- 1Department of Critical Care Medicine, Xiangya Hospital, Central South University, Changsha, China
- 2Department of Urology, Zhongnan Hospital, Wuhan University, Wuhan, China
- 3Department of Emergency Medicine, The Second Xiangya Hospital, Central South University, Changsha, China
- 4Department of Cardiology, The Second Xiangya Hospital, Central South University, Changsha, China
- 5Department of Psychiatry, The Second Xiangya Hospital, Central South University, Changsha, China
Background: Since the coronavirus disease-2019 (COVID-19) outbreak, intensive care unit (ICU) healthcare workers were responsible for the critical infected patients. However, few studies focused on the mental health of ICU healthcare workers. This study aimed to investigate the psychological impact of COVID-19 on ICU healthcare workers in China.
Methods: We distributed the nine-item Patient Health Questionnaire (PHQ-9) and seven-item General Anxiety Disorder questionnaire (GAD-7) online to ICU healthcare workers in China. Respondents were divided into frontline and second-line according to whether they have contact with COVID-19 patients. Depressive and anxiety symptoms of all respondents were evaluated based on their questionnaire scores.
Results: There were 731 ICU healthcare workers finally enrolled in our study, including 303 (41.5%) male, 383 (52.4%) doctors, and 617 (84.4%) aged 26–45 years. All in all, 482 (65.9%) ICU healthcare workers reported symptoms of depression, while 429 (58.7%) reported anxiety. There was no significant difference between frontline (n = 325) and second-line (n = 406) respondents in depression (P = 0.15) and anxiety severity (P = 0.56). Logistic regression analysis showed that being female, ICU work time >5 years, and night duty number ≥10 were risk factors of developing depressive and anxiety symptoms. Income reduction was separately identified as risk of anxiety. Additionally, ICU work time >5 years was also identified as risk of developing moderate–severe depressive and anxiety symptoms.
Conclusions: Frontline ICU work was not associated with higher risk of depressive and anxiety symptoms during COVID-19 pandemic remission period in China. Actions like controlling night duty number, ensuring vacation, and increasing income should be taken to relieve mental health problem. Furthermore, we should pay close attention to those who had worked long years in ICU.
Introduction
In the winter of 2019, a novel coronavirus disease (coronavirus disease-2019, COVID-19) was first reported in Hubei province of China and gradually developed a global public health crisis; over 26 million people have been diagnosed with COVID-19 infection, and nearly 1 million died at the beginning of this in September. The COVID-19 was the third coronavirus disease in the 21st century after severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS); although the three coronavirus diseases shared similar transmission routes mainly by droplet and direct contact spread, the COVID-19 showed much higher infectivity (R0, 2.0–2.68) than SARS (R0, 1.7–1.9) and MERS (R0 <1) (1– 4). COVID-19 had a relatively long median incubation period of 5 days, and up to 50% patients with positive test results could be asymptomatic, which had been proved to be infectious (5–7). Moreover, COVID-19 caused a lower mortality rate of 2.2–3.5% compared to 9.5% for SARS and 34.4% for MERS, which led to less attention both from general population and certain governments (1, 8, 9). All these factors most likely contributed to the transmission of COVID-19. In the process of fighting COVID-19, intensive care unit (ICU) healthcare workers were responsible for the most critically infected patients, and many routine procedures in ICU including intubation, sputum aspiration, or use of nebulizers could be high risk due to the possible aerosol transmission (10). Furthermore, shortage of medical materials, work overload, and up to 50% mortality among severe infection patients in ICU bring mental burden to ICU healthcare workers (11). The experience of battling SARS had already shown adverse psychological impact on medical staff (12). During the COVID-19 pandemic, Kang's study also revealed a 28.6% moderate–severe mental health disturbance among 994 medical workers in Wuhan (13). Similarly, Lai's study reported symptoms of depression for 50.4%, anxiety for 44.6%, and insomnia for 34.0% among 1,021 medical workers in Hubei province and 236 outside Hubei province (14). All these information alerted more attention to mental health of medical workers. However, there were few mental health surveys specially designed for ICU healthcare workers. In order to find out the psychological effects of COVID-19 on ICU healthcare workers in China, we conducted this study.
Materials and Methods
Study Participants
This is a cross-sectional study performed via an online survey run from April 1 to April 8, 2020. The survey period corresponded to the pandemic mitigation period after prevalent peak stage of COVID-19 outbreak in China. We distributed self-administered questionnaires to ICU healthcare workers through an APP called Wenjuanxing (www.wjx.cn).
Before filling in the questionnaires, the respondents were required to fill in the informed consent form, promising that they were ICU medical workers in China and filled in the questionnaires voluntarily.
Questionnaires
The nine-item Patient Health Questionnaire (PHQ-9) and seven-item General Anxiety Disorder questionnaire (GAD-7) were used to assess depressive and anxiety symptoms. Meanwhile, basic demographic information including gender, age, occupation, education, ICU work time, hospital level, marriage, numbers of elderlies and children, vacation days, night duty number, frontline or second-line anti-pandemic work, labor, and income variation were also collected. Frontline anti-pandemic work was defined as contact with confirmed COVID-19 infections; in contrast, second-line was defined as no contact.
Mental Health Assessment
The PHQ-9 scale reflected symptom of depression, which consisted of nine questions each scored 0–3 according to respondents' answer. The final PHQ-9 total scores are categorized as follows: no depression (0–4), mild depression (5–9), moderate depression (10–14), and severe depression (15–27). Similarly, the GAD-7 scale reflected symptom of anxiety, which consisted of seven questions each scored 0–3. The final total scores are also categorized as follows: no anxiety (0–4), mild anxiety (5–9), moderate anxiety (10–14), and severe anxiety (15–21).
Statistical Analysis
Data analysis was performed using SPSS version 22.0 (SPSS Inc., Chicago, IL, USA). For count data, frequencies and percentages were used, and the chi-square test was used to compare the data for different categorical variables. Non-normalized distributed parameters were expressed as median (interquartile range), Mann–Whitney U-test was used to compare non-normalized distributed parameters. A P-value <0.05 was considered statistically significant. Multivariable logistic regression analysis was carried out to evaluate the association between mental health status and potential predictors, and variables were determined to contribute to the model if the significance level for the Wald inclusion test statistic was <0.05.
Results
Basic Demographic Characteristics
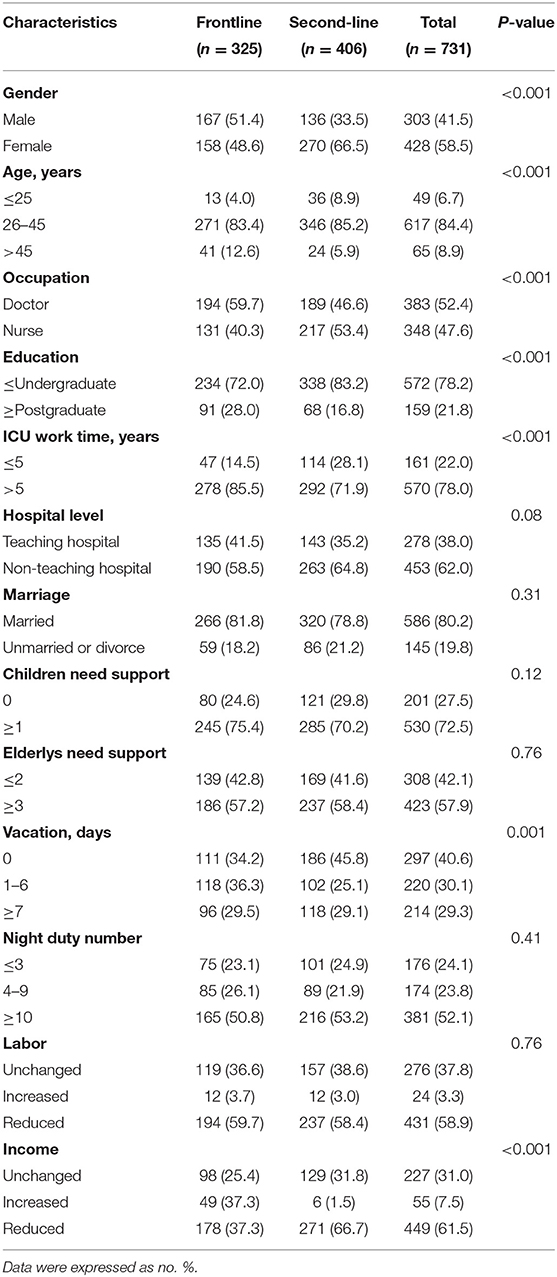
There were 731 ICU healthcare workers who were finally enrolled in our study, including 325 (44.5%) frontline and 406 (55.5%) second-line ICU healthcare workers. In all, 303 (41.5%) were male, 383 (52.4%) were doctors, 617 (84.4%) aged 26–45 years, 278 (38.0%) worked in teaching hospital, 570 (78.0%) had worked in current occupation for more than 5 years, 381 (52.1%) had night duty ≥10, and 449 (61.5%) experienced income reduction during the COVID-19 pandemic. ICU healthcare workers in the frontline were older (P < 0.001), higher educated (P < 0.001), higher paid (P < 0.001), had more working experience (P < 0.001), and more vacation days (P < 0.001); there were also more males (p < 0.001) and doctors (p < 0.001) in frontline group. Detailed basic demographic characteristics are shown in Table 1.
Mental Health Status
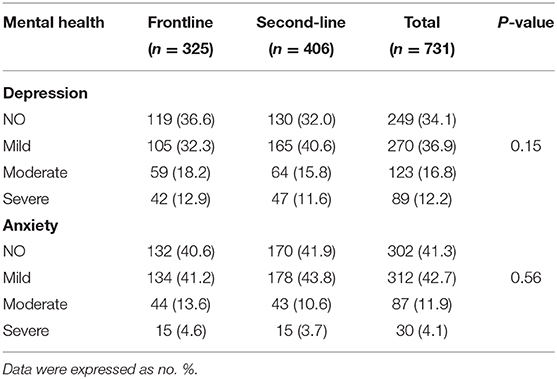
The severity of depressive and anxiety symptoms were categorized according to the PHQ-9 and GAD-7 scores. In this study, only 249 (34.1%) and 302 (41.3%) ICU healthcare workers were finally recorded to be free from depressive and anxiety symptoms, respectively. The rest of the ICU healthcare workers suffered from different degrees of depressive and anxiety symptoms. We further compared mental health status between frontline and second-line ICU healthcare workers, and no significant difference was found in the severity of depressive (P = 0.15) and anxiety (P = 0.56) symptoms. Detailed mental health information are shown in Table 2.
Influencing Factors of Mental Health
Four factors had been identified as being significantly associated with depression symptoms (Figure 1A): being female (OR, 1.74; 95% CI, 1.16–2.60; P = 0.008), ICU work time >5 years (OR, 1.84; 95% CI, 1.13–3.00; P = 0.02), vacation days ≥7 days (OR, 0.66; 95% CI, 0.44–0.99; P = 0.046), and night duty number ≥10 (OR, 1.91; 95% CI, 1.27–2.88; P = 0.002). We also identified six factors as being significantly associated with anxiety symptoms (Figure 1B): being female (OR, 1.48; 95% CI, 1.00–2.18; P = 0.048), ICU work time >5 years (OR, 2.20; 95% CI, 1.38–3.53; P = 0.001), vacation days ≥7 days (OR, 0.67; 95% CI, 0.45–1.00; P = 0.049), night duty number ≥10 (OR, 1.82; 95%CI, 1.22–2.71; P = 0.003), labor increase (OR, 0.38; 95% CI, 0.15–0.98; P = 0.046), and income loss (OR, 1.61; 95% CI, 1.12–2.30; P = 0.01). Additionally, we found ICU work time >5 years (OR, 1.91; 95% CI, 1.12–3.28; P = 0.02) and night duty number ≥10 (OR, 1.65; 95% CI, 1.06–2.57; P = 0.03) were risk factors of developing moderate–severe depressive symptoms (Figure 1C). ICU work time >5 years also helped to develop moderate–severe anxiety symptoms (OR, 2.05; 95% CI, 1.00–4.20; P = 0.049) (Figure 1D).
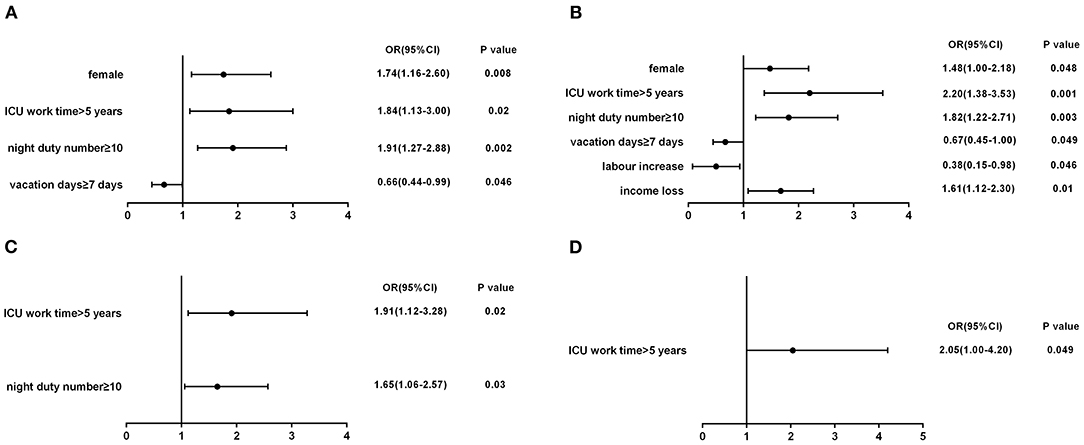
Figure 1. (A) Influencing factors of depression; (B) influencing factors of anxiety; (C) risk factors of moderate-severe depression; (D) risk factor of moderate-severe anxiety.
Discussion
On May 13th, the UN secretary general António Guterres stressed the adverse impact of COVID-19 pandemic on people's mental health, especially health care workers. Among all medical departments, ICU was responsible for the most critical COVID-19 cases, which might bring more mental burden to ICU healthcare workers. This is the first mental health study that examined the psychological impact of COVID-19 pandemic on ICU healthcare workers in China.
Our study revealed a high prevalence of mental disorders among 731 ICU healthcare workers; 65.9 and 58.7% respondents were finally screened symptoms of depression and anxiety, respectively, which were consistent with previous studies (13, 14). However, no significant mental health difference had been found between frontline and second-line ICU healthcare workers in our study. Neither did logistic regression identify frontline work as a risk factor of developing mental disorders. This was quite different from the experience of battling the SARS pandemic, which proved that medical workers who were exposed to SARS were associated with more mental health problems (15, 16). Moreover, Zhou's study also came to the distinct conclusion that frontline medical staff were more easily to suffer from psychological disturbances during the COVID-19 pandemic (17). We think our results could be explained as follows: firstly, frontline ICU healthcare workers in our study were older, higher educated, and there were also more males and doctors in the frontline group. Previously published studies had shown that male, doctors, older age, and higher education level were negatively associated with mental health problems among medical workers (14, 18–23). Additionally, ICU healthcare workers in the frontline were higher paid due to government's financial compensation and had more vacation days, which might help to relieve their mental distress.
Secondly, our study was performed from April 1, 2020 to April 8, 2020, when medical workers obtained enough knowledge about the virus and enough medical supplies especially personal protective equipment in China. According to Maunder's studies, confidence in protective measures could be positive to keep mental health (24). Skoda's study in German also exhibited a similar conclusion that more knowledge about COVID-19 will contribute to reduce psychological burden from the pandemic (23).
Besides, our study showed that being female, longer ICU work time, and more night duty were risk factors of developing depressive and anxiety symptoms, while more vacation days could be protective. Income reduction was separately identified as risk factor of anxiety symptoms. Our results reemphasized the damage of high workload on mental health of medical staff as Zhou's study pointed out (17). To be noted, work experience was generally considered to be beneficial to mental health when treating with emergency public health incidence (25); in our study, longer ICU work time was unexpectedly identified detrimental to maintain mental health. This could be explained by the high prevalence of occupational burnout among ICU healthcare workers especially for those who had worked long years in current occupation, since occupational burnout had been proved to be associated with depressive and anxiety symptoms (26–30). This result raised concern about occupational burnout among ICU healthcare workers with long years of working.
Conclusions
Our study had shown a high prevalence of depressive and anxiety symptoms among ICU healthcare workers. Frontline ICU work was not associated with higher risk of depressive and anxiety symptoms during the COVID-19 pandemic remission period in China. Actions like controlling night duty number, ensuring vacation, and increasing income should be taken to relieve mental health problem. Furthermore, we should pay more attention to those who had worked long years in ICU departments.
Limitations
Following limitations should be considered in our study. Data were obtained via anonymous, self-reported questionnaires online, and the sample size enrolled was relatively small, which would inevitably bring potential selection bias. The risk of COVID-19-related symptoms of depression and anxiety may be influenced by occupational burnout among ICU healthcare workers. Finally, the study only reflected mental health status during the short survey time when China broke through the extreme stress phase of the COVID-19 pandemic.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
XP designed the questionnaire, analyzed the data, and drafted the manuscript. XMe, LL, WL, CH, ZL, and XMa analyzed the data and revised the manuscript. ZZ, ZX, and BL designed the questionnaire and revised the manuscript. DX and LZ revised the manuscript. MP designed the study, analyzed the data, and revised the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Chen J. Pathogenicity and transmissibility of 2019-nCoV-A quick overview and comparison with other emerging viruses. Microbes Infect. (2020) 22:69–71. doi: 10.1016/j.micinf.2020.01.004
2. Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. (2020) 395:689–97. doi: 10.1016/S0140-6736(20)30260-9
3. Petrosillo N, Viceconte G, Ergonul O, Ippolito G, Petersen E. COVID-19 SARS and MERS: are they closely related? Clin Microbiol Infect. (2020) 26:729–34. doi: 10.1016/j.cmi.2020.03.026
4. Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. (2020) 55:105924. doi: 10.1016/j.ijantimicag.2020.105924
5. Arons MM, Hatfield KM, Reddy SC, Kimball A, James A, Jacobs JR, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. (2020) 382:2081–90. doi: 10.1056/NEJMoa2008457
6. Kimball A, Hatfield KM, Arons M, James A, Taylor J, Spicer K, et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility - King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:377–81. doi: 10.15585/mmwr.mm6913e1
7. Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. (2020) 172:577–82. doi: 10.7326/M20-0504
8. Bassetti M, Vena A, Giacobbe DR. The novel Chinese coronavirus (2019-nCoV) infections: challenges for fighting the storm. Eur J Clin Invest. (2020) 50:e13209. doi: 10.1111/eci.13209
9. Munster VJ, Koopmans M, van Doremalen N, van Riel D, de Wit E. A novel coronavirus emerging in China - key questions for impact assessment. N Engl J Med. (2020) 382:692–4. doi: 10.1056/NEJMp2000929
10. van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. (2020) 382:1564–7. doi: 10.1056/NEJMc2004973
11. Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, et al. Covid-19 in critically ill patients in the Seattle Region - case series. N Engl J Med. (2020) 382:2012–22. doi: 10.1056/NEJMoa2004500
12. Nickell LA, Crighton EJ, Tracy CS, Al-Enazy H, Bolaji Y, Hanjrah S, et al. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ. (2004) 170:793–8. doi: 10.1503/cmaj.1031077
13. Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. (2020) 87:11–7. doi: 10.1016/j.bbi.2020.03.028
14. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
15. Maunder RG, Lancee WJ, Rourke S, Hunter JJ, Goldbloom D, Balderson K, et al. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom Med. (2004) 66:938–42. doi: 10.1097/01.psy.0000145673.84698.18
16. Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. (2009) 54:302–11. doi: 10.1177/070674370905400504
17. Zhou Y, Wang W, Sun Y, Qian W, Liu Z, Wang R, et al. The prevalence and risk factors of psychological disturbances of frontline medical staff in china under the COVID-19 epidemic: workload should be concerned. J Affect Disord. (2020) 277:510–4. doi: 10.1016/j.jad.2020.08.059
18. Tang L, Pan L, Yuan L, Zha L. Prevalence and related factors of post-traumatic stress disorder among medical staff members exposed to H7N9 patients. Int J Nurs Sci. (2017) 4:63–7. doi: 10.1016/j.ijnss.2016.12.002
19. Chong MY, Wang WC, Hsieh WC, Lee CY, Chiu NM, Yeh WC, et al. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br J Psychiatry. (2004) 185:127–33. doi: 10.1192/bjp.185.2.127
20. Lung FW, Lu YC, Chang YY, Shu BC. Mental symptoms in different health professionals during the SARS attack: a follow-up Study. Psychiatr Q. (2009) 80:107–16. doi: 10.1007/s11126-009-9095-5
21. Matsuishi K, Kawazoe A, Imai H, Ito A, Mouri K, Kitamura N, et al. Psychological impact of the pandemic (H1N1) 2009 on general hospital workers in Kobe. Psychiatry Clin Neurosci. (2012) 66:353–60. doi: 10.1111/j.1440-1819.2012.02336.x
22. Goulia P, Mantas C, Dimitroula D, Mantis D, Hyphantis T. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infect Dis. (2010) 10:322. doi: 10.1186/1471-2334-10-322
23. Skoda EM, Teufel M, Stang A, Jockel KH, Junne F, Weismuller B, et al. Psychological burden of healthcare professionals in Germany during the acute phase of the COVID-19 pandemic: differences and similarities in the international context. J Public Health. (2020) 42:688–95. doi: 10.1093/pubmed/fdaa124
24. Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B, Evans S, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. (2006) 12:1924–32. doi: 10.3201/eid1212.060584
25. Chowell G, Abdirizak F, Lee S, Lee J, Jung E, Nishiura H, et al. Transmission characteristics of MERS and SARS in the healthcare setting: a comparative study. BMC Med. (2015) 13:210. doi: 10.1186/s12916-015-0450-0
26. Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. An official critical care societies collaborative statement-burnout syndrome in critical care health-care professionals: a call for action. Chest. (2016) 150:17–26. doi: 10.1016/j.chest.2016.02.649
27. Shenoi AN, Kalyanaraman M, Pillai A, Raghava PS, Day S. Burnout and psychological distress among pediatric critical care physicians in the United States. Crit Care Med. (2018) 46:116–22. doi: 10.1097/CCM.0000000000002751
28. Embriaco N, Papazian L, Kentish-Barnes N, Pochard F, Azoulay E. Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care. (2007) 13:482–8. doi: 10.1097/MCC.0b013e3282efd28a
29. Tan B, Kanneganti A, Lim L, Tan M, Chua YX, Tan L, et al. Burnout and associated factors among health care workers in Singapore during the COVID-19 pandemic. J Am Med Dir Assoc. (2020) 21:1751–8.e5. doi: 10.1016/j.jamda.2020.09.035
Keywords: COVID-19, ICU, mental health, depression, anxiety
Citation: Peng X, Meng X, Li L, Hu C, Liu W, Liu Z, Ma X, Xu D, Xing Z, Zhu Z, Liu B, Zhang L and Peng M (2021) Depressive and Anxiety Symptoms of Healthcare Workers in Intensive Care Unit Under the COVID-19 Epidemic: An Online Cross-Sectional Study in China. Front. Public Health 9:603273. doi: 10.3389/fpubh.2021.603273
Received: 22 September 2020; Accepted: 11 January 2021;
Published: 05 March 2021.
Edited by:
Wulf Rössler, Charité – Universitätsmedizin Berlin, GermanyReviewed by:
Madeleine Fink, LVR Krankenhaus Essen, GermanyZezhi Li, Shanghai JiaoTong University, China
Benjamin Tan, National University Hospital, Singapore
Copyright © 2021 Peng, Meng, Li, Hu, Liu, Liu, Ma, Xu, Xing, Zhu, Liu, Zhang and Peng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Milin Peng, pengmilin@csu.edu.cn
 Xiaofan Peng
Xiaofan Peng Xiangyu Meng
Xiangyu Meng Li Li1
Li Li1 Wei Liu
Wei Liu Bangshan Liu
Bangshan Liu Milin Peng
Milin Peng