observational cohort study from the Netherlands. All infants were born between September 2019 and December 2020 and had a gestational age of less than 30 weeks and/or a birth weight below 1,000 grams. All parents of eligible infants were approached shortly after birth and provided written informed consent before inclusion in the study. The study was approved by the Medical Ethical Review Board of the University Medical Center Groningen (METc 2019/128) and this study was also registered online (ISRCTN62164166).
Quantification of neonatal stress
We prospectively collected all stress-related procedures using the Neonatal Infant Stressor Scale (NISS) from the electronic patient files. This scale is developed by Newham and colleagues to reflect cumulative stress exposure for neonates (14). It includes stressful stimuli in different gradations, i.e., ranging from a little stressful (scored 2 points) to extremely stressful (scored 5 points), and both acute and chronic items are included. Examples of acute stressors include for example suctioning of nose and mouth, lumbar punctions, insertion of intravenous access lines or other skin-breaking procedures. Examples of chronic stressors include for example receiving continuous positive airway pressure (CPAP) or phototherapy or suffering from an infection. All these stressors are summed for a single day to reflect cumulative NICU related stress for that day. We summed each day in the first week of life to form a seven-day cumulative score. A previous study from this cohort showed that most stress occurs in this first week of life (15).
Quantification of HRQoL
Parents were asked to complete the Infant Quality of Life Instrument (IQI) at 3, 6, 9 and 12 months corrected age. All parents were asked to complete the IQI as part of the cohort study and received e-mail reminders at the indicated time-points. The IQI is a digital application that covers the seven domains of HRQoL deemed essential by parents and experts in the field of pediatrics (12). These domains are feeding, breathing, stooling, sleeping, skin, interaction, and mood. On a scale of one to four, parents were asked to rate whether there are problems on a certain domain and how severe these problems are in their opinion. They did not provide qualitative details, e.g., examples, on the reported problems.
Statistical analyses
First, we provide descriptive statistics for the cohort of infants. Then, we describe the amount of reported HRQoL problems. As a third step, we summed HRQoL problems and calculated Spearman's correlation coefficients with neonatal stress exposure. Next, we performed more in-depth testing of each domain separately by classifying each domain into 0, not reported as having a problem, and 1, reported to have a problem. In these groups, we compared NISS scores using boxplots and Mann–Whitney U-tests.
Results
In total, 93 infants were eligible to participate in the STRONG study. Of these, 48 did not participate because of missing informed consent due to decease (n = 6), language barrier (n = 2), or logistical reasons including the COVID-19 research stop (n = 25). In total 15 parents declined participation. Of these non-participating infants, some characteristics differed, including being part of a multiple, decease during NICU stay and associated shorter NICU stay and suffering from necrotizing enterocolitis. The final sample consisted of 45 infants, with a median gestational age of 27 weeks (range 26–28 weeks) and a median birth weight of 1,000 grams (range 790–1,248 grams). All participant characteristics are provided in Table 1.
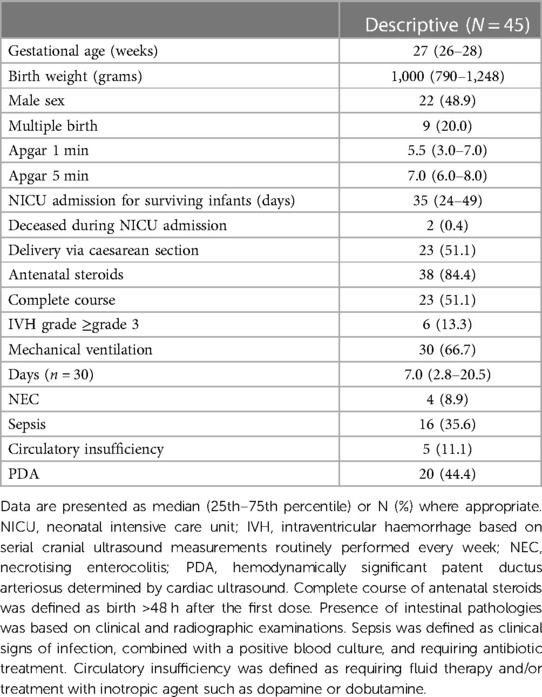
Table 1. Participant characteristics for all infants in the “stress and outcomes in NICU graduates study (STRONG)”.
HRQoL domains
Of the 45 included infants, the IQI was completed for 27 (60%) at 3 months, 15 (33%) at 6 months, 14 (31%) at 9 months and 15 (33%) at 12 months. Parent-reported problems were most common in the feeding, breathing, sleeping, and stooling domains (Figure 1). In the feeding domain, problems were reported to be most severe.
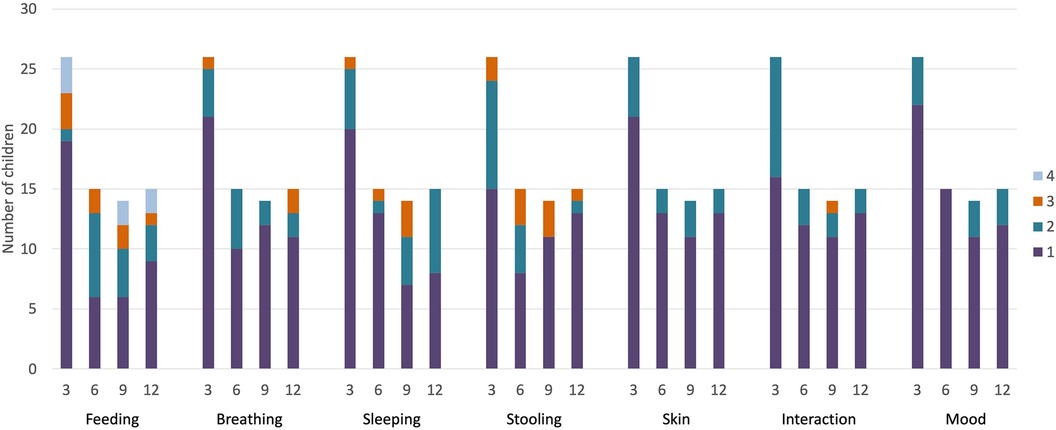
Figure 1. Distribution of parent-reported HRQoL problems for extremely preterm children in the first year after birth. 3 m, 3 months of corrected age; 6 m, 6 months of corrected age; 9 m, 9 months of corrected age; 12 m, 12 months of corrected age. 1, 2, 3 and 4 represent the subsequent levels of problems, ranging from mild to severe.
Relationship between neonatal stress exposure and HRQoL
The HRQoL sum scores were not significantly related to neonatal stress exposure at 3 and 6 months of age (ρ = −0.001 and −0.077 respectively, p > 0.05), whereas at 9 and 12 months of age they were related (ρ = 0.643 and 0.591, p = 0.013 and p = 0.019, respectively). When performing in depth analyses for groups we did not find an association between neonatal stress and feeding problems (Figure 2A). For breathing, we found tendencies towards higher NICU-stress in children with more respiratory problems in the first half year after birth (p = 0.085 at 3 months, p = 0.057 at 6 months), while we found significant differences in the second half year after birth (p = 0.028 at 9 months and p = 0.026 at 12 months; Figure 2B). We also found tendencies towards higher NICU-stress in children with more mood problems in the second half year of life (p = 0.11 at 9 months and p = 0.070 at 12 months; Figure 2G). For the other domains, we did not identify any significant patterns (shown in Figures 2C–F).
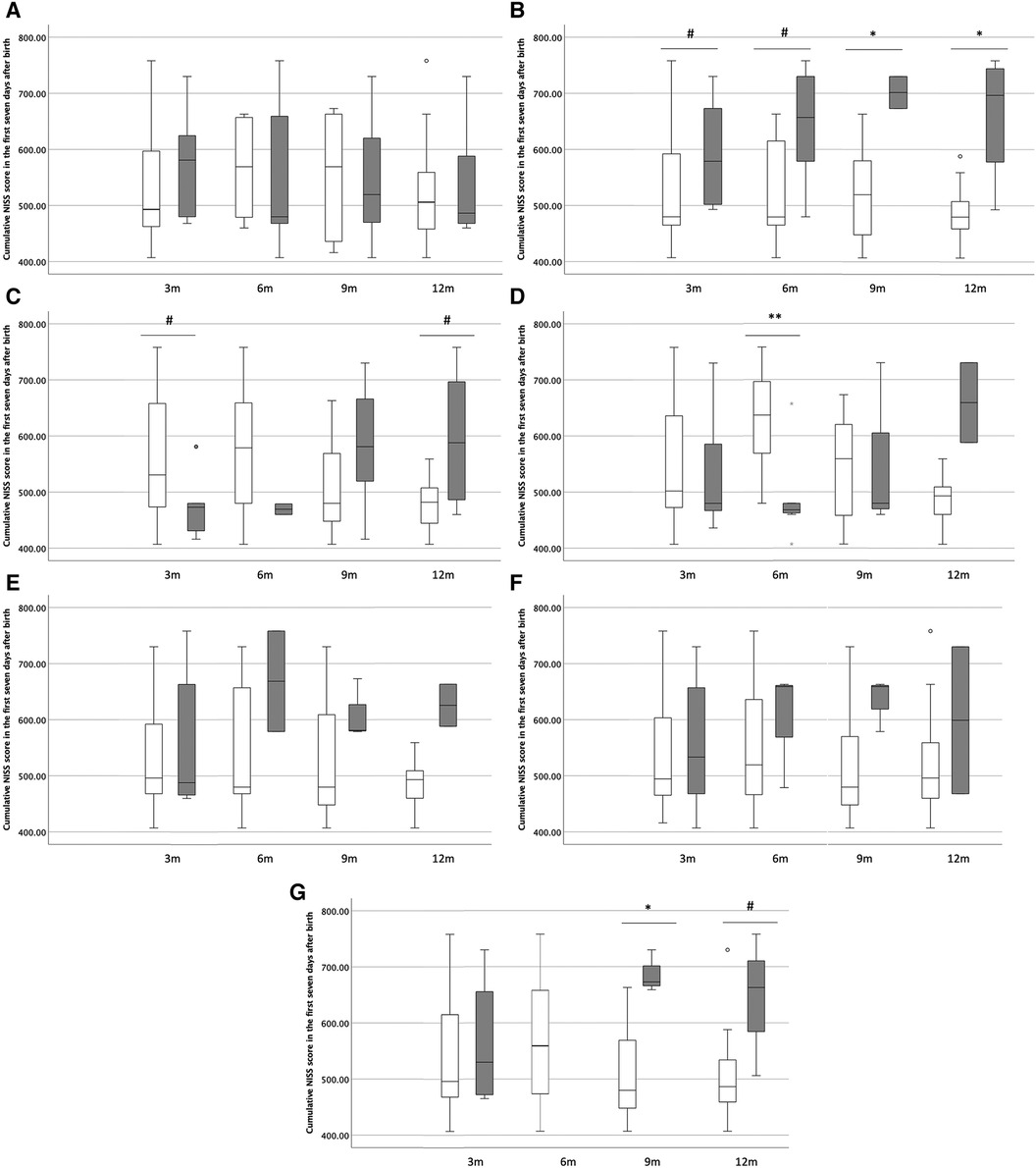
Figure 2. In depth analysis of HRQoL domains in the first year of life. (A) Feeding, (B) breathing, (C) sleeping, (D) stooling, (E) skin, (F) interaction, (G) mood. In the box-whisker plots, the boxes represent the distribution of NISS scores of the first seven days after birth (25th to 75th percentile) and the whiskers represent the width of scores. White boxes represent children without parent-reported problems, while grey boxes represent children with parent-reported problems. 3 m, 3 months of corrected age; 6 m, 6 months of corrected age; 9 m, 9 months of corrected age; 12 m, 12 months of corrected age. NISS, Neonatal Infant Stressor Scale. #p < 0.10, *p < 0.05, **p < 0.005.
Discussion
With this study, we aimed to determine the association between early NICU-related stress and outcomes in HRQoL domains during the first year after birth. We found that overall neonatal stress exposure during the first seven days after birth are related to cumulative HRQoL problems in the second half-year, but not the first half-year after birth. Additionally, with this exploratory study, we suggest that early neonatal stress is associated with breathing problems, and possibly with more mood problems as well, but not with feeding or sleeping problems, nor with the other HRQoL domains.
We were surprised by our finding of an association between cumulative HRQoL problems and neonatal stress in the second half-year of life, but not in the first half-year of life. To the best of our knowledge, ours is the first study to explore the relationship between NICU-related stress exposure and HRQoL in the first year after birth. We therefore are unable to compare our results to others. We speculate that the second half-year of life includes a transformation from tiny baby to infant, including transitions in several of these HRQoL domains. This may lead to increased parent-reported problems in children exposed to more NICU-related stress, who may handle such transitions differently than children exposed to less NICU-related stress. A mechanism may be altered brain development, or altered stress system development, which we know to occur after higher NICU-related stress exposure (8).
For the individual domains, we found the most consistent differences in stress exposure for children with and without breathing problems throughout the first year after birth. We propose that this is partly because the NISS score includes respiratory support, including conventional ventilation, but also CPAP or high flow nasal cannula (HFNC) support (14). Children with higher stress exposure may therefore have been exposed to more respiratory support. However, this study only included the first seven days after birth as a source of stress exposure and did not look beyond. An additional explanation may regard the existence of bronchopulmonary dysplasia (BPD) in extremely preterm children, who may indeed experience more respiratory problems later in life (16). A third explanation derived from clinical practice may be that children are attending daycare in the second half-year, even though it is advised to parents of preterm children not to in the first year of life. We propose a combination of these explanations underlying our findings.
Importantly, respiratory support and respiratory problems in the first year of life may be improved by early interventions. While medical advancements have already employed many of these, including for example early caffeine treatment and altered ventilation practices, non-pharmacological interventions that can be continued beyond the NICU should not be overlooked. Music therapy may be a promising non-pharmacological intervention in this respect. While studies on music therapy in the first year of life are scarce, we do know that breathing exercises, singing, and playing wind instruments at school age are associated with improvements in asthma symptoms (17). The Rhythm Breath and Lullaby method that is adopted more and more in NICUs worldwide also includes interventions focused on infant breathing. As we also observed more reported mood problems in the second half-year of life in infants with higher NICU-related stress exposure, music therapy may also have implications for that HRQoL domain.
This study included HRQoL from a parental perspective. We strongly believe that the parental perspective is invaluable for follow-up care of our most vulnerable patient population. As we know that parents of extremely preterm infants have altered attachment and bonding (18), and may also experience post-traumatic stress during NICU stay and beyond (19), which may affect their perspectives on health problems in their child, integrating parental perspectives of HRQoL is crucial. Besides including the parental perspective, post-traumatic stress during NICU stay and beyond may also affect physiological development of preterm infants and thereby explain our results. Parental resilience and support by other health-care professionals, even in the home setting, may be part of the explanation of our results too. Perhaps interventions are provided in the first months after discharge that are gradually are phased out in the second half-year of life, reflecting the associations found in our study. While these explanations are only speculative, they should be subject of future studies, just as parenting styles, that may impact regulatory problems and thus HRQoL as well (13). By including the parental perspective, follow-up clinics and professionals working in neonatal follow-up are given a tool to start the conversation directed towards individual cases.
Strengths and limitations
To our knowledge, this is one of the first studies to take a close look at HRQoL in the first year of life, including neonatal stress as a specific risk factor. As stated before, we consider the parental perspective that is provided in this study as a strength as well. We acknowledge that our study includes a limited sample of extremely preterm infants and that response rates at later timepoints even make the sample smaller. Findings may either be overestimated in the case that parents will respond more promptly if they experience problems, or underestimated in the case that parents experience more space for study participation when they experience little problems. Therefore, results should be interpreted with caution and should be confirmed in larger prospective studies.
Conclusion
From a parental perspective on HRQoL in seven domains during the first year after birth, extremely preterm infants with higher stress exposure show more problems in the second half-year of life, in particular breathing problems and to a lesser degree mood-related problems. This knowledge may help to improve our neonatal care, both during NICU stay and in follow-up clinics, using tailored interventions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Medisch Ethische Toetsingscommissie (METc) University Medical Center Groningen (METc 2019/128). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
ND: Conceptualization, Data curation, Formal Analysis, Investigation, Project administration, Visualization, Writing – original draft. AB: Conceptualization, Methodology, Supervision, Writing – review & editing. KK: Validation, Writing – review & editing. HB: Data curation, Project administration, Validation, Writing – review & editing. SR: Conceptualization, Validation, Writing – review & editing. PK: Conceptualization, Data curation, Investigation, Resources, Software, Validation, Writing – review & editing. MK: Conceptualization, Methodology, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
ND was financially supported by a grant from the Junior Scientific Masterclass of the University of Groningen. The financers have had no role in any stage of the project, including the decision to submit the manuscript.
Acknowledgments
The authors would like to thank medical and nursing staff of the neonatal intensive care unit, as well as all participating parents. Moreover, we greatly appreciate the help of the research nurses of the neonatal department.
Conflict of interest
The Infant Quality of Life Instrument as used in this paper was developed by PK, as part of academic/commercial activities.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Chawanpaiboon S, Vogel JP, Moller A, Lumbiganon P, Petzold M, Hogan D, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health. (2019) 7:e37–46. doi: 10.1016/S2214-109X(18)30451-0
2. Zeitlin J, Szamotulska K, Drewniak N, Mohangoo AD, Chalmers J, Sakkeus L, et al. Preterm birth time trends in Europe: a study of 19 countries. BJOG. (2013) 120:1356–65. doi: 10.1111/1471-0528.12281
3. Johnson S, Evans TA, Draper ES, Field DJ, Manktelow BN, Marlow N, et al. Neurodevelopmental outcomes following late and moderate prematurity: a population-based cohort study. Arch Dis Child Fetal Neonatal Ed. (2015) 100:F301–308. doi: 10.1136/archdischild-2014-307684
4. Johnson S, Marlow N. Early and long-term outcome of infants born extremely preterm. Arch Dis Child. (2017) 102:97–102. doi: 10.1136/archdischild-2015-309581
5. Johnson S. Cognitive and behavioural outcomes following very preterm birth. Semin Fetal Neonatal Med. (2007) 12:363–73. doi: 10.1016/j.siny.2007.05.004
6. Johnson S, Strauss V, Gilmore C, Jaekel J, Marlow N, Wolke D. Learning disabilities among extremely preterm children without neurosensory impairment: comorbidity, neuropsychological profiles and scholastic outcomes. Early Hum Dev. (2016) 103:69–75. doi: 10.1016/j.earlhumdev.2016.07.009
7. Moore T, Hennessy EM, Myles J, Johnson SJ, Draper ES, Costeloe KL, et al. Neurological and developmental outcome in extremely preterm children born in England in 1995 and 2006: the EPICure studies. Br Med J. (2012) 345:e7961. doi: 10.1136/bmj.e7961
8. van Dokkum NH, de Kroon MLA, Reijneveld SA, Bos AF. Neonatal stress, health, and development in preterms: a systematic review. Pediatrics. (2021) 148:e2021050414. doi: 10.1542/peds.2021-050414
9. Bilgin A, Wolke D. Regulatory problems in very preterm and full-term infants over the first 18 months. J Dev Behav Pediatr. (2016) 37:298–305. doi: 10.1097/DBP.0000000000000297
10. Peacock-Chambers E, Radesky JS, Parker SE, Zuckerman B, Lumeng JC, Silverstein M. Infant regulatory problems and obesity in early childhood. Acta Pediatr. (2017) 17:523–8. doi: 10.1016/j.acap.2016.11.001
11. Breeman LD, Jaekel J, Baumann N, Bartmann P, Bäumi JG, Avram M, et al. Infant regulatory problems, parenting quality and childhood attention problems. Early Hum Dev. (2018) 124:11–6. doi: 10.1016/j.earlhumdev.2018.07.009
12. Jabrayilov R, van Asselt ADI, Vermeulen KM, Volger S, Detzel P, Dainelli L, et al. A descriptive system for the infant health-related quality of life instrument (IQI): measuring health with a mobile app. PLoS ONE. (2018) 13(8):e0203276. doi: 10.1371/journal.pone.0203276
13. Schmid G, Schreier A, Meyer R, Wolke D. Predictors of crying, feeding and sleeping problems: a prospective study. Child Care Health Dev. (2011) 37:493–502. doi: 10.1111/j.1365-2214.2010.01201.x
14. Newnham CA, Inder TE, Milgrom J. Measuring preterm cumulative stressors within the NICU: the neonatal infant stressor scale. Early Hum Dev. (2009) 85:549–55. doi: 10.1016/j.earlhumdev.2009.05.002
15. van Dokkum NH, de Kroon MLA, Dijk PH, Kraft KE, Reijneveld SA, Bos AF. Course of stress during the neonatal intensive care unit stay in preterm infants. Neonatology. (2022) 119:84–92. doi: 10.1159/000520513
16. Hart K, Cousins M, Watkins WJ, Kotecha SJ, Henderson AJ, Kotecha S. Association of early-life factors with prematurity-associated lung disease: prospective cohort study. Eur Respir J. (2022) 59:e2101766. doi: 10.1183/13993003.01766-2021
17. Loewy J, Goldsmith C, Deshpande S, Sun A, Harris J, van Es C, et al. Music therapy in pediatric asthma improves pulmonary function while reducing hospitalizations. J Asthma. (2021) 58:674–82. doi: 10.1080/02770903.2020.1712725
18. Ettenberger M, Bieleninik Ł, Epstein S, Elefant C. Defining attachment and bonding: overlaps, differences and implications for music therapy clinical practice and research in the neonatal intensive care unit (NICU). Int J Environ Res Public Health. (2021) 18:e1733. doi: 10.3390/ijerph18041733
Keywords: health-related quality of life, parental perspectives, extremely preterm infants, neonatal intensive care unit, NICU-related stress
Citation: van Dokkum NH, Bos AF, Kraft KE, Bouma HA, Reijneveld SA, Krabbe PFM and de Kroon MLA (2024) Early stress during NICU stay and parent-reported health-related quality of life after extremely preterm birth: an exploratory study with possible targets for early intervention. Front. Pediatr. 12:1381008. doi: 10.3389/fped.2024.1381008
Received: 2 February 2024; Accepted: 27 March 2024;
Published: 8 April 2024.
Edited by:
Efthymios Papatzikis, Oslo Metropolitan University, NorwayReviewed by:
Eleftheria Hatzidaki, University of Crete, GreeceElise Roze, Erasmus Medical Center, Netherlands
© 2024 van Dokkum, Bos, Kraft, Bouma, Reijneveld, Krabbe and de Kroon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nienke H. van Dokkum n.h.van.dokkum@umcg.nl
 Nienke H. van Dokkum
Nienke H. van Dokkum Arend F. Bos
Arend F. Bos Karianne E. Kraft1
Karianne E. Kraft1  Sijmen A. Reijneveld
Sijmen A. Reijneveld