- 1Department of Neurology and Neurosurgery, Montreal Neurological Institute, Montreal, QC, Canada
- 2Peer Support Centre, McGill University, Montreal, QC, Canada
- 3Department of Medicine, University of British Columbia, Vancouver, BC, Canada
Background: The coronavirus (COVID-19) pandemic has had a significant impact on society's overall mental health. Measures such as mandated lockdowns and physical distancing have contributed to higher levels of anxiety, depression, and other metrics indicating worsening mental health. Peer support, which is peer-to-peer provided social and emotional support, is an underutilized and effective mental health resource that can potentially be used to ameliorate mental health during these times.
Objective: This review aims to summarize the toll that this pandemic has had on society's mental health as found in peer-reviewed literature from October 2019 to March 2021, as well as suggest the utility of peer support to address these needs.
Methods: References for this review were chosen through searches of PubMed, Web of Science, and Google Scholar for articles published between October 2019 and March 2021 that used the terms: “coronavirus,” “COVID-19,” “mental health,” “anxiety,” “depression,” “isolation,” “mental health resources,” “peer support,” “online mental health resources,” and “healthcare workers.” Articles resulting from these searches and relevant references cited in those articles were reviewed. Articles published in English, French and Italian were included.
Results: This pandemic has ubiquitously worsened the mental health of populations across the world. Peer support has been demonstrated to yield generally positive effects on the mental health of a wide variety of recipients, and it can be provided through numerous accessible mediums.
Conclusions: Peer support can overall be beneficial for improving mental health during the COVID-19 pandemic and may be an effective tool should similar events arise in the future, although the presence of a few conflicting studies suggests the need for additional research.
Introduction
The COVID-19 pandemic has had a devastating impact on society, from the closure of businesses, disrupted services, and a mounting death toll of millions worldwide. Many individuals, even those who were not directly impacted by this virus, were placed into lockdowns instituted by their respective municipalities, states/provinces, and countries. This enforced isolation has resulted in greater rates of depression, anxiety, psychological distress, insomnia, denial, and anger around the world (1, 2). As the mandated isolations continue to become more frequent and longer in duration, the rates of depression, anxiety, and loneliness are only predicted to increase, especially among children, adolescents and young adults (18- to 24-year olds) (3).
Given that prolonged isolation can be quite harmful for individuals when left unaddressed, there needs to be a way to live with implemented public health measures while mitigating their negative effects on one's mental health. One could argue that individuals should be more proactive in consulting professional mental health services before their mental health declines significantly. However, only 36% of American university students who screened positive for major depression and 52% of students that screened positive for generalized anxiety disorder or panic disorder pursued professional mental health services, despite the sample having access to nearly universal health insurance and various free mental health resources (4–6). Furthermore, in Canada, it was found that individuals from ages 15 to 24 are the least likely age group to seek professional aid for their mental health, despite being the most affected by mental illness (7). Thus, the need for individuals to better support one another becomes apparent, much like first aid training among the general populous. A way to accomplish this would be through the provision of peer support from one individual to another, and unlike physical first aid, this does not require any official certification. Peer support is defined as the social and emotional support offered by an individual in equal standing, founded on respect, shared responsibility, and a mutual agreement of what is helpful (8). Due to it being an informal form of support that is widely accessible and effective, it led us to hypothesize that it would be a valuable tool in aiding the mental health of individuals who are negatively affected by the pandemic. This review discusses the mental health implications of the COVID-19 pandemic as found in peer-reviewed literature during October 2020–March 2021, and further, we suggest the usefulness of peer support as a form of mental health support during these trying times.
Methods
Database Search for Literature Review
Our protocol was drafted using the Preferred Reporting Items for Systematic Reviews and Meta-analysis Protocols (PRISMA-P). The following databases were searched: PubMed/MEDLINE (October 2020–April 2021), Web of Science (October 2020–April 2021) and Worldcat (October 2020–April 2021). We also searched for literature using the Google search engine and the first 20 results were reviewed as this search engine displays the results by relevance. Articles that were published and peer reviewed, as well as official documentation by the Mental Health Commission of Canada, were examined in this study. The reference lists of articles selected for full-text review were searched for additional articles. We also used Google Scholar to identify other published scholarly literature by performing a title and author searches. All publication/study types and languages were included in this search strategy. There were no limits placed and no restriction on the year of publication, with databases searched back to their inception. Search terms used in Google/online databases to find the article include: “coronavirus,” “COVID-19,” “mental health,” “anxiety,” “depression,” “isolation,” “mental health resources,” “peer support,” “online mental health resources,” and “healthcare workers.” Example of search query used in PubMed database: [(“coronavirus” OR “COVID-19”) AND (“mental health” OR “anxiety” OR “depression” OR “isolation”)].
The Prevalence of Poor Mental Health During the COVID-19 Pandemic
Worsening mental health has become an increasingly concerning issue in countries instituting measures such as mandated lockdowns. Recent survey studies done revealed that large proportions of the sampled population showed a higher prevalence of stress, anxiety, and depression as a result of lockdowns and physical distancing (9). For example, in Italy, the period of the first lockdown had significant detrimental effects on the mental health of its citizens (10). In fact, one survey administered in Italy revealed that the perceived levels of happiness and mental health decreased as a result of the lockdown, while their feelings of loneliness increased (11). Other studies have shown that the negative psychological effects experienced by adults also included confusion, anger, and distress (3). There are several stressors experienced during quarantine which can lead to these negative affective states such as the duration of quarantine, fears of infection, frustration, boredom, insufficient supplies, and inadequate information (12). Additionally, the constant fears of the unknown, stigma, and state of one's finances can continue to act as stressors post-quarantine (12).
Amongst children 11-years of age or younger, and youth 18- to 24-years of age, a significant portion reported experiencing increased loneliness during the pandemic due to lockdowns, social distancing, and school closures, with the latter age group being affected the most (3, 10). The loneliness was associated with depressive symptoms, social isolation, generalized anxiety, suicidal ideation, self-harm, and eating disorder behavior (3). One study which analyzed parent-reported levels of mental well-being of their children isolated in the context of various infections revealed increased levels of adjustment disorder, acute stress, grief, and post-traumatic stress disorder (PTSD). One reason for this could be the important role that peer groups and social identity plays in the development of young individuals (13, 14). This is an issue of great concern as politicians and policymakers in various countries determine the length of instituted lockdowns, school closures, and social distancing in the context of COVID-19.
The Impact of the Pandemic on the Mental Health of Healthcare Workers
One portion of the population that is severely impacted by this pandemic are the frontline medical workers. In fact, surveys done in China, Togo and India during this pandemic have shown that there is a higher prevalence of insomnia, anxiety, depression, somatization, and obsessive-compulsive symptoms in medical workers compared to non-medical workers (15–17). One study that interviewed hospital staff who were quarantined during the first SARS outbreak found that they were more likely to report feeling exhaustion, detachment from others, irritation, poor sleep, poor concentration, and ultimately a decline in their performance in the workplace (18). In fact, survey-based analysis done on healthcare workers during the initial COVID-19 outbreak in China revealed that 23.2% of them experienced anxiety, 22.8% showed prevalence of depression, and 38.9% experienced insomnia (19). Moreover, there were sex-specific differences with female healthcare workers experiencing more of the affective symptoms than their male counterparts (19).
These are extraordinarily difficult times for those working in the inpatient units, consul liaison services, emergency departments, as well as those having to widen their scope of practice in the presence of an overloaded healthcare system (20). This underscores the need for an accessible support system to aid those that directly provide care at the frontlines during the COVID-19 pandemic. To address this decline in healthcare worker mental health, it has been suggested that there be increased provisions of mental health support which will result in greater self-efficacy and confidence (21). Additionally, the use of technology to deliver psychosocial supports while preserving social distancing would be greatly beneficial (21).
The Lack of Accessible and Effective Mental Health Resources During the COVID-19 Pandemic
Social distancing and lockdown measures have forced many individuals to stay inside, leaving them unable to access traditional mental health services. Moreover, many support services are not able to effectively transition to an online delivery model in an accessible manner. To address the issue of dwindling mental health, many governments are making the effort to advertise resources such as telephone helplines, videos, and readable material (22, 23). Though they can serve to inform, they are often inadequate in meeting the increased need of mental health resources caused by the COVID-19 pandemic (24).
Many digital interventions currently exist to address social isolation and loneliness in young people. Computerized cognitive-behavioral therapies such as BRAVE-TA, MoodGym, SPARX, and “Think, Feel, Do” have small, but positive impacts on mental health (25–27). Additionally, self-help interventions such as bibliotherapy and computerized therapy have shown to have a somewhat positive effect on mental health but are agreed to generally be less effective than face to face therapies (28–30). Unfortunately, even though mobile apps are a very accessible and easy-to-use medium of obtaining information and accessing resources, there is a lack of evidence supporting their effectiveness in improving mental health (25, 31, 32).
Fortunately, for healthcare workers, an evidence-based community forum known as Schwartz Rounds allows medical staff from all backgrounds to discuss their emotions regarding work-related matters (33). Moreover, those who used this online forum reported feeling acknowledged and validated (33). Nonetheless, staff are still encouraged to use institutional peer support programs as a single forum-based resource may not be sufficient (34).
In order to make mental health resources more accessible, platforms such as WeChat, Weibo, and WhatsApp are being used in many countries to better connect individuals with psychological counseling services (23, 35). Yet, the risk of increasing suicide mortality amongst regular citizens and health care workers is of great concern given the present economic stress, social isolation, decreased access to community and religious support, and barriers to mental health treatment and illness (36). Hence, it has been suggested that having a telephone support line that is staffed by nurses and/or counselors would be beneficial for individuals in quarantine (37).
Community is sought during times of strife and the differences in access to adequate mental health support across different socioeconomic groups makes it challenging to find a reliable resource (20). This suggests the need for an accessible form of support that can remove barriers between a struggling individual and a supporter. There is currently evidence for the utility of telepsychiatry in aiding the mental health of growing adults and adolescents (38). However, the limitations of this approach include the need for trained psychiatric counselors, as well as the stigma associated with seeking professional help (39).
Peer Support as a Viable Mental Health Resource
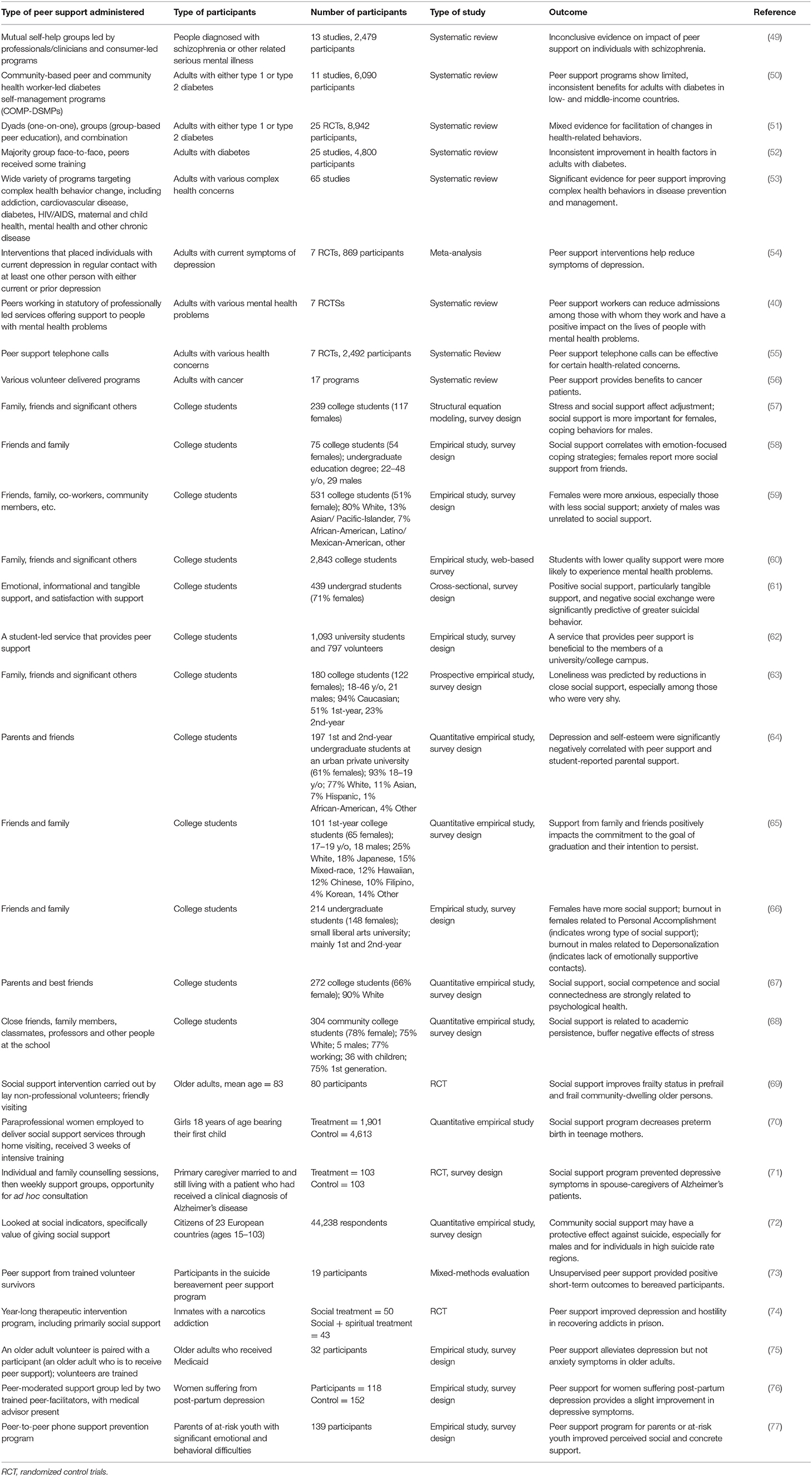
Peer support as a mental health resource has grown exponentially in the last few decades around the world, namely North America and Europe (40). In the US alone, Goldstrom et al. has reported that services run by, and delivered to, people with mental health issues more than double traditional, professional mental health organizations (41). This growth is supported by numerous studies that illustrate the safety and efficacy of peer support which include its ability to improve empowerment, hope, quality of life, self-esteem, social functioning, and care engagement for those accessing its services (40, 42–45). Furthermore, two comprehensive systematic reviews have shown that not only are peer supporters able to achieve similar outcomes to mental health professionals, but that peer supporters reduced inpatient service use and improved relationships with providers, care engagement, and various recovery-related outcomes in people struggling with severe mental illness when compared to professionals (46, 47). On the other hand, one of the systematic reviews did identify a study that found that the presence of a peer increased the number of psychiatric hospitalization days (46). They postulate this could be because the peer heightened the awareness of the clients' suffering and accordingly advocated for interventions leading to additional hospitalizations (48). In the other studies with the positive results, however, the recipients may have felt that the peer support provided was sufficient and that further help in the form of professional services was not required. Overall, there are many peer support services and organizations that are used to aid the mental health of patients with various mental and physical ailments, but the general consensus toward peer support is that it is either inconclusive or yields positive effects (Table 1). Notably, the presence of conflicting results reiterates the need for further research to better characterize the impact of peer support.
Looking specifically at educational institutions, peer support has been shown to improve self-esteem, anxiety, depression, stress, burnout, loneliness, and overall mental well-being, although the literature here is limited (Table 1) (78–81). Interestingly, one of these studies determined that structured peer support is unlikely to have a significant effect on improving early and preventative intervention (79). Although they expected peer support to facilitate early intervention for students reluctant to access professional services, they found that many of the students attending peer support groups had already sought professional support and had been experiencing mental health difficulties for over a year. Therefore, they argue that integrating peer support into professional-led services may maximize outcomes as opposed to pursuing one intervention over the other (79).
However, peer support can pose a few challenges. Previous studies have demonstrated concerns regarding boundaries and power dynamics but also the stress, accountability, and risk assessment peer supporters are faced with in their roles, and so it is imperative that they prioritize their own mental health as well (40, 82–85). One systematic review has found that there was little to no evidence that peer support impacted hospitalization or overall symptoms, and that the positive effects reported on hope, recovery, and empowerment were present but inconsistent (86). Altogether, they state that current evidence is promising but does not support the requirement of mental health services to provide peer support programmes (86). One reason for this could potentially be because peer support is a relatively new phenomenon in the mental health landscape, that is only recently getting traction for being a viable mental health resource. Therefore, additional research studies and clinical trials are required to better understand the role of complex interventions such as peer support.
Strategies for Obtaining and Providing Peer Support in the Context of the COVID-19 Pandemic
Another strength of peer support is its flexibility. Peer support can be provided in various settings through several different mediums as illustrated in Table 1. The first distinction is whether the peer support is provided in a group or an individual setting. Group peer support typically functions with a peer support facilitator and then multiple service users who each share and discuss their experiences with the group. Perhaps the best and oldest example of group peer support, and peer support in general, is Alcoholics Anonymous (AA) (87). AA is an established and heavily researched peer support delivery method with a recent review indicating social support variables such as shared experiences as being a key factor to its effectiveness (87). Group peer support methods have now been successfully deployed in various settings, ranging from mental health focused groups such as the Wellness Recovery Action Plan (WRAP) (88) and Building Recovery of Individual Dreams and Goals through Education and Support (BRIDGES) (89) programmes to supporting HIV-infected adolescents (90) and improving quality of life in breast cancer patients (91).
Individual peer support, on the other hand, is typically a one-on-one delivery with a single supporter and service user (88–91). These interactions have been shown to provide beneficial practical, emotional, and social supports in a non-treatment based, normalizing relationship but are highly understudied and lack evidence regarding the necessary duration, frequency, quality, or intensity to maximize its effectiveness (92). For these reasons, peer support has been acknowledged as a resource that should complement rather than replace professional mental health resources at this time, suggesting the fact that a blended approach may work synergistically to maximize mental health outcomes (79). The benefit of professional mental health services is not to be understated as they indeed have been proven to be very useful for aiding one's mental health, however, numerous barriers can still prevent individuals from obtaining the help they need (93–95). Therefore, alternative sources of support need to be explored, and notably, individual peer support is becoming an extremely common delivery method that continues to grow in popularity (40, 41).
With the arrival of the COVID-19 pandemic and the swift transition of many services to online platforms, virtual peer support services have quickly come to the forefront of novel mental health support delivery methods. By removing traditional barriers to peer support programs such as accessibility and availability, virtual peer support may be a very promising alternative to in-person peer support via utilization of video conferencing software such as Zoom, Google Meets, and Cisco Webex. A 2019 article by Fortuna et al. summarizes the diverse technology modalities that digital peer support can be delivered through, which includes “peer-delivered and smartphone-supported interventions, peer-supported asynchronous technology, artificial peer support, informal peer-to-peer support via social media, video games, and virtual worlds” (96). Unfortunately, research on virtual peer support is limited with various systematic reviews identifying an overall lack of high-quality studies in online peer support, mainly because many of these interventions are used adjunctively and therefore the individual effect of online peer support cannot be clearly demonstrated (97–100). Nonetheless, the findings they do note are promising and could be the next frontier of peer support and mental health care in the future (97–100).
Collectively, through reviewing peer-reviewed studies, we identified the following steps as being effective ways to provide peer support during the COVID-19 pandemic:
In person (for the people within your social-distancing bubble):
1. Find a comfortable and welcoming room/space with minimal interruptions.
2. Reassure the person you will be confidential, non-judgemental, and non-directional toward anything that they will say.
3. Actively listen using minimal encouragers and appropriate body language. Additionally, validate and normalize the individual's thoughts, feelings, and experiences. Note: the supporter should try and maintain a balance between listening 80% of the time and talking 20% of the time.
• Some example phrases/sentence starters to use:
○ “From what I am hearing, it sounds like…”
○ “It is understandable why someone in your position would feel like that.”
○ “Thank you for opening up to me, it takes a lot of courage to share something so personal.”
○ “Your experience is unique, but anyone in a similar position would feel that way.”
4. Paraphrase and summarize the key points of what they are sharing with you. Ask for clarification and allow them to correct you as necessary.
5. Ask open-ended question to encourage conversation and keep it flowing organically.
• Some example open-ended questions to ask:
○ “How did you feel before that happened? How did you feel after?”
○ “How has this affected your sleep, eating habits, etc.”
○ “What do you like to do for self-care?”
○ “How can I offer you support? Please tell me what that looks like to you.”
6. If the individual is seeking advice or counsel, you may brainstorm potential ideas with them non-directionally, but have them lead the discussion.
• This can be done through redirection:
○ “I do not know your experience as well as you do. What do you feel you should do? Why?”
○ “Before I share any of my thoughts, I would love to hear a bit more about what things you have already considered.”
Virtually (for the people outside of your bubble):
1. Find a comfortable room or space with an appropriate/welcoming background and minimal noise.
• Note: using earphones is highly encouraged if there are other people passing by in that area.
2. Open a video conferencing software such as Google Meets, Zoom, WebEx, etc. on a computer or mobile device and send the individual the meeting link.
3. Allow them to keep the video on/off depending on what they prefer and assure them that they are free to leave the call at any time.
4. Reassure the person that you will be confidential, non-judgemental, and non-directional toward anything that they will say.
5. Actively listen using minimal encouragers and appropriate body language. Additionally, validate and normalize the individual's thoughts, feelings, and experiences. Note: the supporter should try and maintain a balance between listening 80% of the time and talking 20% of the time.
• Some example phrases/sentence starters to use:
○ “From what I am hearing, it sounds like…”
○ “It is understandable why someone in your position would feel like that.”
○ “Thank you for opening up to me, it takes a lot of courage to share something so personal.”
○ “Your experience is unique, but anyone in a similar position would feel the same way.”
○ “You're not alone.”
6. Paraphrase and summarize the key points of what they are sharing with you. Ask for clarification and allow them to correct you as necessary.
7. Ask open-ended question to encourage conversation and keep it flowing organically.
• Some example open-ended questions to ask:
○ “How did you feel before that happened? How did you feel after?”
○ “How has this affected your sleep, eating habits, etc.”
○ “What do you like to do for self-care?”
○ “How can I offer you support? Please tell me what that looks like to you.”
8. If the individual is seeking advice or counsel, you may brainstorm potential ideas with them non-directionally, but have them lead the discussion.
• This can be done through redirection:
○ “I do not know your experience as well as you do. What do you feel you should do? Why?”
○ “Before I share any of my thoughts, I would love to hear a bit more about what things you have already considered.”
- Troubleshooting tips for virtual peer support:
• If the video call lags, be honest about it and ask them to repeat what they had said.
• If the call ends unexpectedly, send them another meeting link and continue from where you left-off.
• If the call is lagging excessively, turning off the video may reduce the lag.
Concluding Remarks
The COVID-19 pandemic has had devastating effects on communities all around the world. Notably, its impact on the mental health of individuals by way of instituted lockdowns and social distancing/isolation measures remains to be sufficiently addressed. Although professional mental health services have begun transitioning to online delivery models, this adaptation has not been sufficient to meet the growing need of mental health support. That being said, there still remains viable options for those in need. Peer support, although not a psychiatric or professional service, can be generally beneficial in improving mental health. This review identifies numerous studies illustrating the positive impacts of peer support, but the presence of studies demonstrating its lack of utility should not be ignored. It should be noted that the vast majority of the peer support studies discussed here have not identified any clear adverse outcomes on recipients' mental health and so, it appears that peer support can actually be a quite safe and beneficial resource. More research is necessary, but for the time being, utilizing peer support as a complementary resource to professional services may maximize positive outcomes. During the pandemic, however, peer support stands out as a resource that can be easily provided by members of the community to one another through accessible online mediums, even during times of quarantine and lockdown. As this pandemic draws on for extended periods of time, mental health can deteriorate. However, members of the community can help one another through the provision of peer support to ensure that all members of society are able to endure these trying times.
Author Contributions
RS: conception of review topic, writing of review, table analyzing peer-reviewed literature on peer support, and editing of manuscript. AA: writing of review and editing of manuscript. ZK: table analyzing peer-reviewed literature on peer support. All authors contributed to the article and approved the submitted version.
Funding
The costs associated with publishing were kindly funded by McGill's Peer Support Centre and the Students' Society of McGill University.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
COVID-19, coronavirus-19; PTSD, post-traumatic stress disorder; RCT, randomized controlled trial.
References
1. Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. (2020) 89:531–42. doi: 10.1016/j.bbi.2020.05.048
2. Torales J, O'Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. (2020) 66:317–20. doi: 10.1177/0020764020915212
3. Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. (2020) 59:1218–39.e3. doi: 10.1016/j.jaac.2020.05.009
4. Eisenberg D, Golberstein E, Gollust SE. Help-seeking and access to mental health care in a university student population. Med Care. (2007) 45:594–601. doi: 10.1097/MLR.0b013e31803bb4c1
5. Eisenberg D, Hunt J, Speer N, Zivin K. Mental health service utilization among college students in the United States. J Nerv Ment Dis. (2011) 199:301–8. doi: 10.1097/NMD.0b013e3182175123
6. Pelletier L, O'Donnell S, Dykxhoorn J, McRae L, Patten SB. Under-diagnosis of mood disorders in Canada. Epidemiol Psychiatr Sci. (2017) 26:414–23. doi: 10.1017/S2045796016000329
7. Cyr C. Making the Case for Peer Support: Report to the Peer Support Project Committee of the Mental Health Commission of Canada. The Mental Health Commission of Canada (2016). Available online at: https://www.mentalhealthcommission.ca/English/document/445/making-case-peer-support (accessed May 5, 2021).
8. Solomon P. Peer support/peer provided services underlying processes, benefits, and critical ingredients. Psychiatr Rehabil J. (2004) 27:392–401. doi: 10.2975/27.2004.392.401
9. Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. (2020) 16:57. doi: 10.1186/s12992-020-00589-w
10. Coppola I, Rania N, Parisi R, Lagomarsino F. Spiritual well-being and mental health during the COVID-19 pandemic in Italy. Front Psychiatry. (2021) 12:626944. doi: 10.3389/fpsyt.2021.626944
11. Rania N, Coppola I. Psychological impact of the lockdown in italy due to the COVID-19 outbreak: are there gender differences? Front Psychol. (2021) 12:567470. doi: 10.3389/fpsyg.2021.567470
12. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
13. Brown BB, Eicher SA, Petrie S. The importance of peer group (“crowd”) affiliation in adolescence. J Adolesc. (1986) 9:73–96. doi: 10.1016/S0140-1971(86)80029-X
14. Meeus W, Dekoviic M. Identity development, parental and peer support in adolescence: results of a national Dutch survey. Adolescence. (1995) 30:931–44.
15. Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. (2020) 89:242–50. doi: 10.1159/000507639
16. Kounou KB, Guedenon KM, Dogbe Foli AA, Gnassounou-Akpa E. Mental health of medical professionals during the COVID-19 pandemic in Togo. Psychiatry Clin Neurosci. (2020) 74:559–60. doi: 10.1111/pcn.13108
17. Rehman U, Shahnawaz MG, Khan NH, Kharshiing KD, Khursheed M, Gupta K, et al. Depression, anxiety and stress among Indians in times of covid-19 lockdown. Community Ment Health J. (2020) 57:1–7. doi: 10.1007/s10597-020-00664-x
18. Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. (2009) 54:302–11. doi: 10.1177/070674370905400504
19. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
20. Freeman MP. COVID-19 from a psychiatry perspective: meeting the challenges. J Clin Psychiatry. (2020) 81:20ed13358. doi: 10.4088/JCP.20ed13358
21. Wu PE, Styra R, Gold WL. Mitigating the psychological effects of COVID-19 on health care workers. CMAJ. (2020) 192:E459–60. doi: 10.1503/cmaj.200519
22. Hiremath P, Suhas Kowshik CS, Manjunath M, Shettar M. COVID 19: impact of lock-down on mental health and tips to overcome. Asian J Psychiatr. (2020) 51:102088. doi: 10.1016/j.ajp.2020.102088
23. Ifdil I, Fadli RP, Suranata K, Zola N, Ardi Z. Online mental health services in Indonesia during the COVID-19 outbreak. Asian J Psychiatr. (2020) 51:102153. doi: 10.1016/j.ajp.2020.102153
24. Hu N, Pan S, Sun J, Wang Z, Mao H. Mental health treatment online during the COVID-19 outbreak. Eur Arch Psychiatry Clin Neurosci. (2020) 270:783–4. doi: 10.1007/s00406-020-01129-8
25. Grist R, Croker A, Denne M, Stallard P. Technology delivered interventions for depression and anxiety in children and adolescents: a systematic review and meta-analysis. Clin Child Fam Psychol Rev. (2019) 22:147–71. doi: 10.1007/s10567-018-0271-8
26. Moor S, Williman J, Drummond S, Fulton C, Mayes W, Ward N, et al. ‘E' therapy in the community: examination of the uptake and effectiveness of BRAVE (a self-help computer programme for anxiety in children and adolescents) in primary care. Internet Interv. (2019) 18:100249. doi: 10.1016/j.invent.2019.100249
27. Pennant ME, Loucas CE, Whittington C, Creswell C, Fonagy P, Fuggle P, et al. Computerised therapies for anxiety and depression in children and young people: a systematic review and meta-analysis. Behav Res Ther. (2015) 67:1–18. doi: 10.1016/j.brat.2015.01.009
28. Bennett SD, Cuijpers P, Ebert DD, McKenzie Smith M, Coughtrey AE, Heyman I, et al. Practitioner review: unguided and guided self-help interventions for common mental health disorders in children and adolescents: a systematic review and meta-analysis. J Child Psychol Psychiatry. (2019) 60:828–47. doi: 10.1111/jcpp.13010
29. Creswell C, Violato M, Fairbanks H, White E, Parkinson M, Abitabile G, et al. Clinical outcomes and cost-effectiveness of brief guided parent-delivered cognitive behavioural therapy and solution-focused brief therapy for treatment of childhood anxiety disorders: a randomised controlled trial. Lancet Psychiatry. (2017) 4:529–39. doi: 10.1016/S2215-0366(17)30149-9
30. Lillevoll KR, Vangberg HC, Griffiths KM, Waterloo K, Eisemann MR. Uptake and adherence of a self-directed internet-based mental health intervention with tailored e-mail reminders in senior high schools in Norway. BMC Psychiatry. (2014) 14:14. doi: 10.1186/1471-244X-14-14
31. Grist R, Porter J, Stallard P. Mental health mobile apps for preadolescents and adolescents: a systematic review. J Med Internet Res. (2017) 19:e176. doi: 10.2196/jmir.7332
32. Richardson CG, Slemon A, Gadermann A, McAuliffe C, Thomson K, Daly Z, et al. Use of asynchronous virtual mental health resources for COVID-19 pandemic-related stress among the general population in canada: cross-sectional survey study. J Med Internet Res. (2020) 22:e24868. doi: 10.2196/24868
33. Balasubramanian A, Paleri V, Bennett R, Paleri V. Impact of COVID-19 on the mental health of surgeons and coping strategies. Head Neck. (2020) 42:1638–44. doi: 10.1002/hed.26291
34. Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. (2020) 368:m1211. doi: 10.1136/bmj.m1211
35. Liu S, Yang L, Zhang C, Xiang YT, Liu Z, Hu S, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:e17–e8. doi: 10.1016/S2215-0366(20)30077-8
36. Reger MA, Stanley IH, Joiner TE. Suicide mortality and coronavirus disease 2019-a perfect storm? JAMA Psychiatry. (2020) 77:1093–4. doi: 10.1001/jamapsychiatry.2020.1060
37. Courtet P, Olié E, Debien C, Vaiva G. Keep socially (but not physically) connected and carry on: preventing suicide in the age of COVID-19. J Clin Psychiatry. (2020) 81:20com13370. doi: 10.4088/JCP.20com13370
38. Prisco V, Prisco L, Donnarumma B. Telepsychiatry in adults and adolescents: a useful tool against CoViD-19. Recenti Prog Med. (2020) 111:411–4. doi: 10.1701/3407.33923
39. Bar-Levav R. The stigma of seeing a psychiatrist. Am J Psychother. (1976) 30:473–82. doi: 10.1176/appi.psychotherapy.1976.30.3.473
40. Repper J, Carter T. A review of the literature on peer support in mental health services. J Ment Health. (2011) 20:392–411. doi: 10.3109/09638237.2011.583947
41. Goldstrom ID, Campbell J, Rogers JA, Lambert DB, Blacklow B, Henderson MJ, et al. National estimates for mental health mutual support groups, self-help organizations, and consumer-operated services. Adm Policy Ment Health. (2006) 33:92–103. doi: 10.1007/s10488-005-0019-x
42. Davidson L, Chinman M, Sells D, Rowe M. Peer support among adults with serious mental illness: a report from the field. Schizophr Bull. (2006) 32:443–50. doi: 10.1093/schbul/sbj043
43. Ochocka J, Nelson G, Janzen R, Trainor J. A longitudinal study of mental health consumer/survivor initiatives: Part 3-A qualitative study of impacts of participation on new members. J Community Psychol. (2006) 34:273–83. doi: 10.1002/jcop.20099
44. Puschner B, Repper J, Mahlke C, Nixdorf R, Basangwa D, Nakku J, et al. Using peer support in developing empowering mental health services (UPSIDES): background, rationale and methodology. Ann Glob Health. (2019) 85:53. doi: 10.5334/aogh.2435
45. Resnick SG, Rosenheck RA. Integrating peer-provided services: a quasi-experimental study of recovery orientation, confidence, and empowerment. Psychiatr Serv. (2008) 59:1307–14. doi: 10.1176/ps.2008.59.11.1307
46. Chinman M, George P, Dougherty RH, Daniels AS, Ghose SS, Swift A, et al. Peer support services for individuals with serious mental illnesses: assessing the evidence. Psychiatr Serv. (2014) 65:429–41. doi: 10.1176/appi.ps.201300244
47. Pitt V, Lowe D, Hill S, Prictor M, Hetrick SE, Ryan R, et al. Consumer-providers of care for adult clients of statutory mental health services. Cochrane Database Syst Rev. (2013) 3:CD004807. doi: 10.1002/14651858.CD004807.pub2
48. van Vugt MD, Kroon H, Delespaul PA, Mulder CL. Consumer-providers in assertive community treatment programs: associations with client outcomes. Psychiatr Serv. (2012) 63:477–81. doi: 10.1176/appi.ps.201000549
49. Chien WT, Clifton AV, Zhao S, Lui S. Peer support for people with schizophrenia or other serious mental illness. Cochrane Database Syst Rev. (2019) 4:CD010880. doi: 10.1002/14651858.CD010880.pub2
50. Werfalli M, Raubenheimer PJ, Engel M, Musekiwa A, Bobrow K, Peer N, et al. The effectiveness of peer and community health worker-led self-management support programs for improving diabetes health-related outcomes in adults in low- and-middle-income countries: a systematic review. Syst Rev. (2020) 9:133. doi: 10.1186/s13643-020-01377-8
51. Webel AR, Okonsky J, Trompeta J, Holzemer WL. A systematic review of the effectiveness of peer-based interventions on health-related behaviors in adults. [1541-0048 (Electronic)].
52. Dale JR, Williams S, Bowyer V. What is the effect of peer support on diabetes outcomes in adults? A systematic review. Diabet Med. (2012) 29:1361–77. doi: 10.1111/j.1464-5491.2012.03749.x
53. Fisher EB, Boothroyd RI, Elstad EA, Hays L, Henes A, Maslow GR, et al. Peer support of complex health behaviors in prevention and disease management with special reference to diabetes: systematic reviews. Clin Diabetes Endocrinol. (2017) 3:4. doi: 10.1186/s40842-017-0042-3
54. Pfeiffer PN, Heisler M, Piette JD, Rogers MAM, Valenstein M. Efficacy of peer support interventions for depression: a meta-analysis. Gen Hosp Psychiatry. (2011) 33:29–36. doi: 10.1016/j.genhosppsych.2010.10.002
55. Dale J, Caramlau I, Lindenmeyer A, Williams SM. Peer support telephone calls for improving health. Cochrane Database Syst Rev. (2008) 2008:CD006903. doi: 10.1002/14651858.CD006903.pub2
56. Campbell HS, Phaneuf M, Deane K. Cancer peer support programs-do they work?. Patient Educ Couns. (2004) 55:3–15. doi: 10.1016/j.pec.2003.10.001
57. Asberg KK, Bowers C, Renk K, McKinney C. A structural equation modeling approach to the study of stress and psychological adjustment in emerging adults. Child Psychiatry Hum Dev. (2008) 39:481–501. doi: 10.1007/s10578-008-0102-0
58. Dwyer AL, Cummings AL. Stress, self-efficacy, social support, and coping strategies in university students. Can J Counsel Psychother. (2001) 35:208–18. Available online at: https://cjc-rcc.ucalgary.ca/article/view/58672
59. Hawkins MJ. Anxiety in relation to social support in a college population. J Coll Stud Psychother. (1995) 9:79–88. doi: 10.1300/J035v09n04_07
60. Hefner J, Eisenberg D. Social support and mental health among college students. Am J Orthopsychiatry. (2009) 79:491–9. doi: 10.1037/a0016918
61. Hirsch JK, Barton AL. Positive social support, negative social exchanges, and suicidal behavior in college students. J Am College Health. (2011) 59:393–8. doi: 10.1080/07448481.2010.515635
62. Suresh R, Karkossa Z, Richard J, Karia M. Program evaluation of a student-led peer support service at a Canadian university. Int J Mental Health Syst. (2021) 15:1–11. doi: 10.1186/s13033-021-00479-7
63. Jackson T, Soderlind A, Weiss KE. Personality traits and quality of relationships as predictors of future loneliness among American college students. Soc Behav Pers Int J. (2000) 28:463–70. doi: 10.2224/sbp.2000.28.5.463
64. Li ST, Albert AB, Dwelle DG. Parental and peer support as predictors of depression and self-esteem among college students. J Coll Stud Dev. (2014) 55:120–38. doi: 10.1353/csd.2014.0015
65. Strom RE, Savage MW. Assessing the relationships between perceived support from close others, goal commitment, and persistence decisions at the college level. J Coll Stud Dev. (2014) 55:531–47. doi: 10.1353/csd.2014.0064
66. Weckwerth AC, Flynn DM. Effect of sex on perceived support and burnout in university students. Coll Stud J. (2006) 40:237.
67. Williams KL, Galliher RV. Predicting depression and self-esteem from social connectedness, support, and competence. J Soc Clin Psychol. (2006) 25:855–74. doi: 10.1521/jscp.2006.25.8.855
68. Zavatkay D. Social Support and Community College Student Academic Persistence. Storrs: University of Connecticut Library (2015).
69. Luger E, Dorner TE, Haider S, Kapan A, Lackinger C, Schindler K. Effects of a home-based and volunteer-administered physical training, nutritional, and social support program on malnutrition and frailty in older persons: a randomized controlled trial. J Am Med Directors Assoc. (2016) 17:671.e9-e16. doi: 10.1016/j.jamda.2016.04.018
70. Rogers MM, Peoples-Sheps MD, Suchindran C. Impact of a social support program on teenage prenatal care use and pregnancy outcomes. J Adolesc Health. (1996) 19:132–40. doi: 10.1016/1054-139X(95)00227-J
71. Mittelman MS, Ferris SH, Shulman E, Steinberg G, Ambinder A, Mackell JA, et al. A comprehensive support program: effect on depression in spouse-caregivers of AD patients. Gerontologist. (1995) 35:792–802. doi: 10.1093/geront/35.6.792
72. Šedivy NZ, Podlogar T, Kerr DC, De Leo D. Community social support as a protective factor against suicide: a gender-specific ecological study of 75 regions of 23 European countries. Health Place. (2017) 48:40–6. doi: 10.1016/j.healthplace.2017.09.004
73. Barlow CA, Waegemakers Schiff J, Chugh U, Rawlinson D, Hides E, Leith J. An evaluation of a suicide bereavement peer support program. Death Stud. (2010) 34:915–30. doi: 10.1080/07481181003761435
74. Chen G. Social support, spiritual program, and addiction recovery. Int J Offen Ther Comp Criminol. (2006) 50:306–23. doi: 10.1177/0306624X05279038
75. Chapin RK, Sergeant JF, Landry S, Leedahl SN, Rachlin R, Koenig T, et al. Reclaiming joy: pilot evaluation of a mental health peer support program for older adults who receive Medicaid. Gerontologist. (2013) 53:345–52. doi: 10.1093/geront/gns120
76. Prevatt B-S, Lowder EM, Desmarais SL. Peer-support intervention for postpartum depression: participant satisfaction and program effectiveness. Midwifery. (2018) 64:38–47. doi: 10.1016/j.midw.2018.05.009
77. January S-AA, Hurley KD, Stevens AL, Kutash K, Duchnowski AJ, Pereda N. Evaluation of a community-based peer-to-peer support program for parents of at-risk youth with emotional and behavioral difficulties. J Child Fam Stud. (2016) 25:836–44. doi: 10.1007/s10826-015-0271-y
78. Aladag M, Tezer E. Effects of a peer helping training program on helping skills and self-growth of peer helpers. Int J Adv Counsel. (2009) 31:255. doi: 10.1007/s10447-009-9082-4
79. Byrom N. An evaluation of a peer support intervention for student mental health. J Ment Health. (2018) 27:240–6. doi: 10.1080/09638237.2018.1437605
80. Larsen TB, Urke H, Tobro M, Årdal E, Waldahl RH, Djupedal I, et al. Promoting mental health and preventing loneliness in upper secondary school in norway: effects of a randomized controlled trial. Scand J Educ Res. (2019) 65:1–14. doi: 10.1080/00313831.2019.1659405
81. Sprang G, Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med Public Health Prep. (2013) 7:105–10. doi: 10.1017/dmp.2013.22
82. Chinman M, Young AS, Hassell J, Davidson L. Toward the implementation of mental health consumer provider services. J Behav Health Serv Res. (2006) 33:176–95. doi: 10.1007/s11414-006-9009-3
83. Coleman R, Campbell J. Roads to recovery Peer Development Project: the First Year. Ongoing Evaluation of the Developmental Process. Perth: Working to Recovery Publications (2009).
84. Mead S, Hilton D, Curtis L. Peer support: a theoretical perspective. Psychiatr Rehabil J. (2001) 25:134–41. doi: 10.1037/h0095032
85. Mowbray CT, Moxley DP, Collins ME. Consumers as mental health providers: first-person accounts of benefits and limitations. J Behav Health Serv Res. (1998) 25:397–411. doi: 10.1007/BF02287510
86. Lloyd-Evans B, Mayo-Wilson E, Harrison B, Istead H, Brown E, Pilling S, et al. A systematic review and meta-analysis of randomised controlled trials of peer support for people with severe mental illness. BMC Psychiatry. (2014) 14:39. doi: 10.1186/1471-244X-14-39
87. Groh DR, Jason LA, Keys CB. Social network variables in alcoholics anonymous: a literature review. Clin Psychol Rev. (2008) 28:430–50. doi: 10.1016/j.cpr.2007.07.014
88. Cook JA, Copeland ME, Jonikas JA, Hamilton MM, Razzano LA, Grey DD, et al. Results of a randomized controlled trial of mental illness self-management using wellness recovery action planning. Schizophr Bull. (2012) 38:881–91. doi: 10.1093/schbul/sbr012
89. Cook JA, Steigman P, Pickett S, Diehl S, Fox A, Shipley P, et al. Randomized controlled trial of peer-led recovery education using building recovery of individual dreams and goals through education and support (BRIDGES). Schizophr Res. (2012) 136:36–42. doi: 10.1016/j.schres.2011.10.016
90. Funck-Brentano I, Dalban C, Veber F, Quartier P, Hefez S, Costagliola D, et al. Evaluation of a peer support group therapy for HIV-infected adolescents. AIDS. (2005) 19:1501–8. doi: 10.1097/01.aids.0000183124.86335.0a
91. Tehrani AM, Farajzadegan Z, Rajabi FM, Zamani AR. Belonging to a peer support group enhance the quality of life and adherence rate in patients affected by breast cancer: a non-randomized controlled clinical trial. J Res Med Sci. (2011) 16:658–65.
92. Gidugu V, Rogers ES, Harrington S, Maru M, Johnson G, Cohee J, et al. Individual peer support: a qualitative study of mechanisms of its effectiveness. Community Ment Health J. (2015) 51:445–52. doi: 10.1007/s10597-014-9801-0
93. Aguirre Velasco A, Cruz ISS, Billings J, Jimenez M, Rowe S. What are the barriers, facilitators and interventions targeting help-seeking behaviours for common mental health problems in adolescents? A systematic review. BMC Psychiatry. (2020) 20:293. doi: 10.1186/s12888-020-02659-0
94. Shi W, Shen Z, Wang S, Hall BJ. Barriers to professional mental health help-seeking among chinese adults: a systematic review. Front Psychiatry. (2020) 11:442. doi: 10.3389/fpsyt.2020.00442
95. Vidourek RA, King KA, Nabors LA, Merianos AL. Students' benefits and barriers to mental health help-seeking. Health Psychol Behav Med. (2014) 2:1009–22. doi: 10.1080/21642850.2014.963586
96. Fortuna KL, Venegas M, Umucu E, Mois G, Walker R, Brooks JM. The future of peer support in digital psychiatry: promise, progress, and opportunities. Curr Treat Options Psychiatry. (2019) 6:221–31. doi: 10.1007/s40501-019-00179-7
97. Ali K, Farrer L, Gulliver A, Griffiths KM. Online peer-to-peer support for young people with mental health problems: a systematic review. JMIR Ment Health. (2015) 2:e19. doi: 10.2196/mental.4418
98. Eysenbach G, Powell J, Englesakis M, Rizo C, Stern A. Health related virtual communities and electronic support groups: systematic review of the effects of online peer to peer interactions. BMJ. (2004) 328:1166. doi: 10.1136/bmj.328.7449.1166
99. McColl LD, Rideout PE, Parmar TN, Abba-Aji A. Peer support intervention through mobile application: an integrative literature review and future directions. Can Psychol/Psychol canadienne. (2014) 55:250. doi: 10.1037/a0038095
Keywords: COVID-19, coronavirus pandemic, mental health, peer support, healthcare workers, isolation, lockdown, distress
Citation: Suresh R, Alam A and Karkossa Z (2021) Using Peer Support to Strengthen Mental Health During the COVID-19 Pandemic: A Review. Front. Psychiatry 12:714181. doi: 10.3389/fpsyt.2021.714181
Received: 24 May 2021; Accepted: 14 June 2021;
Published: 12 July 2021.
Edited by:
Ylva Svensson, University West, SwedenCopyright © 2021 Suresh, Alam and Karkossa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rahul Suresh, rahul.suresh2@mail.mcgill.ca
†These authors have contributed equally to this work
 Rahul Suresh
Rahul Suresh Armaghan Alam
Armaghan Alam Zoe Karkossa2
Zoe Karkossa2