Identification and treatment of intestinal malrotation with midgut volvulus in childhood: a multicenter retrospective study
- 1Department of Pediatric Surgery, Binzhou Medical University Hospital, Binzhou, Shandong, China
- 2Department of Surgery, Maternity and Child Health Care of Zaozhuang, Zaozhuang, Shandong, China
- 3Department of Pediatric Surgery, The People’s Hospital of Rizhao, Rizhao, Shandong, China
- 4Department of Surgery, Zibo Maternal and Child Health Hospital, Zibo, Shandong, China
- 5Department of Pediatric Surgery, Liaocheng People’s Hospital, Liancheng, Shandong, China
- 6Department of Pediatric Surgery, Qilu Hospital of Shandong University, Jinan, Shandong, China
Background: Intestinal malrotation is a rare condition, and its delayed diagnosis can lead to fatal consequences. This study aimed to investigate the identification and treatment of malrotation in children.
Methods: Clinical data, imaging, operative findings, and early postoperative outcomes of 75 children with malrotation were retrospectively analyzed.
Results: The mean age was 6.18 ± 4.93 days and 51.26 ± 70.13 months in the neonatal group (56 patients) and non-neonatal group (19 patients), respectively. Sixty-seven patients were under the age of 1 year at the time of diagnosis. The occurrence of bilious vomiting and jaundice was significantly higher in the neonatal group (89.29%) than that in the non-neonatal group (37.5%), p < 0.05 and p < 0.01, respectively. The incidence of abnormal ultrasound (US) findings was 97.30% and 100%, respectively, and the sensitivities of the upper gastrointestinal series were 84.21% and 87.5%, respectively. Sixty-six (88%) patients had midgut volvulus, including in utero volvulus (two patients) and irreversible intestinal ischemia (four patients). Most neonates (89.29%) underwent open Ladd's procedure with a shorter operative time (p < 0.01). Reoperation was performed for postoperative complications (four patients) or missed comorbidities (two patients).
Conclusions: Non-bilious vomiting was the initial symptom in >10% of neonates and nearly 40% of non-neonates. This highlights the importance for emergency physicians and surgeons to be cautious about ruling out malrotation in patients with non-bilious vomiting. Utilizing US can obviate the need for contrast examinations owing to its higher diagnostic accuracy and rapid diagnosis and can be recommended as a first-line imaging technique. Additionally, open surgery is still an option for neonatal patients.
Introduction
Intestinal malrotation, a congenital rotational anomaly, refers to the abnormalities of the intestinal position resulting from non-rotation, incomplete rotation, or abnormal fixation of the embryonic gut (1). The distal duodenum does not reach the left side of the abdomen and, therefore, lacks the stability usually provided by the ligament of Treitz. It is estimated that 3.9–20 of 10,000 newborns present with intestinal malrotation (2–4), which may complicate acute, intermittent, or chronic midgut volvulus in children and adults (5). A high index of suspicion is vital for its accurate and rapid identification (5). However, acute malrotation with volvulus, a life-threatening emergency with high morbidity and mortality, is difficult to diagnose in the non-verbal pediatric populations (3, 6, 7).
Upper gastrointestinal series (UGIs) remains the gold standard for diagnosing malrotation with or without volvulus (8). However, in recent years, ultrasound (US) has been used as the first-line modality for diagnosing malrotation with volvulus (9), even during prenatal screening (10, 11). The treatment of malrotation with volvulus is challenging for emergency physicians and pediatric surgeons. Ladd's procedure is curative for malrotation with good outcomes; however, a higher rate of emergency reoperation has been reported in older children (12). Moreover, controversy remains regarding a surgical approach to Ladd's procedure, and there is no evidence that a laparoscopic Ladd's procedure is superior to open surgery, especially during the neonatal period (5, 13–17).
This study aimed to review the multicenter experience to provide useful information regarding the identification of intestinal malrotation and evidence to support the superiority of laparoscopic Ladd's procedure over open surgery or vice versa in pediatric patients.
Patients and methods
Clinical data
Clinical data from six tertiary hospitals between January 2006 and June 2022 were retrospectively reviewed. The inclusion criteria were those aged ≤18 years and had surgically confirmed intestinal malrotation. Keywords including intestinal malrotation, congenital intestinal malrotation, volvulus, duodenal stenosis or atresia, and annular pancreas were used in the digital integrated case management system. The variables, including demographics (sex, age, and birth weight), medical history, symptoms and signs, laboratory and radiological findings, surgical procedures, and outcomes (operative time, time to initial enteral feeding, length of hospital stay, and occurrence of complications) were collected and analyzed. The time to diagnosis was defined as the period from admission to the initiation of anesthesia. Based on the age at admission, the patients were divided into two groups: the neonatal group (aged ≤28 days) and the non-neonatal group (aged >28 days and ≤18 years). Based on the different surgical approaches, the patients were divided into three groups: open, laparoscopic, and laparoscopic conversion to open Ladd's procedure.
Ethical considerations
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or National Research Committee, and the present study adhered to and was conducted according to the principles of the Declaration of Helsinki in 1964 and its subsequent amendments or comparable ethical standards. Institutional review board approval was not needed, as it is a retrospective analysis. Written informed consent was obtained from the parents/legal guardians of all children involved in the study.
Statistical analysis
All values of quantitative and qualitative variables were expressed as mean and standard deviation or as a percentage. Comparisons were made using a t-test or χ2 test. SPSS software (version 20.0; SPSS, Inc., Chicago, IL, USA) was used for the statistical analysis. A p-value of <0.05 was considered statistically significant.
Results
Seventy-five patients met the inclusion criteria. The data for the entire cohort of patients based on age of onset are summarized in Table 1. Of the 75 patients, 56 (74.67%) belong to the neonatal group and 19 (25.33%) belong to the non-neonatal group. The mean age was 6.18 ± 4.93 days and 51.26 ± 70.13 months in the neonatal and non-neonatal groups, respectively. Approximately three-quarters of patients (76%) were male. Patients presented with vomiting (98.67%), bilious vomiting (82.67%), abdominal distension (37.33%), jaundice (29.33%), hematochezia (9.33%), and hematemesis (2.67%). Vomiting occurred in all neonates and in 94.74% of the non-neonatal patients. Of the 56 neonatal patients, 50 presented with bilious emesis and 21 had jaundice, while in the non-neonatal group, 12 presented with bile-stained emesis and 1 with jaundice (p = 0.024 and p = 0.008, respectively).
The median time to confirm malrotation was 22.5 h (2.5–480 h) in the neonatal group and 17 h (2–288 h) in the non-neonatal group (p = 0.916). More than 24 h was required to confirm the diagnosis in half of the patients (50.67%).
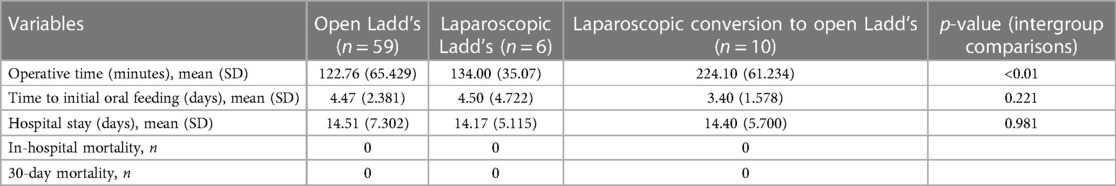
The diagnostic tools included US in 48, abdominal radiography in 39, UGIs in 27, and contrast enema in 13. Abnormal plain abdominal radiographs were observed in 30 patients, including air–fluid level, double bubble sign, intestinal gas accumulation, intestinal obstruction, and pneumoperitoneum. Air–fluid level or scant intestinal gas (Figure 1A) was found in five non-neonatal patients. UGIs revealed duodenal obstruction and/or an abnormal duodenal position of the duodenojejunal junction in 16/19 (84.21%) in the neonatal group and 7/8 (87.50%) in the non-neonatal group (Figure 1B). The contrast enema showed an abnormal position of the cecum in eight out of nine (88.89%) neonatal patients and in all four non-neonatal patients.
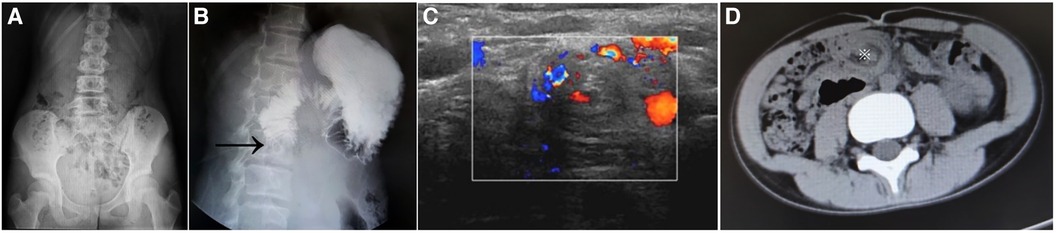
Figure 1. Plain abdominal film showed scant intestinal gas (A). The UGIs demonstrate obstruction of the second part of the duodenum (arrow) (B). Ultrasound shows the “whirlpool” sign, suggestive of malrotation with volvulus of 270°−360° (C). Axial CT image shows the “whirlpool” sign (asterisk) (D). UGIs, upper gastrointestinal series; CT, computed tomography.
Abnormal US findings were found in most neonatal patients (36/37, 97.3%) and all 11 (100%) non-neonatal patients, including superior mesenteric artery–superior mesenteric vein (SMA-SMV) inversion (n = 27 vs. n = 8), “whirlpool” sign (Figure 1C) (n = 21 vs. n = 3), duodenal dilation (n = 17 vs. n = 3), and ascites (n = 4 vs. n = 2) between the neonatal and non-neonatal groups. Two non-neonatal patients showed a “whirlpool” sign at the base of the small bowel mesentery via CT scan (Figure 1D).
Open Ladd's procedure was performed in 50/56 (89.29%) of neonatal patients and 9/19 (47.37%) of non-neonatal patients, the laparoscopic procedure was performed in 1/56 (1.79%) and 5/19 (26.32%), and the remaining 10 patients required laparoscopic conversion to an open Ladd's procedure in 5/56 (8.93%) and 5/19 (26.32%), respectively. Operative time, initial postoperative feeding time, and hospital stay for the three surgical approaches are shown in Table 2. The operative duration for laparoscopic conversion to open Ladd's group (224.10 ± 61.234 min) differed significantly from that of open Ladd's (122.76 ± 65.429 min) and laparoscopic (134.00 ± 35.07 min) procedures (p < 0.01). However, no significant differences were detected between the open and laparoscopic Ladd's procedure groups. Similarly, there were no significant differences in the initial postoperative oral feeding time and length of hospital stay among the three surgical approach groups.
Intraoperative findings revealed 66 patients of complicated midgut volvulus (Figures 2A–C), including 48 neonates (180° in 9 patients, 270° in 5 patients, 360° in 20 patients, 540° in 6 patients, and 720° in 8 patients). Intestinal torsion of 360° was observed in one patient and 720° in two patients, which caused irreversible intestinal ischemia of 30, 35, and 80 cm in length, respectively, and required intestinal resection and primary anastomosis. Eighteen non-neonatal patients were complicated by midgut volvulus with torsions of 180° (five patients), 270° (two patients), 360° (six patients), 540° (one patient), and 720° (four patients).

Figure 2. An 8-day-old boy with bilious vomiting for 8 h, malrotation with midgut volvulus suspected by UGIs. Intraoperative views by open surgical approach show complete small bowel ischemia (black arrow) (A,B) due to a midgut torsion of 720° (blue arrow) (B). After torsion reduction, intestinal viability is restored (C), and the dilated mesenteric vein caused by venous congestion is shown (violet arrow). UGIs, upper gastrointestinal series.
Five neonates required reoperation because of early postoperative recurrent bowel volvulus (one patient), adhesive bowel obstruction (two patients), iatrogenic defect of the hepatic falciform ligament that caused internal hernia and acquired jejunal atresia (one patient), or missed coexisting annular pancreas (one patient). Postoperative recovery was uneventful in all patients.
Discussion
The midgut, perfused by the superior mesentery artery, completes its normal rotation and fixation at 10 weeks of gestation. Malrotations occur in approximately 0.2%–1% of the population (4). Abnormal gut rotation and fixation to the retroperitoneum/peritoneum lead to malrotation of the intestine, usually including non-rotation, malrotation or incomplete rotation, and inverse rotation, depending on the degree and direction of midgut rotation (18, 19). In our case series, all patients had malrotation or incomplete malrotation, which was rotated by 180° and recessed. Abnormal midgut fixation leads to a short mesenteric attachment, which makes the midgut prone to twisting (volvulus) around the SMA and SMV (4, 20–24).
Williams et al. (20) reported that the incidence of malrotation with volvulus decreases with age. In the present case series, 85.71% of neonates had midgut volvulus at the time of presentation, and the incidence was still higher in non-neonatal patients (18/19, 94.74%). Delayed diagnosis of midgut volvulus usually leads to massive intestinal ischemia and necrosis, presenting with hematemesis, hematochezia, abdominal distention, peritonitis, severe shock, and multiple organ dysfunction (4, 24, 25–28). Bile-stained vomiting, usually indicating severe gut pathology, must be taken seriously by all surgeons and general pediatricians (20).
Shalaby et al. (24) reported that 82% of patients experienced midgut volvulus during emergency surgery, and its acute presentation is less common beyond the neonatal period. In this study, the most frequently associated anomalies were the annular pancreas (26.67%), duodenal web (20%), intestinal atresia (20%), and ectopic pancreas (13.33%). Three of the 15 neonates had multiple anomalies, including Meckel's diverticulum, congenital heart disease, gastrointestinal duplication cyst, and trisomy 21, similar to the results described by Kedoin (1), Shehata (29), and Azzam et al. (31). Although coexisting intestinal malrotation and enteric duplication cyst or cardiac anomalies are rare, children with gut duplication or congenital heart problems should be aware of accompanying congenital malrotation (30, 31).
Although a diagnosis of malrotation should always be considered in children with bile-stained vomiting at any age (20, 26, 32), more than 10% of neonates in our study presented with symptoms of non-bilious vomiting. Similarly, bilious vomiting occurred in only 63.16% of non-neonatal patients, and other symptoms included diarrhea, small intestinal obstruction, malnutrition, and failure to thrive, making the diagnosis of malrotation more difficult (2, 14, 22, 28, 32). These findings were similar to those of a previous meta-analysis (23).
UGIs (28, 33, 34) can help make an early accurate diagnosis in different age groups. UGI examination is associated with a sensitivity of 54%–86.5% for detecting midgut volvulus (24, 27, 34). In our case series, the sensitivities of UGIs were 84.21%−87.5%. However, some subtle abnormalities and normal variants can be misinterpreted as normal or mistaken for malrotation.
US can be a useful screening and diagnostic tool (2, 24, 35–40). Abdominal US should be performed in patients with normal duodenojejunal junction on the UGIs and persistent bilious emesis (36). In our case series, the sensitivity of diagnostic US was 97.3% and 100% in the neonatal and non-neonatal groups, respectively. If a midgut volvulus exists, abdominal US can detect “whirlpool” signs, mesenteric edema, ascites, and SMV dilation (23). If the US examination is non-diagnostic and the patient is in a non-acute condition, it is vital to repeat a contrast meal to obtain optional information to diagnose malrotation (20, 40). Moreover, experienced pediatric surgeons and radiologists should play an important role in reviewing equivocal UGIs to make decisions regarding further patient care and avoid significant delays in diagnosis.
In terms of the treatment of malrotation, Ladd's procedure is usually curative (12, 24, 41). The principles of Ladd's procedure for malrotation at any age have remained unchanged with good outcomes (24, 42). However, in older children, intermittent chronic obstruction may lead to a higher emergency reoperation rate. Ladd's procedure with duodenojejunal bypass should be considered (12).
In our case series, approximately half of the non-neonatal patients received a laparoscopic or laparoscopic conversion to open Ladd's procedure, while nearly 90% of neonatal patients underwent open surgery. Laparoscopic conversion to open Ladd's procedure required a significantly longer operative time than open or laparoscopic surgery. Our study revealed that patients, especially small babies, with a high risk of conversion to an open Ladd's procedure should be identified preoperatively using the risk analysis method in future studies (5, 41). Zhu et al. (16) reported that the laparoscopic procedure for neonates with malrotation was associated with a higher risk of recurrent volvulus than open Ladd's procedure.
In terms of the management principles of patients with acute midgut volvulus and hemodynamic instability, aggressive intravenous fluid resuscitation and urgent exploratory laparotomy should be the first choices (5, 24). In terms of reoperation, the causes for reoperation were early postoperative recurrent bowel volvulus, adhesive intestinal obstruction, missed diagnosis of coexisting annular pancreas, internal hernia, and congenital duodenal web (12, 43).
This study has several limitations. The data were collected from six medical centers to improve the sample size to some extent. The total duration of the analyses was 12 years, during which time different clinical management and outcomes were inevitably achieved due to the constant updating of clinical guidelines and imaging techniques; thus, a partial risk of bias cannot be ruled out. The homogeneity of the multicenter retrospective study will be considered in future studies. Regarding the time blocks in patient management, several variables included time and location of initial presentation, US and UGI studies, and surgical consultation. Sabac et al. (26) reported that the median time from initial physician assessment and surgical consultation to surgical incision was over 14 h. The present study did not analyze the effects of these variables on the time to diagnosis. Predicting which patients will develop massive intestinal necrosis is difficult (44), multicenter clinical trials are needed to further assess how long a patient could stand volvulus and help create optimal strategies for malrotation (26).
In conclusion, malrotation with or without midgut volvulus is not rare and should be considered across all age groups. More than 10% of neonatal and nearly 40% of non-neonatal patients with malrotation present with non-bilious vomiting as the initial symptom. Diagnostic suspicion and interdisciplinary coordination are essential for the timely recognition and surgical treatment. Artificial intelligence and machine learning as a novel technique will be helpful in the detection and treatment of malrotation with volvulus (45, 46).
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The requirement of ethical approval was waived by Binzhou Medical University Hospital for the studies involving humans because this study is a retrospective analysis, and institutional review board approval was not needed. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
XY: Conceptualization, Data curation, Writing – original draft, Investigation, Methodology. WW: Data curation, Investigation, Writing – original draft. KW: Data curation, Investigation, Writing – original draft. JZ: Data curation, Investigation, Writing – original draft. LS: Data curation, Investigation, Writing – original draft. SJ: Data curation, Writing – original draft, Methodology. YW: Data curation, Writing – original draft, Investigation. WF: Data curation, Investigation, Writing – original draft. GD: Data curation, Investigation, Writing – original draft. TF: Data curation, Writing – original draft, Conceptualization, Project administration, Software, Supervision, Validation, Writing – review & editing. AL: Conceptualization, Methodology, Supervision, Validation, Writing – review & editing. LG: Conceptualization, Investigation, Methodology, Writing – review & editing.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We thank all the participants and appreciate the cooperation of all the staff.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
SMA, superior mesenteric artery; SMV, superior mesenteric vein; US, ultrasound; UGI, upper gastrointestinal; MR, magnetic resonance; CT, computed tomography.
References
1. Kedoin C, Muto M, Nagano A, Matsui M, Sugita K, Baba T, et al. Notable clinical differences between neonatal and post-neonatal intestinal malrotation: a multicenter review in Southern Japan. J Pediatr Surg. (2024) 59(4):566–70. doi: 10.1016/j.jpedsurg.2023.11.020
2. Nagano A, Sugita K, Harumatsu T, Nishida N, Kedoin C, Murakami M, et al. Predictive factors of bowel resection for midgut volvulus based on an analysis of bi-center experiences in southern Japan. Pediatr Surg Int. (2023) 39(1):113. doi: 10.1007/s00383-023-05406-0
3. Engwall-Gill AJ, Zhou AL, Penikis AB, Sferra SR, Jelin AC, Blakemore KJ, et al. Prenatal sonography in suspected proximal gastrointestinal obstructions: diagnostic accuracy and neonatal outcomes. J Pediatr Surg. (2023) 58(6):1090–4. doi: 10.1016/j.jpedsurg.2023.02.029
4. Adams SD, Stanton MP. Malrotation and intestinal atresias. Early Hum Dev. (2014) 90(12):921–5. doi: 10.1016/j.earlhumdev.2014.09.017
5. Isani MA, Schlieve C, Jackson J, Elizee M, Asuelime G, Rosenberg D, et al. Is less more? Laparoscopic versus open Ladd’s procedure in children with malrotation. J Surg Res. (2018) 229:351–6. doi: 10.1016/j.jss.2018.04.016
6. Moore GP, Byrne A, Davila J, Sarfi E, Bettolli M. Worsening anemia associated with volvulus in a stable neonate with intestinal obstruction. J Neonatal Perinatal Med. (2018) 11(4):417–22. doi: 10.3233/NPM-17118
7. da Costa KM, Saxena AK. Laparoscopic Ladd procedure for malrotation in newborns and infants. Am Surg. (2021) 87(2):253–8. doi: 10.1177/0003134820951424
8. Nehra D, Goldstein AM. Intestinal malrotation: varied clinical presentation from infancy through adulthood. Surgery. (2011) 149(3):386–93. doi: 10.1016/j.surg.2010.07.004
9. Ezer SS, Oguzkurt P, Temiz A, Ince E, Gezer HO, Demir S, et al. Intestinal malrotation needs immediate consideration and investigation. Pediatr Int. (2016) 58(11):1200–4. doi: 10.1111/ped.13075
10. Olutoye OO 2nd, Hammond JD 2nd, Gilley J, Beckman RM, Bulathsinghala M, Keswani SS, et al. Fetal malrotation with midgut volvulus: prenatal diagnosis and planning. J Pediatr Surg Case Rep. (2023) 93:102654. doi: 10.1016/j.epsc.2023.102654
11. Taylor GA, Silva CT. Commentary: sonography as a first-line modality in the diagnosis of malrotation WITH volvulus. Pediatr Radiol. (2023) 53(11):2208–9. doi: 10.1007/s00247-023-05751-1
12. Raitio A, Green PA, Fawkner-Corbett DW, Wilkinson DJ, Baillie CT. Malrotation: age-related differences in reoperation rate. Eur J Pediatr Surg. (2016) 26(1):34–7. doi: 10.1055/s-0035-1563677
13. Huntington JT, Lopez JJ, Mahida JB, Ambeba EJ, Asti L, Deans KJ, et al. Comparing laparoscopic versus open Ladd’s procedure in pediatric patients. J Pediatr Surg. (2017) 52(7):1128–31. doi: 10.1016/j.jpedsurg.2016.10.046
14. Svetanoff WJ, Srivatsa S, Diefenbach K, Nwomeh BC. Diagnosis and management of intestinal rotational abnormalities with or without volvulus in the pediatric population. Semin Pediatr Surg. (2022) 31(1):151141. doi: 10.1016/j.sempedsurg.2022.151141
15. Palanivelu C, Rangarajan M, Shetty AR, Jani K. Intestinal malrotation with midgut volvulus presenting as acute abdomen in children: value of diagnostic and therapeutic laparoscopy. J Laparoendosc Adv Surg Tech A. (2007) 17(4):490–2. doi: 10.1089/lap.2006.0103
16. Zhu H, Zheng S, Alganabi M, Peng X, Dong K, Pierro A, et al. Reoperation after Ladd’s procedure in the neonatal period. Pediatr Surg Int. (2019) 35(1):117–20. doi: 10.1007/s00383-018-4382-6
17. Geng L, Zhou L, Ding GJ, Xu XL, Wu YM, Liu JJ, et al. Alternative technique to save ischemic bowel segment in management of neonatal short bowel syndrome: a case report. World J Clin Cases. (2019) 7(20):3353–7. doi: 10.12998/wjcc.v7.i20.3353
18. Metzger R, Metzger U, Fiegel HC, Kluth D. Embryology of the midgut. Semin Pediatr Surg. (2011) 20(3):145–51. doi: 10.1053/j.sempedsurg.2011.03.005
19. Kawahara R, Horiuchi H, Nogita H, Akashi M, Mikagi K, Yoshitomi M, et al. A case of cancer of the ampulla of Vater accompanied by malrotation. Kurume Med J. (2013) 60(1):33–6. doi: 10.2739/kurumemedj.ms61014
20. Williams H. Green for danger! Intestinal malrotation and volvulus. Arch Dis Child Educ Pract Ed. (2007) 92(3):ep87–91. doi: 10.1136/adc.2007.116244
21. Applegate KE, Anderson JM, Klatte EC. Intestinal malrotation in children: a problem-solving approach to the upper gastrointestinal series. Radiographics. (2006) 26(5):1485–500. doi: 10.1148/rg.265055167
22. Smitthimedhin A, Suarez A, Webb RL, Otero HJ. Mimics of malrotation on pediatric upper gastrointestinal series: a pictorial review. Abdom Radiol (NY). (2018) 43(9):2246–54. doi: 10.1007/s00261-018-1537-9
23. Casalino M, Miscia ME, Lauriti G, Gauda E, Zani A, Zani-Ruttenstock E. Neonatal intestinal segmental volvulus: what are the differences with midgut Volvulus? Eur J Pediatr Surg. (2024) 34(1):9–19. doi: 10.1055/s-0043-1772173
24. Shalaby MS, Kuti K, Walker G. Intestinal malrotation and volvulus in infants and children. Br Med J. (2013) 347:f6949. doi: 10.1136/bmj.f6949
25. Lampl B, Levin TL, Berdon WE, Cowles RA. Malrotation and midgut volvulus: a historical review and current controversies in diagnosis and management. Pediatr Radiol. (2009) 39(4):359–66. doi: 10.1007/s00247-009-1168-y
26. Sabac D, Briatico D, Fitzgerald P. Assessment of care timelines in intestinal malrotation with volvulus: a retrospective chart review. J Pediatr Surg. (2023) 58(5):834–7. doi: 10.1016/j.jpedsurg.2023.01.029
27. Nguyen HN, Navarro OM, Bloom DA, Feinstein KA, Guillerman RP, Munden MM, et al. Ultrasound for midgut malrotation and midgut volvulus: AJR expert panel narrative review. AJR Am J Roentgenol. (2022) 218(6):931–9. doi: 10.2214/AJR.21.27242
28. Langer JC. Intestinal rotation abnormalities and midgut volvulus. Surg Clin North Am. (2017) 97(1):147–59. doi: 10.1016/j.suc.2016.08.011
29. Shehata AE, Helal MA, Ibrahim EA, Magdy B, El Seoudy M, Shaban M, et al. Cecal volvulus in a child with congenital dilated cardiomyopathy: a case report. Int J Surg Case Rep. (2020) 66:30–2. doi: 10.1016/j.ijscr.2019.10.008
30. Azzam A, Abdulkarim AN, Shehata AEM, Mahran I, Arafa A, Arafat A, et al. A report of two infant cases operated for jejunal duplication cyst associated with malrotation and volvulus. Int J Surg Case Rep. (2020) 67:227–30. doi: 10.1016/j.ijscr.2020.02.009
31. Gianino P, Castagno E, Grassino EC, Guidi C, Mostert M. Late and unusual onset of congenital duodenal obstruction due to combination lesion. Minerva Pediatr. (2010) 62(2):223–5.20440242
32. Salehi Karlslätt K, Husberg B, Ullberg U, Nordenskjöld A, Wester T. Intestinal malrotation in children: clinical presentation and outcomes. Eur J Pediatr Surg. (2023) 34(03):228–35. doi: 10.1055/s-0043-1764239
33. Girolamo M, Emanuela G, Yu WMC, Anna M, Marta P, Grazia CM, et al. Diagnostic accuracy of upper gastrointestinal series in children with suspected intestinal malrotation. Updates Surg. (2024) 76(1):201–8. doi: 10.1007/s13304-023-01559-8
34. Kumbhar SS, Qi J. Fluoroscopic diagnosis of malrotation: technique, challenges, and trouble shooting. Curr Probl Diagn Radiol. (2020) 49(6):476–88. doi: 10.1067/j.cpradiol.2019.10.002
35. Taylor GA. Sonographic diagnosis of malrotation: it’s complicated—counterpoint. Pediatr Radiol. (2022) 52(4):723–5. doi: 10.1007/s00247-021-05163-z
36. Shah MR, Levin TL, Blumer SL, Berdon WE, Jan DM, Yousefzadeh DK. Volvulus of the entire small bowel with normal bowel fixation simulating malrotation and midgut volvulus. Pediatr Radiol. (2015) 45(13):1953–6. doi: 10.1007/s00247-015-3430-9
37. El-Ali AM, Ocal S, Hartwell CA, Goldberg JD, Li X, Prestano J, et al. Factors associated with diagnostic ultrasound for midgut volvulus and relevance of the non-diagnostic examination. Pediatr Radiol. (2023) 53(11):2199–207. doi: 10.1007/s00247-023-05727-1
38. Garel J, Daneman A, Rialon K, Zani A, Fecteau A, Piero A. The role of sonography for depiction of a whirlpool sign unrelated to midgut malrotation in neonates. Pediatr Radiol. (2020) 50(1):46–56. doi: 10.1007/s00247-019-04508-z
39. Youssfi M, Goncalves LF. Ultrasound for malrotation and volvulus—point. Pediatr Radiol. (2022) 52(4):716–22. doi: 10.1007/s00247-021-05154-0
40. Fu T, Tong WD, He YJ, Wen YY, Luo DL, Liu BH. Surgical management of intestinal malrotation in adults. World J Surg. (2007) 31(9):1797–803. doi: 10.1007/s00268-007-9018-2
41. Turhan N, Duran C, Kuzan TY, Kuzan BN, Zarbaliyev E. Risk of conversion from laparoscopic appendectomy to open surgery: the role of clinical and radiological factors in prediction. J Laparoendosc Adv Surg Tech A. (2023) 33(12):1176–83. doi: 10.1089/lap.2023.0293
42. Suresh G, Pandey V, Nandan R, Kachhap S. Distal duodenal web with malrotation: an unusual finding. Trop Doct. (2024) 54(1):76–9. doi: 10.1177/00494755231205628
43. Durkin ET, Lund DP, Shaaban AF, Schurr MJ, Weber SM. Age-related differences in diagnosis and morbidity of intestinal malrotation. J Am Coll Surg. (2008) 206(4):658–63. doi: 10.1016/j.jamcollsurg.2007.11.020
44. Seashore JH, Touloukian RJ. Midgut volvulus. An ever-present threat. Arch Pediatr Adolesc Med. (1994) 148(1):43–6. doi: 10.1001/archpedi.1994.02170010045009
45. Bhandari M, Zeffiro T, Reddiboina M. Artificial intelligence and robotic surgery: current perspective and future directions. Curr Opin Urol. (2020) 30(1):48–54. doi: 10.1097/MOU.0000000000000692
Keywords: intestinal malrotation, midgut volvulus, Ladd’s procedure, bilious vomiting, children
Citation: Yang X, Wang W, Wang K, Zhao J, Sun L, Jiang S, Wang Y, Feng W, Ding G, Fu T, Li A and Geng L (2024) Identification and treatment of intestinal malrotation with midgut volvulus in childhood: a multicenter retrospective study. Front. Pediatr. 12:1390856. doi: 10.3389/fped.2024.1390856
Received: 24 February 2024; Accepted: 30 April 2024;
Published: 13 May 2024.
Edited by:
Vasile Valeriu Lupu, Grigore T. Popa University of Medicine and Pharmacy, RomaniaReviewed by:
Heba Taher, Cairo University, EgyptFelicia Galos, Carol Davila University of Medicine and Pharmacy, Romania
© 2024 Yang, Wang, Wang, Zhao, Sun, Jiang, Wang, Feng, Ding, Fu, Li and Geng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shuai Jiang, drjiangshuai@163.com
Guojian Ding, dingguojian2005@163.com
Aiwu Li, liaiwuxie@aliyun.com
Lei Geng, 33181141@qq.com
 Xiaofeng Yang
Xiaofeng Yang Wei Wang2
Wei Wang2  Guojian Ding
Guojian Ding Tingliang Fu
Tingliang Fu