- 1Australian Institute for Suicide Research and Prevention, Griffith University, Brisbane, QLD, Australia
- 2Slovene Center for Suicide Research, Primorska University, Koper, Slovenia
- 3De Leo Fund, Padua, Italy
Background: The way the death of a person is communicated can have a profound impact on the bereavement process. The words and expressions that are used to give the tragic news, the characteristics of who communicates it, the physical setting in which the notification is given, the means used (e.g., in person, via phone call, etc.) are just some of the factors that can influence the way survivors face one of the most difficult moments in their lives.
Aim: To review the literature on the topic of death notification to verify the state of the art related to this important procedure.
Methods: A systematic review was conducted with PRISMA criteria on English-written materials produced from 1966 to 2019.
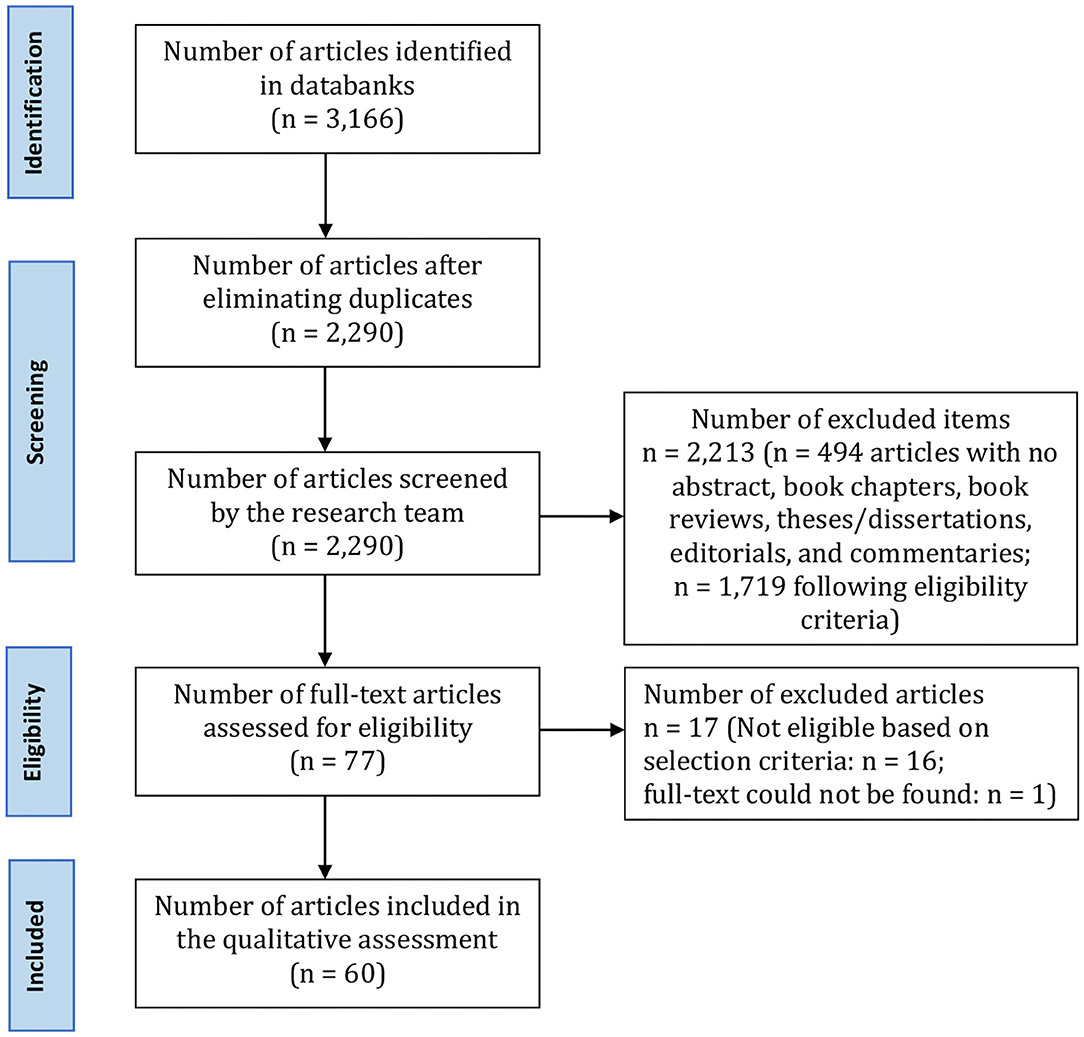
Results: Out of the initial 3,166 titles considered, 60 articles were extracted for this review. A content analysis has revealed four main areas of interest: (1) protocols and guidelines; (2) emotional reactions of recipients and notifiers; (3) professional figures involved in the notification process; and, (4) types of death.
Discussion: The communication of death represents a complex and stressful experience not only for those who receive it but also for those who give it. Alongside the acquisition of a necessary technique and execution methods, the process should involve the selection of notifiers based on personality characteristics and communication styles.
Conclusion: Indications for the need of better training and protocols sensitive to different circumstances emerge. Adequate preparation can positively influence the quality of communication and the effects it produces, both on recipients and notifiers. In vocational training, more space should be devoted to this demanding task.
Introduction
One of the crucial aspects related to the experience of death is the way in which an individual is informed of the loss of a loved one. People who die from sudden and violent causes (such as road accidents, murder, overdose, suicide, accidents at work, natural disasters, terrorist acts, etc.) often have partner, family and friends to whom the events that have led to death must be communicated (Adamowski et al., 1993; Stewart, 1999; Marco and Wetzel, 2012). But “death notification” is a significant moment that could change the life of survivors (those who suffer the loss) forever (Stewart, 1999). The words and expressions that are used to give the tragic news, the characteristics of who communicates it (doctor, policeman, nurse), the physical setting in which the notification is given (home, hospital, patrol car, offices of the police, etc.), the means used (in person, via phone calls, telegram, mail, or instant messaging) are just some of the factors that can influence the way survivors face one of the most difficult moments in their lives (Wheeler, 1994; Stewart, 1999). These circumstances represent painful memories related to the loss that will never be forgotten, and constitute a real break in the narrative story of the person, who will have to reconstruct new meanings around the loss and oneself (Stewart, 1999; Janzen et al., 2003-2004). In fact, most people remember—even after many years—every derelated to this painful communication. It would therefore be desirable that the notification of death could take place under the most appropriate conditions (Smith-Cumberland, 1994, 2007), as it potentially influences the path of elaboration of the mourning of the people involved. In this regard, it has been seen that people who cannot find any kind of meaning in their traumatic experience are more likely to develop persistent psychological distress, psychosomatic disorders, post-traumatic stress disorder (PTSD), and complicated bereavement (Horowitz et al., 1997; Murphy et al., 2002; Neimeyer et al., 2002; Armour, 2003).
De Leo Fund is a non-governmental organization (NGO) that deals with providing psychological support to people who have experienced an unexpected and violent loss (e.g., suicide, road accident, natural disaster, etc.). The people who turn to the NGO often report—together with the description of the experiences related to the loss—the details relating to the moment in which they were told of the death. The peculiarities of that sad notification frequently appear of remarkable importance in the narratives of clients of De Leo Fund, seemingly able to influence their bereavement process. In staff members of the NGO, this has promoted an interest in examining dynamics and variables that occur in the death notification process, by starting with a review of the existing literature on the subject. The main purpose of this study was, therefore, to examine the state of the art of the literature on this topic, with particular attention to critical issues and good practices that should be taken into account in the communication of a traumatic death, in order to eventually provide competent training to operators and improve the notification task.
Among the many issues to clarify are, for example, the identification of the figures most commonly involved in the notification process (e.g., who is responsible for communicating the death? To whom is a death communicated?), and the management of emotional reactions that may involve both the notifier and the target person (recipient) during the notification process, as well as the possible psychopathological consequences associated with the death notification experience. A further question concerns the general recognition in the literature of this area of research, and the current state of the art regarding existing protocols, guidelines, and practical recommendations. Ultimately, the research question from which our systematic review started was to investigate whether there are more adequate strategies or behaviors than others to be considered when it is required to make a death communication to survivors who they have lost a loved one for traumatic, unexpected, and violent death (i.e., an external cause of death: accident, suicide, homicide) and to understand if this process could have consequences on the physical and emotional level of those who are required to communicate and who those who receive the news.
Methods
The compilation of this review followed PRISMA criteria. All the selected studies were examined, while no selection criteria were placed with respect to outcome and design of the individual studies.
There was no review protocol. Articles published in English language from 1966 to 2019 concerning the subject of death notification were selected. All articles that appeared without abstracts, or in the form of editorials or articles in periodicals, book chapters, book reviews or book chapters, dissertations and comments were excluded from the search.
The review of the literature focused on the notification of death in cases of unexpected, traumatic, and violent death. This refers to external causes of death only (i.e., accidents, suicides, and homicides). In light of this, we included only the studies investigating:
A. The characteristics of effective communication of traumatic death (conceptual articles reporting guidelines, protocols, and good practices);
B. Specific aspects of the death report, or seeking to improve the death notification process (e.g., articles assessing the effectiveness of new protocols; communication skills of the notifier, non-verbal language, gestures; needs of training on death notification of specific professional figures (for example, policemen);
C. Possible correlation between death notification and development of psychopathology (i.e., how the level of support perceived during the death notification process could correlate with psychopathological disorders);
D. Risk factors of the person to whom the notification is made; these have to be taken into account at the time of reporting death (e.g., how to communicate the death of a loved one to a drug abuser or a psychotic person);
E. Implications for the notifier (e.g., possible acute stress disorder for those who provide first aid; reactions of medical doctors/psychologists/other health professionals facing the news of the death of a patient);
F. Immediate and/or long-term reactions of those who receive the notification of a traumatic death.
Defining the pertinent criteria was functional in differentiating the collected material and dividing it into more specific areas of investigation. Articles specifically investigating non-traumatic and non-violent death notification were excluded from this research. Deaths associated to palliative care were also excluded from the investigation. Exclusion also concerned:
G. Articles investigating perinatal death and infant death syndrome (SIDS);
H. Articles in which the death notification focused only on cases of cancer, cardiovascular and neurological diseases (these are not external causes of death).
Articles were identified through the following databases: Ebsco PsycINFO, Ebsco CINAHL, Scopus, Web of Science, MEDLINE PubMed, using as keywords: “death notification,” “death communication,” “notification of death,” “communication of death,” notification and “traumatic death,” communication and “traumatic death,” notification and “sudden death,” communication and “udden death.”
Researchers (JZ, AVG, SB, SD) carried out independently the bibliographic search for each keyword, as well as the subsequent elimination of duplicates. Each researcher (JZ, AVG, SB, SD) carried out searches in all databases. In checking for duplicates between the different search engines, the citations with slightly different title and the same abstract, the citations with the same title and abstract but different year of publication, and the citations with the same title and abstract but different title of the magazine were eliminated.
Once the final number of citations was obtained, three independent components of the research team (JZ, AVG, SB) carried out inclusion assessment in a standardized open mode. Disagreements between researchers were resolved by consensus methods. During the screening phase, it was not considered necessary to examine the full text of all articles. A fourth researcher (SD) complemented the reviewing process, while the senior author (DDL) oversaw the entire review process. Figure 1 shows the process of documents identification according to the PRISMA flowchart.
The assessment of risk of bias was performed at the study level. The main risk of bias in the inclusion criteria was related to the decision, implemented before conducting the content analysis, to include studies in which the type of death was not specified and studies that evaluated the overall death notification in relation to traumatic deaths and other types of death. In addition, studies with different size and methodology were also considered, resulting in a strong heterogeneity of the results. The risk of bias associated with the choice of the English language concerned the possibility that this language is associated with studies that are published faster and cited more often.
Figure 1 shows the process of identifying documents according to the PRISMA flowchart.
Results
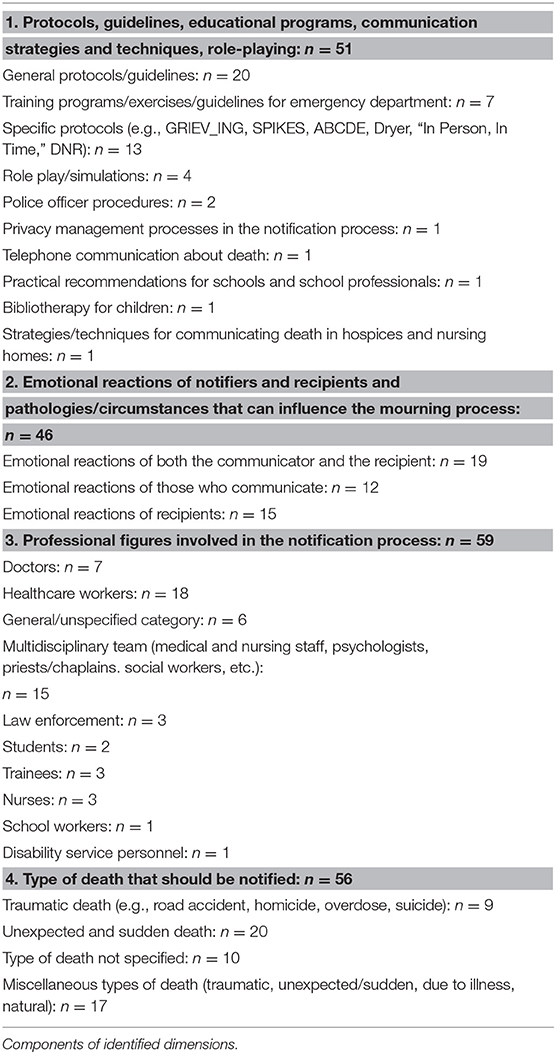
A total of 60 studies were included in our review. The analysis of study contents evidenced a remarkable degree of similarity, with most studies being of narrative type and conceptual content (i.e., most studies aimed at providing a global picture of the many aspects involved in the notification process). Despite the overlapping, we identified four dimensions as representative of the main aspects emerging from the studies. With the term “dimensions,” we want to indicate the main themes that emerged from the content analysis phase, i.e., summaries of information relating to a particular topic or domain of data with shared meanings. In particular, the identification of dimensions followed a reflexive, deductive thematic analysis phase. Once the data collection was complete, four researchers of the team (JZ, AVG, SD, SB) performed individually the analysis phases, during which they took notes on their initial impressions of each article. In a second moment, the contents of interest (i.e., those in line with the research question) were assigned labels (a few words or a short sentence), which had the purpose of clearly evoking the relevant characteristics of the papers, in order to be able to encode them. Then, researchers—with full agreement between them—defined a list of themes, which ended in four dimensions that guided the subsequent research phases. The dimensions identified are: (1) protocols and guidelines (number of studies = 51); (2) emotional reactions of the recipients and those who communicate the news, and/or pathologies that can influence the bereavement process (n = 46); (3) professional figures who perform the notification and recipients of the bad news (n = 59); (4) type of death to be communicated (n = 56) (See Table 1).
As anticipated, the total number of studies from each area exceeds the total number of studies selected due to the overlap of multiple thematic areas within the same study.
Death notification in relation to the first identified dimension concerns the state of the art regarding theories and practical training implemented in communicating death. Here, heterogeneity of collected data and difficulty in distinguishing protocols and guidelines from training programs and simulation exercises should be underlined.
The second area/dimension concerns the role of the emotions of those who communicate and receive the notification of death, and the risk factors/circumstances that can influence the bereavement process (psychopathologies, disabilities, people at risk, etc.).
Nurses, doctors, paramedics, social workers, psychologists, and policemen are placed in the third group of studies as main actors involved in the notification process. Characteristics of the population receiving the notification are also reported in this area.
In relation to the type of death, some studies have addressed the issue of death notification in relation to traumatic deaths, while others have also dealt with natural deaths, or have not specified the type of death or have treated sudden and unexpected death without specifying their cause.
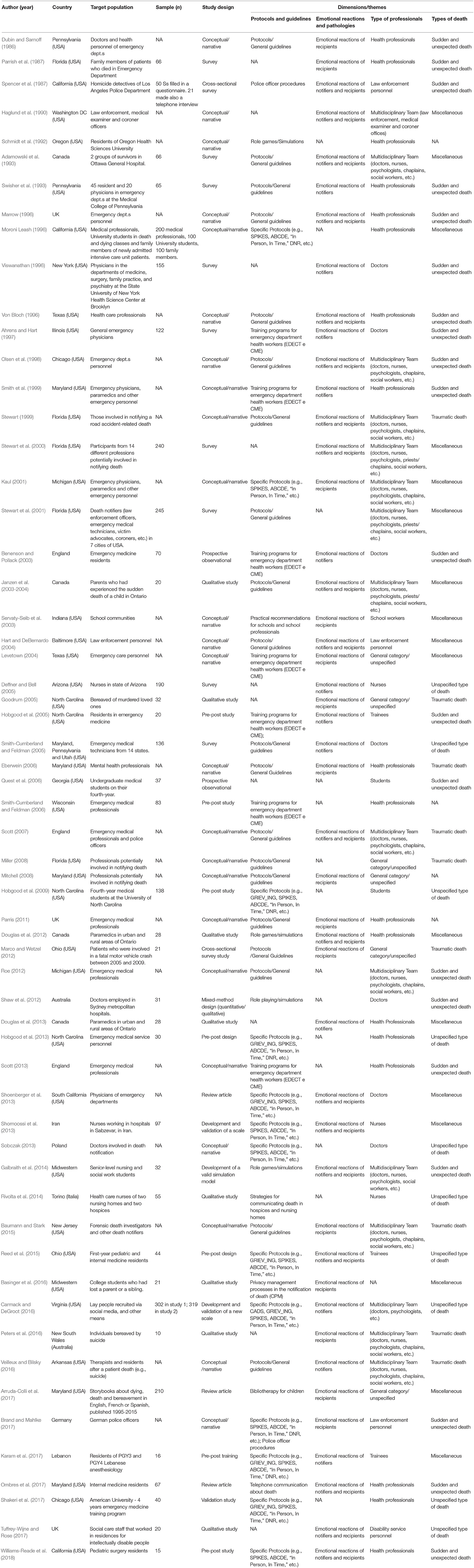
Overall, the evaluation of the 60 studies included in our review revealed the presence of a vast heterogeneity between methodologies and research designs. The typology of the studies appeared distributed as follows (Table 2): conceptual/narrative studies (n = 24), surveys (n = 9), cross-sectional surveys (n = 2), reviews (n = 3), qualitative studies (n = 8), pre-post design studies (n = 7), validation studies (n = 4), prospective observational (n = 2), mixed-method design study (qualitative/quantitative) (n= 1). The prevalence of conceptual/narrative studies within our review and the scarcity of quantitative studies did not permit to aggregate data and provide numbers resulting from contamination. It was not possible to trace the risk of bias of each individual study and carry out an assessment of the outcome and results of each individual work. From our review of the literature we tried to obtain a picture of the state of art of a topic we consider of importance, such as the problem of death communication in the event of an unexpected, traumatic, and violent death.
First Dimension: Protocols and Guidelines
In relation to the first dimension, a total of 51 studies concerning death notification have highlighted the current state of the art regarding intervention plans, guidelines, strategies and protocols to make an adequate communication (see Table 2). In this dimension, a total of 20 studies focused on the description of general protocols and general guidelines that can be used during the death notification process (Table 2).
A total of 7 studies focused on the description of training programs for emergency department health workers aimed at improving the communication skills of the professionals involved in the role of notifier (Table 2). Only one study highlighted the usefulness of a specific training on death education in critical emergency situations, called the “Emergency Death Education and Crisis Training” (EDECT) program. It is a theoretical-experiential training that proposes role-playing and group activities, aimed at modifying the attitudes with respect to the theme of death and most common behaviors of emergency doctors who must carry out death communication. The program also includes specific medical education hours on the notification process (CME) (Smith-Cumberland and Feldman, 2006).
A total of 13 studies have investigated some specific protocols that can be used as a reference during a death notification (Table 2). One of the most used is the GRIEV_ING protocol (Hobgood et al., 2009, 2013; Shoenberger et al., 2013; Reed et al., 2015; Carmack and DeGroot, 2016; Karam et al., 2017; Shakeri et al., 2017). In this regard, the importance of an educational intervention, based on simulation, is highlighted for the acquisition of the skills necessary to face a death notification. In the United States, one of the most popular protocols is the so-called “Six-Step Protocol” for the delivery of bad news (SPIKES: acronym for the words Setting, Perception, Invitation, Knowledge and Empathy). It is a protocol aimed primarily at doctors who provide information on unfavorable prognoses, but can also be used to inform the family of the death of a patient (Scott, 2013; Shomoossi et al., 2013; Williams-Reade et al., 2018). One study described the ABCDE notification strategies that propose accurate intervention plans for healthcare professionals who are required to make a death notification (Shomoossi et al., 2013). A study examined a further protocol, developed by Dyer (2001), in which the more general guidelines for the notification of death are expanded, adding rules relating to telephone communication and the timing appropriate for meeting with the person to whom the death news should be referred (Sobczak, 2013). A study focuses on the communication protocol “In Person, In Time,” which provides useful information to effectively reduce the stress level of the notifier at the time of communication (Sobczak, 2013). An article focused on a learning program, called the DNR approach (Brand and Mahlke, 2017): it is an educational program useful to facilitate learning, based on practical experiences within peer groups, to strengthen notification skills. Four studies have highlighted the usefulness of role-playing and immersive simulation experiences of the notification process (Schmidt et al., 1992; Douglas et al., 2012; Shaw et al., 2012; Galbraith et al., 2014). Two studies have shown notification procedures for law enforcement, in particular police officers, often involved in traumatic death experiences, such as traffic accidents, suicides and homicides (Spencer et al., 1987; Brand and Mahlke, 2017).
A study highlighted the importance of protecting privacy in the information provided to partner/family/friends during the notification of the death of a loved one (Basinger et al., 2016). Another study presented strategies on how to make an adequate death notification commencing by a phone call (Ombres et al., 2017). Whenever possible, phone calls should not be the only way to communicate the traumatic death of someone: direct contact with survivors should always be encouraged.
An article described practical recommendations for notification of death to students in case of a loss within the school environment (Servaty-Seib et al., 2003).
Another study highlighted the potential of bibliotherapy as a tool to facilitate the communication about death to children who need to face the loss of a loved one (Arruda-Colli et al., 2017). A study described some techniques and strategies for communicating the death of a resident in nursing homes and hospice-type structures (Rivolta et al., 2014).
Second Dimension: Emotional Reactions of Notifiers and Recipients and Circumstances or Pathologies That Can Influence the Bereavement Process
A total of 46 studies (Table 2) have investigated death notification in relation to the main emotional experiences that accompany a death notification process, taking into account both the experience of the notifier and those who receive the news. A total of 19 studies (Table 2) described the notification process, taking into account both perspectives. From the notifier's point of view, the notification process is mostly judged as difficult and stressful (Adamowski et al., 1993; Stewart et al., 2000; Janzen et al., 2003-2004; Hart and DeBernardo, 2004; Douglas et al., 2012; Williams-Reade et al., 2018). The reactions most commonly described by the notifier are: anxiety, guilt, sadness, identification with the target, discomfort, avoidance, anguish, frustration, isolation, insomnia, lowering of mood, recurrent nightmares, feelings of helplessness, substance abuse, marital conflict, PTSD, chronic stress response syndrome, and professional burnout (Spencer et al., 1987; Veilleux and Bilsky, 2016; Tuffrey-Wijne and Rose, 2017). In general, professionals involved in communicating the death of a person highlighted a lack of sufficient preparation for carrying out the task and the need to acquire more skills for managing the emotional reactions of those who receive the bad news and own emotions (Olsen et al., 1998; Douglas et al., 2013). Considering the target's perspective, the notification task is more commonly associated with reactions such as: emotional trauma, pain, despair, anger, crying, screaming, sadness, aggression, depression, emotional distress, strengthening of significant relationship ties, perception of stigma, social isolation, avoidance of relationships, distress, sense of emptiness, increased heart rate, fainting, cardiac arrest, and nausea (Haglund et al., 1990; Adamowski et al., 1993; Janzen et al., 2003-2004; Hart and DeBernardo, 2004; Scott, 2007; Galbraith et al., 2014; Basinger et al., 2016).
Twelve studies dealt in particular with the notifier's emotional experience and a total of 15 studies (Table 2) examined the experience of recipients. With regards to the notification experience from the side of the notifier, some detailed information is provided regarding the long-term effects of stress and discomfort perceived during the process, as well as some of the most common psychopathological risk factors (Stewart, 1999; Hobgood et al., 2013). Finally, the studies that highlight the main reactions of those who receive a death notification underline the devastating impact that this experience, if not adequate, could have in the lives of recipients, as well as the significant influence of this experience on the bereavement process and on the onset of psychopathology and possible increase in suicidal risk. Sudden and violent deaths can trigger acute psychological responses; they can increase the risk of developing complicated bereavement, in addition to the onset of physical and psychological symptoms. In turn, these could lead to an increase in suicidal risk and general mortality (Kaul, 2001; Mitchell, 2008; Parris, 2011; Baumann and Stark, 2015; Peters et al., 2016; Brand and Mahlke, 2017; Ombres et al., 2017).
Third Dimension: Professional Figures Involved in the Notification Process
Nearly all studies (n = 59) dealt with this aspect (Table 2). The review revealed significant diversity among operators involved in the death notification process. The professional category most involved in the role of notifier is that of healthcare workers (evidenced in 18 studies). In six studies, professional role of the notifier is unspecified. In others, several professional figures are seen as working synergistically—in communicating the death of a person—within a multidisciplinary team (n = 15). Among these are: medical and nursing staff, religious officers and priests, psychologists, social workers, etc.) (Table 2). A total of seven studies highlighted the role of doctors in the death notification task. Three studies focused on the role of law enforcement officers. Three articles focused on the figure of nurses; another study on that of school operator. Students are also the target of two studies as well as studies on trainees (n = 3). Finally, one article considered staff working in services for people with disabilities (see Table 2 for specific references).
Fourth Dimension: Type of Death to Be Notified
When it comes to death notification, it is fundamental to dwell on the peculiar characteristics of each type of death to examine the components that may influence the different loss experiences. A death from natural causes has a very different impact on partner/family/friends than a death from sudden and violent causes. A total of 56 studies focused on providing information about the different types of death. Nine studies focused on traumatic death experiences (such as traffic accidents, suicides, murders, overdoses) (Table 2). Other studies have examined deaths both from sudden and unexpected causes (n = 20); in some studies the theme of death has been studied without specifying its type (n = 10); finally, a number of studies (n = 17) have considered a miscellaneous ensemble of deaths (traumatic, unexpected and sudden, by disease, natural) (Table 2).
Discussion
In recognition of the importance of the notification process, protocols, and recommendations have been developed to help professionals and rescuers called to perform death notifications (Hall, 1982; Parrish et al., 1987; Collins, 1989; Wells, 1993; Williams and Frangesch, 1995; Byers, 1996; Ptacek and Eberhardt, 1996; Von Bloch, 1996; Spungen, 1998; Boss, 1999, 2002; Stewart, 1999; Benenson and Pollack, 2003; Miller, 2003a,b, 2004; Eberwein, 2006; Nardi and Keefe-Cooperman, 2006). It is important, in fact, that notifiers (doctors and other health workers, psychologists, priests, members of law enforcement, and the school community) do not underestimate the impact that they could have during the first meeting with the partner/family/friends of the deceased. Professionals who do not develop an awareness of how their attitudes can influence the notification process are likely to cause more stress in recipients, often in an unintended way, and to live the moment of communication with greater anxiety.
Ideally, the notifier should be well-informed about the details of the death, have enough time to support the survivors of the deceased, and be able to respond to the physical and emotional reactions exhibited by them (denial, anger, aggression, withdrawal, isolation, tears, pain, guilt, fear, etc.) (Wright, 1996). It is also important to consider the psychophysical characteristics of the individuals who are going to be informed, and evaluate the secondary health risks that may arise following the notification of death. In some cases, it may be useful to evaluate suicide risk or to take individual risk factors into account. For example, it often happens that people with intellectual disabilities are over-protected and often not informed of the death of a loved one (Tuffrey-Wijne and Rose, 2017).
What emerges from the literature is that not much information is available on how to deal with sudden death, and that there is still a shortage of educational material in this area for emergency professionals (Smith et al., 1999). In addition, standardized protocol for making death notifications by phone in different contexts appear to be lacking (Ombres et al., 2017). The professional figures mainly called to deal with the notification processes often do not receive adequate training to learn how to provide painful communications in the most appropriate way. This causes the notification process to be perceived as a particularly difficult and stressful event for notifiers, as well as for those who are required to receive the bad news. It is known, in fact, that this task emotionally involves not only the family members and other survivors of the deceased but also the professionals who are called to communicate death (Meunier et al., 2013). Moreover, communicating death to a close person or family member without an adequate strategic plan can contribute to aggravating the pain of loss (Mitchell, 2008; Ombres et al., 2017). Improving the notifiers' skills and competences, along with understanding the possible reactions of those who receive a death report, can increase the chances that the death notification process may result as sensitive, empathetic, respectful, and compassionate.
The importance of an intervention that aims to facilitate the bereavement process from a traumatic loss has been discussed in the literature by taking into consideration the contribution of different professional groups, including the clergy (Frantz et al., 1996; Weaver et al., 1996), health workers (Gyulay, 1989) and law enforcement (Clark, 1981). A multidisciplinary team engaged in the notification process can be made up of doctors, nurses, psychologists, social workers, policemen, priests and, in general, sensitive, professional and caring staff who act through a cooperative and coordinated approach (Walters and Tupin, 1991; Adamowski et al., 1993; Anderson, 1993). It is essential, in fact, that each team member is aware of their role and the complexity of the notification process, in order to promote and ensure effective support for survivors (Young et al., 2012; Groos and Shakesperare-Finch, 2013).
In this regard, the need for a deeper understanding of the problems that people face when losing a loved one has been well-highlighted, as well as the need for professionals to be better trained in the difficult task of death notification (Gyulay, 1989; Kalkofin, 1989; Neidig and Dalgas-Pelish, 1991; Weaver, 1993; Parry, 1994; Weaver et al., 1996). There is evidence that most staff have a desire to improve their notification skills for managing crisis situations, especially in emergency settings (Olsen et al., 1998).
Studies outlining protocols and guidelines have highlighted some aspects to be especially promoted in the notification process: simplicity, brevity, practicality, proximity, immediacy, and expectation of a reasonable result (Aguilera, 1998; Mitchell, 2004). Some studies have supported the preventive importance of a skilled and sensitive death notification, through a set of fundamental tasks and events, deemed salient regardless of who makes the notification and the setting in which it is carried out. To perform a “proper” death notification, the various components include: (a) correct identification of both the deceased person and the partner/family/friends to be notified; (b) a first contact (preferably not by telephone) with the survivors and an invitation to a meeting at their home or hospital; (c) to provide all the details about the accident and the medical procedures implemented (if any). It has been seen that both the physical setting in which information is given and the speed with which it is exposed can significantly influence the survivors' ability to assimilate all the details of communication; (d) to provide the news of death. In this regard, it is important to use clear and direct language and avoid the use of euphemisms, especially in dealing with children; (e) to respond to survivors' reactions by offering immediate emotional support; (f) to give the opportunity to view the body after the notification; (g) to offer short and long-term assistance through follow-up following the notification process, which guarantees survivors that they may obtain further information on death circumstances (this is particularly important for those types of losses that involve a high risk of developing PTSD) (Dubin and Sarnoff, 1986; Spencer et al., 1987; Cooke, 1993; Tye, 1993; Stewart, 1999; Stone et al., 1999; Kaul, 2001; Stewart et al., 2001; Li et al., 2002).
Several studies that examined the impact on recipients for the notification received revealed significantly worse results if death, and in particular the causes of death, were communicated by telephone. The limits of this approach—which should only be used in cases where survivors are really far away (Stewart, 1999)—have been repeatedly stressed. Nevertheless, telephone notification is still a widely used communication method, in particular by law enforcement officers when they are required to report deaths resulting from road accidents, homicides and/or suicides (Spencer et al., 1987; Stewart, 1999; Miller, 2008). In the particular case of deaths resulting from a murder, it would be appropriate to inform the deceased's partner or family members of the possibility that the media can contact them. It would be also useful to provide them with suggestions on how to manage various aspects, including those related to the protection of privacy (Clark, 2011; Baumann and Stark, 2015).
At least one study has tried to identify practices related to death notification deemed less useful by survivors (Eberwein, 2006). From what emerged, notifiers should avoid providing unsolicited advice or encouragement for a rapid recovery. During notification, they should not endorse any specific emotional attitude or attempt to identify with the survivor's experience. Instead, positive notification approaches would include: authentic expressions of closeness and concern on the part of the notifier, and the opportunity to let survivors venting their feelings while counting on the presence of another person during the notification process. Another aspect considered as important is the type of language to be used (clear, simple, and direct) and the tone of voice (which should express confidence). These are details, in fact, that a survivor could potentially remember throughout his/her life and therefore deserve special attention. On the other hand, people who are experiencing a loss first of all need respect, a fundamental prerequisite for an adequate notification of death (Eberwein, 2006).
The review also revealed that it would be important being able to predict possible emotional responses of survivors, in order to carefully select notifiers, keeping in mind the personality of each operator and their communicative and expressive styles (Adamowski et al., 1993). It has been seen, for example, that a person with high anxiety levels, with fear of death and strong apprehension related to communication, could feel strongly unable to manage a notification process and be predisposed to avoiding issues related to death (Daly and McCroskey, 1984). Indeed, it must be considered that the notification process is a highly stressful task for notifiers, both physically and emotionally (Hart and DeBernardo, 2004). On the other hand, it has been seen that staff anxiety could be reduced with a better understanding of the responses experienced by survivors at the time of notification (Finlay and Dallimore, 1991), such as denial, withdrawal, anger, sadness, isolation, and self-reported auto- or hetero guilt feelings (in the case of deaths by suicide and murder) (Wright, 1996; Constantino et al., 2002).
To date, there are still few studies describing initiatives with training programs that provide practical recommendations on who should carry out a death notification and how and when this should take place. Educational programs have been proposed to improve communication skills (Nordstrom et al., 2011), as well as the integration of death notification protocols within University courses of those students potentially involved in emergency situations (Baghcheghi et al., 2011). The GRIEV_ING Death Notification Program is among the most popular protocols; through the enhancement of specific immersive experiences, simulations and roleplaying, it aims to improve the communication skills necessary to face a death notification task within different contexts (Benenson and Pollack, 2003; Karam et al., 2017). The GRIEV_ING educational intervention is considered useful in improving the notifier's self-efficacy and the general sense of trust within the notification process. Focused on promoting the development of empathic communication, the intervention prepares notifiers to competently address emotionally charged topics, frequently associated with increased stress (Hobgood et al., 2005).
In addition to improved ability to notify, some studies have demonstrated the usefulness of these programs also in improving the self-esteem of the personnel involved in the demanding task of death notification, limiting work stress and burnout (Karam et al., 2017).
Limitations of the Study
Our review has several limitations. First, there was no review protocol. Second, only studies written in English were taken into consideration. Third, the between-study heterogeneity was high with regards to study design, quality of study, types of death, and targets, making quite difficult to create standardized categorizations for all articles. In addition, thematic overlaps were frequent, with the majority of studies reporting general indications on all important areas of the topic, sometimes in a succinct manner, some others in a quite extended one. These limits, together with the difficulty—on some occasions—in distinguishing between guidelines and training programs, created difficulties in the interpretation of results; for example, it was not easy to derive specific indications for specific circumstances. Furthermore, the scarcity of quantitative study doesn't allow identifying the advantages of certain types of intervention compared to others.
Conclusions
The review of the literature and the content analysis underlined the complexity of the death notification process. Numerous variables affect its impact: circumstances of death; quality of communication (verbal or non-verbal); characteristics of the context in which the notification is carried out; presence or absence of sources of support for survivors, personality characteristics of notifier and recipient; etc.
The complexities of this sensitive area reinforce the view that more research is needed, and training gaps exist within the professional paths of the figures potentially involved in this difficult task (Smith et al., 1999; Smith-Cumberland and Feldman, 2005).
Notification skills could be improved through specific educational programs, which can direct eventual notifiers toward the acquisition of communication abilities useful for the management of emergency situations. Some of the training courses and protocols that already exist, in fact, can constitute a resource for improving one's sense of self-efficacy and general confidence in dealing with emotionally charged topics and highly stressful situations (Parrish et al., 1987; Sykes, 1989; Iserson, 1999). The painful experience of having to know that a loved one unexpectedly died can be somewhat contained and alleviated by the use of structured and multidisciplinary approaches by notifiers, as a result of staff education campaigns (Adamowski et al., 1993). Raising awareness on the consequences of a bad notification process and its long-term impact appears as particularly important. Future work could focus on aspects that are still not very well-profiled, such as the definition of notification procedures taking into account situational differences, and professional and personal characteristics of the figures most frequently involved in the task.
Author Contributions
DDL has conceived the work, coordinated the study, and written the final manuscript. AS and CA have contributed to the early stages of the research with literature searches and summary reports. JZ provided literature search and scrutiny and several paper drafts. AVG and SD have contributed to searches and to draft parts of this review. SB made the literature search and screening of papers. All authors contributed to the article and approved the submitted version.
Funding
DDL Fund has supported this study with a liberal grant.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2020.02229/full#supplementary-material
References
Adamowski, K., Dickinson, G., Weitzman, B., Roessler, C., and Carter-Snell, C. (1993). Sudden unexpected death in the emergency department: caring for the survivors. Can. Med. Assoc. J. 149, 1445–1451.
Ahrens, W. R., and Hart, R. G.. (1997). Emergency physicians' experience with pediatric death. Am. J. Emerg. Med. 15, 642–643. doi: 10.1016/S0735-6757(97)90177-7
Armour, M. (2003). Meaning making in the aftermath of homicide. Death Stud. 27, 519–540. doi: 10.1080/07481180302884
Arruda-Colli, M. N. F., Weaver, M. S., and Wiener, L. (2017). Communication about dying, death, and bereavement: a systematic review of children's literature. J. Palliat. Med. 20, 548–559. doi: 10.1089/jpm.2016.0494
Baghcheghi, N., Koohestani, H. R., and Rezaei, K. (2011). A comparison of the cooperative learning and traditional learning methods in theory classes. Nurse Educ. Today 31, 877–882. doi: 10.1016/j.nedt.2011.01.006
Basinger, E. D., Wehrman, E. C., and McAninch, K. G. (2016). Grief communication and privacy rules: examining the communication of individuals bereaved by the death of a family member. J. Fam. Commun. 16, 285–302. doi: 10.1080/15267431.2016.1182534
Baumann, R., and Stark, S. (2015). The role of forensic death investigators interacting with the survivors of death by homicide and suicide. J. Forensic Nurs. 11, 28–32. doi: 10.1097/JFN.0000000000000058
Benenson, R. S., and Pollack, M. L. (2003). Evaluation of emergency medicine resident death notification skills by direct observation. Acad. Emerg. Med. 10, 219–223. doi: 10.1197/aemj.10.3.219
Boss, P. (1999). Ambiguous Loss: Learning to Live With Unresolved Grief. Cambridge, MA: Harvard University Press.
Boss, P. G. (2002). Ambiguous loss: working with families of the missing. Fam. Process. 41, 14–17. doi: 10.1111/j.1545-5300.2002.40102000014.x
Brand, M., and Mahlke, K. (2017). “DNR and the Use of Blended Learning Methodology in German Police Education”, in Advances in Web-Based Learning - ICWL 2017: 16th International Conference, Cape Town, South Africa, September 20-22, 2017, Proceedings, eds H. Xie, E. Popescu, G. Hancke, B. Fernández Manjón (Cham: Springer), 196–201. doi: 10.1007/978-3-319-66733-1_21
Byers, B. (1996). “Death notification: theory and practice,” in Crisis Intervention in Criminal Justice Social Service. eds. J. E. Hendricks and B. Byers (Springeld, IL: CC. Thomas), 287–319.
Carmack, H. J., and DeGroot, J. M. (2016). Development and validation of the communication apprehension about death scale. J. Death Dying 74, 239–259. doi: 10.1177/0030222815598440
Clark, D. (1981). A death in the family: providing consultation to the police on the psychological aspects of suicide and accidental death. Death Educ. 5, 143–155. doi: 10.1080/07481188108252088
Clark, S. (2011). Death Investigation: A Guide for the Scene Investigator. U.S. Department of Justice, Office of Justice Programs: Washington DC.
Collins, S. (1989). Sudden death counseling protocol. Dimens. Crit. Care Nurs. 8, 375–382. doi: 10.1097/00003465-198911000-00016
Constantino, R., Crane, P., Symonds, H., and Sutton, L. (2002). The role of the forensic nurse in the assessment of abuse among female suicide survivors. For. Examiner 11, 22–28.
Cooke, M. (1993). Care of the bereaved in the accident and emergency department. Care Crit Ill 9, 199–201.
Daly, J. A., and McCroskey, J. C. (1984). Avoiding Communication: Shyness, Reticence, and Communication Apprehension. Beverly Hills, CA: Sage.
Deffner, J. M., and Bell, S. K. (2005). Nurses' death anxiety, comfort level during communication with patients and families regarding death, and exposure to communication education. J. Nurses Staff Dev. 21, 19–23. doi: 10.1097/00124645-200501000-00005
Douglas, L. A., Cheskes, S., Feldman, M., and Ratnapalan, S. (2012). Paramedics' experiences with death notification: a qualitative study. J. Paramedic Pract. 4, 533–539. doi: 10.12968/jpar.2012.4.9.533
Douglas, L. A., Cheskes, S., Feldman, M., and Ratnapalan, S. (2013). Death notification education for paramedics: past, present and future directions. J. Paramedic Pract. 5, 152–159. doi: 10.12968/jpar.2013.5.3.152
Dubin, W. R., and Sarnoff, J. R. (1986). Sudden unexpected death: intervention with the survivors. Ann. Emerg. Med. 15, 54–57. doi: 10.1016/S0196-0644(86)80488-7
Dyer, K. A. (2001). Death pronouncement and death notification: what the resident needs to know. Dealing with Death & Dying in Medical Education and Practice. Available from: EPERC (End-of-Life Physician Education Resource Center) www.eperc.mcw.edu
Eberwein, K. E. (2006). A mental health clinician's guide to death notification. Int. J. Emerg. Ment. Health 8, 117–126.
Finlay, I., and Dallimore, D. (1991). Your child is dead. Br. Med. J. 302, 1524–1525. doi: 10.1136/bmj.302.6791.1524
Frantz, T., Trolley, B., and Johll, M. (1996). Religious aspects of bereavement. Pastoral Psychol. 44, 151–163. doi: 10.1007/BF02251401
Galbraith, A., Harder, N., Macomber, C. A., Roe, E., and Roethlisberger, K. S. (2014). Design and implementation of an interprofessional death notification simulation. Clin. Simul. Nurs. 10, 95–102. doi: 10.1016/j.ecns.2013.08.003
Goodrum, S. (2005). The interaction between thoughts and emotions following the news of a loved one's murder. Omega 51, 143–160. doi: 10.2190/A69T-3GLW-A9PR-5QTH
Groos, A., and Shakesperare-Finch, J. (2013). Positive experiences for participants in suicide bereavement groups: a grounded theory model. Death Stud. 37, 1–24. doi: 10.1080/07481187.2012.687898
Gyulay, J. (1989). Sudden death: no farewells. Special issue: the death of a child. Issues Compr. Pediatr. Nurs. 12, 71–101. doi: 10.3109/01460868909038030
Haglund, W., Reay, D. T., and Fligner, C. L. (1990). Death notification. Am. J. Forensic Med. Pathol. 11, 342–347. doi: 10.1097/00000433-199012000-00016
Hall, M. (1982). Law enforcement officers and death notification: a plea for relevant education. J. Police Sci. Admin. 10, 189–193.
Hart, C. W., and DeBernardo, C. R. (2004). Death notification: considerations for law enforcement personnel. Int. J. Emerg. Ment. Health. 1, 33–37.
Hobgood, C., Harward, D., Newton, K., and Davis, W. (2005). The educational intervention “GRIEV_ING” improves the death notification skills of residents. Acad. Emerg. Med. 12, 296–301. doi: 10.1197/j.aem.2004.12.008
Hobgood, C., Mathew, D., Woodyard, D. J., Shofer, F. S., and Brice, J. H. (2013). Death in the field: teaching paramedics to deliver effective death notifications using the educational intervention “GRIEV_ING”. Prehosp. Emerg. Care 17, 501–510. doi: 10.3109/10903127.2013.804135
Hobgood, C. D., Tamayo-Sarver, J. H., Hollar, D. W. Jr, and Sawning, S. (2009). GRIEV_ING: death notification skills and applications for fourth-year medical students. Teach. Learn. Med. 21, 207–219. doi: 10.1080/10401330903018450
Horowitz, M. J., Siegel, B., Holsen, A., Bonnano, G. A., Milbrath, C., and Stinson, C. H. (1997). Diagnostic criteria for complicated grief disorder. Am. J. Psychiatry 154, 904–910. doi: 10.1176/ajp.154.7.904
Iserson, K. (1999). Grave Words: Notifying Survivors About Sudden, Unexpected Deaths. Tucson, AZ: Galen Press. doi: 10.1136/ewjm.173.4.261
Janzen, L., Cadell, S., and Westhues, A. (2003-2004). From death notification through the funeral: bereaved parents'experiences and their advice to professionals. Omega 48, 149–164. doi: 10.2190/6XUW-4PYD-H88Q-RQ08
Kalkofin, R. (1989). After a child dies: a funeral director's perspective. Issues Compr. Pediatr. Nurs. 12, 285–297. doi: 10.3109/01460868909026836
Karam, V. Y., Barakat, H., Aouad, M., Harris, I., Park, Y. S., Youssef, N., et al. (2017). Effect of a simulation-based workshop on breaking bad news for anesthesiology residents: an intervention study. BMC Anesthesiol. 17:77. doi: 10.1186/s12871-017-0374-7
Kaul, R. E. (2001). Coordinating the death notification process: the roles of the emergency room social worker and physician following a sudden death. Brief Treat. Crisis Interv. 1, 101–114. doi: 10.1093/brief-treatment/1.2.101
Levetown, M. (2004). Breaking bad news in the emergency department. Top Emerg. Med. 26, 35–43. doi: 10.1097/00132981-200405000-00026
Li, S. P., Chan, C. W., and Lee, T. (2002). Helpfulness of nursing actions to suddenly bereaved family members in an accident and emergency setting. J. Adv. Nurs. 40, 170–180. doi: 10.1046/j.1365-2648.2002.02359.x
Marco, C. A., and Wetzel, L. R. (2012). Communication with survivors of motor vehicle crashes. Emerg. Med. J. 29, 626–629. doi: 10.1136/emermed-2011-200059
Marrow, J. (1996). Telling relatives that a family member has died suddenly. Postgrad. Med. J. 72, 413–418. doi: 10.1136/pgmj.72.849.413
Meunier, J., Merckaert, I., Libert, Y., Delvaux, N., Etienne, A. M., Liénard, A., et al. (2013). The effect of communication skills training on residents' physiological arousal in a breaking bad news simulated task. Patient Educ. Couns. 93, 40–47. doi: 10.1016/j.pec.2013.04.020
Miller, L. (2003a). Psychological interventions for terroristic trauma: symptoms, syndromes, and treatment strategies. Psychotherapy 39, 283–296. doi: 10.1037/0033-3204.39.4.283
Miller, L. (2003b). Family therapy of terroristic trauma: psychological syndromes and treatment strategies. Am. J. Fam. Ther. 31, 257–280. doi: 10.1080/01926180390201963
Miller, L. (2004). Psychotherapeutic interventions for survivors of terrorism. Am. J. Psychother. 58, 1–16. doi: 10.1176/appi.psychotherapy.2004.58.1.1
Miller, L. (2008). Death notification for families of homicide victims: healing dimensions of a complex process. Omega 57, 367–380. doi: 10.2190/OM.57.4.c
Mitchell, J. T. (2004). Characteristics of successful early intervention programs. Int. J. Emerg. Ment. Health. 6, 175–184.
Moroni Leash, R. (1996). Death notification: pratical guidelines for health care professionals. Crit. Care Nurs. Q. 19, 21–34. doi: 10.1097/00002727-199605000-00005
Murphy, S. A., Johnson, C., and Lohan, J. (2002). The aftermath of the violent death of a child: an integration of the assessments of parents' mental distress and PTSD during the first five years of bereavement. J. Loss Trauma 7, 203–222. doi: 10.1080/10811440290057620
Nardi, T. J., and Keefe-Cooperman, K. (2006). Communicating bad news: a model for emergency mental health helpers. Int. J. Emerg. Ment. Health 8, 203–207.
Neidig, J., and Dalgas-Pelish, P. (1991). Parental grieving and perceptions regarding health care professionals' interventions. Issues Compr. Pediatr. Nurs. 15, 179–191. doi: 10.3109/01460869109014497
Neimeyer, R. A., Prigerson, H. G., and Davies, B. (2002). Mourning and meaning. Am. Behav. Sci. 46, 235–251. doi: 10.1177/000276402236676
Nordstrom, A., Fjellman-Wiklund, A., and Grysell, T. (2011). Drama as a pedagogical tool for practicing death notification experiences from Swedish medical students. BMC Med. Educ. 11:74. doi: 10.1186/1472-6920-11-74
Olsen, J. C., Buenefe, M. L., and Falco, W. E. (1998). Death in the emergency department. Ann. Emerg. Med. 31, 758–765. doi: 10.1016/S0196-0644(98)70236-7
Ombres, R., Montemorano, L., and Becker, D. (2017). Death notification: someone needs to call the family. J. Palliat. Med. 20, 672–675. doi: 10.1089/jpm.2016.0481
Parris, R. J. (2011). Initial management of bereaved relatives following trauma. Trauma 14, 139–155. doi: 10.1177/1460408611420352
Parrish, G. A., Holdren, K. S., Skiendzielewski, J. J., and Lumpkin, O. A. (1987). Emergency department experience with sudden death: a survey of survivors. Ann. Emerg. Med. 16, 792–796. doi: 10.1016/S0196-0644(87)80577-2
Parry, J. (1994). Death review: an important component of grief resolution. Soc. Work Health Care. 20, 95–110. doi: 10.1300/J010v20n02_06
Peters, K., Cunningham, C., Murphy, G., and Jackson, D. (2016). Helpful and unhelpful responses after suicide: experiences of bereaved family members. Int. J. Ment. Health Nurs. 25, 418–425. doi: 10.1111/inm.12224
Ptacek, J. T., and Eberhardt, T. L. (1996). Breaking bad news: a review of the literature. J. Am. Med. Assoc. 276, 496–502. doi: 10.1001/jama.1996.03540060072041
Quest, T. E., Ander, D. S., and Ratcliff, J. J. (2006). The validity and reliability of the affective competency score to evaluate death disclosure using standardized patients. J. Palliat. Med. 9, 361–370. doi: 10.1089/jpm.2006.9.361
Reed, S., Kassis, K., Nagel, R., Verbeck, N., Mahan, J. D., and Shell, R. (2015). Breaking bad news is a teachable skill in pediatric residents: a feasibility study of an educational intervention. Patient Educ. Couns. 98, 748–752. doi: 10.1016/j.pec.2015.02.015
Rivolta, M. M., Rivolta, L., Garrino, L., and Di Giulio, P. (2014). Communication of the death of a patient in hospices and nursing homes: a qualitative study. Eur. J. Oncol. Nurs. 18, 29–34. doi: 10.1016/j.ejon.2013.09.012
Roe, E. (2012). Practical strategies for death notification in the emergency department. J. Emerg. Nurs. 38, 130–134. doi: 10.1016/j.jen.2010.10.005
Schmidt, T. A., Norton, R. L., and Tolle, S. (1992). Sudden death in the ED: educating residents to compassionately inform families. J. Emerg. Med. 10, 643–647. doi: 10.1016/0736-4679(92)90155-M
Scott, T. (2007): Sudden traumatic death: caring for the bereaved. Trauma 9, 103–109. doi: 10.1177/1460408607084127.
Scott, T. (2013). Sudden death in emergency care: responding to bereaved relatives. Emerg. Nurse 21, 36–39. doi: 10.7748/en2013.12.21.8.36.e1237
Servaty-Seib, H. L., Peterson, J., and Spang, D. (2003). Notifying individual students of a death loss: practical recommendations for schoolsand school counselors. Death Stud. 27, 167–186. doi: 10.1080/07481180302891
Shakeri, N., Fant, A., Gisondi, M. A., and Salzman, D. (2017). Assessment of death notification skills among emergency medicine residents using GRIEV_ING in high-fidelity patient simulation. Med. Sci. Educ. 27, 881–886. doi: 10.1007/s40670-017-0449-6
Shaw, J., Dunn, S., and Heinrich, P. (2012). Managing the delivery of bad news: an in-depth analysis of doctors' delivery style. Patient Educ. Couns. 87, 186–192. doi: 10.1016/j.pec.2011.08.005
Shoenberger, J. M., Yeghiazarian, S., Rios, C., and Henderson, S. O. (2013). Death notification in the emergency department: survivors and physicians. Western J. Emerg. Med. 14, 181–185. doi: 10.5811/westjem.2012.10.14193
Shomoossi, N., Rad, M., Kooshan, M., and Ganjloo, J. (2013). Nurses as death notifiers: a report from nurses in Iran. Life Sci. J. 10, 26–31.
Smith, T. L., Walz, B. J., and Smith, R. L. (1999). A death education curriculum for emergency physicians, paramedics, and other emergency personnel. Prehosp. Emerg. Care 3, 37–41. doi: 10.1080/10903129908958904
Smith-Cumberland, T. L. (1994, 2007). Course Lecture Notes on Death and Dying: Death Notification. Baltimore, MD: University of Maryland.
Smith-Cumberland, T. L., and Feldman, R. H. (2005). A survey of EMT's attitudes toward death. Prehosp. Disaster Med. 20, 184–188. doi: 10.1017/S1049023X00002429
Smith-Cumberland, T. L., and Feldman, R. H. (2006). EMTs'attitudes'toward death before and after a death education program. Prehosp. Emerg. Care. 10, 89–95. doi: 10.1080/10903120500365955
Sobczak, K. (2013). The procedure for death notification—- “In Person, In Time…”, Anaesthesiol. Intensive Ther. 45, 241–243. doi: 10.5603/AIT.2013.0046
Spencer, E., Baron, D. A., and Pynoos, R. S. (1987). Death notification. Bull. Am. Acad. Psychiatry Law 15, 275–281.
Spungen, D. (1998). Homicide: the Hidden Victims. A Guide for Professionals. Thousand Oaks, CA: Sage. doi: 10.4135/9781483327389
Stewart, A. E. (1999). Complicated bereavement and posttraumatic stress disorder following fatal car crashes: recommendations for death notification. Death Stud. 23, 289–321. doi: 10.1080/074811899200984
Stewart, A. E., Lord, J. H., and Mercer, D. L. (2000). A survey of professionals' training and experiences in delivering death notifications. Death Stud. 24, 611–631. doi: 10.1080/07481180050132811
Stewart, A. E., Lord, J. H., and Mercer, D. L. (2001). Death notification education: a needs assessment study. J. Traumatic Stress 14, 221–227. doi: 10.1023/A:1007808220228
Stone, G., Huggon, A., and Nayeem, N. (1999). Telephone follow- up of relatives after sudden death: a survey of relatives views. Int. J. Clin. Pract. 53, 107–109.
Swisher, L. A., Nieman, L. Z., Nilsen, G. J., and Spivey, W. H. (1993). Death notification in the emergency department: a survey of residents and attending physicians. Ann. Emerg. Med. 22, 1319–1323. doi: 10.1016/S0196-0644(05)80117-9
Sykes, N. (1989). Medical students' fears about breaking bad news. Lancet 2:564. doi: 10.1016/S0140-6736(89)90688-0
Tuffrey-Wijne, I., and Rose, T. (2017). Investigating the factors that affect the communication of death-related bad news to people with intellectual disabilities by staff in residential and supported living services: an interview study. J. Intellect. Disabil. Res. 61, 727–736. doi: 10.1111/jir.12375
Tye, C. (1993). Qualified nurses' perceptions of the needs of the suddenly bereaved family members in the accident and emergency department. J. Adv. Nurs. 18, 948–957. doi: 10.1046/j.1365-2648.1993.18060948.x
Veilleux, J. C., and Bilsky, S. A. (2016). After a client death: suicide postvention recommendations for training programs and clinics. Train. Educ. Prof. Psychol. 10, 214–222. doi: 10.1037/tep0000127
Viswanathan, R. (1996). Death anxiety, locus of control, and purpose in life of physicians. Their relationship to patient death notification. Psychosomatics 37, 339–345. doi: 10.1016/S0033-3182(96)71546-3
Von Bloch, L. (1996). Breaking the bad news when sudden death occurs. Soc. Work Health Care 23, 91–97. doi: 10.1300/J010v23n04_07
Walters, D. T., and Tupin, J. P. (1991). Family grief in the emergency department. Emerg. Med. Clin. North Am. 9, 189–207.
Weaver, A. (1993). Psychological trauma: what clergy need to know. Pastoral. Psychol. 41, 385–408. doi: 10.1007/BF01032818
Weaver, A. J., Koenig, H. G., and Ochberg, F. M. (1996). Posttraumatic stress, mental health professionals, and the clergy: a need for collaboration, training, and research. J. Trauma. Stress 9, 847–855. doi: 10.1002/jts.2490090412
Wells, P. J. (1993). Preparing for sudden death: social work in the emergency room. Soc. Work 38, 339–342.
Wheeler, I. (1994). The role of meaning and purpose in life in bereaved parents associated with a self-help group: compassionate friends. Omega 28, 261–271. doi: 10.2190/T531-78GF-8NQ3-7E7E
Williams, M., and Frangesch, B. (1995). Developing strategies to assist sudden-death families: a 10-year perspective. Death Stud. 19, 475–487. doi: 10.1080/07481189508253394
Williams-Reade, J., Lobo, E., Arvizú Whittemore, A., Parra, L., and Baerg, J. (2018). Enhancing residents' compassionate communication to family members: a family systems breaking bad news simulation. Fam. Syst. Health. 36, 523–527. doi: 10.1037/fsh0000331
Keywords: death notification, notifiers, recipients, emotional reaction, training, traumatic death, breaking bad news, receiving communication of death
Citation: De Leo D, Zammarrelli J, Viecelli Giannotti A, Donna S, Bertini S, Santini A and Anile C (2020) Notification of Unexpected, Violent and Traumatic Death: A Systematic Review. Front. Psychol. 11:2229. doi: 10.3389/fpsyg.2020.02229
Received: 12 March 2020; Accepted: 10 August 2020;
Published: 24 September 2020.
Edited by:
Karolina Krysinska, The University of Melbourne, AustraliaReviewed by:
Francisco Javier Cano-García, Sevilla University, SpainJane Mowll, University of New South Wales, Australia
Copyright © 2020 De Leo, Zammarrelli, Viecelli Giannotti, Donna, Bertini, Santini and Anile. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Diego De Leo, d.deleo@griffith.edu.au
 Diego De Leo
Diego De Leo Josephine Zammarrelli
Josephine Zammarrelli Andrea Viecelli Giannotti
Andrea Viecelli Giannotti Stefania Donna
Stefania Donna Simone Bertini
Simone Bertini Anna Santini
Anna Santini Cristina Anile3
Cristina Anile3