- 1Department of Psychiatry, Hanyang University Hospital, Seoul, South Korea
- 2Department of Data Science, Evidnet, Seongnam, South Korea
- 3Department of Social and Preventive Medicine, Sungkyunkwan University School of Medicine, Seoul, South Korea
- 4Pfizer Pharmaceuticals Korea Ltd., Seoul, South Korea
- 5Depression Clinical and Research Program, Massachusetts General Hospital, Harvard Medical School, Boston, MA, United States
- 6Department of Psychiatry, College of Medicine, Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, South Korea
- 7Department of Psychiatry, Depression Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, South Korea
- 8Department of Health Sciences and Technology, Samsung Advanced Institute for Health Sciences and Technology (SAIHST), Sungkyunkwan University, Seoul, South Korea
- 9Department of Medical Device Management and Research, Samsung Advanced Institute for Health Sciences and Technology (SAIHST), Sungkyunkwan University, Seoul, South Korea
- 10Department of Clinical Research Design and Evaluation, Samsung Advanced Institute for Health Sciences and Technology (SAIHST), Sungkyunkwan University, Seoul, South Korea
Introduction: Although people who attempted suicide tend to repeat suicide attempts, there is a lack of evidence on the association between psychiatric service factors and suicide reattempt among them.
Methods: We used a nationwide, population-based medical record database of South Korea to investigate the use of psychiatric services before and after the index suicide attempt and the association between psychiatric service factors after the index suicide attempt with the risk of suicide reattempt.
Results: Among 5,874 people who had attempted suicide, the all-cause mortality within 3 months after the suicide attempt was 11.6%. Among all subjects who attempted suicide, 30.6% of them had used psychiatric services within 6 months before the suicide attempt; 43.7% of them had used psychiatric services within 3 months after the suicide attempt. Among individuals who had visited clinics following attempted suicide, the cumulative incidence of suicide reattempt over a mean follow-up period of 5.1 years was 3.4%. About half of suicide reattempts occurred within 1 year after the index suicide attempt. Referral to psychiatric services within 7 days was associated with a decreased risk of suicide reattempt (adjusted hazard ratio, 0.51; 95% confidence intervals, 0.29–0.89).
Conclusion: An early psychiatric referral within 1 week after a suicide attempt was associated with a decreased risk of suicide reattempt.
Introduction
Suicide is a serious public health problem and a major cause of death worldwide (1). Globally, approximately 700,000 people die by suicide every year (2), and there are more than 20 failed suicide attempts for each suicide (3). The incidence of suicide varies across countries, and it is relatively high in South Korea with 26.9 per 100,000 people (4). Although no single risk factor is a strong predictor of suicide (5), previous studies identified risk factors associated with suicidal behaviors as genetic loading (6, 7), brain dysfunction (8, 9), psychopathologies (10, 11), emotional states, such as aggression and impulsivity (7, 12), comorbid physical diseases (13, 14), the use of hypnotics or illicit substances (7), and personal experiences, such as childhood trauma (6, 15).
There are two approaches to the management of suicidal people: suicide-specific treatments and treating the underlying psychiatric disorder (5). Suicide-specific treatments include long-term psychosocial interventions, brief psychosocial interventions, and pharmacological interventions; studies showed the antisuicidal effect of cognitive behavioral therapy (16), dialectical behavior therapy (17), caring contacts (18), and medications such as lithium (19, 20) and ketamine (21, 22). About 60–98% of suicide deaths are associated with primary psychiatric disorders (23). Depression, substance use disorders, schizophrenia, and personality disorders are the main psychiatric disorders that are associated with an increased risk of suicide (24). Moreover, a reduction in the professional care of patients with mental illness showed a strong association with suicide (25), whereas studies showed that the implementation of mental health services can reduce the risk of suicide (26, 27), suggesting the provision of mental health services to be an important aspect to prevent suicide.
A previous suicide attempt is one of the robust predictors of future suicide; about 30% of people who attempt suicide are known to repeat suicide attempts (28). Therefore, people with a history of suicide attempts were included in a high-risk group for suicide and were targeted for secondary prevention of suicide. Although numerous studies discovered the predictors for suicidal behaviors as previously mentioned, clinical predictors for suicide reattempt among subjects who attempted suicide are relatively poorly understood. A community-based study reported age ≤ 25 years, a higher family income, having any psychiatric disorder, poor education, stressful life events, alcohol abuse, and smoking to be associated with suicide reattempts (29). A study conducted on a single study site reported cluster B personality disorder, good treatment compliance, and repeated suicide attempts to be associated with an increased risk of suicide reattempt among subjects who attempted suicide (30). In an observational study, scheduling a single appointment within 7 days after discharge from the emergency room following a suicide attempt was found to lower the risk of suicide reattempt (31). Repeated follow-up among the clinical population was found to reduce the risk of suicide reattempt (32, 33).
The aim of this study was to expand the evidence by investigating the association between psychiatric service use factors with suicide reattempt among subjects who attempted suicide. We hypothesized that (1) the use of psychiatric services after a suicide attempt would prevent suicide reattempt and (2) the timing and frequency of referral to psychiatry after a suicide attempt would be associated with the risk of suicide reattempt.
Materials and methods
Data source
This study was based on the National Health Insurance Sharing Service (NHISS) database of the National Health Insurance Service (NHIS) of South Korea (34, 35). NHIS is a public institution responsible for operationalizing mandatory universal health insurance; approximately 97% of the total population in South Korea is enrolled in this service, while the remaining 3% is covered by the Medical Aid Program. The NHISS database contains medical services claim data (such as information about admission, emergency room visits, ambulatory care visits, and pharmaceutical services) and data on health screening programs. The NHISS data are anonymized to protect the privacy of individuals. The study protocol was approved by the Institutional Review Board of the Samsung Medical Center (No. 2019-03-136).
Population
We used NHISS data for the period from 1 January 2002 to 31 December 2018. We selected people who attempted suicide from 1 January 2003 to 31 December 2017 as subjects to rule out any previous suicide attempt in at least 1 year immediately preceding the index suicide attempt and to ensure a follow-up period of at least 1 year after the index suicide attempt.
People with intentional self-harm codes were identified as subjects based on the International Statistical Classification of Disease and Related Health Problems, 10th revision (ICD-10). We included people aged ≥ 18 years with X60–84 of the ICD-10 codes in the analyses.
Psychiatric service use before the index suicide attempt
We identified psychiatric service use of subjects before the index suicide attempt based on psychiatric outpatient visits, hospitalization in psychiatric wards, or emergency room care within 6 months before the index suicide attempt; psychiatric consultations made during hospitalization in other departments were also included based on the codes of individual psychotherapy. In addition, subjects’ psychiatric diagnosis and the use of psychiatric medications including antidepressants, antipsychotics, benzodiazepines, stimulants, mood stabilizers, and zolpidem were identified.
Deaths after the index suicide attempt
We identified all-cause deaths within the 3 months after the index suicide attempt. Considering the individual differences in the time leading to death, the period was categorized as 7 days, 8–14 days, 15–28 days, and 29–90 days.
Use of psychiatric services after the index suicide attempt
We operationally set 3 months to assess the psychiatric service use related to the index suicide attempt, considering the maximum prescribing period for psychiatric medications in South Korea. During this period, psychiatric outpatient visits, hospitalizations in psychiatric wards, emergency room care, and psychiatric consultations were identified. In addition, the timing of the first visit to the psychiatrist after the index suicide attempt, the frequency of psychiatric care visits, and the use of psychiatric medications during this period were identified.
Suicide reattempts
The primary outcome was suicide reattempts occurring from 3 months after the index suicide attempt. The results obtained within the 3 months immediately after the index suicide attempt were not included in the main outcome analysis; this was because, during this period, the suicide attempt codes could have been used not only for the actual suicide reattempt but also for medical care related to the index suicide attempt. Accordingly, we investigated the occurrence of suicide reattempts in people who had survived the attempt and had the code of suicide attempt from 3 months after the index suicide attempt.
Statistical analysis
We presented the distribution of demographic and socioeconomic characteristics, psychiatric characteristics, survival outcomes, and psychiatric service use factors after the index suicide attempts as numbers and percentages. The incidence of suicide reattempt was calculated, and multivariate regression analyses were performed to calculate the hazard ratios (HRs) for potential risk factors associated with suicide reattempt after adjusting for sex, age, disability severity, psychiatric diagnosis, referral to a psychiatrist within 3 months after the index suicide attempt, and psychiatric medication use within 3 months after the index suicide attempt. All statistical analyses were performed using SAS software version 9.4 (SAS Institute Inc., Cary, NC, United States).
Results
Demographic and socioeconomic characteristics of subjects who attempted suicide
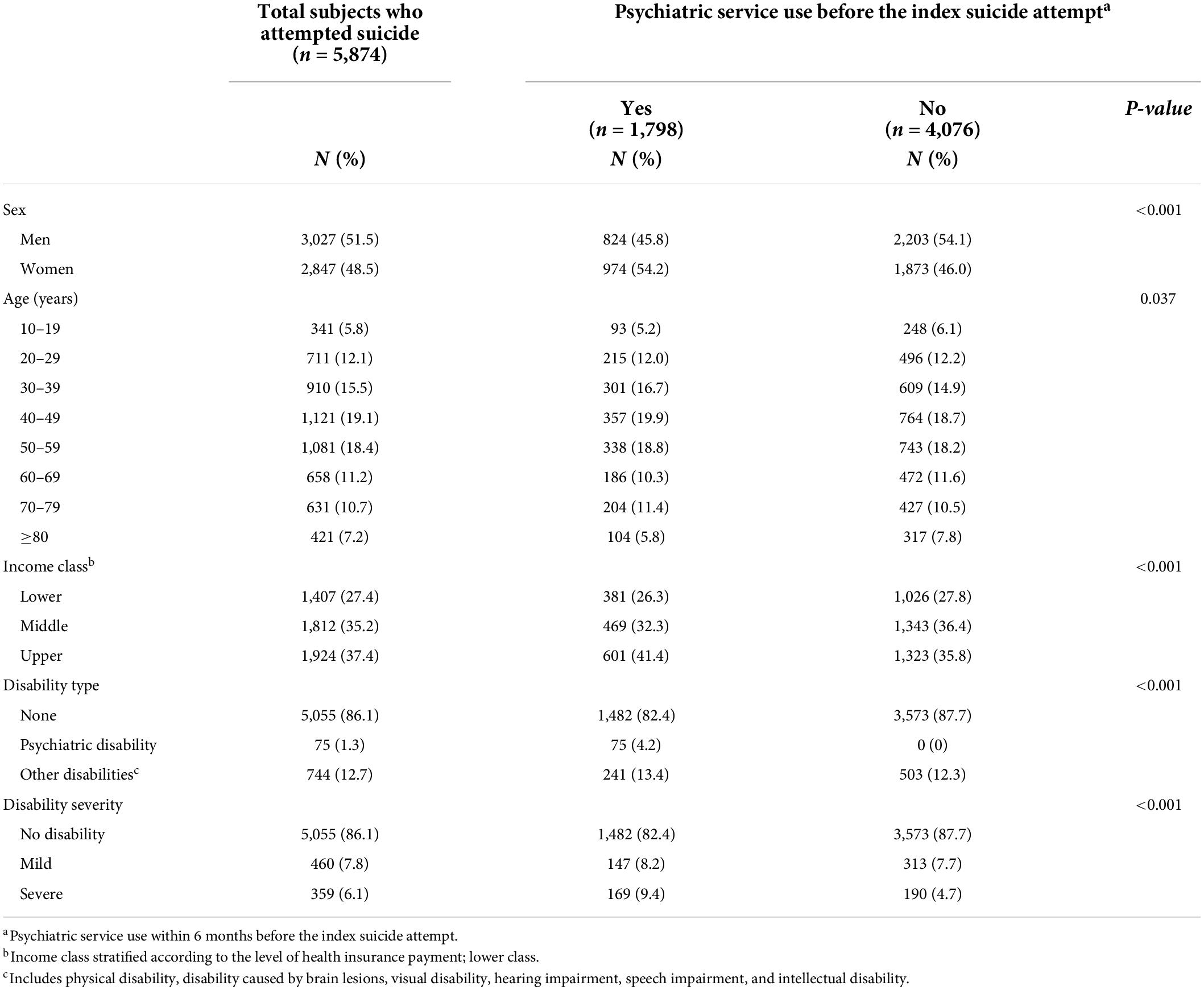
Table 1 and Supplementary Table 1 show the demographic and socioeconomic characteristics of subjects who attempted index suicide (n = 5,874); of these, 51.5% were men, and individuals in the age group of 40–49 years constituted the largest subgroup (19.1%). We categorized the study population into income classes based on the payment of health insurance (In South Korea, the payment of health insurance is determined by income level). Individuals belonging to the upper class accounted for the highest proportion of subjects who attempted index suicide (37.4%), followed by the middle class (35.2%). Approximately 1.3% of the subjects who attempted index suicide had a psychiatric disability, while 12.7% had other disabilities.
Among all the subjects who attempted suicide, 30.6% had visited a psychiatry clinic within 6 months before the index suicide attempt. On stratifying the study population according to psychiatric service use before the index suicide attempt, there were significant differences in the proportion of psychiatric service use before the index suicide attempt by sex, age, residential area, household income, type of disability, and severity of the disability. Men (27.2%) and those above 80 years (24.9%) showed a prominently lower proportion of psychiatric service use before the index suicide attempt.
Psychiatric characteristics of the study population
We investigated the psychiatric characteristics of the study population before the index suicide attempt. The diagnoses of adjustment disorder, depressive disorder, schizophrenia spectrum disorder, bipolar disorder, or other psychiatric disorders were included in the analysis if identified as a primary diagnosis made by a psychiatrist. Insomnia was included in the analysis if it was a primary or secondary diagnosis made by a doctor working in any department. About 39.9% of the subjects were diagnosed with insomnia. Based on the primary diagnosis by a psychiatrist, depressive disorders were the most prevalent psychiatric disorder among subjects who attempted suicide (19.4%), while insomnia accounted for 5.3%; 49.6% of subjects had no psychiatric diagnosis.
Within 6 months before the index suicide attempt, 44.5, 22.8, and 19.8% of the subjects had been prescribed benzodiazepines, antidepressants, and zolpidem, respectively. During this period, 27.4% had visited the psychiatric outpatient clinic and 6.4% had been admitted to the psychiatric wards. In the course of the entire study period before the index suicide attempt, 13.7% had a history of admission to a psychiatric ward (Table 2).
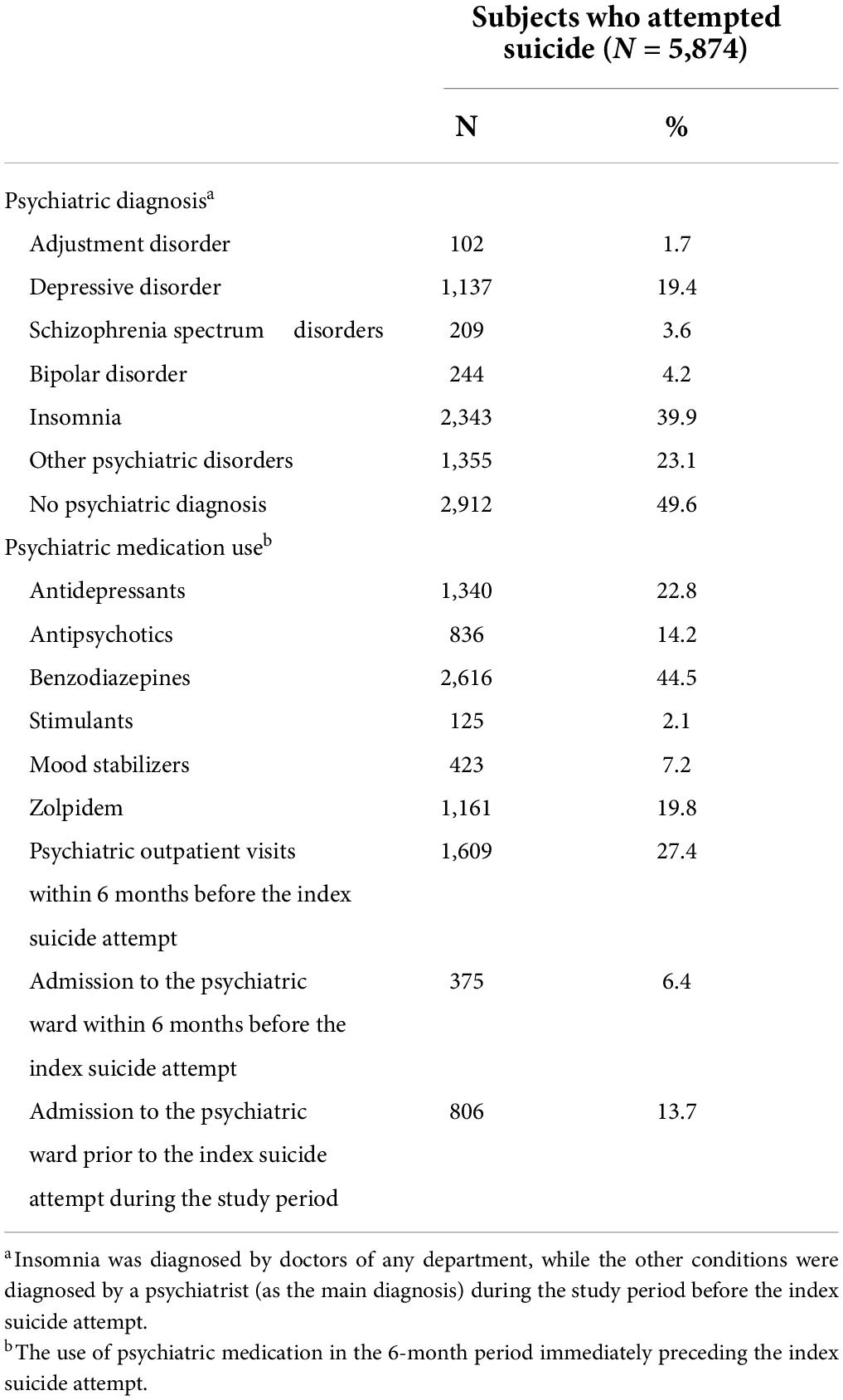
Table 2. Psychiatric characteristics of subjects who attempted suicide before the index suicide attempt.
Methods used for the index suicide attempt
Approximately 68.9% of subjects who attempted suicide tried to poison themselves. Hanging, strangulation, and suffocation accounted for 12.0%, and the use of sharp or blunt objects accounted for 10.9% of suicide attempts (Supplementary Table 2).
Deaths and psychiatric service use within 3 months after an index suicide attempt
Among subjects who attempted index suicide, 88.4% survived 3 months after the index suicide attempt, while 8.0% died within 7 days. Approximately 43.7% of subjects had used psychiatric services within 3 months after the index suicide attempt. After the index suicide attempt, 32.9% had visited their psychiatric service within 7 days, 7.7% within 8–28 days, and 3.1% within 29 days–3 months (Table 3).
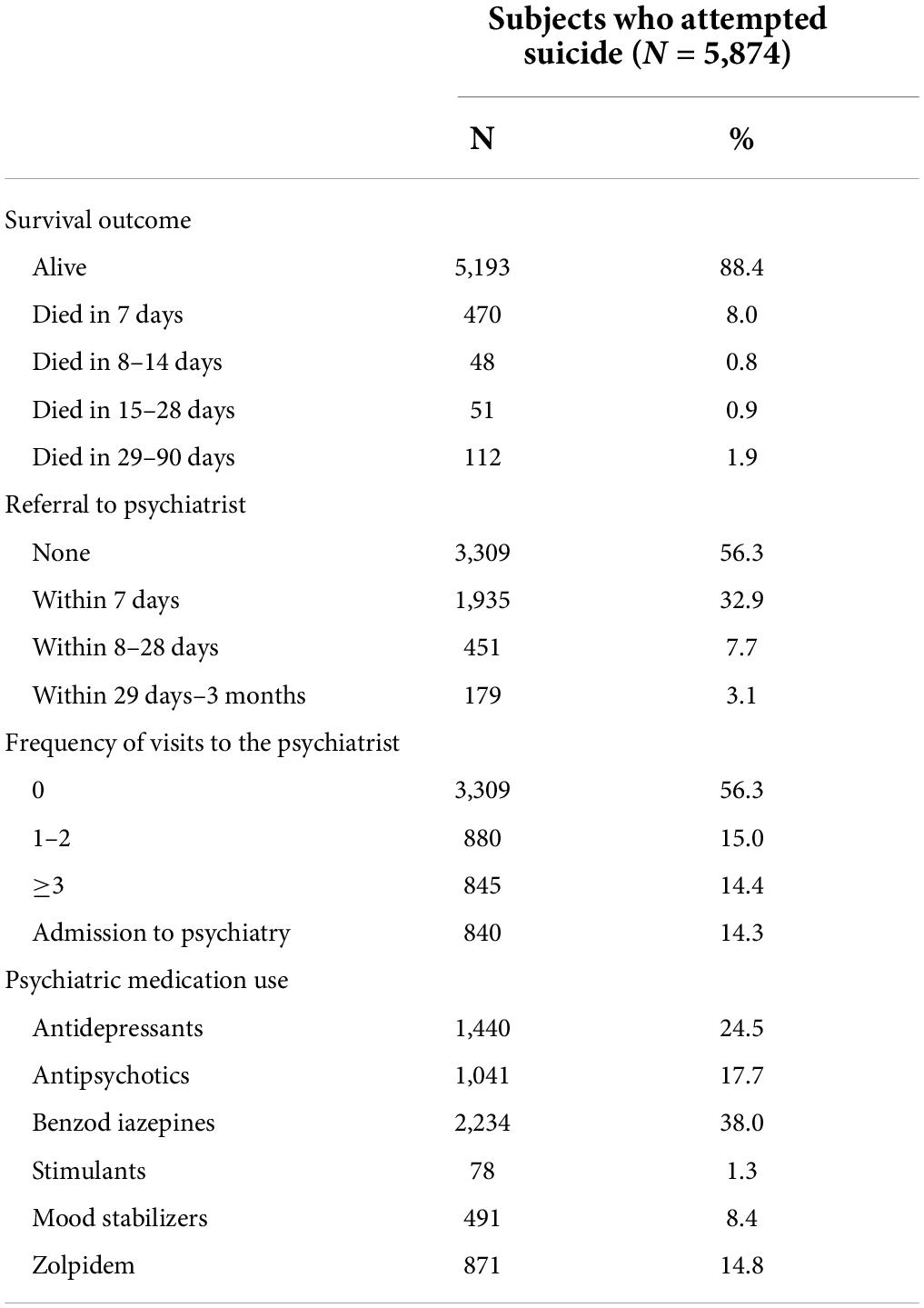
Table 3. Deaths and psychiatric service use of subjects who attempted index suicide within 3 months after the index suicide attempt.
Incidence of suicide reattempt after the index suicide attempt
We investigated the incidence of suicide reattempts from 3 months after the index suicide attempt. The incidence of suicide reattempt in the entire study population over a mean follow-up period of 5.1 years was 3.36% (95% CI: 2.74–4.11). The yearly incidence was the highest in the first year from 3 months after the index suicide attempt (year 1 = 1.7%) (Figure 1).
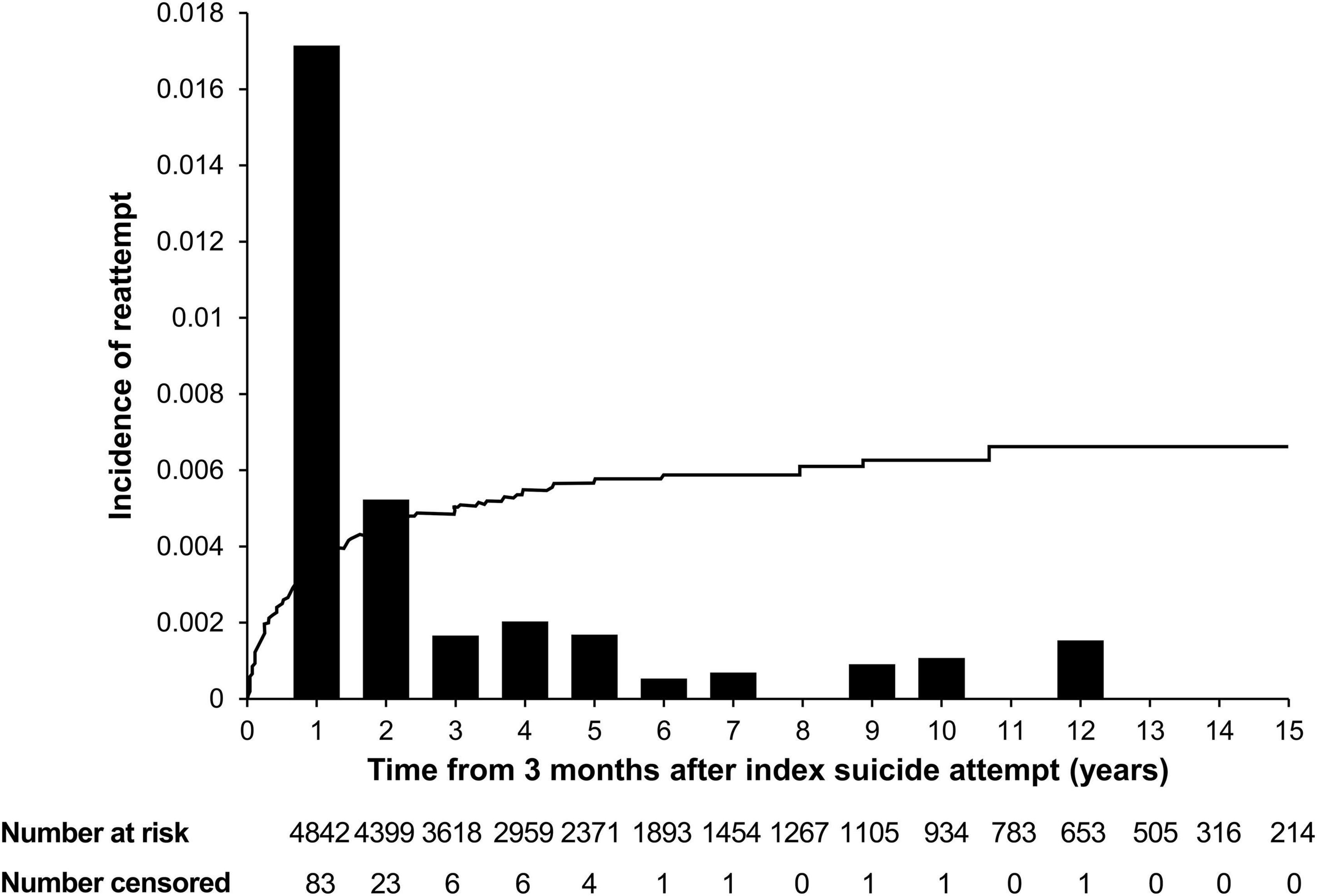
Figure 1. Incidence of suicide reattempt after an index suicide attempt. Incidence of suicide reattempt among individuals who visited clinics with attempted suicide from 3 months after the index suicide attempt. The line represents the cumulative incidence of suicide reattempt after the index suicide attempt, while the bars represent the yearly incidence of suicide reattempt after the index suicide attempt. Yearly incidence: Year 1 = 1.7%, Year 2 = 0.5%, Year 3 = 0.2%, Year 4 = 0.2%, Year 5 = 0.2%, Year 6 = 0.1%, Year 7 = 0.1%, Year 8 = 0%, Year 9 = 0.1%, Year 10 = 0.1%, Year 11 = 0%, Year 12 = 0.2%, Year 13 = 0%, Year 14 = 0%, and Year 15 = 0%.
Regarding referral to a psychiatrist after the index suicide attempt, the incidence of suicide reattempt was 2.82% (95% CI: 2.16–3.69) among individuals who were not referred within 3 months, 3.04% (95% CI: 2.25–4.12) among those who were referred within 7 days, 6.08% (95% CI: 3.29–11.08) among those who were referred within 8–28 days, and 9.73% (95% CI: 2.98–29.30) among those who were referred within 29 days–3 months (Figure 2).
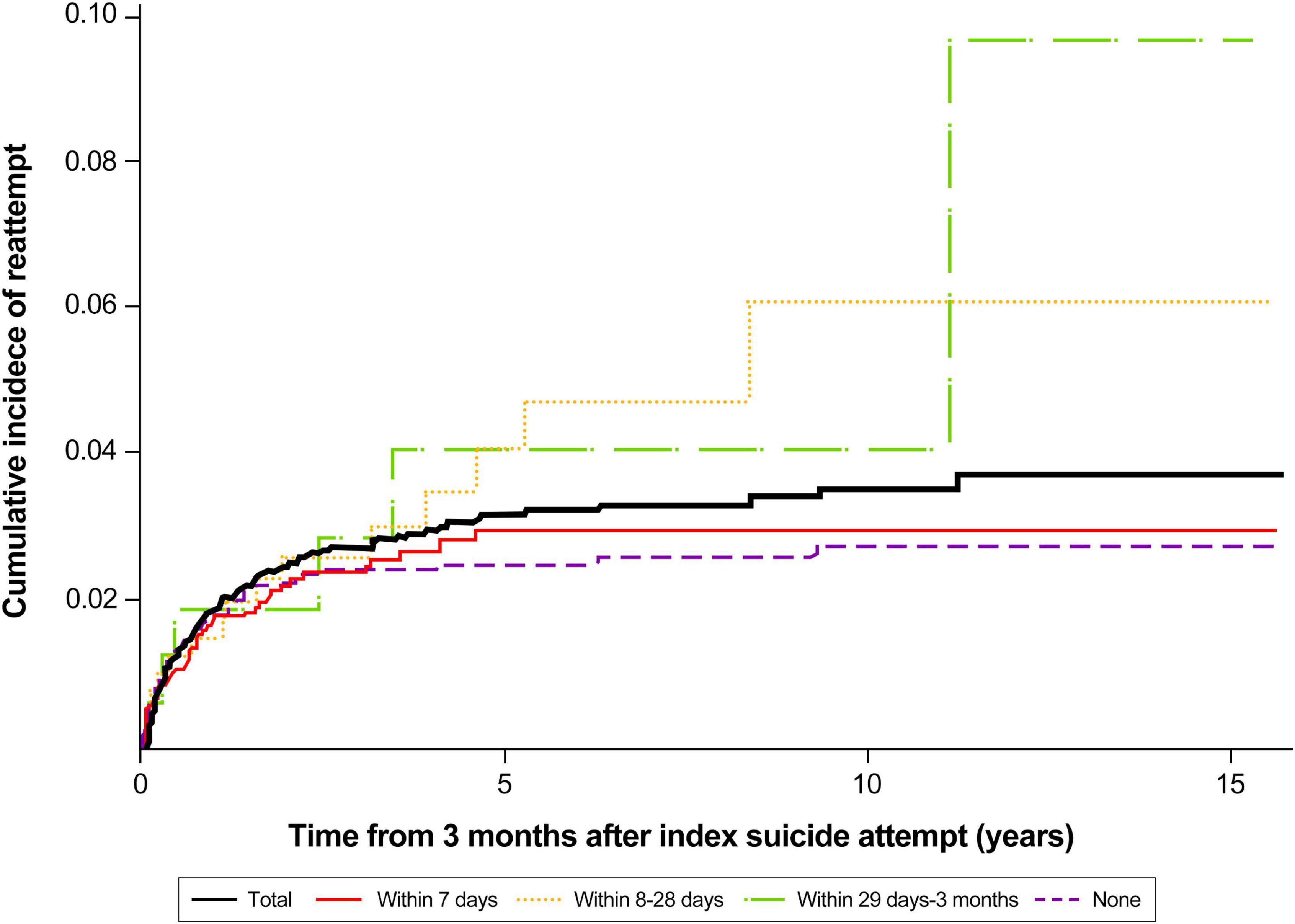
Figure 2. Cumulative incidence of suicide reattempt after index suicide attempt according to the timing of referral to psychiatry.
Adjusted hazard ratios of potential risk factors for suicide reattempts
We investigated the potential risk factors for suicide reattempt in the study population and calculated the corresponding HRs. Mild disability was associated with a significantly higher risk of suicide reattempt compared to the absence of any disability [adjusted hazard ratio (aHR) 2.09, 95% confidence interval (CI): 1.21–3.62, p = 0.008]. Adjustment disorder, depressive disorder, schizophrenia spectrum disorder, bipolar disorder, and insomnia showed no significant association with suicide reattempt. Referral to a psychiatrist within 7 days from the index suicide attempt was associated with a reduced risk of suicide reattempt compared to the absence of psychiatric referral (aHR 0.51, 95% CI: 0.29–0.89, p = 0.018). The use of antidepressants was associated with an increased risk of suicide reattempt (aHR 1.73, 95% CI: 1.08–2.77, p = 0.022), while the use of zolpidem was associated with a decreased risk of suicide reattempt (aHR 0.58, 95% CI: 0.34–0.99, p = 0.045) compared to the non-use of psychiatric medications (Table 4).
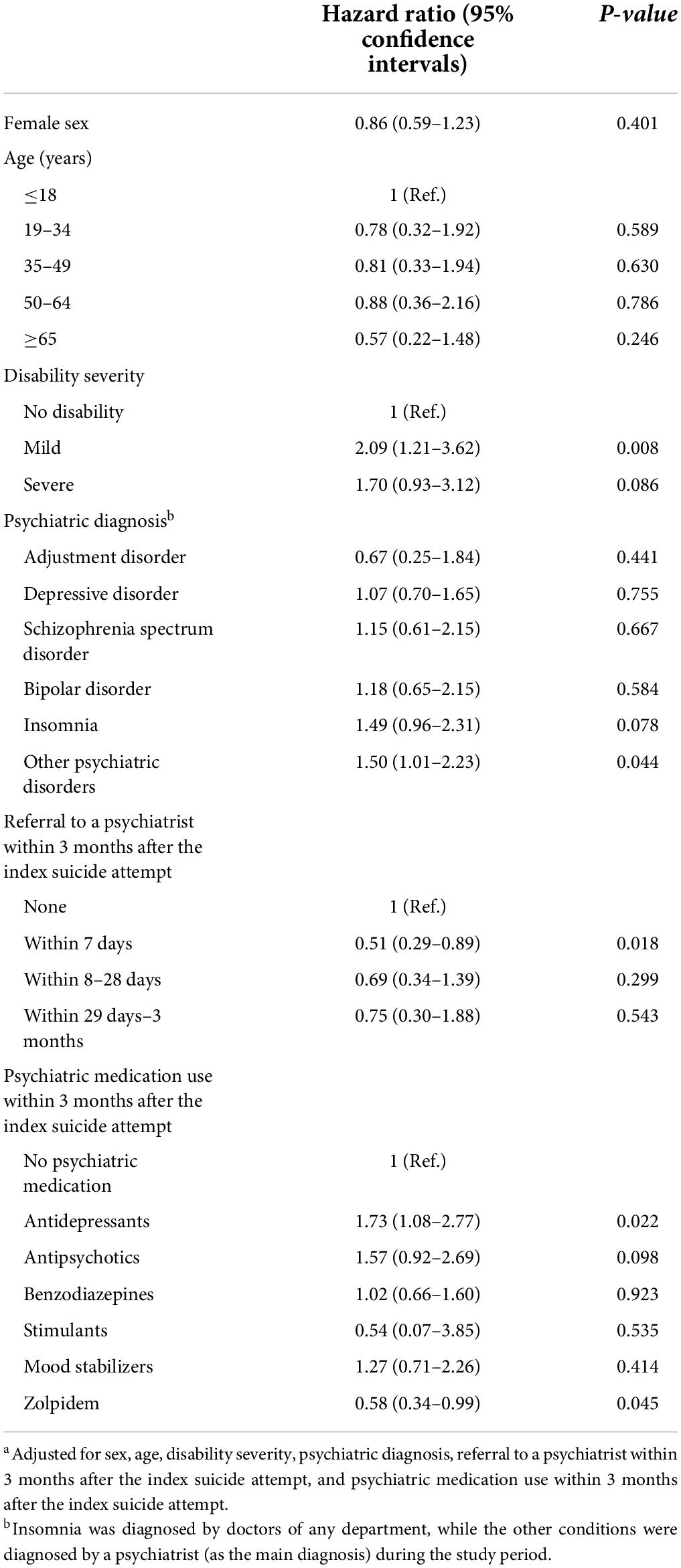
Table 4. Adjusted hazard ratios of potential risk factors for suicide reattempt among subjects who attempted suicide had not reattempted suicide or died within the 3-month period after the index suicide attempt (n = 4,842)a.
On multivariate regression analysis after including the frequency of visits to a psychiatrist during the 3 months instead of referral to a psychiatrist for 3 months, one or two visits after the index suicide attempt were associated with a lower risk of suicide reattempt compared to no visit (aHR 0.25, 95% CI: 0.10–0.59, p = 0.002) (Supplementary Table 3).
Discussion
In this study, we used national claims data to investigate the psychiatric service use factors of subjects who attempted suicide before and after their initial suicide attempt and the association between psychiatric service use after an index suicide attempt and the risk of suicide reattempt. We found that approximately 30% of the subjects who attempted suicide had visited psychiatry within 6 months before the index suicide attempt. About 8 and 12% of subjects who attempted suicide died within 7 days and 3 months after the index suicide attempt, respectively; therefore, the estimated mortality rate for index suicide attempts was 8–12%. Mild disability and the use of antidepressants were associated with an increased risk of suicide reattempt, while the use of zolpidem was associated with a decreased risk of suicide reattempt. Referral to psychiatry within 7 days after the index suicide attempt was associated with a significantly lower risk of suicide reattempt.
While most suicidal behaviors are known to be related to psychiatric diseases, only 30% of the study population had visited psychiatry clinics prior to their index suicide attempt. This finding indicates the undertreatment of the psychiatric problems of subjects who attempted suicide. This phenomenon is likely attributable to access to care. Although the access to care in South Korea could be evaluated as high, considering the high level of healthcare use, low avoidable mortality, and low infant mortality (36), it may differ by individual factors. Therefore, it is necessary to identify the population with low access to care and to prevent any delay in psychiatric intervention for them to prevent suicide reattempt. In addition, the stigma associated with mental illnesses could affect the undertreatment (37); people with suicidal ideation tend to hide their suicidality and refrain from seeking professional help (38–40). Even after it became clear that these individuals were at high risk of suicide after the failed suicide attempt, referrals to psychiatry increased to only 44%. In this study, there were significant differences in the proportion of psychiatric service use before the index suicide attempt by demographic and socioeconomic characteristics, and men and those above 80 years showed further lower use of psychiatric service use before the index suicide attempt, suggesting that they could be high-risk populations for the undertreatment. In a previous study, age, presence of psychotic disorder, and absence of substance use disorder were predictors of referral to psychiatric consultation after the suicide attempt, while the hospital where the subjects who attempted suicide were treated most strongly affected the referral to psychiatry (41). Considering these, additional efforts are needed to ensure the subsequent psychiatric intervention among subjects who attempted suicide.
Referral to psychiatry within 7 days after the index suicide attempt reduced the risk of suicide reattempt by half compared to those who did not visit psychiatry; this suggests the importance of rapid psychiatric intervention after the suicide attempt for secondary prevention of suicide attempts. According to a previous study of subjects who attempted suicide, approximately 49% of subjects required urgent psychiatric care during the follow-up period (42). Indeed, even among subjects who attempted suicide with no mental illness, immediate and brief intervention after suicide attempts resulted in lowering the subsequent suicide rate (43). Early psychiatric intervention can help prevent further suicide attempts by assisting the individual in dealing with suicide-associated stigma and stressful life events in addition to facilitating treatment of mental illnesses. A qualitative study found that the stigma associated with mental illness contributes to suicidality; moreover, suicide survivors experience additional suicide-related stigma (37). Similarly, another study revealed an association between the anticipated stigma of suicide and suicidality; this suggests that the anticipated suicide-related stigma and secrecy can aggravate suicidality in subjects who attempted suicide (44). Suicide-related stigma can lead to a feeling of loneliness or hopelessness, which are precursors of suicidality (37). Thus, we assume that timely psychiatric intervention in the early stages of suicidal behavior may help prevent suicide reattempts.
The use of antidepressants was associated with an increased risk of suicide reattempts, and the use of zolpidem was associated with a decreased risk of them. However, these results should be interpreted with caution as our study is based on claims data; data about clinical variables (such as the severity of depression) were not adequately captured in the database. Regarding antidepressant use, those who used antidepressants might have greater severity of depression or a recurrent course than those who did not use antidepressants, which may affect the increased risk of suicide reattempt. Indeed, there is no clear consensus on the association between the use of antidepressants and suicide risk. After the Food and Drug Administration had issued a black-box warning reflecting reports of an increased risk of suicidal behavior during treatment of young individuals with antidepressants (45, 46), the prescription of antidepressants and the frequency of diagnosis of depression showed a decline, and these resulted in a concomitant increase in the incidence of psychotropic drug poisoning, which is considered a proxy for suicide attempts (47). Similarly, regarding the decreased risk of suicide reattempt among zolpidem users, although this finding is consistent with that of our previous study (48), there also have been several studies reporting the opposite results (49–51). The reason for these opposite results is assumed that various confounders related to the use of zolpidem can affect suicidal behavior and methodologic differences in consideration of this might differ between studies. That is, in addition to the single factor of “use of zolpidem,” various clinical factors in the individual might affect suicidal behaviors, such as degree of insomnia, other psychiatric medications, and comorbid mental disorders.
This study has strength, in that it employed real-world data based on a national sample to characterize the use of psychiatric services by subjects who attempted suicide and investigated the long-term effects of potential risk factors for suicide reattempt. However, some limitations of this study should be considered while interpreting the results. First, we used intentional self-harm codes as per ICD-10 to define subjects who attempted suicide. Self-harm by concept includes suicide attempts; however, it is possible that people with non-suicidal self-harm were also included in this study. Second, we operationally set a 3-month period after the index suicide attempt for the occurrence of deaths and psychiatric service use after the index suicide attempt and followed up suicide reattempts after this period. However, it is highly possible that suicide reattempt occurs within 3 months after the index suicide attempt. A previous study found that about 50% of suicide reattempts occur within the first 6 months after the index suicide attempt (30). Similarly, delayed management following the index suicide attempt might have been included in the analysis for suicide reattempt.
Conclusion
This retrospective cohort study using national claims data discovered that early psychiatric referral of subjects who attempted suicide, especially within 1 week after the initial attempt, can reduce the risk of suicide reattempt. Individuals who attempt suicide tend to repeat suicide attempts; in the process, their suicidal capability increases with a consequent increase in the probability of death (52). Physicians should be aware of this phenomenon and identify individuals undergoing this process; immediate referrals of these individuals to psychiatry may help stop this devastating process.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://nhiss.nhis.or.kr/ (Research management number: NHIS-2019-1-520).
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of the Samsung Medical Center. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
HK contributed to the conceptualization, data curation, investigation, methodology, and writing the original draft of the manuscript. YK and M-HS contributed to the data analysis. H-EP and Y-JP contributed to the conceptualization and project administration. HJJ contributed to the conceptualization, project administration, and supervision. All authors contributed to the writing and editing the manuscript.
Conflict of interest
This study was sponsored by Pfizer Pharmaceuticals Korea Ltd. The funder had the following involvement with the study: conceptualization, project administration, writing the manuscript, and decision to submit the manuscript for publication.
HJJ was a paid consultant for Pfizer Pharmaceuticals Korea Ltd. Y-JP was a full-time employee of Pfizer Korea and holds stocks in Pfizer Inc. H-EP was a previous employee of Pfizer Korea and holds stocks in Pfizer Inc. DM received research support from Nordic Naturals. He provided unpaid consulting for Pharmavite LLC and Gnosis USA, Inc. He received honoraria for speaking from the Massachusetts General Hospital Psychiatry Academy, Blackmores, Harvard Blog, and PeerPoint Medical Education Institute, LLC. He received royalties from Lippincott Williams and Wilkins for the published book “Natural Medications for Psychiatric Disorders: Considering the Alternatives”. He also works with the MGH Clinical Trials Network and Institute, which has received research funding from multiple pharmaceutical companies and NIMH. MF received research support from Acadia Pharmaceuticals, Allergan, Alkermes, Inc., Aptinyx, Avanir Pharmaceuticals Inc., Axsome, Benckiser Pharmaceuticals, Inc., BioClinica, Inc., Biogen, BioHaven, Cambridge Science Corporation, Cerecor, Gate Neurosciences, Inc., GenOmind, LLC, Gentelon, LLC, Happify, Johnson and Johnson, Lundbeck Inc., Marinus Pharmaceuticals, Methylation Sciences, Inc., Millennium Pharmaceutics, Inc., Minerva Neurosciences, Neuralstem, NeuroRX Inc., Novartis, Otsuka, Pfizer, Premiere Research International, Relmada Therapeutics Inc., Reckitt, Shenox Pharmaceuticals, Stanley Medical Research Institute (SMRI), Taisho, Takeda, Vistagen, National Institute of Drug Abuse (NIDA); National Institutes of Health (NIH), National Institute of Mental Health (NIMH), and PCORI. He not done any personal consulting. Any consulting he has done has been on behalf of the Massachusetts General Hospital. He equity holdings: Compellis; Psy Therapeutics. He royalty/patent, other income: Patents for Sequential Parallel Comparison Design (SPCD), licensed by MGH to Pharmaceutical Product Development, LLC (PPD) (US_7840419, US_7647235, US_7983936, US_8145504, US_8145505); and patent application for a combination of Ketamine plus Scopolamine in Major Depressive Disorder (MDD), licensed by MGH to Biohaven. Patents for pharmacogenomics of Depression Treatment with Folate (US_9546401, US_9540691). He copyright for the MGH Cognitive and Physical Functioning Questionnaire (CPFQ), Sexual Functioning Inventory (SFI), Antidepressant Treatment Response Questionnaire (ATRQ), Discontinuation-Emergent Signs and Symptoms (DESS), Symptoms of Depression Questionnaire (SDQ), and SAFER; Lippincott Williams and Wilkins; Wolkers Kluwer; World Scientific Publishing Co., Pte., Ltd. This study was funded by Pfizer Pharmaceuticals Korea Ltd. and had a significant role in the conceptualization, manuscript preparation, and decision to publish.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.607892/full#supplementary-material
References
1. Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. (2008) 30:133–54. doi: 10.1093/epirev/mxn002
2. WHO. Suicide Prevention. (2022). Available online at: https://www.who.int/health-topics/suicide (accessed June 22, 2022).
3. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. (1998) 59 Suppl 20:22–33; quiz4–57.
4. Korea Foundation for Suicide Prevention. 2021 White Paper on Suicide Prevention. New York, NY: Korea Foundation for Suicide Prevention (2021).
5. Turecki G, Brent DA, Gunnell D, O’Connor RC, Oquendo MA, Pirkis J, et al. Suicide and suicide risk. Nat Rev Dis Primers. (2019) 5:74. doi: 10.1038/s41572-019-0121-0
6. Mann JJ. Neurobiology of suicidal behaviour. Nat Rev Neurosci. (2003) 4:819–28. doi: 10.1038/nrn1220
7. Turecki G. The molecular bases of the suicidal brain. Nat Rev Neurosci. (2014) 15:802–16. doi: 10.1038/nrn3839
8. Kim K, Kim SW, Myung W, Han CE, Fava M, Mischoulon D, et al. Reduced orbitofrontal-thalamic functional connectivity related to suicidal ideation in patients with major depressive disorder. Sci Rep. (2017) 7:15772. doi: 10.1038/s41598-017-15926-0
9. Valdizan EM, Diez-Alarcia R, Gonzalez-Maeso J, Pilar-Cuellar F, Garcia-Sevilla JA, Meana JJ, et al. alpha(2)-adrenoceptor functionality in postmortem frontal cortex of depressed suicide victims. Biol Psychiatry. (2010) 68:869–72. doi: 10.1016/j.biopsych.2010.07.023
10. Jeon HJ, Park JI, Fava M, Mischoulon D, Sohn JH, Seong S, et al. Feelings of worthlessness, traumatic experience, and their comorbidity in relation to lifetime suicide attempt in community adults with major depressive disorder. J Affect Disord. (2014) 166:206–12. doi: 10.1016/j.jad.2014.05.010
11. Kim H, Choi KW, Na EJ, Hong JP, Fava M, Mischoulon D, et al. Anxiety attacks with or without life-threatening situations, major depressive disorder, and suicide attempt: a nationwide community sample of Korean adults. Psychiatry Res. (2018) 270:257–63. doi: 10.1016/j.psychres.2018.09.050
12. Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. (1999) 156:181–9. doi: 10.1176/ajp.156.2.181
13. Hawton K, van Heeringen K. Suicide. Lancet. (2009) 373:1372–81. doi: 10.1016/S0140-6736(09)60372-X
14. Zaorsky NG, Zhang Y, Tuanquin L, Bluethmann SM, Park HS, Chinchilli VM. Suicide among cancer patients. Nat Commun. (2019) 10:207. doi: 10.1038/s41467-018-08170-1
15. Jeon HJ, Roh MS, Kim KH, Lee JR, Lee D, Yoon SC, et al. Early trauma and lifetime suicidal behavior in a nationwide sample of Korean medical students. J Affect Disord. (2009) 119:210–4. doi: 10.1016/j.jad.2009.03.002
16. Tarrier N, Taylor K, Gooding P. Cognitive-behavioral interventions to reduce suicide behavior: a systematic review and meta-analysis. Behav Modif. (2008) 32:77–108. doi: 10.1177/0145445507304728
17. Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry. (2006) 63:757–66. doi: 10.1001/archpsyc.63.7.757
18. Riblet NBV, Shiner B, Young-Xu Y, Watts BV. Strategies to prevent death by suicide: meta-analysis of randomised controlled trials. Br J Psychiatry. (2017) 210:396–402. doi: 10.1192/bjp.bp.116.187799
19. Hayes JF, Pitman A, Marston L, Walters K, Geddes JR, King M, et al. Self-harm, unintentional injury, and suicide in bipolar disorder during maintenance mood stabilizer treatment: a UK population-based electronic health records study. JAMA Psychiatry. (2016) 73:630–7. doi: 10.1001/jamapsychiatry.2016.0432
20. Song J, Sjölander A, Joas E, Bergen SE, Runeson B, Larsson H, et al. Suicidal behavior during lithium and valproate treatment: a within-individual 8-year prospective study of 50,000 patients with bipolar disorder. Am J Psychiatry. (2017) 174:795–802. doi: 10.1176/appi.ajp.2017.16050542
21. Grunebaum MF, Galfalvy HC, Choo TH, Keilp JG, Moitra VK, Parris MS, et al. Ketamine for rapid reduction of suicidal thoughts in major depression: a midazolam-controlled randomized clinical trial. Am J Psychiatry. (2018) 175:327–35. doi: 10.1176/appi.ajp.2017.17060647
22. Murrough JW, Soleimani L, DeWilde KE, Collins KA, Lapidus KA, Iacoviello BM, et al. Ketamine for rapid reduction of suicidal ideation: a randomized controlled trial. Psychol Med. (2015) 45:3571–80. doi: 10.1017/s0033291715001506
23. Bachmann S. Epidemiology of suicide and the psychiatric perspective. Int J Environ Res Public Health. (2018) 15:1425. doi: 10.3390/ijerph15071425
24. Bertolote JM, Fleischmann A, De Leo D, Wasserman D. Psychiatric diagnoses and suicide: revisiting the evidence. Crisis. (2004) 25:147–55. doi: 10.1027/0227-5910.25.4.147
25. Appleby L, Dennehy JA, Thomas CS, Faragher EB, Lewis G. Aftercare and clinical characteristics of people with mental illness who commit suicide: a case-control study. Lancet. (1999) 353:1397–400. doi: 10.1016/S0140-6736(98)10014-4
26. Layman DM, Kammer J, Leckman-Westin E, Hogan M, Goldstein Grumet J, Labouliere CD, et al. The Relationship between suicidal behaviors and zero suicide organizational best practices in outpatient mental health clinics. Psychiatr Serv. (2021) 72:1118–25. doi: 10.1176/appi.ps.202000525
27. While D, Bickley H, Roscoe A, Windfuhr K, Rahman S, Shaw J, et al. Implementation of mental health service recommendations in England and Wales and suicide rates, 1997-2006: a cross-sectional and before-and-after observational study. Lancet. (2012) 379:1005–12. doi: 10.1016/S0140-6736(11)61712-1
28. Carter GL, Clover KA, Bryant JL, Whyte IM. Can the Edinburgh risk of repetition scale predict repetition of deliberate self-poisoning in an Australian clinical setting? Suicide Life Threat Behav. (2002) 32:230–9. doi: 10.1521/suli.32.3.230.22175
29. Esmaeili ED, Farahbakhsh M, Sarbazi E, Khodamoradi F, Gaffari Fam S, Azizi H. Predictors and incidence rate of suicide re-attempt among suicide attempters: a prospective study. Asian J Psychiatr. (2022) 69:102999. doi: 10.1016/j.ajp.2021.102999
30. Irigoyen M, Porras-Segovia A, Galvan L, Puigdevall M, Giner L, De Leon S, et al. Predictors of re-attempt in a cohort of suicide attempters: a survival analysis. J Affect Disord. (2019) 247:20–8. doi: 10.1016/j.jad.2018.12.050
31. Martinez-Ales G, Jimenez-Sola E, Roman-Mazuecos E, Sanchez-Castro MP, de Dios C, Rodriguez-Vega B, et al. An emergency department-initiated intervention to lower relapse risk after attempted suicide. Suicide Life Threat Behav. (2019) 49:1587–99. doi: 10.1111/sltb.12542
32. Farre A, Portella MJ, De Angel L, Diaz A, de Diego-Adelino J, Vegue J, et al. Benefits of a secondary prevention program in suicide. Crisis. (2016) 37:281–9. doi: 10.1027/0227-5910/a000388
33. Plancke L, Amariei A, Danel T, Debien C, Duhem S, Notredame CE, et al. Effectiveness of a French program to prevent suicide reattempt (VigilanS). Arch Suicide Res. (2020) 25:570–81. doi: 10.1080/13811118.2020.1735596
34. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the national health insurance service-national sample cohort (NHIS-NSC), South Korea. Int J Epidemiol. (2017) 46:e15. doi: 10.1093/ije/dyv319
35. Shin DW, Cho B, Guallar E. Korean national health insurance database. JAMA Intern Med. (2016) 176:138. doi: 10.1001/jamainternmed.2015.7110
36. Organisation for Economic Co-operation and Development. OECD Health Statistics 2021. (2021). Available online at: https://www.oecd.org/health/health-data.htm (accessed June 23, 2022).
37. Oexle N, Herrmann K, Staiger T, Sheehan L, Rusch N, Krumm S. Stigma and suicidality among suicide attempt survivors: a qualitative study. Death Stud. (2019) 43:381–8. doi: 10.1080/07481187.2018.1474286
38. Busch KA, Fawcett J, Jacobs DG. Clinical correlates of inpatient suicide. J Clin Psychiatry. (2003) 64:14–9. doi: 10.4088/jcp.v64n0105
39. Friedlander A, Nazem S, Fiske A, Nadorff MR, Smith MD. Self-concealment and suicidal behaviors. Suicide Life Threat Behav. (2012) 42:332–40. doi: 10.1111/j.1943-278X.2012.00094.x
40. Waern M, Beskow J, Runeson B, Skoog I. Suicidal feelings in the last year of life in elderly people who commit suicide. Lancet. (1999) 354:917–8. doi: 10.1016/S0140-6736(99)93099-4
41. Suominen KH, Isometsa ET, Lonnqvist JK. Attempted suicide and psychiatric consultation. Eur Psychiatry. (2004) 19:140–5. doi: 10.1016/j.eurpsy.2003.12.004
42. Lopez-Goni JJ, Goni-Sarries A, Azcarate-Jimenez L, Sabater-Maestro P. Suicidal behaviour recurrence in psychiatric emergency departments of patients without a prior suicide attempt, index and reattempters: a prospective study. Rev Psiquiatr Salud Ment. (2018) 13:192–201. doi: 10.1016/j.rpsm.2018.07.003
43. Givon L, Levi A, Bloch B, Fruchter E. Immediate and brief intervention after suicide attempts on patients without major psychiatric morbidity-A pilot study in northern Israel. Eur Psychiatry. (2018) 51:20–4. doi: 10.1016/j.eurpsy.2018.01.006
44. Mayer L, Rusch N, Frey LM, Nadorff MR, Drapeau CW, Sheehan L, et al. Anticipated suicide stigma, secrecy, and suicidality among suicide attempt survivors. Suicide Life Threat Behav. (2020) 50:706–13. doi: 10.1111/sltb.12617
45. Hall WD. How have the SSRI antidepressants affected suicide risk? Lancet. (2006) 367:1959–62. doi: 10.1016/S0140-6736(06)68860-0
46. Friedman RA, Leon AC. Expanding the black box – depression, antidepressants, and the risk of suicide. N Engl J Med. (2007) 356:2343–6. doi: 10.1056/NEJMp078015
47. Licata SC, Jensen JE, Conn NA, Winer JP, Lukas SE. Zolpidem increases GABA in depressed volunteers maintained on SSRIs. Psychiatry Res. (2014) 224:28–33. doi: 10.1016/j.pscychresns.2014.05.009
48. Kim H, Kim Y, Myung W, Fava M, Mischoulon D, Lee U, et al. Risks of suicide attempts after prescription of zolpidem in people with depression: a nationwide population study in South Korea. Sleep. (2020) 43:zsz235. doi: 10.1093/sleep/zsz235
49. Sun Y, Lin CC, Lu CJ, Hsu CY, Kao CH. Association between zolpidem and suicide: a nationwide population-based case-control study. Mayo Clin Proc. (2016) 91:308–15. doi: 10.1016/j.mayocp.2015.10.022
50. Brower KJ, McCammon RJ, Wojnar M, Ilgen MA, Wojnar J, Valenstein M. Prescription sleeping pills, insomnia, and suicidality in the national comorbidity survey replication. J Clin Psychiatry. (2011) 72:515–21. doi: 10.4088/JCP.09m05484gry
51. Choi B, Sung HG, Nam JH, Shin JY. Zolpidem use and suicide death in South Korea: a population-based case-control study. Suicide Life Threat Behav. (2019) 49:1653–67. doi: 10.1111/sltb.12548
Keywords: suicide attempt, suicide reattempt, psychiatric service use, psychiatric referral, suicide prevention
Citation: Kim H, Kim Y, Shin M-H, Park Y-J, Park H-E, Fava M, Mischoulon D, Park MJ, Kim EJ and Jeon HJ (2022) Early psychiatric referral after attempted suicide helps prevent suicide reattempts: A longitudinal national cohort study in South Korea. Front. Psychiatry 13:607892. doi: 10.3389/fpsyt.2022.607892
Received: 18 September 2020; Accepted: 10 August 2022;
Published: 06 September 2022.
Edited by:
Antoine Bechara, University of Southern California, United StatesReviewed by:
Alberto Forte, Sapienza University of Rome, ItalyM. David Rudd, University of Memphis, United States
Copyright © 2022 Kim, Kim, Shin, Park, Park, Fava, Mischoulon, Park, Kim and Jeon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hong Jin Jeon, jeonhj@skku.edu
 Hyewon Kim
Hyewon Kim Yuwon Kim2
Yuwon Kim2 David Mischoulon
David Mischoulon Hong Jin Jeon
Hong Jin Jeon