Modulation of Reactive Oxygen Species Homeostasis as a Pleiotropic Effect of Commonly Used Drugs
- 1Laboratory of Energy Metabolism Institute of Translational Medicine Department of Health Sciences and Technology ETH Zurich, Schwerzenbach, Switzerland
- 2Molecular Biology and Biochemistry, Gottfried Schatz Research Center, Medical University of Graz, Graz, Austria
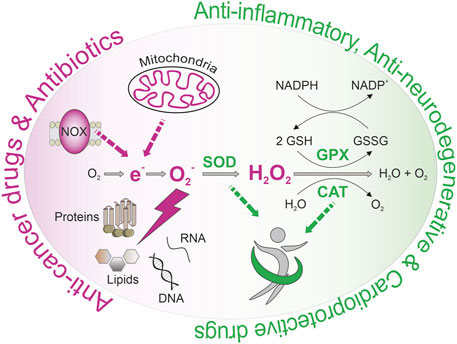
Age-associated diseases represent a growing burden for global health systems in our aging society. Consequently, we urgently need innovative strategies to counteract these pathological disturbances. Overwhelming generation of reactive oxygen species (ROS) is associated with age-related damage, leading to cellular dysfunction and, ultimately, diseases. However, low-dose ROS act as crucial signaling molecules and inducers of a vaccination-like response to boost antioxidant defense mechanisms, known as mitohormesis. Consequently, modulation of ROS homeostasis by nutrition, exercise, or pharmacological interventions is critical in aging. Numerous nutrients and approved drugs exhibit pleiotropic effects on ROS homeostasis. In the current review, we provide an overview of drugs affecting ROS generation and ROS detoxification and evaluate the potential of these effects to counteract the development and progression of age-related diseases. In case of inflammation-related dysfunctions, cardiovascular- and neurodegenerative diseases, it might be essential to strengthen antioxidant defense mechanisms in advance by low ROS level rises to boost the individual ROS defense mechanisms. In contrast, induction of overwhelming ROS production might be helpful to fight pathogens and kill cancer cells. While we outline the potential of ROS manipulation to counteract age-related dysfunction and diseases, we also raise the question about the proper intervention time and dosage.
1 Highlights
• Age-related diseases are associated with defective ROS homeostasis.
• Approved drugs exhibit pleiotropic effects on ROS homeostasis.
• Enforcement of antioxidant defense mechanisms positively affects cardiovascular and neurodegenerative diseases.
• Overwhelming ROS production might be used to fight pathogens and kill cancer cells.
2 Introduction
2.1 Reactive Oxygen Species Modulation as a Potential Treatment Strategy
The global number of elderly over age 80 will triple from 2015 until 2050. Since aging is associated with the progressive decline of functionality and regenerative potential of tissues, there is an urgent need to prolong a healthy lifespan and to find strategies to delay the onset of age-related dysfunctions such as chronic inflammation and pain, diabetes, cardiovascular diseases (CVD), neurodegenerative diseases, and cancer (Sun et al., 2010; Tejero et al., 2019). On a cellular level, dysfunctions in cellular signaling, proteostasis, autophagy, and mitochondrial homeostasis are closely intertwined in a vicious circle leading to loss of cellular homeostasis and health. For instance, poor protein quality control leads to defective organelles that produce enhanced levels of reactive oxygen species (ROS). These highly reactive chemicals are based on reduced molecular oxygen and include superoxide, hydroxyl radicals, singlet oxygen, and peroxides (Sun et al., 2010; Tejero et al., 2019). In addition to superoxide, nitric oxide synthases (NOS) also produce nitric oxide that interacts with ROS to rapidly produce reactive nitrogen species (RNS) such as peroxynitrite (Sun et al., 2010; Tejero et al., 2019). Due to the electron transport chain (ETC), mitochondria are the cell’s main production sites of ROS (Sun et al., 2010; Tejero et al., 2019). Notably, a reduction in mitochondrial content was found to counteract the process of aging in vivo (Correia-Melo et al., 2016), suggesting that mitochondrial activity gets detrimental during aging. Besides, an enormous number of more than 200 clinical disorders, including type 2 diabetes mellitus (T2DM), degenerative brain impairments like Alzheimer’s disease (AD) and Parkinson’s disease (PD), cardiovascular dysfunction, and cancer, have been associated with early dysregulations in redox homeostasis through so-called ROS and NOS (Kaul et al., 2001; Farah et al., 2018). Besides, experiments in various species revealed an inverse (Schulz et al., 2007; Singh et al., 2011; Ristow and Schmeisser, 2014; Cai et al., 2017) correlation between ROS production rates and lifespan (Sun et al., 2010; Tejero et al., 2019). Align with these findings, increased formation of mitochondrial ROS (mtROS) was postulated as the primary cause of aging in (Harman, 1956) in the Free Radical Theory of Aging (Sun et al., 2010; Tejero et al., 2019). Consequently, in the hope of successfully counteracting age-related diseases, numerous clinical trials tested the impact of antioxidants, including natural or artificial ROS scavenging substances, on the development or progression of age-related diseases. Unfortunately, most clinical trials failed to reveal a benefit from the use of antioxidants or were even related to harmful side-effects on human health like cancer growth. For instance, a randomized controlled trial found that supplementation with vitamin E over 7 years does not prevent cancer or major cardiovascular events but increases the risk for heart failure in patients with vascular diseases or diabetes mellitus (Sun et al., 2010; Tejero et al., 2019). While the application of antioxidants failed to prove a beneficial effect in clinical trials, interventions boosting the body’s antioxidant defense mechanisms are associated with enhanced health and lifespan in various species. A transient ROS burst functions like a vaccine, thereby enabling an adaptational response with enhanced antioxidant defense mechanisms. Notably, behavioral interventions like caloric restriction or physical activity, both known to positively affect health and lifespan, as well as compounds like green tea catechins, long time associated with healthy aging, might trigger these vaccination-like ROS level rises (Merry and Ristow, 2016), (Schulz et al., 2007; Singh et al., 2011; Ristow and Schmeisser, 2014; Cai et al., 2017). Based on these reports, it might be essential to strengthen antioxidant defense mechanisms in advance by low ROS level rises to maintain a proper ROS homeostasis during age and to prevent age-related diseases (Ristow and Schmeisser, 2014). It remains questionable whether selectively targeting certain ROS species within the cell might be an intervention strategy when lacking the potential to induce antioxidant defense mechanisms, for instance, in the case of amyotrophic lateral sclerosis (ALS) (Carrera-Juliá et al., 2020). In contrast, overwhelming ROS production might also be desirable under certain conditions, including fighting off pathogens (Paiva and Bozza, 2014) or cancerous cells (Liou and Storz, 2010).
A strategy to delay the onset of age-related diseases by ROS modulation might require drug administration to still healthy and comparably young individuals for extended periods. Consequently, respective drug candidates are needed to be safe and exhibit a minimum of side effects in the long-term use. To identify drugs least likely to cause harm while still providing benefit, numerous classes of potential geroprotective compounds are currently tested in model organisms like Saccharomyces cerevisiae, Caenorhabditis elegans, and Drosophila melanogaster (Janssens and Houtkooper, 2020). According to the U.S. Food and Drug Administration (FDA), an experimental drug takes 12 years on average to progress from bench to market. Usually, only 5 out of 5000 pre-clinically tested compounds will be used in clinical trials, and only one out of these five clinically tested compounds will receive approval for therapeutic use (Kraljevic et al., 2004). Consequently, it might be worthwhile to evaluate whether approved drugs that are already characterized regarding their long-term safety and side effects might be repurposed to modulate ROS homeostasis. Notably, several drugs in clinical use exhibited pleiotropic antioxidative effects and were found to delay aging in various aging models (Steven et al., 2015; Janssens and Houtkooper, 2020). The current review provides an up-to-date overview of how approved drugs interfere with ROS homeostasis and evaluates their potential to counteract the age-related decline in cellular function.
2.2 Molecular targets
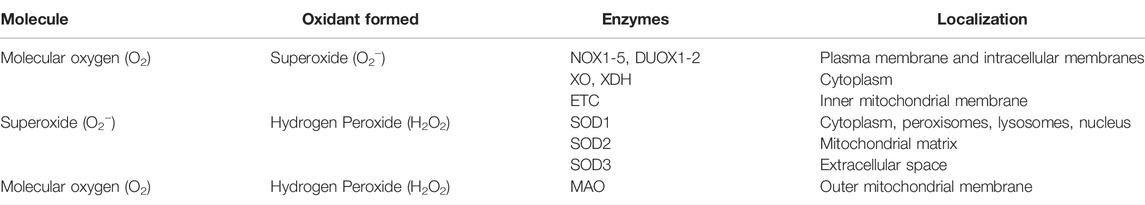
2.2.1 ROS production sites
2.2.1.1 Mitochondrial
Mitochondria are the main production site of ROS (Boveris et al., 1972). Superoxide and hydrogen peroxide are generated as a side product of mitochondrial respiration during electron leakage at the respiratory chain complexes I, II, and III in the inner mitochondrial membrane (Goncalves et al., 2015) ( Table 1). Since excessive mtROS production is associated with age-related dysfunction and pathologies, including tumor growth (Bell et al., 2011) and hypertension (Kimura et al., 2005; Dikalova et al., 2010), mtROS was long time seen as a harmful by-product of respiration only. However, moderate levels of mtROS are crucial for various signaling pathways (Collins et al., 2012), such as response to hypoxia (Guzy and Schumacker, 2006), cell differentiation (Mandal et al., 2011), autophagy (Lee et al., 2012a), inflammation (Zhou et al., 2011), and immune response (West et al., 2011). Notably, mitochondrial damage-associated molecular patterns (mtDAMP), which are indicators of mitochondrial dysfunction, play a critical role in ROS-mediated inflammatory processes. For example, oxidated mtDAMPs such as mitochondrial DNA (mtDNA) were shown to activate the NLR family pyrin domain containing 3 (NLRP3) inflammasome, an essential component of the innate immune system (Shimada et al., 2012; Zhong et al., 2013).
Monoamine oxidase (MAO): The mitochondrial monoamine oxidases (MAOs) A and B degrade a variety of neurotransmitters, including norepinephrine, serotonin, dopamine, and tyramine (Sub Laban and Saadabadi, 2021), by catalyzing the oxidative deamination of their amines (Tipton, 2018). Thereby, hydrogen peroxide is generated as a side product at the outer mitochondrial membrane that possibly contributes to oxidative stress (Table 1). Nonetheless, there is no clinical proof that MAO inhibitors reduce levels of toxic and prooxidant MAO products until now (Tipton, 2018). In the clinic, selective MAO-A inhibitors are used as amine-depleting drugs against depression (Kline, 1958; Zeller et al., 1959). In contrast, selective MAO-B inhibitors work as dopamine-sparing compounds against PD (selective MAO-B inhibitors) (Birkmayer et al., 1983).
2.2.1.2 Non-Mitochondrial
NADPH oxidase 1–7: NADPH oxidases (NOXs) are transmembrane enzymes that specifically generate radical superoxide anions by reducing molecular oxygen using nicotinamide adenine dinucleotide phosphate (NADPH) (Table 1). The NOX family consists of 7 members, including NOX1-5, as well as the dual oxidases 1 and 2 (DUOX1; DUOX2), which are expressed in endothelial cells, vascular smooth muscle cells, cardiac myocytes and fibroblasts, adipocytes, macrophages, stem cells, and adventitial fibroblasts (Lassègue et al., 2012). Although the prooxidant role of NOXs is crucial in cellular physiology, such as differentiation, proliferation, apoptosis, inflammatory responses, host defense, and redox signaling (Lassègue et al., 2012; Vermot et al., 2021), increased NOX activity was also correlated with several pathologies such as neurodegenerative diseases, including AD and PD (Sorce and Krause, 2009; Popa-Wagner et al., 2013; Vermot et al., 2021) and cancer (Juhasz et al., 2009; Meitzler et al., 2014; Wang et al., 2015; You et al., 2018). Targeting NOXs might therefore represent a suitable approach for disease-specific therapies (Spencer and Engelhardt, 2014).
Xanthine oxidoreductase: The xanthine oxidoreductase (XOR) belongs to the family of molybdoenzymes (Kisker et al., 1997) and is expressed in human tissues such as the liver, small intestine, mammary gland (Linder et al., 1999), and heart (Muxfeldt and Schaper, 1987; Abadeh et al., 1993; Vickers et al., 1998). XOR can be interconverted into xanthine dehydrogenase (XDH) and xanthine oxidase (XO) (Stirpe et al., 1969). Both XDH and XO are involved in the metabolism of hypoxanthine/xanthine to uric acid during purine degradation (Xu et al., 1996; Okamoto et al., 2013) upon generation of superoxide anion (Battelli et al., 2016) (Table 1). Besides the involvement of XOR in purine catabolism, there is evidence for a broader range of benefits. For example, it was speculated that XOR-derived uric acid positively impacts oxidative stress-associated aging and cancer and thus promotes the extension of life span in humans (Ames et al., 1981).
Nitric oxide synthase (NOS): The family of nitric oxide synthases includes neuronal NOS (nNOS), inducible NOS (iNOS), and endothelial NOS (eNOS). These enzymes generate nitric oxide upon L-arginine utilization which plays an essential part in vascular regulation, inflammation, and intracellular signaling. Besides these physiological functions, nitric oxide also represents a harmful contributor to oxidative stress as it can react to cytotoxic peroxynitrite in the presence of oxygen (Adams et al., 2015).
2.2.2 The Antioxidant System
The cellular antioxidant system is subdivided into enzymatic antioxidants, including the glutathione and thioredoxin system, and nonenzymatic antioxidants, such as dietary vitamins. Polymorphisms in involved proteins such as superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GPX) were associated with various human metabolic disorders such as diabetes, CVD, and cancer (Crawford et al., 2012; Hebert-Schuster et al., 2012), emphasizing the critical role of enzymatic antioxidant systems.
Superoxide dismutase 1–3: The family of superoxide dismutases (SODs) consists of the copper-zinc superoxide dismutase (SOD1 gene) localized in the cytoplasm, peroxisomes, lysosomes, and the nucleus (Chang et al., 1988; Keller et al., 1991; Crapo et al., 1992; Liou et al., 1993), as well as the manganese superoxide dismutase (SOD2 gene) present in the mitochondrial matrix (Weisiger and Fridovich, 1973), and the extracellular superoxide dismutase (SOD3 gene) (Marklund, 1984). SODs are the only class of enzymes catalyzing the reduction of superoxide to hydrogen peroxide and O2 (Genestra, 2007) and thus playing a significant role in redox regulation (Table 1). Malfunction of SOD is associated with several clinical pathologies. For example, SOD1 mutations were able to mimic ALS-associated dysregulation in several mouse models (Bruijn et al., 2004). In addition, SOD2 mutations are associated with cardiomyopathy, sporadic motor neuron defects, and cancer (Hiroi et al., 1999). On the other hand, overexpression of SOD1 proved beneficial against neurological injuries and brain diseases in animal studies (Kamii et al., 1999; Morita-Fujimura et al., 2000; Sugawara et al., 2002; Yu et al., 2006; Endo et al., 2007).
Catalase: Human CAT is a peroxisomal enzyme that detoxifies hydrogen peroxide by catalyzing its reduction to H2O and O2 (Putnam et al., 2000). Overexpression of catalases in mitochondria results in extended life span with attenuated age-related pathologies (Schriner et al., 2005; Treuting et al., 2008; Dai et al., 2009; Olsen et al., 2013) and protects against CVD (Yang et al., 2003; Yang et al., 2009; Maiellaro-Rafferty et al., 2011) and diabetic nephropathy (Brezniceanu et al., 2007; Shi et al., 2013) in mice. In contrast, patients that lack catalase expression are prone to develop T2DM (Avraham et al., 1988).
Thioredoxin system: The thioredoxin system involves several players and types of redox reactions. In first-line are peroxiredoxins (PRX1-6), a family of peroxidases (Wood et al., 2003; Flohé et al., 2011; Rhee and Woo, 2011) that catalyze the reduction of hydrogen peroxide by oxidation of their active PRX disulfides. Regeneration of oxidized PRX is achieved by reduction through small thiol-disulfide oxidoreductases, so-called thioredoxins (TRX). Thioredoxins are eventually reduced by thioredoxin reductases (TR) upon utilization of the reductive potential of reduced NADPH (Lillig and Holmgren, 2007; Lu and Holmgren, 2014). Strengthening the thioredoxin system manifests in several health-beneficial alterations. For example, overexpression of PRX3 reduced cardiac failure upon myocardial infarction in murine heart mitochondria (Matsushima et al., 2006) and counteracted hyperglycemia and glucose intolerance of mice (Chen et al., 2008). TRX1 was detected in the plasma during inflammation and oxidative stress (Nakamura et al., 1996) and proposed as antioxidant therapy (Nakamura et al., 2009; Watanabe et al., 2010; Matsuo and Yodoi, 2013). Moreover, TRX1 and TRX80 displayed protective effects in AD in humans (Gil-Bea et al., 2012).
Glutathione system: Glutathione peroxidases (GPXs) use a reducing equivalence of glutathione (GSH) to reduce peroxides and hydroxy radicals into nontoxic derivatives (Brigelius-Flohé, 1999; Flohé et al., 2011). The resulting oxidized glutathione (GSSG) is reduced to GSH by glutathione reductase (GR) through the oxidation of NADPH to NADP+ (Birben et al., 2012). Another representative of the glutathione system is the class of glutaredoxins (GRXs), which are oxidoreductases mainly responsible for the reduction of GSH-disulfides (Holmgren, 1976) and deglutathionylation of S-glutathionylated proteins (Holmgren et al., 2005). The glutathione system is the principal regulator of the cellular redox balance, and the GSH/GSSG ratio is used as an oxidative stress biomarker for several diseases, including CVD, AD, PD, ALS, multiple sclerosis (MS), and cancer (Frijhoff et al., 2015). GPX1 knock-out increases oxidative stress and the prevalence of AD-associated neurotoxicity and heart ischemia-reperfusion injury in mice (Yoshida et al., 1997; Fu et al., 1999; Klivenyi et al., 2000; Crack et al., 2006; Lim et al., 2009). In contrast, GPX1 overexpression protected against oxidative stress, cerebral ischemia/reperfusion damage, and neurodegenerative pathologies such as PD (Weisbrot-Lefkowitz et al., 1998; Sheldon et al., 2004; Ridet et al., 2006). Several clinical trials linked polymorphisms of GPX and consequently decreased enzyme activity to an increased risk for T2DM (Ramprasath et al., 2012), cardiovascular dysregulations in T2DM patients (Hamanishi et al., 2004), breast cancer (Ravn-Haren et al., 2006), and colorectal adenomas (Hansen et al., 2005).
Nonenzymatic antioxidants: Nonenzymatic antioxidants include low molecular mass molecules such as carotenoids, vitamin A, ascorbic acid (vitamin C), α-tocopherol (vitamin E), polyphenols, minerals such as selenium and zinc, as well as various drugs including acetylcysteine (Pisoschi and Pop, 2015). The antioxidant potential of vitamin A, C, and E, as well as phenolic acids, is given by their ability to scavenge free radicals in the form of ROS and RNS (Burton and Ingold, 1984; Burton and Traber, 1990). In addition, carotenoids and vitamin E prevent lipid peroxidation by direct reduction of peroxyl radicals (Burton and Ingold, 1984). Minerals, instead, are crucial components of antioxidant enzymes and consequently crucial for their activity (Tabassum et al., 2010). Zinc, for example, is an inhibitor of NADPH oxidase and a part of superoxide dismutase and thus contributes to the antioxidant system. Although more than 100 clinical trials tested nutritional interventions with vitamins, polyphenols, and minerals have been conducted during the last twodecades (Bjelakovic et al., 2007; Bjelakovic et al., 2012), the vast majority failed to reveal the beneficial effects of dietary antioxidant supplementation (Goodman et al., 2011; Bjelakovic et al., 2012; Halliwell, 2013), questioning the total suppression of ROS generation as a therapeutical approach.
3 The implication of Reactive Oxygen Species in Age-Related Diseases
3.1 Cardiovascular Diseases
3.1.1 Clinical Significance
Cardiovascular diseases (CVD) like ischemic heart diseases and stroke are the leading disease burden worldwide, causing the majority of cases in global mortality and contributing to various disabilities. There has been a worrying trend, with cases of CVD roughly doubling from 1990 to 2019, reaching 18.6 million (Roth et al., 2020). Deterioration of ROS homeostasis is a common hallmark in CVD, and ROS-modified molecules might even serve as biomarkers for the progression of CVD. For instance, clinical trials have revealed an association between increased levels of circulating oxidative low-density lipoprotein (LDL) and atherosclerotic CVD (Gao and Liu, 2017). Moreover, 8-hydroxy-2-deoxyguanosine, a marker for oxidative DNA damage, is significantly increased in the serum patients with dilated cardiomyopathy (Kono et al., 2006), and the concentration in the urine correlates with heart failure (Kobayashi et al., 2011). Besides, 8-iso-prostaglandin F2α, a by-product of lipid peroxides generated during oxidative stress, is increased in patients with symptomatic heart failure and correlated with the functional severity of heart failure (Mallat et al., 1998). In contrast, another primary lipid peroxidation product, 4-hydroxy-2-nonenal-modified protein, was found to be elevated in the myocardium of hypertrophic cardiomyopathy patients (Nakamura et al., 2005). Despite the strong implication of ROS in CVD, clinical trials have failed to provide evidence for a therapeutic benefit of potent antioxidants in treating CVD so far (Panth et al., 2016), potentially due to blocking signaling function of ROS and by preventing ROS-induced upregulation of ROS defense mechanisms.
3.1.2 Cellular Mechanisms and Signaling
ROS have a crucial signaling function in the cardiovascular system. For instance, ROS contribute to the signal transduction pathway of angiotensin II, causing cardiac growth and hypertrophy in neonatal rat cardiomyocytes (Shih et al., 2001). Moreover, ROS adjust the iron homeostasis in response to catecholamines in cardiomyocytes, a process essential to maintaining proper metabolic activity (Costa et al., 2009). Notably, enhanced ROS production is associated with left ventricular hypertrophy, and heart failure in experimental guinea pig models with left ventricular hypertrophy exhibited a progressive expression increase in several NADPH oxidase subunits (Li et al., 2002). Notably, the expression of NOX2 was also found to be increased in infarcted areas but unchanged in unaffected regions of cardiac samples from patients who had died from acute myocardial infarction (Krijnen et al., 2003). Platelet-derived ROS function as signaling molecules but might induce a vicious circle resulting in a platelet procoagulant phenotype and apoptosis, enhancing the thrombotic risk (Masselli et al., 2020). Besides, a deterioration of ROS defense mechanisms might contribute to the genesis and progression of CVD. Experiments in a cardiomyocyte-specific SOD2 deficient mouse strain revealed that deficiency of SOD2 results in increased ROS levels and subsequent overproduction of electrophilic aldehydes, which serve as mediators of mitochondrial dysfunction and boost cardiomyopathy (Sharma et al., 2020). Besides, attenuated SOD2 activity resulted in enhanced mitochondrial oxidative stress and plaque instability in hyperlipidemic mice during aging (Vendrov et al., 2017). Enhanced ROS production and decreased ROS detoxification might also facilitate the formation of peroxynitrite that harms the vascular endothelium, smooth muscle, and myocardium (Pacher and Szabo, 2006). Besides, peroxynitrite formation reduces the amount of available nitric oxide that inhibits platelet activation and aggregation, cell adhesion molecule expression, and vascular smooth muscle proliferation and is, therefore, a crucial vasoprotective substance (Naseem, 2005).
3.2 Type 2 Diabetes Mellitus
3.2.1 Clinical Significance
Type 2 diabetes mellitus (T2DM) is characterized by insufficient insulin secretion, an uncontrolled rise in blood glucose levels, and insulin resistance of peripheral tissues (Rochette et al., 2014). Besides genetic components and age, obesity, diminished physical activity, chronic inflammation, and elevated cholesterol and triglyceride levels are the main primary risk factors of T2DM (Zeller et al., 2008; Olsson et al., 2011; Verdile et al., 2015), emphasizing the importance of functional metabolic regulations. An untreated T2DM condition and prolonged periods of high blood glucose may cause damage to the vascular system, subsequently leading to stroke, peripheral vascular diseases, neuropathy, retinopathy, and nephropathy (Wallace and Matthews, 2004; Asmat et al., 2016). Notably, the severity and T2DM-related mortality are linked to vascular complications and positively correlate with the degree of oxidative stress and ROS (Andreev and Rybakov, 1975; Domingueti et al., 2016). Cellular damage was associated with a ROS-dependent activation of stress pathways such as nuclear factor kappa-light-chain-enhancer of activated B cells (NF-kB), c-jun N-terminal kinase (JNK)/stress-activated phosphor-kinase (SAPK), and p38 MAPK in T2DM with vascular complications (Evans et al., 2003). Other publications could measure elevated levels of NADPH and superoxide during vascular dysfunction in diabetic patients (Guzik et al., 2002; Ergul et al., 2005). Further evidence of increased ROS levels manifests in increased lipid peroxidation (Davì et al., 1999; Bandeira et al., 2012) and carbonylation of serum proteins of type 2 diabetes mellitus individuals (Pandey et al., 2010; Gradinaru et al., 2013). Besides, oxidative markers such as F2-isoprostane, nitrotyrosine (Ceriello et al., 2001; Odegaard et al., 2016), and glycated hemoglobin (HbA1c) (Ryden et al., 2013) are commonly found in plasma, urine, and tissues of T2DM patients and serve as biomarkers for hyperglycemia.
3.2.2 Cellular Mechanisms and Signaling
ROS signaling plays a significant role in the metabolic activity of pancreatic β-cells (Ahmed Alfar et al., 2017), as well as downstream insulin signaling and glucose uptake in adipocytes by activation of the phosphoinositol 3-kinase and protein kinase B (AKT) (Mahadev et al., 2001), most likely mediated by NOX4-dependent ROS generation (Mahadev et al., 2004). Thereby, the high ROS sensitivity of pancreatic β cells is crucial for a functional physiological metabolism, as well as β cell regeneration and proliferation (Ahmed Alfar et al., 2017; Wang and Wang, 2017). However, the comparably low levels of antioxidant proteins such as GPX, CAT, SOD, and TR (Evans et al., 2003; Newsholme et al., 2007), make β-cells highly vulnerable to oxidative stress and ROS overload provoked by stimulation of the respiratory chain activity or NOX activity (Newsholme et al., 2007; Newsholme et al., 2012). Chronic oxidative stress impairs the cellular function of β-cells. It results in apoptotic cell death via p38 MAPK, JNK, and NF-kB signaling (Heimberg et al., 2001; Gurzov and Eizirik, 2011), reducing insulin secretion and provoking hyperglycemia. In turn, hyperglycemia excessively generates electron donors in the tricarboxylic acid (TCA) cycle and thus, promotes hyperpolarization of the mitochondrial membrane potential (Ψmito) and adenosine triphosphate (ATP) generation, followed by inhibition of complex III of the respiratory chain and electron accumulation at coenzyme Q. Consequently, oxygen is only partially reduced, boosting the production of superoxide radicals (Korshunov et al., 1997; Nishikawa et al., 2000; Brownlee, 2001). In addition, inflammation-associated ROS was shown to inhibit insulin receptor activity, the respective signaling, and consequently the response to insulin (Newsholme et al., 2014; Verdile et al., 2015), eventually leading to insulin resistance. Furthermore, it was shown that vascular homeostasis and anti-inflammatory processes are impaired in diabetes due to poor production of nitric oxide (Shi and Vanhoutte, 2017), potentially due to enhanced peroxynitrite formation (Caldwell et al., 2015). The interplay of poor NO levels, increased peroxynitrite concentrations, and elevated production of ROS does consequently further increase oxidative stress in diabetes (Pacher and Szabo, 2006).
3.3 Neurodegenerative Diseases
3.3.1 Clinical Significance
Alzheimer’s disease (AD) is a neurodegenerative disorder characterized by neuroinflammation, synaptic disruption, and abnormalities in mitochondrial structure and function (Hirai et al., 2001; Selkoe, 2002; Swerdlow and Khan, 2004; Barsoum et al., 2006; Wyss-Coray, 2006; Swerdlow et al., 2010), resulting in loss of memory and cognitive decline (Bertoni-Freddari et al., 1990; DeKosky et al., 1996; Tampellini and Gouras, 2010). (Walsh and Selkoe, 2007). As a consequence of an increasing global life expectancy (Jaul and Barron, 2017) and due to a growing population, the number of patients suffering from AD is predicted to increase in the future dramatically. While 35.6 million people were diagnosed with dementia in 2010, this number is estimated to reach 115.4 million people by 2050 (Prince et al., 2013) and thus strongly impacts worldwide health systems. One hallmark of AD is amyloid-β (Aβ) plaque formation due to abnormal processing of the amyloid precursor protein. Under pathological conditions, the amyloid precursor protein is cleaved into Aβ fragments (LaFerla et al., 2007), which oligomerize into soluble aggregates and subsequently accumulate to insoluble and toxic Aβ plaques. Consequently, oxidative damage of proteins, DNA, RNA, and lipids was found in AD patients’ brains (Reddy, 2006; Chaturvedi and Beal, 2008; Reddy and Beal, 2008). Thereby, oxidation productions such as 8-hydroxyguanosine and heme oxygenase serve as diagnostic markers in AD patients (Chaturvedi and Beal, 2008). Another important marker for AD is nitrotyrosine, a product of protein oxidation via nitric oxide (Good et al., 1996; Smith et al., 1997). Moreover, peroxynitrite production seems to be responsible for lysine, arginine, proline, and histidine oxidation in AD patients (Stadtman, 1990; Smith et al., 1997). Dysregulations in AD are undoubtedly associated with an imbalance in ROS homeostasis and subsequent oxidative damage in the brain of aged organisms (Migliaccio et al., 1999; Giorgio et al., 2005; Calkins et al., 2012). However, the molecular mechanisms are still elusive.
Parkinson’s disease (PD) is the fastest-growing neurodegenerative disease (Collaborators GBDN, 2019), and the number of people affected is predicted to double by 2040 (Dorsey and Bloem, 2018). PD is characterized by a progressive loss of dopaminergic neurons in the brain region substantia nigra (SN), leading to motor deficiencies such as tremor, rigidity, and bradykinesia. Another hallmark of PD is the development of insoluble inclusions consisting of aggregated α-synucleins, so-called Lewy bodies (Spillantini et al., 1997; Bellucci et al., 2012; Bellucci et al., 2016). While monomeric and tetrameric α-synucleins fulfill their physiological function as transport molecules, the formation of oligomers and fibrils is caused by α-synuclein mutation and contributes to pathological dysregulations (Bartels et al., 2011; Marques and Outeiro, 2012). Besides mutations in α-synuclein, familiar forms of PD might exhibit mutations in PTEN-induced kinase 1 (PINK) and E3 ubiquitin ligase (PARKIN), two proteins involved in autophagy (Lazarou et al., 2015; Pickrell and Youle, 2015), Parkinson’s disease protein 1 (PARK7 a redox-chaperone acting as oxidative stress sensor (Canet-Avilés et al., 2004), (Zondler et al., 2014), and leucine-rich repeat kinase 2 (LRRK2). Notably, these proteins are relevant for mitochondrial function and ROS homeostasis (Polymeropoulos et al., 1997; Bonifati et al., 2003; Valente et al., 2004; Gilks et al., 2005; Nichols et al., 2005). Indeed, the accumulation of damaged mitochondria is a further determinant for the mediation of PD pathology (Koentjoro et al., 2017). Neurons in the SN are highly vulnerable to oxidative stress and neurodegeneration, as seen in healthy elderly brains that contain double the number of oxidized proteins compared to other brain regions (Floor and Wetzel, 1998). Additionally, postmortem analyses of healthy aged brains compared to young controls revealed a decrease in SOD, GPX, and glutathione reductase activities (Venkateshappa et al., 2012), suggesting age-related loss of antioxidant enzyme activity. Another source of ROS represents the oxidative metabolism of dopamine, as hydrogen peroxide is produced as a side product of oxidative deamination of dopamine by MAO (Goldstein et al., 2013; Meiser et al., 2013). Furthermore, PD brains exhibit iron-enriched neurons in the SN (Dexter et al., 1987; Dexter et al., 1989; Michaeli et al., 2007; Pyatigorskaya et al., 2015), making this brain region highly vulnerable to oxidative stress (Brian J. Tabner et al., 2001; Jellen et al., 2013). Together with dopamine, labile iron is part of a prooxidant synergic interplay in aged SN (Hare and Double, 2016), leading to increased production of highly toxic dopamine-o-quinones (Tse et al., 1976; Graham, 1978; Zhou et al., 2010). The dopamine-o-quinones derivatives tetrahydroisoquinoline salsolinol and 6-hydroxydopamine were shown to increase ROS and oxidative stress by impairing ETC function (Su et al., 2013; Puspita et al., 2017). Chelation of iron as a treatment for PD was successful in animal models (Devos et al., 2014) and is currently tested in patients with early-stage PD by FAIRPARKII (ClinicalTrials.gov Identifier: NCT02655315).
3.3.2 Cellular Mechanisms and Signaling
Alzheimer’s disease (AD): Neuronal function is strongly dependent on a high energy supply. Based on calculations, neurons use up to 50% of their ATP for homeostasis and re-establishment of the ion gradient and 30% for synaptic transmission (Ames, 2000; Attwell and Laughlin, 2001). Consequently, neurons strongly rely on oxygen availability and functional mitochondrial oxidative phosphorylation for ATP generation. However, high oxygen levels and enhanced mitochondrial activity provoke the formation of ROS (Zorov et al., 2014). In addition, neurons contain elevated levels of lipids and comparably low amounts of antioxidant enzymes, making them highly vulnerable to oxidative stress (Jang et al., 2010). Also, the synaptic transmission that includes vesicle formation is energy-intense (Attwell and Laughlin, 2001). Therefore, ATP-generating mitochondria need to undergo axonal transport from the soma to the distant periphery to supply synapses with sufficient energy. Notably, impairment of this process was found in a range of neurodegenerative diseases such as ALS, Huntington’s disease, AD, and PD (Martin, 2011; Schon and Przedborski, 2011; Reddy and Shirendeb, 2012), once again emphasizing the importance of mitochondria for neuronal function. Several authors suggest that lack of mitochondrial transport represents an early event during neurodegeneration and the pathology of AD (Rui et al., 2006; Wang et al., 2010a; Du et al., 2010; Calkins and Reddy, 2011). Importantly, dysfunctional mitochondrial transport, enormous mitochondrial fragmentation, attenuated synaptic ATP, and synaptic dysfunction in AD neurons were associated with increased oxidative stress (Reddy et al., 2012) (Reddy, 2006). Similar observations were found in the brains of AD patients, which exhibited attenuated ATP levels, elevated levels of free radicals, OXPHOS disruptions, and mitochondrial dysfunctions (Gibson et al., 1998; Maurer et al., 2000; Wang et al., 2005; Devi et al., 2006; Wang et al., 2008; Reddy, 2009; Reddy et al., 2010).
Parkinson’s disease (PD): The susceptibility towards oxidative damage is based on several specific features of dopaminergic neurons. First, neurons of the SN are comparably large and unmyelinated (Pissadaki and Bolam, 2013), resulting in high demand for ATP to maintain the Ψmito, action potential, and synaptic transmission. Secondly, SN dopaminergic neurons generate constant action potentials autonomously without dependency on synaptic input to maintain dopamine levels in surrounding brain regions (Grace and Bunney, 1983; Romo and Schultz, 1990). Thirdly, dopaminergic neurons are Ca2+ pacemakers with constant buffering activity (Olson et al., 2005). Increased Ca2+ levels might boost ETC activity leading to a pathological increase in ROS and the initiation of apoptotic pathways (Joza et al., 2001; Malhotra and Kaufman, 2007). In summary, all these processes contribute to an immense metabolic burden and the need for functional mitochondria, ROS′ major primary production site. Besides that, the accumulation of α-synuclein itself provokes the generation of mtROS. Data of transgenic mouse models could prove that α-synuclein aggregation diminishes complex I activity and increase ROS levels (Hsu et al., 2000; Martin et al., 2006) before dopaminergic neuron loss (Subramaniam et al., 2014). Inhibition of complex I, ROS production, and neuronal cell death via apoptosis and autophagy was also linked to the presence of PD-associated gene mutations [α-synuclein (SNCA), LRRK2, PARK7, PARK2, PINK1] (Müftüoglu et al., 2004; Yamada et al., 2004; Iaccarino et al., 2007; Hayashi et al., 2009; Ho et al., 2009; Gusdon et al., 2012; Venderova and Park, 2012; Dias et al., 2013; Blesa et al., 2015; Gegg and Schapira, 2016). Oxidative stress by complex I inhibition can be pharmacologically mimicked by environmental toxins, including 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridin (MPTP) and rotenone (Mizuno et al., 1987; Schapira et al., 1990; Ramsay et al., 1991; Richardson et al., 2005), leading to superoxide generation and reduction of ATP synthesis. Treatment with these substances shows similar upregulation of cell death pathways as seen in PD (Hayley et al., 2004; Clayton et al., 2005; Perier et al., 2005).
3.4 Cancer
3.4.1 Clinical Significance
While malignant tumors can occur at any age, cancer disproportionately strikes the elderly aged 65 years or older. The median age of cancer-related death is 71–77 years, independent of sex and race (Yancik, 2005). Consequently, in an aging society, the cancer burden is still expected to increase in the following centuries. The hallmarks of cancer include genome instability, mutations, replicative immortality, and cell death resistance, as well as angiogenesis, deregulation of cellular metabolism, tumor-promoting inflammation, and avoidance of immune destruction. Therefore, cancer cells exhibit high rates of proliferation, invasion, and metastasis (Somarelli et al., 2020). Mitochondria provide energy and building blocks for new cells and modulate ROS homeostasis, oncogenic signaling, and apoptosis. Consequently, these organelles are essential in cancer development and progression (Zong et al., 2016). While the Warburg effect suggested that cancer is accompanied by mitochondrial defects, forcing cancer cells into increased aerobic glycolysis, it was proven in the following years that cancer cells still exhibit functional mitochondria and also rely on mitochondrial respiration to obtain sufficient energy (Mazurek, 2011). Mitochondria also seem to play a crucial role in the development of tumors by triggering cell integrity loss through mutations in mtDNA and the generation of ROS (Badrinath and Yoo, 2018). In line with these in vitro findings, clinical trials revealed that oxidative stress correlates with the development and progression of various cancer types, including colorectal cancer (Boakye et al., 2020; Janion et al., 2020), bladder cancer (Wigner et al., 2021), breast cancer (Lee et al., 2017), and prostate cancer (Oh et al., 2016).
3.4.2 Cellular Mechanisms and Signaling
Cancer cells exhibit significantly higher levels of ROS than corresponding non-cancerous cells. This increase in ROS is triggered by enhanced metabolic rate, gene mutation, and hypoxia (Perillo et al., 2020). Adaption to these excessive ROS conditions is achieved by cancer cells through enhanced antioxidant capacity. Therefore, the main transcription factor involved in the antioxidant defense, the nuclear factor erythroid 2-related factor 2 (NRF2), is often upregulated in cancer cells and helps via boosting antioxidant defense mechanisms the proliferation of cancer cells (Jaramillo and Zhang, 2013). Besides, glutathione and thioredoxin antioxidant pathways synergize to drive cancer initiation and progression. For instance, inhibition of glutathione synthesis resulted in enhanced levels of thioredoxins. Consequently, just combined blockage of glutathione and thioredoxins resulted in cancer cell death in vitro and in vivo (Harris et al., 2015). Besides, the antioxidant potential might be further promoted through NADPH production. Interestingly, pyruvate kinase M2 was found to be predominantly present in a dimeric state in cancer cells, exhibiting less activity and forming a bottleneck in glycolysis. Consequently, the glucose flux gets redirected to the pentose phosphate pathway, where NADPH is produced (Mazurek et al., 2005; Hawk et al., 2016). Thereby, the antioxidant potential of cancer cells gets again improved.
3.5 Inflammation and Pain
3.5.1 Clinical Significance
Inflammation is the body’s response to pathogens, external injuries, damaged cells, or irritants. Thereby, immune cells release various inflammatory mediators to dilate small blood vessels. The thereby increased blood flow allows the transport of immune system cells to the affected tissues for repair (Abdulkhaleq et al., 2018). The release of proinflammatory and immune-active substances like cytokines and chemokines can result in nerve irritation and pain signals (Abdulkhaleq et al., 2018). For instance, the proinflammatory mediator histamine is well-known to induce itching (Shim and Oh, 2008). While injuries or infections might cause intermittent increases in inflammation, chronic systemic inflammation represents the main cause for diseases such as CVD, diabetes mellitus, cancer, chronic kidney and liver diseases, and autoimmune and neurodegenerative disorders, which strongly contribute to disability and mortality worldwide (Furman et al., 2019). Inflammatory processes induce oxidative stress and reduce cellular antioxidant capacity, causing loss of tissue integrity, impaired protein function, and DNA damage. Consequently, the combination of chronic inflammation and oxidative stress is a major hallmark of age-related diseases (Khansari et al., 2009). For instance, oxidative stress parameters like enhanced levels of malonaldehyde and superoxide anions and decreased SOD activity correlated with inflammation markers, including high sensitive C-reactive protein and fibrinogen, in patients with coronary heart disease (Kotur-Stevuljevic et al., 2007). Also, a correlation between inflammation and ROS levels was suggested as a universal parameter in patients with infective endocarditis (Ostrowski et al., 2012). Besides, spontaneous ROS production by neutrophils was associated with low-grade inflammation in the elderly (Ogawa et al., 2008), emphasizing that ROS production might represent a crucial aspect in age-associated immune dysregulation.
3.5.2 Cellular Signaling and Mechanisms
While pro-inflammatory processes increase ROS production (Yang et al., 2007), ROS are, in turn, also involved in the activation of pro-inflammatory processes such as mast cell activation and subsequent release of pro-inflammatory mediators (Son et al., 2006). For instance, hydrogen peroxide was shown to modulate the NF-kB signaling pathway associated with an inflammatory response. Several ROS-induced modifications were found at NF-kB, leading to activation of the NF-kB at the early phase of oxidative stress but attenuation of NF-kB activity in case of sustained stress (Lingappan, 2018). In addition, ROS are also utilized by inflammatory agonists as signaling molecules. For instance, oxidative stress produced by polymorphonuclear neutrophils during inflammation causes the opening of inter-endothelial junctions and thereby allows inflammatory cells to pass the endothelial barrier. Then, the migrated inflammatory cells contribute to the clearance of pathogens and also lead to tissue injury. Besides, ROS quickly react with nitric oxide to generate reactive nitrogen species, which induces nitrosative stress, and so adds to the pro-inflammatory impact of ROS (Mittal et al., 2014). Moreover, mitochondrial ROS production was found to convey lipopolysaccharide-driven production of proinflammatory cytokines (Bulua et al., 2011) and was identified as a major step in the activation of inflammasomes, multiprotein oligomers, which promote the secretion of pro-inflammatory cytokines (Yang et al., 2019). Acute inflammations are often induced by infections caused by bacteria, viruses, protozoa, or fungi. Thereby, ROS are used by the immune system to protect the host organism against infections. In response to inflammatory processes, phagocytes reside within the tissue to phagocyte microbes. Dependent on the microbe, phagocytes generate ROS signals to directly kill the microbes and activate ROS bursts within the cell to induce respective signaling cascades in order to eliminate pathogenes by non-oxidative mechanisms (Paiva and Bozza, 2014). Besides, ROS and peroxynitrite are also directly engaged in the nociceptive signaling by altering protein kinase A and calcium/calmodulin-dependent protein kinase type II-mediated signaling, glutamatergic neurotransmission, transient receptor potential cation channel subfamily V member 1 (TRPVI) sensitization, and cyclooxygenase enzyme (COX) activation (Salvemini et al., 2011). Interestingly, clinical trials revealed that administration of SOD1, known as the drug orgotein, reduced symptoms of osteoarthrosis of the knee joint significantly better than methylprednisolone acetate (Gammer and Brobäck, 1984), emphasizing the crucial role of ROS in the development of pain and the potential of ROS manipulation as a treatment of pain.
4 Reactive Oxygen Species Modulation by Approved Drugs
4.1 Cardioprotective Drugs
4.1.1 Beta-Blocker
Beta-blockers comprise compounds that inhibit the activation of β-adrenergic receptors by endogenous catecholamines. The first beta blocker, propranolol, was approved in the 1960s to treat angina pectoris and revolutionized the treatment of CVD. Nonselective β1 and β2 adrenoreceptor blockers like propranolol and carvedilol and specific β1 adrenoreceptor blockers such as atenolol, metoprolol, and bisoprolol are nowadays widely used to ameliorate cardiac function and reduce the mortality rate in heart failure patients (Srinivasan, 2019). Moreover, beta-blockers are widely used medications to treat hypertension. Stimulation of β1 receptors induces positive chronotropic and inotropic effects in the heart muscle and modulates arterial vasoconstriction by the release of renin in the kidney. β2-adrenergic receptors are located in various organs, including the liver and vascular smooth muscle, and β2 receptor activation causes smooth muscle relaxation (Farzam and January 2021). Beta-blockers affect ROS homeostasis indirectly via different mechanisms. First, inhibition of β1 adrenergic receptors prevents oxidative stress due to catecholamine-induced reactions. Notably, ROS might be essential in conveying the action of catecholamines by adjusting the homeostasis of mitochondrial iron, critical for rate-limiting enzymes of the TCA cycle and for the mitochondrial electron transport chain (Tapryal et al., 2015). However, elevated levels of the catecholamines adrenaline and noradrenaline are associated with enhanced oxidative stress and were found in various cardiovascular dysfunctions and diseases, including tachycardia, arrhythmias, heart failure, and ischemic reperfusion injury (Nakamura et al., 2011). For instance, incubation of freshly isolated rat cardiomyocytes with adrenaline boosted the activity of mitochondrial complexes and caused increased expression of SOD2 after 3 h of incubation, potentially due to enhanced electron leakage from the ETC and a boost in ROS production (Costa et al., 2009). Second, beta-blocker might reduce ROS production indirectly by lowering mechanical stress in vessels. Cyclic stretching increased ROS and a ROS-dependent activation of a signaling cascade, including extracellular signal-regulated kinases (ERK1/2) and JNK in neonatal rat ventricular myocytes (Pimentel et al., 2001). Third, the nonselective β1 and β2 adrenoreceptor blocker carvedilol was found to scavenge ROS directly and might also inhibit α1 stimulated hypertrophic signaling mediated by ROS (Nakamura et al., 2011). Due to its pleiotropic effects, including antioxidant actions or enhancement of insulin sensitivity (Nguyen et al., 2019), carvedilol was speculated to be more effective than other beta-blockers like metoprolol or bisoprolol in reducing the mortality rate in humans (Rain and Rada, 2015). However, a clinical trial in patients with chronic systolic heart failure revealed carvedilol to be less effective than bisoprolol in decreasing levels of troponin T, ameliorating inflammation, and increasing forced expiratory volume. Nevertheless, the impact of carvedilol on oxidative stress markers was more pronounced (Toyoda et al., 2020). For instance, carvedilol was applied in patients with dilated cardiomyopathy and enhanced oxidative DNA damage, significantly reducing oxidative DNA damage, lipid peroxidation and ameliorating heart failure (Nakamura et al., 2002; Kono et al., 2006). Besides carvedilol, also the β1-selective beta-blocker nebivolol was shown as a direct antioxidant either by scavenging free radicals or by acting as a chain breaker through proton donation or electron stabilization (Gao and Vanhoutte, 2012). Besides, nebivolol was found to inhibit ROS formation by reducing the activity and expression of the vascular NOX in angiotensin II-treated animals and cells (Oelze et al., 2006). Notably, the ratio of reduced glutathione to oxidized glutathione was significantly increased in patients with essential hypertension after treatment with carvedilol, while nebivolol-treated patients did not show significant differences in this parameter but showed increased nitrogen dioxide plasma concentrations (Zepeda et al., 2012). These reports suggest that the proper use of different beta-blockers might be dependent on the individual pathophysiology.
4.1.2 ACE Inhibitors/AT1 Antagonists
Angiotensin-converting enzyme (ACE) inhibitors prevent the conversion of angiotensin I into angiotensin II that binds to the angiotensin II receptor (AT1) in blood vessels to mediate its vasoconstrictive effect (Burnier, 2001), whereas AT1 receptor antagonists directly inhibit the binding of angiotensin II to AT1 receptors (Gradman, 2002). Consequently, ACE inhibitors are used to control blood pressure to reduce mortality in patients with congestive heart failure and in patients with high cardiovascular risk profiles, including diabetes. Moreover, ACE inhibitors are essential in delaying the progression of chronic renal diseases since they lower proteinuria. The first orally active ACE inhibitor, captopril, got approved by the FDA in 1981. Similar effects as for ACE inhibitors could be achieved by applying AT1 receptor antagonists, first approved by the FDA as losartan in 1995 (Ripley and Hirsch, 2010). ACE inhibitors and AT1 antagonists are supposed to diminish the angiotensin II-mediated generation of ROS and partly also directly scavenge ROS production. Angiotensin II was found to modulate the pressor effect through ROS signaling in the glutamatergic neuron in stress-induced hypertensive rats. Thereby, NAPDH oxidase-derived ROS activates the SAPK and the JNK, promoting the expression of AT1 receptors in glutamatergic neurons. Consequently, glutamate gets released into the spinal cord and leads to the pressor response (Jiang et al., 2018). Besides, the AT1 receptor antagonist candesartan was found to blunt the tumor necrose factor α (TNFα)-induced inflammatory cytokine production of embryonic kidney epithelial cells by inhibiting oxidative stress. Notably, knockdown of the AT1 receptor did not alter candesartan’s impact on ROS activity in humans (Yu et al., 2019). Angiotensin II was found to enhance ROS formation via AT1 receptor activation in old sheep, which was counteracted by the application of ACEII inhibitors (Gwathmey et al., 2010). Moreover, disruption of the AT1 receptor in mice caused reduced oxidative damage and significantly promoted longevity (Benigni et al., 2009). Application of the ACE inhibitor lisinopril attenuated ROS formation and counteracted cardiovascular remodeling in diabetic rats to the same extent as the antioxidant N-acetyl-l-cysteine (NAC) (Fiordaliso et al., 2006). Notably, combined application of the ACE inhibitor temocapril with the AT1 antagonist olmesartan induced a more pronounced suppression of ventricular hypertrophy and fibrosis in a diastolic heart failure rat model in comparison to the monotherapy with temocapril. This benefit was associated with an additive effect on the blockage of ROS generation and inflammation signaling (Yoshida et al., 2004). Besides, it was discussed whether thiol-carrying compounds like alacepril might function as direct ROS scavenging agents. For instance, 0.6–0.7 mM of alacepril reduced ROS production in bronchoalveolar lavage cells from chronic obstructive pulmonary disease patients by 50%, while 3–4 mM of thiol-free lisinopril was necessary to achieve the same effect (Teramoto et al., 2000), suggesting that Moreover, thiol-carrying captopril was more effective against copper-induced oxidative modification on lipids and proteins than the non-thiol ACE inhibitors enalapril and lisinopril (Fernandes et al., 1996). However, the non-thiol carrying AT1 receptor antagonist candesartan inhibited oxidative stress in embryonic kidney epithelial cells independent of AT1 receptor activity (Yu et al., 2019). Consequently, it remains questionable whether the thiol-group is necessary for the direct antioxidant properties of some ACE inhibitors and AT1 antagonists.
4.1.3 Statins
Statins inhibit the rate-limiting step in cholesterol synthesis by blocking the liver enzyme 3-hydroxy-3-methyl-glutaryl-coenzyme A (HMG-CoA) reductase that converts HMG-CoA to mevalonic acid. Consequently, cholesterol levels in the blood drop, and the potential side effects of hyperlipidemia are prevented. The first statin approved by the FDA as therapy for preventing coronary atherosclerotic events was lovastatin in 1987 (Harrington, 2017). HMG-CoA reductase is a crucial enzyme in the mevalonate pathway. Blocking of HMG-CoA reductase also reduces the bioavailability of various products of the mevalonate pathway, including heme A, ubiquinone, isoprenoids, corticosteroids, and vitamin D. Consequently, statins affect mitochondrial function indirectly via mevalonate pathway metabolite depletion. Besides, also direct impairment of the ETC activity was reported (Mollazadeh et al., 2021). Notably, statins exhibit opposite effects on mitochondria of cardiac and skeletal muscles (Sirvent et al., 2005; Bouitbir et al., 2012). A different effect on mitochondrial respiration is discussed as a potential reason. For instance, simvastatin was found to inhibit complex I of the ETC in human and rat skeletal muscle samples, while cardiomyocytes remained largely unaffected (Sirvent et al., 2005). Notably, statins were found to trigger a mitohormetic response by a transient ROS signaling in cardiac tissues, resulting in the upregulation of ROS detoxifying enzymes. At the same time, an enhanced level of ROS displayed harmful actions on skeletal muscle tissues (Bouitbir et al., 2012). In line with this finding, ROS production was decreased and oxidative capacities and peroxisome proliferator-activated receptor-gamma activator 1 (PGC-1) expression enhanced in the atrium of patients treated with atorvastatin, while statin-induced muscular myopathy was accompanied by reduced oxidative capacities, a side-effect counteracted by the application of antioxidant molecules (Bouitbir et al., 2012). Analysis of skeletal muscle biopsy samples from patients with statin-associated myopathy confirmed an enhanced hydrogen peroxide production after statin treatment. However, a difference between slow- and fast-twitching muscle fibers fueled by a greater extent of glycolysis could be detected: Atorvastatin treatment increased hydrogen peroxide accumulation, decreased GSH/GSSG ratios, and triggered apoptotic pathways in the glycolytic plantaris muscle of rats, while the oxidative soleus muscle was largely unaffected due to high antioxidative capacity (Bouitbir et al., 2016). Consequently, the response of different cell types to statin-induced initial ROS burst is probably dependent on the individual metabolic state and potential for antioxidant actions. Thereby, oxidative muscle fibers might be better adjusted to enhanced mitochondrial activity and to related side products like ROS. For instance, an increase in ROS is limited in cardiac myofibres due to their highly efficient antioxidant systems, causing PGC-1α activation and, thereby, mitochondrial biogenesis and function, while cells with lower antioxidant capacity face a giant ROS burst and cellular damage (Mollazadeh et al., 2021). Treatment with antioxidants might be a potential solution to counteract the destructive action of statins in muscle fibers. However, a clinical study revealed that tocopherol supplementation in addition to pravastatin treatment for half a year did not further improve lipid levels or the frequency of adverse effects, including muscle damage in older adults (Carlsson et al., 2002), highlighting that boosting cellular antioxidant defense mechanisms might be a more promising strategy to counteract potential side-effects of statins. Besides, lipophilic statins like cerivastatin, fluvastatin, atorvastatin, and simvastatin specifically decreased glutamate-driven state 3 respiration and induced mitochondrial swelling, cytochrome c release, and DNA fragmentation in rat skeletal muscle cells. In contrast, the hydrophilic pravastatin did not impair mitochondrial function (Kaufmann et al., 2006). Based on these results, administration of hydrophilic statins might prevent mitochondrial accumulation and, thus, harmful effects on the skeletal muscles.
4.1.4 Platelet Aggregation Inhibitors (“Antiplatelets”)
Antiplatelet medications are used in the primary and secondary prevention of thrombotic diseases by decreasing platelet aggregation and thrombus formation. Oral antiplatelets are classified regarding their mechanism of action, including platelet aggregation inhibitors aspirin and clopidogrel. Low-dose aspirin, 75–150 mg once a day (Cryer, 2002), is the most prominent antiplatelet drug, suppressing prostaglandin and thromboxane production through irreversible inactivation of COX. Thereby, the formation of the pro-thrombotic thromboxane A2 in platelets is blocked (Iqbal et al., 2021). Approved around 1900 to treat fever, pain, and inflammation, the compound experienced a revival in the last decades of the 20th century by widespread use as prevention against cardiovascular incidents (Tsoucalas et al., 2011). Nowadays, low-dose aspirin is one of the most popular antiplatelet therapies for the treatment of patients with the acute coronary syndrome (Amsterdam et al., 2014; Roffi et al., 20152016) and for the prevention of atherothrombotic complications in high-risk patients (Parekh et al., 2013; Patrono, 2015). Aspirin was found to inhibit ROS production by downregulation of NOX4 and the inducible nitric oxide synthase in human endothelial cells exposed to oxidized LDL (Chen et al., 2012). Besides, low doses of aspirin also increased the expression of SOD1 and SOD2 in rat astrocytes treated with the toxic peptide Aβ (Jorda et al., 2020). Notably, a double-blind, randomized study revealed that the combined application of low-dose aspirin with vitamin E caused a significant reduction in platelet adhesiveness compared to aspirin only. However, the incidence of hemorrhagic strokes increased in patients treated with both drugs, reaching no statistical significance due to the low number of cases (Steiner et al., 1995). These findings highlight the potential of antioxidant defense mechanisms in the prevention of platelet aggregation but once again question the usage of ROS scavengers.
4.2 Oral Antidiabetic Drugs
4.2.1 Metformin
Metformin was first approved in the United Kingdom in 1958 and got the first-line therapy for T2DM (Scarpello and Howlett, 2008). Metformin shows versatile anti-diabetic effects in various organs and tissues (Foretz et al., 2019). Firstly, metformin impairs glucose absorption in the intestine by increasing the secretion of glucose-lowering hormone glucagon-like peptide (GLP-1) (Mannucci et al., 2004). Secondly, metformin promotes glucose uptake in peripheral tissues by glucose transporter 4 (GLUT4) translocation to the plasma membrane, which allows increased blood glucose clearance and thus counteracts glycemia (Musi et al., 2002; Natali and Ferrannini, 2006; Boyle et al., 2011; Grzybowska et al., 2011; Lee et al., 2012b; Mummidi et al., 2016). Consequently, metformin attenuates fasting plasma insulin levels and helps to restore insulin sensitivity (Grzybowska et al., 2011). Thirdly, metformin inhibits complex I of the respiratory chain, causing an energy deficit leading to the activation of AMP-activated protein kinase (AMPK) (El-Mir et al., 2000; Owen et al., 2000; Zhou et al., 2001). AMPK signaling, in turn, hampers glucose production by inhibition of mitochondrial glycerol-3 phosphate dehydrogenase (Madiraju et al., 2014) and glucagon-stimulated hepatic gluconeogenesis (Miller et al., 2013). Besides that, pAMPK signaling regulates multiple other downstream pathways such as (Jaul and Barron, 2017) nutrient sensing by inhibition of mTORC1 and activation of SIRT1, as well as (Hayyan et al., 2016) initiation of mitochondrial biogenesis through PGC1α, (Tejero et al., 2019), inhibition of pro-inflammatory signaling via NFkB, and (Sun et al., 2010) the regulation of autophagy (Semancik and Vanderwoude, 1976; Suwa et al., 2006; Salminen and Kaarniranta, 2012; Aatsinki et al., 2014; Barzilai et al., 2016; Zhou et al., 2016; Herzig and Shaw, 2018). In addition, metformin-induced AMPK signaling stabilizes the transcription factor NRF2 (Onken and Driscoll, 2010), a master regulator of redox regulations, consequently initiating the expression of antioxidant genes such as CAT, GSH, SOD (Ashabi et al., 2015). The upregulation of antioxidant defense enzymes eventually leads to a decrease in ROS, an impairment of NOX, and a boost of SOD expression (Diniz Vilela et al., 2016; Shin et al., 2017). Inhibition of NOX by metformin highly contributes to the regulation of redox homeostasis as NOX-derived ROS represents the primary source of high glucose-induced oxidative stress (Inoguchi et al., 2000; Kim et al., 2002; Inoguchi et al., 2003). In addition, metformin interferes with RNS production and thereby diminishes nitro-oxidative stress. For instance, it was shown that the bioavailability of nitric oxide, a contributor to endothelial function, was improved by metformin, while levels of cytotoxic peroxynitrite were decreased in diabetic rats (Sambe et al., 2018).
In accordance with metformin-dependent activation of AMPK signaling and the consequent induction of redox regulatory processes, several in vitro studies presented antioxidant effects of metformin (Marycz et al., 2016; Ahangarpour et al., 2017; Smieszek et al., 2017; Algire et al., 2012; Abd-Elsameea et al., 2014). A randomized clinical trial investigating the impact of metformin on ROS homeostasis of T2DM patients found an improvement in the antioxidant status and a cardioprotective effect upon metformin treatment (Chakraborty et al., 2011). In addition to the interference with redox regulatory processes, metformin itself displays direct antioxidant actions by detoxifying hydroxyl radicals, as seen in murine in vitro and in vivo models of oxidative liver injury and cardiac fibrosis and human monocytes/macrophages (Mummidi et al., 2016; Dai et al., 2014; Buldak et al., 2014). Metformin supplementation was further linked to anti-inflammatory and anti-apoptotic processes in several studies investigating neurodegeneration and multiple sclerosis (Nath et al., 2009; Ullah et al., 2012; Alzoubi et al., 2014). Metformin interferes with the production of IL1β, a pro-inflammatory cytokine responsible for pancreatic β-cell apoptosis (Kelly et al., 2015). This mechanism counteracts ROS-dependent increases in IL1β expression in an AMPK-independent fashion (Bauernfeind et al., 2011). The same study revealed that metformin raises levels of the anti-inflammatory cytokine IL-10 (Bauernfeind et al., 2011). Clinical studies observed metformin’s role in preserving cognitive function (Ng et al., 2014), resulting in reduced depressive behavior (Guo et al., 2014) and decreased mortality in diabetic patients (Barzilai et al., 2016). Importantly, metformin-dependent health benefits go beyond glycemic control and include beneficial effects against various types of cancer (Heckman-Stoddard et al., 2017), CVD (Rena and Lang, 2018), neurodegenerative disorders (Rotermund et al., 2018), and autoimmune diseases (Ursini et al., 2018). Several preclinical and clinical studies have strong evidence for a geroprotective potential of metformin (Barzilai et al., 2016; Glossmann and Lutz, 2019; Piskovatska et al., 2019; Soukas et al., 2019). In addition, epidemiological and association studies show that metformin is linked to reduced incidences and all-cause mortalities in several age-related diseases, such as age-associated cancers and AD (Barzilai et al., 2016; Campbell et al., 2017; Valencia et al., 2017). Based on these promising results, the “targeting aging with metformin” (TAME, ClinicalTrials.gov Identifier: NCT02118727) study currently investigates metformin’s potential in aging and its therapeutical potential in age-related diseases (Campisi et al., 2019; Wang et al., 2020).
4.2.2 DPP4 Inhibitors and GLP-1 Agonists
Inhibitors of dipeptidyl peptidase 4 (DPP4), so-called gliptins, and glucagon-like protein 1 (GLP-1) receptor agonists (GLP-1RAs), also known as incretin mimetics, represent two drug classes that tackle the same pathway by acting in opposing ways. While gliptins increase the stability of GLP-1 by preventing its degradation, GLP-1RAs mimic GLP-1 and thus promotes glucagon suppression and insulin secretion (Deacon et al., 2012). DPP4 is a serine protease responsible for the degradation of proteins, including the incretins GLP-1 and gastric inhibitory peptide (GIP), two metabolic hormones involved in the attenuation of blood glucose levels. Elevated DPP4 activity is a risk factor for developing metabolic syndrome and T2DM (Zheng et al., 2014) and is associated with insulin resistance (Sell et al., 2013). As a result, DPP4 deficiency in mice manifests in improved glucose tolerance (Marguet et al., 2000) and decreased obesity and insulin resistance (Conarello et al., 2003). Besides lowering plasma insulin levels, treatment with the DPP4 inhibitors vildagliptin and sitagliptin successfully improved oxidative stress parameters in obese insulin-resistant rats (Apaijai et al., 2013). Another study reported that vildagliptin and sitagliptin positively affected mitochondrial oxidative stress and mitochondrial function, resulting in enhanced cognition and hippocampal brain function in high-fat diet-induced insulin-resistant Wistar rats (Pintana et al., 2013). Advanced glycation endproducts (AGEs) represent a measure of oxidative stress in T2DM. It was shown that crosstalk between AGEs, the receptor for AGEs (RAGE), and the DPP4-incretin system adds up to diabetic vascular complications (Yamagishi et al., 2015). Thereby, DPP4 positively correlates with ROS production and RAGE gene expression (Ishibashi et al., 2013). This process could be reversed by DPP4 inhibition via linagliptin supplementation in endothelial cells (Ishibashi et al., 2013). Similar results were obtained upon teneligliptin treatment resulting in reduced adverse effects of AGEs in mouse peritoneal macrophages and THP-1 cells (Terasaki et al., 2020). In general, oxidative stress markers and inflammatory cytokines were attenuated in T2DM patients receiving DPP4 inhibitor treatment for 4–16 weeks (Rizzo et al., 2012; Tremblay et al., 2014). Besides counteracting oxidative stress, DPP4 inhibitors improve mitochondrial function in rats on a high-fat diet (Apaijai et al., 2013; Pintana et al., 2013; Pipatpiboon et al., 2013) and increase mitochondrial biogenesis and exercise capacity in a mouse model for ischemic heart failure (Takada et al., 2016). Similar to this, GLP-1 agonists stimulated mitochondrial biogenesis and antioxidant defense systems by modulation of PPAR signaling in PC12 cells and mice treated with GLP-1RA (An et al., 2015). This manifests in increased mitochondrial mass and function associated with improved pancreatic β-cell function in INS-1 rat insulinoma cells (Kang et al., 2015). From a mechanistic point of view, treatment with the GLP-1 agonist extendin-4 resulted in upregulation of superoxide dismutase and protected against ROS-induced apoptosis in adipose-derived mesenchymal stem cells (Zhou et al., 2014). Moreover, the GLP-1 agonists, liraglutide, D-ser2-oxyntomodulin, a GLP-1/GIP dual receptor agonist, dAla (2)-GIP-GluPal, Val(8)GLP-1-GluPal and exendin-4 enhanced the expression of the autophagy-associated marker protein atg7 and pyruvate dehydrogenase and improved mitochondrial function in neuronal SH-SY5Y cells (Jalewa et al., 2016).
4.2.3 Glitazones
Glitazones, also known as thiazolidinediones (TZDs), are approved antidiabetic drugs and include compounds such as rosiglitazone and pioglitazone (Hauner, 2002). They represent specific agonists of the peroxisome proliferator-activated receptor γ (PPARγ) and thereby modulate its downstream metabolic regulations (Day, 1999). Their hypoglycemic and antidiabetic effects result from increased glucose absorption and insulin sensitivity in peripheral tissues (Hauner, 2002). Similar to metformin, TZDs were described to inhibit complex I of the respiratory chain in vitro activity assays (Brunmair et al., 2004) and promote cell survival by maintaining the Ψmito via PPARγ signaling in lymphocytes (Wang et al., 2002). Pioglitazone was shown to counteract oxidative stress and inflammation, increase mitochondrial biogenesis in non-alcoholic fatty liver disease (Bogacka et al., 2005), and attenuate mitochondrial-induced oxidative damage in human subcutaneous adipose tissue human neuron-like cells (Bogacka et al., 2005; Ghosh et al., 2007). In accordance with these findings, pioglitazone increases the SOD1 activity and inhibits NOX expression in rat mesangial cells (Wang et al., 2013). Bolten et al. (Bolten et al., 2007) concluded that observed hypoglycemic effects are more likely a consequence of improved mitochondrial function rather than PPARγ signaling. In contrast, treatment of human hepatoma cells with troglitazone caused severe side effects and mitochondrial structure injuries, which were less potent upon treatment with rosiglitazone or pioglitazone in similar concentrations (Hu et al., 2015). As a consequence, troglitazone was withdrawn as an antidiabetic drug due to hepatotoxicity and mitochondrial toxicity side effects just 3 years after its approval in 2000 (Hu et al., 2015).
4.2.4 SGLT2 Inhibitors
Glucose is re-absorbed via active or passive transport processes during blood filtration in the proximal renal tubule of kidneys (Vallon and Thomson, 2017). One crucial player during this process is the sodium-glucose cotransporter 2 (SGLT2) (Kalra, 2014), which can be pharmacologically inhibited by SGLT2 inhibitors. Such compounds prevent the re-uptake of glucose and favor glucose secretion independent of insulin (Chao, 2014), thus representing antidiabetic drugs to counteract glycemia. Furthermore, SGLT2 inhibitors impair gluconeogenesis and increase insulin sensitivity and insulin secretion of β-cells (Han et al., 2008; Ferrannini et al., 2014; Wilding et al., 2014; Kern et al., 2016). More importantly, SGLT2 inhibitors comprise antioxidant properties by reducing free radical production and strengthening the antioxidant system (Osorio et al., 2012; Ishibashi et al., 2016). Experiments in mice revealed an improved redox state, diminished oxidative damage (Sugizaki et al., 2017), and enhanced mitochondrial function, eventually leading to a balanced ROS homeostasis in the brain (Sa-Nguanmoo et al., 2017). Mechanistically, SGLT2 inhibitors affect the activity and expression of prooxidant enzymes such as NOX, eNOS, and XO (Oelze et al., 2014; Kawanami et al., 2017). For instance, empagliflozin treatment in diabetic rat models led to the downregulation of NOX1 and NOX2 (Oelze et al., 2014). Moreover, NOX4 expression was shown to be impaired by dapagliflozin (Steven et al., 2017). In both cases, free-radical generation and oxidative damage are counteracted (Habibi et al., 2017; Steven et al., 2017). In addition to the depletion of prooxidant processes, SGLT2 inhibitors also strengthen the antioxidant defense system. Several studies show that expression of CAT, SOD, and GPX are increased in diabetic animal models in the presence of phlorizin (Osorio et al., 2012), dapagliflozin (Shin et al., 2016), and TA-1887 (Sugizaki et al., 2017), another SGLT2 inhibitor.
4.2.5 Alpha-Glucosidase Inhibitors
Alpha-glucosidase inhibitors, such as acarbose and miglitol, delay the digestion of carbohydrates by inhibiting alpha-glucosidase enzymes in the small intestines and thereby preventing postprandial hyperglycemia. The alpha-glucosidase inhibitor acarbose reduces inflammatory cytokine production, as seen in reduced levels of interferon-gamma induced protein 10 kD, monocyte chemoattractant protein-1, macrophage-derived chemokines, TNFα as well as NF-kB activity in THP-1 cells (Lin et al., 2019). Moreover, it was observed that acarbose co-treatment with insulin reduced inflammation and oxidative stress in diabetic individuals (Li et al., 2016). Reduced levels of superoxide might be the consequence of acarbose-dependent inhibition of NOXes in the aorta, heart, and kidney of obese diabetic rats (Rösen and Osmers, 2006). Furthermore, inhibition of NOX4 oxidase-dependent superoxide production was seen in rat aortic endothelial cells and is linked to anti-inflammatory regulations (Li et al., 2019).
4.2.6 Sulfonylurea and Glinide
Sulfonylurea inhibits ATP-sensitive K+ channels in the plasma membrane of β-cells and initiates insulin release and hypoglycemia (Groop, 1992). Sulfonylureas, including gliclazide, glibenclamide, and glimepiride, do also affect ATP-sensitive K+ channels in the inner mitochondrial membrane and thereby modify mitochondrial function (Inoue et al., 1991; Suzuki et al., 1997; Szewczyk et al., 1997; Argaud et al., 2009). Moreover, gliclazide treatment in rat models reduces oxidative stress and inflammation via several mechanisms, including upregulation of antioxidant enzymes such as SOD, CAT, and GPX1 (Del Guerra et al., 2007; Alp et al., 2012; Araújo et al., 2019).
4.3 Anti-degenerative Drugs
4.3.1l-Dopa (or Levodopa) and Dopamine Agonists
Until now, l-dopa is considered as “gold standard” for PD therapy (Nagatsu and Sawada, 2009). In the late 1960s, high-dose l-dopa treatment was shown to result in remarkable clinical efficacy in PD patients by restoring dopamine levels in the brain (Barbeau et al., 1961) and was first approved in 1970 (Abbott, 2010). Despite its effectiveness, long-term treatment with l-dopa often results in motor complications, including abnormal involuntary movements (Pahwa et al., 2006; Fabbrini et al., 2007). Similar to this, treatment with dopamine agonists is associated with a range of side effects, from mild to severe implications (Faulkner, 2014). It was shown that degradation of dopamine after l-dopa supplementation results in a dose-dependent increase in ROS and cell death of serotonergic neurons (Stansley and Yamamoto, 2013). These observations underline that both l-dopa and dopamine agonists are thought to act symptomatically only (Bonuccelli, 2003; Segawa et al., 2003; Nagatsu and Sawada, 2009; Blandini and Armentero, 2014), emphasizing the urgent need for more potent drugs that target early dysregulations of the disease, such as oxidative stress.
4.3.2 MAO-B Inhibitors
MAO-B-inhibitors against PD include the irreversible inhibitor selegiline (L-deprenyl), which was first approved by the FDA in 1996, followed by rasagiline in 2006 (Knudsen Gerber, 2011), as well as safinamide, the first reversible FDA-approved MAO-B inhibitor against PD available for clinical use since 2015 (Deeks, 2015). In preclinical models, selegiline was shown to increase levels of antioxidant enzymes such as glutathione and SOD, improve oxidative stress biomarkers, and reduce neuronal loss in rats (Kumar et al., 2018; Ahmari et al., 2020). Similar effects were obtained with rasagiline which attenuated oxidative stress in rats, as measured by levels of 7-ketocholesterol and GSSG/GSH ratio (Aluf et al., 2013).
Clinical trials with safinamide alone or in combination with levodopa or dopamine agonists (pergolide, ropinirole, pramipexole, cabergoline) confirmed improved PD symptoms (Martínez-Martín et al., 1994; Stocchi et al., 2006; Wasan et al., 2021). However, the clinical potential of MAO-B inhibitors to attenuate oxidative stress by inhibiting MAO-induced hydrogen peroxide production remains to be shown as clinical evidence of improved oxidant status in PD patients is lacking. Consequently, it is questionable whether observed positive effects with MAO-B inhibitors are due to neuroprotection or instead limited to symptomatic benefits such as maintaining dopamine levels (Schulzer et al., 1992; Shoulson, 1992; Stocchi et al., 2006).
4.3.3 Repurposing of Antidiabetics as Antidementia Drug
Notably, AD and PD show alterations in oxidative stress levels, hyperglycemia, mitochondrial dysfunction, glucose metabolism, insulin signaling, insulin resistance, and inflammatory processes (Baker et al., 2011; Moran et al., 2013; Willette et al., 2015; Morsi et al., 2018; Sergi et al., 2019; Cheng et al., 2020). Brains of AD individuals show a deficiency of GLUT1 and GLUT3 expression (Simpson et al., 1994) as a result of decreased activity of enzymes involved in glycolysis and TCA cycle (Manczak et al., 2004; Bubber et al., 2005; Manczak and Reddy, 2012). Moreover, AD brains often exhibit impaired insulin receptors activity (Frölich et al., 1998; Talbot et al., 2012), attenuated levels of insulin and insulin growth factor 1 as well as decreased levels of downstream proteins such as insulin receptor substrate 1 (Rivera et al., 2005; Moloney et al., 2010; Talbot et al., 2012). These characteristics positively correlate with cognitive impairments (Talbot et al., 2012) and the progression of AD (Rivera et al., 2005). In conclusion, T2DM and AD share common derangements in glucose metabolism, which led to the term “type III diabetes” and the classification of AD as a metabolic disease that might alternatively be treated with antidiabetics as a novel therapeutic strategy (de la Monte and Wands, 2005). Similar to AD, PD has overlapping dysregulations with diabetes. For example, 50–80% of PD patients have decreased glucose tolerance (Sandyk, 1993) and impaired glucose metabolism, which is considered an early event in the pathology of PD (Borghammer et al., 2012; Dunn et al., 2014). An integrative network analysis compared gene expression in PD and T2DM and elucidated dysregulation of 7 genes involved in insulin and IR signaling as a common mechanism of action (Santiago and Potashkin, 2013). Another common feature of PD and T2DM pathogenesis is mitochondrial dysfunction and impairment of the mitochondrial complex I (Esteves et al., 2008). Consequently, targeting metabolic dysregulations in neurodegenerative diseases has gained great therapeutical interest due to strong similarities to T2DM.
By strengthening the antioxidant system, metformin was shown to extinct ROS from brain tissues (Garg et al., 2017; Tang et al., 2017; Ruegsegger et al., 2019; Docrat et al., 2020) and thereby caught attention as a possible off-label treatment for AD. Indeed, preclinical animal studies suggest a role of metformin in preventing neuropathology in AD and T2DM models (Kickstein et al., 2010; Li et al., 2012; Cardoso and Moreira, 2020) as well as reducing the risk for AD development (Chin-Hsiao, 2019). Interestingly, metformin treatment interferes with amyloid plaque deposition and promotes hippocampal neurogenesis (Ou et al., 2018). In addition, it activates insulin signaling, inhibits structural changes under hyperinsulinemic conditions (Gupta et al., 2011), and restores mitochondrial function in an AMPK-dependent fashion (Chiang et al., 2016). A pilot clinical study observed that improved cognitive function, learning performance, and memory were positively correlated with metformin treatment (Koenig et al., 2017). However, these observations are controversial as other studies reported elevated Aβ levels (Chen et al., 2009) and an increased risk of AD (Imfeld et al., 2012). Thus, the effects of metformin on the pathology of AD remain to be investigated in more detail to conclude on its therapeutic potential. Metformin acts neuroprotective in the development and progression of PD (Paudel et al., 2020). These effects manifest in reduced neuroinflammation and dopaminergic cell death (Lu et al., 2016), reduced α-synuclein aggregation (Pérez-Revuelta et al., 2014; Saewanee et al., 2021), and improved cognitive and locomotor function in animals (Patil et al., 2014; Lu et al., 2016). However, clinical studies validating these metformin-specific effects in PD are still inconclusive or lacking, as metformin was most effective when combined with other antidiabetics, such as sulfonylurea (Wahlqvist et al., 2012).
4.4 Anti-cancer Drugs
ROS production plays an essential role in anticancer therapies. Depending on the actual level, ROS either act as tumor-suppressing or as a tumor-promoting agent (Sahoo et al., 2021). For instance, a moderate increase of intracellular ROS levels triggers cell proliferation and angiogenesis and inactivates tumor suppressor genes, promoting tumor progression (Kumari et al., 2018; Perillo et al., 2020). In contrast, overwhelming ROS levels that overcome the antioxidant defensive system of cancer cells induce cancer cell death (Galadari et al., 2017). Recent studies demonstrate that ROS levels exceeding the redox capacity might be used as anticancer therapies. Thereby, an accelerated accumulation of ROS by a selective triggering of a ROS burst or by inhibition of antioxidant processes disturbs the redox homeostasis and leads to extensive cellular damage and cell death (Wang and Yi, 2008; Trachootham et al., 2009). Enhanced ROS generation is either achieved through exogenous approaches or by endogenous ROS release (Van Loenhout et al., 2020). Several studies demonstrated that exogenous and endogenous ROS bursts actively contribute to the mechanism of action of anti-cancer therapies such as radiotherapy and chemotherapy and, therefore, enhance their efficacy (Ozben, 2007; Zhang et al., 2009; Kim et al., 2019). Physical interventions like radiotherapy or photodynamic therapy are exogenous ROS sources (Van Loenhout et al., 2020). Besides, various agents induce oxidative stress via endogenous ROS generation and accumulation. Compounds that generate high levels of ROS include anthracyclines including doxorubicin, platinum coordination complexes such as cisplatin, alkylating agents like cyclophosphamide, camptothecins, arsenic agents, and topoisomerase inhibitors (Weiner, 1979). Thereby, these agents either directly induce ROS generation or inhibit antioxidant defense mechanisms (Kim et al., 2019). For instance, motexafin gadolinium, doxorubicin, cisplatin, and 2-methoxyestradiol act by direct ROS generation. Thereby, motexafin gadolinium accepts electrons to form superoxide (Magda and Miller, 2006), doxorubicin induces chelation of iron to generate hydroxyl radicals (Kotamraju et al., 2002), cisplatin induces ROS generation by damaging mtDNA and the electron transport chain (Marullo et al., 2013), and 2-methoxyestradiol inhibits the ETC complex 1 (Hagen et al., 2004). Even though anticancer drugs with direct ROS-accumulating activity have been helpful in combating various cancers, their effects on normal cells remain controversial as they harm both cancer cells and normal cells (Francis et al., 2009; Cardinale et al., 2015). In contrast, the antioxidant process is, for example, inhibited by buthionine sulfoximine and imexon. Both disrupt GSH activity and disturb the Ψmito, generating oxidative stress in cancer cells (Griffith and Meister, 1979; Moulder et al., 2010; Sheveleva et al., 2012). However, the inhibition of antioxidative enzymes also has side effects on normal cells and tissues (Dvorakova et al., 2002; Abdelhamid and El-Kadi, 2015). Consequently, it might be helpful to specifically target these agents to cancer cells in vivo, for instance, by using characteristic molecular signals of cancer cells. Notably, therapeutic strategies affecting ROS homeostasis are predominantly used to attack late-stage cancer cells since early-stage cancer cells are often able to actively counteract ROS disturbances by adjusting their redox status through the upregulation of antioxidant enzymes. Late-stage cancer cells already exhibit higher basal ROS levels, and additional ROS bursts are more effective to severe cytotoxic effects (Kim et al., 2019), inducing apoptosis, autophagic cell death, or necroptosis (Kim et al., 2019; Perillo et al., 2020).
4.5 Analgetics
Acetaminophen, also known as N-acetyl-p-aminophenol or paracetamol, is one of the most commonly used medications for pain worldwide. Approved in 2002 by the FDA, it is used as an analgesic and antipyretic agent and is recommended as first-line treatment in geriatric patients (Abdulla et al., 2013), pregnant women (Aitkin et al., 1996), and children (Cranswick and Coghlan, 2000; Purssell, 2002). Acetaminophen exerts its effects by blocking the synthesis of prostaglandins from arachidonic acid and via actions of its metabolite AM404 (Flower and Vane, 1972; Ghanem et al., 2016). Inhibition of prostaglandin synthesis is achieved by hampering the activity of COX-1 and COX-2 (Esh et al., 2021). COX-1 is expressed in most tissues and regulates basal levels of prostaglandins which control platelet activation and protect the lining of the gastrointestinal tract (Crofford, 1997). COX-2 is inducible and responsible for releasing prostaglandins after infection, in case of injury, or during cancer development. Prostaglandins mediate a number of biological effects, including the induction of an inflammatory immune response (Ornelas et al., 2017). In case of low levels of arachidonic acid and peroxide, therapeutic concentrations of acetaminophen inhibit COX activity sufficiently. However, acetaminophen has little effect when arachidonic acid or peroxide levels are high, as seen in severe inflammatory conditions such as rheumatoid arthritis (Boutaud et al., 2002). Accordingly, the anti-inflammatory action of acetaminophen is modest (Graham et al., 2013). Besides blocking prostaglandin synthesis, the metabolite of acetaminophen, AM404, displays analgetic effects. AMA404 is formed from 4-aminophenol by the action of fatty acid amide hydrolase and has been detected in cerebrospinal fluid of humans treated with acetaminophen (Ghanem et al., 2016; Sharma et al., 2017). AMA404 works as a weak agonist of cannabinoid receptors CB1 and CB2, as an inhibitor of endocannabinoid transporter, and a potent activator of TRPVI receptor (Anderson, 2008; Ghanem et al., 2016). Notably, acetaminophen also inhibits prostaglandin synthesis indirectly by scavenging peroxynitrite, an activator of COX (Schildknecht et al., 2008). When used in recommended doses, acetaminophen has few side effects, and iatrogenic complications are infrequent and minor (Cranswick and Coghlan, 2000; Warwick, 2008). However, in overdose, acetaminophen is hepatotoxic as it induces oxidative stress that subsequently causes mitochondrial impairment and hepatic necroptosis (Cranswick and Coghlan, 2000; Warwick, 2008). When acetaminophen is metabolized, the highly toxic acetaminophen metabolite N-acetyl-p-benzoquinone-imine is formed and gets conjugated to the hepatic store of reduced GSH. In case of acetaminophen overdose, N-acetyl-p-benzoquinone-imine reacts further with cellular proteins causing oxidative stress, lipid peroxidation, and excessive free radical production. Consequently, numerous studies in cells and animals have proven that oxidative stress plays an essential role in the toxic effects induced by acetaminophen (Wang et al., 2017). For example, 0.1 mM of acetaminophen decreased levels of cellular GSH and elevated levels of malondialdehyde, a highly reactive product from lipid peroxidation, in rat hepatocytes, while the antioxidant compound saponarin ameliorated acetaminophen-induced hepatoxicity by restoring GSH and malondialdehyde levels (Simeonova et al., 2013). Moreover, 6 mM of acetaminophen decreased GSH levels significantly and enhanced telomerase activity in rat embryonic liver cells (Bader et al., 2011). Even lower concentrations of acetaminophen, ranging from 0.05 to 0.3 mM, were found to increase ROS generation in mitochondria and induced the gene expression of NRF2, crucial for maintaining cellular redox homeostasis, in mouse hepatoma cells (Perez et al., 2011). Clinical trials revealed that acetaminophen treatment for more than 1 week decreases the antioxidative capacity in elderlies (Pujos-Guillot et al., 2012) and febrile children (Kozer et al., 2003). Moreover, a gradual decrease in serum antioxidant capacity, eventually by a reduction in GSH, was found in men and women after ingestion of maximum therapeutic doses of acetaminophen for 14 days (Nuttall et al., 2003). Combined administration of acetaminophen and N-acetyl-cysteine amide prevented the drop in levels of reduced GSH in liver mitochondria and reduced histopathologic hepatic lesions in C57BL/6 mice. Notably, the impact of N-acetylcysteine amide was superior to NAC, possible due to the derivative’s improved lipophilicity, membrane permeability, and antioxidant property (Khayyat et al., 2016). Moreover, recent studies also revealed hepatoprotective effects of the mitochondria-targeted antioxidant Mito-TEMPO in mice at late-stage acetaminophen overdose (Abdullah-Al-Shoeb et al., 2020), suggesting that scavenging of mtROS might be a promising approach to counteract acetaminophen-induced hepatotoxicity.
Acetylsalicylic acid, also known as aspirin and already introduced into the chapter “Antiplatelets”, is mainly used to reduce pain, fever, and inflammation. Moreover, acetylsalicylic acid is also specifically used to treat pericarditis, rheumatic fever, Kawasaki disease (Agarwal and Agrawal, 2017; Cortellini et al., 2017; Imazio et al., 2017). In addition to modulating the inflammatory response, acetylsalicylic acid affects the physiological function of platelets, counteracting the clotting. As discussed in the chapter “Antiplatelets”, low-dose acetylsalicylic acid is one of the most popular antiplatelet therapies for the treatment of patients with the acute coronary syndrome (Amsterdam et al., 2014), (Roffi et al., 20152016) and for the secondary prevention of atherothrombotic complications in high-risk patients (Parekh et al., 2013), (Patrono, 2015). Besides, several studies provided convincing evidence that regular low-dose acetylsalicylic acid use significantly lowers the risk of cancer (Rothwell et al., 2010; Algra and Rothwell, 2012; Chan et al., 2012; Ishikawa et al., 2013; Patrignani et al., 2017; Bosetti et al., 2020). Acetylsalicylic acid contains higher anti-inflammatory properties than acetaminophen (Mburu et al., 1990), probably because salicylic acid and its derivates also modulate signaling through NF-kB, which plays a crucial role in inflammation (McCarty and Block, 2006; Lawrence, 2009; Chen et al., 2018). It has also been suggested that aspirin converts COX-2 to lipoxygenase-like enzymes, which additionally results in the formation of mediators contributing to the anti-inflammatory effects of aspirin (Serhan and Chiang, 2013; Romano et al., 2015; Weylandt, 2016). Aspirin is the only non-steroidal anti-inflammatory drug (NSAID) not associated with increased cardiovascular events (Ghosh et al., 2015). Similar to acetaminophen and like the majority of NSAIDs, acetylsalicylic acid exerts its anti-inflammatory effects through inhibition of COX enzymes regulating the production of prostaglandins (Crofford, 1997). How acetylsalicylic acid influences ROS homeostasis seems partly unclear. Some studies show that aspirin decreases levels of ROS (Kim et al., 2017; Liu et al., 2019a; Liu et al., 2019b). For example, human hepatoma cells treated with 2- and 4-mM aspirin showed that aspirin remarkably decreased ROS levels (Liu et al., 2019a). Nucleus pulposus cells treated with 5 or 25 μg/ml aspirin significantly attenuated the production of NO and ROS (Liu et al., 2019b). Possibly, an application of rather low levels of aspirin or an application over short periods of time could eventually trigger mitohormetic responses (which is further discussed in chapter “Antiplatelets”) and thereby decrease ROS levels. Other studies propose an increase of ROS production in rat adipocytes, 1 µM of acetylsalicylic acid caused the activation of the NOX4 isoform of NADPH oxidase, boosting the generation of hydrogen peroxide (Vázquez-Meza et al., 2013). Moreover, 1 mM acetylsalicylic acid was found to increase lipid peroxidation in gastric small intestinal cells of rats (Nagano et al., 2012).
Opioids, which are often used as substitutes in the maintenance treatment for heroin addiction, modulate ROS homeostasis as well (Schiavone et al., 2019). Opioid use increases the production of ROS, which is suggested to play a role in opioid use disorders. It also leads to a decrease in the function of enzymatic antioxidants such as superoxide dismutase, catalase, and GPX and can elevate the risk of vitamin deficiency (Zahmatkesh et al., 2017; Salarian et al., 2018). Supplementation with antioxidants may help to restore the redox equilibrium. However, antioxidant therapy has not yet been proven to have a significant effect in randomized trials (Zahmatkesh et al., 2017).
4.6 Antibiotics
It has been demonstrated that major classes of bactericidal antibiotics, regardless of their molecular targets, trigger cell death in bacteria by acting as stressors leading to ROS overproduction (Dwyer et al., 2007; Kohanski et al., 2007; Wang et al., 2010b; Grant et al., 2012; Liu et al., 2012; Van Acker and Coenye, 2017). The mechanisms causing ROS overproduction involve the disruption of the TCA cycle and the ETC (Kohanski et al., 2007; Kohanski et al., 2008), as well as metabolism-related NADH depletion, damage of iron-sulfur clusters in proteins, and stimulation of the Fenton reaction (Dwyer et al., 2007; Kohanski et al., 2007; Van Acker and Coenye, 2017), mechanisms essential to maintain ROS homeostasis. Besides, studies suggested that low levels of ROS produced by sublethal levels of antibiotics might help bacteria to develop antibiotic resistance (Van Acker and Coenye, 2017; Rowe et al., 2020). Thereby, ROS might, for instance, trigger stress resistance mechanisms (Poole, 2012; Wu et al., 2012) or cause mutagenesis (Neeley and Essigmann, 2006; Kohanski et al., 2010; Jee et al., 2016; Van Acker and Coenye, 2017), helping bacteria to escape the bacteriocidic effect of antibiotics. According to the bacterial origin of mammalian cells’ mitochondria proposed by the endosymbiotic theory (Gray et al., 1999), it might be assumed that antibiotics target both pathogens and mitochondria of healthy cells. Indeed, bactericidal and bacteriostatic antibiotics have been shown to target mitochondrial components and function (Gootz et al., 1990; Hutchin and Cortopassi, 1994; McKee et al., 2006; Hobbie et al., 2008; Pochini et al., 2008; Lowes et al., 2009; Kalghatgi et al., 2013). For instance, chloramphenicol reversibly binds to the 50S subunit of the 70S ribosome in both prokaryotic organisms and mitochondria (Balbi, 2004), inhibiting peptidyl transferase, which catalyzes principal chemical reactions of protein synthesis. Align with this finding, tetracyclines like doxycycline and minocycline have been shown to impair mitochondrial biogenesis (Kroon and Van den Bogert, 1983), mitochondrial respiratory chain activity (Chatzispyrou et al., 2015), and mitochondrial protein synthesis (Fuentes-Retamal et al., 2020). Moreover, the macrolide antibiotic azithromycin has been shown to cause disruption of the Ψmito (Xiao et al., 2019), ROS production (Jiang et al., 2019), and cytochrome c release (Salimi et al., 2016).
Regardless of their specific molecular targets, three major classes of bactericidal antibiotics—quinolones, aminoglycosides, and β-lactams—have been associated with cause mitochondrial dysfunction, which leads to DNA-, protein-, and lipid damage, causing ROS-induced damage in mammalian cells (Kalghatgi et al., 2013). Consequently, oxidative cellular damage induced by bactericidal antibiotics may cause adverse side effects in humans after long-term use, including ototoxicity, nephrotoxicity, and tendinopathy (Brummett and Fox, 1989; Mingeot-Leclercq and Tulkens, 1999; Khaliq and Zhanel, 2003; Kalghatgi et al., 2013). Patients with weakened antioxidant defense systems or people genetically disposed to developing a mitochondrial dysfunction disease (Schaefer et al., 2008) may be at higher risk from bactericidal antibiotic treatments. Notably, co-administration of bactericidal antibiotics and NAC reduced side effects without reducing the bacterial killing efficacy of antibiotics (Kalghatgi et al., 2013). Besides, bacteriostatic antibiotics, such as tetracycline, did not contribute to the overwhelming production of ROS in mammalian cells (Kohanski et al., 2007) and showed fewer side effects (Kalghatgi et al., 2013). Notably, it has been proposed that the usage of specific antibiotics such as tetracyclines might be even beneficial due to the generation of mild mitochondrial stress that leads to activation of the mitochondrial unfolded protein response and enhanced stress resistance (Suárez-Rivero et al., 2021). In addition, doxycycline was found to promote fitness and survival in a Leigh syndrome mouse model and to rescue cell death and inflammatory signatures in cells carrying mitochondrial mutations by inducing a mitohormetic response (Perry et al., 2021). In summary, it seems crucial to which extent antibiotics cause ROS production and whether treated individuals exhibit a functional antioxidant defense system.
5 Conclusion
The current review provides an overview of the implication of ROS in pathological dysregulations and age-related diseases and the mechanisms of how approved drugs modulate ROS homeostasis (Figure 1). Drug classes of antibiotics and anti-cancer agents induce overwhelming ROS production and might thereby help to trigger the death of pathogens or cancer cells. However, thereby may also harm healthy cells. In contrast, drugs against diabetes, neurodegeneration, and CVD, as well as anti-inflammatory compounds, are often associated with boosting antioxidant defense mechanisms and thus preventing ROS-mediated damage of DNA, RNA, lipids, and proteins. In addition, the review highlights the potential of repurposing drugs against metabolic diseases for the treatment of neurodegenerative diseases. For most described drugs, it remains to be questionable whether ROS manipulation is a desirable side-effect or suitable as a drug’s primary mode of action. Moreover, repurposing drugs in use might help to spare time in clinical trials since safety is already confirmed, but specific targeting of ROS sources or detoxification sites might be necessary to enhance the effect or avoid multiple targets and, thereby, side-effects. The individual ROS homeostasis and antioxidant potential undergo crucial alterations during aging (Beal, 2002; Suh et al., 2003; Choksi et al., 2008). Consequently, it might be essential to determine the proper intervention time and adjust the dosage of drugs dependent on the individual oxidative state. Besides, it still has to be clarified which intensity and duration of ROS signals are suitable to induce long-lasting effects in signaling. Moreover, fundamental questions must be solved, including determining the intensity and duration of ROS modulation to cause a long-lasting impact. Thereby, live-cell imaging methods enabling the real-time tracking of various ROS species in different cellular organelles are essential, and reliable blood markers for ROS generation and detoxification might have to be characterized to monitor patients. Manipulating ROS might be a promising strategy to induce toxic effects against pathogens or cancer cells. In addition, specific modulation of ROS levels during aging might be utilized to enhance defense mechanisms and, thereby, prevent the development and progression of cardiovascular and neurodegenerative diseases.
Author Contributions
Wrote and contributed to the writing of the manuscript: CT, LW, EM, MR, and CM-S. Designed and planned the manuscript: CM-S, MR.
Funding
The Madreiter laboratory is funded by the FWF (J4205-B27) and MEFOgraz. The Ristow laboratory is funded by the Swiss National Science Foundation (Schweizerischer Nationalsfonds, SNF 31003A_156031 and 310030_204511).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aatsinki, S.-M., Buler, M., Salomäki, H., Koulu, M., Pavek, P., and Hakkola, J. (2014). Metformin Induces PGC-1α Expression and Selectively Affects Hepatic PGC-1α Functions. Br. J. Pharmacol. 171 (9), 2351–2363. doi:10.1111/bph.12585
Abadeh, S., Case, P. C., and Harrison, R. (1993). Purification of Xanthine Oxidase from Human Heart. Biochem. Soc. Trans. 21 (2), 99S. doi:10.1042/bst021099s
Abd-Elsameea, A. A., Moustaf, A. A., and Mohamed, A. M. (2014). Modulation of the Oxidative Stress by Metformin in the Cerebrum of Rats Exposed to Global Cerebral Ischemia and Ischemia/reperfusion. Eur. Rev. Med. Pharmacol. Sci. 18 (16), 2387–2392.
Abdelhamid, G., and El-Kadi, A. O. S. (2015). Buthionine Sulfoximine, an Inhibitor of Glutathione Biosynthesis, Induces Expression of Soluble Epoxide Hydrolase and Markers of Cellular Hypertrophy in a Rat Cardiomyoblast Cell Line: Roles of the NF-Κb and MAPK Signaling Pathways. Free Radic. Biol. Med. 82, 1–12. doi:10.1016/j.freeradbiomed.2015.01.005
Abdulkhaleq, L. A., Assi, M. A., Abdullah, R., Zamri-Saad, M., Taufiq-Yap, Y. H., and Hezmee, M. N. M. (2018). The Crucial Roles of Inflammatory Mediators in Inflammation: A Review. Vet. World 11 (5), 627–635. doi:10.14202/vetworld.2018.627-635
Abdulla, A., Adams, N., Bone, M., Elliott, A. M., Gaffin, J., Jones, D., et al. (2013). Guidance on the Management of Pain in Older People. Age Ageing 42 (Suppl. 1), i1–57. doi:10.1093/ageing/afs200
Abdullah-Al-Shoeb, M., Sasaki, K., Kikutani, S., Namba, N., Ueno, K., Kondo, Y., et al. (2020). The Late-Stage Protective Effect of Mito-TEMPO against Acetaminophen-Induced Hepatotoxicity in Mouse and Three-Dimensional Cell Culture Models. Antioxidants (Basel) 9 (10). doi:10.3390/antiox9100965
Adams, L., Franco, M. C., and Estevez, A. G. (2015). Reactive Nitrogen Species in Cellular Signaling. Exp. Biol. Med. (Maywood) 240 (6), 711–717. doi:10.1177/1535370215581314
Agarwal, S., and Agrawal, D. K. (2017). Kawasaki Disease: Etiopathogenesis and Novel Treatment Strategies. Expert Rev. Clin. Immunol. 13 (3), 247–258. doi:10.1080/1744666x.2017.1232165
Ahangarpour, A., Zeidooni, L., Rezaei, M., Alboghobeish, S., Samimi, A., and Oroojan, A. A. (2017). Protective Effect of Metformin on Toxicity of Butyric Acid and Arsenic in Isolated Liver Mitochondria and Langerhans Islets in Male Mice: an In Vitro Study. Iran. J. Basic Med. Sci. 20 (12), 1297–1305. doi:10.22038/IJBMS.2017.9567
Ahmari, M., Sharafi, A., Mahmoudi, J., Jafari-Anarkoli, I., Gharbavi, M., and Hosseini, M.-J. (2020). Selegiline (L-Deprenyl) Mitigated Oxidative Stress, Cognitive Abnormalities, and Histopathological Change in Rats: Alternative Therapy in Transient Global Ischemia. J. Mol. Neurosci. 70 (10), 1639–1648. doi:10.1007/s12031-020-01544-5
Ahmed Alfar, E., Kirova, D., Konantz, J., Birke, S., Mansfeld, J., and Ninov, N. (2017). Distinct Levels of Reactive Oxygen Species Coordinate Metabolic Activity with Beta-Cell Mass Plasticity. Sci. Rep. 7 (1), 3994. doi:10.1038/s41598-017-03873-9
Aitkin, L., Nelson, J., and Shepherd, R. (1996). Development of Hearing and Vocalization in a Marsupial, the Northern Quoll,Dasyurus Hallucatus. J. Exp. Zool. 276 (6), 394–402. doi:10.1002/(sici)1097-010x(19961215)276:6<394::aid-jez3>3.0.co;2-i
Algire, C., Moiseeva, O., Deschênes-Simard, X., Amrein, L., Petruccelli, L., Birman, E., et al. (2012). Metformin Reduces Endogenous Reactive Oxygen Species and Associated DNA Damage. Cancer Prev. Res. 5 (4), 536–543. doi:10.1158/1940-6207.capr-11-0536
Algra, A. M., and Rothwell, P. M. (2012). Effects of Regular Aspirin on Long-Term Cancer Incidence and Metastasis: a Systematic Comparison of Evidence from Observational Studies versus Randomised Trials. Lancet Oncol. 13 (5), 518–527. doi:10.1016/s1470-2045(12)70112-2
Alp, H., Varol, S., Celik, M. M., Altas, M., Evliyaoglu, O., Tokgoz, O., et al. (2012). Protective Effects of Beta Glucan and Gliclazide on Brain Tissue and Sciatic Nerve of Diabetic Rats Induced by Streptozosin. Exp. Diabetes Res. 2012, 230342. doi:10.1155/2012/230342
Aluf, Y., Vaya, J., Khatib, S., Loboda, Y., and Finberg, J. P. M. (2013). Selective Inhibition of Monoamine Oxidase A or B Reduces Striatal Oxidative Stress in Rats with Partial Depletion of the Nigro-Striatal Dopaminergic Pathway. Neuropharmacology 65, 48–57. doi:10.1016/j.neuropharm.2012.08.023
Alzoubi, K., Khabour, O., Al-Azzam, S., Tashtoush, M., and Mhaidat, N. (2014). Metformin Eased Cognitive Impairment Induced by Chronic L-Methionine Administration: Potential Role of Oxidative Stress. Curr Neuropharmacol 12 (2), 186–192. doi:10.2174/1570159x11666131120223201
Ames, A. (2000). CNS Energy Metabolism as Related to Function. Brain Res. Brain Res. Rev. 34 (1-2), 42–68. doi:10.1016/s0165-0173(00)00038-2
Ames, B. N., Cathcart, R., Schwiers, E., and Hochstein, P. (1981). Uric Acid Provides an Antioxidant Defense in Humans against Oxidant- and Radical-Caused Aging and Cancer: a Hypothesis. Proc. Natl. Acad. Sci. U.S.A. 78 (11), 6858–6862. doi:10.1073/pnas.78.11.6858
Amsterdam, E. A., Wenger, N. K., Brindis, R. G., Casey, D. E., Ganiats, T. G., Holmes, D. R., et al. (2014). 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-elevation Acute Coronary Syndromes. J. Am. Coll. Cardiol. 64 (24), e139–e228. doi:10.1016/j.jacc.2014.09.017
An, F.-M., Chen, S., Xu, Z., Yin, L., Wang, Y., Liu, A.-R., et al. (2015). Glucagon-like Peptide-1 Regulates Mitochondrial Biogenesis and Tau Phosphorylation against Advanced Glycation End Product-Induced Neuronal Insult: Studies In Vivo and In Vitro. Neuroscience 300, 75–84. doi:10.1016/j.neuroscience.2015.05.023
Anderson, B. J. (2008). Paracetamol (Acetaminophen): Mechanisms of Action. Paediatr. Anaesth. 18 (10), 915–921. doi:10.1111/j.1460-9592.2008.02764.x
Andreev, V. S., and Rybakov, V. N. (1975). Determination of the Indicators of Acid-Base Equilibrium by the Methods of Conductometric Titration. Lab. Delo (4), 208–214.
Apaijai, N., Pintana, H., Chattipakorn, S. C., and Chattipakorn, N. (2013). Effects of Vildagliptin versus Sitagliptin, on Cardiac Function, Heart Rate Variability and Mitochondrial Function in Obese Insulin-Resistant Rats. Br. J. Pharmacol. 169 (5), 1048–1057. doi:10.1111/bph.12176
Araújo, A. A., Morais, H. B., Medeiros, C. A. C. X., Brito, G. A. C., Guedes, P. M. M., Hiyari, S., et al. (2019). Gliclazide Reduced Oxidative Stress, Inflammation, and Bone Loss in an Experimental Periodontal Disease Model. J. Appl. Oral Sci. 27, e20180211. doi:10.1590/1678-7757-2018-0211
Argaud, L., Garrier, O., Loufouat, J., Gomez, L., Couture-Lepetit, E., Gateau-Roesch, O., et al. (2009). Second-generation Sulfonylureas Preserve Inhibition of Mitochondrial Permeability Transition by the Mitochondrial K+ Atp Opener Nicorandil in Experimental Myocardial Infarction. Shock 32 (3), 247–252. doi:10.1097/shk.0b013e31819c3794
Ashabi, G., Khalaj, L., Khodagholi, F., Goudarzvand, M., and Sarkaki, A. (2015). Pre-treatment with Metformin Activates Nrf2 Antioxidant Pathways and Inhibits Inflammatory Responses through Induction of AMPK after Transient Global Cerebral Ischemia. Metab. Brain Dis. 30 (3), 747–754. doi:10.1007/s11011-014-9632-2
Asmat, U., Abad, K., and Ismail, K. (2016). Diabetes Mellitus and Oxidative Stress-A Concise Review. Saudi Pharm. J. 24 (5), 547–553. doi:10.1016/j.jsps.2015.03.013
Attwell, D., and Laughlin, S. B. (2001). An Energy Budget for Signaling in the Grey Matter of the Brain. J. Cereb. Blood Flow. Metab. 21 (10), 1133–1145. doi:10.1097/00004647-200110000-00001
Avraham, K. B., Schickler, M., Sapoznikov, D., Yarom, R., and Groner, Y. (1988). Down's Syndrome: Abnormal Neuromuscular Junction in Tongue of Transgenic Mice with Elevated Levels of Human Cu/Zn-Superoxide Dismutase. Cell 54 (6), 823–829. doi:10.1016/s0092-8674(88)91153-1
Bader, A., Oliver, P., Keller, M., and Pavlica, S. (2011). Paracetamol Treatment Increases Telomerase Activity in Rat Embryonic Liver Cells. Pharmacol. Rep. 63 (6), 1435–1441. doi:10.1016/s1734-1140(11)70707-1
Badrinath, N., and Yoo, S. Y. (2018). Mitochondria in Cancer: in the Aspects of Tumorigenesis and Targeted Therapy. Carcinogenesis 39 (12), 1419–1430. doi:10.1093/carcin/bgy148
Baker, L. D., Cross, D. J., Minoshima, S., Belongia, D., Watson, G. S., and Craft, S. (2011). Insulin Resistance and Alzheimer-like Reductions in Regional Cerebral Glucose Metabolism for Cognitively Normal Adults with Prediabetes or Early Type 2 Diabetes. Arch. Neurol. 68 (1), 51–57. doi:10.1001/archneurol.2010.225
Balbi, H. J. (2004). Chloramphenicol: a Review. Pediatr. Rev. 25 (8), 284–288. doi:10.1542/pir.25-8-284
Bandeira, Sde. M., Guedes, Gda. S., da Fonseca, L. J., Pires, A. S., Gelain, D. P., Moreira, J. C., et al. (2012). Characterization of Blood Oxidative Stress in Type 2 Diabetes Mellitus Patients: Increase in Lipid Peroxidation and SOD Activity. Oxid. Med. Cell Longev. 2012, 819310. doi:10.1155/2012/819310
Barbeau, A., Murphy, G. F., and Sourkes, T. L. (1961). Excretion of Dopamine in Diseases of Basal Ganglia. Science 133 (3465), 1706–1707. doi:10.1126/science.133.3465.1706-b
Barsoum, M. J., Yuan, H., Gerencser, A. A., Liot, G., Kushnareva, Y., Gräber, S., et al. (2006). Nitric Oxide-Induced Mitochondrial Fission Is Regulated by Dynamin-Related GTPases in Neurons. EMBO J. 25 (16), 3900–3911. doi:10.1038/sj.emboj.7601253
Bartels, T., Choi, J. G., and Selkoe, D. J. (2011). α-Synuclein Occurs Physiologically as a Helically Folded Tetramer that Resists Aggregation. Nature 477 (7362), 107–110. doi:10.1038/nature10324
Barzilai, N., Crandall, J. P., Kritchevsky, S. B., and Espeland, M. A. (2016). Metformin as a Tool to Target Aging. Cell Metab. 23 (6), 1060–1065. doi:10.1016/j.cmet.2016.05.011
Battelli, M. G., Polito, L., Bortolotti, M., and Bolognesi, A. (2016). Xanthine Oxidoreductase-Derived Reactive Species: Physiological and Pathological Effects. Oxid. Med. Cell Longev. 2016, 3527579. doi:10.1155/2016/3527579
Bauernfeind, F., Bartok, E., Rieger, A., Franchi, L., Núñez, G., and Hornung, V. (2011). Cutting Edge: Reactive Oxygen Species Inhibitors Block Priming, but Not Activation, of the NLRP3 Inflammasome. J. I. 187 (2), 613–617. doi:10.4049/jimmunol.1100613
Beal, M. F. (2002). Oxidatively Modified Proteins in Aging and Disease1,2 1Guest Editor: Earl Stadtman 2This Article Is Part of a Series of Reviews on "Oxidatively Modified Proteins in Aging and Disease." the Full List of Papers May Be Found on the Homepage of the Journal. Free Radic. Biol. Med. 32 (9), 797–803. doi:10.1016/s0891-5849(02)00780-3
Bell, E. L., Emerling, B. M., Ricoult, S. J. H., and Guarente, L. (2011). SirT3 Suppresses Hypoxia Inducible Factor 1α and Tumor Growth by Inhibiting Mitochondrial ROS Production. Oncogene 30 (26), 2986–2996. doi:10.1038/onc.2011.37
Bellucci, A., Mercuri, N. B., Venneri, A., Faustini, G., Longhena, F., Pizzi, M., et al. (2016). Review: Parkinson's Disease: from Synaptic Loss to Connectome Dysfunction. Neuropathol. Appl. Neurobiol. 42 (1), 77–94. doi:10.1111/nan.12297
Bellucci, A., Zaltieri, M., Navarria, L., Grigoletto, J., Missale, C., and Spano, P. (2012). From α-synuclein to Synaptic Dysfunctions: New Insights into the Pathophysiology of Parkinson's Disease. Brain Res. 1476, 183–202. doi:10.1016/j.brainres.2012.04.014
Benigni, A., Corna, D., Zoja, C., Sonzogni, A., Latini, R., Salio, M., et al. (2009). Disruption of the Ang II Type 1 Receptor Promotes Longevity in Mice. J. Clin. Invest. 119 (3), 524–530. doi:10.1172/jci36703
Bertoni-Freddari, C., Fattoretti, P., Casoli, T., Meier-Ruge, W., and Ulrich, J. (1990). Morphological Adaptive Response of the Synaptic Junctional Zones in the Human Dentate Gyrus during Aging and Alzheimer's Disease. Brain Res. 517 (1-2), 69–75. doi:10.1016/0006-8993(90)91009-6
Birben, E., Sahiner, U. M., Sackesen, C., Erzurum, S., and Kalayci, O. (2012). Oxidative Stress and Antioxidant Defense. World Allergy Organ. J. 5 (1), 9–19. doi:10.1097/wox.0b013e3182439613
Birkmayer, W., Knoll, J., Riederer, P., and Youdim, M. B. (1983). (-)-Deprenyl Leads to Prolongation of L-Dopa Efficacy in Parkinson's Disease. Mod. Probl. Pharmacopsychiatry 19, 170–176. doi:10.1159/000407513
Bjelakovic, G., Nikolova, D., Gluud, L. L., Simonetti, R. G., and Gluud, C. (2012). Antioxidant Supplements for Prevention of Mortality in Healthy Participants and Patients with Various Diseases. Cochrane Database Syst. Rev. 3, CD007176. doi:10.1002/14651858.CD007176.pub2
Bjelakovic, G., Nikolova, D., Gluud, L. L., Simonetti, R. G., and Gluud, C. (2007). Mortality in Randomized Trials of Antioxidant Supplements for Primary and Secondary Prevention. JAMA 297 (8), 842–857. doi:10.1001/jama.297.8.842
Blandini, F., and Armentero, M.-T. (2014). Dopamine Receptor Agonists for Parkinson's Disease. Expert Opin. Investigational Drugs 23 (3), 387–410. doi:10.1517/13543784.2014.869209
Blesa, J., Trigo-Damas, I., Quiroga-Varela, A., and Jackson-Lewis, V. R. (2015). Oxidative Stress and Parkinson's Disease. Front. Neuroanat. 9, 91. doi:10.3389/fnana.2015.00091
Boakye, D., Jansen, L., Schöttker, B., Jansen, E. H. J. M., Schneider, M., Halama, N., et al. (2020). Blood Markers of Oxidative Stress Are Strongly Associated with Poorer Prognosis in Colorectal Cancer Patients. Int. J. Cancer 147 (9), 2373–2386. doi:10.1002/ijc.33018
Bogacka, I., Xie, H., Bray, G. A., and Smith, S. R. (2005). Pioglitazone Induces Mitochondrial Biogenesis in Human Subcutaneous Adipose Tissue In Vivo. Diabetes 54 (5), 1392–1399. doi:10.2337/diabetes.54.5.1392
Bolten, C. W., Blanner, P. M., McDonald, W. G., Staten, N. R., Mazzarella, R. A., Arhancet, G. B., et al. (2007). Insulin Sensitizing Pharmacology of Thiazolidinediones Correlates with Mitochondrial Gene Expression rather Than Activation of PPAR Gamma. Gene Regul. Syst. Bio 1, 73–82. doi:10.1177/117762500700100008
Bonifati, V., Rizzu, P., van Baren, M. J., Schaap, O., Breedveld, G. J., Krieger, E., et al. (2003). Mutations in the DJ-1 Gene Associated with Autosomal Recessive Early-Onset Parkinsonism. Science 299 (5604), 256–259. doi:10.1126/science.1077209
Bonuccelli, U. (2003). Comparing Dopamine Agonists in Parkinsonʼs Disease. Curr. Opin. Neurology 16 (Suppl. 1), S13–S19. doi:10.1097/00019052-200312001-00004
Borghammer, P., Hansen, S. B., Eggers, C., Chakravarty, M., Vang, K., Aanerud, J., et al. (2012). Glucose Metabolism in Small Subcortical Structures in Parkinson's Disease. Acta Neurol. Scand. 125 (5), 303–310. doi:10.1111/j.1600-0404.2011.01556.x
Bosetti, C., Santucci, C., Gallus, S., Martinetti, M., and La Vecchia, C. (2020). Aspirin and the Risk of Colorectal and Other Digestive Tract Cancers: an Updated Meta-Analysis through 2019. Ann. Oncol. 31 (5), 558–568. doi:10.1016/j.annonc.2020.02.012
Bouitbir, J., Charles, A.-L., Echaniz-Laguna, A., Kindo, M., Daussin, F., Auwerx, J., et al. (2012). Opposite Effects of Statins on Mitochondria of Cardiac and Skeletal Muscles: a 'mitohormesis' Mechanism Involving Reactive Oxygen Species and PGC-1. Eur. Heart J. 33 (11), 1397–1407. doi:10.1093/eurheartj/ehr224
Bouitbir, J., Singh, F., Charles, A.-L., Schlagowski, A.-I., Bonifacio, A., Echaniz-Laguna, A., et al. (2016). Statins Trigger Mitochondrial Reactive Oxygen Species-Induced Apoptosis in Glycolytic Skeletal Muscle. Antioxidants Redox Signal. 24 (2), 84–98. doi:10.1089/ars.2014.6190
Boutaud, O., Aronoff, D. M., Richardson, J. H., Marnett, L. J., and Oates, J. A. (2002). Determinants of the Cellular Specificity of Acetaminophen as an Inhibitor of Prostaglandin H 2 Synthases. Proc. Natl. Acad. Sci. U.S.A. 99 (10), 7130–7135. doi:10.1073/pnas.102588199
Boveris, A., Oshino, N., and Chance, B. (1972). The Cellular Production of Hydrogen Peroxide. Biochem. J. 128 (3), 617–630. doi:10.1042/bj1280617
Boyle, J. G., Logan, P. J., Jones, G. C., Small, M., Sattar, N., Connell, J. M. C., et al. (2011). AMP-activated Protein Kinase Is Activated in Adipose Tissue of Individuals with Type 2 Diabetes Treated with Metformin: a Randomised Glycaemia-Controlled Crossover Study. Diabetologia 54 (7), 1799–1809. doi:10.1007/s00125-011-2126-4
Brezniceanu, M. L., Liu, F., Wei, C. C., Tran, S., Sachetelli, S., Zhang, S. L., et al. (2007). Catalase Overexpression Attenuates Angiotensinogen Expression and Apoptosis in Diabetic Mice. Kidney Int. 71 (9), 912–923. doi:10.1038/sj.ki.5002188
Brian J. Tabner, B. S. P., Stuart Turnbull, B. S. P., Omar M.A. El-Agnaf, B. S. P., and David Allsop, B. S. P. (2001). Production of Reactive Oxygen Species from Aggregating Proteins Implicated in Alzheimers Disease, Parkinsons Disease and Other Neurodegenerative Diseases. Ctmc 1 (6), 507–517. doi:10.2174/1568026013394822
Brigelius-Flohé, R. (1999). Tissue-specific Functions of Individual Glutathione Peroxidases. Free Radic. Biol. Med. 27 (9-10), 951–965. doi:10.1016/s0891-5849(99)00173-2
Brownlee, M. (2001). Biochemistry and Molecular Cell Biology of Diabetic Complications. Nature 414 (6865), 813–820. doi:10.1038/414813a
Bruijn, L. I., Miller, T. M., and Cleveland, D. W. (2004). Unraveling the Mechanisms Involved in Motor Neuron Degeneration in ALS. Annu. Rev. Neurosci. 27, 723–749. doi:10.1146/annurev.neuro.27.070203.144244
Brummett, R. E., and Fox, K. E. (1989). Aminoglycoside-induced Hearing Loss in Humans. Antimicrob. Agents Chemother. 33 (6), 797–800. doi:10.1128/aac.33.6.797
Brunmair, B., Staniek, K., Gras, F., Scharf, N., Althaym, A., Clara, R., et al. (2004). Thiazolidinediones, like Metformin, Inhibit Respiratory Complex I. Diabetes 53 (4), 1052–1059. doi:10.2337/diabetes.53.4.1052
Bubber, P., Haroutunian, V., Fisch, G., Blass, J. P., and Gibson, G. E. (2005). Mitochondrial Abnormalities in Alzheimer Brain: Mechanistic Implications. Ann. Neurol. 57 (5), 695–703. doi:10.1002/ana.20474
Buldak, L., Labuzek, K., Buldak, R. J., Kozlowski, M., Machnik, G., Liber, S., et al. (2014). Metformin Affects Macrophages' Phenotype and Improves the Activity of Glutathione Peroxidase, Superoxide Dismutase, Catalase and Decreases Malondialdehyde Concentration in a Partially AMPK-independent Manner in LPS-Stimulated Human Monocytes/macrophages. Pharmacol. Rep. 66 (3), 418–429.
Bulua, A. C., Simon, A., Maddipati, R., Pelletier, M., Park, H., Kim, K.-Y., et al. (2011). Mitochondrial Reactive Oxygen Species Promote Production of Proinflammatory Cytokines and Are Elevated in TNFR1-Associated Periodic Syndrome (TRAPS). J. Exp. Med. 208 (3), 519–533. doi:10.1084/jem.20102049
Burnier, M. (2001). Angiotensin II Type 1 Receptor Blockers. Circulation 103 (6), 904–912. doi:10.1161/01.cir.103.6.904
Burton, G. W., and Ingold, K. U. (1984). β-Carotene: an Unusual Type of Lipid Antioxidant. Science 224 (4649), 569–573. doi:10.1126/science.6710156
Burton, G. W., and Traber, M. G. (1990). Vitamin E: Antioxidant Activity, Biokinetics, and Bioavailability. Annu. Rev. Nutr. 10, 357–382. doi:10.1146/annurev.nu.10.070190.002041
Cai, H., Rasulova, M., Vandemeulebroucke, L., Meagher, L., Vlaeminck, C., Dhondt, I., et al. (2017). Life-Span Extension by Axenic Dietary Restriction Is Independent of the Mitochondrial Unfolded Protein Response and Mitohormesis in Caenorhabditis elegans. J. Gerontol. A Biol. Sci. Med. Sci. 72 (10), 1311–1318. doi:10.1093/gerona/glx013
Caldwell, R. B., Toque, H. A., Narayanan, S. P., and Caldwell, R. W. (2015). Arginase: an Old Enzyme with New Tricks. Trends Pharmacol. Sci. 36 (6), 395–405. doi:10.1016/j.tips.2015.03.006
Calkins, M. J., and Reddy, P. H. (2011). Amyloid Beta Impairs Mitochondrial Anterograde Transport and Degenerates Synapses in Alzheimer's Disease Neurons. Biochimica Biophysica Acta (BBA) - Mol. Basis Dis. 1812 (4), 507–513. doi:10.1016/j.bbadis.2011.01.007
Calkins, M., Manczak, M., and Reddy, P. (2012). Mitochondria-Targeted Antioxidant SS31 Prevents Amyloid Beta-Induced Mitochondrial Abnormalities and Synaptic Degeneration in Alzheimer’s Disease. Pharmaceuticals 5 (10), 1103–1119. doi:10.3390/ph5101103
Campbell, J. M., Bellman, S. M., Stephenson, M. D., and Lisy., K. (2017). Metformin Reduces All-Cause Mortality and Diseases of Ageing Independent of its Effect on Diabetes Control: A Systematic Review and Meta-Analysis. Ageing Res. Rev. 40, 31–44. doi:10.1016/j.arr.2017.08.003
Campisi, J., Kapahi, P., Lithgow, G. J., Melov, S., Newman, J. C., and Verdin, E. (2019). From Discoveries in Ageing Research to Therapeutics for Healthy Ageing. Nature 571 (7764), 183–192. doi:10.1038/s41586-019-1365-2
Canet-Avilés, R. M., Wilson, M. A., Miller, D. W., Ahmad, R., McLendon, C., Bandyopadhyay, S., et al. (2004). The Parkinson's Disease Protein DJ-1 Is Neuroprotective Due to Cysteine-Sulfinic Acid-Driven Mitochondrial Localization. Proc. Natl. Acad. Sci. U.S.A. 101 (24), 9103–9108. doi:10.1073/pnas.0402959101
Cardinale, D., Colombo, A., Bacchiani, G., Tedeschi, I., Meroni, C. A., Veglia, F., et al. (2015). Early Detection of Anthracycline Cardiotoxicity and Improvement with Heart Failure Therapy. Circulation 131 (22), 1981–1988. doi:10.1161/circulationaha.114.013777
Cardoso, S., and Moreira, P. I. (2020). Antidiabetic Drugs for Alzheimer's and Parkinson's Diseases: Repurposing Insulin, Metformin, and Thiazolidinediones. Int. Rev. Neurobiol. 155, 37–64. doi:10.1016/bs.irn.2020.02.010
Carlsson, C. M., Papcke-Benson, K., Carnes, M., McBride, P. E., and Stein, J. H. (2002). Health-related Quality of Life and Long-Term Therapy with Pravastatin and Tocopherol (Vitamin E) in Older Adults. Drugs & Aging 19 (10), 793–805. doi:10.2165/00002512-200219100-00008
Carrera-Juliá, S., Moreno, M. L., Barrios, C., de la Rubia Ortí, J. E., and Drehmer, E. (2020). Antioxidant Alternatives in the Treatment of Amyotrophic Lateral Sclerosis: A Comprehensive Review. Front. Physiol. 11, 63. doi:10.3389/fphys.2020.00063
Ceriello, A., Mercuri, F., Quagliaro, L., Assaloni, R., Motz, E., Tonutti, L., et al. (2001). Detection of Nitrotyrosine in the Diabetic Plasma: Evidence of Oxidative Stress. Diabetologia 44 (7), 834–838. doi:10.1007/s001250100529
Chakraborty, A., Chowdhury, S., and Bhattacharyya, M. (2011). Effect of Metformin on Oxidative Stress, Nitrosative Stress and Inflammatory Biomarkers in Type 2 Diabetes Patients. Diabetes Res. Clin. Pract. 93 (1), 56–62. doi:10.1016/j.diabres.2010.11.030
Chan, A. T., Arber, N., Burn, J., Chia, W. K., Elwood, P., Hull, M. A., et al. (2012). Aspirin in the Chemoprevention of Colorectal Neoplasia: an Overview. Cancer Prev. Res. 5 (2), 164–178. doi:10.1158/1940-6207.capr-11-0391
Chang, L. Y., Slot, J. W., Geuze, H. J., and Crapo, J. D. (1988). Molecular Immunocytochemistry of the CuZn Superoxide Dismutase in Rat Hepatocytes. J. Cell Biol. 107 (6 Pt 1), 2169–2179. doi:10.1083/jcb.107.6.2169
Chao, E. C. (2014). SGLT-2 Inhibitors: A New Mechanism for Glycemic Control. Clin. Diabetes 32 (1), 4–11. doi:10.2337/diaclin.32.1.4
Chaturvedi, R. K., and Beal, M. F. (2008). Mitochondrial Approaches for Neuroprotection. Ann. N. Y. Acad. Sci. 1147, 395–412. doi:10.1196/annals.1427.027
Chatzispyrou, I. A., Held, N. M., Mouchiroud, L., Auwerx, J., and Houtkooper, R. H. (2015). Tetracycline Antibiotics Impair Mitochondrial Function and its Experimental Use Confounds Research. Cancer Res. 75 (21), 4446–4449. doi:10.1158/0008-5472.can-15-1626
Chen, B., Zhao, J., Zhang, S., Wu, W., and Qi, R. (2012). Aspirin Inhibits the Production of Reactive Oxygen Species by Downregulating Nox4 and Inducible Nitric Oxide Synthase in Human Endothelial Cells Exposed to Oxidized Low-Density Lipoprotein. J. Cardiovasc. Pharmacol. 59 (5), 405–412. doi:10.1097/fjc.0b013e318248acba
Chen, L., Deng, H., Cui, H., Fang, J., Zuo, Z., Deng, J., et al. (2018). Inflammatory Responses and Inflammation-Associated Diseases in Organs. Oncotarget 9 (6), 7204–7218. doi:10.18632/oncotarget.23208
Chen, L., Na, R., Gu, M., Salmon, A. B., Liu, Y., Liang, H., et al. (2008). Reduction of Mitochondrial H2O2by Overexpressing Peroxiredoxin 3 Improves Glucose Tolerance in Mice. Aging Cell 7 (6), 866–878. doi:10.1111/j.1474-9726.2008.00432.x
Chen, Y., Zhou, K., Wang, R., Liu, Y., Kwak, Y.-D., Ma, T., et al. (2009). Antidiabetic Drug Metformin (Glucophage R ) Increases Biogenesis of Alzheimer's Amyloid Peptides via Up-Regulating BACE1 Transcription. Proc. Natl. Acad. Sci. U.S.A. 106 (10), 3907–3912. doi:10.1073/pnas.0807991106
Cheng, H., Gang, X., Liu, Y., Wang, G., Zhao, X., and Wang, G. (2020). Mitochondrial Dysfunction Plays a Key Role in the Development of Neurodegenerative Diseases in Diabetes. Am. J. Physiology-Endocrinology Metabolism 318 (5), E750–E764. doi:10.1152/ajpendo.00179.2019
Chiang, M.-C., Cheng, Y.-C., Chen, S.-J., Yen, C.-H., and Huang, R.-N. (2016). Metformin Activation of AMPK-dependent Pathways Is Neuroprotective in Human Neural Stem Cells against Amyloid-Beta-Induced Mitochondrial Dysfunction. Exp. Cell Res. 347 (2), 322–331. doi:10.1016/j.yexcr.2016.08.013
Chin-Hsiao, T. (2019). Metformin and the Risk of Dementia in Type 2 Diabetes Patients. Aging Dis. 10 (1), 37–48. doi:10.14336/ad.2017.1202
Choksi, K. B., Nuss, J. E., Deford, J. H., and Papaconstantinou, J. (2008). Age-related Alterations in Oxidatively Damaged Proteins of Mouse Skeletal Muscle Mitochondrial Electron Transport Chain Complexes. Free Radic. Biol. Med. 45 (6), 826–838. doi:10.1016/j.freeradbiomed.2008.06.006
Clayton, R., Clark, J. B., and Sharpe, M. (2005). Cytochrome C Release from Rat Brain Mitochondria Is Proportional to the Mitochondrial Functional Deficit: Implications for Apoptosis and Neurodegenerative Disease. J. Neurochem. 92 (4), 840–849. doi:10.1111/j.1471-4159.2004.02918.x
Collaborators Gbdn, (2019). Global, Regional, and National Burden of Neurological Disorders, 1990-2016: a Systematic Analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18 (5), 459–480. doi:10.1016/S1474-4422(18)30499-X
Collins, Y., Chouchani, E. T., James, A. M., Menger, K. E., Cochemé, H. M., and Murphy, M. P. (2012). Mitochondrial Redox Signalling at a Glance. J. Cell Sci. 125 (Pt 4), 801–806. doi:10.1242/jcs.098475
Conarello, S. L., Li, Z., Ronan, J., Roy, R. S., Zhu, L., Jiang, G., et al. (2003). Mice Lacking Dipeptidyl Peptidase IV Are Protected against Obesity and Insulin Resistance. Proc. Natl. Acad. Sci. U.S.A. 100 (11), 6825–6830. doi:10.1073/pnas.0631828100
Correia-Melo, C., Marques, F. D., Anderson, R., Hewitt, G., Hewitt, R., Cole, J., et al. (2016). Mitochondria Are Required for Pro-ageing Features of the Senescent Phenotype. EMBO J. 35 (7), 724–742. doi:10.15252/embj.201592862
Cortellini, G., Caruso, C., and Romano, A. (2017). Aspirin Challenge and Desensitization: How, when and Why. Curr. Opin. Allergy Clin. Immunol. 17 (4), 247–254. doi:10.1097/aci.0000000000000374
Costa, V. M., Silva, R., Tavares, L. C., Vitorino, R., Amado, F., Carvalho, F., et al. (2009). Adrenaline and Reactive Oxygen Species Elicit Proteome and Energetic Metabolism Modifications in Freshly Isolated Rat Cardiomyocytes. Toxicology 260 (1-3), 84–96. doi:10.1016/j.tox.2009.03.012
Crack, P. J., Cimdins, K., Ali, U., Hertzog, P. J., and Iannello, R. C. (2006). Lack of Glutathione Peroxidase-1 Exacerbates Aβ-Mediated Neurotoxicity in Cortical Neurons. J. Neural Transm. 113 (5), 645–657. doi:10.1007/s00702-005-0352-y
Cranswick, N., and Coghlan, D. (2000). Paracetamol Efficacy and Safety in Children. Am. J. Ther. 7 (2), 135–142. doi:10.1097/00045391-200007020-00010
Crapo, J. D., Oury, T., Rabouille, C., Slot, J. W., and Chang, L. Y. (1992). Copper,zinc Superoxide Dismutase Is Primarily a Cytosolic Protein in Human Cells. Proc. Natl. Acad. Sci. U.S.A. 89 (21), 10405–10409. doi:10.1073/pnas.89.21.10405
Crawford, A., Fassett, R. G., Geraghty, D. P., Kunde, D. A., Ball, M. J., Robertson, I. K., et al. (2012). Relationships between Single Nucleotide Polymorphisms of Antioxidant Enzymes and Disease. Gene 501 (2), 89–103. doi:10.1016/j.gene.2012.04.011
Crofford, L. J. (1997). COX-1 and COX-2 Tissue Expression: Implications and Predictions. J. Rheumatol. Suppl. 49, 15–19.
Cryer, B. (2002). Gastrointestinal Safety of Low-Dose Aspirin. Am. J. Manag. Care 8 (22 Suppl. l), S701–S708.
Dai, D.-F., Santana, L. F., Vermulst, M., Tomazela, D. M., Emond, M. J., MacCoss, M. J., et al. (2009). Overexpression of Catalase Targeted to Mitochondria Attenuates Murine Cardiac Aging. Circulation 119 (21), 2789–2797. doi:10.1161/circulationaha.108.822403
Dai, J., Liu, M., Ai, Q., Lin, L., Wu, K., Deng, X., et al. (2014). Involvement of Catalase in the Protective Benefits of Metformin in Mice with Oxidative Liver Injury. Chemico-Biological Interact. 216, 34–42. doi:10.1016/j.cbi.2014.03.013
Davì, G., Ciabattoni, G., Consoli, A., Mezzetti, A., Falco, A., Santarone, S., et al. (1999). In Vivo formation of 8-Iso-Prostaglandin F2alpha and Platelet Activation in Diabetes Mellitus: Effects of Improved Metabolic Control and Vitamin E Supplementation. Circulation 99 (2), 224–229. doi:10.1161/01.cir.99.2.224
Day, C. (1999). Thiazolidinediones: a New Class of Antidiabetic Drugs. Diabet. Med. 16 (3), 179–192. doi:10.1046/j.1464-5491.1999.00023.x
de la Monte, S. M., and Wands, J. R. (2005). Review of Insulin and Insulin-like Growth Factor Expression, Signaling, and Malfunction in the Central Nervous System: Relevance to Alzheimer's Disease. Jad 7 (1), 45–61. doi:10.3233/jad-2005-7106
Deacon, C. F., Mannucci, E., and Ahrén, B. (2012). Glycaemic Efficacy of Glucagon-like Peptide-1 Receptor Agonists and Dipeptidyl Peptidase-4 Inhibitors as Add-On Therapy to Metformin in Subjects with Type 2 Diabetes-A Review and Meta Analysis. Diabetes Obes. Metab. 14 (8), 762–767. doi:10.1111/j.1463-1326.2012.01603.x
Deeks, E. D. (2015). Safinamide: First Global Approval. Drugs 75 (6), 705–711. doi:10.1007/s40265-015-0389-7
DeKosky, S. T., Scheff, S. W., and Styren, S. D. (1996). Structural Correlates of Cognition in Dementia: Quantification and Assessment of Synapse Change. Neurodegeneration 5 (4), 417–421. doi:10.1006/neur.1996.0056
Del Guerra, S., Grupillo, M., Masini, M., Lupi, R., Bugliani, M., Torri, S., et al. (2007). Gliclazide Protects Human Islet Beta-Cells from Apoptosis Induced by Intermittent High Glucose. Diabetes Metab. Res. Rev. 23 (3), 234–238. doi:10.1002/dmrr.680
Devi, L., Prabhu, B. M., Galati, D. F., Avadhani, N. G., and Anandatheerthavarada, H. K. (2006). Accumulation of Amyloid Precursor Protein in the Mitochondrial Import Channels of Human Alzheimer's Disease Brain Is Associated with Mitochondrial Dysfunction. J. Neurosci. 26 (35), 9057–9068. doi:10.1523/jneurosci.1469-06.2006
Devos, D., Moreau, C., Devedjian, J. C., Kluza, J., Petrault, M., Laloux, C., et al. (2014). Targeting Chelatable Iron as a Therapeutic Modality in Parkinson's Disease. Antioxidants Redox Signal. 21 (2), 195–210. doi:10.1089/ars.2013.5593
Dexter, D. T., Wells, F. R., Agid, F., Agid, Y., Lees, A. J., Jenner, P., et al. (1987). Increased Nigral Iron Content in Postmortem Parkinsonian Brain. Lancet 330 (8569), 1219–1220. doi:10.1016/s0140-6736(87)91361-4
Dexter, D. T., Wells, F. R., Lee, A. J., Agid, F., Agid, Y., Jenner, P., et al. (1989). Increased Nigral Iron Content and Alterations in Other Metal Ions Occurring in Brain in Parkinson's Disease. J. Neurochem. 52 (6), 1830–1836. doi:10.1111/j.1471-4159.1989.tb07264.x
Dias, V., Junn, E., and Mouradian, M. M. (2013). The Role of Oxidative Stress in Parkinson's Disease. J. Park. Dis. 3 (4), 461–491. doi:10.3233/jpd-130230
Dikalova, A. E., Bikineyeva, A. T., Budzyn, K., Nazarewicz, R. R., McCann, L., Lewis, W., et al. (2010). Therapeutic Targeting of Mitochondrial Superoxide in Hypertension. Circulation Res. 107 (1), 106–116. doi:10.1161/circresaha.109.214601
Diniz Vilela, D., Gomes Peixoto, L., Teixeira, R. R., Belele Baptista, N., Carvalho Caixeta, D., Vieira de Souza, A., et al. (2016). The Role of Metformin in Controlling Oxidative Stress in Muscle of Diabetic Rats. Oxid. Med. Cell Longev. 2016, 6978625. doi:10.1155/2016/6978625
Docrat, T. F., Nagiah, S., Naicker, N., Baijnath, S., Singh, S., and Chuturgoon, A. A. (2020). The Protective Effect of Metformin on Mitochondrial Dysfunction and Endoplasmic Reticulum Stress in Diabetic Mice Brain. Eur. J. Pharmacol. 875, 173059. doi:10.1016/j.ejphar.2020.173059
Domingueti, C. P., Dusse, L. M. S. A., Carvalho, M. d. G., de Sousa, L. P., Gomes, K. B., and Fernandes, A. P. (2016). Diabetes Mellitus: The Linkage between Oxidative Stress, Inflammation, Hypercoagulability and Vascular Complications. J. Diabetes its Complicat. 30 (4), 738–745. doi:10.1016/j.jdiacomp.2015.12.018
Dorsey, E. R., and Bloem, B. R. (2018). The Parkinson Pandemic-A Call to Action. JAMA Neurol. 75 (1), 9–10. doi:10.1001/jamaneurol.2017.3299
Du, H., Guo, L., Yan, S., Sosunov, A. A., McKhann, G. M., and ShiDu Yan, S. (2010). Early Deficits in Synaptic Mitochondria in an Alzheimer's Disease Mouse Model. Proc. Natl. Acad. Sci. U.S.A. 107 (43), 18670–18675. doi:10.1073/pnas.1006586107
Dunn, L., Allen, G. F., Mamais, A., Ling, H., Li, A., Duberley, K. E., et al. (2014). Dysregulation of Glucose Metabolism Is an Early Event in Sporadic Parkinson's Disease. Neurobiol. Aging 35 (5), 1111–1115. doi:10.1016/j.neurobiolaging.2013.11.001
Dvorakova, K., Payne, C. M., Landowski, T. H., Tome, M. E., Halperin, D. S., and Dorr, R. T. (2002). Imexon Activates an Intrinsic Apoptosis Pathway in RPMI8226 Myeloma Cells. Anti-Cancer Drugs 13 (10), 1031–1042. doi:10.1097/00001813-200211000-00007
Dwyer, D. J., Kohanski, M. A., Hayete, B., and Collins, J. J. (2007). Gyrase Inhibitors Induce an Oxidative Damage Cellular Death Pathway in Escherichia coli. Mol. Syst. Biol. 3, 91. doi:10.1038/msb4100135
El-Mir, M.-Y., Nogueira, V., Fontaine, E., Avéret, N., Rigoulet, M., and Leverve, X. (2000). Dimethylbiguanide Inhibits Cell Respiration via an Indirect Effect Targeted on the Respiratory Chain Complex I. J. Biol. Chem. 275 (1), 223–228. doi:10.1074/jbc.275.1.223
Endo, H., Nito, C., Kamada, H., Yu, F., and Chan, P. H. (2007). Reduction in Oxidative Stress by Superoxide Dismutase Overexpression Attenuates Acute Brain Injury after Subarachnoid Hemorrhage via Activation of Akt/Glycogen Synthase Kinase-3β Survival Signaling. J. Cereb. Blood Flow. Metab. 27 (5), 975–982. doi:10.1038/sj.jcbfm.9600399
Ergul, A., Johansen, J. S., Strømhaug, C., Harris, A. K., Hutchinson, J., Tawfik, A., et al. (2005). Vascular Dysfunction of Venous Bypass Conduits Is Mediated by Reactive Oxygen Species in Diabetes: Role of Endothelin-1. J. Pharmacol. Exp. Ther. 313 (1), 70–77. doi:10.1124/jpet.104.078105
Esh, C. J., Chrismas, B. C. R., Mauger, A. R., and Taylor, L. (2021). Pharmacological Hypotheses: Is Acetaminophen Selective in its Cyclooxygenase Inhibition? Pharmacol. Res. Perspect. 9 (4), e00835. doi:10.1002/prp2.835
Esteves, A. R. F., Domingues, A. F., Ferreira, I. L., Januário, C., Swerdlow, R. H., Oliveira, C. R., et al. (2008). Mitochondrial Function in Parkinson's Disease Cybrids Containing an Nt2 Neuron-like Nuclear Background. Mitochondrion 8 (3), 219–228. doi:10.1016/j.mito.2008.03.004
Evans, J. L., Goldfine, I. D., Maddux, B. A., and Grodsky, G. M. (2003). Are Oxidative Stress−Activated Signaling Pathways Mediators of Insulin Resistance and β-Cell Dysfunction? Diabetes 52 (1), 1–8. doi:10.2337/diabetes.52.1.1
Fabbrini, G., Brotchie, J. M., Grandas, F., Nomoto, M., and Goetz, C. G. (2007). Levodopa‐induced Dyskinesias. Mov. Disord. 22 (10), 1379–1389. doi:10.1002/mds.21475
Farah, C., Michel, L. Y. M., and Balligand, J.-L. (2018). Nitric Oxide Signalling in Cardiovascular Health and Disease. Nat. Rev. Cardiol. 15 (5), 292–316. doi:10.1038/nrcardio.2017.224
Faulkner, M. A. (2014). Safety Overview of FDA-Approved Medications for the Treatment of the Motor Symptoms of Parkinson's Disease. Expert Opin. Drug Saf. 13 (8), 1055–1069. doi:10.1517/14740338.2014.931369
Fernandes, A. C., Filipe, P. M., Freitas, J. P., and Manso, C. F. (1996). Different Effects of Thiol and Nonthiol Ace Inhibitors on Copper-Induced Lipid and Protein Oxidative Modification. Free Radic. Biol. Med. 20 (4), 507–514. doi:10.1016/0891-5849(95)02086-1
Ferrannini, E., Muscelli, E., Frascerra, S., Baldi, S., Mari, A., Heise, T., et al. (2014). Metabolic Response to Sodium-Glucose Cotransporter 2 Inhibition in Type 2 Diabetic Patients. J. Clin. Invest. 124 (2), 499–508. doi:10.1172/jci72227
Fiordaliso, F., Cuccovillo, I., Bianchi, R., Bai, A., Doni, M., Salio, M., et al. (2006). Cardiovascular Oxidative Stress Is Reduced by an ACE Inhibitor in a Rat Model of Streptozotocin-Induced Diabetes. Life Sci. 79 (2), 121–129. doi:10.1016/j.lfs.2005.12.036
Flohé, L., Toppo, S., Cozza, G., and Ursini, F. (2011). A Comparison of Thiol Peroxidase Mechanisms. Antioxidants Redox Signal. 15 (3), 763–780. doi:10.1089/ars.2010.3397
Floor, E., and Wetzel, M. G. (1998). Increased Protein Oxidation in Human Substantia Nigra Pars Compacta in Comparison with Basal Ganglia and Prefrontal Cortex Measured with an Improved Dinitrophenylhydrazine Assay. J. Neurochem. 70 (1), 268–275. doi:10.1046/j.1471-4159.1998.70010268.x
Flower, R. J., and Vane, J. R. (1972). Inhibition of Prostaglandin Synthetase in Brain Explains the Anti-pyretic Activity of Paracetamol (4-acetamidophenol). Nature 240 (5381), 410–411. doi:10.1038/240410a0
Foretz, M., Guigas, B., and Viollet, B. (2019). Understanding the Glucoregulatory Mechanisms of Metformin in Type 2 Diabetes Mellitus. Nat. Rev. Endocrinol. 15 (10), 569–589. doi:10.1038/s41574-019-0242-2
Francis, D., Richards, G. M., Forouzannia, A., Mehta, M. P., and Khuntia, D. (2009). Motexafin Gadolinium: a Novel Radiosensitizer for Brain Tumors. Expert Opin. Pharmacother. 10 (13), 2171–2180. doi:10.1517/14656560903179325
Frijhoff, J., Winyard, P. G., Zarkovic, N., Davies, S. S., Stocker, R., Cheng, D., et al. (2015). Clinical Relevance of Biomarkers of Oxidative Stress. Antioxidants Redox Signal. 23 (14), 1144–1170. doi:10.1089/ars.2015.6317
Frölich, L., Blum-Degen, D., Bernstein, H. G., Engelsberger, S., Humrich, J., Laufer, S., et al. (1998). Brain Insulin and Insulin Receptors in Aging and Sporadic Alzheimer's Disease. J. Neural Transm. (Vienna) 105 (4-5), 423–438. doi:10.1007/s007020050068
Fu, Y., Cheng, W. H., Porres, J. M., Ross, D. A., and Lei, X. G. (1999). Knockout of Cellular Glutathione Peroxidase Gene Renders Mice Susceptible to Diquat-Induced Oxidative Stress. Free Radic. Biol. Med. 27 (5-6), 605–611. doi:10.1016/s0891-5849(99)00104-5
Fuentes-Retamal, S., Sandoval-Acuña, C., Peredo-Silva, L., Guzmán-Rivera, D., Pavani, M., Torrealba, N., et al. (2020). Complex Mitochondrial Dysfunction Induced by TPP+-Gentisic Acid and Mitochondrial Translation Inhibition by Doxycycline Evokes Synergistic Lethality in Breast Cancer Cells. Cells 9 (2). doi:10.3390/cells9020407
Furman, D., Campisi, J., Verdin, E., Carrera-Bastos, P., Targ, S., Franceschi, C., et al. (2019). Chronic Inflammation in the Etiology of Disease across the Life Span. Nat. Med. 25 (12), 1822–1832. doi:10.1038/s41591-019-0675-0
Galadari, S., Rahman, A., Pallichankandy, S., and Thayyullathil, F. (2017). Reactive Oxygen Species and Cancer Paradox: To Promote or to Suppress? Free Radic. Biol. Med. 104, 144–164. doi:10.1016/j.freeradbiomed.2017.01.004
Gammer, W., and Brobäck, L.-G. (1984). Clinical Comparison of Orgotein and Methylpredisolone Acetate in the Treatment of Osteoarthrosis of the Knee Joint. Scand. J. Rheumatology 13 (2), 108–112. doi:10.3109/03009748409100372
Gao, S., and Liu, J. (2017). Association between Circulating Oxidized Low‐density Lipoprotein and Atherosclerotic Cardiovascular Disease. Chronic Dis. Transl. Med. 3 (2), 89–94. doi:10.1016/j.cdtm.2017.02.008
Gao, Y., and Vanhoutte, P. M. (2012). Nebivolol. J. Cardiovasc. Pharmacol. 59 (1), 16–21. doi:10.1097/fjc.0b013e3182073e27
Garg, G., Singh, S., Singh, A. K., and Rizvi, S. I. (2017). Antiaging Effect of Metformin on Brain in Naturally Aged and Accelerated Senescence Model of Rat. Rejuvenation Res. 20 (3), 173–182. doi:10.1089/rej.2016.1883
Gegg, M. E., and Schapira, A. H. V. (2016). Mitochondrial Dysfunction Associated with Glucocerebrosidase Deficiency. Neurobiol. Dis. 90, 43–50. doi:10.1016/j.nbd.2015.09.006
Genestra, M. (2007). Oxyl Radicals, Redox-Sensitive Signalling Cascades and Antioxidants. Cell. Signal. 19 (9), 1807–1819. doi:10.1016/j.cellsig.2007.04.009
Ghanem, C. I., Pérez, M. J., Manautou, J. E., and Mottino, A. D. (2016). Acetaminophen from Liver to Brain: New Insights into Drug Pharmacological Action and Toxicity. Pharmacol. Res. 109, 119–131. doi:10.1016/j.phrs.2016.02.020
Ghosh, R., Alajbegovic, A., and Gomes, A. V. (2015). NSAIDs and Cardiovascular Diseases: Role of Reactive Oxygen Species. Oxid. Med. Cell Longev. 2015, 536962. doi:10.1155/2015/536962
Ghosh, S., Patel, N., Rahn, D., McAllister, J., Sadeghi, S., Horwitz, G., et al. (2007). The Thiazolidinedione Pioglitazone Alters Mitochondrial Function in Human Neuron-like Cells. Mol. Pharmacol. 71 (6), 1695–1702. doi:10.1124/mol.106.033845
Gibson, G. E., Sheu, K. F., and Blass, J. P. (1998). Abnormalities of Mitochondrial Enzymes in Alzheimer Disease. J. Neural Transm. (Vienna) 105 (8-9), 855–870. doi:10.1007/s007020050099
Gil-Bea, F., Akterin, S., Persson, T., Mateos, L., Sandebring, A., Avila-Cariño, J., et al. (2012). Thioredoxin-80 Is a Product of Alpha-Secretase Cleavage that Inhibits Amyloid-Beta Aggregation and Is Decreased in Alzheimer's Disease Brain. EMBO Mol. Med. 4 (10), 1097–1111. doi:10.1002/emmm.201201462
Gilks, W. P., Abou-Sleiman, P. M., Gandhi, S., Jain, S., Singleton, A., Lees, A. J., et al. (2005). A Common LRRK2 Mutation in Idiopathic Parkinson's Disease. Lancet 365 (9457), 415–416. doi:10.1016/s0140-6736(05)17830-1
Giorgio, M., Migliaccio, E., Orsini, F., Paolucci, D., Moroni, M., Contursi, C., et al. (2005). Electron Transfer between Cytochrome C and p66Shc Generates Reactive Oxygen Species that Trigger Mitochondrial Apoptosis. Cell 122 (2), 221–233. doi:10.1016/j.cell.2005.05.011
Glossmann, H. H., and Lutz, O. M. D. (2019). Metformin and Aging: A Review. Gerontology 65 (6), 581–590. doi:10.1159/000502257
Goldstein, D. S., Sullivan, P., Holmes, C., Miller, G. W., Alter, S., Strong, R., et al. (2013). Determinants of Buildup of the Toxic Dopamine Metabolite DOPAL in Parkinson's Disease. J. Neurochem. 126 (5), 591–603. doi:10.1111/jnc.12345
Goncalves, R. L. S., Quinlan, C. L., Perevoshchikova, I. V., Hey-Mogensen, M., and Brand, M. D. (2015). Sites of Superoxide and Hydrogen Peroxide Production by Muscle Mitochondria Assessed Ex Vivo under Conditions Mimicking Rest and Exercise. J. Biol. Chem. 290 (1), 209–227. doi:10.1074/jbc.m114.619072
Good, P. F., Werner, P., Hsu, A., Olanow, C. W., and Perl, D. P. (1996). Evidence of Neuronal Oxidative Damage in Alzheimer's Disease. Am. J. Pathol. 149 (1), 21–28.
Goodman, M., Bostick, R. M., Kucuk, O., and Jones, D. P. (2011). Clinical Trials of Antioxidants as Cancer Prevention Agents: Past, Present, and Future. Free Radic. Biol. Med. 51 (5), 1068–1084. doi:10.1016/j.freeradbiomed.2011.05.018
Gootz, T. D., Barrett, J. F., and Sutcliffe, J. A. (1990). Inhibitory Effects of Quinolone Antibacterial Agents on Eucaryotic Topoisomerases and Related Test Systems. Antimicrob. Agents Chemother. 34 (1), 8–12. doi:10.1128/aac.34.1.8
Grace, A. A., and Bunney, B. S. (1983). Intracellular and Extracellular Electrophysiology of Nigral Dopaminergic Neurons-2. Action Potential Generating Mechanisms and Morphological Correlates. Neuroscience 10 (2), 317–331. doi:10.1016/0306-4522(83)90136-7
Gradinaru, D., Borsa, C., Ionescu, C., and Margina, D. (2013). Advanced Oxidative and Glycoxidative Protein Damage Markers in the Elderly with Type 2 Diabetes. J. Proteomics 92, 313–322. doi:10.1016/j.jprot.2013.03.034
Gradman, A. H. (2002). AT(1)-receptor Blockers: Differences that Matter. J. Hum. Hypertens. 16 Suppl 3 (Suppl. 3), S9–S16. doi:10.1038/sj.jhh.1001434
Graham, D. G. (1978). Oxidative Pathways for Catecholamines in the Genesis of Neuromelanin and Cytotoxic Quinones. Mol. Pharmacol. 14 (4), 633–643.
Graham, G. G., Davies, M. J., Day, R. O., Mohamudally, A., and Scott, K. F. (2013). The Modern Pharmacology of Paracetamol: Therapeutic Actions, Mechanism of Action, Metabolism, Toxicity and Recent Pharmacological Findings. Inflammopharmacol 21 (3), 201–232. doi:10.1007/s10787-013-0172-x
Grant, S. S., Kaufmann, B. B., Chand, N. S., Haseley, N., and Hung, D. T. (2012). Eradication of Bacterial Persisters with Antibiotic-Generated Hydroxyl Radicals. Proc. Natl. Acad. Sci. U.S.A. 109 (30), 12147–12152. doi:10.1073/pnas.1203735109
Gray, M. W., Burger, G., and Lang, B. F. (1999). Mitochondrial Evolution. Science 283 (5407), 1476–1481. doi:10.1126/science.283.5407.1476
Griffith, O. W., and Meister, A. (1979). Potent and Specific Inhibition of Glutathione Synthesis by Buthionine Sulfoximine (S-N-Butyl Homocysteine Sulfoximine). J. Biol. Chem. 254 (16), 7558–7560. doi:10.1016/s0021-9258(18)35980-5
Groop, L. C. (1992). Sulfonylureas in NIDDM. Diabetes Care 15 (6), 737–754. doi:10.2337/diacare.15.6.737
Grzybowska, M., Bober, J., and Olszewska, M. (2011). Metformina - Mechanizmy Działania I Zastosowanie W Terapii Cukrzycy Typu 2[i][/i]. Postepy Hig. Med. Dosw 65, 277–285. doi:10.5604/17322693.941655
Guo, M., Mi, J., Jiang, Q. M., Xu, J. M., Tang, Y. Y., Tian, G., et al. (2014). Metformin May Produce Antidepressant Effects through Improvement of Cognitive Function Among Depressed Patients with Diabetes Mellitus. Clin. Exp. Pharmacol. Physiol. 41 (9), 650–656. doi:10.1111/1440-1681.12265
Gupta, A., Bisht, B., and Dey, C. S. (2011). Peripheral Insulin-Sensitizer Drug Metformin Ameliorates Neuronal Insulin Resistance and Alzheimer's-like Changes. Neuropharmacology 60 (6), 910–920. doi:10.1016/j.neuropharm.2011.01.033
Gurzov, E. N., and Eizirik, D. L. (2011). Bcl-2 Proteins in Diabetes: Mitochondrial Pathways of β-cell Death and Dysfunction. Trends Cell Biol. 21 (7), 424–431. doi:10.1016/j.tcb.2011.03.001
Gusdon, A. M., Zhu, J., Van Houten, B., and Chu, C. T. (2012). ATP13A2 Regulates Mitochondrial Bioenergetics through Macroautophagy. Neurobiol. Dis. 45 (3), 962–972. doi:10.1016/j.nbd.2011.12.015
Guzik, T. J., Mussa, S., Gastaldi, D., Sadowski, J., Ratnatunga, C., Pillai, R., et al. (2002). Mechanisms of Increased Vascular Superoxide Production in Human Diabetes Mellitus. Circulation 105 (14), 1656–1662. doi:10.1161/01.cir.0000012748.58444.08
Guzy, R. D., and Schumacker, P. T. (2006). Oxygen Sensing by Mitochondria at Complex III: the Paradox of Increased Reactive Oxygen Species during Hypoxia. Exp. Physiol. 91 (5), 807–819. doi:10.1113/expphysiol.2006.033506
Gwathmey, T. M., Pendergrass, K. D., Reid, S. D., Rose, J. C., Diz, D. I., and Chappell, M. C. (2010). Angiotensin-(1-7)-angiotensin-converting Enzyme 2 Attenuates Reactive Oxygen Species Formation to Angiotensin II within the Cell Nucleus. Hypertension 55 (1), 166–171. doi:10.1161/hypertensionaha.109.141622
Habibi, J., Aroor, A. R., Sowers, J. R., Jia, G., Hayden, M. R., Garro, M., et al. (2017). Sodium Glucose Transporter 2 (SGLT2) Inhibition with Empagliflozin Improves Cardiac Diastolic Function in a Female Rodent Model of Diabetes. Cardiovasc Diabetol. 16 (1), 9. doi:10.1186/s12933-016-0489-z
Hagen, T., D’Amico, G., Quintero, M., Palacios-Callender, M., Hollis, V., Lam, F., et al. (2004). Inhibition of Mitochondrial Respiration by the Anticancer Agent 2-methoxyestradiol. Biochem. Biophysical Res. Commun. 322 (3), 923–929. doi:10.1016/j.bbrc.2004.07.204
Halliwell, B. (2013). The Antioxidant Paradox: Less Paradoxical Now? Br. J. Clin. Pharmacol. 75 (3), 637–644. doi:10.1111/j.1365-2125.2012.04272.x
Hamanishi, T., Furuta, H., Kato, H., Doi, A., Tamai, M., Shimomura, H., et al. (2004). Functional Variants in the Glutathione Peroxidase-1 (GPx-1) Gene Are Associated with Increased Intima-Media Thickness of Carotid Arteries and Risk of Macrovascular Diseases in Japanese Type 2 Diabetic Patients. Diabetes 53 (9), 2455–2460. doi:10.2337/diabetes.53.9.2455
Han, S., Hagan, D. L., Taylor, J. R., Xin, L., Meng, W., Biller, S. A., et al. (2008). Dapagliflozin, a Selective SGLT2 Inhibitor, Improves Glucose Homeostasis in Normal and Diabetic Rats. Diabetes 57 (6), 1723–1729. doi:10.2337/db07-1472
Hansen, R., Sæbø, M., Skjelbred, C. F., Nexø, B. A., Hagen, P. C., Bock, G., et al. (2005). GPX Pro198Leu and OGG1 Ser326Cys Polymorphisms and Risk of Development of Colorectal Adenomas and Colorectal Cancer. Cancer Lett. 229 (1), 85–91. doi:10.1016/j.canlet.2005.04.019
Hare, D. J., and Double, K. L. (2016). Iron and Dopamine: a Toxic Couple. Brain 139 (Pt 4), 1026–1035. doi:10.1093/brain/aww022
Harman, D. (1956). Aging: a Theory Based on Free Radical and Radiation Chemistry. J. Gerontology 11 (3), 298–300. doi:10.1093/geronj/11.3.298
Harrington, R. A. (2017). Statins-Almost 30 Years of Use in the United States and Still Not Quite There. JAMA Cardiol. 2 (1), 66. doi:10.1001/jamacardio.2016.4709
Harris, I. S., Treloar, A. E., Inoue, S., Sasaki, M., Gorrini, C., Lee, K. C., et al. (2015). Glutathione and Thioredoxin Antioxidant Pathways Synergize to Drive Cancer Initiation and Progression. Cancer Cell 27 (2), 211–222. doi:10.1016/j.ccell.2014.11.019
Hauner, H. (2002). The Mode of Action of Thiazolidinediones. Diabetes Metab. Res. Rev. 18 Suppl 2 (Suppl. 2), S10–S15. doi:10.1002/dmrr.249
Hawk, M. A., McCallister, C., and Schafer, Z. T. (2016). Antioxidant Activity during Tumor Progression: A Necessity for the Survival of Cancer Cells? Cancers (Basel) 8 (10). doi:10.3390/cancers8100092
Hayashi, T., Ishimori, C., Takahashi-Niki, K., Taira, T., Kim, Y.-c., Maita, H., et al. (2009). DJ-1 Binds to Mitochondrial Complex I and Maintains its Activity. Biochem. Biophysical Res. Commun. 390 (3), 667–672. doi:10.1016/j.bbrc.2009.10.025
Hayley, S., Crocker, S. J., Smith, P. D., Shree, T., Jackson-Lewis, V., Przedborski, S., et al. (2004). Regulation of Dopaminergic Loss by Fas in a 1-Methyl-4-Phenyl-1,2,3,6-Tetrahydropyridine Model of Parkinson's Disease. J. Neurosci. 24 (8), 2045–2053. doi:10.1523/jneurosci.4564-03.2004
Hayyan, M., Hashim, M. A., and AlNashef, I. M. (2016). Superoxide Ion: Generation and Chemical Implications. Chem. Rev. 116 (5), 3029–3085. doi:10.1021/acs.chemrev.5b00407
Hebert-Schuster, M., Fabre, E. E., and Nivet-Antoine, V. (2012). Catalase Polymorphisms and Metabolic Diseases. Curr. Opin. Clin. Nutr. Metabolic Care 15 (4), 397–402. doi:10.1097/mco.0b013e328354a326
Heckman-Stoddard, B. M., DeCensi, A., Sahasrabuddhe, V. V., and Ford, L. G. (2017). Repurposing Metformin for the Prevention of Cancer and Cancer Recurrence. Diabetologia 60 (9), 1639–1647. doi:10.1007/s00125-017-4372-6
Heimberg, H., Heremans, Y., Jobin, C., Leemans, R., Cardozo, A. K., Darville, M., et al. (2001). Inhibition of Cytokine-Induced NF-Κb Activation by Adenovirus-Mediated Expression of a NF-Κb Super-repressor Prevents β-Cell Apoptosis. Diabetes 50 (10), 2219–2224. doi:10.2337/diabetes.50.10.2219
Herzig, S., and Shaw, R. J. (2018). AMPK: Guardian of Metabolism and Mitochondrial Homeostasis. Nat. Rev. Mol. Cell Biol. 19 (2), 121–135. doi:10.1038/nrm.2017.95
Hirai, K., Aliev, G., Nunomura, A., Fujioka, H., Russell, R. L., Atwood, C. S., et al. (2001). Mitochondrial Abnormalities in Alzheimer's Disease. J. Neurosci. 21 (9), 3017–3023. doi:10.1523/jneurosci.21-09-03017.2001
Hiroi, S., Harada, H., Nishi, H., Satoh, M., Nagai, R., and Kimura, A. (1999). Polymorphisms in the SOD2 and HLA-DRB1 Genes Are Associated with Nonfamilial Idiopathic Dilated Cardiomyopathy in Japanese. Biochem. Biophysical Res. Commun. 261 (2), 332–339. doi:10.1006/bbrc.1999.1036
Ho, C. C.-Y., Rideout, H. J., Ribe, E., Troy, C. M., and Dauer, W. T. (2009). The Parkinson Disease Protein Leucine-Rich Repeat Kinase 2 Transduces Death Signals via Fas-Associated Protein with Death Domain and Caspase-8 in a Cellular Model of Neurodegeneration. J. Neurosci. 29 (4), 1011–1016. doi:10.1523/jneurosci.5175-08.2009
Hobbie, S. N., Akshay, S., Kalapala, S. K., Bruell, C. M., Shcherbakov, D., and Böttger, E. C. (2008). Genetic Analysis of Interactions with Eukaryotic rRNA Identify the Mitoribosome as Target in Aminoglycoside Ototoxicity. Proc. Natl. Acad. Sci. U.S.A. 105 (52), 20888–20893. doi:10.1073/pnas.0811258106
Holmgren, A., Johansson, C., Berndt, C., Lönn, M. E., Hudemann, C., and Lillig, C. H. (2005). Thiol Redox Control via Thioredoxin and Glutaredoxin Systems. Biochem. Soc. Trans. 33 (Pt 6), 1375–1377. doi:10.1042/BST20051375
Holmgren, A. (1976). Hydrogen Donor System for Escherichia coli Ribonucleoside-Diphosphate Reductase Dependent upon Glutathione. Proc. Natl. Acad. Sci. U.S.A. 73 (7), 2275–2279. doi:10.1073/pnas.73.7.2275
Hsu, L. J., Sagara, Y., Arroyo, A., Rockenstein, E., Sisk, A., Mallory, M., et al. (2000). α-Synuclein Promotes Mitochondrial Deficit and Oxidative Stress. Am. J. Pathology 157 (2), 401–410. doi:10.1016/s0002-9440(10)64553-1
Hu, D., Wu, C.-q., Li, Z.-j., Liu, Y., Fan, X., Wang, Q.-j., et al. (2015). Characterizing the Mechanism of Thiazolidinedione-Induced Hepatotoxicity: An In Vitro Model in Mitochondria. Toxicol. Appl. Pharmacol. 284 (2), 134–141. doi:10.1016/j.taap.2015.02.018
Hutchin, T., and Cortopassi, G. (1994). Proposed Molecular and Cellular Mechanism for Aminoglycoside Ototoxicity. Antimicrob. Agents Chemother. 38 (11), 2517–2520. doi:10.1128/aac.38.11.2517
Iaccarino, C., Crosio, C., Vitale, C., Sanna, G., Carrì, M. T., and Barone, P. (2007). Apoptotic Mechanisms in Mutant LRRK2-Mediated Cell Death. Hum. Mol. Genet. 16 (11), 1319–1326. doi:10.1093/hmg/ddm080
Imazio, M., Battaglia, A., Gaido, L., and Gaita, F. (2017). Recurrent Pericarditis. La Rev. Médecine Interne 38 (5), 307–311. doi:10.1016/j.revmed.2016.12.006
Imfeld, P., Bodmer, M., Jick, S. S., and Meier, C. R. (2012). Metformin, Other Antidiabetic Drugs, and Risk of Alzheimer's Disease: a Population-Based Case-Control Study. J. Am. Geriatr. Soc. 60 (5), 916–921. doi:10.1111/j.1532-5415.2012.03916.x
Inoguchi, T., Sonta, T., Tsubouchi, H., Etoh, T., Kakimoto, M., Sonoda, N., et al. (2003). Protein Kinase C-dependent Increase in Reactive Oxygen Species (ROS) Production in Vascular Tissues of Diabetes: Role of Vascular NAD(P)H Oxidase. J. Am. Soc. Nephrol. 14 (8 Suppl. 3), S227–S232. doi:10.1097/01.asn.0000077407.90309.65
Inoguchi, T., Li, P., Umeda, F., Yu, H. Y., Kakimoto, M., Imamura, M., et al. (2000). High Glucose Level and Free Fatty Acid Stimulate Reactive Oxygen Species Production through Protein Kinase C--dependent Activation of NAD(P)H Oxidase in Cultured Vascular Cells. Diabetes 49 (11), 1939–1945. doi:10.2337/diabetes.49.11.1939
Inoue, I., Nagase, H., Kishi, K., and Higuti, T. (1991). ATP-sensitive K+ Channel in the Mitochondrial Inner Membrane. Nature 352 (6332), 244–247. doi:10.1038/352244a0
Iqbal, A. M., Lopez, R. A., and Hai, O. (2021). Antiplatelet Medications. Treasure Island (FL): StatPearls.
Ishibashi, Y., Matsui, T., and Yamagishi, S. (2016). Tofogliflozin, A Highly Selective Inhibitor of SGLT2 Blocks Proinflammatory and Proapoptotic Effects of Glucose Overload on Proximal Tubular Cells Partly by Suppressing Oxidative Stress Generation. Horm. Metab. Res. 48 (3), 191–195. doi:10.1055/s-0035-1555791
Ishibashi, Y., Matsui, T., Maeda, S., Higashimoto, Y., and Yamagishi, S.-i. (2013). Advanced Glycation End Products Evoke Endothelial Cell Damage by Stimulating Soluble Dipeptidyl Peptidase-4 Production and its Interaction with Mannose 6-phosphate/insulin-like Growth Factor II Receptor. Cardiovasc Diabetol. 12, 125. doi:10.1186/1475-2840-12-125
Ishikawa, H., Wakabayashi, K., Suzuki, S., Mutoh, M., Hirata, K., Nakamura, T., et al. (2013). Preventive Effects of Low‐dose Aspirin on Colorectal Adenoma Growth in Patients with Familial Adenomatous Polyposis: Double‐blind, Randomized Clinical Trial. Cancer Med. 2 (1), 50–56. doi:10.1002/cam4.46
Jalewa, J., Sharma, M. K., and Hölscher, C. (2016). Novel Incretin Analogues Improve Autophagy and Protect from Mitochondrial Stress Induced by Rotenone in SH-Sy5y Cells. J. Neurochem. 139 (1), 55–67. doi:10.1111/jnc.13736
Jang, Y. C., Lustgarten, M. S., Liu, Y., Muller, F. L., Bhattacharya, A., Liang, H., et al. (2010). Increased Superoxide In Vivo Accelerates Age‐associated Muscle Atrophy through Mitochondrial Dysfunction and Neuromuscular Junction Degeneration. FASEB J. 24 (5), 1376–1390. doi:10.1096/fj.09-146308
Janion, K., Szczepańska, E., Nowakowska-Zajdel, E., Strzelczyk, J., and Copija, A. (2020). Selected Oxidative Stress Markers in Colorectal Cancer Patients in Relation to Primary Tumor Location-A Preliminary Research. Med. Kaunas. 56 (2). doi:10.3390/medicina56020047
Janssens, G. E., and Houtkooper, R. H. (2020). Identification of Longevity Compounds with Minimized Probabilities of Side Effects. Biogerontology 21 (6), 709–719. doi:10.1007/s10522-020-09887-7
Jaramillo, M. C., and Zhang, D. D. (2013). The Emerging Role of the Nrf2-Keap1 Signaling Pathway in Cancer. Genes Dev. 27 (20), 2179–2191. doi:10.1101/gad.225680.113
Jaul, E., and Barron, J. (2017). Age-Related Diseases and Clinical and Public Health Implications for the 85 Years Old and over Population. Front. Public Health 5, 335. doi:10.3389/fpubh.2017.00335
Jee, J., Rasouly, A., Shamovsky, I., Akivis, Y., R. Steinman, S., Mishra, B., et al. (2016). Rates and Mechanisms of Bacterial Mutagenesis from Maximum-Depth Sequencing. Nature 534 (7609), 693–696. doi:10.1038/nature18313
Jellen, L. C., Lu, L., Wang, X., Unger, E. L., Earley, C. J., Allen, R. P., et al. (2013). Iron Deficiency Alters Expression of Dopamine-Related Genes in the Ventral Midbrain in Mice. Neuroscience 252, 13–23. doi:10.1016/j.neuroscience.2013.07.058
Jiang, L., Zhou, X., Yang, H., Guan, R., Xin, Y., Wang, J., et al. (2018). Upregulation of AT1 Receptor Mediates a Pressor Effect through ROS-SAPK/JNK Signaling in Glutamatergic Neurons of Rostral Ventrolateral Medulla in Rats with Stress-Induced Hypertension. Front. Physiol. 9, 1860. doi:10.3389/fphys.2018.01860
Jiang, X., Baucom, C., and Elliott, R. L. (2019). Mitochondrial Toxicity of Azithromycin Results in Aerobic Glycolysis and DNA Damage of Human Mammary Epithelia and Fibroblasts. Antibiot. (Basel) 8 (3). doi:10.3390/antibiotics8030110
Jorda, A., Aldasoro, M., Aldasoro, C., Guerra-Ojeda, S., Iradi, A., Vila, J. M., et al. (2020). Action of Low Doses of Aspirin in Inflammation and Oxidative Stress Induced by Aβ1-42 on Astrocytes in Primary Culture. Int. J. Med. Sci. 17 (6), 834–843. doi:10.7150/ijms.40959
Joza, N., Susin, S. A., Daugas, E., Stanford, W. L., Cho, S. K., Li, C. Y. J., et al. (2001). Essential Role of the Mitochondrial Apoptosis-Inducing Factor in Programmed Cell Death. Nature 410 (6828), 549–554. doi:10.1038/35069004
Juhasz, A., Ge, Y., Markel, S., Chiu, A., Matsumoto, L., van Balgooy, J., et al. (2009). Expression of NADPH Oxidase Homologues and Accessory Genes in Human Cancer Cell Lines, Tumours and Adjacent Normal Tissues. Free Radic. Res. 43 (6), 523–532. doi:10.1080/10715760902918683
Kalghatgi, S., Spina, C. S., Costello, J. C., Liesa, M., Morones-Ramirez, J. R., Slomovic, S., et al. (2013). Bactericidal Antibiotics Induce Mitochondrial Dysfunction and Oxidative Damage in Mammalian Cells. Sci. Transl. Med. 5 (192), 192ra85. doi:10.1126/scitranslmed.3006055
Kalra, S. (2014). Sodium Glucose Co-transporter-2 (SGLT2) Inhibitors: A Review of Their Basic and Clinical Pharmacology. Diabetes Ther. 5 (2), 355–366. doi:10.1007/s13300-014-0089-4
Kamii, H., Kato, I., Kinouchi, H., Chan, P. H., Epstein, C. J., Akabane, A., et al. (1999). Amelioration of Vasospasm after Subarachnoid Hemorrhage in Transgenic Mice Overexpressing CuZn-Superoxide Dismutase. Stroke 30 (4), 867–872. doi:10.1161/01.str.30.4.867
Kang, M. Y., Oh, T. J., and Cho, Y. M. (2015). Glucagon-Like Peptide-1 Increases Mitochondrial Biogenesis and Function in INS-1 Rat Insulinoma Cells. Endocrinol. Metab. 30 (2), 216–220. doi:10.3803/enm.2015.30.2.216
Kaufmann, P., Török, M., Zahno, A., Waldhauser, K. M., Brecht, K., and Krähenbühl, S. (2006). Toxicity of Statins on Rat Skeletal Muscle Mitochondria. Cell Mol. Life Sci. 63 (19-20), 2415–2425. doi:10.1007/s00018-006-6235-z
Kaul, M., Garden, G. A., and Lipton, S. A. (2001). Pathways to Neuronal Injury and Apoptosis in HIV-Associated Dementia. Nature 410 (6831), 988–994. doi:10.1038/35073667
Kawanami, D., Matoba, K., Takeda, Y., Nagai, Y., Akamine, T., Yokota, T., et al. (2017). SGLT2 Inhibitors as a Therapeutic Option for Diabetic Nephropathy. Int. J. Mol. Sci. 18 (5). doi:10.3390/ijms18051083
Keller, G. A., Warner, T. G., Steimer, K. S., and Hallewell, R. A. (1991). Cu,Zn Superoxide Dismutase Is a Peroxisomal Enzyme in Human Fibroblasts and Hepatoma Cells. Proc. Natl. Acad. Sci. U.S.A. 88 (16), 7381–7385. doi:10.1073/pnas.88.16.7381
Kelly, B., Tannahill, G. M., Murphy, M. P., and O'Neill, L. A. J. (2015). Metformin Inhibits the Production of Reactive Oxygen Species from NADH:Ubiquinone Oxidoreductase to Limit Induction of Interleukin-1β (IL-1β) and Boosts Interleukin-10 (IL-10) in Lipopolysaccharide (LPS)-activated Macrophages. J. Biol. Chem. 290 (33), 20348–20359. doi:10.1074/jbc.m115.662114
Kern, M., Klöting, N., Mark, M., Mayoux, E., Klein, T., and Blüher, M. (2016). The SGLT2 Inhibitor Empagliflozin Improves Insulin Sensitivity in Db/db Mice Both as Monotherapy and in Combination with Linagliptin. Metabolism 65 (2), 114–123. doi:10.1016/j.metabol.2015.10.010
Khaliq, Y., and Zhanel, G. G. (2003). Fluoroquinolone-associated Tendinopathy: a Critical Review of the Literature. Clin. Infect. Dis. 36 (11), 1404–1410. doi:10.1086/375078
Khansari, N., Shakiba, Y., and Mahmoudi, M. (2009). Chronic Inflammation and Oxidative Stress as a Major Cause of Age- Related Diseases and Cancer. Iad 3 (1), 73–80. doi:10.2174/187221309787158371
Khayyat, A., Tobwala, S., Hart, M., and Ercal, N. (2016). N -acetylcysteine Amide, a Promising Antidote for Acetaminophen Toxicity. Toxicol. Lett. 241, 133–142. doi:10.1016/j.toxlet.2015.11.008
Kickstein, E., Krauss, S., Thornhill, P., Rutschow, D., Zeller, R., Sharkey, J., et al. (2010). Biguanide Metformin Acts on Tau Phosphorylation via mTOR/protein Phosphatase 2A (PP2A) Signaling. Proc. Natl. Acad. Sci. U.S.A. 107 (50), 21830–21835. doi:10.1073/pnas.0912793107
Kim, J., Lee, K.-S., Kim, J.-H., Lee, D.-K., Park, M., Choi, S., et al. (2017). Aspirin Prevents TNF-α-Induced Endothelial Cell Dysfunction by Regulating the NF-κb-dependent miR-155/eNOS Pathway: Role of a miR-155/eNOS axis in Preeclampsia. Free Radic. Biol. Med. 104, 185–198. doi:10.1016/j.freeradbiomed.2017.01.010
Kim, S. J., Kim, H. S., and Seo, Y. R. (2019). Understanding of ROS-Inducing Strategy in Anticancer Therapy. Oxid. Med. Cell Longev. 2019, 5381692. doi:10.1155/2019/5381692
Kim, Y. K., Lee, M.-S., Son, S. M., Kim, I. J., Lee, W. S., Rhim, B. Y., et al. (2002). Vascular NADH Oxidase Is Involved in Impaired Endothelium-dependent Vasodilation in OLETF Rats, a Model of Type 2 Diabetes. Diabetes 51 (2), 522–527. doi:10.2337/diabetes.51.2.522
Kimura, S., Zhang, G.-X., Nishiyama, A., Shokoji, T., Yao, L., Fan, Y.-Y., et al. (2005). Mitochondria-Derived Reactive Oxygen Species and Vascular MAP Kinases. Hypertension 45 (3), 438–444. doi:10.1161/01.hyp.0000157169.27818.ae
Kisker, C., Schindelin, H., and Rees, D. C. (1997). Molybdenum-cofactor-containing Enzymes: Structure and Mechanism. Annu. Rev. Biochem. 66, 233–267. doi:10.1146/annurev.biochem.66.1.233
Kline, N. S. (1958). Clinical Experience with Iproniazid (Marsilid). J. Clin. Exp. Psychopathol. 19 (2Suppl. 1), 72–79.
Klivenyi, P., Andreassen, O. A., Ferrante, R. J., Dedeoglu, A., Mueller, G., Lancelot, E., et al. (2000). Mice Deficient in Cellular Glutathione Peroxidase Show Increased Vulnerability to Malonate, 3-nitropropionic Acid, and 1-Methyl-4-Phenyl-1,2,5,6-Tetrahydropyridine. J. Neurosci. 20 (1), 1–7. doi:10.1523/jneurosci.20-01-00001.2000
Knudsen Gerber, D. S. (2011). Selegiline and Rasagiline: Twins or Distant Cousins? Guidelines. Consult. Pharm. 26 (1), 48–51. doi:10.4140/tcp.n.2011.48
Kobayashi, S., Susa, T., Tanaka, T., Wada, Y., Okuda, S., Doi, M., et al. (2011). Urinary 8-Hydroxy-2′-Deoxyguanosine Reflects Symptomatic Status and Severity of Systolic Dysfunction in Patients with Chronic Heart Failure. Eur. J. Heart Fail. 13 (1), 29–36. doi:10.1093/eurjhf/hfq178
Koenig, A. M., Mechanic-Hamilton, D., Xie, S. X., Combs, M. F., Cappola, A. R., Xie, L., et al. (2017). Effects of the Insulin Sensitizer Metformin in Alzheimer Disease. Alzheimer Dis. Assoc. Disord. 31 (2), 107–113. doi:10.1097/wad.0000000000000202
Koentjoro, B., Park, J.-S., and Sue, C. M. (2017). Nix Restores Mitophagy and Mitochondrial Function to Protect against PINK1/Parkin-Related Parkinson's Disease. Sci. Rep. 7, 44373. doi:10.1038/srep44373
Kohanski, M. A., DePristo, M. A., and Collins, J. J. (2010). Sublethal Antibiotic Treatment Leads to Multidrug Resistance via Radical-Induced Mutagenesis. Mol. Cell 37 (3), 311–320. doi:10.1016/j.molcel.2010.01.003
Kohanski, M. A., Dwyer, D. J., Hayete, B., Lawrence, C. A., and Collins, J. J. (2007). A Common Mechanism of Cellular Death Induced by Bactericidal Antibiotics. Cell 130 (5), 797–810. doi:10.1016/j.cell.2007.06.049
Kohanski, M. A., Dwyer, D. J., Wierzbowski, J., Cottarel, G., and Collins, J. J. (2008). Mistranslation of Membrane Proteins and Two-Component System Activation Trigger Antibiotic-Mediated Cell Death. Cell 135 (4), 679–690. doi:10.1016/j.cell.2008.09.038
Kono, Y., Nakamura, K., Kimura, H., Nishii, N., Watanabe, A., Banba, K., et al. (2006). Elevated Levels of Oxidative DNA Damage in Serum and Myocardium of Patients with Heart Failure. Circ. J. 70 (8), 1001–1005. doi:10.1253/circj.70.1001
Korshunov, S. S., Skulachev, V. P., and Starkov, A. A. (1997). High Protonic Potential Actuates a Mechanism of Production of Reactive Oxygen Species in Mitochondria. FEBS Lett. 416 (1), 15–18. doi:10.1016/s0014-5793(97)01159-9
Kotamraju, S., Chitambar, C. R., Kalivendi, S. V., Joseph, J., and Kalyanaraman, B. (2002). Transferrin Receptor-dependent Iron Uptake Is Responsible for Doxorubicin-Mediated Apoptosis in Endothelial Cells. J. Biol. Chem. 277 (19), 17179–17187. doi:10.1074/jbc.m111604200
Kotur-Stevuljevic, J., Memon, L., Stefanovic, A., Spasic, S., Spasojevic-Kalimanovska, V., Bogavac-Stanojevic, N., et al. (2007). Correlation of Oxidative Stress Parameters and Inflammatory Markers in Coronary Artery Disease Patients. Clin. Biochem. 40 (3-4), 181–187. doi:10.1016/j.clinbiochem.2006.09.007
Kozer, E., Evans, S., Barr, J., Greenberg, R., Soriano, I., Bulkowstein, M., et al. (2003). Glutathione, Glutathione-dependent Enzymes and Antioxidant Status in Erythrocytes from Children Treated with High-Dose Paracetamol. Br. J. Clin. Pharmacol. 55 (3), 234–240. doi:10.1046/j.1365-2125.2003.01723.x
Kraljevic, S., Stambrook, P. J., and Pavelic, K. (2004). Accelerating Drug Discovery. EMBO Rep. 5 (9), 837–842. doi:10.1038/sj.embor.7400236
Krijnen, P. A. J., Meischl, C., Hack, C. E., Meijer, C. J., Visser, C. A., Roos, D., et al. (2003). Increased Nox2 Expression in Human Cardiomyocytes after Acute Myocardial Infarction. J. Clin. Pathology 56 (3), 194–199. doi:10.1136/jcp.56.3.194
Kroon, A. M., and Van den Bogert, C. (1983). Antibacterial Drugs and Their Interference with the Biogenesis of Mitochondria in Animal and Human Cells. Pharm. Weekbl. Sci. Ed. 5 (3), 81–87. doi:10.1007/bf01960982
Kumar, S., Dang, S., Nigam, K., Ali, J., and Baboota, S. (2018). Selegiline Nanoformulation in Attenuation of Oxidative Stress and Upregulation of Dopamine in the Brain for the Treatment of Parkinson's Disease. Rejuvenation Res. 21 (5), 464–476. doi:10.1089/rej.2017.2035
Kumari, S., Badana, A. K., G, M. M., and Gg, S. (2018). Reactive Oxygen Species: A Key Constituent in Cancer Survival. Biomark. Insights 13, 1177271918755391. doi:10.1177/1177271918755391
LaFerla, F. M., Green, K. N., and Oddo, S. (2007). Intracellular Amyloid-β in Alzheimer's Disease. Nat. Rev. Neurosci. 8 (7), 499–509. doi:10.1038/nrn2168
Lassègue, B., San Martín, A., and Griendling, K. K. (2012). Biochemistry, Physiology, and Pathophysiology of NADPH Oxidases in the Cardiovascular System. Circ. Res. 110 (10), 1364–1390. doi:10.1161/circresaha.111.243972
Lawrence, T. (2009). The Nuclear Factor NF- B Pathway in Inflammation. Cold Spring Harb. Perspect. Biol. 1 (6), a001651. doi:10.1101/cshperspect.a001651
Lazarou, M., Sliter, D. A., Kane, L. A., Sarraf, S. A., Wang, C., Burman, J. L., et al. (2015). The Ubiquitin Kinase PINK1 Recruits Autophagy Receptors to Induce Mitophagy. Nature 524 (7565), 309–314. doi:10.1038/nature14893
Lee, J. D., Cai, Q., Shu, X. O., and Nechuta, S. J. (2017). The Role of Biomarkers of Oxidative Stress in Breast Cancer Risk and Prognosis: A Systematic Review of the Epidemiologic Literature. J. Women's Health 26 (5), 467–482. doi:10.1089/jwh.2016.5973
Lee, J., Giordano, S., and Zhang, J. (2012). Autophagy, Mitochondria and Oxidative Stress: Cross-Talk and Redox Signalling. Biochem. J. 441 (2), 523–540. doi:10.1042/bj20111451
Lee, J. O., Lee, S. K., Kim, J. H., Kim, N., You, G. Y., Moon, J. W., et al. (2012). Metformin Regulates Glucose Transporter 4 (GLUT4) Translocation through AMP-Activated Protein Kinase (AMPK)-mediated Cbl/CAP Signaling in 3T3-L1 Preadipocyte Cells. J. Biol. Chem. 287 (53), 44121–44129. doi:10.1074/jbc.m112.361386
Li, F.-F., Fu, L.-Y., Xu, X.-H., Su, X.-F., Wu, J.-D., Ye, L., et al. (2016). Analysis of the Add-On Effect of α-glucosidase Inhibitor, Acarbose in Insulin Therapy: A Pilot Study. Biomed. Rep. 5 (4), 461–466. doi:10.3892/br.2016.744
Li, J.-M., Gall, N. P., Grieve, D. J., Chen, M., and Shah, A. M. (2002). Activation of NADPH Oxidase during Progression of Cardiac Hypertrophy to Failure. Hypertension 40 (4), 477–484. doi:10.1161/01.hyp.0000032031.30374.32
Li, J., Deng, J., Sheng, W., and Zuo, Z. (2012). Metformin Attenuates Alzheimer's Disease-like Neuropathology in Obese, Leptin-Resistant Mice. Pharmacol. Biochem. Behav. 101 (4), 564–574. doi:10.1016/j.pbb.2012.03.002
Li, X.-X., Ling, S.-K., Hu, M.-Y., Ma, Y., Li, Y., and Huang, P.-L. (2019). Protective Effects of Acarbose against Vascular Endothelial Dysfunction through Inhibiting Nox4/NLRP3 Inflammasome Pathway in Diabetic Rats. Free Radic. Biol. Med. 145, 175–186. doi:10.1016/j.freeradbiomed.2019.09.015
Lillig, C. H., and Holmgren, A. (2007). Thioredoxin and Related Molecules-From Biology to Health and Disease. Antioxidants Redox Signal. 9 (1), 25–47. doi:10.1089/ars.2007.9.25
Lim, C. C., Bryan, N. S., Jain, M., Garcia-Saura, M. F., Fernandez, B. O., Sawyer, D. B., et al. (2009). Glutathione Peroxidase Deficiency Exacerbates Ischemia-Reperfusion Injury in Male but Not Female Myocardium: Insights into Antioxidant Compensatory Mechanisms. Am. J. Physiology-Heart Circulatory Physiology 297 (6), H2144–H2153. doi:10.1152/ajpheart.00673.2009
Lin, Y.-C., Chen, Y.-C., Hsiao, H.-P., Kuo, C.-H., Chen, B.-H., Chen, Y.-T., et al. (2019). The Effects of Acarbose on Chemokine and Cytokine Production in Human Monocytic THP-1 Cells. Hormones 18 (2), 179–187. doi:10.1007/s42000-019-00101-z
Linder, N., Rapola, J., and Raivio, K. O. (1999). Cellular Expression of Xanthine Oxidoreductase Protein in Normal Human Tissues. Lab. Invest 79 (8), 967–974.
Lingappan, K. (2018). NF-κB in Oxidative Stress. Curr. Opin. Toxicol. 7, 81–86. doi:10.1016/j.cotox.2017.11.002
Liou, G.-Y., and Storz, P. (2010). Reactive Oxygen Species in Cancer. Free Radic. Res. 44 (5), 479–496. doi:10.3109/10715761003667554
Liou, W., Chang, L., Geuze, H., Strous, G., Crapo, J., and Slot, J. (1993). Distribution of CuZn Superoxide Dismutase in Rat Liver. Free Radic. Biol. Med. 14 (2), 201–207. doi:10.1016/0891-5849(93)90011-i
Liu, Y., Lin, J., Wu, X., Guo, X., Sun, H., Yu, B., et al. (2019). Aspirin-Mediated Attenuation of Intervertebral Disc Degeneration by Ameliorating Reactive Oxygen Species In Vivo and In Vitro. Oxid. Med. Cell Longev. 2019, 7189854. doi:10.1155/2019/7189854
Liu, Y.-x., Feng, J.-y., Sun, M.-m., Liu, B.-w., Yang, G., Bu, Y.-n., et al. (2019). Aspirin Inhibits the Proliferation of Hepatoma Cells through Controlling GLUT1-Mediated Glucose Metabolism. Acta Pharmacol. Sin. 40 (1), 122–132. doi:10.1038/s41401-018-0014-x
Liu, Y., Liu, X., Qu, Y., Wang, X., Li, L., and Zhao, X. (2012). Inhibitors of Reactive Oxygen Species Accumulation Delay And/or Reduce the Lethality of Several Antistaphylococcal Agents. Antimicrob. Agents Chemother. 56 (11), 6048–6050. doi:10.1128/aac.00754-12
Lonn, E., Bosch, J., Yusuf, S., Sheridan, P., Pogue, J., Arnold, J. M., et al. (2005). Effects of Long-Term Vitamin E Supplementation on Cardiovascular Events and Cancer: a Randomized Controlled Trial. JAMA 293 (11), 1338–1347. doi:10.1001/jama.293.11.1338
Lowes, D. A., Wallace, C., Murphy, M. P., Webster, N. R., and Galley, H. F. (2009). The Mitochondria Targeted Antioxidant MitoQ Protects against Fluoroquinolone-Induced Oxidative Stress and Mitochondrial Membrane Damage in Human Achilles Tendon Cells. Free Radic. Res. 43 (4), 323–328. doi:10.1080/10715760902736275
Lu, J., and Holmgren, A. (2014). The Thioredoxin Antioxidant System. Free Radic. Biol. Med. 66, 75–87. doi:10.1016/j.freeradbiomed.2013.07.036
Lu, M., Su, C., Qiao, C., Bian, Y., Ding, J., and Hu, G. (2016). Metformin Prevents Dopaminergic Neuron Death in MPTP/P-Induced Mouse Model of Parkinson's Disease via Autophagy and Mitochondrial ROS Clearance. Int. J. Neuropsychopharmacol. 19 (9). doi:10.1093/ijnp/pyw047
Madiraju, A. K., Erion, D. M., Rahimi, Y., Zhang, X.-M., Braddock, D. T., Albright, R. A., et al. (2014). Metformin Suppresses Gluconeogenesis by Inhibiting Mitochondrial Glycerophosphate Dehydrogenase. Nature 510 (7506), 542–546. doi:10.1038/nature13270
Magda, D., and Miller, R. A. (2006). Motexafin Gadolinium: a Novel Redox Active Drug for Cancer Therapy. Seminars Cancer Biol. 16 (6), 466–476. doi:10.1016/j.semcancer.2006.09.002
Mahadev, K., Motoshima, H., Wu, X., Ruddy, J. M., Arnold, R. S., Cheng, G., et al. (2004). The NAD(P)H Oxidase Homolog Nox4 Modulates Insulin-Stimulated Generation of H 2 O 2 and Plays an Integral Role in Insulin Signal Transduction. Mol. Cell Biol. 24 (5), 1844–1854. doi:10.1128/mcb.24.5.1844-1854.2004
Mahadev, K., Wu, X., Zilbering, A., Zhu, L., Lawrence, J. T. R., and Goldstein, B. J. (2001). Hydrogen Peroxide Generated during Cellular Insulin Stimulation Is Integral to Activation of the Distal Insulin Signaling Cascade in 3T3-L1 Adipocytes. J. Biol. Chem. 276 (52), 48662–48669. doi:10.1074/jbc.m105061200
Maiellaro-Rafferty, K., Weiss, D., Joseph, G., Wan, W., Gleason, R. L., and Taylor, W. R. (2011). Catalase Overexpression in Aortic Smooth Muscle Prevents Pathological Mechanical Changes Underlying Abdominal Aortic Aneurysm Formation. Am. J. Physiology-Heart Circulatory Physiology 301 (2), H355–H362. doi:10.1152/ajpheart.00040.2011
Malhotra, J. D., and Kaufman, R. J. (2007). Endoplasmic Reticulum Stress and Oxidative Stress: a Vicious Cycle or a Double-Edged Sword? Antioxidants Redox Signal. 9 (12), 2277–2294. doi:10.1089/ars.2007.1782
Mallat, Z., Philip, I., Lebret, M., Chatel, D., Maclouf, J., and Tedgui, A. (1998). Elevated Levels of 8-Iso-Prostaglandin F 2α in Pericardial Fluid of Patients with Heart Failure. Circulation 97 (16), 1536–1539. doi:10.1161/01.cir.97.16.1536
Manczak, M., Park, B. S., Jung, Y., and Reddy, P. H. (2004). Differential Expression of Oxidative Phosphorylation Genes in Patients with Alzheimer's Disease: Implications for Early Mitochondrial Dysfunction and Oxidative Damage. Nmm 5 (2), 147–162. doi:10.1385/nmm:5:2:147
Manczak, M., and Reddy, P. H. (2012). Abnormal Interaction of VDAC1 with Amyloid Beta and Phosphorylated Tau Causes Mitochondrial Dysfunction in Alzheimer's Disease. Hum. Mol. Genet. 21 (23), 5131–5146. doi:10.1093/hmg/dds360
Mandal, S., Lindgren, A. G., Srivastava, A. S., Clark, A. T., and Banerjee, U. (2011). Mitochondrial Function Controls Proliferation and Early Differentiation Potential of Embryonic Stem Cells. Stem Cells 29 (3), 486–495. doi:10.1002/stem.590
Mannucci, E., Tesi, F., Bardini, G., Ognibene, A., Petracca, M. G., Ciani, S., et al. (2004). Effects of Metformin on Glucagon-like Peptide-1 Levels in Obese Patients with and without Type 2 Diabetes. Diabetes Nutr. Metab. 17 (6), 336–342.
Marguet, D., Baggio, L., Kobayashi, T., Bernard, A.-M., Pierres, M., Nielsen, P. F., et al. (2000). Enhanced Insulin Secretion and Improved Glucose Tolerance in Mice Lacking CD26. Proc. Natl. Acad. Sci. U.S.A. 97 (12), 6874–6879. doi:10.1073/pnas.120069197
Marklund, S. L. (1984). Extracellular Superoxide Dismutase and Other Superoxide Dismutase Isoenzymes in Tissues from Nine Mammalian Species. Biochem. J. 222 (3), 649–655. doi:10.1042/bj2220649
Marques, O., and Outeiro, T. F. (2012). Alpha-synuclein: from Secretion to Dysfunction and Death. Cell Death Dis. 3, e350. doi:10.1038/cddis.2012.94
Martin, L. J. (2011). Mitochondrial Pathobiology in ALS. J. Bioenerg. Biomembr. 43 (6), 569–579. doi:10.1007/s10863-011-9395-y
Martin, L. J., Pan, Y., Price, A. C., Sterling, W., Copeland, N. G., Jenkins, N. A., et al. (2006). Parkinson's Disease -Synuclein Transgenic Mice Develop Neuronal Mitochondrial Degeneration and Cell Death. J. Neurosci. 26 (1), 41–50. doi:10.1523/jneurosci.4308-05.2006
Martínez-Martín, P., Gil-Nagel, A., Gracia, L. M., Gómez, J. B., Martínez-Sarriés, J., and Bermejo, F. (1994). Unified Parkinson's Disease Rating Scale Characteristics and Structure. Mov. Disord. 9 (1), 76–83. doi:10.1002/mds.870090112
Marullo, R., Werner, E., Degtyareva, N., Moore, B., Altavilla, G., Ramalingam, S. S., et al. (2013). Cisplatin Induces a Mitochondrial-ROS Response that Contributes to Cytotoxicity Depending on Mitochondrial Redox Status and Bioenergetic Functions. PLoS One 8 (11), e81162. doi:10.1371/journal.pone.0081162
Marycz, K., Tomaszewski, K. A., Kornicka, K., Henry, B. M., Wroński, S., Tarasiuk, J., et al. (2016). Metformin Decreases Reactive Oxygen Species, Enhances Osteogenic Properties of Adipose-Derived Multipotent Mesenchymal Stem Cells In Vitro, and Increases Bone Density In Vivo. Oxid. Med. Cell Longev. 2016, 9785890. doi:10.1155/2016/9785890
Masselli, E., Pozzi, G., Vaccarezza, M., Mirandola, P., Galli, D., Vitale, M., et al. (2020). ROS in Platelet Biology: Functional Aspects and Methodological Insights. Int. J. Mol. Sci. 21 (14). doi:10.3390/ijms21144866
Matsuo, Y., and Yodoi, J. (2013). Extracellular Thioredoxin: a Therapeutic Tool to Combat Inflammation. Cytokine & Growth Factor Rev. 24 (4), 345–353. doi:10.1016/j.cytogfr.2013.01.001
Matsushima, S., Ide, T., Yamato, M., Matsusaka, H., Hattori, F., Ikeuchi, M., et al. (2006). Overexpression of Mitochondrial Peroxiredoxin-3 Prevents Left Ventricular Remodeling and Failure after Myocardial Infarction in Mice. Circulation 113 (14), 1779–1786. doi:10.1161/circulationaha.105.582239
Maurer, I., Zierz, S., and Moller, H. J. (2000). A Selective Defect of Cytochrome C Oxidase Is Present in Brain of Alzheimer Disease Patients. Neurobiol. Aging 21 (3), 455–462. doi:10.1016/s0197-4580(00)00112-3
Mazurek, S., Boschek, C. B., Hugo, F., and Eigenbrodt, E. (2005). Pyruvate Kinase Type M2 and its Role in Tumor Growth and Spreading. Seminars Cancer Biol. 15 (4), 300–308. doi:10.1016/j.semcancer.2005.04.009
Mazurek, S. (2011). Pyruvate Kinase Type M2: a Key Regulator of the Metabolic Budget System in Tumor Cells. Int. J. Biochem. Cell Biol. 43 (7), 969–980. doi:10.1016/j.biocel.2010.02.005
Mburu, D. N., Maitho, T. E., and Lökken, P. (1990). Acetylsalicylic Acid or Paracetamol? East Afr. Med. J. 67 (5), 302–310.
McCarty, M. F., and Block, K. I. (2006). Preadministration of High-Dose Salicylates, Suppressors of NF-Κb Activation, May Increase the Chemosensitivity of Many Cancers: An Example of Proapoptotic Signal Modulation Therapy. Integr. Cancer Ther. 5 (3), 252–268. doi:10.1177/1534735406291499
McKee, E. E., Ferguson, M., Bentley, A. T., and Marks, T. A. (2006). Inhibition of Mammalian Mitochondrial Protein Synthesis by Oxazolidinones. Antimicrob. Agents Chemother. 50 (6), 2042–2049. doi:10.1128/aac.01411-05
Meiser, J., Weindl, D., and Hiller, K. (2013). Complexity of Dopamine Metabolism. Cell Commun. Signal 11 (1), 34. doi:10.1186/1478-811x-11-34
Meitzler, J. L., Antony, S., Wu, Y., Juhasz, A., Liu, H., Jiang, G., et al. (2014). NADPH Oxidases: a Perspective on Reactive Oxygen Species Production in Tumor Biology. Antioxidants Redox Signal. 20 (17), 2873–2889. doi:10.1089/ars.2013.5603
Merry, T. L., and Ristow, M. (2016). Mitohormesis in Exercise Training. Free Radic. Biol. Med. 98, 123–130. doi:10.1016/j.freeradbiomed.2015.11.032
Michaeli, S., öz, G., Sorce, D. J., Garwood, M., Ugurbil, K., Majestic, S., et al. (2007). Assessment of Brain Iron and Neuronal Integrity in Patients with Parkinson's Disease Using Novel MRI Contrasts. Mov. Disord. 22 (3), 334–340. doi:10.1002/mds.21227
Migliaccio, E., Giorgio, M., Mele, S., Pelicci, G., Reboldi, P., Pandolfi, P. P., et al. (1999). The P66shc Adaptor Protein Controls Oxidative Stress Response and Life Span in Mammals. Nature 402 (6759), 309–313. doi:10.1038/46311
Miller, R. A., Chu, Q., Xie, J., Foretz, M., Viollet, B., and Birnbaum, M. J. (2013). Biguanides Suppress Hepatic Glucagon Signalling by Decreasing Production of Cyclic AMP. Nature 494 (7436), 256–260. doi:10.1038/nature11808
Mingeot-Leclercq, M.-P., and Tulkens, P. M. (1999). Aminoglycosides: Nephrotoxicity. Antimicrob. Agents Chemother. 43 (5), 1003–1012. doi:10.1128/aac.43.5.1003
Mittal, M., Siddiqui, M. R., Tran, K., Reddy, S. P., and Malik, A. B. (2014). Reactive Oxygen Species in Inflammation and Tissue Injury. Antioxidants Redox Signal. 20 (7), 1126–1167. doi:10.1089/ars.2012.5149
Mizuno, Y., Sone, N., and Saitoh, T. (1987). Effects of 1-Methyl-4-Phenyl-1,2,3,6-Tetrahydropyridine and 1-Methyl-4-Phenylpyridinium Ion on Activities of the Enzymes in the Electron Transport System in Mouse Brain. J. Neurochem. 48 (6), 1787–1793. doi:10.1111/j.1471-4159.1987.tb05737.x
Mollazadeh, H., Tavana, E., Fanni, G., Bo, S., Banach, M., Pirro, M., et al. (2021). Effects of Statins on Mitochondrial Pathways. J. Cachexia, Sarcopenia Muscle 12 (2), 237–251. doi:10.1002/jcsm.12654
Moloney, A. M., Griffin, R. J., Timmons, S., O’Connor, R., Ravid, R., and O’Neill, C. (2010). Defects in IGF-1 Receptor, Insulin Receptor and IRS-1/2 in Alzheimer's Disease Indicate Possible Resistance to IGF-1 and Insulin Signalling. Neurobiol. Aging 31 (2), 224–243. doi:10.1016/j.neurobiolaging.2008.04.002
Moran, C., Phan, T. G., Chen, J., Blizzard, L., Beare, R., Venn, A., et al. (2013). Brain Atrophy in Type 2 Diabetes. Diabetes Care 36 (12), 4036–4042. doi:10.2337/dc13-0143
Morita-Fujimura, Y., Fujimura, M., Gasche, Y., Copin, J.-C., and Chan, P. H. (2000). Overexpression of Copper and Zinc Superoxide Dismutase in Transgenic Mice Prevents the Induction and Activation of Matrix Metalloproteinases after Cold Injury-Induced Brain Trauma. J. Cereb. Blood Flow. Metab. 20 (1), 130–138. doi:10.1097/00004647-200001000-00017
Morsi, M., Maher, A., Aboelmagd, O., Johar, D., and Bernstein, L. (2018). A Shared Comparison of Diabetes Mellitus and Neurodegenerative Disorders. J Cell. Biochem. 119 (2), 1249–1256. doi:10.1002/jcb.26261
Moulder, S., Dhillon, N., Ng, C., Hong, D., Wheler, J., Naing, A., et al. (2010). A Phase I Trial of Imexon, a Pro-oxidant, in Combination with Docetaxel for the Treatment of Patients with Advanced Breast, Non-small Cell Lung and Prostate Cancer. Invest New Drugs 28 (5), 634–640. doi:10.1007/s10637-009-9273-1
Müftüoglu, M., Elibol, B., Dalmızrak, Ö., Ercan, A., Kulaksız, G., Ögüs, H., et al. (2004). Mitochondrial Complex I and IV Activities in Leukocytes from Patients with Parkin Mutations. Mov. Disord. 19 (5), 544–548. doi:10.1002/mds.10695
Mummidi, S., Das, N. A., Carpenter, A. J., Kandikattu, H., Krenz, M., Siebenlist, U., et al. (2016). Metformin Inhibits Aldosterone-Induced Cardiac Fibroblast Activation, Migration and Proliferation In Vitro, and Reverses Aldosterone+salt-Induced Cardiac Fibrosis In Vivo. J. Mol. Cell. Cardiol. 98, 95–102. doi:10.1016/j.yjmcc.2016.07.006
Musi, N., Hirshman, M. F., Nygren, J., Svanfeldt, M., Bavenholm, P., Rooyackers, O., et al. (2002). Metformin Increases AMP-Activated Protein Kinase Activity in Skeletal Muscle of Subjects with Type 2 Diabetes. Diabetes 51 (7), 2074–2081. doi:10.2337/diabetes.51.7.2074
Muxfeldt, M., and Schaper, W. (1987). The Activity of Xanthine Oxidase in Heart of Pigs, guinea Pigs, Rabbits, Rats, and Humans. Basic Res. Cardiol. 82 (5), 486–492. doi:10.1007/bf01907096
Nagano, Y., Matsui, H., Shimokawa, O., Hirayama, A., Tamura, M., Nakamura, Y., et al. (2012). Rebamipide Attenuates Nonsteroidal Anti-inflammatory Drugs (NSAID) Induced Lipid Peroxidation by the Manganese Superoxide Dismutase (MnSOD) Overexpression in Gastrointestinal Epithelial Cells. J. Physiol. Pharmacol. 63 (2), 137–142.
Nagatsu, T., and Sawada, M. (2009). L-Dopa Therapy for Parkinson's Disease: Past, Present, and Future. Park. Relat. Disord. 15 (Suppl. 1), S3–S8. doi:10.1016/s1353-8020(09)70004-5
Nakamura, H., De Rosa, S., Roederer, M., Anderson, M. T., Dubs, J. G., Yodoi, J., et al. (1996). Elevation of Plasma Thioredoxin Levels in HIV-Infected Individuals. Int. Immunol. 8 (4), 603–611. doi:10.1093/intimm/8.4.603
Nakamura, H., Hoshino, Y., Okuyama, H., Matsuo, Y., and Yodoi, J. (2009). Thioredoxin 1 Delivery as New Therapeutics. Adv. Drug Deliv. Rev. 61 (4), 303–309. doi:10.1016/j.addr.2009.01.003
Nakamura, K., Kusano, K. F., Matsubara, H., Nakamura, Y., Miura, A., Nishii, N., et al. (2005). Relationship between Oxidative Stress and Systolic Dysfunction in Patients with Hypertrophic Cardiomyopathy. J. Cardiac Fail. 11 (2), 117–123. doi:10.1016/j.cardfail.2004.05.005
Nakamura, K., Kusano, K., Nakamura, Y., Kakishita, M., Ohta, K., Nagase, S., et al. (2002). Carvedilol Decreases Elevated Oxidative Stress in Human Failing Myocardium. Circulation 105 (24), 2867–2871. doi:10.1161/01.cir.0000018605.14470.dd
Nakamura, K., Murakami, M., Miura, D., Yunoki, K., Enko, K., Tanaka, M., et al. (2011). Beta-Blockers and Oxidative Stress in Patients with Heart Failure. Pharmaceuticals 4 (8), 1088–1100. doi:10.3390/ph4081088
Naseem, K. M. (2005). The Role of Nitric Oxide in Cardiovascular Diseases. Mol. Asp. Med. 26 (1-2), 33–65. doi:10.1016/j.mam.2004.09.003
Natali, A., and Ferrannini, E. (2006). Effects of Metformin and Thiazolidinediones on Suppression of Hepatic Glucose Production and Stimulation of Glucose Uptake in Type 2 Diabetes: a Systematic Review. Diabetologia 49 (3), 434–441. doi:10.1007/s00125-006-0141-7
Nath, N., Khan, M., Paintlia, M. K., Hoda, M. N., Giri, S., and Giri, S. (2009). Metformin Attenuated the Autoimmune Disease of the Central Nervous System in Animal Models of Multiple Sclerosis. J. Immunol. 182 (12), 8005–8014. doi:10.4049/jimmunol.0803563
Neeley, W. L., and Essigmann, J. M. (2006). Mechanisms of Formation, Genotoxicity, and Mutation of Guanine Oxidation Products. Chem. Res. Toxicol. 19 (4), 491–505. doi:10.1021/tx0600043
Newsholme, P., Haber, E. P., Hirabara, S. M., Rebelato, E. L., Procopio, J., Morgan, D., et al. (2007). Diabetes Associated Cell Stress and Dysfunction: Role of Mitochondrial and Non-mitochondrial ROS Production and Activity. J. Physiol. 583 (Pt 1), 9–24. doi:10.1113/jphysiol.2007.135871
Newsholme, P., Cruzat, V., Arfuso, F., and Keane, K. (2014). Nutrient Regulation of Insulin Secretion and Action. J. Endocrinol. 221 (3), R105–R120. doi:10.1530/joe-13-0616
Newsholme, P., Gaudel, C., and Krause, M. (2012). Mitochondria and Diabetes. An Intriguing Pathogenetic Role. Adv. Exp. Med. Biol. 942, 235–247. doi:10.1007/978-94-007-2869-1_10
Ng, T. P., Feng, L., Yap, K. B., Lee, T. S., Tan, C. H., and Winblad, B. (2014). Long-term Metformin Usage and Cognitive Function Among Older Adults with Diabetes. Jad 41 (1), 61–68. doi:10.3233/jad-131901
Nguyen, L. V., Ta, Q. V., Dang, T. B., Nguyen, P. H., Nguyen, T., Pham, T. V. H., et al. (2019). Carvedilol Improves Glucose Tolerance and Insulin Sensitivity in Treatment of Adrenergic Overdrive in High Fat Diet-Induced Obesity in Mice. PLoS One 14 (11), e0224674. doi:10.1371/journal.pone.0224674
Nichols, W., Pankratz, N., Hernandez, D., Paisanruiz, C., Jain, S., Halter, C., et al. (2005). Genetic Screening for a Single Common Mutation in Familial Parkinson's Disease. Lancet 365 (9457), 410–412. doi:10.1016/s0140-6736(05)70235-x
Nishikawa, T., Edelstein, D., and Brownlee, M. (2000). The Missing Link: a Single Unifying Mechanism for Diabetic Complications. Kidney Int. 58, S26–S30. doi:10.1046/j.1523-1755.2000.07705.x
Nuttall, S. L., Khan, J. N., Thorpe, G. H., Langford, N., and Kendall, M. J. (2003). The Impact of Therapeutic Doses of Paracetamol on Serum Total Antioxidant Capacity. J. Clin. Pharm. Ther. 28 (4), 289–294. doi:10.1046/j.1365-2710.2003.00493.x
Odegaard, A. O., Jacobs, D. R., Sanchez, O. A., Goff, D. C., Reiner, A. P., and Gross, M. D. (2016). Oxidative Stress, Inflammation, Endothelial Dysfunction and Incidence of Type 2 Diabetes. Cardiovasc Diabetol. 15, 51. doi:10.1186/s12933-016-0369-6
Oelze, M., Daiber, A., Brandes, R. P., Hortmann, M., Wenzel, P., Hink, U., et al. (2006). Nebivolol Inhibits Superoxide Formation by NADPH Oxidase and Endothelial Dysfunction in Angiotensin II-Treated Rats. Hypertension 48 (4), 677–684. doi:10.1161/01.hyp.0000239207.82326.29
Oelze, M., Kröller-Schön, S., Welschof, P., Jansen, T., Hausding, M., Mikhed, Y., et al. (2014). The Sodium-Glucose Co-transporter 2 Inhibitor Empagliflozin Improves Diabetes-Induced Vascular Dysfunction in the Streptozotocin Diabetes Rat Model by Interfering with Oxidative Stress and Glucotoxicity. PLoS One 9 (11), e112394. doi:10.1371/journal.pone.0112394
Ogawa, K., Suzuki, K., Okutsu, M., Yamazaki, K., and Shinkai, S. (2008). The Association of Elevated Reactive Oxygen Species Levels from Neutrophils with Low-Grade Inflammation in the Elderly. Immun. Ageing 5, 13. doi:10.1186/1742-4933-5-13
Oh, B., Figtree, G., Costa, D., Eade, T., Hruby, G., Lim, S., et al. (2016). Oxidative Stress in Prostate Cancer Patients: A Systematic Review of Case Control Studies. Prostate Int. 4 (3), 71–87. doi:10.1016/j.prnil.2016.05.002
Okamoto, K., Kusano, T., and Nishino, T. (2013). Chemical Nature and Reaction Mechanisms of the Molybdenum Cofactor of Xanthine Oxidoreductase. Cpd 19 (14), 2606–2614. doi:10.2174/1381612811319140010
Olsen, R. H. J., Johnson, L. A., Zuloaga, D. G., Limoli, C. L., and Raber, J. (2013). Enhanced Hippocampus-dependent Memory and Reduced Anxiety in Mice Over-expressing Human Catalase in Mitochondria. J. Neurochem. 125 (2), 303–313. doi:10.1111/jnc.12187
Olson, P. A., Tkatch, T., Hernandez-Lopez, S., Ulrich, S., Ilijic, E., Mugnaini, E., et al. (2005). G-protein-coupled Receptor Modulation of Striatal CaV1.3 L-type Ca2+ Channels Is Dependent on a Shank-Binding Domain. J. Neurosci. 25 (5), 1050–1062. doi:10.1523/jneurosci.3327-04.2005
Olsson, A. H., Rönn, T., Elgzyri, T., Hansson, O., Eriksson, K.-F., Groop, L., et al. (2011). The Expression of Myosin Heavy Chain (MHC) Genes in Human Skeletal Muscle Is Related to Metabolic Characteristics Involved in the Pathogenesis of Type 2 Diabetes. Mol. Genet. Metabolism 103 (3), 275–281. doi:10.1016/j.ymgme.2011.03.017
Onken, B., and Driscoll, M. (2010). Metformin Induces a Dietary Restriction-like State and the Oxidative Stress Response to Extend C. elegans Healthspan via AMPK, LKB1, and SKN-1. PLoS One 5 (1), e8758. doi:10.1371/journal.pone.0008758
Ornelas, A., Zacharias-Millward, N., Menter, D. G., Davis, J. S., Lichtenberger, L., Hawke, D., et al. (2017). Beyond COX-1: the Effects of Aspirin on Platelet Biology and Potential Mechanisms of Chemoprevention. Cancer Metastasis Rev. 36 (2), 289–303. doi:10.1007/s10555-017-9675-z
Osorio, H., Coronel, I., Arellano, A., Pacheco, U., Bautista, R., Franco, M., et al. (2012). Sodium-glucose Cotransporter Inhibition Prevents Oxidative Stress in the Kidney of Diabetic Rats. Oxid. Med. Cell Longev. 2012, 542042. doi:10.1155/2012/542042
Ostrowski, S., Marcinkiewicz, A., Nowak, D., Zwoliński, R., and Jaszewski, R. (2012). Comparison of the Clinical Application of Reactive Oxygen Species and Inflammatory Markers in Patients with Endocarditis. aoms 2 (2), 244–249. doi:10.5114/aoms.2012.28551
Ou, Z., Kong, X., Sun, X., He, X., Zhang, L., Gong, Z., et al. (2018). Metformin Treatment Prevents Amyloid Plaque Deposition and Memory Impairment in APP/PS1 Mice. Brain, Behav. Immun. 69, 351–363. doi:10.1016/j.bbi.2017.12.009
Owen, M. R., Doran, E., and Halestrap, A. P. (2000). Evidence that Metformin Exerts its Anti-diabetic Effects through Inhibition of Complex 1 of the Mitochondrial Respiratory Chain. Biochem. J. 348 (Pt 3), 607–614. doi:10.1042/bj3480607
Ozben, T. (2007). Oxidative Stress and Apoptosis: Impact on Cancer Therapy. J. Pharm. Sci. 96 (9), 2181–2196. doi:10.1002/jps.20874
Pacher, P., and Szabo, C. (2006). Role of Peroxynitrite in the Pathogenesis of Cardiovascular Complications of Diabetes. Curr. Opin. Pharmacol. 6 (2), 136–141. doi:10.1016/j.coph.2006.01.001
Pahwa, R., Factor, S. A., Lyons, K. E., Ondo, W. G., Gronseth, G., Bronte-Stewart, H., et al. (2006). Practice Parameter: Treatment of Parkinson Disease with Motor Fluctuations and Dyskinesia (An Evidence-Based Review): [RETIRED]. Neurology 66 (7), 983–995. doi:10.1212/01.wnl.0000215250.82576.87
Paiva, C. N., and Bozza, M. T. (2014). Are Reactive Oxygen Species Always Detrimental to Pathogens? Antioxidants Redox Signal. 20 (6), 1000–1037. doi:10.1089/ars.2013.5447
Pandey, K. B., Mishra, N., and Rizvi, S. I. (2010). Protein Oxidation Biomarkers in Plasma of Type 2 Diabetic Patients. Clin. Biochem. 43 (4-5), 508–511. doi:10.1016/j.clinbiochem.2009.11.011
Panth, N., Paudel, K. R., and Parajuli, K. (2016). Reactive Oxygen Species: A Key Hallmark of Cardiovascular Disease. Adv. Med. 2016, 9152732. doi:10.1155/2016/9152732
Parekh, A. K., Galloway, J. M., Hong, Y., and Wright, J. S. (2013). Aspirin in the Secondary Prevention of Cardiovascular Disease. N. Engl. J. Med. 368 (3), 204–205. doi:10.1056/nejmp1213380
Patil, S. P., Jain, P. D., Ghumatkar, P. J., Tambe, R., and Sathaye, S. (2014). Neuroprotective Effect of Metformin in MPTP-Induced Parkinson's Disease in Mice. Neuroscience 277, 747–754. doi:10.1016/j.neuroscience.2014.07.046
Patrignani, P., Sacco, A., Sostres, C., Bruno, A., Dovizio, M., Piazuelo, E., et al. (2017). Low-Dose Aspirin Acetylates Cyclooxygenase-1 in Human Colorectal Mucosa: Implications for the Chemoprevention of Colorectal Cancer. Clin. Pharmacol. Ther. 102 (1), 52–61. doi:10.1002/cpt.639
Patrono, C. (2015). The Multifaceted Clinical Readouts of Platelet Inhibition by Low-Dose Aspirin. J. Am. Coll. Cardiol. 66 (1), 74–85. doi:10.1016/j.jacc.2015.05.012
Paudel, Y. N., Angelopoulou, E., Piperi, C., Shaikh, M. F., and Othman, I. (2020). Emerging Neuroprotective Effect of Metformin in Parkinson's Disease: A Molecular Crosstalk. Pharmacol. Res. 152, 104593. doi:10.1016/j.phrs.2019.104593
Perez, M., Gonzalez-Sanchez, E., Gonzalez-Loyola, A., Gonzalez-Buitrago, J., and Marin, J. (2011). Mitochondrial Genome Depletion Dysregulates Bile Acid- and Paracetamol-Induced Expression of the Transporters Mdr1, Mrp1 and Mrp4 in Liver Cells. Br. J. Pharmacol. 162 (8), 1686–1699. doi:10.1111/j.1476-5381.2010.01174.x
Pérez-Revuelta, B. I., Hettich, M. M., Ciociaro, A., Rotermund, C., Kahle, P. J., Krauss, S., et al. (2014). Metformin Lowers Ser-129 Phosphorylated α-synuclein Levels via mTOR-dependent Protein Phosphatase 2A Activation. Cell Death Dis. 5, e1209. doi:10.1038/cddis.2014.175
Perier, C., Tieu, K., Guégan, C., Caspersen, C., Jackson-Lewis, V., Carelli, V., et al. (2005). Complex I Deficiency Primes Bax-dependent Neuronal Apoptosis through Mitochondrial Oxidative Damage. Proc. Natl. Acad. Sci. U.S.A. 102 (52), 19126–19131. doi:10.1073/pnas.0508215102
Perillo, B., Di Donato, M., Pezone, A., Di Zazzo, E., Giovannelli, P., Galasso, G., et al. (2020). ROS in Cancer Therapy: the Bright Side of the Moon. Exp. Mol. Med. 52 (2), 192–203. doi:10.1038/s12276-020-0384-2
Perry, E. A., Bennett, C. F., Luo, C., Balsa, E., Jedrychowski, M., O’Malley, K. E., et al. (2021). Tetracyclines Promote Survival and Fitness in Mitochondrial Disease Models. Nat. Metab. 3 (1), 33–42. doi:10.1038/s42255-020-00334-y
Pickrell, A. M., and Youle, R. J. (2015). The Roles of PINK1, Parkin, and Mitochondrial Fidelity in Parkinson's Disease. Neuron 85 (2), 257–273. doi:10.1016/j.neuron.2014.12.007
Pimentel, D. R., Amin, J. K., Xiao, L., Miller, T., Viereck, J., Oliver-Krasinski, J., et al. (2001). Reactive Oxygen Species Mediate Amplitude-dependent Hypertrophic and Apoptotic Responses to Mechanical Stretch in Cardiac Myocytes. Circulation Res. 89 (5), 453–460. doi:10.1161/hh1701.096615
Pintana, H., Apaijai, N., Chattipakorn, N., and Chattipakorn, S. C. (2013). DPP-4 Inhibitors Improve Cognition and Brain Mitochondrial Function of Insulin-Resistant Rats. J. Endocrinol. 218 (1), 1–11. doi:10.1530/joe-12-0521
Pipatpiboon, N., Pintana, H., Pratchayasakul, W., Chattipakorn, N., and Chattipakorn, S. C. (2013). DPP4-inhibitor Improves Neuronal Insulin Receptor Function, Brain Mitochondrial Function and Cognitive Function in Rats with Insulin Resistance Induced by High-Fat Diet Consumption. Eur. J. Neurosci. 37 (5), 839–849. doi:10.1111/ejn.12088
Piskovatska, V., Stefanyshyn, N., Storey, K. B., Vaiserman, A. M., and Lushchak, O. (2019). Metformin as a Geroprotector: Experimental and Clinical Evidence. Biogerontology 20 (1), 33–48. doi:10.1007/s10522-018-9773-5
Pisoschi, A. M., and Pop, A. (2015). The Role of Antioxidants in the Chemistry of Oxidative Stress: A Review. Eur. J. Med. Chem. 97, 55–74. doi:10.1016/j.ejmech.2015.04.040
Pissadaki, E. K., and Bolam, J. P. (2013). The Energy Cost of Action Potential Propagation in Dopamine Neurons: Clues to Susceptibility in Parkinson's Disease. Front. Comput. Neurosci. 7, 13. doi:10.3389/fncom.2013.00013
Pochini, L., Galluccio, M., Scumaci, D., Giangregorio, N., Tonazzi, A., Palmieri, F., et al. (2008). Interaction of β-lactam Antibiotics with the Mitochondrial Carnitine/acylcarnitine Transporter. Chemico-Biological Interact. 173 (3), 187–194. doi:10.1016/j.cbi.2008.03.003
Polymeropoulos, M. H., Lavedan, C., Leroy, E., Ide, S. E., Dehejia, A., Dutra, A., et al. (1997). Mutation in the α-Synuclein Gene Identified in Families with Parkinson's Disease. Science 276 (5321), 2045–2047. doi:10.1126/science.276.5321.2045
Poole, K. (2012). Stress Responses as Determinants of Antimicrobial Resistance in Gram-Negative Bacteria. Trends Microbiol. 20 (5), 227–234. doi:10.1016/j.tim.2012.02.004
Popa-Wagner, A., Mitran, S., Sivanesan, S., Chang, E., and Buga, A. M. (2013). ROS and Brain Diseases: the Good, the Bad, and the Ugly. Oxid. Med. Cell Longev. 2013, 963520. doi:10.1155/2013/963520
Prince, M., Bryce, R., Albanese, E., Wimo, A., Ribeiro, W., and Ferri, C. P. (2013). The Global Prevalence of Dementia: a Systematic Review and Metaanalysis. Alzheimer's & Dement. 9 (1), 63–75 e2. doi:10.1016/j.jalz.2012.11.007
Pujos-Guillot, E., Pickering, G., Lyan, B., Ducheix, G., Brandolini-Bunlon, M., Glomot, F., et al. (2012). Therapeutic Paracetamol Treatment in Older Persons Induces Dietary and Metabolic Modifications Related to Sulfur Amino Acids. Age 34 (1), 181–193. doi:10.1007/s11357-011-9218-4
Purssell, E. (2002). Treating Fever in Children: Paracetamol or Ibuprofen? Br. J. Community Nurs. 7 (6), 316–320. doi:10.12968/bjcn.2002.7.6.10477
Puspita, L., Chung, S. Y., and Shim, J.-w. (2017). Oxidative Stress and Cellular Pathologies in Parkinson's Disease. Mol. Brain 10 (1), 53. doi:10.1186/s13041-017-0340-9
Putnam, C. D., Arvai, A. S., Bourne, Y., and Tainer, J. A. (2000). Active and Inhibited Human Catalase Structures: Ligand and NADPH Binding and Catalytic Mechanism 1 1Edited by R. Huber. J. Mol. Biol. 296 (1), 295–309. doi:10.1006/jmbi.1999.3458
Pyatigorskaya, N., Sharman, M., Corvol, J.-C., Valabregue, R., Yahia-Cherif, L., Poupon, F., et al. (2015). High Nigral Iron Deposition in LRRK2 and Parkin Mutation Carriers Using R2* Relaxometry. Mov. Disord. 30 (8), 1077–1084. doi:10.1002/mds.26218
Rain, C., and Rada, G. (2015). Is Carvedilol Better Than Other Beta-Blockers for Heart Failure? Medwave 15 (Suppl. 1), e6168. doi:10.5867/medwave.2015.6168
Ramprasath, T., Murugan, P. S., Kalaiarasan, E., Gomathi, P., Rathinavel, A., and Selvam, G. S. (2012). Genetic Association of Glutathione Peroxidase-1 (GPx-1) and NAD(P)H:Quinone Oxidoreductase 1(NQO1) Variants and Their Association of CAD in Patients with Type-2 Diabetes. Mol. Cell Biochem. 361 (1-2), 143–150. doi:10.1007/s11010-011-1098-5
Ramsay, R. R., Krueger, M. J., Youngster, S. K., Gluck, M. R., Casida, J. E., and Singer, T. P. (1991). Interaction of 1-Methyl-4-Phenylpyridinium Ion (MPP+) and its Analogs with the Rotenone/piericidin Binding Site of NADH Dehydrogenase. J. Neurochem. 56 (4), 1184–1190. doi:10.1111/j.1471-4159.1991.tb11409.x
Ravn-Haren, G., Olsen, A., Tjønneland, A., Dragsted, L. O., Nexø, B. A., Wallin, H., et al. (2006). Associations between GPX1 Pro198Leu Polymorphism, Erythrocyte GPX Activity, Alcohol Consumption and Breast Cancer Risk in a Prospective Cohort Study. Carcinogenesis 27 (4), 820–825. doi:10.1093/carcin/bgi267
Reddy, P. H., Manczak, M., Mao, P., Calkins, M. J., Reddy, A. P., and Shirendeb, U. (2010). Amyloid-beta and Mitochondria in Aging and Alzheimer's Disease: Implications for Synaptic Damage and Cognitive Decline. J. Alzheimers Dis. 20 Suppl 2 (Suppl. 2), S499–S512. doi:10.3233/JAD-2010-100504
Reddy, P. H. (2006). Mitochondrial Oxidative Damage in Aging and Alzheimer's Disease: Implications for Mitochondrially Targeted Antioxidant Therapeutics. J. Biomed. Biotechnol. 2006 (3), 31372. doi:10.1155/JBB/2006/31372
Reddy, P. H. (2009). Amyloid Beta, Mitochondrial Structural and Functional Dynamics in Alzheimer's Disease. Exp. Neurol. 218 (2), 286–292. doi:10.1016/j.expneurol.2009.03.042
Reddy, P. H., and Beal, M. F. (2008). Amyloid Beta, Mitochondrial Dysfunction and Synaptic Damage: Implications for Cognitive Decline in Aging and Alzheimer's Disease. Trends Mol. Med. 14 (2), 45–53. doi:10.1016/j.molmed.2007.12.002
Reddy, P. H., and Shirendeb, U. P. (2012). Mutant Huntingtin, Abnormal Mitochondrial Dynamics, Defective Axonal Transport of Mitochondria, and Selective Synaptic Degeneration in Huntington's Disease. Biochimica Biophysica Acta (BBA) - Mol. Basis Dis. 1822 (2), 101–110. doi:10.1016/j.bbadis.2011.10.016
Reddy, P. H., Tripathi, R., Troung, Q., Tirumala, K., Reddy, T. P., Anekonda, V., et al. (2012). Abnormal Mitochondrial Dynamics and Synaptic Degeneration as Early Events in Alzheimer's Disease: Implications to Mitochondria-Targeted Antioxidant Therapeutics. Biochimica Biophysica Acta (BBA) - Mol. Basis Dis. 1822 (5), 639–649. doi:10.1016/j.bbadis.2011.10.011
Rena, G., and Lang, C. C. (2018). Repurposing Metformin for Cardiovascular Disease. Circulation 137 (5), 422–424. doi:10.1161/circulationaha.117.031735
Rhee, S. G., and Woo, H. A. (2011). Multiple Functions of Peroxiredoxins: Peroxidases, Sensors and Regulators of the Intracellular Messenger H2O2, and Protein Chaperones. Antioxidants Redox Signal. 15 (3), 781–794. doi:10.1089/ars.2010.3393
Richardson, J. R., Quan, Y., Sherer, T. B., Greenamyre, J. T., and Miller, G. W. (2005). Paraquat Neurotoxicity Is Distinct from that of MPTP and Rotenone. Toxicol. Sci. 88 (1), 193–201. doi:10.1093/toxsci/kfi304
Ridet, J.-L., Bensadoun, J.-C., Déglon, N., Aebischer, P., and Zurn, A. D. (2006). Lentivirus-mediated Expression of Glutathione Peroxidase: Neuroprotection in Murine Models of Parkinson's Disease. Neurobiol. Dis. 21 (1), 29–34. doi:10.1016/j.nbd.2005.06.003
Ripley, E., and Hirsch, A. (2010). Fifteen Years of Losartan: what Have We Learned about Losartan that Can Benefit Chronic Kidney Disease Patients? Ijnrd 3, 93–98. doi:10.2147/ijnrd.s7038
Ristow, M., and Schmeisser, K. (2014). Mitohormesis: Promoting Health and Lifespan by Increased Levels of Reactive Oxygen Species (ROS). Dose Response 12 (2), 288–341. doi:10.2203/dose-response.13-035.Ristow
Rivera, E. J., Goldin, A., Fulmer, N., Tavares, R., Wands, J. R., and de la Monte, S. M. (2005). Insulin and Insulin-like Growth Factor Expression and Function Deteriorate with Progression of Alzheimer's Disease: Link to Brain Reductions in Acetylcholine. Jad 8 (3), 247–268. doi:10.3233/jad-2005-8304
Rizzo, M. R., Barbieri, M., Marfella, R., and Paolisso, G. (2012). Reduction of Oxidative Stress and Inflammation by Blunting Daily Acute Glucose Fluctuations in Patients with Type 2 Diabetes. Diabetes Care 35 (10), 2076–2082. doi:10.2337/dc12-0199
Rochette, L., Zeller, M., Cottin, Y., and Vergely, C. (2014). Diabetes, Oxidative Stress and Therapeutic Strategies. Biochimica Biophysica Acta (BBA) - General Subj. 1840 (9), 2709–2729. doi:10.1016/j.bbagen.2014.05.017
Roffi, M., Patrono, C., Collet, J.-P., Mueller, C., Valgimigli, M., Andreotti, F., et al. (20152016). 2015 ESC Guidelines for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation. Eur. Heart J. 37 (3), 267–315. doi:10.1093/eurheartj/ehv320
Romano, M., Cianci, E., Simiele, F., and Recchiuti, A. (2015). Lipoxins and Aspirin-Triggered Lipoxins in Resolution of Inflammation. Eur. J. Pharmacol. 760, 49–63. doi:10.1016/j.ejphar.2015.03.083
Romo, R., and Schultz, W. (1990). Dopamine Neurons of the Monkey Midbrain: Contingencies of Responses to Active Touch during Self-Initiated Arm Movements. J. Neurophysiology 63 (3), 592–606. doi:10.1152/jn.1990.63.3.592
Rösen, P., and Osmers, A. (2006). Oxidative Stress in Young Zucker Rats with Impaired Glucose Tolerance Is Diminished by Acarbose. Horm. Metab. Res. 38 (9), 575–586. doi:10.1055/s-2006-950397
Rotermund, C., Machetanz, G., and Fitzgerald, J. C. (2018). The Therapeutic Potential of Metformin in Neurodegenerative Diseases. Front. Endocrinol. 9, 400. doi:10.3389/fendo.2018.00400
Roth, G. A., Mensah, G. A., Johnson, C. O., Addolorato, G., Ammirati, E., Baddour, L. M., et al. (2020). Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update from the GBD 2019 Study. J. Am. Coll. Cardiol. 76 (25), 2982–3021. doi:10.1016/j.jacc.2020.11.010
Rothwell, P. M., Wilson, M., Elwin, C.-E., Norrving, B., Algra, A., Warlow, C. P., et al. (2010). Long-term Effect of Aspirin on Colorectal Cancer Incidence and Mortality: 20-year Follow-Up of Five Randomised Trials. Lancet 376 (9754), 1741–1750. doi:10.1016/s0140-6736(10)61543-7
Rowe, S. E., Wagner, N. J., Li, L., Beam, J. E., Wilkinson, A. D., Radlinski, L. C., et al. (2020). Reactive Oxygen Species Induce Antibiotic Tolerance during Systemic Staphylococcus aureus Infection. Nat. Microbiol. 5 (2), 282–290. doi:10.1038/s41564-019-0627-y
Ruegsegger, G. N., Vanderboom, P. M., Dasari, S., Klaus, K. A., Kabiraj, P., McCarthy, C. B., et al. (2019). Exercise and Metformin Counteract Altered Mitochondrial Function in the Insulin-Resistant Brain. JCI Insight 4 (18). doi:10.1172/jci.insight.130681
Rui, Y., Tiwari, P., Xie, Z., and Zheng, J. Q. (2006). Acute Impairment of Mitochondrial Trafficking by Beta-Amyloid Peptides in Hippocampal Neurons. J. Neurosci. 26 (41), 10480–10487. doi:10.1523/jneurosci.3231-06.2006
Ryden, L., Rydén, L., Grant, P. J., Anker, S. D., Berne, C., Cosentino, F., et al. (2013). ESC Guidelines on Diabetes, Pre-diabetes, and Cardiovascular Diseases Developed in Collaboration with the EASD: the Task Force on Diabetes, Pre-diabetes, and Cardiovascular Diseases of the European Society of Cardiology (ESC) and Developed in Collaboration with the European Association for the Study of Diabetes (EASD). Eur. Heart J. 34 (39), 3035–3087. doi:10.1093/eurheartj/eht108
Sa-Nguanmoo, P., Tanajak, P., Kerdphoo, S., Jaiwongkam, T., Pratchayasakul, W., Chattipakorn, N., et al. (2017). SGLT2-inhibitor and DPP-4 Inhibitor Improve Brain Function via Attenuating Mitochondrial Dysfunction, Insulin Resistance, Inflammation, and Apoptosis in HFD-Induced Obese Rats. Toxicol. Appl. Pharmacol. 333, 43–50. doi:10.1016/j.taap.2017.08.005
Saewanee, N., Praputpittaya, T., Malaiwong, N., Chalorak, P., and Meemon, K. (2021). Neuroprotective Effect of Metformin on Dopaminergic Neurodegeneration and α-synuclein Aggregation in C. elegans Model of Parkinson's Disease. Neurosci. Res. 162, 13–21. doi:10.1016/j.neures.2019.12.017
Sahoo, B. M., Banik, B. K., Borah, P., and Jain, A. (2021). Reactive Oxygen Species (ROS): Key Components in Cancer Therapies. Anticancer Agents Med. Chem.
Salarian, A., Kadkhodaee, M., Zahmatkesh, M., Seifi, B., Bakhshi, E., Akhondzadeh, S., et al. (2018). Opioid Use Disorder Induces Oxidative Stress and Inflammation: The Attenuating Effect of Methadone Maintenance Treatment. Iran. J. Psychiatry 13 (1), 46–54.
Salimi, A., Eybagi, S., Seydi, E., Naserzadeh, P., Kazerouni, N. P., and Pourahmad, J. (2016). Toxicity of Macrolide Antibiotics on Isolated Heart Mitochondria: a Justification for Their Cardiotoxic Adverse Effect. Xenobiotica 46 (1), 82–93. doi:10.3109/00498254.2015.1046975
Salminen, A., and Kaarniranta, K. (2012). AMP-activated Protein Kinase (AMPK) Controls the Aging Process via an Integrated Signaling Network. Ageing Res. Rev. 11 (2), 230–241. doi:10.1016/j.arr.2011.12.005
Salvemini, D., Little, J. W., Doyle, T., and Neumann, W. L. (2011). Roles of Reactive Oxygen and Nitrogen Species in Pain. Free Radic. Biol. Med. 51 (5), 951–966. doi:10.1016/j.freeradbiomed.2011.01.026
Sambe, T., Mason, R. P., Dawoud, H., Bhatt, D. L., and Malinski, T. (2018). Metformin Treatment Decreases Nitroxidative Stress, Restores Nitric Oxide Bioavailability and Endothelial Function beyond Glucose Control. Biomed. Pharmacother. 98, 149–156. doi:10.1016/j.biopha.2017.12.023
Sandyk, R. (1993). The Relationship between Diabetes Mellitus and Parkinson's Disease. Int. J. Neurosci. 69 (1-4), 125–130. doi:10.3109/00207459309003322
Santiago, J. A., and Potashkin, J. A. (2013). Integrative Network Analysis Unveils Convergent Molecular Pathways in Parkinson's Disease and Diabetes. PLoS One 8 (12), e83940. doi:10.1371/journal.pone.0083940
Scarpello, J. H., and Howlett, H. C. (2008). Metformin Therapy and Clinical Uses. Diabetes Vasc. Dis. Res. 5 (3), 157–167. doi:10.3132/dvdr.2008.027
Schaefer, A. M., McFarland, R., Blakely, E. L., He, L., Whittaker, R. G., Taylor, R. W., et al. (2008). Prevalence of Mitochondrial DNA Disease in Adults. Ann. Neurol. 63 (1), 35–39. doi:10.1002/ana.21217
Schapira, A. H. V., Cooper, J. M., Dexter, D., Clark, J. B., Jenner, P., and Marsden, C. D. (1990). Mitochondrial Complex I Deficiency in Parkinson's Disease. J. Neurochem. 54 (3), 823–827. doi:10.1111/j.1471-4159.1990.tb02325.x
Schiavone, S., Neri, M., and Harvey, B. H. (2019). Pathological Consequences of Drug Abuse: Implication of Redox Imbalance. Oxid. Med. Cell Longev. 2019, 4780852. doi:10.1155/2019/4780852
Schildknecht, S., Daiber, A., Ghisla, S., Cohen, R. A., and Bachschmid, M. M. (2008). Acetaminophen Inhibits Prostanoid Synthesis by Scavenging the PGHS‐activator Peroxynitrite. FASEB J. 22 (1), 215–224. doi:10.1096/fj.06-8015com
Schon, E. A., and Przedborski, S. (2011). Mitochondria: the Next (Neurode)generation. Neuron 70 (6), 1033–1053. doi:10.1016/j.neuron.2011.06.003
Schriner, S. E., Linford, N. J., Martin, G. M., Treuting, P., Ogburn, C. E., Emond, M., et al. (2005). Extension of Murine Life Span by Overexpression of Catalase Targeted to Mitochondria. Science 308 (5730), 1909–1911. doi:10.1126/science.1106653
Schulz, T. J., Zarse, K., Voigt, A., Urban, N., Birringer, M., and Ristow, M. (2007). Glucose Restriction Extends Caenorhabditis elegans Life Span by Inducing Mitochondrial Respiration and Increasing Oxidative Stress. Cell Metab. 6 (4), 280–293. doi:10.1016/j.cmet.2007.08.011
Schulzer, M., Mak, E., and Calne, D. B. (1992). The Antiparkinson Efficacy of Deprenyl Derives from Transient Improvement that Is Likely to Be Symptomatic. Ann. Neurol. 32 (6), 795–798. doi:10.1002/ana.410320614
Segawa, M., Nomura, Y., and Nishiyama, N. (2003). Autosomal Dominant Guanosine Triphosphate Cyclohydrolase I Deficiency (Segawa Disease). Ann. Neurol. 54 (Suppl. 6), S32–S45. doi:10.1002/ana.10630
Selkoe, D. J. (2002). Alzheimer's Disease Is a Synaptic Failure. Science 298 (5594), 789–791. doi:10.1126/science.1074069
Sell, H., Blüher, M., Klöting, N., Schlich, R., Willems, M., Ruppe, F., et al. (2013). Adipose Dipeptidyl Peptidase-4 and Obesity. Diabetes Care 36 (12), 4083–4090. doi:10.2337/dc13-0496
Semancik, J. S., and Vanderwoude, W. J. (1976). Exocortis Viroid: Cytopathic Effects at the Plasma Membrane in Association with Pathogenic RNA. Virology 69 (2), 719–726. doi:10.1016/0042-6822(76)90500-6
Sergi, D., Renaud, J., Simola, N., and Martinoli, M.-G. (2019). Diabetes, a Contemporary Risk for Parkinson's Disease: Epidemiological and Cellular Evidences. Front. Aging Neurosci. 11, 302. doi:10.3389/fnagi.2019.00302
Serhan, C. N., and Chiang, N. (2013). Resolution Phase Lipid Mediators of Inflammation: Agonists of Resolution. Curr. Opin. Pharmacol. 13 (4), 632–640. doi:10.1016/j.coph.2013.05.012
Sharma, C., Long, J. H., Shah, S., Rahman, J., Perrett, D., Ayoub, S., et al. (2017). First Evidence of the Conversion of Paracetamol to AM404 in Human Cerebrospinal Fluid. Jpr 10, 2703–2709. doi:10.2147/jpr.s143500
Sharma, S., Bhattarai, S., Ara, H., Sun, G., St Clair, D. K., Bhuiyan, M. S., et al. (2020). SOD2 Deficiency in Cardiomyocytes Defines Defective Mitochondrial Bioenergetics as a Cause of Lethal Dilated Cardiomyopathy. Redox Biol. 37, 101740. doi:10.1016/j.redox.2020.101740
Sheldon, R. A., Jiang, X., Francisco, C., Christen, S., Vexler, Z. S., Täuber, M. G., et al. (2004). Manipulation of Antioxidant Pathways in Neonatal Murine Brain. Pediatr. Res. 56 (4), 656–662. doi:10.1203/01.pdr.0000139413.27864.50
Sheveleva, E. V., Landowski, T. H., Samulitis, B. K., Bartholomeusz, G., Powis, G., and Dorr, R. T. (2012). Imexon Induces an Oxidative Endoplasmic Reticulum Stress Response in Pancreatic Cancer Cells. Mol. Cancer Res. 10 (3), 392–400. doi:10.1158/1541-7786.mcr-11-0359
Shi, Y., Lo, C.-S., Chenier, I., Maachi, H., Filep, J. G., Ingelfinger, J. R., et al. (2013). Overexpression of Catalase Prevents Hypertension and Tubulointerstitial Fibrosis and Normalization of Renal Angiotensin-Converting Enzyme-2 Expression in Akita Mice. Am. J. Physiology-Renal Physiology 304 (11), F1335–F1346. doi:10.1152/ajprenal.00405.2012
Shi, Y., and Vanhoutte, P. M. (2017). Macro- and Microvascular Endothelial Dysfunction in Diabetes. J. Diabetes 9 (5), 434–449. doi:10.1111/1753-0407.12521
Shields, H. J., Traa, A., and Van Raamsdonk, J. M. (2021). Beneficial and Detrimental Effects of Reactive Oxygen Species on Lifespan: A Comprehensive Review of Comparative and Experimental Studies. Front. Cell Dev. Biol. 9, 628157. doi:10.3389/fcell.2021.628157
Shih, N.-L., Cheng, T.-H., Loh, S.-H., Cheng, P.-Y., Wang, D. L., Chen, Y.-S., et al. (2001). Reactive Oxygen Species Modulate Angiotensin II-Induced β-Myosin Heavy Chain Gene Expression via Ras/Raf/Extracellular Signal-Regulated Kinase Pathway in Neonatal Rat Cardiomyocytes. Biochem. Biophysical Res. Commun. 283 (1), 143–148. doi:10.1006/bbrc.2001.4744
Shim, W. S., and Oh, U. (2008). Histamine-induced Itch and its Relationship with Pain. Mol. Pain 4, 29. doi:10.1186/1744-8069-4-29
Shimada, K., Crother, T. R., Karlin, J., Dagvadorj, J., Chiba, N., Chen, S., et al. (2012). Oxidized Mitochondrial DNA Activates the NLRP3 Inflammasome during Apoptosis. Immunity 36 (3), 401–414. doi:10.1016/j.immuni.2012.01.009
Shin, H.-S., Ko, J., Kim, D.-A., Ryu, E.-S., Ryu, H.-M., Park, S.-H., et al. (2017). Metformin Ameliorates the Phenotype Transition of Peritoneal Mesothelial Cells and Peritoneal Fibrosis via a Modulation of Oxidative Stress. Sci. Rep. 7 (1), 5690. doi:10.1038/s41598-017-05836-6
Shin, S. J., Chung, S., Kim, S. J., Lee, E.-M., Yoo, Y.-H., Kim, J.-W., et al. (2016). Effect of Sodium-Glucose Co-transporter 2 Inhibitor, Dapagliflozin, on Renal Renin-Angiotensin System in an Animal Model of Type 2 Diabetes. PLoS One 11 (11), e0165703. doi:10.1371/journal.pone.0165703
Shoulson, I. (1992). An Interim Report of the Effect of Selegiline (L-Deprenyl) on the Progression of Disability in Early Parkinson's Disease. The Parkinson Study Group. Eur. Neurol. 32 (Suppl. 1), 46–53. doi:10.1159/000116869
Simeonova, R., Vitcheva, V., Kondeva-Burdina, M., Krasteva, I., Manov, V., and Mitcheva, M. (2013). Hepatoprotective and Antioxidant Effects of Saponarin, Isolated from Gypsophila Trichotoma Wend. On Paracetamol-Induced Liver Damage in Rats. Biomed. Res. Int. 2013, 757126. doi:10.1155/2013/757126
Simpson, I. A., Chundu, K. R., Davies-Hill, T., Honer, W. G., and Davies, P. (1994). Decreased Concentrations of GLUT1 and GLUT3 Glucose Transporters in the Brains of Patients with Alzheimer's Disease. Ann. Neurol. 35 (5), 546–551. doi:10.1002/ana.410350507
Singh, B. N., Shankar, S., and Srivastava, R. K. (2011). Green Tea Catechin, Epigallocatechin-3-Gallate (EGCG): Mechanisms, Perspectives and Clinical Applications. Biochem. Pharmacol. 82 (12), 1807–1821. doi:10.1016/j.bcp.2011.07.093
Sirvent, P., Bordenave, S., Vermaelen, M., Roels, B., Vassort, G., Mercier, J., et al. (2005). Simvastatin Induces Impairment in Skeletal Muscle while Heart Is Protected. Biochem. Biophysical Res. Commun. 338 (3), 1426–1434. doi:10.1016/j.bbrc.2005.10.108
Smieszek, A., Strek, Z., Kornicka, K., Grzesiak, J., Weiss, C., and Marycz, K. (2017). Antioxidant and Anti-senescence Effect of Metformin on Mouse Olfactory Ensheathing Cells (mOECs) May Be Associated with Increased Brain-Derived Neurotrophic Factor Levels-An Ex Vivo Study. Int. J. Mol. Sci. 18 (4).
Smith, M. A., Richey Harris, P. L., Sayre, L. M., Beckman, J. S., and Perry, G. (1997). Widespread Peroxynitrite-Mediated Damage in Alzheimer's Disease. J. Neurosci. 17 (8), 2653–2657. doi:10.1523/jneurosci.17-08-02653.1997
Somarelli, J. A., Gardner, H., Cannataro, V. L., Gunady, E. F., Boddy, A. M., Johnson, N. A., et al. (2020). Molecular Biology and Evolution of Cancer: From Discovery to Action. Mol. Biol. Evol. 37 (2), 320–326. doi:10.1093/molbev/msz242
Son, A., Nakamura, H., Kondo, N., Matsuo, Y., Liu, W., Oka, S.-i., et al. (2006). Redox Regulation of Mast Cell Histamine Release in Thioredoxin-1 (TRX) Transgenic Mice. Cell Res. 16 (2), 230–239. doi:10.1038/sj.cr.7310031
Sorce, S., and Krause, K.-H. (2009). NOX Enzymes in the Central Nervous System: from Signaling to Disease. Antioxidants Redox Signal. 11 (10), 2481–2504. doi:10.1089/ars.2009.2578
Soukas, A. A., Hao, H., and Wu, L. (2019). Metformin as Anti-aging Therapy: Is it for Everyone? Trends Endocrinol. Metabolism 30 (10), 745–755. doi:10.1016/j.tem.2019.07.015
Spencer, N. Y., and Engelhardt, J. F. (2014). The Basic Biology of Redoxosomes in Cytokine-Mediated Signal Transduction and Implications for Disease-specific Therapies. Biochemistry 53 (10), 1551–1564. doi:10.1021/bi401719r
Spillantini, M. G., Schmidt, M. L., Lee, V. M.-Y., Trojanowski, J. Q., Jakes, R., and Goedert, M. (1997). α-Synuclein in Lewy Bodies. Nature 388 (6645), 839–840. doi:10.1038/42166
Srinivasan, A. (2019). Propranolol: A 50-Year Historical Perspective. Ann. Indian Acad. Neurol. 22 (1), 21–26. doi:10.4103/aian.aian_201_18
Stadtman, E. R. (1990). Metal Ion-Catalyzed Oxidation of Proteins: Biochemical Mechanism and Biological Consequences. Free Radic. Biol. Med. 9 (4), 315–325. doi:10.1016/0891-5849(90)90006-5
Stansley, B. J., and Yamamoto, B. K. (2013). L-dopa-induced Dopamine Synthesis and Oxidative Stress in Serotonergic Cells. Neuropharmacology 67, 243–251. doi:10.1016/j.neuropharm.2012.11.010
Steiner, M., Glantz, M., and Lekos, A. (1995). Vitamin E Plus Aspirin Compared with Aspirin Alone in Patients with Transient Ischemic Attacks. Am. J. Clin. Nutr. 62 (6 Suppl. l), 1381S–1384S. doi:10.1093/ajcn/62.6.1381S
Steven, S., Münzel, T., and Daiber, A. (2015). Exploiting the Pleiotropic Antioxidant Effects of Established Drugs in Cardiovascular Disease. Ijms 16 (8), 18185–18223. doi:10.3390/ijms160818185
Steven, S., Oelze, M., Hanf, A., Kröller-Schön, S., Kashani, F., Roohani, S., et al. (2017). The SGLT2 Inhibitor Empagliflozin Improves the Primary Diabetic Complications in ZDF Rats. Redox Biol. 13, 370–385. doi:10.1016/j.redox.2017.06.009
Stirpe, F., Della Corte, E., and Lorenzoni, E. (1969). The Regulation of Rat Liver Xanthine Oxidase. J. Biol. Chem. 244 (14), 3855–3863. doi:10.1016/s0021-9258(17)36428-1
Stocchi, F., Vacca, L., Grassini, P., De Pandis, M. F., Battaglia, G., Cattaneo, C., et al. (2006). Symptom Relief in Parkinson Disease by Safinamide: Biochemical and Clinical Evidence of Efficacy beyond MAO-B Inhibition. Neurology 67 (7 Suppl. 2), S24–S29. doi:10.1212/wnl.67.7_suppl_2.s24
Su, Y., Duan, J., Ying, Z., Hou, Y., Zhang, Y., Wang, R., et al. (2013). Increased Vulnerability of Parkin Knock Down PC12 Cells to Hydrogen Peroxide Toxicity: the Role of Salsolinol and NM-salsolinol. Neuroscience 233, 72–85. doi:10.1016/j.neuroscience.2012.12.045
Suárez-Rivero, J. M., Pastor-Maldonado, C. J., Povea-Cabello, S., Álvarez-Córdoba, M., Villalón-García, I., Talaverón-Rey, M., et al. (2021). Mitochondria and Antibiotics: For Good or for Evil? Biomolecules 11 (7). doi:10.3390/biom11071050
Sub Laban, T., and Saadabadi, A. (2021). Monoamine Oxidase Inhibitors (MAOI). Island FL: StatPearls. Treasure.
Subramaniam, S. R., Vergnes, L., Franich, N. R., Reue, K., and Chesselet, M.-F. (2014). Region Specific Mitochondrial Impairment in Mice with Widespread Overexpression of Alpha-Synuclein. Neurobiol. Dis. 70, 204–213. doi:10.1016/j.nbd.2014.06.017
Sugawara, T., Lewén, A., Gasche, Y., Yu, F., and Chan, P. H. (2002). Overexpression of SOD1 Protects Vulnerable Motor Neurons after Spinal Cord Injury by Attenuating Mitochondrial Cytochrome C Release. FASEB J. 16 (14), 1997–1999. doi:10.1096/fj.02-0251fje
Sugizaki, T., Zhu, S., Guo, G., Matsumoto, A., Zhao, J., Endo, M., et al. (2017). Treatment of Diabetic Mice with the SGLT2 Inhibitor TA-1887 Antagonizes Diabetic Cachexia and Decreases Mortality. NPJ Aging Mech. Dis. 3, 12. doi:10.1038/s41514-017-0012-0
Suh, J. H. H., Heath, T. M., and Hagen, T. M. (2003). Two Subpopulations of Mitochondria in the Aging Rat Heart Display Heterogenous Levels of Oxidative Stress. Free Radic. Biol. Med. 35 (9), 1064–1072. doi:10.1016/s0891-5849(03)00468-4
Sun, J., Druhan, L. J., and Zweier, J. L. (2010). Reactive Oxygen and Nitrogen Species Regulate Inducible Nitric Oxide Synthase Function Shifting the Balance of Nitric Oxide and Superoxide Production. Archives Biochem. Biophysics 494 (2), 130–137. doi:10.1016/j.abb.2009.11.019
Suwa, M., Egashira, T., Nakano, H., Sasaki, H., and Kumagai, S. (2006). Metformin Increases the PGC-1alpha Protein and Oxidative Enzyme Activities Possibly via AMPK Phosphorylation in Skeletal Muscle In Vivo. J. Appl. Physiol. (1985) 101 (6), 1685–1692. doi:10.1152/japplphysiol.00255.2006
Suzuki, M., Kotake, K., Fujikura, K., Inagaki, N., Suzuki, T., Gonoi, T., et al. (1997). Kir6.1: A Possible Subunit of ATP-Sensitive K+Channels in Mitochondria. Biochem. Biophysical Res. Commun. 241 (3), 693–697. doi:10.1006/bbrc.1997.7891
Swerdlow, R. H., Burns, J. M., and Khan, S. M. (2010). The Alzheimer's Disease Mitochondrial Cascade Hypothesis. J. Alzheimers Dis. 20 (Suppl. 2), S265–S279. doi:10.3233/JAD-2010-100339
Swerdlow, R. H., and Khan, S. M. (2004). A "mitochondrial Cascade Hypothesis" for Sporadic Alzheimer's Disease. Med. Hypotheses 63 (1), 8–20. doi:10.1016/j.mehy.2003.12.045
Szewczyk, A., Wójcik, G., Lobanov, N. A., and Nałecz, M. J. (1997). The Mitochondrial Sulfonylurea Receptor: Identification and Characterization. Biochem. Biophysical Res. Commun. 230 (3), 611–615. doi:10.1006/bbrc.1996.6023
Tabassum, A., Bristow, R. G., and Venkateswaran, V. (2010). Ingestion of Selenium and Other Antioxidants during Prostate Cancer Radiotherapy: a Good Thing? Cancer Treat. Rev. 36 (3), 230–234. doi:10.1016/j.ctrv.2009.12.008
Takada, S., Masaki, Y., Kinugawa, S., Matsumoto, J., Furihata, T., Mizushima, W., et al. (2016). Dipeptidyl Peptidase-4 Inhibitor Improved Exercise Capacity and Mitochondrial Biogenesis in Mice with Heart Failure via Activation of Glucagon-like Peptide-1 Receptor Signalling. Cardiovasc Res. 111 (4), 338–347. doi:10.1093/cvr/cvw182
Talbot, K., Wang, H.-Y., Kazi, H., Han, L.-Y., Bakshi, K. P., Stucky, A., et al. (2012). Demonstrated Brain Insulin Resistance in Alzheimer's Disease Patients Is Associated with IGF-1 Resistance, IRS-1 Dysregulation, and Cognitive Decline. J. Clin. Invest. 122 (4), 1316–1338. doi:10.1172/jci59903
Tampellini, D., and Gouras, G. K. (2010). Synapses, Synaptic Activity and Intraneuronal Abeta in Alzheimer's Disease. Front. Aging Neurosci. 2. doi:10.3389/fnagi.2010.00013
Tang, G., Yang, H., Chen, J., Shi, M., Ge, L., Ge, X., et al. (2017). Metformin Ameliorates Sepsis-Induced Brain Injury by Inhibiting Apoptosis, Oxidative Stress and Neuroinflammation via the PI3K/Akt Signaling Pathway. Oncotarget 8 (58), 97977–97989. doi:10.18632/oncotarget.20105
Tapryal, N., Vivek G, V., and Mukhopadhyay, C. K. (2015). Catecholamine Stress Hormones Regulate Cellular Iron Homeostasis by a Posttranscriptional Mechanism Mediated by Iron Regulatory Protein. J. Biol. Chem. 290 (12), 7634–7646. doi:10.1074/jbc.m114.592519
Tejero, J., Shiva, S., and Gladwin, M. T. (2019). Sources of Vascular Nitric Oxide and Reactive Oxygen Species and Their Regulation. Physiol. Rev. 99 (1), 311–379. doi:10.1152/physrev.00036.2017
Teramoto, S., Suzuki, M., Matsuse, T., Ishii, T., Fukuchi, Y., and Ouchi, Y. (2000). Effects of Angiotensin-Converting Enzyme Inhibitors on Spontaneous or Stimulated Generation of Reactive Oxygen Species by Bronchoalveolar Lavage Cells Harvested from Patients with or without Chronic Obstructive Pulmonary Disease. Jpn. J. Pharmacol. 83 (1), 56–62. doi:10.1016/s0021-5198(19)30627-4
Terasaki, M., Yashima, H., Mori, Y., Saito, T., Matsui, T., Hiromura, M., et al. (2020). A Dipeptidyl Peptidase-4 Inhibitor Inhibits Foam Cell Formation of Macrophages in Type 1 Diabetes via Suppression of CD36 and ACAT-1 Expression. Int. J. Mol. Sci. 21 (13). doi:10.3390/ijms21134811
Tipton, K. F. (2018). 90 Years of Monoamine Oxidase: Some Progress and Some Confusion. J. Neural Transm. 125 (11), 1519–1551. doi:10.1007/s00702-018-1881-5
Toyoda, S., Haruyama, A., Inami, S., Arikawa, T., Saito, F., Watanabe, R., et al. (2020). Effects of Carvedilol vs Bisoprolol on Inflammation and Oxidative Stress in Patients with Chronic Heart Failure. J. Cardiol. 75 (2), 140–147. doi:10.1016/j.jjcc.2019.07.011
Trachootham, D., Alexandre, J., and Huang, P. (2009). Targeting Cancer Cells by ROS-Mediated Mechanisms: a Radical Therapeutic Approach? Nat. Rev. Drug Discov. 8 (7), 579–591. doi:10.1038/nrd2803
Tremblay, A. J., Lamarche, B., Deacon, C. F., Weisnagel, S. J., and Couture, P. (2014). Effects of Sitagliptin Therapy on Markers of Low-Grade Inflammation and Cell Adhesion Molecules in Patients with Type 2 Diabetes. Metabolism 63 (9), 1141–1148. doi:10.1016/j.metabol.2014.06.004
Treuting, P. M., Linford, N. J., Knoblaugh, S. E., Emond, M. J., Morton, J. F., Martin, G. M., et al. (2008). Reduction of Age-Associated Pathology in Old Mice by Overexpression of Catalase in Mitochondria. Journals Gerontology Ser. A Biol. Sci. Med. Sci. 63 (8), 813–822. doi:10.1093/gerona/63.8.813
Tse, D. C. S., McCreery, R. L., and Adams, R. N. (1976). Potential Oxidative Pathways of Brain Catecholamines. J. Med. Chem. 19 (1), 37–40. doi:10.1021/jm00223a008
Tsoucalas, G., Karamanou, M., and Androutsos, G. (2011). Travelling through Time with Aspirin, a Healing Companion. Eur. J. Inflamm. 9 (1), 13–16. doi:10.1177/1721727x1100900102
Ullah, I., Ullah, N., Naseer, M. I., Lee, H. Y., and Kim, M. O. (2012). Neuroprotection with Metformin and Thymoquinone against Ethanol-Induced Apoptotic Neurodegeneration in Prenatal Rat Cortical Neurons. BMC Neurosci. 13, 11. doi:10.1186/1471-2202-13-11
Ursini, F., Russo, E., Pellino, G., D’Angelo, S., Chiaravalloti, A., De Sarro, G., et al. (2018). Metformin and Autoimmunity: A "New Deal" of an Old Drug. Front. Immunol. 9, 1236. doi:10.3389/fimmu.2018.01236
Valencia, W. M., Palacio, A., Tamariz, L., and Florez, H. (2017). Metformin and Ageing: Improving Ageing Outcomes beyond Glycaemic Control. Diabetologia 60 (9), 1630–1638. doi:10.1007/s00125-017-4349-5
Valente, E. M., Abou-Sleiman, P. M., Caputo, V., Muqit, M. M. K., Harvey, K., Gispert, S., et al. (2004). Hereditary Early-Onset Parkinson's Disease Caused by Mutations in PINK1. Science 304 (5674), 1158–1160. doi:10.1126/science.1096284
Vallon, V., and Thomson, S. C. (2017). Targeting Renal Glucose Reabsorption to Treat Hyperglycaemia: the Pleiotropic Effects of SGLT2 Inhibition. Diabetologia 60 (2), 215–225. doi:10.1007/s00125-016-4157-3
Van Acker, H., and Coenye, T. (2017). The Role of Reactive Oxygen Species in Antibiotic-Mediated Killing of Bacteria. Trends Microbiol. 25 (6), 456–466. doi:10.1016/j.tim.2016.12.008
Van Loenhout, J., Peeters, M., Bogaerts, A., Smits, E., and Deben, C. (2020). Oxidative Stress-Inducing Anticancer Therapies: Taking a Closer Look at Their Immunomodulating Effects. Antioxidants (Basel) 9 (12). doi:10.3390/antiox9121188
Vázquez-Meza, H., de Piña, M., Pardo, J., Riveros-Rosas, H., Villalobos-Molina, R., and Piña, E. (2013). Non-steroidal Anti-inflammatory Drugs Activate NADPH Oxidase in Adipocytes and Raise the H2O2 Pool to Prevent cAMP-Stimulated Protein Kinase a Activation and Inhibit Lipolysis. BMC Biochem. 14, 13. doi:10.1186/1471-2091-14-13
Venderova, K., and Park, D. S. (2012). Programmed Cell Death in Parkinson's Disease. Cold Spring Harb. Perspect. Med. 2 (8). doi:10.1101/cshperspect.a009365
Vendrov, A. E., Stevenson, M. D., Alahari, S., Pan, H., Wickline, S. A., Madamanchi, N. R., et al. (2017). Attenuated Superoxide Dismutase 2 Activity Induces Atherosclerotic Plaque Instability during Aging in Hyperlipidemic Mice. J. Am. Heart Assoc. 6 (11). doi:10.1161/JAHA.117.006775
Venkateshappa, C., Harish, G., Mythri, R. B., Mahadevan, A., Srinivas Bharath, M. M., and Shankar, S. K. (2012). Increased Oxidative Damage and Decreased Antioxidant Function in Aging Human Substantia Nigra Compared to Striatum: Implications for Parkinson's Disease. Neurochem. Res. 37 (2), 358–369. doi:10.1007/s11064-011-0619-7
Verdile, G., Keane, K. N., Cruzat, V. F., Medic, S., Sabale, M., Rowles, J., et al. (2015). Inflammation and Oxidative Stress: The Molecular Connectivity between Insulin Resistance, Obesity, and Alzheimer's Disease. Mediat. Inflamm. 2015, 105828. doi:10.1155/2015/105828
Vermot, A., Petit-Härtlein, I., Smith, S. M. E., and Fieschi, F. (2021). NADPH Oxidases (NOX): An Overview from Discovery, Molecular Mechanisms to Physiology and Pathology. Antioxidants (Basel) 10 (6). doi:10.3390/antiox10060890
Vickers, S., Schiller, H. J., Hildreth, J. E. K., and Bulkley, G. B. (1998). Immunoaffinity Localization of the Enzyme Xanthine Oxidase on the outside Surface of the Endothelial Cell Plasma Membrane. Surgery 124 (3), 551–560. doi:10.1016/s0039-6060(98)70102-3
Wahlqvist, M. L., Lee, M.-S., Hsu, C.-C., Chuang, S.-Y., Lee, J.-T., and Tsai, H.-N. (2012). Metformin-inclusive Sulfonylurea Therapy Reduces the Risk of Parkinson's Disease Occurring with Type 2 Diabetes in a Taiwanese Population Cohort. Park. Relat. Disord. 18 (6), 753–758. doi:10.1016/j.parkreldis.2012.03.010
Wallace, T. M., and Matthews, D. R. (2004). Recent Advances in the Monitoring and Management of Diabetic Ketoacidosis. QJM 97 (12), 773–780. doi:10.1093/qjmed/hch132
Walsh, D. M., and Selkoe, D. J. (2007). A? Oligomers ? a Decade of Discovery. J. Neurochem. 101 (5), 1172–1184. doi:10.1111/j.1471-4159.2006.04426.x
Wang, C., Chen, B., Feng, Q., Nie, C., and Li, T. (2020). Clinical Perspectives and Concerns of Metformin as an Anti‐aging Drug. Aging Med. 3 (4), 266–275. doi:10.1002/agm2.12135
Wang, J., and Wang, H. (2017). Oxidative Stress in Pancreatic Beta Cell Regeneration. Oxid. Med. Cell Longev. 2017, 1930261. doi:10.1155/2017/1930261
Wang, J., Xiong, S., Xie, C., Markesbery, W. R., and Lovell, M. A. (2005). Increased Oxidative Damage in Nuclear and Mitochondrial DNA in Alzheimer's Disease. J. Neurochem. 93 (4), 953–962. doi:10.1111/j.1471-4159.2005.03053.x
Wang, J., and Yi, J. (2008). Cancer Cell Killing via ROS: to Increase or Decrease, that Is the Question. Cancer Biol. Ther. 7 (12), 1875–1884. doi:10.4161/cbt.7.12.7067
Wang, P., Shi, Q., Deng, W. H., Yu, J., Zuo, T., Mei, F. C., et al. (2015). Relationship between Expression of NADPH Oxidase 2 and Invasion and Prognosis of Human Gastric Cancer. Wjg 21 (20), 6271–6279. doi:10.3748/wjg.v21.i20.6271
Wang, S., Ye, S. D., Sun, W. J., and Hu, Y. Y. (2013). Pioglitazone Inhibits the Expression of Nicotinamide Adenine Dinucleotide Phosphate Oxidase and P38 Mitogen-Activated Protein Kinase in Rat Mesangial Cells. Chin. Med. J. Engl. 126 (21), 4054–4059.
Wang, X., Perry, G., Smith, M. A., and Zhu, X. (2010). Amyloid-beta-derived Diffusible Ligands Cause Impaired Axonal Transport of Mitochondria in Neurons. Neurodegener. Dis. 7 (1-3), 56–59. doi:10.1159/000283484
Wang, X., Su, B., Fujioka, H., and Zhu, X. (2008). Dynamin-like Protein 1 Reduction Underlies Mitochondrial Morphology and Distribution Abnormalities in Fibroblasts from Sporadic Alzheimer's Disease Patients. Am. J. Pathology 173 (2), 470–482. doi:10.2353/ajpath.2008.071208
Wang, X., Wu, Q., Liu, A., Anadón, A., Rodríguez, J.-L., Martínez-Larrañaga, M.-R., et al. (2017). Paracetamol: Overdose-Induced Oxidative Stress Toxicity, Metabolism, and Protective Effects of Various Compoundsin Vivo and In Vitro. Drug Metab. Rev. 49 (4), 395–437. doi:10.1080/03602532.2017.1354014
Wang, X., Zhao, X., Malik, M., and Drlica, K. (2010). Contribution of Reactive Oxygen Species to Pathways of Quinolone-Mediated Bacterial Cell Death. J. Antimicrob. Chemother. 65 (3), 520–524. doi:10.1093/jac/dkp486
Wang, Y. L., Frauwirth, K. A., Rangwala, S. M., Lazar, M. A., and Thompson, C. B. (2002). Thiazolidinedione Activation of Peroxisome Proliferator-Activated Receptor γ Can Enhance Mitochondrial Potential and Promote Cell Survival. J. Biol. Chem. 277 (35), 31781–31788. doi:10.1074/jbc.m204279200
Warwick, C. (2008). Paracetamol and Fever Management. J. R. Soc. Promot. Health 128 (6), 320–323. doi:10.1177/1466424008092794
Wasan, H., Singh, D., and Kh, R. (2021). Safinamide in Neurological Disorders and beyond: Evidence from Preclinical and Clinical Studies. Brain Res. Bull. 168, 165–177. doi:10.1016/j.brainresbull.2020.12.018
Watanabe, R., Nakamura, H., Masutani, H., and Yodoi, J. (2010). Anti-oxidative, Anti-cancer and Anti-inflammatory Actions by Thioredoxin 1 and Thioredoxin-Binding Protein-2. Pharmacol. Ther. 127 (3), 261–270. doi:10.1016/j.pharmthera.2010.04.004
Weiner, D. B. (1979). The Apprenticeship of Philippe Pinel: a New Document, "observations of Citizen Pussin on the Insane". Am. J. Psychiatry 136 (9), 1128–1134. doi:10.1176/ajp.136.9.1128
Weisbrot-Lefkowitz, M., Reuhl, K., Perry, B., Chan, P. H., Inouye, M., and Mirochnitchenko, O. (1998). Overexpression of Human Glutathione Peroxidase Protects Transgenic Mice against Focal Cerebral Ischemia/reperfusion Damage. Brain Res. Mol. Brain Res. 53 (1-2), 333–338. doi:10.1016/s0169-328x(97)00313-6
Weisiger, R. A., and Fridovich, I. (1973). Mitochondrial Superoxide Dismutase. J. Biol. Chem. 248 (13), 4793–4796. doi:10.1016/s0021-9258(19)43735-6
West, A. P., Shadel, G. S., and Ghosh, S. (2011). Mitochondria in Innate Immune Responses. Nat. Rev. Immunol. 11 (6), 389–402. doi:10.1038/nri2975
Weylandt, K.-H. (2016). Docosapentaenoic Acid Derived Metabolites and Mediators - the New World of Lipid Mediator Medicine in a Nutshell. Eur. J. Pharmacol. 785, 108–115. doi:10.1016/j.ejphar.2015.11.002
Wigner, P., Szymańska, B., Bijak, M., Sawicka, E., Kowal, P., Marchewka, Z., et al. (2021). Oxidative Stress Parameters as Biomarkers of Bladder Cancer Development and Progression. Sci. Rep. 11 (1), 15134. doi:10.1038/s41598-021-94729-w
Wilding, J. P., Woo, V., Rohwedder, K., Sugg, J., Parikh, S., and Dapagliflozin, D. S. G. (0062). Dapagliflozin in Patients with Type 2 Diabetes Receiving High Doses of Insulin: Efficacy and Safety over 2 Years. Diabetes Obes. Metab. 16 (2), 124–136. doi:10.1111/dom.12187
Willette, A. A., Modanlo, N., Kapogiannis, D., and Alzheimer's Disease Neuroimaging, I. (2015). Insulin Resistance Predicts Medial Temporal Hypermetabolism in Mild Cognitive Impairment Conversion to Alzheimer Disease. Diabetes 64 (6), 1933–1940. doi:10.2337/db14-1507
Wood, Z. A., Schröder, E., Robin Harris, J., and Poole, L. B. (2003). Structure, Mechanism and Regulation of Peroxiredoxins. Trends Biochem. Sci. 28 (1), 32–40. doi:10.1016/s0968-0004(02)00003-8
Wu, Y., Vulić, M., Keren, I., and Lewis, K. (2012). Role of Oxidative Stress in Persister Tolerance. Antimicrob. Agents Chemother. 56 (9), 4922–4926. doi:10.1128/aac.00921-12
Wyss-Coray, T. (2006). Inflammation in Alzheimer Disease: Driving Force, Bystander or Beneficial Response? Nat. Med. 12 (9), 1005–1015. doi:10.1038/nm1484
Xiao, Y., Xiong, T., Meng, X., Yu, D., Xiao, Z., and Song, L. (2019). Different Influences on Mitochondrial Function, Oxidative Stress and Cytotoxicity of Antibiotics on Primary Human Neuron and Cell Lines. J. Biochem. Mol. Toxicol. 33 (4), e22277. doi:10.1002/jbt.22277
Xu, P., Huecksteadt, T. P., and Hoidal, J. R. (1996). Molecular Cloning and Characterization of the Human Xanthine Dehydrogenase Gene (XDH). Genomics 34 (2), 173–180. doi:10.1006/geno.1996.0262
Yamada, M., Iwatsubo, T., Mizuno, Y., and Mochizuki, H. (2004). Overexpression of Alpha-Synuclein in Rat Substantia Nigra Results in Loss of Dopaminergic Neurons, Phosphorylation of Alpha-Synuclein and Activation of Caspase-9: Resemblance to Pathogenetic Changes in Parkinson's Disease. J. Neurochem. 91 (2), 451–461. doi:10.1111/j.1471-4159.2004.02728.x
Yamagishi, S.-i., Fukami, K., and Matsui, T. (2015). Crosstalk between Advanced Glycation End Products (AGEs)-Receptor RAGE axis and Dipeptidyl Peptidase-4-Incretin System in Diabetic Vascular Complications. Cardiovasc Diabetol. 14, 2. doi:10.1186/s12933-015-0176-5
Yancik, R. (2005). Population Aging and Cancer. Cancer J. 11 (6), 437–441. doi:10.1097/00130404-200511000-00002
Yang, D., Elner, S. G., Bian, Z.-M., Till, G. O., Petty, H. R., and Elner, V. M. (2007). Pro-inflammatory Cytokines Increase Reactive Oxygen Species through Mitochondria and NADPH Oxidase in Cultured RPE Cells. Exp. Eye Res. 85 (4), 462–472. doi:10.1016/j.exer.2007.06.013
Yang, H., Shi, M., VanRemmen, H., Chen, X., Vijg, J., Richardson, A., et al. (2003). Reduction of Pressor Response to Vasoconstrictor Agents by Overexpression of Catalase in Mice. Am. J. Hypertens. 16 (1), 1–5. doi:10.1016/s0895-7061(02)03086-8
Yang, H., Zhou, L., Wang, Z., Roberts, L. J., Lin, X., Zhao, Y., et al. (2009). Overexpression of Antioxidant Enzymes in ApoE-Deficient Mice Suppresses Benzo(a)pyrene-Accelerated Atherosclerosis. Atherosclerosis 207 (1), 51–58. doi:10.1016/j.atherosclerosis.2009.03.052
Yang, Y., Wang, H., Kouadir, M., Song, H., and Shi, F. (2019). Recent Advances in the Mechanisms of NLRP3 Inflammasome Activation and its Inhibitors. Cell Death Dis. 10 (2), 128. doi:10.1038/s41419-019-1413-8
Yoshida, J., Yamamoto, K., Mano, T., Sakata, Y., Nishikawa, N., Nishio, M., et al. (2004). AT1 Receptor Blocker Added to ACE Inhibitor Provides Benefits at Advanced Stage of Hypertensive Diastolic Heart Failure. Hypertension 43 (3), 686–691. doi:10.1161/01.hyp.0000118017.02160.fa
Yoshida, T., Maulik, N., Engelman, R. M., Ho, Y. S., Magnenat, J. L., Rousou, J. A., et al. (1997). Glutathione Peroxidase Knockout Mice Are Susceptible to Myocardial Ischemia Reperfusion Injury. Circulation 96 (9 Suppl. l), II–21620.
You, X., Ma, M., Hou, G., Hu, Y., and Shi, X. (2018). Gene Expression and Prognosis of NOX Family Members in Gastric Cancer. Ott 11, 3065–3074. doi:10.2147/ott.s161287
Yu, F., Sugawara, T., Nishi, T., Liu, J., and Chan, P. H. (2006). Overexpression of SOD1 in Transgenic Rats Attenuates Nuclear Translocation of Endonuclease G and Apoptosis after Spinal Cord Injury. J. Neurotrauma 23 (5), 595–603. doi:10.1089/neu.2006.23.595
Yu, Y., Jiang, H., Niu, Y., Zhang, X., Zhang, Y., Liu, X. I., et al. (2019). Candesartan Inhibits Inflammation through an Angiotensin II Type 1 Receptor Independent Way in Human Embryonic Kidney Epithelial Cells. Acad Bras Cienc 91 (2), e20180699. doi:10.1590/0001-3765201920180699
Zahmatkesh, M., Kadkhodaee, M., Salarian, A., Seifi, B., and Adeli, S. (2017). Impact of Opioids on Oxidative Status and Related Signaling Pathways: An Integrated View. J Opioid Manag. 13 (4), 241–251. doi:10.5055/jom.2017.0392
Zeller, M., Steg, P. G., Ravisy, J., Lorgis, L., Laurent, Y., Sicard, P., et al. (2008). Relation between Body Mass Index, Waist Circumference, and Death after Acute Myocardial Infarction. Circulation 118 (5), 482–490. doi:10.1161/circulationaha.107.753483
Zeller, P., Pletscher, A., Gey, K. F., Gutmann, H., Hegedus, B., and Straub, O. (1959). Amino Acid and Fatty Acid Hydrazides: Chemistry and Action on Monoamine Oxidase. Ann. N. Y. Acad. Sci. 80, 555–567. doi:10.1111/j.1749-6632.1959.tb49234.x
Zepeda, R. J., Castillo, R., Rodrigo, R., Prieto, J. C., Aramburu, I., Brugere, S., et al. (2012). Effect of Carvedilol and Nebivolol on Oxidative Stress-Related Parameters and Endothelial Function in Patients with Essential Hypertension. Basic Clin. Pharmacol. Toxicol. 111 (5), 309–316. doi:10.1111/j.1742-7843.2012.00911.x
Zhang, B., Wang, Y., and Su, Y. (2009). Peroxiredoxins, a Novel Target in Cancer Radiotherapy. Cancer Lett. 286 (2), 154–160. doi:10.1016/j.canlet.2009.04.043
Zheng, T., Gao, Y., Baskota, A., Chen, T., Ran, X., and Tian, H. (2014). Increased Plasma DPP4 Activity Is Predictive of Prediabetes and Type 2 Diabetes Onset in Chinese over a Four-Year Period: Result from the China National Diabetes and Metabolic Disorders Study. J. Clin. Endocrinol. Metab. 99 (11), E2330–E2334. doi:10.1210/jc.2014-1480
Zhong, Z., Zhai, Y., Liang, S., Mori, Y., Han, R., Sutterwala, F. S., et al. (2013). TRPM2 Links Oxidative Stress to NLRP3 Inflammasome Activation. Nat. Commun. 4, 1611. doi:10.1038/ncomms2608
Zhou, G., Myers, R., Li, Y., Chen, Y., Shen, X., Fenyk-Melody, J., et al. (2001). Role of AMP-Activated Protein Kinase in Mechanism of Metformin Action. J. Clin. Invest. 108 (8), 1167–1174. doi:10.1172/jci13505
Zhou, H., Yang, J., Xin, T., Li, D., Guo, J., Hu, S., et al. (2014). Exendin-4 Protects Adipose-Derived Mesenchymal Stem Cells from Apoptosis Induced by Hydrogen Peroxide through the PI3K/Akt-Sfrp2 Pathways. Free Radic. Biol. Med. 77, 363–375. doi:10.1016/j.freeradbiomed.2014.09.033
Zhou, R., Yazdi, A. S., Menu, P., and Tschopp, J. (2011). A Role for Mitochondria in NLRP3 Inflammasome Activation. Nature 469 (7329), 221–225. doi:10.1038/nature09663
Zhou, Z., Tang, Y., Jin, X., Chen, C., Lu, Y., Liu, L., et al. (2016). Metformin Inhibits Advanced Glycation End Products-Induced Inflammatory Response in Murine Macrophages Partly through AMPK Activation and RAGE/NFκB Pathway Suppression. J. Diabetes Res. 2016, 4847812. doi:10.1155/2016/4847812
Zhou, Z. D., Lan, Y. H., Tan, E. K., and Lim, T. M. (2010). Iron Species-Mediated Dopamine Oxidation, Proteasome Inhibition, and Dopaminergic Cell Demise: Implications for Iron-Related Dopaminergic Neuron Degeneration. Free Radic. Biol. Med. 49 (12), 1856–1871. doi:10.1016/j.freeradbiomed.2010.09.010
Zondler, L., Miller-Fleming, L., Repici, M., Gonçalves, S., Tenreiro, S., Rosado-Ramos, R., et al. (2014). DJ-1 Interactions with α-synuclein Attenuate Aggregation and Cellular Toxicity in Models of Parkinson's Disease. Cell Death Dis. 5, e1350. doi:10.1038/cddis.2014.307
Zong, W.-X., Rabinowitz, J. D., and White, E. (2016). Mitochondria and Cancer. Mol. Cell 61 (5), 667–676. doi:10.1016/j.molcel.2016.02.011
Keywords: Aging, Reactive Oxygen Species, Mitohormesis, drugs, Pharmacology, pleiotropy
Citation: Thomas C, Wurzer L, Malle E, Ristow M and Madreiter-Sokolowski CT (2022) Modulation of Reactive Oxygen Species Homeostasis as a Pleiotropic Effect of Commonly Used Drugs. Front. Aging 3:905261. doi: 10.3389/fragi.2022.905261
Received: 26 March 2022; Accepted: 18 May 2022;
Published: 14 June 2022.
Edited by:
Haim Cohen, Bar-Ilan University, IsraelReviewed by:
Gautham Yepuri, New York University, United StatesIrene Martinez De Toda, Complutense University of Madrid, Spain
Copyright © 2022 Thomas, Wurzer, Malle, Ristow and Madreiter-Sokolowski. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Corina T. Madreiter-Sokolowski, corina.madreiter@medunigraz.at
 Carolin Thomas
Carolin Thomas Lia Wurzer2
Lia Wurzer2  Ernst Malle
Ernst Malle Corina T. Madreiter-Sokolowski
Corina T. Madreiter-Sokolowski