- 1Department of Psychology, Stockholm University, Stockholm, Sweden
- 2Centre for Psychiatry Research, Department of Clinical Neuroscience, Karolinska Institutet, & Stockholm Health Care Services, Stockholm County Council, Stockholm, Sweden
- 3Center for Dependency Disorders, Stockholm Health Care Services, Stockholm County Council, Stockholm, Sweden
- 4Mimerse, Stockholm, Sweden
- 5Department of Psychology, University of Southern Denmark, Odense, Denmark
Depression is a common mental disorder with a large treatment gap. Low-intensity, automated virtual reality (VR) interventions (not requiring a therapist) is a scalable and promising solution now that VR is an accessible and mature, consumer technology. Yet unlike with phobias, there have been few attempts at translating evidence-based cognitive behavioral therapeutic (CBT) techniques for depression into the VR modality. In this paper, we discuss how specific CBT techniques can be made into VR experiences, including psychoeducation, behavioral activation, cognitive restructuring, and social skills training. We also discuss how VR-unique experiences, such as alternative embodiment and virtual pet interactions, can be made therapeutic. Creating a pre-clinical and clinical evidence base for these types of novel interventions should be considered a research priority, and high-quality development on par with other consumer VR applications will be essential to the success of any consumer-targeted intervention. If this is achieved, low-intensity VR interventions for depression have great potential to make an impact on public mental health.
Introduction
Depression is a major contributor to the global burden of disease (1), with an estimated 10% of the Swedish population reporting clinically significant symptoms (2). While spontaneous remission is not uncommon (3), depression episodes commonly become recurrent (4) and only an estimated half of sufferers seek treatment (5). Cognitive behavior therapy (CBT) refers to a diverse yet coherent collection of therapeutic techniques that aim to promote change in behavior and cognition. CBT is demonstrably effective in reducing depressive symptoms (6) and has proven remarkably flexible in terms of format: in addition to the traditional therapist-led format, Internet-delivered CBT self-help, with or without guidance, is also an evidence-based intervention for depression (7). Burgeoning evidence suggests that smartphone applications are also a viable and efficacious delivery format (8).
Another consumer technology with potential to act as a delivery format for CBT for depression is Virtual Reality (VR), a technology that allows the user to feel immersed in virtual, computer-generated world (9). This is typically achieved using a head-mounted display that withholds the outside world, while a stereoscopic display creates the illusion of depth perception, the presentation of which is interactive to head movements (measured using gyroscopes), allowing the user to look around the virtual environment. Sound effects can be used to strengthen immersion, and handheld controllers provide an additional means of interacting with the virtual environment by acting as a mouse pointer or virtual hands. High-quality, standalone mobile VR platforms now cost as little as 240 USD and feature mature and rich digital marketplaces for easy dissemination of applications, making VR an affordable and accessible consumer technology (10).
VR technology provides full control over the user’s experience, which can be used for therapeutic purposes. Most past research on VR interventions for mental health have been focused on treating anxiety disorders (9, 11), and for pain distraction (12, 13) and relaxation (14, 15). There is ample evidence to support efficacy in these areas, even as automated self-help applications (16–18). There is however a striking dearth of VR interventions for depression (19). From a technological perspective, it is relatively easy to present the user with either a virtual equivalent of the phobic stimulus to enable exposure therapy (for anxiety disorders), use immersive game mechanics for sensory distraction (for pain relief), or situating the user in a calming natural environment (for relaxation). As evident by the scarce extant literature, translating evidence-based CBT techniques used in treating depression into the VR modality has however proven a much greater challenge.
In this paper, we discuss ways of translating traditional CBT techniques for depression into the VR modality, as well as how to make use of the inherent capabilities of VR-unique experiences to treat depression, especially in the form of low-intensity interventions. We hope that these discussion points inspire and inform a new generation of consumer-targeted VR interventions for depression.
Translating CBT Techniques Into VR
Immersive Psychoeducation and Problem Solving
Almost all psychotherapeutic techniques require psychoeducation to some degree, which at minimum includes conveying a coherent conceptualization of the symptom/syndrome in question, and possibly a derived treatment rationale and instructions for exercises. Even passive psychoeducation has a small anti-depressive effect (20). In CBT, this often includes generic problem-solving skills such as breaking larger goals and tasks into smaller units, how to plan, record and evaluate exercises, brainstorming ideas and filtering, and similar skills.
Immersive VR experiences rely on a clear, binary distinction between the virtual and real world, making it suboptimal to use VR as a bridge between the therapeutic context (planning, tracking, and evaluating) and the real-life setting where the exercise is performed. Traditional pen-and-paper, or companion smartphone applications are better choices here. VR is however inherently very well suited for passive psychoeducation. Recent automated VR applications have taken conservative approaches to conveying psychoeducation in VR, e.g., in the form of a virtual therapist office and projector screen (18), yet VR can be used to create much more immersive and thereby likely efficacious psychoeducation. Here, the fields of educational and entertainment VR may serve as an inspiration and source of knowledge. VR is considered a powerful educational tool since it allows user to experience, rather than simply perceive, what is to be learned (21). Thus, VR holds an advantage over traditional, non-immersive delivery only when the experience is complex, dynamic, exciting, and instills a sense of presence (22, 23). CBT often encourages viewing things as objectively as possible in order to disprove experiences and cognitions that are contaminated by negative emotions. Using VR, the user could for example first experience a learning example scenario in the first or second person, and then view the same scenario as a third person (observer) and be asked to note discrepancies. Further, with VR, it is not only possible but preferable to animate the therapeutic material to a coherent and continuous narrative, pausing only for interactive elements that can be used to tailor the experience. A recently developed, single-session VR intervention for depressed adolescents that teaches and encourages a growth mindset, incorporates many of these elements (24).
Behavioral Activation and Physical Activity
Behavioral activation (BA) is a core part of CBT for depression and departs from an operant view of depression as a vicious circle of withdrawal from rewarding activities (25), the remedy for which is functional assessment and stepwise activity scheduling in order for the patient to once again come in contact with natural reinforcers (26). While it would certainly be appropriate to present the treatment rational and specific techniques in an immersive fashion using VR (as discussed above), actually performing appropriate activities in VR has some inherent caveats. Primarily, BA typically focuses on decreasing solitary, at-home technology use (often part of the clinical presentation of depression) and instead promoting engagement with the outside world. Simply recreating VR equivalents of the everyday tasks often used as targets in ordinary BA is thus unlikely to be effective or appropriate, although this is ultimately an empirical question, as of yet unanswered.
Physical activity and social gatherings in VR would however be clinically appropriate targets to increase the frequency of. From a behavioral therapeutic perspective, physical activity can be seen as a special case of BA, and there are several large trials showing comparable effects on depression of BA versus physical activity (27, 28). Combining VR and moderate physical activity is relatively straightforward: any type of physical activity that can be performed on the spot and involves no quick, continuous head movements (which would induce motion sickness) can be done while wearing a mobile VR unit. In fact, VR exercise applications are some of the most popular on digital marketplaces, offering activities, such as VR boxing and tennis. Combining such activities with a BA treatment rationale (27) within a dedicated application has the potential to achieve similar anti-depressive effects as traditional physical activity.
The other appropriate VR BA target is to engage in virtual social gatherings. There are already several popular social VR applications that allow users not only to meet through avatars and voice chat but also to share experiences such as playing board games, singing karaoke, hosting movie nights, attending concerts, and more. A dedicated VR BA application could be designed to suggest social activities based on provided data and direct users to virtual gatherings through linkage to existing social VR applications.
Cognitive Restructuring
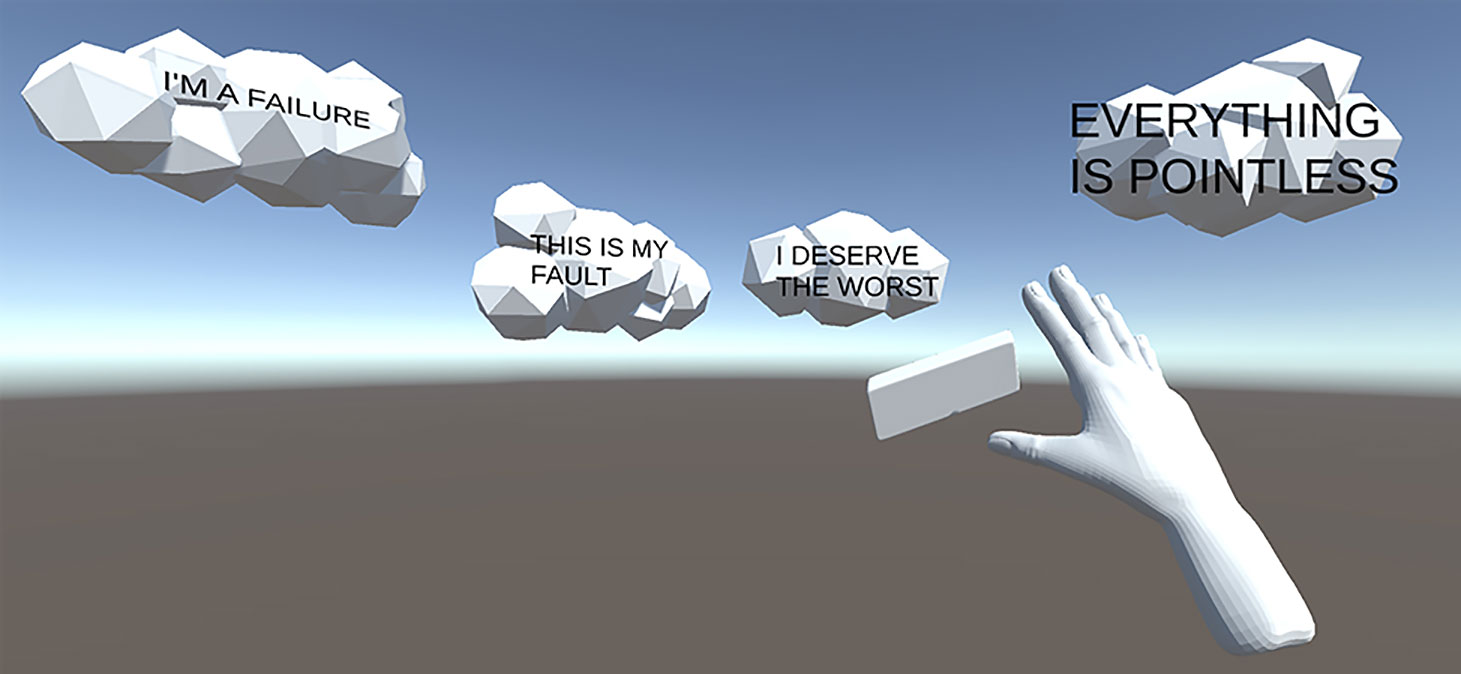
Cognitive restructuring refers to a collection of therapeutic techniques designed to identify cognitive patterns that maintain depressed mood, and to modify these (29). We see two attractive alternatives for translating this set of techniques into the VR modality: using VR as interactive visualization aid, and for imagery rescripting and positive imagery training. The former would entail making use of the powerful visual capabilities of VR and having the user create, manipulate, and observe therapeutic material in an immersive manner. Many cognitive exercises require the patient to imagine an example situation from which to extract and manipulate cognitions for exercise purposes; VR would enable virtually situating the user in this example situation, playing the example scenario, allowing the user to pause the scenario, and e.g. report negative automatic thoughts by visualizing them as speech balloon type objects. Handheld controllers may then be used to manipulate these objects in accordance with the aim of the exercise, e.g., using a virtual eraser, drag-and-drop sorting of matching cognitive distortions, or identifying evidence for and against underlying assumptions, etc. See Figure 1 for a demonstration. One recent study (30) provides a proof-of-concept for this approach, allowing the user to suspend self-critical words in virtual space and manipulate these objects with handheld controllers. Lasting clinical efficacy on depressive symptoms has however not yet been demonstrated.
A related type of cognitive exercise well-suited for the VR modality is imagery rescripting (31, 32) and positive imagery training (33). Both these techniques involve the patient using mental imagery to either recreate a memory (rescripting) or expand upon an example scenario in a prompted direction (positive imagery training), in their mind, as vividly as possible. In the case of rescripting, the patient is tasked with finding alternative solutions to the imagined situation that reduces their distress, and then rehearses a novel solution in greater and greater detail. In positive imagery training, the patient is instead prompted with a (positive) message and tasked with imagining the outcome, and repeating with a new scenario and message. In both these techniques, imagery vividness has been postulated as an important mediator of treatment effects, as is the case with imaginal exposure for anxiety disorders (34). Alas, there is great variability between individuals in vividness of mental imagery, measured both subjectively and with neuroimaging (35). VR could alleviate this issue by either completely replacing mental imagery with actual virtual scene-building and experiencing different alterations, or by acting as a powerful visual booster prior to subsequent mental imagery in order to increase vividness without the need for full scene-building.
An application for the latter would be easier to develop yet would still require mental imagery and be susceptible to inter-individual differences in vividness, while the former would require an advanced and content-rich sandbox type application (non-VR equivalents of which are already commercially available). Perfect agreement between the virtual scene and a memory is unlikely to ever be achieved, yet it is an open empirical question whether this is necessary or beneficial. Decades of research on VR exposure therapy for post-traumatic stress disorder with good but non-perfect agreement (36) suggests that this is not a prerequisite for efficacy. Congruently, one recent, innovative but low-powered study on exposure therapy for worry compared standardized VR scenarios against personalized imaginal exposure and found no difference in elicited anxiety (37). These findings do not however rule out the possibility that greater effects are possible with better agreement between idiosyncratic imagery and the VR material presented.
Social Skills Training
Social skills training is a generic CBT technique that conceptualizes everyday social behaviors as skills to be taught, practiced, and implemented in order to live a functional and fulfilling life (38). Such skills may include correctly interpreting and norm-appropriate responding to verbal and non-verbal social cues, conversational skills, assertiveness training, and relationship building. VR is uniquely well suited for training social skills via virtual conversational agents and immersive scenarios. VR social skill training interventions for autism (39) and schizophrenia (40) have already been evaluated and show promise, and the generic nature of this therapeutic technique suggests equally good results for depression.
Making Anti-Depressive Use of VR-Unique Experiences
Embodiment Experiences
VR allows unique and powerful experiences, which can be translated into unconventional clinical applications, granted that there is a theoretical rationale and pre-clinical evidence to support efficacy. One innovative example used VR and virtual embodiment to address self-criticism in depressed patients by having them first convey compassion to a crying virtual child while embodied in a virtual adult body, then receive the same, motion- and audio-captured acts of compassion when embodied in the child’s body, leading to decreased self-criticism and depressive symptoms (41). So-called avatar therapy is a related concept that could be made more powerful with VR (42) and possibly used in treating depression. Originally developed for patients with psychosis, avatar therapy involves the patient creating a virtual avatar and externalizing auditory verbal hallucinations to this avatar through seeing and hearing this avatar perform lines that the patient would otherwise have attributed to the verbal hallucinations (43). Avatar therapy could, in principle, also be used to externalize the self-criticism and other negative automatic thoughts frequently reported by depressed patients. This may help make cognitive exercises in identifying and disproving them, more concrete and easier to execute, leading to decreased frequency and alleviated depressive symptoms.
Positive Affect Through Virtual Gardens and Animals
The majority of CBT techniques target the excess of negative affect (sadness) aspect of depression, and even techniques such as BA have a limited effect on the deficit in positive affect (anhedonia) (44). A recently developed CBT paradigm, which includes augmented BA, mental imagery, and specifically targets deficit reward sensitivity, has however been shown to reduce anhedonia (45). Performing specific types of pleasurable activities in VR, and using virtual perspective changing and alternative embodiment in lieu of mental imagery, is both feasible and clinically appropriate; a clinical trial using a related approach is ongoing (NCT03715400). Such pleasurable activities may include virtual gardening and virtual pet interactions, akin to concentrated forms of gardening therapy (46) and animal-assisted therapy (47).
Discussion
Despite decades of research showing that VR technology can be used to treat phobias, stress and pain—which all require relatively simple virtual environments—there have been very few attempts to develop anti-depressive VR interventions. In this paper, we have discussed ways of translating existing CBT techniques into the VR modality, and how to make anti-depressive use of VR-unique experiences. While not without its challenges, we argue that some CBT techniques are not only suitable for the VR modality, but that the inherent capabilities of VR can even be used to augment the effect of these techniques.
Since VR is built on excluding the outside world and generating a virtual one, this medium is inherently well suited for delivery of so called low-intensity interventions that are scalable and require few resources to disseminate, which does not necessarily equate to being less intense for the person engaging with it. All the techniques discussed above can be automated, most at little extra development costs; interventions that require complex decision tress (e.g. to realistically mimic social interactions) will require more development resources but are certainly feasible using today’s technology. Automated VR treatments—for which there is growing evidence in the field of anxiety (16–18)—would then require no therapist to deliver and could be disseminated using ordinary digital marketplaces (18, 48) and reach hundreds of thousands of sufferers, promising a potent public health impact.
Unlike VR interventions for phobias, pain, and stress, for which there is already an evidence base, the field of anti-depressive VR applications is at an early stage, constituting an important limitation to the current state of research. Both pre-clinical research (e.g. on presumed mechanisms and human–computer interaction) and high-quality clinical trials should be considered a research priority. This is especially important for the VR-unique interventions discussed above, like alternative embodiment, where there is no evidence base from in-vivo equivalents. The field should strive to avoid a situation akin to the questionable clinical utility of consumer-targeted CBT smartphone applications for depression (49): however, the uniqueness of the VR medium along with the lack of an evidence base, entails that the future assortment of consumer-targeted VR interventions for depression available at digital marketplaces will likely end up with an equally poor clinical utility. Research must keep up with the expected market-driven application development in order to guide it. As with all low-intensity interventions and the stepped care model, inefficacious low-intensity VR interventions, or a mismatch between severity and care step, will delay care provided at the appropriate and satisfactory level.
All the VR techniques discussed above will benefit immensely from high-quality development on par with the commercial VR applications (e.g. regular games) that will realistically compete for the user’s time, especially if disseminated as consumer-targeted applications on regular digital marketplaces. High-quality development includes a visually pleasing graphical user interface, user-friendly design, gamification elements to promote repeated use, and other aspects that consumers expect from any application. In many VR therapeutic techniques, sense of presence not only moderates but also mediates outcomes, and presence-breaking elements and events must be avoided at all costs (including sacrificing maximum graphical fidelity). Careful design considerations should be made at an early stage in development and revised through iterative testing, taking into account core characteristics of both the disorder, therapeutic mechanism, and user experience (50).
Conclusions
VR is a clinically appropriate treatment modality for many existing CBT techniques and the extant literature suggests that VR-unique experiences can be put to anti-depressive use. Low-intensity, consumer-targeted VR interventions built around evidence-based therapeutic techniques have great potential to decrease the depression treatment gap and make an impact on public mental health.
Author Contributions
Drafted the manuscript: PL. Made significant contributions to the manuscript: WH, AM, and PC.
Conflict of Interest
Author WH is the founder and chief technology officer of Mimerse, a company specializing in developing VR interventions for mental health. Author PL has consulted for Mimerse but holds no financial stake in the company.
References
1. James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global burden of disease study 2017. Lancet (2018) 392:1789–858. doi: 10.1016/S0140-6736(18)32279-7
2. Johansson R, Carlbring P, Heedman Å, Paxling B, Andersson G. Depression, anxiety and their comorbidity in the Swedish general population: point prevalence and the effect on health-related quality of life. PeerJ (2013) 1:e98. doi: 10.7717/peerj.98
3. Whiteford HA, Harris MG, McKeon G, Baxter A, Pennell C, Barendregt JJ, et al. Estimating remission from untreated major depression: a systematic review and meta-analysis. Psychol Med (2013) 43:1569–85. doi: 10.1017/S0033291712001717
4. Mueller TI, Leon AC, Keller MB, Solomon DA, Endicott J, Coryell W, et al. Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. Am J Psychiatry (1999) 156:1000–6. doi: 10.1176/ajp.156.7.1000
5. Kohn R, Saxena S, Levav I, Saraceno B. The treatment gap in mental health care. Bull World Health Organ (2004) 82:858–66. doi: /S0042-96862004001100011
6. Cuijpers P, Cristea IA, Karyotaki E, Reijnders M, Huibers MJH. How effective are cognitive behavior therapies for major depression and anxiety disorders? A meta-analytic update of the evidence. World Psychiatry (2016) 15:245–58. doi: 10.1002/wps.20346
7. Carlbring P, Andersson G, Cuijpers P, Riper H, Hedman-Lagerlöf E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: an updated systematic review and meta-analysis. Cogn Behav Ther (2018) 47(1):1–18. doi: 10.1080/16506073.2017.1401115
8. Firth J, Torous J, Nicholas J, Carney R, Pratap A, Rosenbaum S, et al. The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials. World Psychiatry (2017) 16:287–98. doi: 10.1002/wps.20472
9. Botella C, Fernández-Álvarez J, Guillén V, García-Palacios A, Baños R. Recent progress in virtual reality exposure therapy for phobias: a systematic review. Curr Psychiatry Rep (2017) 19:42. doi: 10.1007/s11920-017-0788-4
10. Lindner P, Miloff A, Fagernäs S, Andersen J, Sigeman M, Andersson G, et al. Therapist-led and self-led one-session virtual reality exposure therapy for public speaking anxiety with consumer hardware and software: a randomized controlled trial. J Anxiety Disord (2019a) 61:45–54. doi: 10.1016/j.janxdis.2018.07.003
11. Carl E, Stein AT, Levihn-Coon A, Pogue JR, Rothbaum B, Emmelkamp P, et al. Virtual reality exposure therapy for anxiety and related disorders: a meta-analysis of randomized controlled trials. J Anxiety Disord (2019) 61:27–36. doi: 10.1016/j.janxdis.2018.08.003
12. Kenney MP, Milling LS. The effectiveness of virtual reality distraction for reducing pain: a meta-analysis. Psychol Conscious Theory Res Pract (2016) 3:199–210. doi: 10.1037/cns0000084
13. Malloy KM, Milling LS. The effectiveness of virtual reality distraction for pain reduction: a systematic review. Clin Psychol Rev (2010) 30:1011–8. doi: 10.1016/j.cpr.2010.07.001
14. Anderson AP, Mayer MD, Fellows AM, Cowan DR, Hegel MT, Buckey JC. Relaxation with Immersive Natural Scenes Presented Using Virtual Reality. Aerosp Med Hum Perform (2017) 88:520–6. doi: 10.3357/AMHP.4747.2017
15. Serrano B, Baños RM, Botella C. Virtual reality and stimulation of touch and smell for inducing relaxation: a randomized controlled trial. Comput Hum Behav (2016) 55:1–8. doi: 10.1016/j.chb.2015.08.007
16. Donker T, Cornelisz I, van Klaveren C, van Straten A, Carlbring P, Cuijpers P, et al. Effectiveness of self-guided app-based virtual reality cognitive behavior therapy for acrophobia. JAMA Psychiatry (2019) 76(7):682–90. doi: 10.1001/jamapsychiatry.2019.0219
17. Freeman D, Haselton P, Freeman J, Spanlang B, Kishore S, Albery E, et al. Automated psychological therapy using immersive virtual reality for treatment of fear of heights: a single-blind, parallel-group, randomised controlled trial. Lancet Psychiatry (2018) 5:625–32. doi: 10.1016/S2215-0366(18)30226-8
18. Miloff A, Lindner P, Dafgård P, Deak S, Garke M, Hamilton W, et al. Automated virtual reality exposure therapy for spider phobia vs. in-vivo one-session treatment: a randomized non-inferiority trial. Behav Res Ther (2019) 118:130–40. doi: 10.1016/j.brat.2019.04.004
19. Freeman D, Reeve S, Robinson A, Ehlers A, Clark D, Spanlang B, et al. Virtual reality in the assessment, understanding, and treatment of mental health disorders. Psychol Med (2017) 47:2393–400. doi: 10.1017/S003329171700040X
20. Donker T, Griffiths KM, Cuijpers P, Christensen H. Psychoeducation for depression, anxiety and psychological distress: a meta-analysis. BMC Med (2009) 7:79. doi: 10.1186/1741-7015-7-79
21. Lamb R, Antonenko P, Etopio E, Seccia A. Comparison of virtual reality and hands on activities in science education via functional near infrared spectroscopy. Comput Educ (2018) 124:14–26. doi: 10.1016/j.compedu.2018.05.014
22. Jensen L, Konradsen F. A review of the use of virtual reality head-mounted displays in education and training. Educ Inf Technol (2018) 23:1515–29. doi: 10.1007/s10639-017-9676-0
23. Mikropoulos TA, Natsis A. Educational virtual environments: A ten-year review of empirical research (1999-2009). Comput Educ (2011) 56:769–80. doi: 10.1016/j.compedu.2010.10.020
24. Schleider JL, Mullarkey MC, Weisz JR. Protocol for a three-arm randomized trial of virtual reality and web-based growth mindset interventions for adolescent depression (Preprint). JMIR Res Protoc (2019) 8(7):e13368. doi: 10.2196/13368
25. Ramnerö J, Folke F, Kanter JW. A learning theory account of depression. Scand J Psychol (2016) 57:73–82. doi: 10.1111/sjop.12233
26. Dimidjian S, Barrera M, Martell C, Muñoz RF, Lewinsohn PM. The origins and current status of behavioral activation treatments for depression. Annu Rev Clin Psychol (2011) 7:1–38. doi: 10.1146/annurev-clinpsy-032210-104535
27. Nyström MBT, Stenling A, Sjöström E, Neely G, Lindner P, Hassmén P, et al. Behavioral Activation versus Physical Activity via the Internet: A Randomized Controlled Trial. J Affect Disord (2017) 215:85–93. doi: 10.1016/j.jad.2017.03.018
28. Soucy I, Provencher M, Fortier M, McFadden T. Efficacy of guided self-help behavioural activation and physical activity for depression: a randomized controlled trial. Cogn Behav Ther (2017) 46:493–506. doi: 10.1080/16506073.2017.1337806
29. Lorenzo-Luaces L, German RE, DeRubeis RJ. It’s complicated: The relation between cognitive change procedures, cognitive change, and symptom change in cognitive therapy for depression. Clin Psychol Rev (2015) 41:3–15. doi: 10.1016/j.cpr.2014.12.003
30. Prudenzi A, Rooney B, Presti G, Lombardo M, Lombardo D, Messina C, et al. Testing the effectiveness of virtual reality as a defusion technique for coping with unwanted thoughts. Virtual Real (2019) 23:179–85. doi: 10.1007/s10055-018-0372-1
31. Wheatley J, Hackmann A. Using imagery rescripting to treat major depression: theory and practice. Cogn Behav Pract (2011) 18:444–53. doi: 10.1016/j.cbpra.2010.06.004
32. Wild J, Clark DM. Imagery rescripting of early traumatic memories in social phobia. Cogn Behav Pract (2011) 18:433–43. doi: 10.1016/j.cbpra.2011.03.002
33. Holmes EA, Blackwell SE, Burnett Heyes S, Renner F, Raes F. Mental imagery in depression: phenomenology, potential mechanisms, and treatment implications. Annu Rev Clin Psychol (2016) 12(1):249–80. doi: 10.1146/annurev-clinpsy-021815-092925
34. Mota NP, Schaumberg K, Vinci C, Sippel LM, Jackson M, Schumacher JA, et al. Imagery vividness ratings during exposure treatment for posttraumatic stress disorder as a predictor of treatment outcome. Behav Res Ther (2015) 69:22–8. doi: 10.1016/j.brat.2015.03.003
35. Cui X, Jeter CB, Yang D, Montague PR, Eagleman DM. Vividness of mental imagery: Individual variability can be measured objectively. Vision Res (2007) 47:474–8. doi: 10.1016/j.visres.2006.11.013
36. Reger GM, Koenen-Woods P, Zetocha K, Smolenski DJ, Holloway KM, Rothbaum BO, et al. Randomized controlled trial of prolonged exposure using imaginal exposure vs. virtual reality exposure in active duty soldiers with deployment-related posttraumatic stress disorder (PTSD). J Consult Clin Psychol (2016) 84:946–59. doi: 10.1037/ccp0000134
37. Guitard T, Bouchard S, Bélanger C, Berthiaume M. Exposure to a standardized catastrophic scenario in virtual reality or a personalized scenario in imagination for generalized anxiety disorder. J Clin Med (2019) 8:309. doi: 10.3390/jcm8030309
38. Kopelowicz A, Liberman RP, Zarate R. Recent advances in social skills training for schizophrenia. Schizophr Bull (2006) 32 Suppl 1:S12–23. doi: 10.1093/schbul/sbl023
39. Didehbani N, Allen T, Kandalaft M, Krawczyk D, Chapman S. Virtual reality social cognition training for children with high functioning autism. Comput Hum Behav (2016) 62:703–11. doi: 10.1016/j.chb.2016.04.033
40. Park K-M, Ku J, Choi S-H, Jang H-J, Park J-Y, Kim SI, et al. A virtual reality application in role-plays of social skills training for schizophrenia: a randomized, controlled trial. Psychiatry Res (2011) 189:166–72. doi: 10.1016/j.psychres.2011.04.003
41. Falconer CJ, Rovira A, King JA, Gilbert P, Antley A, Fearon P, et al. Embodying self-compassion within virtual reality and its effects on patients with depression. BJPsych Open (2016) 2:74–80. doi: 10.1192/bjpo.bp.115.002147
42. du Sert OP, Potvin S, Lipp O, Dellazizzo L, Laurelli M, Breton R, et al. Virtual reality therapy for refractory auditory verbal hallucinations in schizophrenia: a pilot clinical trial. Schizophr Res (2018) 197:176–81. doi: 10.1016/j.schres.2018.02.031
43. Craig TK, Rus-Calafell M, Ward T, Leff JP, Huckvale M, Howarth E, et al. AVATAR therapy for auditory verbal hallucinations in people with psychosis: a single-blind, randomised controlled trial. Lancet Psychiatry (2018) 5:31–40. doi: 10.1016/S2215-0366(17)30427-3
44. Craske MG, Meuret AE, Ritz T, Treanor M, Dour HJ. Treatment for anhedonia: a neuroscience driven approach. Depress Anxiety (2016) 33:927–38. doi: 10.1002/da.22490
45. Craske MG, Treanor M, Dour H, Meuret A, Ritz T. Positive Affect treatment for depression and anxiety: a randomized clinical trial for a core feature of anhedonia. J Consult Clin Psychol (2019) 87:457–71. doi: 10.1037/ccp0000396
46. Soga M, Gaston KJ, Yamaura Y. Gardening is beneficial for health: a meta-analysis. Prev Med Rep (2017) 5:92–9. doi: 10.1016/j.pmedr.2016.11.007
47. Kamioka H, Okada S, Tsutani K, Park H, Okuizumi H, Handa S, et al. Effectiveness of animal-assisted therapy: a systematic review of randomized controlled trials. Complement Ther Med (2014) 22:371–90. doi: 10.1016/j.ctim.2013.12.016
48. Lindner P, Miloff A, Hamilton W, Carlbring P. The potential of consumer-targeted virtual reality relaxation applications: descriptive usage, uptake and application performance statistics for a first-generation Application. Front Psychol (2019b) 10:1–6. doi: 10.3389/fpsyg.2019.00132
49. Huguet A, Rao S, McGrath PJ, Wozney L, Wheaton M, Conrod J, et al. A systematic review of cognitive behavioral therapy and behavioral activation apps for depression. PLoS One (2016) 11:e0154248. doi: 10.1371/journal.pone.0154248
50. Lindner P, Miloff A, Hamilton W, Reuterskiöld L, Andersson G, Powers MB, et al. Creating state of the art, next-generation Virtual Reality exposure therapies for anxiety disorders using consumer hardware platforms: design considerations and future directions. Cogn Behav Ther (2017) 46:404–20. doi: 10.1080/16506073.2017.1280843
Keywords: depression, virtual reality, cognitive behavior theory, human–computer interaction, self-help
Citation: Lindner P, Hamilton W, Miloff A and Carlbring P (2019) How to Treat Depression With Low-Intensity Virtual Reality Interventions: Perspectives on Translating Cognitive Behavioral Techniques Into the Virtual Reality Modality and How to Make Anti-Depressive Use of Virtual Reality–Unique Experiences. Front. Psychiatry 10:792. doi: 10.3389/fpsyt.2019.00792
Received: 05 July 2019; Accepted: 04 October 2019;
Published: 31 October 2019.
Edited by:
Annet Kleiboer, Vrije Universiteit Amsterdam, NetherlandsReviewed by:
Jude Uzoma Ohaeri, University of Nigeria, Nsukka, NigeriaJana Chihai, Nicolae Testemit¸anu State University of Medicine and Pharmacy, Moldova
Copyright © 2019 Lindner, Hamilton, Miloff and Carlbring. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Philip Lindner, philip.lindner@psychology.su.se
 Philip Lindner
Philip Lindner William Hamilton4
William Hamilton4 Alexander Miloff
Alexander Miloff Per Carlbring
Per Carlbring