- 1Division of Mental Health and Addiction, Oslo University Hospital, Oslo, Norway
- 2Norwegian Centre for Mental Disorders Research, Faculty of Medicine, University of Oslo, Oslo, Norway
Background: Use of antipsychotic medication is central in the treatment of psychotic disorders. However, there is limited knowledge about prescription practice of antipsychotics in the critical early phase of these disorders. Clinical guidelines recommend low dosages, but no discontinuation of antipsychotic medication during the first year of treatment in first episode patients. The main aim of this study was to identify clinical predictors for dosage change or discontinuation of antipsychotics during this period.
Methods: A total of 426 antipsychotic-using patients with schizophrenia spectrum or bipolar disorder, including both a first treatment sample and a sample of patients with previous treated episodes (“multi-episode” sample) from the same diagnostic groups, underwent thorough clinical and sociodemographic assessment at study baseline and after 1 year. Prescribed dosage levels at baseline and follow-up and change in dosage or discontinuation of antipsychotics from baseline to follow-up were compared between groups, controlling for possible confounders.
Results: We found reduced dosages over the first year in both first treatment groups across diagnoses, but not in multi-episode groups. Weight increase predicted dosage reduction in the schizophrenia group, while the level of psychotic symptoms at baseline predicted dosage reduction in the bipolar group. We found higher baseline levels of antipsychotic use in the schizophrenia group than in the bipolar group.
Conclusion: We found indications of a trans-diagnostic reduction of prescribed dosages of antipsychotics over the first year in treatment, but with different predictors for this reduction in the two diagnostic groups. The findings increase the understanding of drivers of early medication change in psychotic disorder.
Background
Psychopharmacological agents are one of the main treatment approaches in clinical psychiatry. Antipsychotics (“neuroleptics”) were introduced for the treatment of schizophrenia in 1956, and have persisted as the cornerstone of treatment for schizophrenia and related psychotic disorders (1, 2). They also effectively reduce the psychotic symptoms of affective psychoses in manic or depressive episodes (3), and some are approved as mood stabilizers in bipolar disorder (4, 5). There is however growing controversy around the use of antipsychotics (6, 7), including criticism of inadequate side effect management (8–11).
Prospective studies show beneficial effects of earlier adequate treatment in psychotic disorders, and treatments given in the early phases of illness seem to be of particular importance for short- and long-term outcome (12–14). Studies also indicate that first-treatment patients are more sensitive to lower dosages of antipsychotics than multi-episode patients, both in their responses to and in their experiences of adverse effects (15). Use of unnecessarily high dosages may lead to adverse effects and negative opinions about antipsychotics, with long-term consequences for treatment compliance. New treatment guidelines recommend the use of monotherapy and low dosages for the first psychotic episode and subsequent maintenance therapy for schizophrenia spectrum disorders (2, 11, 16). Discontinuing antipsychotic treatment in the first year of treatment is not recommended. In clinical practice, the choice of which antipsychotic to use and the dosage to administer is highly individualized (17–19). Factors which may affect the choice of individual treatment include diagnosis, current symptomatology, insight into the illness, known side effects of the drug in question, degree of functional loss, as well as perceived adherence to medical advice (20, 21). There are no specific recommendations for antipsychotic treatment of patients with bipolar disorder.
The efficacy of current antipsychotics is dependent on their effects on the dopamine neurotransmitter system in the central nervous system. Since drug uptake, first-pass metabolism and passage over the blood–brain barrier are highly individual there is no fixed dose–response (22, 23), and antipsychotic treatments typically have an aspect of trial and error (24). This carries risks, both for the use of ineffective dosages over too long periods of time, and for the use of too high dosages causing unnecessary side effects. An increase in knowledge to guide the choice of first treatment in psychotic disorder is thus warranted. Identifying predictors of discontinuation or change in dosages of antipsychotics during the first year of treatment can help to better understand the mechanisms behind the individual decision-making processes. Such insight may be important in guiding the complex task of finding the optimal treatment.
The current study is based on a 1-year follow-up of comprehensively characterized patients with schizophrenia and bipolar disorder, including both first-treatment and multi-episode patients from the same catchment areas, and thus using the same treatment services. These services give treatment based on guidelines that recommend low dosages of antipsychotics for first-treatment schizophrenia for 2 years, but with no particular advice for the dosages and length of maintenance treatment in first-treatment bipolar disorder. The study had the following aims:
1. Are there differences in the use of antipsychotics, between first-treatment and multi- episode patients in patients with schizophrenia spectrum and bipolar disorder at study baseline?
2. What dosage changes or discontinuation rates of antipsychotic medication are there over the subsequent year? Do these predictors differ between patients with schizophrenia spectrum and bipolar disorder, or between first-treatment and multi- episode patients?
3. What are the predictors of changes in the dosages or discontinuation of antipsychotics, and are there different predictors between patients with schizophrenia spectrum and bipolar disorder, and between first-treatment and multi-episode patients?
Materials and Methods
The current study is a component of the TOP (Thematically Organized Psychosis research) Study, which is approved by the Regional Committee for Medical Research Ethics and the Norwegian Data Inspectorate. Recruitment was done from 2003 until 2017 from major hospitals in the Oslo area, Norway. The TOP study comprises several smaller sub-studies. All first treatment patients are included in prospective cohorts with planned follow-up studies. Multi-episode patients were part of smaller follow-up studies, based on the focus of ongoing projects. The reasons for multi-episode patients to participate, or not to participate, in follow-up studies were thus administrative (based in project design and funding) with no identified selection bias involved. There were no significant differences in baseline demographic and clinical characteristics between multi-episode patients participating or not participating in follow-ups. For a more detailed description, see Faerden et al. (25), Hellvin et al. (26), and Kvitland et al. (27).
Inclusion criteria at baseline: age 17 to 67 years and meeting the DSM-IV criteria for a diagnosis of schizophrenia, schizophreniform disorder, schizoaffective disorder, psychotic disorder NOS, delusional disorder or bipolar I, II or NOS disorder. Exclusion criteria were: presence of a diagnosis of a developmental disorder, IQ < 70 or acquired brain damage (head injury with hospitalization), and lack of fluency in a Scandinavian language. There were no exclusion criteria based on course of illness, history of treatment or substance use. Patients were recruited consecutively from in- and outpatient psychiatric units in the collaborating hospitals. There were no other treatment organizations serving these areas, allowing for a high degree of representation for participating patients. For details, see Ringen et al. (28). Each patient was referred to the project by their treating clinician, after an initial evaluation of their eligibility and ability to give informed consent. Emphasis was put on recruiting all patients regardless of the level of adherence to their respective treatment programs. All patients gave written informed consent to participation and for follow-up. The assessments were conducted by trained clinicians working as research fellows (MDs or clinical psychologists). The recruitment teams were primarily based in the outpatient clinics, where patients are transferred for treatment after the acute illness phases. The study thus mainly includes patients who were symptomatically stable at the point of baseline assessments.
Assessments of Diagnosis, Onset of Illness, Treatment History and Sociodemographics at First Assessment; Creating of Groups
Diagnosis, onset of illness and treatment history at baseline were established using the Structural Clinical Instrument of Diagnosis for DSM-IV axis I disorders (SCID – I), modules A–E, with the aid of medical charts (29). All interviewers completed a training course in SCID assessment based on the training program at the University of California Los Angeles (30) and participated in regular diagnostic consensus meetings led by a clinically well-experienced professor of psychiatry. To evaluate reliability of actual study interviews, a stratified random sample was drawn, consisting of cases from every assessment staff member. Anonymous vignettes describing symptoms and development of the illness were then rated by two experts blind to the study ratings. For the 28 vignettes evaluated, the overall agreement for the nine DSM-IV diagnostic categories was 82% and the overall Kappa 0.77 (95% CI: 0.60–0.94).
The duration of untreated illness (DUI) was defined as the time (in weeks) from the onset of the first SCID verified illness episode to the start of use of adequate medication. For Bipolar disorder specifically, DUI was defined as time from first affective episode (regardless of polarity), to the start of adequate treatment, defined as either antipsychotic or mood-stabilizing medication for mania or mixed episodes (in appropriate dosages for minimum 6 weeks) according to available treatment guidelines for BD I (31).
Data was collected on marital status, occupational status, and educational level. Four groups were defined: “First treatment patients” were defined based on treatment history as patients receiving their first adequate treatment of the disorder in question within the last 12 months. “Schizophrenia spectrum” (SS) included schizophrenia, schizophreniform disorder, schizoaffective disorder, psychotic disorder NOS and delusional disorder and was further divided into “First Treatment Schizophrenia Spectrum” and “Multi-episode Schizophrenia Spectrum” based on treatment history. “Bipolar disorder” (BD) included bipolar disorder I, II and NOS and was divided into “First Treatment Bipolar Disorder” and “Multi-episode Bipolar Disorder.”
Assessment of Medication, Functioning, Symptoms and Socio-Demographical Characteristics at First Assessment (Baseline) and 12 Months Follow-Up
All patients were assessed at first recruitment (“Baseline”) and 12 months later. At both time points, information on type and dosage of all antipsychotic medication was collected. Defined daily doses (DDD) were defined according to the WHO criteria (32, 33). For comparison of DDDs and Chlorpromazine equivalents, see Table 1. The ratios of currently prescribed daily dosage of an antipsychotic (PDD) and the corresponding DDD (PDD/DDD) were calculated for each prescribed antipsychotic. The sum of all PDD/DDD ratios for each participant was used as an estimate of current load of antipsychotics across different types of drugs. “PDD/DDD change” was created by subtracting PDD/DDD at 12 months follow-up from PDD/DDD at baseline (including cases not using antipsychotics, i.e., PDD/DDD = 0, at follow-up). The Udvalg for Kliniske Undersøgelser (UKU) side effect rating scale (34) was used to measure type and severity of side effects. All items in the UKU scale were scored from 0 to 3, where 0 indicated no side-effect, and scores 1–3 indicated presence of side-effect with increasing severity.
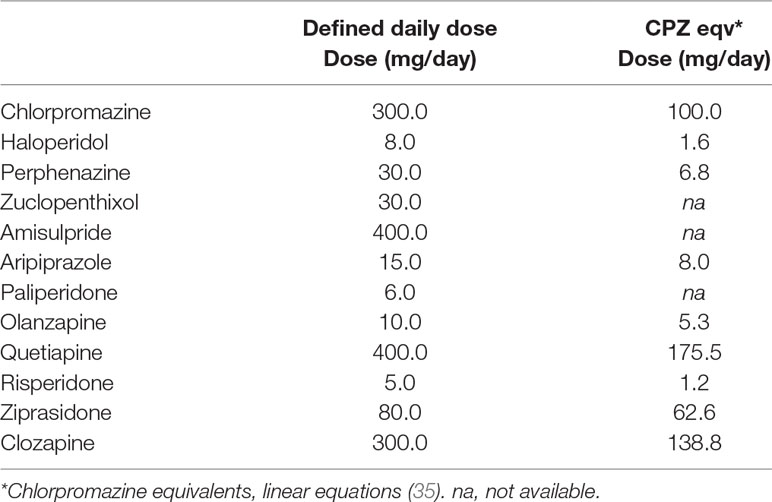
Table 1 Prescribed antipsychotics and comparison of defined daily dose and chlorpromazine equivalents.
Insight was measured by the Birchwood Insight scale (36) items 2 and 8, and low levels of insight were defined as a score of 3 or higher. Level of physical activity was assessed by the clinicians as “light,” “medium,” or “heavy.” Patients were interviewed about substance use prior to first assessment and in the follow-up period based on a common semi-structured interview form and from section “E” of the SCID (29). Current global functioning and symptoms were assessed by the Global Assessment of Functioning Scale (GAF), using the split version of GAF, with separate scores for symptoms and functioning (37). Current psychotic symptoms were assessed by the Positive and Negative Syndrome Scale (PANSS) (38). Current depressive symptoms were measured with the Inventory of Depressive Symptoms – Clinician rated (IDS-C) (39), and current manic symptoms were rated with the Young Mania Rating Scale (YMRS) (40). The Alcohol Use Disorders Identification Test (AUDIT) (41) was used to identify problematic alcohol use.
The inter-rater reliability of the symptom assessments in the TOP study have been shown to be good with an Intraclass Coefficient (ICC) (42) of 0.82 for PANSS positive symptoms and 0.86 for GAF (28).
Statistics
All analyses were performed using the Statistical Package for the Social Sciences (SPSS version 25.0, SPSS Inc., Chicago, IL, USA). Differences between categorical variables were analyzed using chi square tests. Differences between normally distributed continuous variables were analyzed using univariate analyses of variance with post hoc Bonferroni corrections and paired t-tests as appropriate. Significance level was set to 0.05, two-tailed.
A two-way between-groups analysis of variance was conducted to explore the impact of diagnostic group (schizophrenia spectrum or bipolar disorder spectrum) and treatment group (first treatment or multi-episode) on change in dosage of antipsychotics. To identify predictors for change in dosages of antipsychotics from first treatment we performed a series of follow-up multivariate analyses for each group. We here used multiple linear regression analyses for normally distributed dependent variables, with independents entered hierarchically in several blocks. Age and sex were selected as priori independent variables, in addition to baseline measures regarded as plausible predictive factors for inducing change, including measures of common side-effects, insight and reported compliance. Additional putative predictors were added based on findings of significant bivariate associations to changes in dosage of antipsychotic medication in the current sample. The assumption of a linear relationship was evaluated based on examinations of residual plots for each analysis, and on examination of influential observations based on leverages and Cox distances. The final model with the best fits is presented in the paper.
Results
A total of 426 patients were included in the current study, with assessments both at baseline and follow-up. Their demographic and clinical characteristics at baseline are described in Table 2. Out of these, 136 patients did not use antipsychotics at baseline (First Treatment Schizophrenia Spectrum: 40 (21% within the diagnostic group); First Treatment Bipolar Disorder: 47 (47% within the diagnostic group); Multi-episode Schizophrenia Spectrum: 10 (15% within the diagnostic group); Multi-episode Bipolar Disorder: 39 (57% within the diagnostic group)). Eight patients did not have reliable information for antipsychotic use at follow-up. For the 286 patients with information on dosage of antipsychotics at baseline, the schizophrenia spectrum patients used significantly higher dosages of antipsychotics than bipolar disorder patients (Table 3). There were no significant differences between first-episode and multi-episode groups.
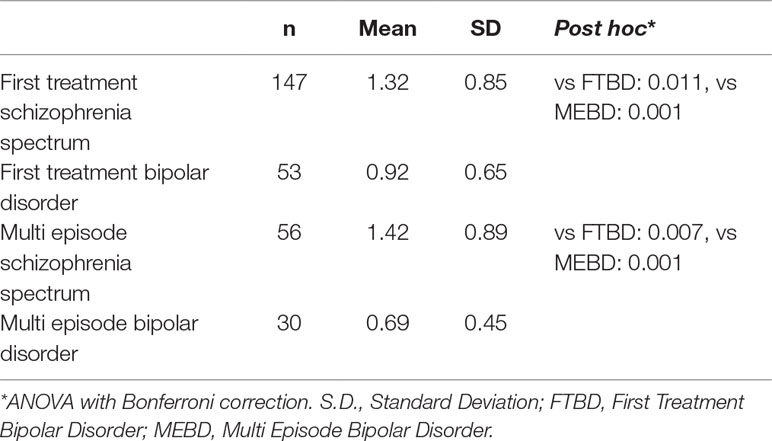
Table 3 Total dosage of prescribed antipsychotics per defined daily dose (PDD/DDD) of all antipsychotics in use at baseline. N = 286 with information on PDD/DDD at baseline.
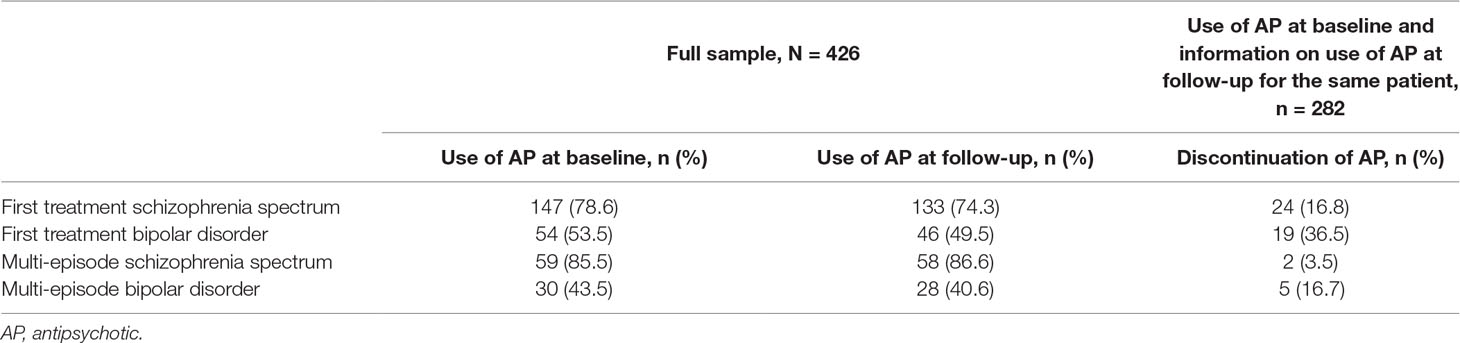
Use of antipsychotics and discontinuation rates for the different groups at baseline and follow-up are shown in Table 4. Of the 290 patients using antipsychotics at baseline, we had information on use of antipsychotics at follow-up for 282, of these 50 (18%) discontinued use. The difference in discontinuation rates between First Treatment Schizophrenia Spectrum and First Treatment Bipolar Disorder was statistically significant (x2 = 4.6, p = 0.032). Thirteen (68%) of those discontinuing antipsychotics in the First Treatment Bipolar Disorder group had however changed to mood stabilizers at follow-up.
There was a statistically significant reduction in antipsychotic dosage for both the First Treatment Schizophrenia Spectrum group and the First Treatment Bipolar Disorder group. There were no significant changes in antipsychotic use in the two multi-episode illness groups (Figure 1). A two-way between-groups analysis of variance with change in PDD/DDD ratios as dependent variable showed a statistically significant main effect for treatment group (first-treatment versus multi-episode) (F = 4.66, p = 0.032), however with a small effect size (ခη20.02). There was no significant main effect for diagnostic group and no significant interaction effects.
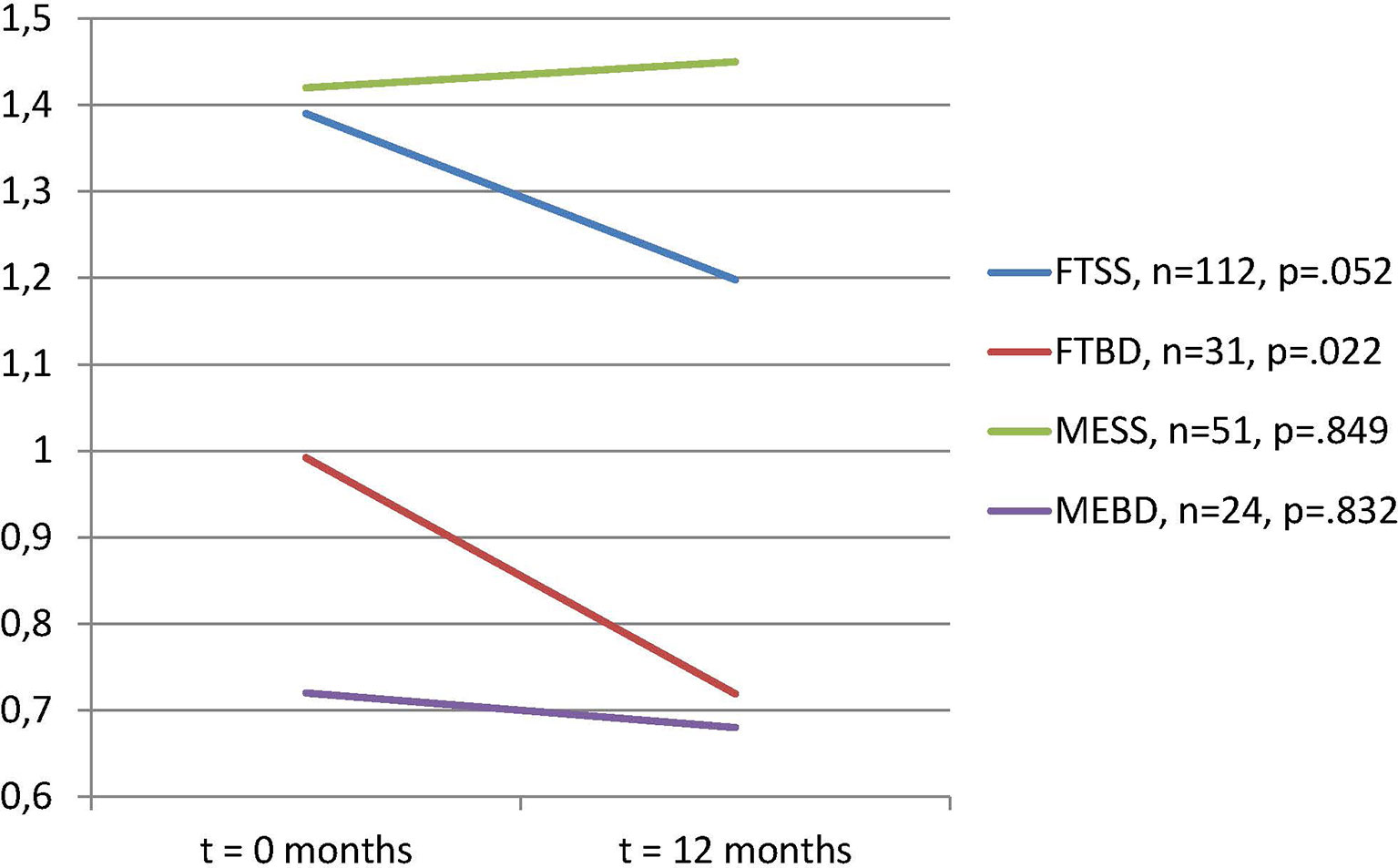
Figure 1 Total dosage of prescribed antipsychotics per defined daily dose (PDD/DDD) of all antipsychotics in use, paired samples of subjects with dosages >0 at t = 0. Paired t-tests. N = 218 with information on PDD/DDD and use at both time points.
Bivariate analyses showed the following group-wise significant associations with change in dosage of antipsychotics measured as PDD/DDD ratio: First Treatment Schizophrenia Spectrum: Age (+), PDD/DDD for all antipsychotics at baseline (−), UKU weight gain (−), UKU investigators’ assessment of global side effect load (−) and level of physical activity (−); First Treatment Bipolar Disorder: PDD/DDD for all antipsychotics at baseline (−), UKU hypokinesia (−), GAF-F (+), and PANSS-P scores (−). Since there were no changes for multi-episode patients, we did not do follow-up analyses for these groups.
Final combined models for the multivariate linear regressions analyses are presented in Supplementary Tables 1A, B. In First Treatment Schizophrenia Spectrum, a reduction in antipsychotic PDD/DDD ratio was significantly associated, with a small effect size, with baseline weight increase as a side effect of medication, as judged by the person conducting the assessment. In First Treatment Bipolar Disorder, a reduction in antipsychotic PDD/DDD ratio was significantly associated, with a small to medium effect size, with baseline higher levels of positive psychotic symptoms as measured by the PANSS.
The logistic regression analysis with discontinuation as the dependent variable showed significant contributions to the risk of discontinuation from higher GAF-F and alcohol use (AUDIT scores) at baseline in First Treatment Schizophrenia Spectrum, and from increased age in First Treatment Bipolar Disorder, significant odds ratios were in the range from 1.06 to 1.11 (Supplementary Tables 2A, B).
Discussion
As expected, and in line with current clinical recommendations (43, 44), we found that patients with schizophrenia spectrum disorders used higher dosages of antipsychotics compared to patients with bipolar disorders in both first-treatment and multi-episode groups. Contrary to clinical recommendations, we did not find that first-treatment patients used lower dosages at baseline as compared to multi-episode patients in both diagnostic groups. However, both first treatment groups showed significant reductions in dosages of antipsychotics over the first year of treatment, while both multi-episode groups did not show significant change.
In First Treatment Schizophrenia Spectrum, weight gain at baseline was a statistically significant predictor of dosage reduction over the first year of treatment. Although the effect size was modest, the association between weight gain and dosage reduction may be taken as an indication of awareness of the risks associated with obesity in this patient group, an aspect which is receiving increasing focus in clinical guidelines (2, 45).
In the First Treatment Bipolar Disorder group, the baseline level of positive psychotic symptoms predicted dosage reduction of antipsychotics, although with a small to moderate effect size. The higher dosages of antipsychotics in the First Treatment Bipolar Disorder compared to the Multi-episode Bipolar Disorder group at baseline could thus partly be explained by the first treatment patients being closer in time to an acute phase with high symptom levels. Antipsychotics are recommended for the acute phase of mania (44), and the high dosages observed could be a transient response to treatment needs in this phase and thus in line with main guidelines (1, 2, 5). Taken together, our findings point to diagnostic-specific associations with dosage reductions in first treatment patients.
The discontinuation rates found in the First Treatment Schizophrenia Spectrum group are in line with previous findings (46). We found that high levels of functioning and problematic use of alcohol at baseline significantly predicted discontinuation in this group. These findings are clinically meaningful, as alcohol abuse has been shown to affect adherence to medical advice (45). To the best of our knowledge, there are no previous reports of discontinuations rates of antipsychotics in First Treatment Bipolar Disorder. The rate in this group is higher than that observed in the other three groups, again indicating that the medication at baseline is a transient response to acute mania. In the First Treatment Bipolar Disorder group we found that increased age was a significant predictor of discontinuation of antipsychotics. Increased age is usually associated with improved adherence to treatment; however, in this case the patients discontinued antipsychotic treatment and changed to other psychopharmacological agents. A possible explanation could be that clinicians felt more confident of their diagnosis of BD in the older patients and thus were more prone to change to mood stabilizing medication for secondary prevention.
In this context, we should note that adherence to prescribed medication is a major challenge for first episode patients (47, 48). In addition, previous studies have found that physicians’ adherence to guidelines is adequate in the initial phase of treatment but reduces over time (49). The recommendation of low dosages for first-treatment phases also pertains to the acute phases of illness, and previous studies indicate that lower acute phase dosages is an achievable goal (50). Our findings may thus indicate that early dosage practices are more driven by acute phase symptoms than by guideline recommendations. Relapse prevention dosages are however in line with recommendations, with a particular emphasis on risk associated with obesity in First Treatment Schizophrenia Spectrum. In First Treatment Bipolar Disorder, antipsychotics appear to be used mainly as an acute phase treatment and not as relapse prevention.
The main strength of the current study is the well characterized and relatively large prospective sample of first-treatment patients with, both schizophrenia- and bipolar spectrum disorders followed over the early treatment phase. The catchment area based and consecutive sampling procedure, including both in-and outpatient treatment services, gives the sample a high degree of representation. The study also has some limitations. Although our cohorts of first treatment patients are large compared to other studies of bipolar disorders, some of the subgroups were relatively small which may increase the risk of type II errors. The study also used cross-sectional assessments at two time points, and there were thus restricted possibilities for a temporal sequencing of events in the follow-up period.
In conclusion, a statistically significant reduction in dosages over the first 12 months of treatment was associated with early medication-related weight increase in first treatment schizophrenia, and with higher levels of psychotic symptoms at baseline in first treatment bipolar disorder. Our findings thus document potentially clinically meaningful diagnostic differences in patterns of prescription and adaptive prescription changes in the early treatment phases of psychotic disorders, and add to the understanding of what drives early antipsychotic dosage change. We did not find indications of lower dosages of antipsychotics at baseline in first-treatment patients compared to multi-episode patients across diagnostic groups. Further, our findings emphasize the risks for discontinuation associated with all types of substance abuse, including alcohol. There is a need for more specific treatment recommendations for the use of antipsychotics in the early treated phases of bipolar disorder. Further studies should preferably investigate motivations for medication change for the physicians, in addition to patients.
Ethics Statement
All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by The Regional Committee on Research Ethics of South Eastern Norway.
Author Contributions
PR and IM contributed to the conception and design of the study, performed the statistical analysis, and wrote the first draft of the manuscript. PR organized the database. ER, TV, OA, and NS wrote sections of the manuscript. All authors contributed to manuscript revision, and read and approved the submitted version.
Funding
The study received funding from the Oslo University Hospital, the Regional Health Authority South Eastern Norway (Grant #2014-102) and the Research Council of Norway (Grant #223273).
Conflict of Interest Statement
OA received speakers’ honoraria from Lundbeck.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank the participating patients. We thank Kevin O’Connell at the University of Oslo for help with language.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2019.00649/full#supplementary-material
References
1. American Psychiatric Association Practice Guidelines for the treatment of psychiatric disorders: compendium 2006. Arlington (VA): American Psychiatric Pub (2006).
2. NICE. Psychosis and schizophrenia in adults: prevention and management: National Institute for Clinical Excellence; 2014 [updated March 201410. 07.2018]. Available from: https://www.nice.org.uk/guidance/cg178.
3. Ogawa Y, Tajika A, Takeshima N, Hayasaka Y, Furukawa TA. Mood stabilizers and antipsychotics for acute mania: a systematic review and meta-analysis of combination/augmentation therapy versus monotherapy. CNS Drugs (2014) 28(11):989–1003. doi: 10.1007/s40263-014-0197-8
4. Lindström L, Lindström E, Nilsson M, Höistad M. Maintenance therapy with second generation antipsychotics for bipolar disorder – a systematic review and meta-analysis. J Affective Disord (2017) 213:138–50. doi: 10.1016/j.jad.2017.02.012
5. Fountoulakis KN, Grunze H, Vieta E, Young A, Yatham L, Blier P, et al. The International College of Neuro-Psychopharmacology (CINP) treatment guidelines for bipolar disorder in adults (CINP-BD-2017), Part 3: The Clinical Guidelines. Int J Neuropsychopharmacol (2017) 20(2):180–95. doi: 10.1093/ijnp/pyw109
6. Correll CU, Rubio JM, Kane JM. What is the risk–benefit ratio of long-term antipsychotic treatment in people with schizophrenia? World Psychiatry (2018) 17(2):149–60. doi: 10.1002/wps.20516
7. Wunderink L, Nieboer RM, Wiersma D, Sytema S, Nienhuis FJ. Recovery in remitted first-episode psychosis at 7 years of follow-up of an early dose reduction/discontinuation or maintenance treatment strategy: long-term follow-up of a 2-year randomized clinical trial. JAMA Psychiatry (2013) 70(9):913–20. doi: 10.1001/jamapsychiatry.2013.19
8. Gøtzsche PC. Deadly medicines and organised crime. In: How big pharma has corrupted healthcare. Radcliffe Publishing (2013).
9. Huhtaniska S, Jääkelälinen E, Hirvonen N, Remes J, Murray GK, et al. Long-term antipsychotic use and brain changes in schizophrenia — a systematic review and meta-analysis. Hum Psychopharmacol: Clin Exp (2017) 32(2):e2574. doi: 10.1002/hup.2574
10. Moncrieff J. Antipsychotic maintenance treatment: time to rethink? PLoS Med (2015) 12(8):e1001861. doi: 10.1371/journal.pmed.1001861
11. Murray RM, Quattrone D, Natesan S, van Os J, Nordentoft M, Howes O, et al. Should psychiatrists be more cautious about the long-term prophylactic use of antipsychotics? Br J Psychiatry (2018) 209(5):361–5. doi: 10.1192/bjp.bp.116.182683
12. Friis S, Melle I, Johannessen JO, Røssberg JI, Barder HE, Evensen JH, et al. Early predictors of ten-year course in first-episode psychosis. Psychiatric Serv (2016) 67(4):438–43. doi: 10.1176/appi.ps.201400558
13. Santesteban-Echarri O, Paino M, Rice S, González-Blanch C, McGorry P, Gleeson J, et al. Predictors of functional recovery in first-episode psychosis: a systematic review and meta-analysis of longitudinal studies. Clin Psychol Rev (2017) 58:59–75. doi: 10.1016/j.cpr.2017.09.007
14. Melle I, Larsen TK, Haahr U, Friis S, Johannessen JO, Opjordsmoen S, et al. Reducing the duration of untreated first-episode psychosis: effects on clinical presentation. Arch Gen Psychiatry (2004) 61(2):143–50. doi: 10.1001/archpsyc.61.2.143
15. Huq Z-U. A trial of low doses of risperidone in the treatment of patients with first-episode schizophrenia, schizophreniform disorder, or schizoaffective disorder. J Clin Psychopharmacol (2004) 24(2):220–4. doi: 10.1097/01.jcp.0000115663.45074.8a
16. International Early Psychosis Association Writing Group. International clinical practice guidelines for early psychosis. Br J Psychiatry Suppl (2005) 48:120–4. doi: 10.1192/bjp.187.48.s120
17. Adrian H, Mark L, Alison Y, MA DH. Prescribing in schizophrenia and psychosis: increasing polypharmacy over time. Human Psychopharmacology. Clin Exp (2017) 32(2):e2579. doi: 10.1002/hup.2579
18. Mojtabai R, Olfson M. National trends in psychotropic medication polypharmacy in office-based psychiatry. Arch Gen Psychiatry (2010) 67(1):26–36. doi: 10.1001/archgenpsychiatry.2009.175
19. Tang Y, Chang C-CH, Lave JR, Gellad WF, Huskamp HA, Donohue JM. Patient, physician and organizational influences on variation in antipsychotic prescribing behavior. J Mental Health Policy Econ (2016) 19(1):45–59.
20. Franz M, Ranger J, Hanewald B, Gallhofer B, Lay B. Influences on therapist’s decisions for neuroleptic treatment in schizophrenia: the role of characteristics of the patient and the physician. Pharmacopsychiatry (2012) 45(07):261–8. doi: 10.1055/s-0032-1312609
21. Hoblyn J, Noda A, Yesavage JA, Brooks JO, Sheikh J, Lee T, et al. Factors in choosing atypical antipsychotics: toward understanding the bases of physicians’ prescribing decisions. J Psychiatric Res (2006) 40(2):160–6. doi: 10.1016/j.jpsychires.2005.06.004
22. Kaddurah-Daouk R, Weinshilboum RM. Pharmacometabolomics: implications for clinical pharmacology and systems pharmacology. Clin Pharmacol Ther (2014) 95(2):154–67. doi: 10.1038/clpt.2013.217
23. Amato D, Vernon AC, Papaleo F. Dopamine, the antipsychotic molecule: a perspective on mechanisms underlying antipsychotic response variability. Neurosci Biobehav Rev (2018) 85:146–59. doi: 10.1016/j.neubiorev.2017.09.027
24. Arango C, Kapur S, Kahn RS. Going beyond “trial-and-error” in psychiatric treatments: OPTiMiSE-ing the treatment of first episode of schizophrenia. Schizophr Bull (2015) 41(3):546–8. doi: 10.1093/schbul/sbv026
25. Faerden A, Finset A, Friis S, Agartz I, Barrett EA, Nesvåg R, et al. Apathy in first episode psychosis patients: one year follow up. Schizophr Res (2010) 116(1):20–6. doi: 10.1016/j.schres.2009.10.014
26. Hellvin T, Sundet K, Simonsen C, Aminoff SR, Lagerberg TV, Andreassen OA, et al. Neurocognitive functioning in patients recently diagnosed with bipolar disorder. Bipolar Disord (2012) 14(3):227–38. doi: 10.1111/j.1399-5618.2012.01004.x
27. Kvitland LR, Melle I, Aminoff SR, Demmo C, Lagerberg TV, Andreassen OA, et al. Continued cannabis use at one year follow up is associated with elevated mood and lower global functioning in bipolar I disorder. BMC Psychiatry (2015) 15:11. doi: 10.1186/s12888-015-0389-x
28. Ringen PA, Lagerberg TV, Birkenaes AB, Engh JA, Faerden A, Jonsdottir H, et al. Differences in prevalence and patterns of substance use in schizophrenia and bipolar disorder. Psychol Med (2008) 38(9):1241–9. doi: 10.1017/S003329170700236X
29. First MB, Tasman A. DSM-IV-TR mental disorders. Diagnosis, etiology and treatment. Chichester: Wiley (2004). p. 2004.
30. Ventura J, Liberman RP, Green MF, Shaner A, Mintz J. Training and quality assurance with the Structured Clinical Interview for DSM-IV (SCID-I/P). Psychiatry Res (1998) 79(2):163–73. doi: 10.1016/S0165-1781(98)00038-9
31. Goodwin FK, Jamison KR. Manic-Depressive Illness. 2nd edn. New York: Oxford University Press (2007)
32. WHO Collaborating Centre for Drug Statistics Methodology ATC classification index with DDDs 2008 Oslo, Norway.
33. Leucht S, Samara M, Heres S, Davis JM. Dose equivalents for antipsychotic drugs: the DDD method. Schizophr Bull (2016) 42(suppl_1):S90–4. doi: 10.1093/schbul/sbv167
34. Lingjærde O, Ahlfors UG, Bech P, Dencker SJ, Elgen K. The UKU side effect rating scale: a new comprehensive rating scale for psychotropic drugs and a cross-sectional study of side effects in neuroleptic-treated patients. Acta Psychiatrica Scandinavica (1987) 76(s334):1–100. doi: 10.1111/j.1600-0447.1987.tb10566.x
35. Patel MX, Arista IA, Taylor M, Barnes TRE. How to compare doses of different antipsychotics: a systematic review of methods. Schizophr Res (2013) 149(1):141–8. doi: 10.1016/j.schres.2013.06.030
36. Birchwood M, Smith J, Drury V, Healy J, Macmillan F, Slade M. A self-report insight scale for psychosis: reliability, validity and sensitivity to change. Acta Psychiatr Scand (1994) 89(1):62–7. doi: 10.1111/j.1600-0447.1994.tb01487.x
37. Pedersen G, Hagtvet KA, Karterud S. Generalizability studies of the global assessment of functioning-split version. Compr Psychiatry (2007) 48(1):88–94. doi: 10.1016/j.comppsych.2006.03.008
38. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull (1987) 13(2):261–76. doi: 10.1093/schbul/13.2.261
39. Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH. The Inventory of Depressive Symptomatology (IDS): psychometric properties. Psychol Med (1996) 26(3):477–86. doi: 10.1017/S0033291700035558
40. Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry (1978) 133:429–35. doi: 10.1192/bjp.133.5.429
41. Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption—II. Addiction (1993) 88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x
42. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull (1979) 86(2):420–8. doi: 10.1037//0033-2909.86.2.420
43. Hasan A, Falkai P, Wobrock T, Lieberman J, Glenthoj B, Gattaz WF, et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, Part 1: Update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J Biol Psychiatry (2012) 13(5):318–78. doi: 10.3109/15622975.2012.696143
44. Grunze H, Vieta E, Goodwin GM, Bowden C, Licht RW, Möller H-J, et al. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders: update 2009 on the treatment of acute mania. World J Biol Psychiatry (2009) 10(2):85–116. doi: 10.1080/15622970902823202
45. Baldessarini RJ, Perry R, Pike J. Factors associated with treatment nonadherence among US bipolar disorder patients. Hum Psychopharmacol: Clin Exp (2008) 23(2):95–105. doi: 10.1002/hup.908
46. Landolt K, Rössler W, Ajdacic-Gross V, Derks EM, Libiger J, Kahn RS, et al. Predictors of discontinuation of antipsychotic medication and subsequent outcomes in the European First Episode Schizophrenia Trial (EUFEST). Schizophr Res (2016) 172(1):145–51. doi: 10.1016/j.schres.2016.01.046
47. Abdel-Baki A, Ouellet-Plamondon C, Malla A. Pharmacotherapy challenges in patients with first-episode psychosis. J Affective Disord (2012) 138:S3–14. doi: 10.1016/j.jad.2012.02.029
48. García S, Martínez-Cengotitabengoa M, López-Zurbano S, Zorrilla I, López P, Vieta E, et al. Adherence to antipsychotic medication in bipolar disorder and schizophrenic patients: a systematic review. J Clin Psychopharmacol (2016) 36(4):355–71. doi: 10.1097/JCP.0000000000000523
49. Yeisen RAH, Joa I, Johannessen JO, Opjordsmoen S. Use of medication algorithms in first episode psychosis: a naturalistic observational study. Early Interv Psychiatry (2016) 10(6):503–10. doi: 10.1111/eip.12203
Keywords: antipsychotics, schizophrenia, bipolar disorder, prescription, dosage
Citation: Ringen PA, Reponen EJ, Vedal TSJ, Andreassen OA., Steen NE and Melle I (2019) Predictors for Antipsychotic Dosage Change in the First Year of Treatment in Schizophrenia Spectrum and Bipolar Disorders. Front. Psychiatry 10:649. doi: 10.3389/fpsyt.2019.00649
Received: 28 November 2018; Accepted: 12 August 2019;
Published: 10 September 2019.
Edited by:
Silvio Bellino, University of Turin, ItalyReviewed by:
Joshua T. Kantrowitz, Columbia University, United StatesLaila Asmal, Stellenbosch University, South Africa
Copyright © 2019 Ringen, Reponen, Vedal, Andreassen, Steen and Melle. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Petter Andreas Ringen, p.a.ringen@medisin.uio.no
 Petter Andreas Ringen
Petter Andreas Ringen Elina Johanna Reponen
Elina Johanna Reponen Trude Seselie Jahr Vedal2
Trude Seselie Jahr Vedal2 Ola A. Andreassen
Ola A. Andreassen Nils Eiel Steen
Nils Eiel Steen Ingrid Melle
Ingrid Melle