- 1Department of Health Informatics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 2eHealth Lab Ethiopia, University of Gondar, Gondar, Ethiopia
- 3Department of Computer Science, College of Informatics, University of Gondar, Gondar, Ethiopia
- 4ICT Directorate, University of Gondar, Gondar, Ethiopia
- 5Department of Information System, College of Informatics, University of Gondar, Gondar, Ethiopia
Background: In Ethiopia and other developing countries, electronic medical record systems and other health information technology are being introduced. However, a small proportion of low-income countries have successfully implemented national health information systems. One cause for this can be the lack of digital literacy among medical practitioners. As a result, this study aimed to assess health professionals’ digital literacy level and associated factors in Northwest Ethiopia.
Method: A quantitative cross-sectional study was employed among 423 health professionals working in a teaching and referral hospital in Northwest Ethiopia. We modified and applied the European commission’s framework for digital competency to assess the level of digital literacy among health professionals. We used stratified random sampling with proportional allocation to the size of the departments in the hospital to select study participants. Data were collected using a semi-structured, self-administered, and pretested questionnaire. Descriptive and binary logistic regression analysis techniques were used to describe respondents’ digital literacy level and identify its associated factor, respectively. The odds ratio with 95% CI and value of p were used to assess the strength of the association and statistical significance, respectively.
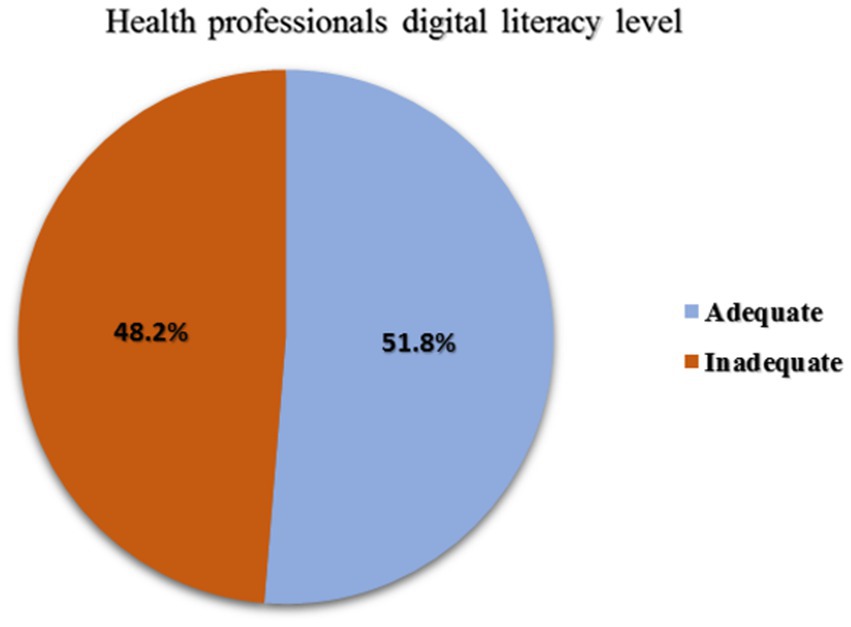
Results: Out of 411 participants, 51.8% (95% CI, 46.9–56.6%) of health professionals had adequate digital literacy. Holding a master’s degree (Adjusted OR = 2.13, 95% CI: 1.18–3.85), access to digital technology (AOR = 1.89, 95% CI: 1.12–3.17), having training in digital technology (AOR = 1.65, 95% CI: 1.05–2.59), and having a positive attitude towards digital health technology (AOR = 1.64, 95% CI: 1.02–2.68) were found to be significant factors associated with health professionals digital literacy level of health professionals.
Conclusion: Low level of digital literacy among health professionals was observed, with nearly half (48.2%) of them having poor digital literacy levels. Access to digital technology, training on digital technology, and attitude toward digital health technology were significant factors associated with digital literacy. It is suggested to increase computer accessibility, provide a training program on digital health technology, and promote a positive attitude toward this technology to improve the deployment of health information systems.
Background
Digital technology has a tremendous effect on improving the quality of health services in both developed and developing nations by enhancing the accessibility of health information and creating an efficient service provision (1). In high-income countries, digital health solutions are gradually being implemented in healthcare settings (2). However, only 35% of lower-middle-income nations and 15% of low-income countries have implemented national electronic health record systems in hospitals (3, 4). Most health facilities rely on paper-based systems, leading to inaccuracies in data management practice, which impacts the quality of healthcare delivery (5, 6).
Evidence suggests that healthcare information systems can enhance the quality of healthcare delivery and are expected to be implemented in all healthcare services (7). Therefore, using and operating information technology is a requirement for healthcare workers. Digital health technology refers to the collection, sharing, and analysis of health information using digital information, data, and communication technologies to enhance patient health and healthcare provision (8, 9). Examples include computers, tablets, smartphones, digital medical equipment, smartwatches, and other digital technology. The term digital literacy refers to “the ability to use technology to participate in and contribute to modern social, cultural, political, and economic life” (10). For the successful transformation of healthcare delivery, digital literacy is a prerequisite (11). Technologically savvy health workers can better manage their patients (12). Excellent digital literacy can lead to increased readiness for electronic health record systems (13). In turn, this might improve healthcare systems’ efficiency and long-term viability.
Ethiopia has several eHealth project initiatives underway, and most of the nation’s previously implemented health information systems faced sustainability challenges (14, 15). The main reason for low adoption or sustainability issues for EHR systems is a lack of pre-implementation efforts, such as a lack of digital literacy among health professionals (16–18). As a result, identifying areas and requirements before implementation could assist in determining the areas of focus that must be addressed throughout implementation.
Various studies are being conducted worldwide to evaluate healthcare professionals’ knowledge, perception, and willingness in using digital health tools (19, 20). Evidence also supports medical professionals’ adoption of digital health technologies for clinical services in response to the COVID 19 pandemic (21, 22). Previous studies in similar situations demonstrate that a lack of digital literacy among health practitioners is a significant factor in digital health system failure (5, 18, 23). Healthcare practitioners in low-income nations such as Ethiopia should have at least a basic knowledge of digital technology to implement e-health systems successfully (16). According to studies, healthcare workers’ digital skill gaps must be bridged for technology to be transferred to the point where health service quality can be maintained (5, 24).
Currently, the University of Gondar, in collaboration with the Ethiopian Ministry of Health (FMOH) and Digital Health Activities (DHA) agreed to customize and implement an Electronic Medical Record (EMR) at the University of Gondar Specialized and Comprehensive Hospital. The hospital serves as the sole referral center in Northwest Ethiopia, with a range of speciality healthcare services and a teaching and research center. Despite the range of services that it provides, its information system is not yet computerized. As a result of the adoption of e-health initiatives, the University of Gondar specialized hospital has been chosen as the pilot study for the EMR deployment. As far as we know, there are limited evidences available regarding the level of digital competency among healthcare professionals working in hospital settings. Hence, before starting a costly implementation, it is essential to assess the level of digital literacy of health professionals working at the implementation site. Therefore, this study aimed to evaluate the level of digital literacy and identify its associated factors among health workers at the University of Gondar Specialized and Comprehensive Hospital. Understanding the digital literacy of health workers could help take appropriate measures to successfully implement an EMR system at the hospital.
Methods
Study design and setting
An institutional-based cross-sectional study was conducted among health professionals at the University of Gondar specialized and comprehensive hospital from June 2 to June 25, 2022. The University of Gondar Specialized Hospital is located in the historic town of Gondar, northwest Ethiopia. Gondar is approximately 168 kilometres from Bahir Dar and 772 kilometres from Addis Abeba, the country’s capital. Nearly seven million people are served by the University of Gondar Comprehensive Specialized Hospital, one of the largest referral and teaching hospitals in the Amhara region (25). It employed 1,520 healthcare professionals across more than 20 departments to treat an average of 1,000 patients daily.
Study sample and eligibility criteria
All health professionals working at the University of Gondar Specialized and Comprehensive Hospital were included in this study. However, health professionals with less than six months of experience, those who will not be present in hospitals for various reasons, and those on yearly leave during the data collection period were excluded from the study.
Sample size determination and sampling procedure
The sample size was calculated using the single population proportion formula n= using the following assumptions (26). Since there is a study in Ethiopia addressing the digital literacy of health professionals working in primary health centers (p = 50%) (5), based on the assumptions of a 95% CI (z α/2 = 1.96), a 5% degree of precision (d), the final sample size becomes 384. A total of 423 healthcare professionals were included in the study after accounting for the 10% non-respondent rate. Each department served as a stratum in our department-based stratified random sampling design. A list of health professionals was used as the sampling frame. The level of digital literacy and related parameters were evaluated by proportionally allocating the sample to each department based on the number of healthcare providers. Participants in each department were then selected using a computer-generated simple random sampling technique.
Study variables
The dependent variable in this study was the digital literacy level of the healthcare practitioners, while the independent variables were socio-demographic characteristics (sex, Age, Profession, Educational level, Work experience), technological variables (Access to digital technology, Internet access, Training on digital technology), organizational variables (Staff motivation and workloads), and attitudes towards the use of digital health technology.
Measuring instruments
Digital literacy: Twenty-one item questions were adapted from the European Commission’s digital competency framework and used to assess health workers’ digital literacy (27). The digital literacy level is measured using a 5-point scale (Very Good, Good, Acceptable, Poor, and Very Poor) and separated into five primary components (Information processing, content creation, Communication, Safety, and Problem-solving). Since the data is not normally distributed, a median of the 21 questions about health professionals’ digital literacy level was calculated, and those who scored higher than the median were classified as having adequate digital literacy. In contrast, those who scored lower were classified as having inadequate digital literacy (5).
Attitude towards digital health technology: sixteen questions adapted from The Digital Health Scale were used to measure the health professionals’ attitude toward using digital health technology (28). The attitude toward digital health technology was measured using a 5-point scale (Strongly Agree, Agree, Neutral, Disagree, and Strongly Disagree). The item scores for each composite variable were added and divided by the number of items to create a composite variable ranging from scores 1 to 5 for the data analysis (29–31). As a result, the above three of final scores (strongly Agree, and Agree) were labelled as “Favorable attitude’. In contrast, final scores of three or less (strongly disagree, disagree, and neutral) were categorized as “Unfavorable attitude’ (31, 32).
Data collection tool and quality control
The questionnaires used in this study were developed after a review of related literature (5, 27, 28). A self-administered and pretested questionnaire was developed in English to collect the required data. The questionnaires assess the level of digital literacy among health professionals and their attitudes toward digital health technology, socio-demographic variables, technological attributes, and organizational characteristics. The data collection process involved two supervisors and twelve data collectors. Supervisors and data collectors received three days of training to minimize ambiguity. A pretest was conducted outside the study area, in Gondar town health centers, with 10% of the study population. The pretest results were used to evaluate the data collection instrument’s validity and reliability. Cronbach’s alpha scores were used to assess the data collection instrument’s internal consistency. As a result, the Cronbach alphas for digital literacy level (0.97) and attitude toward digital technology use (0.91) were found to be within the acceptable range.
Data processing and analysis
The Epi Data version 4.6 software packages were used for data entry, and the Statistical Package for Social Sciences (SPSS) version 25 was used for analysis. Descriptive statistics were computed to describe socio-demographic variables and health professionals’ digital literacy levels. Bivariable and multivariable binary logistic regression analyses were used to identify the relationship between the dependent and independent variables. Variables with a value of p less than 0.2 in the bivariable regression analysis were considered potential candidates for the multivariable regression analysis to assess their adjusted impacts on the dependent variables. An odds ratio with a 95 percent confidence level and p-value was calculated to determine the association’s strength and statistical significance. The cut-off value for all significantly associated variables was p < 0.05.
Ethics approval and consent to participate
Ethical clearance and approval letters were obtained from the Institutional Review Board (IRB) of the University of Gondar with reference number (Rfe. VP/RTT/05/571/2022). After explaining the study’s objective, each health professional signed a written consent form. The University of Gondar’s specialized hospital also obtained a letter of support. Confidentiality and privacy were ensured during data collection by keeping participants anonymous.
Results
Socio-demographic characteristics
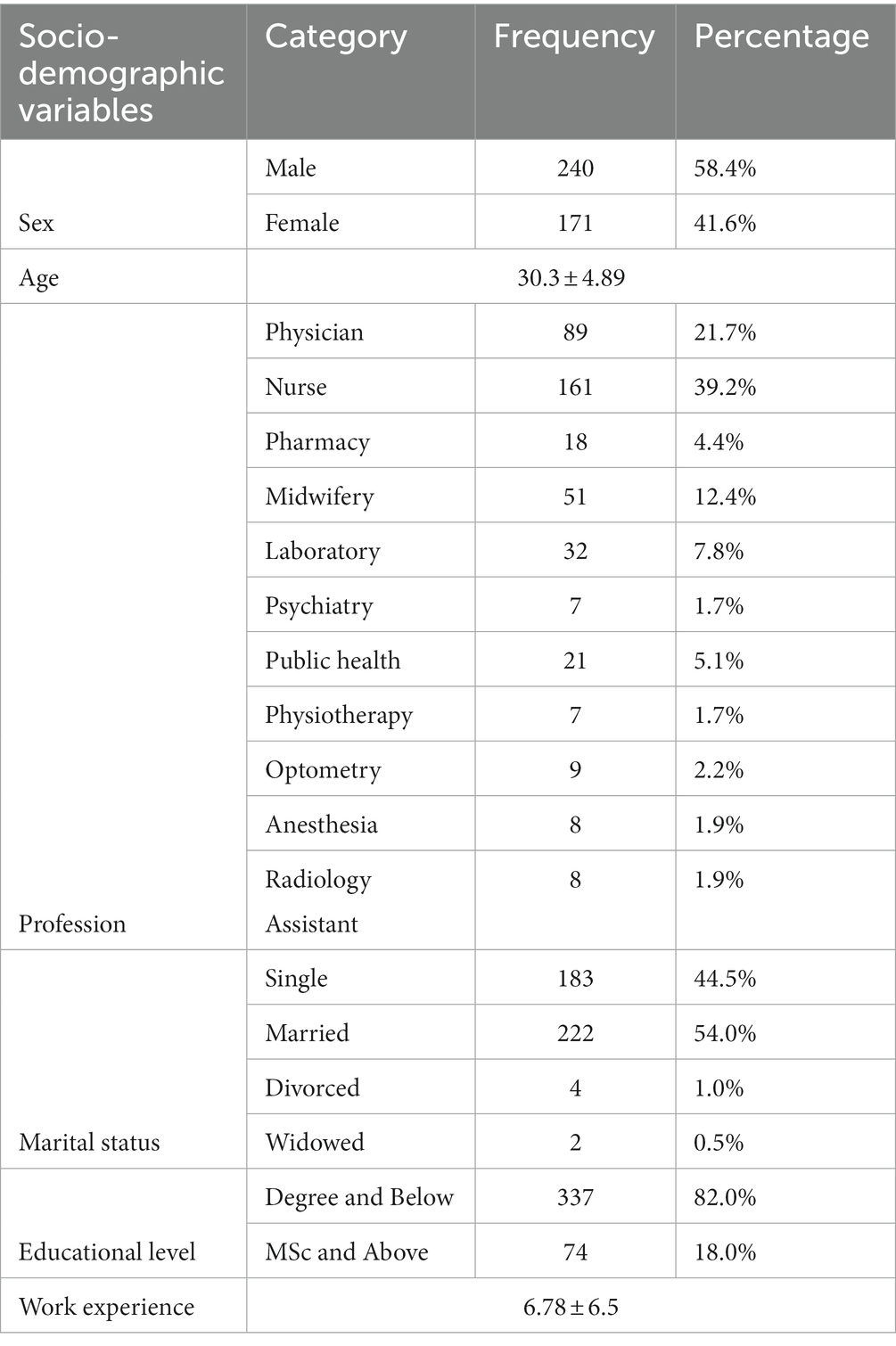
This study enrolled 411 health professionals, and the response rate was 97.1%. The participants’ average age was 30.3 years, with a standard deviation of +4.8 years, and a minimum and maximum age of 21 and 60, respectively. Of all participants, 240 (58.1%) were men, and 161 (39.2%) of the respondents identified as nurses. The majority of 336 (81.8%) health professionals had a degree or below in education, and 222 (54.0%) were married at the time. Regarding employment history, participants had an average of 6 years of experience (Table 1).
Technological and organizational factors
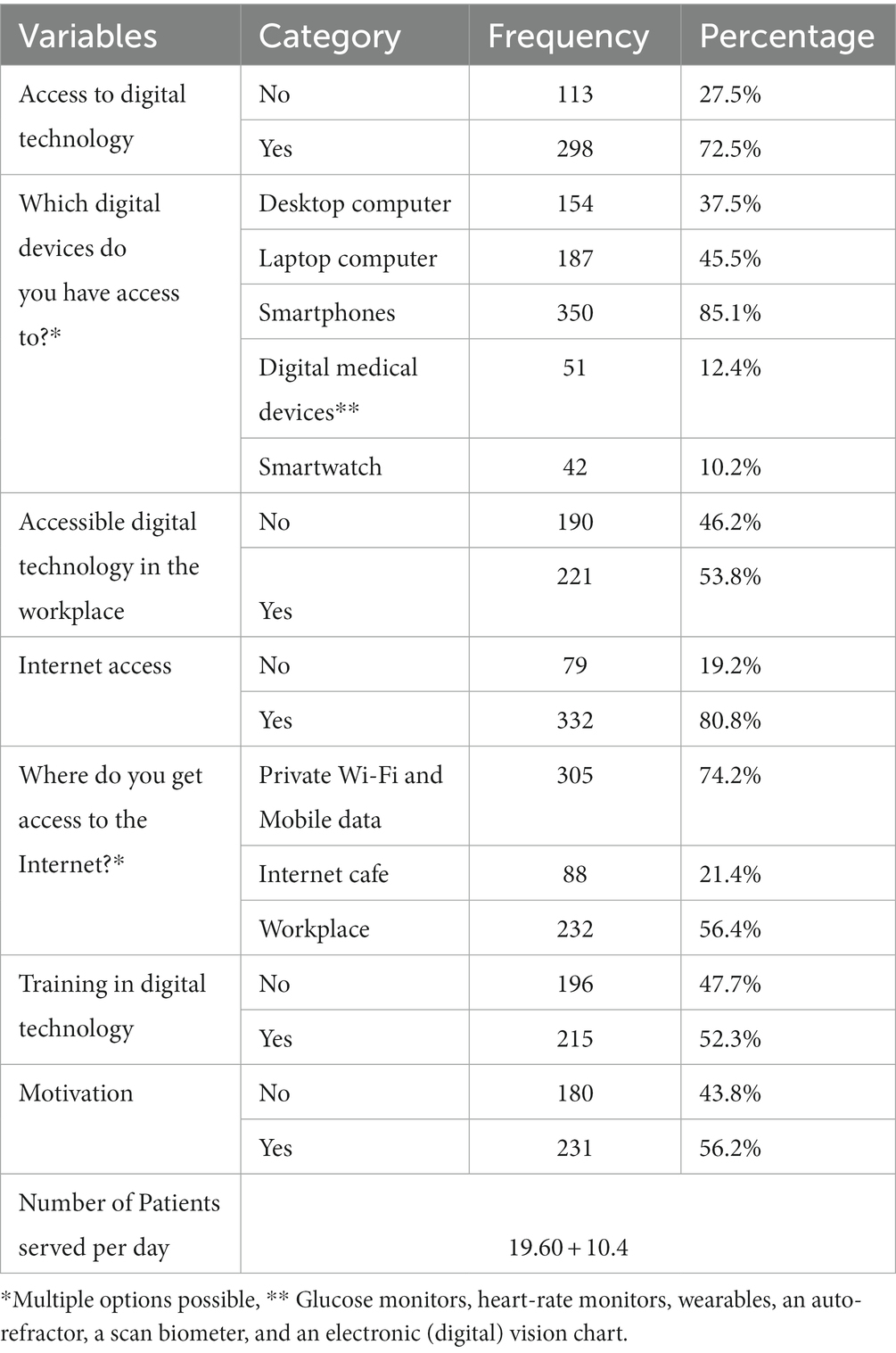
Most health professionals, 298 (72.5%), have access to digital devices like computers, tablets, smartphones, digital medical devices, smart watches, etc. Of all respondents, around 350 (85.1%) have access to a smartphone. A desktop computer, a laptop computer, and smartwatches are accessible to 154 (37%), 187 (45%), and 42 (10.2%) health professionals, respectively. However, only 51 (12.4%) health workers had access to one of the digital medical devices, such as an electronic (digital) vision chart, wearables, an auto-refractor, a scan biometer, glucose monitors and heart-rate monitors. Accessible digital medical equipment included glucose monitors, heart-rate monitors, wearables, an auto-refractor, a scan biometer, and an electronic (digital) vision chart. Nearly half, 221 (53.8%) of the respondents had access to one of the aforementioned digital technologies at work, and 332 (80.8%) of them had access to an internet connection (Table 2).
Regarding organizational characteristics, health professionals claimed that they visit an average of 19 and more patients daily. From the total of 231 (56.2%) respondents, the staff is also driven to use digital technology for patient care. Furthermore, 215 (52.3%) health professionals have received training in digital technology.
Attitude towards digital health technology
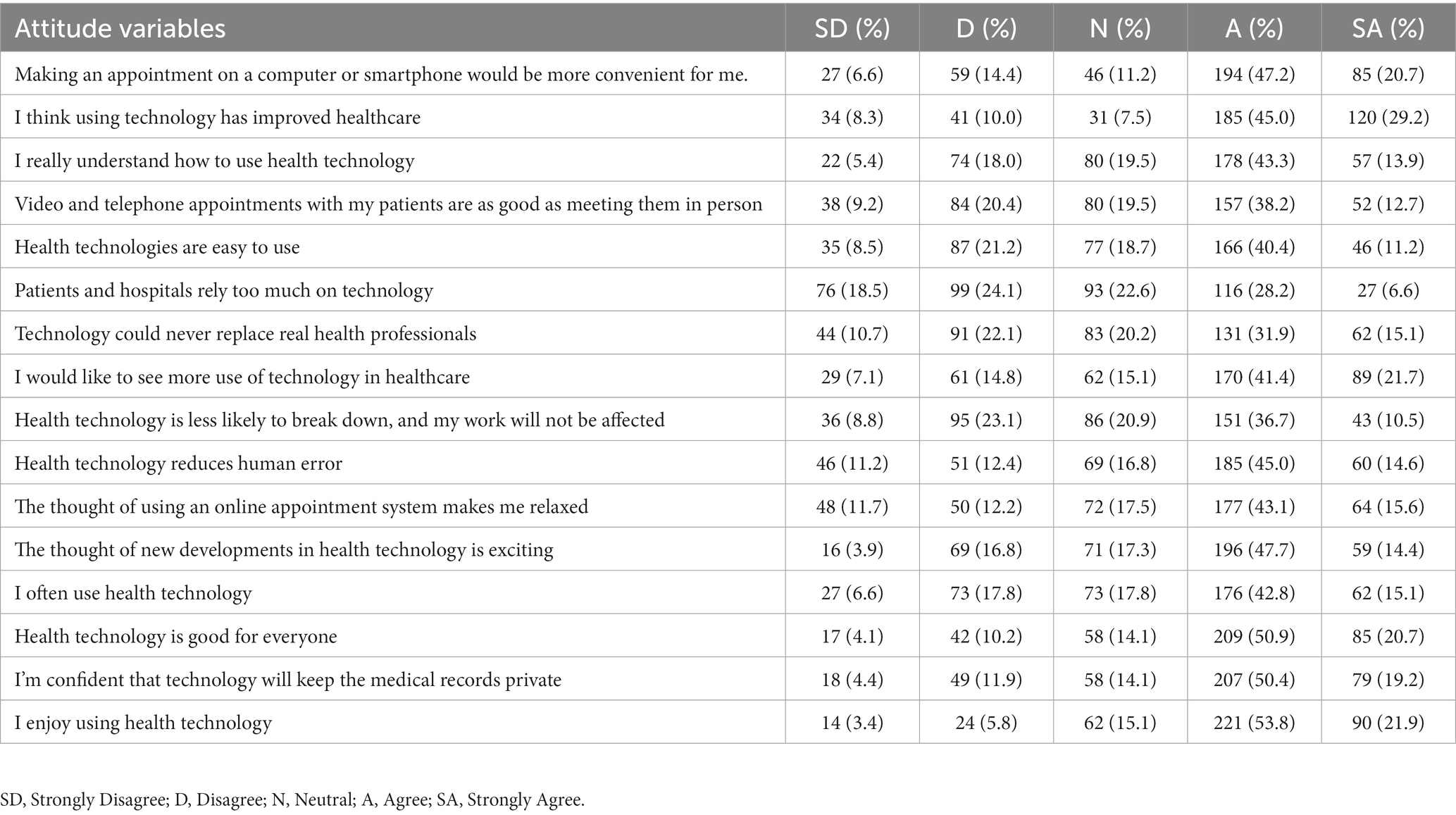
Of the total respondents in this study, 307 (74.7%) with (95% CI:70.4–78.9%) had a favourable attitude towards using digital health technology to provide patient care.
Table 3 shows that 194 (47.2%) health professionals agreed that booking an appointment on a computer or smartphone was more practical. A total of 185 (45.0%) respondents said using technology had improved healthcare. Around 44% of health professionals responded that they understand how to use digital health technology. Surprisingly, 157 (38.2) respondents asserted that video and telephone appointments with patients are just as effective as in-person meetings. Nearly half of the responders (209) (50.9%) believed that health technology benefits everyone. Similarly, 207 (50.4%) of participants expressed confidence in the confidentiality of medical records due to technology. Additionally, 170 (41.4) respondents were enthusiastic about the increased usage of technology in healthcare.
Health professionals’ digital literacy level
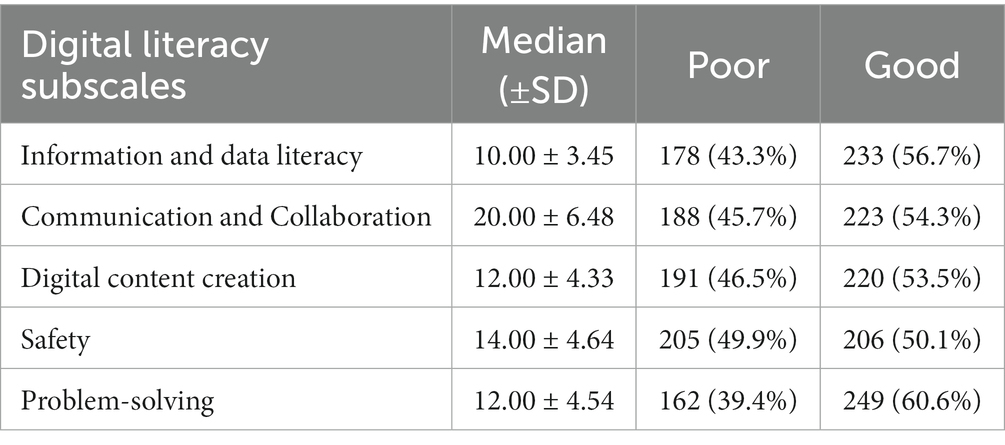
Overall, 213 (51.8%) (95% CI, 46.9–56.6%) health professionals have adequate digital literacy levels (Figure 1). As shown in Table 4, the combination of five digital literacy components, information and data literacy, collaboration and communication literacy, literacy in creating digital content, safety, and problem-solving, was used to assess the respondents’ overall levels of digital literacy. Of the total, 233 (56.7%) had adequate information and data literacy. Regarding collaboration and communication, more than half of the health professionals, 223 (54.3%), possessed adequate literacy. Of the total respondents, 220 (53.5%) had adequate literacy in digital content creation. Additionally, 206 (50.1%) and 249 (60.6%) exhibited adequate literacy levels in safety and problem-solving, respectively.
Factors associated with health professionals’ digital literacy level
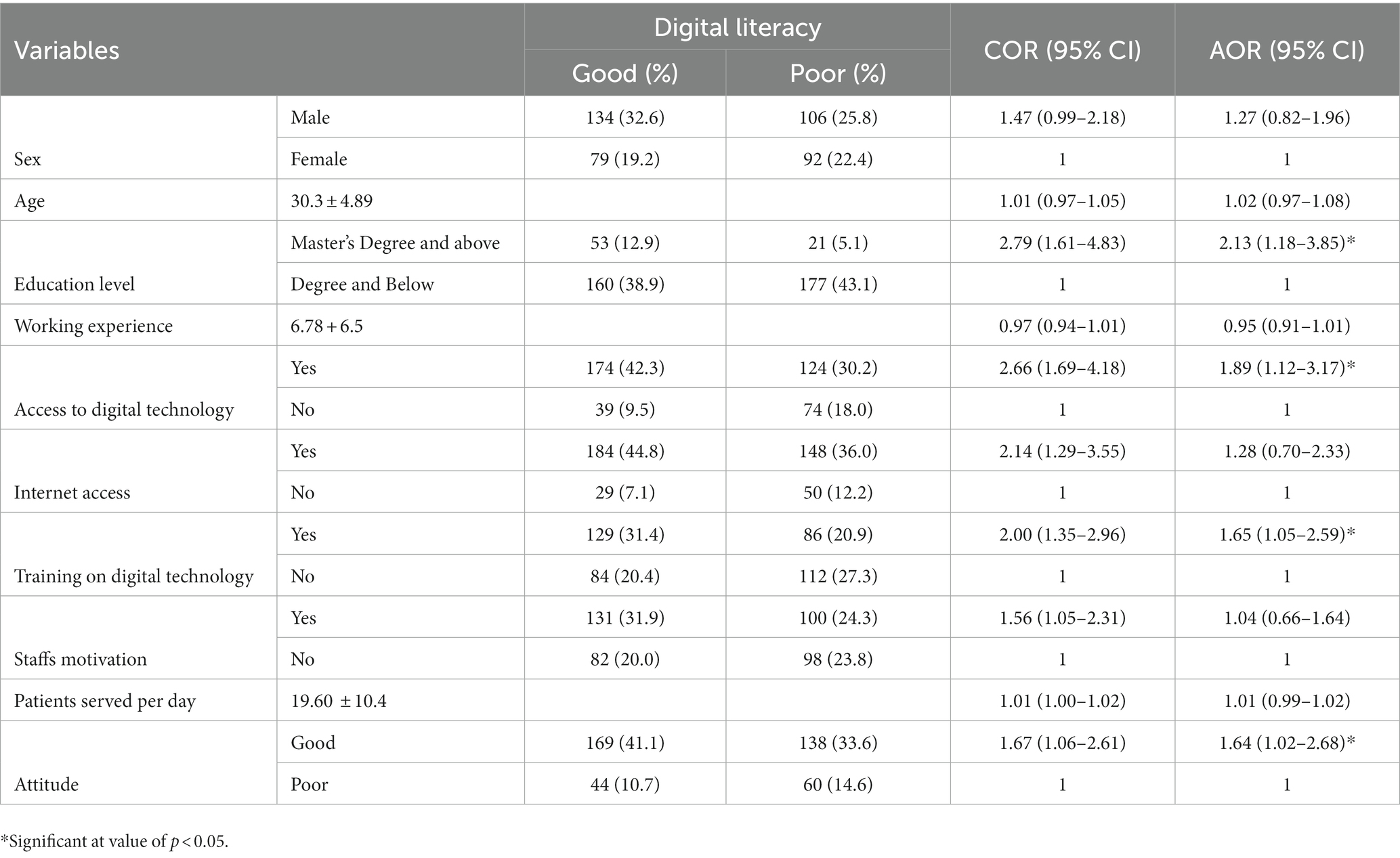
The factors affecting the level of digital literacy among health professionals were examined using bivariable and multivariable logistic regression analysis. In the bivariate analysis, sex, age, educational status, monthly income, work experience, access to digital technology, internet access, training on digital technology, organizational motivation, attitude towards digital technology, and patient served per day were taken into consideration as candidates for the multivariable logistic regression analysis.
According to the multivariable logistic regression analysis results, respondents with master’s degrees were 2.13 times more likely to have good digital literacy than those with degrees and below educational levels (AOR = 2.13, 95% CI: 1.18–3.85). Health professionals with access to digital technology were 1.89 times more likely to have adequate digital literacy than those without (AOR = 1.89, 95% CI: 1.12–3.17). The current study also found that healthcare professionals who had received training in digital technology were 1.65 times more likely to have adequate digital literacy than their counterparts (AOR = 1.65, 95% CI: 1.05–2.59). Additionally, Health professionals with a favourable attitude toward digital health technology were 1.64 times more likely to have adequate digital literacy than those with unfavourable attitudes (AOR = 1.64, 95% CI: 1.02–2.68) Table 5.
Discussion
The results of this study revealed that 51.8% of health professionals have adequate digital literacy levels. This finding is consistent with studies in Ethiopia (5) and other studies conducted in Indonesia (7). However, our finding is lower compared to those of research studies which are conducted in Australia (33), Vietnam (34), and India (6). The discrepancy could result from variations in internet usage and ICT facilities among countries compared to Ethiopia. Evidence suggests that Ethiopia lags behind Africa’s average internet penetration rate (39%) (35).
The other explanation for this discrepancy could be that only roughly two-thirds (72%) of the study’s participants had access to digital technology, which is much fewer than in other wealthy nations like Australia (33) and may result in lower levels of digital literacy among health professionals in Ethiopia. In most affluent countries, digital health system implementation has been effective due to high computer literacy (33, 36). However, in underdeveloped countries, there is a low level of digital literacy among health workers, resulting in the stoppage of many e-health projects (37, 38). As a result, given the growing usage of technology in healthcare, it is critical that healthcare professionals are digitally literate (39, 40).
Respondents with master’s degrees were 2.13 times more likely to have adequate digital literacy than those with a degree and below educational levels. This finding is in line with previous research studies indicating that health professionals with higher education levels were more likely to have adequate digital literacy (5). This might be because health professionals with higher education levels were more likely to use digital technology for their education, such as research and data gathering tools, which were more frequently employed by master’s-level and more educated health professionals.
The current study also found that healthcare professionals receiving training in digital technology were 1.65 times more likely to have adequate digital literacy than their counterparts. The findings align with earlier studies conducted among nurses in Indonesia (7) and health professionals in Austral (33). This finding implies that general training on digital health technology and the specific eHealth software application that will be implemented may significantly impact how well the healthcare system adopts technology.
Health professionals with access to digital technology were 1.89 times more likely to be highly digitally literate than those without. This finding is in line with other research showing that medical personnel with access to digital devices, including computers, laptops, smartphones, and digital medical equipment, have a high level of digital literacy (41–44). This indicates that the Ethiopian ministry of health should increase the accessibility of digital health technology in the hospital setting to increase digital literacy among health professionals and successfully implement clinical health information systems.
Furthermore, this study found a significant association between the level of digital literacy and attitudes toward digital health technology. Health workers with a favourable attitude toward digital health technology were 1.64 times more likely to have good digital literacy than those with unfavourable attitudes. This conclusion is supported by earlier research showing that a positive attitude toward digital technology is associated with a greater likelihood of digital competence (33). This suggested that initiatives were required to alter health professionals’ attitudes toward digital health technology. This is because adopting a new mindset significantly contributes to efficiently integrating health information technologies into the healthcare system (45).
Implication for policy and practice
This study has an implication for future digital health systems implementations. A possible way to raise the success rate of eHealth project implementations in Ethiopia is to increase computer accessibility, offer a training programme on digital health technology, and encourage a favourable attitude toward this technology. The study serves as a basis for the continuous implementation and customization of the electronic medical record at the University of Gondar Specialized and Comprehensive Hospital. Determining the level of digital literacy among the medical professionals working at the implementation location was the major objective to increase implementation success.
Conclusion and recommendation
This study aimed to determine the digital literacy level of health professionals and the associated factors that have implications for future digital health systems implementation. The results of this study help us better understand the level of digital literacy among health professionals at the specialized hospital where an EMR system will be implemented. The results of this study demonstrated that health professionals have a relatively low level of digital literacy. It is suggested to increase computer accessibility, provide a training program on digital health technology, and promote a positive attitude toward this technology to improve the deployment of health information systems.
Limitations and future works
The limitation of this study is that the data was collected through self-report, which could be prone to social desirability bias, so participants may have overestimated their responses. However, we tried to reduce this bias by making the questions as fair, neutral, and unthreatening as possible. Future work is required to determine the current status of adopting digital health tools by health professionals in Ethiopia. This will provide reliable data to assess interventions intended to increase the efficiency of various eHealth initiatives in Ethiopia.
Data availability statement
The data presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical clearance and approval letters were obtained from the Institutional Review Board (IRB) of the University of Gondar with refernace number (Rfe. VP/RTT/05/571/2022). After explaining the study’s objective, each health professional signed a written consent form. The University of Gondar’s specialized hospital also obtained a letter of support. Confidentiality and privacy were ensured during data collection by keeping participants anonymous. The patients/participants provided their written informed consent to participate in this study.
Author contributions
TY and MT made significant contributions to the conceptualization, design, data collection supervision, data analysis, interpretation, and writing of the publication. BT, AMa, HK, FN, EZ, AMe, GS, RG, HG, AS, and ST contributed equally to the data collection, analysis, interpretation, and manuscript review. All authors contributed to the article and approved the submitted version.
Funding
The data collection for this study was funded by the University of Gondar (EMR customization and implementation project). The University of Gondar (EMR customization and implementation project) had no role in the study’s design, data collection, analysis, or interpretation of data, the decision to publish in peer-reviewed publications, or manuscript preparation.
Acknowledgments
We want to thank the University of Gondar, College of Medicine and Health Sciences, for allowing us to perform this research. Our gratitude also goes to the University of Gondar’s comprehensive specialized hospital administrators for providing all of the required information and assistance.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
E-health, Electronic health; EMR, Electronic medical record; FMOH, Federal ministry of health; DHA, Digital health analysis; CBMP, Capacity building and mentorship project; DUP, Data use partnership; AOR, Adjusted odds ratio; COR, Crude odds ratio; CI, Confidence interval; SPSS, Statistical Package for Social Science.
References
1. Tran Ngoc, C, Bigirimana, N, Muneene, D, Bataringaya, JE, Barango, P, Eskandar, H, et al. Conclusions of the digital health hub of the transform Africa summit (2018): strong government leadership and public-private-partnerships are key prerequisites for sustainable scale up of digital health in Africa In: BMC proceedings : (2018). 17. doi: 10.1186/s12919-018-0156-3
2. Piette, JD, Lun, K, Moura, LA Jr, Fraser, HS, Mechael, PN, Powell, J, et al. Impacts of e-health on the outcomes of care in low-and middle-income countries: where do we go from here? Bull World Health Organ. (2012) 90:365–72. doi: 10.2471/BLT.11.099069
3. WHO. Electronic health records (2021). [cited 2022 October 23]. Available at: https://www.who.int/home/cms-decommissioning.
4. Mohammed, E, Andargie, G, Meseret, S, and Girma, E. Knowledge and utilization of computer among health workers in Addis Ababa hospitals, Ethiopia: computer literacy in the health sector. BMC Res Notes. (2013) 6:1–8. doi: 10.1186/1756-0500-6-106
5. Shiferaw, KB, Tilahun, BC, and Endehabtu, BF. Healthcare providers’ digital competency: a cross-sectional survey in a low-income country setting. BMC Health Serv Res. (2020) 20:1021–7. doi: 10.1186/s12913-020-05848-5
6. Brar, IS, Editor digital information literacy among health sciences professionals: a case study of GGS medical college, Faridkot, Punjab, India. SITE 2015: Informing Science+ IT Education Conferences: USA (2015).
7. Mutiar, A, MKep ES. Digital media literacy level among nurses in urban area of Indonesia. Int Public Health J. (2021) 13:213–8.
8. Turakhia, MP, Desai, SA, and Harrington, RA. The outlook of digital health for cardiovascular medicine: challenges but also extraordinary opportunities. JAMA Cardiol. (2016) 1:743–4. doi: 10.1001/jamacardio.2016.2661
9. Beam, AL, and Kohane, IS. Translating artificial intelligence into clinical care. JAMA. (2016) 316:2368–9. doi: 10.1001/jama.2016.17217
10. Inskip, C. Developing library staff digital literacies, Journal Digital Literacy Unpacked, (2018). 139–152. doi: 10.29085/9781783301997.012
11. Nouri, S, Khoong, EC, Lyles, CR, and Karliner, L. Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catalyst Innov Care Delivery. (2020) 1, 1–13. doi: 10.1056/CAT.19.1111
12. Zakaria, N, and Yusof, SAM. Understanding technology and people issues in hospital information system (HIS) adoption: case study of a tertiary hospital in Malaysia. J Infect Public Health. (2016) 9:774–80. doi: 10.1016/j.jiph.2016.08.017
13. Ajami, S, and Bagheri-Tadi, T. Barriers for adopting electronic health records (EHRs) by physicians. Acta Informatica Medica. (2013) 21:129–34. doi: 10.5455/aim.2013.21.129-134
14. Fraser, HS, and Blaya, J, Editors. Implementing medical information systems in developing countries, what works and what doesn’t. AMIA Annual Symposium Proceedings; 2010: American Medical Informatics Association. (2010).
15. Luna, D, Otero, C, and Marcelo, A. Health informatics in developing countries: systematic review of reviews contribution of the IMIA working group health informatics for development. Yearb Med Inform. (2013) 22:28–33. doi: 10.1055/s-0038-1638829
16. Ghazisaeidi, M, Ahmadi, M, Sadoughi, F, and Safdari, R. A roadmap to pre-implementation of electronic health record: the key step to success. Acta Informatica Medica. (2014) 22:133–8. doi: 10.5455/aim.2014.22.133-138
17. Lorenzi, NM, Kouroubali, A, Detmer, DE, and Bloomrosen, M. How to successfully select and implement electronic health records (EHR) in small ambulatory practice settings. BMC Med Inform Decis Mak. (2009) 9:1–13. doi: 10.1186/1472-6947-9-15
18. Biruk, S, Yilma, T, Andualem, M, and Tilahun, B. Health professionals’ readiness to implement electronic medical record system at three hospitals in Ethiopia: a cross sectional study. BMC Med Inform Decis Mak. (2014) 14:115–8. doi: 10.1186/s12911-014-0115-5
19. Thapa, S, Nielsen, JB, Aldahmash, AM, Qadri, FR, and Leppin, A. Willingness to use digital health tools in patient care among health care professionals and students at a University Hospital in Saudi Arabia: quantitative cross-sectional survey. JMIR Medical Educ. (2021) 7:e18590. doi: 10.2196/18590
20. Abodunrin, O, and Akande, T. Knowledge and perception of e-health and telemedicine among health professionals in LAUTECH teaching hospital, Osogbo, Nigeria. Int J Health Res. (2009) 2. e2113p121–e2113p130. doi: 10.4314/ijhr.v2i1.55388
21. Anthony, JB. Implications of telehealth and digital care solutions during COVID-19 pandemic: a qualitative literature review. Inform Health Social Care. (2021) 46:68–83. doi: 10.1080/17538157.2020.1839467
22. Bokolo, AJ. Application of telemedicine and eHealth technology for clinical services in response to COVID-19 pandemic. Heal Technol. (2021) 11:359–66. doi: 10.1007/s12553-020-00516-4
23. Ruxwana, NL, Herselman, ME, and Conradie, DP. ICT applications as e-health solutions in rural healthcare in the eastern Cape Province of South Africa. Health Inform Manag J. (2010) 39:17–29. doi: 10.1177/183335831003900104
24. Asi, YM, and Williams, C. The role of digital health in making progress toward sustainable development goal (SDG) 3 in conflict-affected populations. Int J Med Inform. (2018) 114:114–20. doi: 10.1016/j.ijmedinf.2017.11.003
25. Abdella, NM, Tefera, MA, Eredie, AE, Landers, TF, Malefia, YD, and Alene, KA. Hand hygiene compliance and associated factors among health care providers in Gondar University hospital, Gondar, north West Ethiopia. BMC Int Health Hum Rights. (2014) 14:1–7. doi: 10.1186/1471-2458-14-96
26. Naing, L, Winn, T, and Rusli, B. Practical issues in calculating the sample size for prevalence studies. Arch Orofac Sci. (2006) 1:9–14. doi: 10.12691/ajcp-3-1-3
27. Commission E. The European digital competence Frameworkfor citizens (2016). [cited 2022 January2]. Available at: https://ec.europa.eu/social/BlobServlet?docId=15688&langId=en
28. DigitalHealthScale. A validated measure of attitudes towards digitising healthcare services (2020). [cited 2022 January 15]. Available at: https://digitalhealthscale.com/
30. MacLure, K, and Stewart, D. Self-reported digital literacy of the pharmacy workforce in north East Scotland. Pharmacy. (2015) 3:182–96. doi: 10.3390/pharmacy3040182
31. Tegegne, MD, Endehabtu, BF, Guadie, HA, and Yilma, TM. Health professionals’ attitude towards the use of social media for COVID-19 related information in Northwest Ethiopia: a cross-sectional study. Front Public Health. (2022) 10:1736. doi: 10.3389/fpubh.2022.900293
32. Campbell, GJ, and McDowell, DE. Computer literacy of nurses in a community hospital: where are we today?. J Cont Educ Nursing (2011) 42:365–70. doi: 10.3928/00220124-20110215-01
33. Kuek, A, and Hakkennes, S. Healthcare staff digital literacy levels and their attitudes towards information systems. Health Informatics J. (2020) 26:592–612. doi: 10.1177/1460458219839613
34. Nguyen, LHT, Vo, MTH, Tran, LTM, Dadaczynski, K, Okan, O, Murray, L, et al. Digital health literacy about COVID-19 as a factor mediating the association between the importance of online information search and subjective well-being among university students in Vietnam. Front Digital Health. (2021):3. doi: 10.3389/fdgth.2021.739476
35. Datareportal. DIGITAL 2020: ETHIOPIA (2020). [cited 2022 October 23]. Available at: https://datareportal.com/reports/digital-2020-ethiopia
36. Jha, AK, DesRoches, CM, Campbell, EG, Donelan, K, Rao, SR, Ferris, TG, et al. Use of electronic health records in US hospitals. N Engl J Med. (2009) 360:1628–38. doi: 10.1056/NEJMsa0900592
37. Mogessie, YG, Ntacyabukura, B, Mengesha, DT, Musa, MB, Wangari, M-C, Claude, N, et al. Digital health and COVID-19: challenges of use and implementation in sub-Saharan Africa. Pan Afr Med J. (2021) 38:38. doi: 10.11604/pamj.2021.38.240.27948
38. Ibeneme, S, Ukor, N, Ongom, M, Dasa, T, Muneene, D, and Okeibunor, J. Strengthening capacities among digital health leaders for the development and implementation of national digital health programs in Nigeria In: BMC proceedings; 2020: BioMed central. (2020).
39. Jones, EB, and Furukawa, MF. Adoption and use of electronic health records among federally qualified health centers grew substantially during 2010–12. Health Aff. (2014) 33:1254–61. doi: 10.1377/hlthaff.2013.1274
40. DePasse, J, Caldwell, A, Santorino, D, Bailey, E, Gudapakkam, S, Bangsberg, D, et al. Affordable medical technologies: bringing value-based design into global health. BMJ Innov. (2016) 2:bmjinnov-2015-000069:4–7. doi: 10.1136/bmjinnov-2015-000069
41. Nelson, K, Courier, M, and Joseph, GW. An investigation of digital literacy needs of students. J Inf Syst Educ. (2011) 22:95–110.
42. Alwan, K, Awoke, T, and Tilahun, B. Knowledge and Utilization of Computers Among Health Professionals in a Developing Country: A Cross-Sectional Study. JMIR Hum Factors. (2015) 2:e4. doi: 10.2196/humanfactors.4184
43. Ameen, K, and Gorman, G. Information and digital literacy: a stumbling block to development? A Pakistan perspective. Libr Manag. (2009) 30:99–112. doi: 10.1108/01435120910927565
44. Oo, HM, Htun, YM, Win, TT, Han, ZM, Zaw, T, and Tun, KM. Information and communication technology literacy, knowledge and readiness for electronic medical record system adoption among health professionals in a tertiary hospital, Myanmar: a cross-sectional study. PLoS One. (2021) 16:e0253691. doi: 10.1371/journal.pone.0253691
Keywords: digital literacy, health professionals, associated factors, Northwest Ethiopia, referral and teaching hospital, digital health systems
Citation: Tegegne MD, Tilahun B, Mamuye A, Kerie H, Nurhussien F, Zemen E, Mebratu A, Sisay G, Getachew R, Gebeyehu H, Seyoum A, Tesfaye S and Yilma TM (2023) Digital literacy level and associated factors among health professionals in a referral and teaching hospital: An implication for future digital health systems implementation. Front. Public Health. 11:1130894. doi: 10.3389/fpubh.2023.1130894
Edited by:
Alberto Quílez-Robres, University of Zaragoza, SpainReviewed by:
Pillaveetil Sathyadas Indu, Government Medical College, IndiaBokolo Anthony Jnr., Institute for Energy Technology, Norway
Rebecca Erschens, University of Tübingen, Germany
Copyright © 2023 Tegegne, Tilahun, Mamuye, Kerie, Nurhussien, Zemen, Mebratu, Sisay, Getachew, Gebeyehu, Seyoum, Tesfaye and Yilma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tesfahun Melese Yilma, tesfahunmelese@gmail.com
 Masresha Derese Tegegne
Masresha Derese Tegegne Binyam Tilahun1,2
Binyam Tilahun1,2 Fedlu Nurhussien
Fedlu Nurhussien Tesfahun Melese Yilma
Tesfahun Melese Yilma