- 1Center for Community Health Alignment, The University of South Carolina Arnold School of Public Health, Columbia, SC, United States
- 2Center for Applied Research and Evaluation, The University of South Carolina Arnold School of Public Health, Columbia, SC, United States
- 3Baylor Scott & White Health, Dallas, TX, United States
Introduction: Community health workers (CHWs) are critical members of the public health workforce, who connect the individuals they serve with resources, advocate for communities facing health and racial inequities, and improve the quality of healthcare. However, there are typically limited professional and career building pathways for CHWs, which contribute to low wages and lack of career advancement, further resulting in turnover, attrition, and workforce instability.
Methods: The Center for Community Health Alignment (CCHA), within the Arnold School of Public Health at the University of South Carolina, utilized a mixed-method data collection strategy to provide a more in-depth understanding of this issue and ways that employers, advocates, and CHWs can address it.
Results: Themes across data sources emphasized the importance of retaining skilled and experienced CHWs and educating other health professions about CHWs' critical roles, and reported that doing so will result in decreased attrition professional growth, and improved program quality. CHWs and allies concluded that higher wages, valuing lived experience over formal education, and participation in additional training opportunities should be the primary factors considered for career advancement.
Discussion: Utilizing input from experienced CHWs and CHW allies nationally, this article describes the importance of supporting CHW career advancement, shares best practices, and suggestions for designing strategies that organizations/employers can use to improve CHW career pathways to better support the CHW workforce and reduce attrition.
1. Introduction
There is growing recognition of how community health workers (CHWs) make significant impacts on the health and wellbeing of individuals and communities most affected by inequities (1–8). The American Public Health Association (APHA) definition of a CHW, endorsed by the National Association of CHWs (NACHW), is “a frontline public health worker who is a trusted member of and/or has an unusually close understanding of the community served. This trusting relationship enables the worker to serve as a liaison/link/intermediary between health/social services and the community to facilitate access to services and improve the quality and cultural competence of service delivery (9).”
Several systematic reviews and randomized control trials have found CHWs are associated with improved health outcomes in diabetes (10–13), multiple chronic diseases (14–16), cardiovascular risk reduction (17), hypertension (18), cancer screenings (19, 20), asthma (21), and mental health (22). CHWs help healthcare to accomplish the “Triple Aim” by contributing to improved care experiences and outcomes while maintaining cost-effectiveness (17, 19, 23–28). In addition, CHWs can contribute to enhancing the quality and cultural responsiveness of health and social services and support system-level changes that can have long-lasting impact (29).
While CHWs have been working in the United States for generations, during the recent 20 years, professional institutions have increasingly recognized their role and value in addressing health needs and gaps. In 2002, one of the Institute of Medicine's findings in their “Unequal Treatment” report was “Community Health Workers offer promise as a community-based resource to increase racial and ethnic minorities' access to health care and to serve as a liaison between healthcare providers and the communities they serve (2).” In 2010, the U.S. Department of Labor created a “Standard Occupational Classification” for CHWs, 21-1094. Furthermore, in 2010, the Patient Protection and Affordable Care Act mentioned CHWs 14 times, identified CHWs as a healthcare profession, and called for funding allocation for health promotion among underserved populations (30). During the COVID-19 pandemic, institutions such as the U.S. Centers for Disease Control and Surveillance (CDC) have funded and collaborated with CHWs to provide health outreach and education to hard-hit communities (31). Similarly, in 2022, the American Rescue Plan awarded over 220 million dollars toward community health worker training and capacity building nationwide (32).
As frontline public health workers during the COVID-19 pandemic, CHWs played important roles including communicating COVID-19 prevention and vaccination information to their communities in culturally responsive terms (33), as well as assisting in navigating the overwhelmed healthcare system and connecting clients to virtual medical care and mental health services (34). They also had a critical role in helping people address the myriad of social needs that the pandemic raised. As a result of the increased need in healthcare and public health spaces, coupled with increased evidence of effectiveness, the community health worker workforce is evolving rapidly in terms of professional identification and institutional recognition.
In practice, “CHW” is an umbrella term that encompasses dozens of titles, including peer health advisor, care navigator, outreach worker, community health representative, promotores, and more. This multitude of titles is one factor that has affected the potential consolidation of the role into a recognizable and definable profession (35). To address this, the CHW Core Consensus Project (C3 Project), building off the 1998 National Community Health Advisor Study, defined a set of core CHW roles and competencies in 2016 that CHW membership associations, public health institutions, and several states have endorsed (36).
The C3 Project and its predecessors identified CHWs' “connection to the community served” as their “most critical quality” (36). CHW employers prioritize this quality to identify and hire CHWs, more so than levels of formal education or years of employment experience. However, the latter forms the basis for how many institutions and organizations calculate salaries within their compensation and promotion structures. The result is that CHWs often have low salaries and status in the workplace and few opportunities for professional growth without leaving the profession.
The National CHW Common Indicators Project, a multi-institution national initiative to synthesize and improve CHW evaluation, highlights the importance of CHW workforce conditions and career advancement via two indicators. Indicator #1 is “CHWs' level of compensation, benefits, and promotion,” prioritizing this as an indicator of program quality. Indicator #12 is “Supportive and Reflective Supervision,” with CHWs recognizing this as, “...crucial factors affecting the ability of CHWs to grow as professionals, experience job satisfaction, and effectively promote health in their communities.” Considering that the improvement of the CHW work environment is reflected in two priority indicators for CHW success, pathways for advancement should be more clearly defined and incorporated into the workflow of organizations that employ CHWs.
The literature on the CHW workforce is growing, yet still somewhat limited. Global literature identifies high attrition rates for CHWs, with contributing factors including low and inconsistent salaries, lack of support, and leaving for better positions (37–45). In a systematic review, Kok et al. found professional growth as a motivating factor for CHWs, and a lack of career advancement options as a demotivating one (46).
In the United States, CHW attrition rates can also be high, with low salaries, low professional status, and lack of opportunities for professional growth driving dissatisfaction (47, 48). Farrar et al. (48) found that addressing barriers to education, training, and promotion led to an improvement in job satisfaction for CHWs. Anabui et al. (47) found that despite the challenges faced in the workplace, most CHWs want to retain their identities, rather than move to other health or helping professions for advancement. They found that clear criteria and opportunities for promotion within their field, including incentives that recognize lived experiences, were motivating for CHWs.
While NACHW, APHA, and the C3 Project have defined CHWs' roles, skills, and qualities, and many state CHW associations have established core competency training and certifications, there is minimal standardized guidance around best practices for hiring or promoting CHWs. Existing guidance emerged from the 1998 National Community Health Advisor (NCHA) Study, which recommended 18 qualities that employers should seek when hiring CHWs. This guidance, although not commonly adopted, could be built upon and shared to promote the enhancement of the CHW workforce. Opportunities for advancement are particularly critical for CHWs, many of whom are themselves from (or closely tied to) populations experiencing inequities, such as members of racial minority groups, immigrants, people with low income, people who were formerly incarcerated, or people in recovery. Lack of mobility may perpetuate their economic and social vulnerabilities.
The purpose of this project was to gather and synthesize first-hand perspectives from CHWs and their allies on this workforce challenge. By collecting CHW input from multiple sources, we describe why it is important to support CHW career advancement, and what employers and advocates can do to develop CHW career tiers or advancement strategies and reduce the threat of losing this vital workforce at a time when the need for their work and expertise has become even more evident.
2. Methods
With support from Johnson & Johnson, in line with their Our Race to Health Equity initiative (49), the Center for Community Health Alignment's Community Health Worker Institute (CHWI) and Center for Applied Research and Evaluation (CARE) at the University of South Carolina Arnold School of Public Health (ASPH) gathered insight from four sources for this project: qualitative data from the South Carolina CHW Ambassadors and CHW Best Practices Council; the National Association of CHWs' (NACHW) 2021 Annual CHW Workforce Survey, a rapid-feedback session of CHWs at the NACHW Unity Conference; and qualitative interviews with six CHW managers or supervisors. The Institutional Review Board at the University of South Carolina approved the study.
2.1. The South Carolina CHW ambassadors and CHW best practices council
A foundational component of CHWI is its engagement of a team of “CHW Ambassadors,” experienced CHWs representing a variety of races, ethnicities, geographical locations, populations served, and organizational affiliations. In 2019, the CHWI team selected 10 applicants to be the first cohort of CHW Ambassadors. They contributed to developing plans and strategies for CHW training, capacity building, data collection, and other critical components of CHWI's mission. In addition to the Ambassadors, CHWI invited seven CHW managers or supervisors to be part of a CHW Best Practices Experts Council, whose goal was to determine best practices for implementing and developing CHW programs and growing the CHW workforce in South Carolina effectively. The input from the Best Practices Expert Council on the need for CHW career advancement and a tiered certification structure was the primary impetus for this study. For a year, the council met six times to discuss job descriptions and the factors that should merit increased benefits, recognition, pay, and leadership opportunities for CHWs. The Council discussed various viewpoints until a consensus was reached.
2.2. NACHW's 2021 National CHW workforce survey
The National Association of CHWs (NACHW) invited key influencers, funders, and CHWs leaders to join workgroup sessions toward developing this survey. The workgroup conducted extensive literature review searches, cross-referenced keywords, and identified knowledge gaps regarding the profession. CHWI collaborated with NACHW and its team of CHW advisors to add three additional questions regarding career advancement to the 51-question survey. The survey launched in June 2021, and collected responses through September 2021, ultimately compiling 867 completed surveys (772 in English and 95 in Spanish).
2.3. A rapid feedback session at the 2021 NACHW annual Unity Conference
In July 2021, 160 CHWs and CHW allies attended an invited session at the virtual NACHW Unity Conference, titled “CHWs' Career advancement strategies: Nothing about us without us.” Two CHW leaders from the Center for Community Health Alignment conducted the session, which was in English. The facilitators posed open-ended questions about CHW career pathways and collected responses via Mentimeter, an online polling platform. In total, 80 individuals responded to four questions posed in a rapid-polling activity. Among attendees that responded to the poll, 70 (87%) identified as CHWs, and 10 (13%) as CHW allies (a supporter, an employer, or a researcher of CHWs). Of CHWs, 35% had been a CHW for more than 5 years, 18% for < 1 year, and 36% between 1 and 4 years. Most of the CHWs and allies worked in a healthcare setting (34%) or a community-based organization (33%). Others worked in a public health department (9%), university (9%), or CHW organization or association (8%). Participants did not divulge their geographical locations. The questions were either open-ended or multiple choice and were collected and organized by themes using a deductive approach.
2.4. Individual interviews
Members of the research team conducted six semi-structured interviews with CHWs that are managers or supervisors of other CHWs. The interview guide consisted of several open-ended questions about the CHW career paths at their organizations. Topics included CHW compensation, promotion opportunities, and ways to support future CHWs in career progression. Four CHW managers were from South Carolina organizations, with another from Chicago, Illinois, and one from Dallas, Texas. Three managers worked in community-based settings, while the others worked in healthcare settings. Interviews were conducted via the Zoom telecommunication platform. CHWI recruited interviewees based on their knowledge of the CHW profession and experience managing CHW teams. To protect participant privacy, recordings, transcriptions, and analyses were de-identified and stored on a private cloud-based drive. In recognition of their content expertise, participants received a stipend for their participation. The interviews were transcribed using Otter.ai software.
To analyze data, information was coded and analyzed for themes using Microsoft Excel (50, 51). The study team used the constant comparative method (52). As a group, we read through each transcript, noted emergent themes, and compared themes identified in previous transcripts. Furthermore, the study team discussed various viewpoints between team members until a consensus was reached.
3. Results
Several themes emerged across the data sources regarding the need to advance the CHW workforce (the “why”) including the importance of retaining skilled CHWs, building respect and appreciation for the profession, and professional growth that will improve program and organizational quality. The themes about the development of opportunities for CHW advancement (the “how”) included the importance of salary improvement, making advancement decisions based on lived experience more than formal education, and providing opportunities for additional CHW training and professional development. The responses to the NACHW workforce survey are listed in Tables 1, 2, and Unity Conference session feedback is in Tables 3–5.
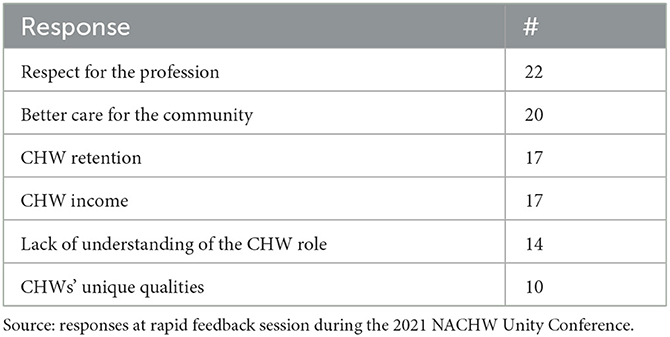
Table 3. Most frequently appearing codes for responses to open-ended question, “Why is more attention needed on CHW career advancement options?”

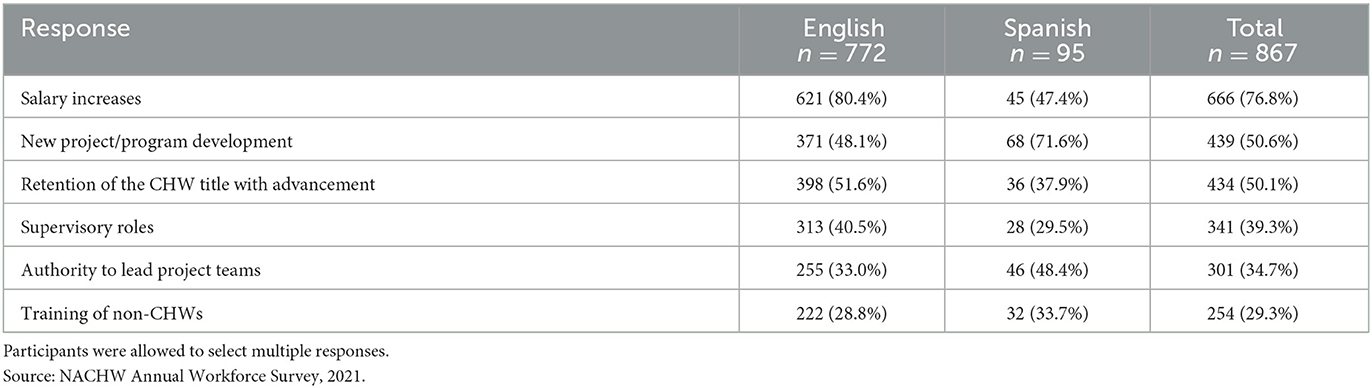
Table 4. Benefits CHWs believe should be available as they advance in their careers, in descending order.
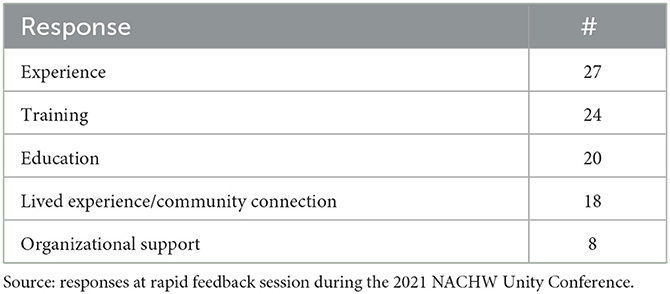
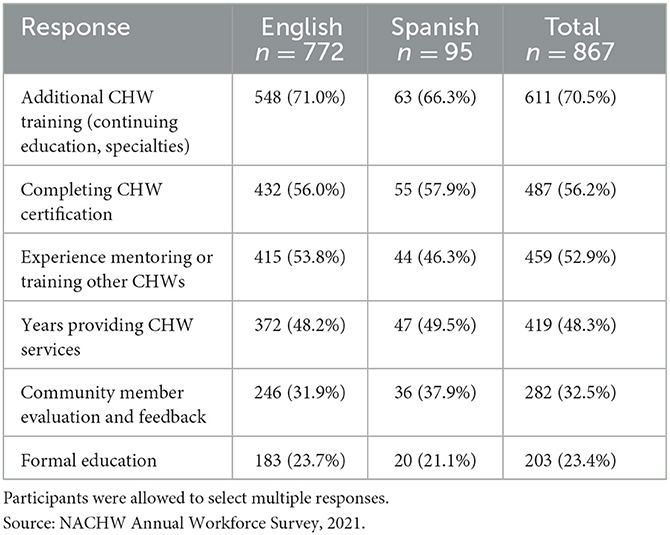
Table 5. Most frequently appearing codes for responses to open-ended question, “What factors need to be considered to move CHWs from one level to the next?”
3.1. CHW advancement is critical: “The why”
3.1.1. Retention
Studies about CHW attrition found that a lack of opportunities for professional growth contributes to turnover rates (47, 48). This is reflected in our findings, first emerging from the CHW Best Practices Council, which identified that the lack of advancement opportunities caused many CHWs to leave the field. They advocated that employers of CHWs and the South Carolina CHW Credentialing Council make CHW retention a high priority by developing tiered levels of certification.
Participants at the Unity Conference agreed, “Having more options for career advancement generally means more people staying in the field, only becoming better at what they do, with the pay they deserve, helping as much people as they can.” Another said, “Because the way things are now, we are losing strong CHWs from the field. Those that are most connected to the community are now removed which causes a loss of trust.”
3.1.2. Respect for the CHW position
The relationship between CHW advancement and a perceived lack of respect from other professionals emerged at the Unity Conference (Table 3). One CHW stated, “We are treated like housekeeping... a necessary position that is undervalued.” Another respondent said, “We are living in poverty, have skills and experience and education, but are trapped, underpaid and underappreciated with no hope of improvement; we are dedicated missionaries.” Another wrote, “Because for many companies [the CHW profession] is an unknown field and they do not understand how valuable CHWs are and don't know what to do with us.” Yet another stated, “I think people believe it's just volunteer work.”
The interviewed managers agreed. One manager stated, “Yeah, I just think the... [profession]... is brand new. Like, we are learning about all the benefits that our work offers to the community. … We need to create awareness to the funders about the value that we provide to the community and to the medical services and the government, how much money they saved… I think like doing research, like a study of the return on investment… real numbers that you can show to the funders, so they can see the benefit of our profession.” Another suggested that awareness building is an important role for CHW allies, “Continue to work and push work with organizations, to develop Community Health Worker programs, and help them to understand the role of Community Health Workers and why they're important, continue to advocate for Community Health Worker pay.” Educating other professionals and team members about the role of CHWs will help showcase their value in the workplace, further incentivizing them to stay and grow.
3.1.3. Professional growth and quality improvement
The interviewees also mentioned that CHWs' professional growth will ultimately result in improved services to patients and participants. “We all want to get better all the time and, and make more money, and just think that you are growing, that you are learning, and that you are growing in your profession. Just like it is good for us and it motivates you to have like a better position, a better salary. I think that's important for everybody.” Another interviewee stated, “Oh, it gives them something to strive for, it gives them something to look forward to, you know, I'm saying it allows them to take the initiative to improve themselves, in professional development.”
3.2. Factors to consider when developing CHW advancement pathways: “The how”
3.2.1. Salary
Across data sources, CHWs identified “salary increases” as the most important factor to consider in advancement opportunities. “Higher salary” was the most frequently mentioned priority for CHWs in both the NACHW Workforce Survey (Table 1) and the Unity Conference session (Table 4) when asked what should be incorporated into advancement pathways. One conference attendee commented, “CHWs are often one paycheck away from needing the services we provide.”
The CHW managers are aware of the impact of low salaries on their CHWs; one said, “It's just I have been advocating for my team to get a better salary, but it is very hard for us to get the resources. … I really would like to have more for my Community Health Workers because they work so hard. And they really deserve to have a better salary.” However, they also deal with the challenges of finding funding sources for those salaries. One manager said, “You know how it works when you work with grants, you have this person for 1 year and she learned so many things, she's gained so many skills, and then she has to leave because I don't have any more funds.” Two CHW managers suggested institutional funds or insurance payments be aligned with CHW services. One suggested, “Oh, that's the biggest challenge for me that I would really like... maybe the hospitals to take over these programs and say, ‘okay, I'm going to pay you like, to permanently to do the work.”' Another mentioned, “[A] patient came in, and we assisted them with food insecurity, boom, that should be a code. Right? That should be a compensation point.”
3.2.2. Valuing lived experience above formal education
At the Unity conference session, many responses to the question, “What factors should be considered to move CHWs from one level to the next?” were related to experience as CHWs and lived experience as a member of the communities served (Table 5). Answers to the question included, “Respecting experience and not just the letters after your name,” and “Experience in the field and the resources we bring... how we are respected in the community.” One CHW said, “Because CHW's speak in everyday people's language! That's why what we do works!”
Multiple interviewed CHW managers agreed they would hire or promote other CHWs based on lived experience. One manager stated, “So I struggle with that sometimes, because I sometimes do get caught in okay, what kind of education do they have? … But then I had to, I had to catch myself sometimes. That's not what is at the heart of a Community Health Worker. It's the community. It's the person. Its, you know, what role have they played in their community?” When asked what factors are important in promoting CHWs, another CHW manager stated that, “experience dealing with the population that we're trying to target… and being able to meet those patients where they're at,” was important. Another manager said, “I found out some of the ones, you know, that that didn't have that that degree or, or may not always have had a medical experience are the best ones.”
The value of lived experience and community connections contrasts with many employing institutions' emphasis on formal education and credentials. In the NACHW workforce survey, when asked about barriers to their success as CHWs, 25% of CHWs identified higher-level education and 21% “other credentials” (53). CHWs have deep knowledge and experience in the community; determining how to place value on this quality in an institutional setting is critical.
3.2.3. CHW training and professional development
While most respondents did not prioritize associating CHW advancement with formal education, there is a theme of wanting CHW training, professional development, and certification as means of advancing. The CHW Best Practices Council recommended that additional CHW-focused education and experience should help move a CHW from one tier to the next.
The national survey respondents agreed; CHWs ranked “additional CHW training” as the top factor to be valued in their career paths (Table 2). This was followed by CHW certification, then experience mentoring other CHWs. An interviewee also agreed, suggesting training as a method of supporting CHW advancement, “I would say continue to provide educational pathways for Community Health Workers, professional development.” Another interviewee suggested that organizations should, “…assess company needs and provide training and education.”
4. Discussion
These findings show that more effective and equitable career pathways for CHWs would provide motivation for CHWs to remain in the workforce, promote retention, recognize effective work and leadership, and contribute to organizational quality improvement. CHW career advancement pathways should recognize the unique contributions of CHWs to health improvement, take into consideration the best practices offered by the workforce, and support CHWs in addressing the challenges and barriers that exist.
In the past few years, a growing number of institutions and organizations have realized the need to hire and integrate CHWs into their work. However, the CHW field faces multiple threats that can result in attrition and burnout and put the workforce and employers at risk of not being able to meet the growing demand. CHWs have reported feeling undervalued, underpaid, and not respected. By not providing opportunities for CHWs to grow in their field, organizations risk losing those CHWs with the most experience, as opposed to building on that expertise to support newer CHWs.
4.1. Challenges to be addressed
The barrier that was most frequently mentioned by CHWs and CHW allies was funding, both in terms of having enough funding to offer higher salaries and having sustainable funding so that positions are not dependent on grants and other one-time funding sources. Due to the value of CHWs' lived experience and connection to the populations they serve, CHWs can be at high risk of poverty, which makes offering livable wages essential. In addition, time limited and insufficient compensation pose substantial risks to the CHW workforce. Our findings suggest that having more sustainable and equitable funding will facilitate the retention of CHWs.
Another major challenge pertains to human resource systems and processes placing value on higher education and formal degrees rather than lived experience. Foremost, higher education can be financially cumbersome for CHWs, many of whom hail from marginalized populations. Similarly, CHW managers, CHWs, and the C3 Project agree that lived experience is a core quality of a CHW. Therefore, loosening requirements surrounding formal education and valuing lived experience can assist in finding and promoting the right individuals for CHW positions. It can also assist in building financial equity for CHWs because they will have opportunities for advancement without incurring additional debt. Further emphasis needs to be placed on understanding and dismantling systemic racism within organizations due to the part that it plays in maintaining hierarchical leadership that keeps those with privilege in power. The role of privilege and power dynamics needs to be recognized and addressed in order to determine paths to leadership that are more equitable, open, and transparent.
Finally, there is a need for more awareness of CHW's roles and contributions to public health and healthcare. Many stated that employers such as hospitals and state or federal agencies lack awareness of the roles, qualities, and importance of CHWs. Similarly, community members may not understand the role of a CHW. Developing strong communication plans that include training employers and marketing to the public can assist in raising awareness of the CHW profession, creating more respect for the CHW role and scope, helping keep experienced CHWs in the workforce, and incentivizing others to join the field.
4.2. Designing CHW advancement pathways
Almost all CHWs and allies reported that most CHWs want to stay in and be able to progress within their field, as opposed to having to leave the CHW workforce to pursue additional opportunities. However, many CHWs stated that employers will not allow them to progress without adopting a new title or professional identity. Developing a tiered CHW advancement framework, such as the ones in the case examples included, can guide employers and advocates in their efforts to promote and retain CHWs. Advancement factors can include additional training, professional development, certifications, mentorship of other CHWs, years in the CHW field, and the quality of their work. CHWs strongly favor their profession's own training, certification, and experience as factors for advancement, more than formal education or external qualifications. Upon advancing, CHWs should be granted opportunities to participate in leadership roles, mentorship, program design, and advocacy.
4.3. Examples
Later are two examples of organizations that have created and implemented CHW career advancement pathways, with strong and intentional input from CHWs.
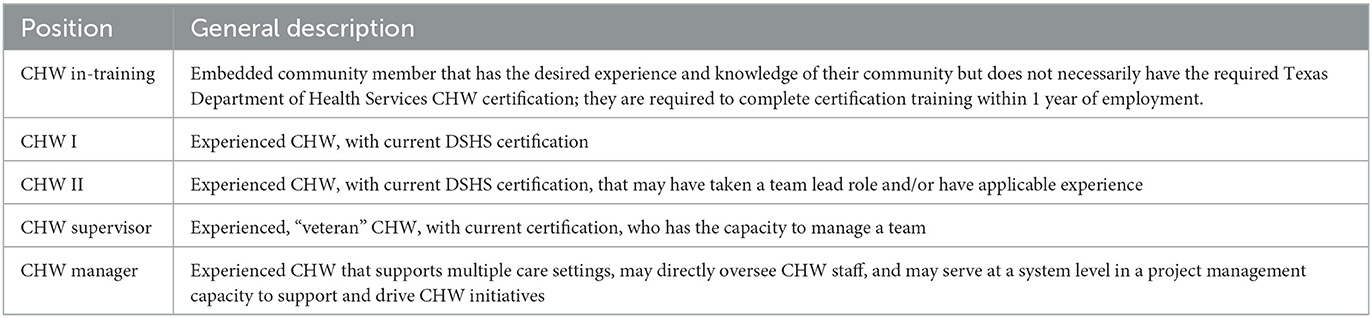
4.3.1. CHW tiered system at Baylor Scott & White Health
Baylor Scott & White Health (BSWH), the largest not-for-profit healthcare system in Texas and one of the largest in the United States, employs CHWs to help patients navigate an increasingly complex healthcare system, facilitate self-management of chronic diseases, and connect patients to primary care medical homes. BSWH CHWs act as peers, navigators, advocates, educators, and promoters of improving outcomes and quality of life for the patients they serve.
In 2007, BSWH hired one CHW as a diabetes educator. In 2009, the team expanded to four CHWs through the Diabetes Equity Project, and in 2011, BSWH created new positions, marking the start of BSWH's current CHW career ladder efforts. Between 2011 and 2014, the integration of CHWs expanded even more through various grant and funding opportunities.
As the system developed more CHW programs, CHW supervisors recognized the need for a systemic approach to CHW support that could bridge the programs. They created the CHW Development Council to meet this need. This Council utilized key data derived from annual workforce feedback surveys at the BSWH CHW Summit and the Texas core competencies for public health professionals to build a career ladder. Rather than encouraging BSWH CHWs to pursue growth through other career ladders such as becoming social workers or other healthcare professionals, they determined it was more effective and supportive to build a CHW career ladder that respects the CHWs' passion and path, thus allowing BSWH to retain talented and invaluable CHWs at all levels for the last decade.
The CHW Development Council developed the advancement levels in Table 6 and provided the levels to supervisors as a framework they can use to help grow and retain their CHWs. Currently, BSWH employs over 120 CHWs.
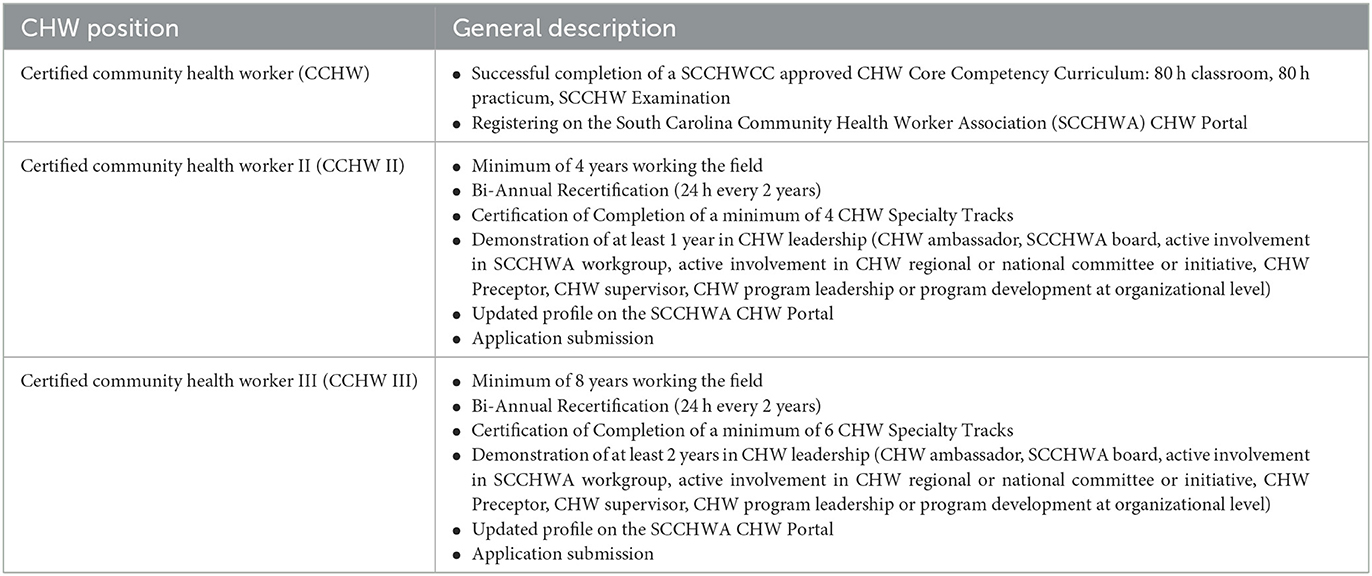
4.3.2. South Carolina CHW tiers
As previously mentioned, the South Carolina CHW Best Practices Council (BPC) identified CHW career advancement as a high priority for the CHW workforce in South Carolina. The South Carolina CHW Credentialing Council (SCCHWCC), which is supported by the South Carolina Community Health Worker Association, is the statewide approving body for CHW training programs, certification, and continuing education. The SCCHWCC is composed of at least 51% CHWs, along with representatives from the state Medicaid institution, the state public health department, AHEC, higher education, and a health insurance entity.
The BPC worked to draft examples of tiered CHW job descriptions, based on the different requirements for the position. The Council also recommended that, statewide, there should be multiple tiers of CHW certification, and that additional CHW-focused education and experience should be what help move a CHW from one tier to the next.
Based on the work initiated by the BPC, CHWCC made enhancements to the CHW credentialing process, creating a three-tiered system for certified CHWs. The Credentialing Council drafted these tiers and reviewed them multiple times with the BPC. In April 2022, the three-tiered certification in Table 7 was approved and it was launched in January 2023. In the future, efforts will be made to educate employers on the certification tiers, to encourage them to adopt them, along with appropriate advancement in salaries and opportunities for CHWs.
4.4. Limitations
Limitations of this study include a lack of consistency across data sources; the questions were similar, but not identical. To address this, the team gathered data from multiple sources to make sure the themes were accurate and consistent.
Respondents of the national CHW survey may have been impacted by survey fatigue bias, due to the length of the questionnaire. In addition, the interviews and Unity Conference sessions were in English. Aligning interview data of Spanish speakers with the survey data could have brought more insight to researchers around the differences between how English and Spanish-speaking CHWs are employed and promoted. Further research can be conducted in various languages and with CHWs from different backgrounds to determine if there are nuances in factors affecting CHW advancement.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by University of South Carolina Institutional Review Board. The NACHW survey and conference poll were anonymous, and did not require written consent. Individual interview participants provided their verbal consent to participate in this study.
Author contributions
JS and MY designed the study and led data collection. JN and SC-K contributed to analyzing the data and preparing the manuscript. AR reviewed for relevancy to the field and provided case study input. All authors contributed to the article and approved the submitted version.
Funding
Funding to support this study was provided by Johnson & Johnson.
Acknowledgments
We would like to express appreciation to all the CHWs who participated in interviews and shared their ideas and opinions on this topic, and the allies that provided input at the 2021 Unity Conference. In particular, we want to thank the following CHWs who participated in the CHW Best Practices Council or contributed their expertise to the project: Yajaira Benet-Uzcategui, Marek Calhoun, Bonita Clemons, Nora Curiel, Whitney Davis, Barb Dendy, Vanessa Earle, Ashley Ford, William Garrett, Andrea Heyward, Cartia Higgins, Kim Jay, Terri Jowers, Renee Linyard-Gary, Donna Mack, Maria Martin, Reeshemah McKelvey, Chief Michelle Mitchum, Agner Muñoz, Rebekah Shilling, and Virginia Berry White. We would also like to thank the South Carolina CHW Credentialing Council and Baylor Scott & White Health for sharing their career advancement models and LaSheba Boyd for assisting with data collection.
Conflict of interest
AR was employed by Baylor Scott & White Health.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Shantharam S, Andrade N, Bhatt A, Bostic M, Chase A, Fulmer E, et al. Best Practices for Heart Disease and Stroke: A Guide to Effective Approaches and Strategies. Atlanta, GA: Centers for Disease Control and Prevention (2022).
2. Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press (2003).
3. Heart Disease Stroke Prevention: Interventions Engaging Community Health Workers: Community Preventive Services Task Force. (2017). Available online at: https://www.thecommunityguide.org/media/pdf/HDSP-CHW-508.pdf
4. Diabetes Management: Interventions Engaging Community Health Workers. Community Preventive Services Task Force Finding and Rationale Statement. (2017). Available online at: https://www.thecommunityguide.org/sites/default/files/assets/Diabetes-Management-Community-Health-Workers.pdf
5. Diabetes Prevention: Interventions Engaging Community Health Workers: Community Preventive Services Task Force. (2016). Available online at: https://www.thecommunityguide.org/sites/default/files/assets/Diabetes-Prevention-Community-Health-Workers.pdf
6. Cancer Screening: Interventions Engaging Community Health Workers - Breast Cancer; Community Preventive Services Task Force Finding Rationale Statement. (2019). Available online at: https://www.thecommunityguide.org/sites/default/files/assets/Breast-Cancer-Screening-CHW-508.pdf
7. Cancer Screening: Interventions Engaging Community Health Workers - Cervical Cancer; Community Preventive Services Task Force Finding Rationale Statement. (2019). Available online at: https://www.thecommunityguide.org/sites/default/files/assets/Cervical-Cancer-Screening-CHW-508.pdf
8. Cancer Screening: Interventions Engaging Community Health Workers - Colorectal Cancer; Community Preventive Services Task Force Finding Rationale Statement. (2019). Available online at: https://www.thecommunityguide.org/content/tffrs-cancer-screening-interventions-engaging-community-health-workers-colorectal-cancer
9. Community Health Workers: American Public Health Association. Available online at: https://www.apha.org/apha-communities/member-sections/community-health-workers
10. Gary TL, Bone LR, Levine DM, McGuire M, Saudek C, Brancati FL. Randomized controlled trial of the effects of nurse case manager and community health worker interventions on risk factors for diabetesrelated complications in urban African Americans. Prevent Med. (2003) 37:23–32. doi: 10.1016/S0091-7435(03)00040-9
11. Palmas W, March D, Darakjy S, Findley SE, Teresi J, Carrasquillo O, et al. Community health worker interventions to improve glycemic control in people with diabetes: a systematic review and meta-analysis. J Gen Intern Med. (2015) 30:1004–12. doi: 10.1007/s11606-015-3247-0
12. Perez-Escamilla R, Damio G, Chhabra J, Fernandez ML, Segura-Perez S, Vega-Lopez S, et al. Impact of a community health workers-led structured program on blood glucose control among latinos with type 2 diabetes: the DIALBEST trial. Diabetes Care. (2015) 38:197–205. doi: 10.2337/dc14-0327
13. Spencer MS, Rosland A-M, Kieffer EC, Sinco BR, Valerio M, Palmisano G, et al. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. Am J Public Health. (2011) 101:2253–60. doi: 10.2105/AJPH.2010.300106
14. Kangovi S, Mitra N, Grande D, Huo H, Smith RA, Long JA. Community health worker support for disadvantaged patients with multiple chronic diseases: a randomized clinical trial. Am J Public Health. (2017) 107:1660–7. doi: 10.2105/AJPH.2017.303985
15. Kangovi S, Mitra N, Grande D, White ML, McCollum S, Sellman J, et al. Patient-centered community health worker intervention to improve posthospital outcomes: a randomized clinical trial. JAMA Intern Med. (2014) 174:535–43. doi: 10.1001/jamainternmed.2013.14327
16. Kennedy MA, Hatchell KE, DiMilia PR, Kelly SM, Blunt HB, Bagley PJ, et al. Community health worker interventions for older adults with complex health needs: a systematic review. J Am Geriatr Soc. (2021) 69:1670–82. doi: 10.1111/jgs.17078
17. Kim K, Choi JS, Choi E, Nieman CL, Joo JH, Lin FR, et al. Effects of community-based health worker interventions to improve chronic disease management and care among vulnerable populations: a systematic review. Am J Public Health. (2016) 106:e3–e28. doi: 10.2105/AJPH.2015.302987
18. Brownstein JN, Chowdhury FM, Norris SL, Horsley T, Jack L, Zhang X, et al. Effectiveness of community health workers in the care of people with hypertension. Am J Prev Med. (2007) 32:435–47. doi: 10.1016/j.amepre.2007.01.011
19. Attipoe-Dorcoo S, Chattopadhyay SK, Verughese J, Ekwueme DU, Sabatino SA, Peng Y. Engaging community health workers to increase cancer screening: a community guide systematic economic review. Am J Prev Med. (2021) 60:e189–e97. doi: 10.1016/j.amepre.2020.08.011
20. Savas LS, Heredia NI, Coan SP, Fernandez ME. Effectiveness of a community health worker-delivered intervention to increase breast and cervical cancer screening among medically underserved hispanics. JCO Global Oncol. (2018) 4:70400. doi: 10.1200/jgo.18.70400
21. Krieger J, Takaro TK, Song L, Beaudet N, Edwards K. A randomized controlled trial of asthma self-management support comparing clinic-based nurses and in-home community health workers: the seattle–king county healthy homes II projec. Arch Pediatric Adolesc Med. (2009) 163:141–9. doi: 10.1001/archpediatrics.2008.532
22. Weaver A, Lapidos A. Mental health interventions with community health workers in the United States: a systematic review. J Health Care Poor Underserved. (2018) 29:159–80. doi: 10.1353/hpu.2018.0011
23. Allen J, Dennison Himmelfarb C, Szanton S, Frick K. Cost-effectiveness of nurse practitioner/community health worker care to reduce cardiovascular health disparities. J Cardiovasc Nurs. (2014) 29:308–14. doi: 10.1097/JCN.0b013e3182945243
24. Coleman EA, Parry C, Chalmers S, Sung-joon Min P. The care transitions intervention: results of a randomized controlled trial. Arch Internal Med. (2016) 166:1822–8. doi: 10.1001/archinte.166.17.1822
25. Felix HC, Mays GP, Stewart MK, Cottoms N, Olson M. Medicaid savings resulted when community health workers matched those with needs to home and community care. Health Aff. (2011) 30:1366–74. doi: 10.1377/hlthaff.2011.0150
26. Findley S, Matos S, Hicks A, Chang J, Reich D. Community health worker integration into the health care team accomplishes the triple aim in a patient-centered medical home: a Bronx tale. J Ambul Care Manag. (2014) 37:82–91. doi: 10.1097/JAC.0000000000000011
27. Kozhimannil KB HR, Alarid-Escudero F, Vogelsang CA, Blauer-Peterson C, Howell EA. Modeling the cost-effectiveness of doulacare associated with reductions in preterm birth and cesarean delivery. Birth. (2016) 43:20–7. doi: 10.1111/birt.12218
28. Smith L, Atherly A, Campbell J, Flattery N, Coronel S, Krantz M. Cost-effectiveness of a statewide public health intervention to reduce cardiovascular disease risk. BMC Public Health. (2019) 19:1234. doi: 10.1186/s12889-019-7573-8
29. Matthew RA, Willms L, Voravudhi A, Smithwick J, Jennings P, Machado-Escudero Y. Advocates for community health and social justice: a case example of a multisystemic promotores organization in South Carolina. J Commun Pract. (2017) 25:344–64. doi: 10.1080/10705422.2017.1359720
30. Bovbjerg RB, Eyster L, Ormond BA, Anderson T, Richardson E. Opportunities for Community Health Workers in the Era of Health Reform. Washington, DC: The Urban Institute (2013).
31. CDC. CDC Announces More Than $300 Million in Funding to Support Community Health Workers. (2021). Available online at: https://www.cdc.gov/media/releases/2021/p0903-health-worker-funding.html
32. HHS. HHS Announces $226.5 Million to Launch Community Health Worker Training Program. (2022). Available online at: https://www.hhs.gov/about/news/2022/04/15/hhs-announces-226-million-launch-community-health-worker-training-program.html
33. Mayfield-Johnson S, Smith DO, Crosby SA, Haywood CG, Castillo J, Bryant-Williams D, et al. Insights on COVID-19 from community health worker state leaders. J Ambul Care Manage. (2020) 43:268–77. doi: 10.1097/JAC.0000000000000351
34. Goldfield NI, Crittenden R, Fox D, McDonough J, Nichols L, Lee Rosenthal E. COVID-19 crisis creates opportunities for community-centered population health: community health workers at the center. J Ambul Care Manage. (2020) 43:184–90. doi: 10.1097/JAC.0000000000000337
35. Sabo S, Allen CG, Sutkowi K, Wennerstrom A. Community health workers in the United States: challenges in identifying, surveying, and supporting the workforce. Am J Public Health. (2017) 107:1964–9. doi: 10.2105/AJPH.2017.304096
36. Rosenthal EL, Menking P, John JS. The Community Health Worker Core Consensus (C3) Project: A Report of the C3 Project Phase 1 and 2, Together Leaning Toward the Sky. A National Project to Inform CHW Policy and Practice. El Paso, TX: Texas Tech University Health Sciences Center (2018).
37. Nkonki L, Cliff J, Sanders D. Lay health worker attrition: important but often ignored. Bull World Health Organ. (2011) 89:919–23. doi: 10.2471/BLT.11.087825
38. Lehmann U, Sanders D. Community Health Workers: What do We Know About Them? The State of the Evidence on Programmes, Activities, Costs and Impact on Health Outcomes of Using Community Health Workers. Geneva: World Health Organization (2007).
39. Ofosu-Amaah V. National Experience in the Use of Community Health Workers: A Review of Current Issues and Problems. Geneva: World Health Organization (1983).
40. Bhattacharyya K, Winch P, LeBan K, Tien M. Community Health Worker Incentives and Disincentives: How They Affect Motivation, Retention, and Sustainability. Arlington, VA: United States Agency for International Development (2001).
41. Khan SH, Chowdhury AM, Karim F, Barua MK. Training and retaining Shasthyo Shebika: reasons for turnover of community health workers in Bangladesh. Health Care Superv. (1998) 17:37–47.
42. Chevalier C, Lapo A, O'Brien J, Wierzba TF. Why do village health workers drop out? World Health Forum. (1993) 14:258–61.
43. Crigler L, Hill K. Rapid Assessment of Community Health Worker Programs in USAID Priority MCH Countries: Draft Tool for Field Testing. Bethesda, MD: United States Agency for International Development (2009).
44. Colvin C. What Motivates Community Health Workers? Designing Programs that Incentivize Community Health Worker Performance and Retention Incentives Developing and Strengthening Community Health Worker Programs at Scale A Reference Guide for Program Managers and Policy Makers. Washington, DC: United States Agency for International Development: Maternal and Child Health Integrated Program (2014).
45. Strachan DL, Källander K, Ten Asbroek AHA, Asbroek T, Kirkwood B, Meek SR, et al. Interventions to improve motivation and retention of community health workers delivering integrated community case management (iCCM): stakeholder perceptions and priorities. Am J Trop Med Hyg. (2012) 87:111–9. doi: 10.4269/ajtmh.2012.12-0030
46. Kok MC, Dieleman M, Taegtmeyer M, Broerse JE, Kane SS, Ormel H, et al. Which intervention design factors influence performance of community health workers in low- and middle-income countries? A systematic review. Health Policy Plan. (2015) 30:1207–27. doi: 10.1093/heapol/czu126
47. Anabui O, Carter T, Phillippi M, Ruggieri DG, Kangovi S. Developing Sustainable Community Health Worker Career Paths. New York, NY: Milbank Memorial Fund (2021).
48. Farrar B, Morgan JC, Chuang E, Konrad TR. Growing your own: community health workers and jobs to careers. J Ambul Care Manag. (2011) 34:234–46. doi: 10.1097/JAC.0b013e31821c6408
49. Johnson & Johnson. Johnson & Johnson Our Race to Health Equity. (2022). Available online at: https://www.jnj.com/our-race-to-health-equity
50. Ose SO. Using excel and word to structure qualitative data. J Appl Soc Sci. (2016) 10:147–62. doi: 10.1177/1936724416664948
51. Meyer DZ, Avery LM. Excel as a qualitative data analysis tool. Field Methods. (2008) 21:91–112. doi: 10.1177/1525822X08323985
52. Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL: Aldine Publishing (1967).
53. Community Health Worker Career Gateways Requirements Pathways and Barriers. National Association of Community Health Workers. (2021). Available online at: https://nachw.org/wp-content/uploads/2022/12/CHW_career.pdf
Appendix
CHW interview guide
Do I have permission to record this interview?
Thank you for taking the time to interview with me today. First, I'm going to get some information about you and your role within your organization.
1. Tell me a little about yourself and your work at your organization.
a. How long have you been a CHW? How long have you worked at your organization?
b. About how many CHWs does your organization employ?
c. How many do you directly supervise?
d. What are the funding sources for your CHWs pay?
2. Next, we're going to discuss the career path for CHWs in your organization. When I say career path, I mean how people grow or advance in their job, such as opportunities for promotions or pay raises. Does your organization have a career ladder for CHWs? If so, tell me about them.
a. Does your organization have education or experience requirements to promote CHWs?
b. What barriers or challenges have you faced when developing a career ladder? How did you address these barriers?
c. Why do you think having a career ladder is important?
d. What factors should be considered to move CHWs from 1 level to the next?
e. What qualities/personality traits do you look for when hiring or promoting a CHW?
3. What does compensation look like for CHWs at your organization? What is the lowest and highest salary range?
a. What types of benefits do your CHWs receive?
b. Any other benefits (mileage, per diem, etc)
c. What about the CHW model at your organization do you think is unique?
4. If you had the opportunity to change anything about the CHW profession, what would it be?
a. Have you heard anything from former CHWs about why they left the position?
5. In your opinion, how can we better support CHWs in advancing their careers?
6. What else can you share with me that could be helpful as we try to work on this?
Keywords: community health worker, workforce development, career pathway, COVID-19, professional development, health equity, leadership, promotores de salud
Citation: Smithwick J, Nance J, Covington-Kolb S, Rodriguez A and Young M (2023) “Community health workers bring value and deserve to be valued too:” Key considerations in improving CHW career advancement opportunities. Front. Public Health 11:1036481. doi: 10.3389/fpubh.2023.1036481
Received: 04 September 2022; Accepted: 06 February 2023;
Published: 08 March 2023.
Edited by:
Julie Ann St. John, Texas Tech University Health Sciences Center, United StatesReviewed by:
Noelle Wiggins, Independent Researcher, Portland, OR, United StatesPaige Menking, National Center for Farmworker Health, United States
Copyright © 2023 Smithwick, Nance, Covington-Kolb, Rodriguez and Young. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Julie Smithwick, julie.smithwick@sc.edu
 Julie Smithwick
Julie Smithwick Jenesha Nance2
Jenesha Nance2 Sarah Covington-Kolb
Sarah Covington-Kolb Ashley Rodriguez
Ashley Rodriguez