- 1Psychiatry Department, Massachusetts General Hospital, Harvard Medical School, Charlestown, MA, United States
- 2Depression Clinical and Research Program, Massachusetts General Hospital, Boston, MA, United States
Major depressive disorder (MDD) is one of the most prevalent mental illnesses in America. Current treatments for MDD are unsatisfactory given high non-response rates, high relapse rates, and undesirable side effects. Accumulating evidence suggests that Tai Chi, a popular mind–body intervention that originated as a martial art, can significantly regulate emotion and relieve the symptoms of mood disorders. In addition, the availability of instructional videos and the development of more simplified and less structured Tai Chi has made it a promising low-intensity mind-body exercise. In this article, we first examine a number of clinical trials that implemented Tai Chi as a treatment for depression. Then, we explore several mechanisms by which Tai Chi may alleviate depressive symptoms, hypothesizing that the intervention may modulate the activity and connectivity of key brain regions involved in mood regulation, reduce neuro-inflammatory sensitization, modulate the autonomic nervous system, and regulate hippocampal neurogenesis. Finally, we discuss common challenges of the intervention and possible ways to address them. Specifically, we pose developing a simplified and tailored Tai Chi protocol for patients with depression, comparatively investigating Tai Chi with other mind–body interventions such as yoga and Baduanjin, and developing new mind–body interventions that merge the advantages of multiple mind–body exercises.
Introduction
Major depressive disorder (MDD) is a highly prevalent mental illness in the United States (1). Psychotherapy and pharmacotherapy are the mainstay treatments for MDD (2). However, treatment of the disorder is associated with substantial direct and indirect costs, and the clinical efficacy of the treatments has been criticized (3–5). Psychotherapy poses significant time costs on both health professionals and patients, and many patients are troubled by medication side effects such as “sexual dysfunction, weight gain, and sleep disturbance” (6). A significant proportion of patients respond only partially to antidepressants and may require augmentation with other agents in order to enhance the limited effect of the medication (7). Given the disadvantages of first-line treatments, some researchers have begun to explore the effectiveness of alternative therapies.
Tai Chi, a popular mind–body intervention, has recently drawn the attention of the public and researchers alike. Traditional Tai Chi training requires direct supervision from mentors following strict postures. With modern technology and video-sharing sites like Youtube, Tai Chi is becoming increasingly accessible to the general public. We feel it qualifies as a low-intensity exercise, for 1) it can be practiced with video alone and does not require the assistance of a formally trained Tai Chi instructor, and 2) more simplified and less structured Tai Chi has been developed in recent years to accommodate different populations.
Tai Chi employs slow, gentle movements, breathing techniques, and cognitive tools (i.e., attention, imagery) to strengthen, integrate, and relax the body and mind (8). It can be practiced by people of all age groups with varying physical conditions and requires very little physical space. The benefits of Tai Chi on MDD have been supported by a number of well-designed studies (9–11). An advantage of using Tai Chi to treat or augment treatment of MDD is that it is safe and not associated with the adverse events commonly seen with pharmacological agents.
Although promising, Tai Chi’s therapeutic effect needs to be further explored, as the underlying mechanism of the intervention remains unclear. Although different styles of Tai Chi exist, none of these styles have been developed to specifically target patients with depression. The complexity of Tai Chi exercise further inhibits its application in patients with depression. Thus, there is an urgent need to develop a simplified Tai Chi protocol that is tailored for depression.
In this manuscript, we first summarize the findings of clinical studies on Tai Chi treatment of depression. Then, we attempt to summarize the potential mechanisms by which the intervention treats depressive symptoms. Finally, we propose a new direction of Tai Chi research, including a new Tai Chi protocol based on these putative mechanisms. Please also see several recently published review papers on the beneficial effects of Tai Chi for individuals with depression and mood disorders (8, 12, 13).
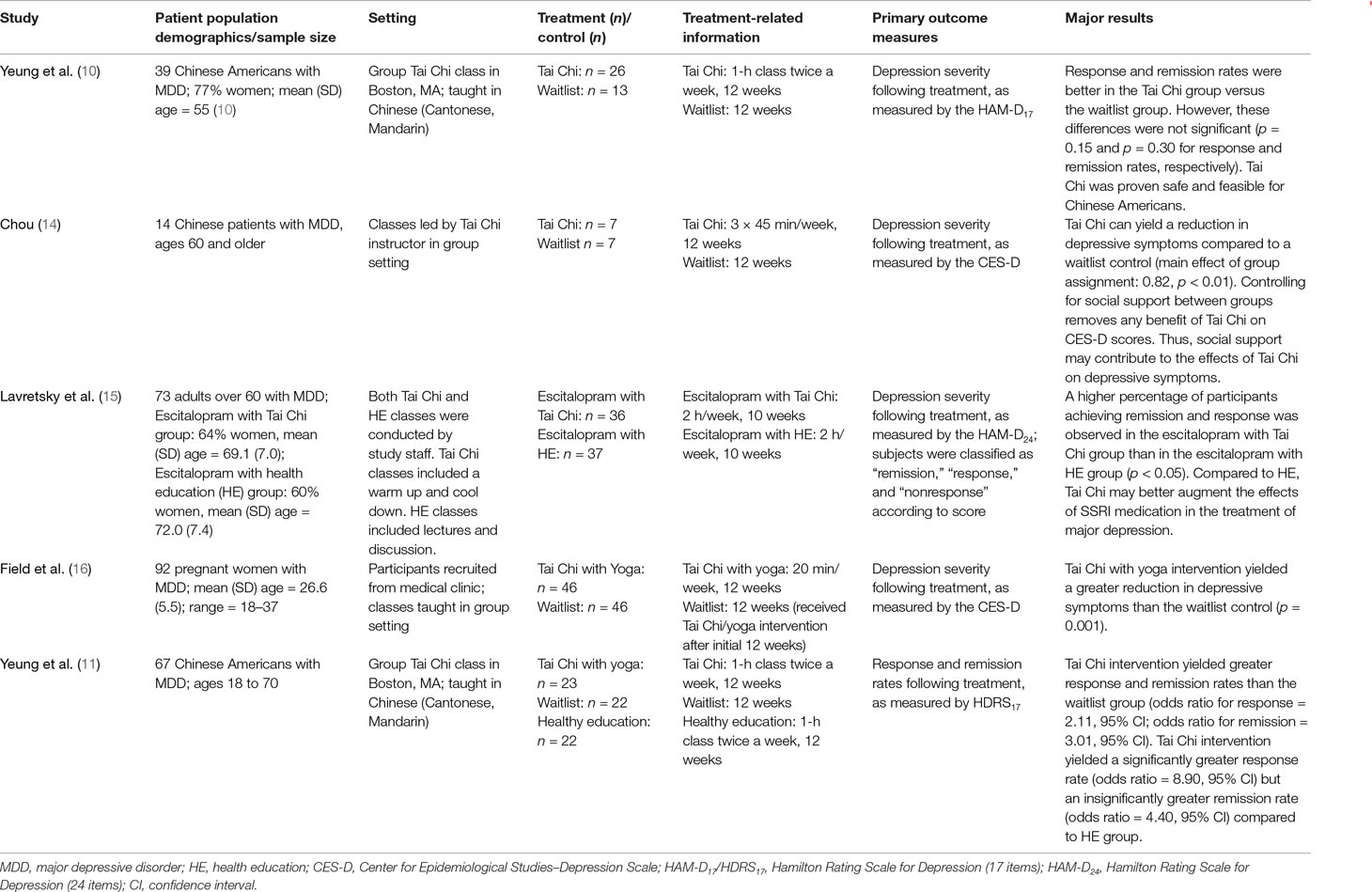
Potential of Tai Chi Treatment of Depression—Results From Clinical Studies
In an earlier study, Chou (14) investigated the effects of Tai Chi on the depressive symptoms of 14 older Chinese patients. Researchers found that 3 months of Tai Chi intervention can significantly reduce scores on the Center for Epidemiological Studies Depression Scale (CES-D) and all of its subscales (including symptoms related to somatic, negative affect, interpersonal relations, and well-being) as compared to a waitlist control. These decreased scores remained significant after controlling for age, gender, and education but not after controlling for social support changes, as measured by the Lubben Social Network Scale (LSNS). This finding suggests that social support may contribute to the effect of Tai Chi on depressive symptoms. This was one of the earliest studies investigating the effect of Tai Chi on depression with positive and notable findings. However, it was limited by a small sample size and the use of a passive control.
In a follow-up study, Lavretsky et al. (15) explored if SSRI (escitalopram) treatment supplemented with 10 weeks of Tai Chi, as compared to health education (HE), would enhance depression treatment in 73 older adults. They found that patients in the Tai Chi-supplemented condition were more likely to 1) experience a greater improvement in depressive symptoms or achieve depression remission and 2) have greater improvements in C-reactive protein levels and the 36-Item Short Form Health Survey physical functioning and cognitive tests compared to the control group. These findings suggest that supplementing pharmacologic treatment with Tai Chi may yield greater clinical improvement for individuals with geriatric depression. This study had a large sample size and obtained positive findings in both patients’ subjective ratings and in inflammatory marker levels. It demonstrates the benefits of adding Tai Chi to an antidepressant regimen but does not examine the specific effect of Tai Chi on depression.
Field et al. (16) investigated the effects of combined Tai Chi/yoga in 92 prenatally depressed pregnant women. They found that women practicing Tai Chi/yoga (20 min per week for 12 weeks) had lower depression, anxiety, and sleep disturbance scores compared to a waitlist control group (Table 1). This study had a large sample size and provided important evidence on the effects of Tai Chi on depressed pregnant women, who generally would avoid pharmacologic treatment. However, combining Tai Chi and yoga is uncommon in the real world, and a waitlist is considered a weak control.
In another study, Yeung and colleagues (10) examined the practicality and outcome of using Tai Chi to treat depressive symptoms in 39 Chinese Americans with MDD. They found that 73% of patients in the Tai Chi group completed the intervention, and no adverse events were reported. This was a proof-of-concept study with a small sample size to investigate the feasibility and safety of Tai Chi for depressed Chinese Americans, a population that tends to avoid conventional mental health services due to their high levels of stigma against having mental illnesses. In a following study with a larger sample size (n = 67) (11), researchers found that following a 12-week intervention, “response rates were 25%, 21%, and 56%, and remission rates were 10%, 21%, and 50% for the waitlisted, education, and Tai Chi intervention groups, respectively.” Participants randomized to the Tai Chi group experienced a greater response to treatment than did individuals randomized to the waitlist and education groups. Further, participants in the Tai Chi group experienced a significantly greater remission rate than the waitlist group and “a trend of improved remission compared to the education group” (Table 1). This study provided preliminary evidence on the effectiveness of Tai Chi on depressed Chinese Americans, using both passive and active control groups. When the Tai Chi group was compared to the passive control group, improvements in both response rate and remission rate showed statistical significance. Yet, when the Tai Chi group was compared to the active control group, improvement in response rate showed statistical significance but not for improvement in remission rate. The relatively small sample in each of the study groups may explain this negative finding. Studies with larger sample sizes will be needed to provide a more definitive conclusion.
Depression is also a common disorder among elderly adults, and many studies have explored depression treatment for this population (17, 18). Brown et al. (19), for instance, compared psychological changes associated with 16 weeks of moderate-intensity walking (MW), low-intensity walking (LW), low-intensity walking plus relaxation response (LWR), and Tai Chi in healthy, sedentary adults. They found that women in the Tai Chi group experienced decreased mood disturbance (tension, depression, anger, confusion, and total mood disturbance) and an improvement in general mood. Women randomized to the MW group also reported increased satisfaction with physical attributes (body cathexis), while men in the same group reported increased positive affect. These results suggest that mind–body interventions such as Tai Chi may have more psychological benefits than exercises without a cognitive component, thus demonstrating Tai Chi’s value in promoting mental health.
Finally, there is accumulating evidence that Tai Chi can relieve depressive symptoms in patients with fibromyalgia (20, 21), arthritis (22–24), multiple sclerosis (MS) (25), heart failure (26–28), mild dementia (29), and cerebrovascular disorder (30).
Mechanisms of Tai Chi Treatment of Depression
Tai Chi Can Modulate the Brain Regions/Networks Associated With Depression
Studies have shown that depression is linked to structural and functional abnormalities in brain regions that are associated with emotion processing, self-representation, reward, and external stimulus (i.e., stress, distress) interactions (31–39). Among these brain regions are the hippocampus, amygdala, anterior cingulate, ventromedial prefrontal cortex, and dorsomedial prefrontal cortex.
Studies also suggest that core components of mind–body interventions such as Tai Chi may include attentional control, emotion regulation, and self-awareness (40). Although no brain-imaging study has directly investigated the modulation effect of Tai Chi in patients with depression, brain-imaging studies in healthy subjects and other patient populations have endorsed the potential pathways of Tai Chi modulation. Furthermore, results from intervention studies support that the target brain regions outlined in this manuscript can indeed be altered by various interventions in patients with depression (Figure 1). For instance, a systematic review by Gudayol-Ferre et al. notes that “antidepressive treatment is capable of normalizing brain activations in depressed patients during affective tasks in areas such as the DLPFC,” and treatments for depression are associated with alterations in the default mode network (DMN) (41).
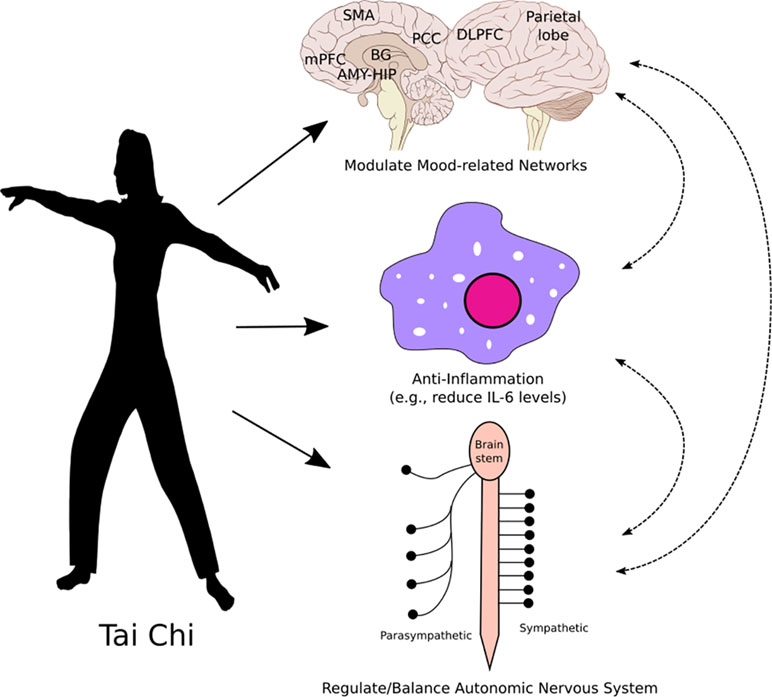
Figure 1 Hypothesized mechanisms of Tai Chi treatment of depression: directly and indirectly modulating the activity and connectivity of key brain regions involved in depression and mood regulation, reducing neuro-inflammatory sensitization, and modulating the autonomic nervous system. Abbreviations: AMY, amygdala; BG, basal ganglia; DLPFC, dorsolateral prefrontal cortex; HIP, hippocampus; mPFC, medial prefrontal cortex; PCC, posterior cingulate cortex; SMA, supplementary motor area.
One potential mechanism of Tai Chi on MDD may occur via the cognitive (attentional) control network (40). During Tai Chi, attention is focused on body posture/movement and breathing regulation and is shifted away from the stressor. Thus, repeated Tai Chi exercise (movement in a mindful way) can modulate the attentional control network and relieve depressive symptoms, and noradrenaline may be heavily involved in attention regulation (42).
In support of this hypothesis, we found that Tai Chi can significantly modulate resting state functional connectivity (rsFC) of the dorsolateral prefrontal cortex (DLPFC), a key region of the cognitive (attentional) control network, with the medial prefrontal cortex and anterior cingulate cortex (MPFC/ACC), key regions of the DMN and limbic system, in healthy elderly adults (43) and patients with fibromyalgia (44). In another study, Wei et al. found that Tai Chi may decrease fractional amplitude of low-frequency fluctuations (fALFF) in the bilateral frontoparietal network (executive/attentional control network). Researchers also identified an association between cognitive control performance and fALFF of the frontoparietal network (45). In a more recent study (46), investigators found that Tai Chi can significantly decrease the functional connectivity between the DLPFC and the thalamus, ventral striatum, and right middle frontal gyrus compared to the control group.
Studies suggest that Tai Chi can also modulate the DMN, a brain network involved in self-referential processing, affective cognition, and emotion regulation (47–54). For instance, results from a previous study revealed significantly decreased fALFF in the Tai Chi condition compared to a control, as well as a significant association between mind–body practice experience and fALFF in the DMN (45). As mentioned above, we also found that Tai Chi can modulate functional connectivity between the cognitive control network and key regions of the DMN (MPFC/ACC), indicating that Tai Chi can modulate the interaction of the two networks. One of the most reliable brain-imaging findings on MDD is the disruption of the DMN (55–61). Thus, Tai Chi may also relieve depressive symptoms by modulating the DMN. In addition, studies have shown that Tai Chi can significantly modulate brain structures in areas related to mood regulation, such as the insula, putamen, and medial temporal pole (62, 63). Taken together, the above findings suggest that the central nervous system may play an important role in the modulation effect of Tai Chi.
Tai Chi may Relieve Symptoms of Depression by Reducing Stress and Modulating the Inflammation System
Stress is produced as the brain and body respond to demands. Literature suggests that stress, particularly long-term stress, may initiate cognitive, affective, and biological processes that increase one’s risk for depression (64, 65) and that inflammation may be involved in this process. Specifically, stress-provoked neuro-inflammatory sensitization can lead to significant behavioral changes and the onset of common depressive symptoms, such as sad mood, anhedonia, fatigue, psychomotor retardation, and social–behavioral withdrawal (64–67). The hypothalamus, anterior insula, and ACC may be involved in this process (64).
Recent studies have suggested that mind–body interventions like Tai Chi may reduce stress and modulate the inflammation process (68, 69) (Figure 1). For instance, Jin (70) found that Tai Chi can raise heart rate, increase noradrenaline excretion in urine, and decrease salivary cortisol concentrations. Compared to baseline levels, subjects reported less tension, depression, anger, fatigue, confusion, and anxiety and felt more vigorous. Irwin and Olmstead (71) evaluated the effects of Tai Chi on circulating markers of inflammation in older adults and found that, among those with elevated Interleukin 6 (IL-6) at entry, Tai Chi yielded a reduction in IL-6 levels comparable to those found in Tai Chi and HE subgroups who had low levels of IL-6 at entry. Meanwhile, IL-6 in HE subgroups remained higher than the Tai Chi and HE subgroups with low IL-6 at entry. Depressive symptom decreases in the two treatment groups were correlated with IL-6 decreases.
Finally, Tai Chi is a mild to moderate exercise, and many studies (72, 73) have suggested that physical exercise itself can modulate the immune and inflammation systems. Such findings endorse the role of Tai Chi in reducing stress and producing anti-inflammatory effects.
Other Potential Mechanisms
Previous studies have suggested that MDD is associated with decreased activity of the parasympathetic nervous system (74–77). Heart rate variability (HRV) is a noninvasive index for monitoring the dynamic equilibrium between sympathetic and parasympathetic nervous system activity. Studies have shown that the high-frequency (HF)–HRV component is inversely correlated with depression severity and a marker of treatment response (75, 78–80).
Lu and Kuo (81) found that Tai Chi can yield increased vagal modulation and shift the sympathovagal balance towards decreased sympathetic modulation in elderly individuals. Audette and colleagues (82) compared the effects of a shortened Tai Chi regimen and a brisk walking training program on metrics such as aerobic capacity, HRV, and strength in elderly sedentary women, and researchers found a significant improvement in estimated VO2 max in the Tai Chi group. In the Tai Chi group only, the mean within-person change of HF power in normalized units was increased, representing increased parasympathetic activity. Meanwhile, low-frequency (LF) power in normalized units (nu) decreased, representing decreased sympathetic activity. In a recent meta-analysis on 17 randomized controlled trials (RCTs), investigators (83) found that combined Tai Chi/yoga produced significantly beneficial effects on HRV parameters (normalized LF, normalized HF, and LF-to-HF ratio) and stress level. These results suggest that the autonomic nervous system may also be involved in the modulation effects of Tai Chi on depressive symptoms (Figure 1).
According to the neurogenic theory (84), depression results from impaired adult hippocampal neurogenesis, the restoration of which leads to recovery. Studies have shown that Tai Chi can significantly modulate the gray matter volume of the hippocampus (63) and rsFC of the hippocampus with the medial prefrontal cortex, a key region of the DMN (85). These findings imply that Tai Chi may alter hippocampal neurogenesis to reduce depressive symptoms (86). The various mechanisms by which Tai Chi may improve depressive symptoms is illustrated in Figure 1.
Challenges and Future Directions
Simplification of Tai Chi Protocol
The complexity of some Tai Chi movements has significantly limited its application as a clinical intervention. Also, not all elements of Tai Chi are relevant to mood regulation and the maintenance of health. Thus, there is a pressing need to develop simplified Tai Chi protocols.
The simplification of Tai Chi has recently begun in China, its country of origin. An example of such simplification is the eight-style Tai Chi that is considered a part of the Chinese martial arts system. Eight-style Tai Chi consists of 10 total postures, including the beginning, the end, and eight main actions from Yang-style Tai Chi.
One attempt to simplify Tai Chi in the Western world is the 12-week Tai Chi protocol developed by Dr. Peter Wayne. The first section introduces several traditional Tai Chi warm-up exercises that can last 15–30 min. The second section focuses on five core Tai Chi movements following the Cheng Ma Ching Yang-style short form. Participants progressively add these movements over the course of the 12 weeks. The program concludes with 5 min of simple cool-down exercises. The total exercise lasts about 45–60 min (87).
Given the ease of the simplified Tai Chi protocols, novice students may practice Tai Chi by following the instructors’ movements in class or at home using videotaped clips. It is worth noting that although these simplified protocols are encouraging, how they differ from traditional Tai Chi remains unknown. Comparative studies are needed to compare the beneficial effects of traditional Tai Chi and simplified Tai Chi.
How Tai Chi Differs From Other Mind–Body Exercises
Mind–body exercise encompasses a family of complex practices such as Tai Chi, yoga, and Baduanjin, each with different characteristics and foci. Although the exact mechanisms of these interventions are still under investigation, studies have found that the underlying mechanisms of different mindfulness movements may not be identical (88, 89).
In previous studies, we compared the modulation effect of Tai Chi and Baduanjin, another mind–body exercise. Baduanjin consists of only eight postures; thus, it is much simpler than other mind–body exercises and can be easily practiced by older adults, specifically those with cognitive decline, when guided by video or audio at home. As a result, we found that Baduanjin can produce greater and more extensive improvements in Wechsler Memory Scale (WMS) subscores and gray matter brain volume changes than Tai Chi in healthy older adults (63).
In another study (90), we compared the modulation effect of Tai Chi with Baduanjin on the DMN. We found that compared to the control group, Tai Chi increased posterior cingulate cortex rsFC with the right putamen/caudate, while Baduanjin decreased rsFC between the mPFC and orbital prefrontal gyrus/putamen. Direct comparison between the two mind–body interventions revealed that Tai Chi was significantly associated with increased rsFC between the mPFC and right putamen/caudate compared to Baduanjin, suggesting that these interventions may be associated with different mechanisms and treatment effects.
Developing a Tailored Tai Chi Protocol for Different Disorders
One important direction of Tai Chi research may be to create a tailored Tai Chi regimen for different disorders and individuals. Specifying a Tai Chi protocol for a particular population may significantly enhance the benefits of Tai Chi and reduce potential adverse effects.
In one such attempt, Tai Chi practitioner and researcher Dr. Albert Yeung developed a Tai Chi protocol specifically for individuals with mood disorders: Tai Chi for Mood (Tai ChiM). The Tai ChiM protocol consists of 12 separate Tai Chi moves along with mental focus and deep, paced breathing. Tai ChiM excludes the complex transitions between Tai Chi movements, making it easier to learn and potentially a stronger intervention. A unique characteristic of Tai ChiM is that it focuses more on meditative movements, relaxation, and paced breathing and less on physical strength training. Such characteristics make it an optimal choice for those with MDD and other mood disorders.
While furthering the development of Tai Chi may be enhanced with tailored protocols, this area of research also demands more fully powered RCTs. The studies summarized in this manuscript support the efficacy of Tai Chi in improving depressive symptoms, but future studies should strive to increase their sample sizes. Conducting studies with larger and more diverse samples will allow us to test the effects of Tai Chi on different subgroups of the MDD patient population. In addition, most of the current studies have been performed on an Asian population, and future studies targeting other populations are needed. Finally, future research should examine the differences between traditional Tai Chi and simplified, low-intensity Tai Chi to identify the most crucial components of this promising mind–body intervention. For instance, it is worth investigating which elements of traditional Tai Chi can be excluded without sacrificing the efficacy of the practice. We believe that the results obtained will facilitate the acceptance of Tai Chi and lower the cost of the practice, thereby making it a more economical and accessible alternative to pharmacologic and other treatments for depression.
We believe that Tai ChiM could be a potential solution to the shortage of mental health providers and well-trained Tai Chi instructors worldwide. Further, it could reduce disparities in mental health treatment among ethnic minority populations who tend to avoid conventional psychiatric treatment due to stigmas surrounding mental illness. To enhance its availability, a video demonstrating Tai Chi for mood is publicly available on YouTube with Chinese, English, and Spanish subtitles (https://youtu.be/08IFKiXb3bA).
In summary, although Tai Chi has demonstrated its potential in mood regulation and relieving depressive symptoms, its underlying mechanism of action remains to be discovered. The instructional videos and the development of less structured Tai Chi has made it a promising low-intensity mind-body therapy. A fully powered RCT would largely benefit the development of Tai Chi, as would an exploration of ways to lower the cost of the intervention. Most importantly, a simplified and tailored Tai Chi—or a new intervention that combines Tai Chi and other mind–body exercises to enhance modulation effects on a specific patient population or individual—may represent a direction for further development of modern Tai Chi.
Author Contributions
JK and AY conceived of the ideas presented in this manuscript. All authors contributed to manuscript preparation.
Funding
JK is supported by R01 AT008563, R33AT009310, and R21AT008707 from NIH/NCCIH.
Conflict of Interest Statement
JK holds equity in a startup company (MNT) and a pending patent to develop a new neuromodulation device.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Hasin DS, Sarvet AL, Meyers JL, Saha TD, Ruan WJ, Stohl M, et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry (2018) 75(4):336–46. doi: 10.1001/jamapsychiatry.2017.4602
2. Leichsenring F, Steinert C, Hoyer J. Psychotherapy versus pharmacotherapy of depression: what’s the evidence? Z Psychosom Med Psychother (2016) 62(2):190–5. doi: 10.13109/zptm.2016.62.2.190
3. Jakobsen JC, Katakam KK, Schou A, Hellmuth SG, Stallknecht SE, Leth-Moller K, et al. Selective serotonin reuptake inhibitors versus placebo in patients with major depressive disorder. BMC Psychiatry (2017) 17(1):58. doi: 10.1186/s12888-016-1173-2
4. Jakobsen JC, Hansen JL, Storebo OJ, Simonsen E, Gluud C. The effects of cognitive therapy versus ‘no intervention’ for major depressive disorder. PLoS One (2011) 6(12):e28299. doi: 10.1371/journal.pone.0028299
5. Jakobsen JC, Lindschou Hansen J, Storebo OJ, Simonsen E, Gluud C. The effects of cognitive therapy versus ‘treatment as usual’ in patients with major depressive disorder. PLoS One (2011) 6(8):e22890. doi: 10.1371/journal.pone.0022890
6. Ferguson JM. SSRI Antidepressant medications: adverse effects and tolerability. Prim Care Companion J Clin Psychiatry (2001) 3(1):22–7. doi: 10.4088/PCC.v03n0105
7. Shelton RC, Osuntokun O, Heinloth AN, Corya SA. Therapeutic options for treatment-resistant depression. CNS Drugs (2010) 24(2):131–61. doi: 10.2165/11530280-000000000-00000
8. Zou L, Yeung A, Li C, Wei GX, Chen KW, Kinser PA, et al. Effects of meditative movements on major depressive disorder: a systematic review and meta-analysis of randomized controlled trials. J Clin Med (2018) 7(8):195. doi: 10.3390/jcm7080195
9. Laird KT, Paholpak P, Roman M, Rahi B, Lavretsky H. Mind–body therapies for late-life mental and cognitive health. Curr Psychiatry Rep (2018) 20(1):2. doi: 10.1007/s11920-018-0864-4
10. Yeung A, Lepoutre V, Wayne P, Yeh G, Slipp LE, Fava M, et al. Tai Chi treatment for depression in Chinese Americans: a pilot study. Am J Phys Med Rehabil (2012) 91(10):863–70. doi: 10.1097/PHM.0b013e31825f1a67
11. Yeung AS, Feng R, Kim DJH, Wayne PM, Yeh GY, Baer L, et al. A pilot, randomized controlled study of Tai Chi with passive and active controls in the treatment of depressed Chinese Americans. J Clin Psychiatry (2017) 78(5):e522–e528. doi: 10.4088/JCP.16m10772
12. Wang F, Lee EK, Wu T, Benson H, Fricchione G, Wang W, et al. The effects of tai chi on depression, anxiety, and psychological well-being: a systematic review and meta-analysis. Int J Behav Med (2014) 21(4):605–17. doi: 10.1007/s12529-013-9351-9
13. Payne P, Crane-Godreau MA. Meditative movement for depression and anxiety. Front Psychiatry (2013) 4:71. doi: 10.3389/fpsyt.2013.00071
14. Chou KL. Effect of Tai Chi on depressive symptoms amongst Chinese older patients with major depression: the role of social support. Med Sport Sci (2008) 52:146–54. doi: 10.1159/000134295
15. Lavretsky H, Alstein LL, Olmstead RE, Ercoli LM, Riparetti-Brown M, Cyr NS, et al. Complementary use of tai chi chih augments escitalopram treatment of geriatric depression: a randomized controlled trial. Am J Geriatr Psychiatry (2011) 19(10):839–50. doi: 10.1097/JGP.0b013e31820ee9ef
16. Field T, Diego M, Delgado J, Medina L. Tai chi/yoga reduces prenatal depression, anxiety and sleep disturbances. Complement Ther Clin Pract (2013) 19(1):6–10. doi: 10.1016/j.ctcp.2012.10.001
17. Yildirim P, Ofluoglu D, Aydogan S, Akyuz G. Tai Chi vs. J Back Musculoskelet Rehabil (2016) 29(3):493–501. doi: 10.3233/BMR-150645
18. Zhang X, Ni X, Chen P. Study about the effects of different fitness sports on cognitive function and emotion of the aged. Cell Biochem Biophys (2014) 70(3):1591–6. doi: 10.1007/s12013-014-0100-8
19. Brown DR, Wang Y, Ward A, Ebbeling CB, Fortlage L, Puleo E, et al. Chronic psychological effects of exercise and exercise plus cognitive strategies. Med Sci Sports Exerc (1995) 27(5):765–75. doi: 10.1249/00005768-199505000-00021
20. Wang C, Schmid CH, Fielding RA, Harvey WF, Reid KF, Price LL, et al. Effect of tai chi versus aerobic exercise for fibromyalgia: comparative effectiveness randomized controlled trial. BMJ (2018) 360:k851. doi: 10.1136/bmj.k851
21. Wang C, Schmid CH, Rones R, Kalish R, Yinh J, Goldenberg DL, et al. A randomized trial of tai chi for fibromyalgia. N Engl J Med (2010) 363(8):743–54. doi: 10.1056/NEJMoa0912611
22. Wang C. Tai Chi improves pain and functional status in adults with rheumatoid arthritis: results of a pilot single-blinded randomized controlled trial. Med Sport Sci (2008) 52:218–29. doi: 10.1159/000134302
23. Wang C, Schmid CH, Hibberd PL, Kalish R, Roubenoff R, Rones R, et al. Tai Chi is effective in treating knee osteoarthritis: a randomized controlled trial. Arthritis Rheum (2009) 61(11):1545–53. doi: 10.1002/art.24832
24. Driban JB, Morgan N, Price LL, Cook KF, Wang C. Patient-Reported Outcomes Measurement Information System (PROMIS) instruments among individuals with symptomatic knee osteoarthritis: a cross-sectional study of floor/ceiling effects and construct validity. BMC Musculoskelet Disord (2015) 16:253. doi: 10.1186/s12891-015-0715-y
25. Burschka JM, Keune PM, Oy UH, Oschmann P, Kuhn P. Mindfulness-based interventions in multiple sclerosis: beneficial effects of Tai Chi on balance, coordination, fatigue and depression. BMC Neurol (2014) 14:165. doi: 10.1186/s12883-014-0165-4
26. Yeh GY, Wood MJ, Wayne PM, Quilty MT, Stevenson LW, Davis RB, et al. Tai chi in patients with heart failure with preserved ejection fraction. Congest Heart Fail (2013) 19(2):77–84. doi: 10.1111/chf.12005
27. Redwine LS, Tsuang M, Rusiewicz A, Pandzic I, Cammarata S, Rutledge T, et al. A pilot study exploring the effects of a 12-week t’ai chi intervention on somatic symptoms of depression in patients with heart failure. J Altern Complement Med (2012) 18(8):744–8. doi: 10.1089/acm.2011.0314
28. Barrow DE, Bedford A, Ives G, O’Toole L, Channer KS. An evaluation of the effects of Tai Chi Chuan and Chi Kung training in patients with symptomatic heart failure: a randomised controlled pilot study. Postgrad Med J (2007) 83(985):717–21. doi: 10.1136/pgmj.2007.061267
29. Cheng ST, Chow PK, Yu EC, Chan AC. Leisure activities alleviate depressive symptoms in nursing home residents with very mild or mild dementia. Am J Geriatr Psychiatry (2012) 20(10):904–8. doi: 10.1097/JGP.0b013e3182423988
30. Wang W, Sawada M, Noriyama Y, Arita K, Ota T, Sadamatsu M, et al. Tai Chi exercise versus rehabilitation for the elderly with cerebral vascular disorder: a single-blinded randomized controlled trial. Psychogeriatrics (2010) 10(3):160–6. doi: 10.1111/j.1479-8301.2010.00334.x
31. Davidson RJ, Pizzagalli D, Nitschke JB, Putnam K. Depression: perspectives from affective neuroscience. Annu Rev Psychol (2002) 53:545–74. doi: 10.1146/annurev.psych.53.100901.135148
32. Greicius M. Resting-state functional connectivity in neuropsychiatric disorders. Curr Opin Neurol (2008) 21(4):424–30. doi: 10.1097/WCO.0b013e328306f2c5
33. Northoff G, Wiebking C, Feinberg T, Panksepp J. The ‘resting-state hypothesis’ of major depressive disorder—a translational subcortical–cortical framework for a system disorder. Neurosci Biobehav Rev (2011) 35(9):1929–45. doi: 10.1016/j.neubiorev.2010.12.007
34. Pizzagalli DA. Frontocingulate dysfunction in depression: toward biomarkers of treatment response. Neuropsychopharmacology (2011) 36(1):183–206. doi: 10.1038/npp.2010.166
35. Mwangi B, Ebmeier KP, Matthews K, Steele JD. Multi-centre diagnostic classification of individual structural neuroimaging scans from patients with major depressive disorder. Brain (2012) 135(Pt 5):1508–21. doi: 10.1093/brain/aws084
36. Silbersweig D. Default mode subnetworks, connectivity, depression and its treatment: toward brain-based biomarker development. Biol Psychiatry (2013) 74(1):5–6. doi: 10.1016/j.biopsych.2013.05.011
37. Hasler G, Northoff G. Discovering imaging endophenotypes for major depression. Mol Psychiatry (2011) 16(6):604–19. doi: 10.1038/mp.2011.23
38. Wang Z, Liu J, Zhong N, Qin Y, Zhou H, Li K. Changes in the brain intrinsic organization in both on-task state and post-task resting state. Neuroimage (2012) 62(1):394–407. doi: 10.1016/j.neuroimage.2012.04.051
39. Hwang J, Egorova N, Yang XQ, Zhang WY, Chen J, Yang XY, et al. Subthreshold depression is associated with impaired resting state functional connectivity of the cognitive control network. Transl Psychiatry (2015) 5(11):e683. doi: 10.1038/tp.2015.174
40. Tang YY, Holzel BK, Posner MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci (2015) 16(4):213–25. doi: 10.1038/nrn3916
41. Gudayol-Ferre E, Pero-Cebollero M, Gonzalez-Garrido AA, Guardia-Olmos J. Changes in brain connectivity related to the treatment of depression measured through fMRI: a systematic review. Front Hum Neurosci (2015) 9:582. doi: 10.3389/fnhum.2015.00582
42. Russell TA, Arcuri SM. A neurophysiological and neuropsychological consideration of mindful movement: clinical and research implications. Front Hum Neurosci (2015) 9:282. doi: 10.3389/fnhum.2015.00282
43. Tao J, Chen XL, Egorova N, Liu J, Xue XH, Huang J, et al. Tai Chi Chuan and Baduanjin practice modulates functional connectivity of the cognitive control network in older adults. Sci Rep (2017) 7(41581):1–9. doi: 10.1038/srep41581
44. Kong J, Wolcott E, Wang Z, Jorgenson K, Harvey WF, Tao J, et al. Altered resting state functional connectivity of the cognitive control network in fibromyalgia and the modulation effect of mind-body intervention. Brain Imaging Behav (2018). doi: 10.1007/s11682-018-9875-3
45. Wei GX, Gong ZQ, Yang Z, Zuo XN. Mind–body practice changes fractional amplitude of low frequency fluctuations in intrinsic control networks. Front Psychol (2017) 8:1049. doi: 10.3389/fpsyg.2017.01049
46. Liu Z, Wu Y, Li L, Guo X. Functional connectivity within the executive control network mediates the effects of long-term Tai Chi exercise on elders’ emotion regulation. Front Aging Neurosci (2018) 10:315. doi: 10.3389/fnagi.2018.00315
47. Buckner RL, Andrews-Hanna JR, Schacter DL. The brain’s default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci (2008) 1124:1–38. doi: 10.1196/annals.1440.011
48. Andrews-Hanna JR, Reidler JS, Sepulcre J, Poulin R, Buckner RL. Functional-anatomic fractionation of the brain’s default network. Neuron (2010) 65(4):550–62. doi: 10.1016/j.neuron.2010.02.005
49. Connolly CG, Wu J, Ho TC, Hoeft F, Wolkowitz O, Eisendrath S, et al. Resting-state functional connectivity of subgenual anterior cingulate cortex in depressed adolescents. Biol Psychiatry (2013) 74(12):898–907. doi: 10.1016/j.biopsych.2013.05.036
50. Berman MG, Peltier S, Nee DE, Kross E, Deldin PJ, Jonides J. Depression, rumination and the default network. Soc Cogn Affect Neurosci (2011) 6(5):548–55. doi: 10.1093/scan/nsq080
51. Buckner RL, Sepulcre J, Talukdar T, Krienen FM, Liu H, Hedden T, et al. Cortical hubs revealed by intrinsic functional connectivity: mapping, assessment of stability, and relation to Alzheimer’s disease. J Neurosci (2009) 29(6):1860–73. doi: 10.1523/JNEUROSCI.5062-08.2009
52. Etkin A, Egner T, Kalisch R. Emotional processing in anterior cingulate and medial prefrontal cortex. Trends Cogn Sci (2011) 15(2):85–93. doi: 10.1016/j.tics.2010.11.004
53. Nejad AB, Fossati P, Lemogne C. Self-referential processing, rumination, and cortical midline structures in major depression. Front Hum Neurosci (2013) 7:666. doi: 10.3389/fnhum.2013.00666
54. Fang J, Rong P, Hong Y, Fan Y, Liu J, Wang H, et al. Transcutaneous vagus nerve stimulation modulates default mode network in major depressive disorder. Biol Psychiatry (2016) 79(4):266–73. doi: 10.1016/j.biopsych.2015.03.025
55. Greicius MD, Flores BH, Menon V, Glover GH, Solvason HB, Kenna H, et al. Resting-state functional connectivity in major depression: abnormally increased contributions from subgenual cingulate cortex and thalamus. Biol Psychiatry (2007) 62(5):429–37. doi: 10.1016/j.biopsych.2006.09.020
56. Bluhm R, Williamson P, Lanius R, Theberge J, Densmore M, Bartha R, et al. Resting state default-mode network connectivity in early depression using a seed region-of-interest analysis: decreased connectivity with caudate nucleus. Psychiatry Clin Neurosci (2009) 63(6):754–61. doi: 10.1111/j.1440-1819.2009.02030.x
57. Wang L, Hermens DF, Hickies IB, Lagopoulos J. A systematic review of resting-state functional-MRI studies in major depression. J Affect Disord (2012) 142(1-3):6–12. doi: 10.1016/j.jad.2012.04.013
58. Posner J, Hellerstein DJ, Gat I, Mechling A, Klahr K, Wang Z, et al. Antidepressants normalize the default mode network in patients with dysthymia. JAMA Psychiatry (2013) 70(4):373–82. doi: 10.1001/jamapsychiatry.2013.455
59. Liston C, Chen AC, Zebley BD, Drysdale AT, Gordon R, Leuchter B, et al. Default mode network mechanisms of transcranial magnetic stimulation in depression. Biol Psychiatry (2014) 76(7):517–26. doi: 10.1016/j.biopsych.2014.01.023
60. Zhu X, Wang X, Xiao J, Liao J, Zhong M, Wang W, et al. Evidence of a dissociation pattern in resting-state default mode network connectivity in first-episode, treatment-naive major depression patients. Biol Psychiatry (2012) 71(7):611–7. doi: 10.1016/j.biopsych.2011.10.035
61. Wu D, Yuan Y, Bai F, You J, Li L, Zhang Z. Abnormal functional connectivity of the default mode network in remitted late-onset depression. J Affect Disord (2013) 147(1–3):277–87. doi: 10.1016/j.jad.2012.11.019
62. Wei GX, Xu T, Fan FM, Dong HM, Jiang LL, Li H, et al. Can Taichi reshape the brain? A brain morphometry study. PLoS One (2013) 8(4):e61038. doi: 10.1371/journal.pone.0061038
63. Tao J, Liu J, Liu W, Huang J, Xue X, Chen X, et al. Tai Chi Chuan and Baduanjin increase grey matter volume in older adults: a brain imaging study. J Alzheimers Dis (2017) 60(2):389–400. doi: 10.3233/JAD-170477
64. Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull (2014) 140(3):774–815. doi: 10.1037/a0035302
65. Gold PW. The organization of the stress system and its dysregulation in depressive illness. Mol Psychiatry (2015) 20(1):32–47. doi: 10.1038/mp.2014.163
66. Rieder R, Wisniewski PJ, Alderman BL, Campbell SC. Microbes and mental health: a review. Brain Behav Immun (2017) 66:9–17. doi: 10.1016/j.bbi.2017.01.016
67. Crupi R, Cuzzocrea S. Neuroinflammation and immunity: a new pharmacological target in depression. CNS Neurol Disord Drug Targets (2016) 15(4):464–76. doi: 10.2174/1871527315666160321105339
68. Bower JE, Irwin MR. Mind-body therapies and control of inflammatory biology: a descriptive review. Brain Behav Immun (2016) 51:1–11. doi: 10.1016/j.bbi.2015.06.012
69. Morgan N, Irwin MR, Chung M, Wang C. The effects of mind-body therapies on the immune system: meta-analysis. PLoS One (2014) 9(7):e100903. doi: 10.1371/journal.pone.0100903
70. Jin P. Changes in heart rate, noradrenaline, cortisol and mood during Tai Chi. J Psychosom Res (1989) 33(2):197–206. doi: 10.1016/0022-3999(89)90047-0
71. Irwin MR, Olmstead R. Mitigating cellular inflammation in older adults: a randomized controlled trial of Tai Chi Chih. Am J Geriatr Psychiatry (2012) 20(9):764–72. doi: 10.1097/JGP.0b013e3182330fd3
72. Leal LG, Lopes MA, Batista ML Jr. Physical exercise-induced myokines and muscle-adipose tissue crosstalk: a review of current knowledge and the implications for health and metabolic diseases. Front Physiol (2018) 9:1307. doi: 10.3389/fphys.2018.01307
73. Simpson RJ, Kunz H, Agha N, Graff R. Exercise and the regulation of immune functions. Prog Mol Biol Transl Sci (2015) 135:355–80. doi: 10.1016/bs.pmbts.2015.08.001
74. Jandackova VK, Britton A, Malik M, Steptoe A. Heart rate variability and depressive symptoms: a cross-lagged analysis over a 10-year period in the Whitehall II study. Psychol Med (2016) 46(10):2121–31. doi: 10.1017/S003329171600060X
75. Vazquez L, Blood JD, Wu J, Chaplin TM, Hommer RE, Rutherford HJ, et al. High frequency heart-rate variability predicts adolescent depressive symptoms, particularly anhedonia, across one year. J Affect Disord (2016) 196:243–7. doi: 10.1016/j.jad.2016.02.040
76. Udupa K, Sathyaprabha TN, Thirthalli J, Kishore KR, Lavekar GS, Raju TR, et al. Alteration of cardiac autonomic functions in patients with major depression: a study using heart rate variability measures. J Affect Disord (2007) 100(1–3):137–41. doi: 10.1016/j.jad.2006.10.007
77. Carney RM, Blumenthal JA, Freedland KE, Stein PK, Howells WB, Berkman LF, et al. Low heart rate variability and the effect of depression on post-myocardial infarction mortality. Arch Intern Med (2005) 165(13):1486–91. doi: 10.1001/archinte.165.13.1486
78. Koenig J, Kemp AH, Beauchaine TP, Thayer JF, Kaess M. Depression and resting state heart rate variability in children and adolescents—a systematic review and meta-analysis. Clin Psychol Rev (2016) 46:136–50. doi: 10.1016/j.cpr.2016.04.013
79. Sgoifo A, Carnevali L, Alfonso Mde L, Amore M. Autonomic dysfunction and heart rate variability in depression. Stress (2015) 18(3):343–52. doi: 10.3109/10253890.2015.1045868
80. Wang Y, Zhao X, O’Neil A, Turner A, Liu X, Berk M. Altered cardiac autonomic nervous function in depression. BMC Psychiatry (2013) 13:187. doi: 10.1186/1471-244X-13-187
81. Lu WA, Kuo CD. The effect of Tai Chi Chuan on the autonomic nervous modulation in older persons. Med Sci Sports Exerc (2003) 35(12):1972–6. doi: 10.1249/01.MSS.0000099242.10669.F7
82. Audette JF, Jin YS, Newcomer R, Stein L, Duncan G, Frontera WR. Tai Chi versus brisk walking in elderly women. Age Ageing (2006) 35(4):388–93. doi: 10.1093/ageing/afl006
83. Zou L, Sasaki JE, Wei GX, Huang T, Yeung AS, Neto OB, et al. Effects of mind–body exercises (Tai Chi/yoga) on heart rate variability parameters and perceived stress: a systematic review with meta-analysis of randomized controlled trials. J Clin Med (2018) 7(11):E404. doi: 10.3390/jcm7110404
84. Miller BR, Hen R. The current state of the neurogenic theory of depression and anxiety. Curr Opin Neurobiol (2015) 30:51–8. doi: 10.1016/j.conb.2014.08.012
85. Tao J, Liu J, Egorova N, Chen X, Sun S, Xue X, et al. Increased hippocampus-medial prefrontal cortex resting-state functional connectivity and memory function after Tai Chi Chuan practice in elder adults. Front Aging Neurosci (2016) 8:25. doi: 10.3389/fnagi.2016.00025
86. Yuan TF, Li A, Sun X, Arias-Carrion O, Machado S. Vagus nerve stimulation in treating depression: a tale of two stories. Curr Mol Med (2016) 16(1):33–9. doi: 10.2174/1566524016666151222143609
87. Wayne P, Fuerst M. The Harvard medical school guide to Tai Chi. Boulder, Colorado: Shambhala Publications (2013).
88. Tao J, Liu J, Tu Y, Hu K, Tu Y, Lin M, et al. Different types of exercise relieve pain symptoms of knee osteoarthritis by modulating the cognitive control network. Ann Phys Rehabil Med (2018) 61(Supplement):e127. doi: 10.1016/j.rehab.2018.05.280
89. Tao J, Chen X, Liu J, Egorova N, Xue X, Liu W, et al. Tai Chi Chuan and Baduanjin mind–body training changes resting-state low-frequency fluctuations in the frontal lobe of older adults: a resting-state fMRI study. Front Hum Neurosci (2017) 11:514. doi: 10.3389/fnhum.2017.00514
Keywords: Tai Chi, mind–body intervention, major depressive disorder, depression, brain network, anti-inflammation
Citation: Kong J, Wilson G, Park J, Pereira K, Walpole C and Yeung A (2019) Treating Depression With Tai Chi: State of the Art and Future Perspectives. Front. Psychiatry 10:237. doi: 10.3389/fpsyt.2019.00237
Received: 14 December 2018; Accepted: 28 March 2019;
Published: 12 April 2019.
Edited by:
Saeed Farooq, Keele University, United KingdomReviewed by:
Farooq Naeem, University of Toronto, CanadaJung Eun Shin, Yonsei University, South Korea
Copyright © 2019 Kong, Wilson, Park, Pereira, Walpole and Yeung. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Georgia Wilson, gjwilson@mgh.harvard.edu
 Jian Kong
Jian Kong Georgia Wilson
Georgia Wilson Joel Park
Joel Park Kaycie Pereira
Kaycie Pereira Courtney Walpole
Courtney Walpole Albert Yeung
Albert Yeung