Tendency of microbial adhesion to denture base resins: a systematic review
- Department of Substitutive Dental Sciences, College of Dentistry, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia
Objectives: Digital denture fabrication became an alternative method to conventional denture fabrication. However reviewing the antimicrobial performance of newly introduced digital fabrication methods in comparison to the conventional method is neglected. Aim of study: this review was to compare the antiadherence properties of various CAD-CAM subtractive (milled), additive (3D printed) conventional denture base resins. In order to answer the developed PICO question: “Does CAD-CAM milled and 3D printed denture base resins have microbiological antiadherence properties over the conventional ones?” We included comparative studies on digitally fabricated Denture base resins with conventionally fabricated one in term of microbial adhesion.
Methods: All in vitro studies investigated the microbial adherence to CAD-CAM milled and 3D printed denture base resins in comparison to conventional were searched in the PubMed, Web of Sciences, and Scopus databases up to December 2023.
Results: Fifteen studies have been investigated the microbial adhesion to milled and 3D printed denture base resins. CAD-CAM milled resins significantly decreased the microbial adhesion when compared with the conventional resins and 3D printed resins, while the later showed a high tendency for microbial adhesion. The addition of antifungal agents to 3D printed resins significantly reduced C. albicans adhesion. In terms of 3D printing parameters, printing orientation affected adherence while printing technology had no effect on microbial adhesion.
Conclusion: Denture base materials and fabrication methods significantly affect the microbial adhesion. CAD-CAM milled denture base resins demonstrated low microbial adhesion. 3D-printed resins showed high tendency for C. albicans adhesion. The antiadherent properties of 3D-printed resins can be improved by incorporating antifungal agents or changing the printing parameters, but further investigations are required to validate these modifications.
1 Introduction
The most common clinical problem associated with patients wearing complete dentures is denture stomatitis (DS). This infection is primarily caused by Candida albicans adhesion to the denture base surface (1). Surface properties are considered the most important factor in C. albicans adhesion and colonization, along with other factors such as poor oral hygiene and ill-fitting dentures (2). It was reported that DS occurrence rate is about 30%–75% of denture wearers and high recurrence rate even with antifungal treatment (3). This situation increased as the surface properties change (increasing Ra and contact angle and decreasing hardness) where rougher surfaces act as a nest and become an adequate environment for microbial adhesion and colonization (2). The surface properties of denture base resins affected by the fabrication method, and CAD-CAM milled denture base resins had superior surface properties (4–6). Therefore, denture base resins with smooth surfaces that are less appealing to microbial adhesion contributed to denture longevity when combined with healthy denture foundation tissue.
For digital denture fabrication, the use of computer-aided-design-computer-aided-manufacture (CAD-CAM) methods is becoming more popular. This is due to many advantages over conventional method such as reducing the number of appointments, laboratory time required for prostheses fabrication, reducing laboratory errors, and the ability to store data for future fabrication (7–9). CAD-CAM fabricated prostheses demonstrated better adaption than conventionally-fabricated ones (10) in addition to their superior physical properties (11). CAD-CAM denture fabrication includes two methods; milling denture from prepolymerized Polymethylmethacrylate (PMMA) acrylic discs that polymerized under high pressure/temperature (subtractive method, SM) and building the denture in layers using photopolymerized resins (additive method, AM) also known as three-dimensionally (3D) printed denture base resins (12, 13). SM is the most commonly used method because it was developed before AM and has superior mechanical properties when compared to AM (7). However, AM has some advantages such as no material waste and no milling bur deterioration (12). In addition to the fabrication methods, the composition of denture base materials material has a role in the in results variations. The conventional and CAD-CAM milled are PMMA-Based while 3D printed either PMMA- or ester-based light polymerized resin (7, 11–13).
Although AM advantages, there are some drawbacks such as low mechanical properties and poor surface characteristics (14). The low physical and mechanical performance of AM has been attributed to the printing method (layer-by-layer) and polymerization method (photo-polymerization) (12, 14). Many attempts have been made to overcome these drawbacks by using different printing technologies, modifying printing parameters, and/or adding reinforcement and antimicrobial agents (15).
Studies have shown a relationship between C. albican adherence, colonization, and biofilm formation and the surface properties of denture base resins including roughness, porosities, and contact angle/hydrophilicity (1). Many studies (1, 16–18) compared surface properties of conventionally and CAD-CAM denture base resins in term of surface roughness and wettability and variation between findings was reported. Furthermore, surface roughness affected both hydrophobicity and adherence activities (13). While previous investigation demonstrated no linear relationship between the surface roughness of denture base resin and C. albican adhesion (19).
Authors of previous studies (1, 16–18) stated that the hydrophilic denture bases are less vulnerable to microbial adherence. CAD-CAM dentures base showed more wettability and showed reduced microbial adhesion compared with conventional one (1, 4, 5, 11). Another study (5) found that milled and 3D printed denture base materials were biocompatible and had similar surface characteristics. Fouda et al. (20), found that there was no difference in surface roughness between 3D printed, milled, and conventional rein, and that the adherence of C. albicans to all resins behaved similarly. Due the variations in surface properties of denture base resins and amount of microbial adhesions, authors suggested evaluating different CAD-CAM systems with different resins materials.
There have been no previous studies reviewing the microbiological antiadherence properties of digitally fabricated denture base resins. This review was conducted to evaluate the microbial adherence properties of CAD-CAM fabricated denture base resins in comparison to conventional ones, as well as to answer the research question “Does CAD-CAM milled and 3D printed denture base resins have microbiological antiadherence properties over to conventional ones?”
2 Materials and methods
2.1 Focused question
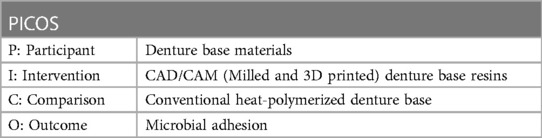
PICOS (Table 1) revealed the following study question; “Does CAD-CAM milled and 3D printed denture base resins have microbiological antiadherence properties over the conventional ones?”
2.2 Study design
To conduct this review, the preferred reporting items for systematic reviews and meta-analysis (PRISMA) recommendations (21) were followed.
2.3 Search strategy
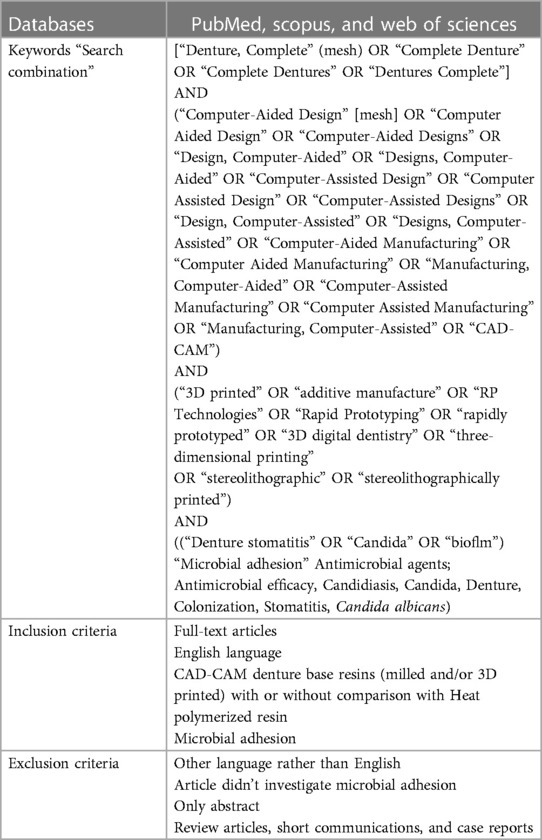
Searching for relative published literatures up to December 2023 was done through PubMed, Web of sciences, and Scopus databases. For the research strategy, both controlled and non-controlled descriptors and Boolean terms (OR, AND) were used (Table 2).
2.4 Inclusion and exclusion criteria
In vitro studies, full article published in English language studies investigated microbial adhesions to CAD-CAM manufactured denture base resins (Milled and 3D printed) and compared with conventionally fabricated were targeted and included. Other studies that did not investigate CAD-CAM denture base resins and had no microbial adhesion test were excluded. In addition to the fallowing excluded studies: not published in English, case reports, reviews, short communications, letters to the editor, and only available in abstract form (Table 2).
2.5 Study selection, data extraction, and method of analysis
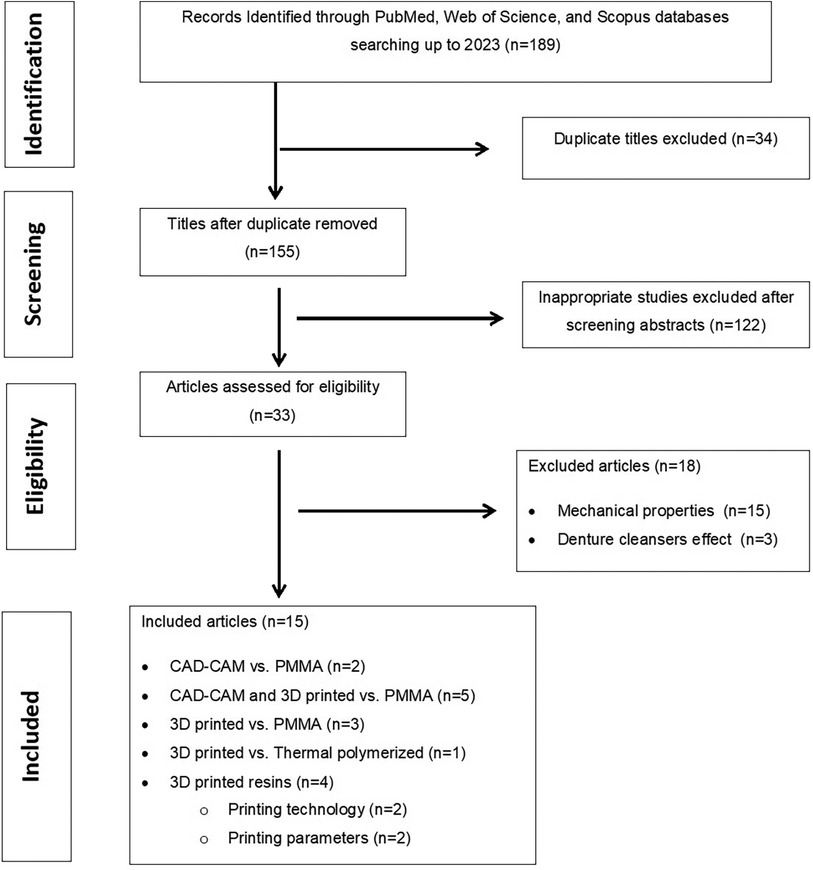
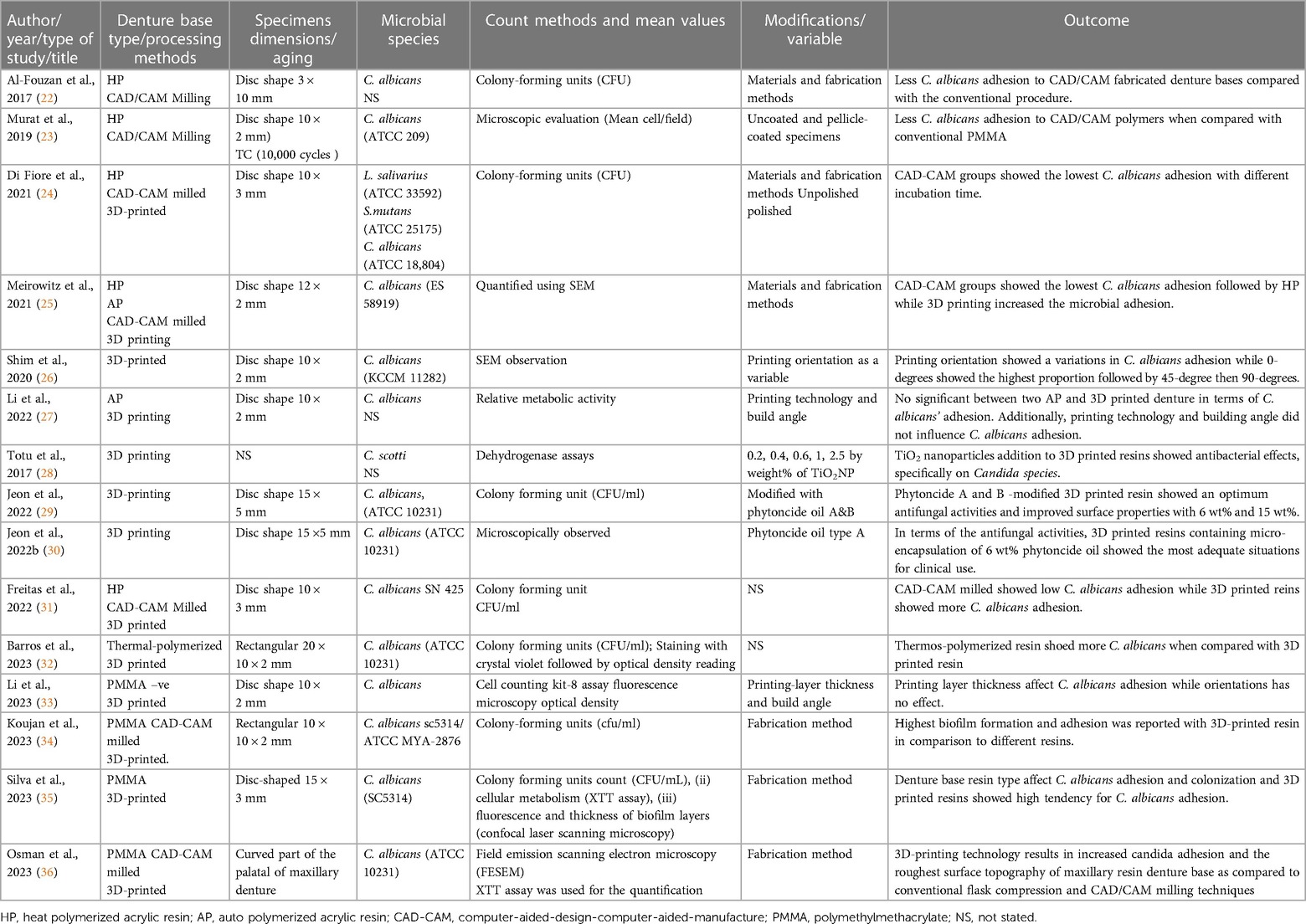
Figure 1 shows how all articles were screened for included studies selections. Following the deletion of duplicated studies, the title and abstract of each study were individually screened and analyzed by two authors (F.K.A. and M.M.G) in accordance with the inclusion criteria. Disagreements are resolved through discussion between the two authors. Following approval, the full text of relevant studies meeting the eligibility criteria was read, followed by data collection and tabulation (Table 3). Data was descriptively assessed in terms of microbial adhesion to the milled and 3D printed materials, and then compared to conventional denture base resins.
2.6 Quality assessment
According to the method and criteria detailed in previous studies (37–39), the included studied were investigated for risk of bias (Table 4) for study quality assessment. Two independent authors screened included studies using the risk of bias tool guidelines (adapted and modified from Cochrane risk of bias tool) (37–39).
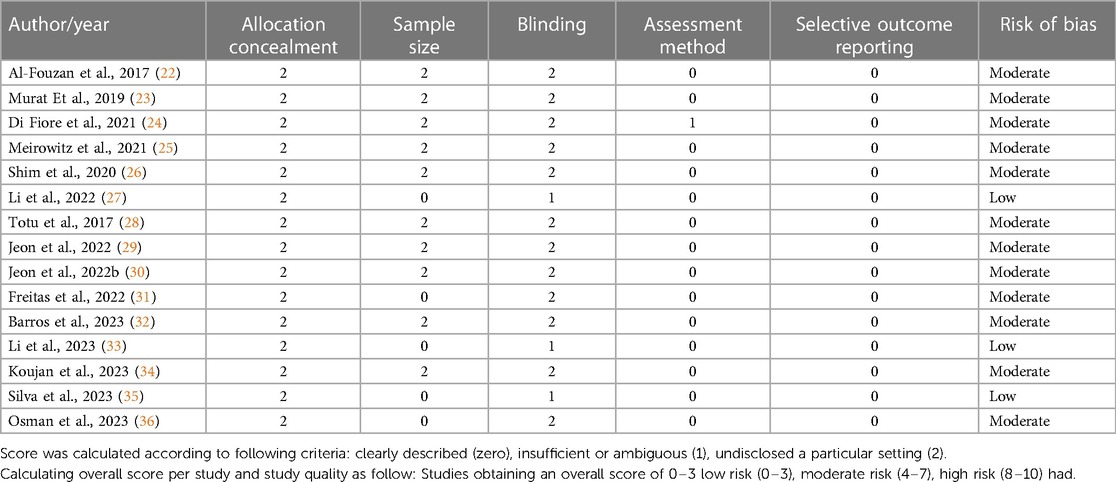
Table 4. Quality assessment and risk of bias considering aspects reported in material and methods section (risk of bias tool (adapted and modified from cochrane risk of bias tool).
3 Results
Out of 189, 15 studies (22–36) investigated the effect of microbial adhesion on CAD-CAM milled and 3D printed denture base resins. Two studies compared CAD-CAM milled resins to conventional denture base resins (22, 23), and 5 studies compared CAD-CAM milled and 3D printed resins with conventional denture base resins (24, 25, 31, 34, 36). Five studies investigated microbial adhesion to 3D printed resins (26–30); two studies investigated the effect of printing technology and printing orientation (26, 27), while three studies investigated 3D printed dentur base resins modified with TiO2 nanoparticles (28) and Phytoncide oil A&B (29, 30). C. albicans is most frequently investigated in all included studies except two studies included Candida scotti (28), and Lactobacillus salivarius, Streptococcus mutans (24). Different microbial assay methods were included; colony-forming units (CFU) (22, 24, 29, 31, 32, 34, 35), microscopic evaluation (Mean cell/field) (23, 25, 29), quantified using scanning electron microscopy (25, 26, 30, 33, 36), Relative metabolic activity (27), and Dehydrogenase assays (28).
Table 4 summarizes the quality assessment of the included studies. Out of the included studies, twelv studies revealed a moderate risk of bias, low risk was noted in three studies. Primarily the risk was attributed to the lack of allocation concealment, sample size calculation and examiner blinding.
Despite differences in denture base resin type and microbial assay between the included studies, CAD-CAM milled denture base resins demonstrated the lowest microbial adhesion compared to conventional, while 3D printed dentures demonstrated the highest microbial adhesion (31). For 3D printed resins, the proportions of microbial adhesion were highest at 0 degrees and lowest at 90 degrees (25). While the combined effect of printing technology (SLA and DLP) and printing orientation had no effect on microbial adherence (27). On the level of 3D printed resin modifications, both additives TiO2 nanoparticles (28), and Phytoncide oil A&B (29, 30) decreased the microbial adhesion.
4 Discussion
In subtractive method, the fabrication of denture base from prefabricated PMMA discs improved the mechanical behavior as well as the surface properties when compared to conventional heat polymerized denture base (4). As a result of the good surface properties of CAD-CAM milled denture base resins, less microbial adherence is expected. This was confirmed by all authors (22–36), who reported that milled denture base resins had lower C. albicans adhesion f and reduce the occurrence of DS in long-term denture use. Di Fiore et al. (24) used scanning electron microscope (SEM) to examine the surface topography of each material and found that the conventional ones had multiple grooves and deep scratches with a porous surface, whereas CAD-CAM milled had a smooth surface with fewer scratches.
3D printed resins have low surface properties when compared to milled and conventional ones. In between the included studies, two studies (24, 25) compared the C. albicans adhesion of 3D printed with CAD-CAM milled denture base resins and conventional and found that 3D printed resins exhibited significantly more microbial adhesion. This was primarily due to the nature of the printing technology; layer-by-layer object building and this layering technique resulted in stepwise edges on the specimens' surfaces (24, 25). Based on SEM analysis of specimens' surface by Di Fiore et al. (24), 3D printed resins showed more surface irregularities, multiple dots, and serrations that probably attributed to the layering of printed objects and the polymerization method (24). Previous researches (4, 31) assessed the surface roughness of 3D printed resins and found rougher surfaces than conventional even when the printing parameters were changed. While another study found no difference between CAD-CAM milled and 3D printed denture base resins in terms of surface roughness (5, 31).
The printing technology was thought to be a factor influencing the properties of 3D printed objects (15). SLA and DLP are the most commonly used technologies for fabricating denture bases (40). Surface roughness differences were reported between the two technologies (27), with SLA exhibiting irregular surfaces and DLP printed specimens exhibiting clear and regular texture. However, Li et al. found no difference in C. albicans adhesion between SLA and DLP technology (27).
Another factor was the printing orientation (26, 27), which could result in different surface patterns depending on the printing layer directions (27). According to Li et al. (33), printing orientation has a significant impact on Ra values regardless of printing technology (25, 41). Some surface features were observed with different printing angles (45° and 90°) and exhibited a ladder-like surface structure (33). Roughness changes in relation to building direction were caused by the height of step edges and the stepwise connection between printed layers (26). Li et al. (33) investigated the same orientations and two AM methods (SLA and DLP) and found no significant differences in C. albicans adhesion. When the printing orientation and post-curing time were varied, Al-Dulaijan et al. found no change in the surface roughness of 3D printed resins (42). With changing printing orientation, the layer direction is changed and affected the specimens' surface, 0-degree is expected to be smooth as the surface of specimens formed by the last printed layer (26). However, Shim et al. (26), printed specimens with different orientations (0-, 45-, and 90-degree) and evaluated the microbial adhesion and found that 0-degree showed the highest proportion. This conflict (smooth surface with more Candida adherence) could be clarified based on the surface wettability of 0-egree showed the highest hydrophilicity value according to Shim et al. (26). These findings support the hypothesis that the microbial adhesion of 3D printed resins is primarily due to surface features and wettability (1). Surface coatings of conventional PMMA denture base resins were suggested as a possible method to create a smooth surface denture base to overcome the low surface properties (43). However, this has not been investigated as of yet, so further research is advised.
Incorporating antifungal agents within the 3D printed fluid resin was another method for improving antimicrobial activity (28, 30). Two antimicrobial agents, TiO2 nanoparticles (28) and Phytoncide oil A&B (29, 30), were successfully added as antimicrobial agents to 3D printed resins. TiO2's antimicrobial effect is primarily due to its photocatalytic effect, in which UV irradiation results in oxidization decomposition (44, 45). By coordinating electron-donating groups, this effect resulted in the deactivation of cellular enzymes. This process ended by gabs in cell allowing higher permeability cell death (44). As phytoncide concentrations increased, the viability of fungal cells and optical density decreased, consequently increasing the number of atypical cells morphologically (45). In addition to having antimicrobial effect, phytoncide-filled microcapsules; the microbial adhesion, attachment, and growth were inhibited significantly when incorporated into 3D printed resins regardless of pH value (29, 30). The effect of phytoncide-filled microcapsule concentrations was found to significantly reduce C. albicans adhesion with increasing concentrations. In addition, the surface roughness increased with concentration but had no effect on C. albicans adhesion, confirming the antifungal activity of 3D-printed resin containing phytoncide-filled microcapsules (29, 30). As a result of the antifungal activities being reported and demonstrating significantly less candida adhesion when compared to the unmodified one. Both studies (29, 30) recommended using the introduced modified-3D printed resins for denture base fabrication.
Although modified 3D printed resins were found to have a positive antifungal effect, the lack of comparison with conventional or CAD-CAM milled denture base resins was considered a limitation in both studies (not used as control). In light of the findings of both studies, additional research on antimicrobial-modified 3D printed resins in comparison with conventional and CAD-CAM denture base resins is recommended rather than a comparison with the unmodified one. This was due to the fact that the modification effect was good, but still highly significant when compared to the conventional method. Moreover, microbial adhesion and related surface properties testing in terms of hydrophobicity are required (1).
Based on the review findings, CAD-CAM milled denture base resins were found to be the most appropriate materials for denture base fabrication with low microbial adhesion. 3D printed resins were more susceptible to microbial adhesion and require additional research with different printing technologies, resin modifications, or printed object surface modifications before clinical recommendations.
Although the importance of the subject in which this systematic review was able to compare the most recent literatures on microbial adhesion to different denture base resins, nevertheless, the included articles were limited to in vitro studies reducing the scientific evidence of study point. In addition to other limitations due to the small number of studies included, as well as differences in resin type, fabrication method, variables investigated, and microbial assessment methods. All of these constraints made it difficult to reach a clear conclusion based on the study objective. As a result, a future systematic review was suggested.
5 Conclusions
CAD-CAM milled denture base resin had lower microbial adhesion. When compared to conventional heat polymerized and CAD/CAM milled denture base resins, 3D printed resins have a high tendency for microbial adhesion due to their poor surface properties. The addition of antimicrobial agents to 3D printed resins reduced microbial adhesion. However, more research is needed to prove the effects of these additives when combined with different printing parameters.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
FKA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MMG: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gad MM, Abualsaud R, Khan SQ. Hydrophobicity of denture base resins: a systematic review and meta-analysis. J Int Soc Prev Community Dent. (2022) 12(2):139–59. doi: 10.4103/jispcd.JISPCD_213_21
2. Gendreau L, Loewy ZG. Epidemiology and etiology of denture stomatitis. J Prosthod. (2011) 20(4):251–60. doi: 10.1111/j.1532-849X.2011.00698.x
3. Al-Khalifa KS, Gad MM, Alshahrani FA, Alqarawi FK, Hassanein FR, Khurshid Z, et al. Influence of propolis extract (caffeic acid phenethyl ester) addition on the Candida albicans adhesion and surface properties of autopolymerized acrylic resin. Int J Dent. (2022) 2022:6118660. doi: 10.1155/2022/6118660
4. Helal MA, Fadl-Alah A, Baraka YM, Gad MM, Emam AM. In-vitro comparative evaluation for the surface properties and impact strength of CAD/CAM milled, 3D printed, and polyamide denture base resins. J Int Soc Prev Community Dent. (2022) 12(1):126–31. doi: 10.4103/jispcd.JISPCD_293_21
5. Srinivasan M, Kalberer N, Kamnoedboon P, Mekki M, Durual S, Özcan M, et al. CAD-CAM complete denture resins: an evaluation of biocompatibility, mechanical properties, and surface characteristics. J Dent. (2021) 114:103785. doi: 10.1016/j.jdent.2021.103785
6. Al-Qarni FD, Goodacre CJ, Kattadiyil MT, Baba NZ, Paravina RD. Stainability of acrylic resin materials used in CAD-CAM and conventional complete dentures. J Prosthet Dent. (2020) 123(6):880–7. doi: 10.1016/j.prosdent.2019.07.004
7. Steinmassl PA, Klaunzer F, Steinmassl O, Dumfahrt H, Grunert I. Evaluation of currently available CAD/CAM denture systems. Int J Prosthodont. (2017) 30(2):116–22. doi: 10.11607/ijp.5031
8. Saponaro PC, Yilmaz B, Heshmati RH, McGlumphy EA. Clinical performance of CAD-CAM-fabricated complete dentures: a cross-sectional study. J Prosthet Dent. (2016) 116(3):431–45. doi: 10.1016/j.prosdent.2016.03.017
9. Goodacre CJ, Garbacea A, Naylor WP, Daher T, Marchack CB, Lowry J. CAD/CAM fabricated complete dentures: concepts and clinical methods of obtaining required morphological data. J Prosthet Dent. (2012) 107(1):34–46. doi: 10.1016/S00223913(12)60015-8
10. Wang C, Shi YF, Xie PJ, Wu JH. Accuracy of digital complete dentures: a systematic review of in vitro studies. J Prosthet Dent. (2021) 125(2):249–56. doi: 10.1016/j.prosdent.2020.01.004
11. Baba NZ. CAD/CAM complete denture systems and physical properties: a review of the literature. J Prosthodont. (2021) 30(S2):113–24. doi: 10.1111/jopr.13243
12. Kalberer N, Mehl A, Schimmel M, Müller F, Srinivasan M. CAD-CAM milled versus rapidly prototyped (3D-printed) complete dentures: an in vitro evaluation of trueness. J Prosthet Dent. (2019) 121(4):637–43. doi: 10.1016/j.prosdent.2018.09.001
13. Steinmassl PA, Wiedemair V, Huck C, Klaunzer F, Steinmassl O, Grunert I, et al. Do CAD/CAM dentures really release less monomer than conventional dentures? Clin Oral Investig. (2017) 21(5):1697–705. doi: 10.1007/s00784-016-1961-6
14. Fouda SM, Gad MM, Abualsaud R, Ellakany P, AlRumaih HS, Khan SQ, et al. Flexural properties and hardness of CAD-CAM denture base materials. J Prosthodont. (2023) 32(4):318–24. doi: 10.1111/jopr.13535
15. Gad MM, Fouda SM. Factors affecting flexural strength of 3D-printed resins: a systematic review. J Prosthodont. (2023) 32(S1):96–110. doi: 10.1111/jopr.13640
16. Alammari MR. The influence of polishing techniques on pre-polymerized CAD/CAM acrylic resin denture bases. Electron Physician. (2017) 9(10):5452–8. doi: 10.19082/5452
17. Steinmassl O, Dumfahrt H, Grunert I, Steinmassl PA. Influence of CAD/CAM fabrication on denture surface properties. J Oral Rehabil. (2018) 45(5):406–13. doi: 10.1111/joor.12621
18. Arslan M, Murat S, Alp G, Zaimoglu A. Evaluation of flexural strength and surface properties of prepolymerized CAD/CAM PMMA-based polymers used for digital 3D complete dentures. Int J Comput Dent. (2018) 21:31–40.29610779
19. Hahnel S, Rosentritt M, Handel G, Bürgers R. In vitro evaluation of artificial ageing on surface properties and early Candida albicans adhesion to prosthetic resins. J Mater Sci Mater Med. (2009) 20(1):249–55. doi: 10.1007/s10856-008-3570-7
20. Fouda SM, Gad MM, Abualsaud R, Ellakany P, AlRumaih HS, Farooqi FA, et al. In vitro evaluation of Candida albicans adhesion and related surface properties of CAD/CAM denture base resins. Eur J Dent. (2023). doi: 10.1055/s-0043-1774319. [Epub ahead of print]38086425
21. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Br Med J. (2015) 350:g7647. doi: 10.1136/bmj.g7647
22. Al-Fouzan AF, Al-Mejrad LA, Albarrag AM. Adherence of Candida to complete denture surfaces in vitro: a comparison of conventional and CAD/CAM complete dentures. J Adv Prosthodont. (2017) 9(5):402–8. doi: 10.4047/jap.2017.9.5.402
23. Murat S, Alp G, Alatalı C, Uzun M. In vitro evaluation of adhesion of Candida albicans on CAD/CAM PMMA-based polymers. J Prosthodont. (2019) 28(2):873–9. doi: 10.1111/jopr.12942
24. Di Fiore A, Meneghello R, Brun P, Rosso S, Gattazzo A, Stellini E, et al. Comparison of the flexural and surface properties of milled, 3D-printed, and heat polymerized PMMA resins for denture bases: an in vitro study. J Prosthodont Res. (2021) 66(3):502–8. doi: 10.2186/jpr.JPR_D_21_00116
25. Meirowitz A, Rahmanov A, Shlomo E, Zelikman H, Dolev E, Sterer N. Effect of denture base fabrication technique on Candida albicans adhesion in vitro. Materials (Basel). (2021) 14(1):221. doi: 10.3390/ma14010221
26. Shim JS, Kim JE, Jeong SH, Choi YJ, Ryu JJ. Printing accuracy, mechanical properties, surface characteristics, and microbial adhesion of 3D-printed resins with various printing orientations. J Prosthet Dent. (2020) 124(4):468–75. doi: 10.1016/j.prosdent.2019.05.034
27. Li P, Fernandez PK, Spintzyk S, Schmidt F, Beuer F, Unkovskiy A. Effect of additive manufacturing method and build angle on surface characteristics and Candida albicans adhesion to 3D printed denture base polymers. J Dent. (2022) 116:103889. doi: 10.1016/j.jdent.2021.103889
28. Totu EE, Nechifor AC, Nechifor G, Aboul-Enein HY, Cristache CM. Poly(methyl methacrylate) with TiO2 nanoparticles inclusion for stereolitographic complete denture manufacturing—the future in dental care for elderly edentulous patients? J Dent. (2017) 59:68–77. doi: 10.1016/j.jdent.2017.02.012
29. Jeon S, Jo YH, Yoon HI, Han JS. Antifungal effect, surface roughness, and cytotoxicity of three-dimensionally printed denture base with phytoncide-filled microcapsules: an in-vitro study. J Dent. (2022) 120:104098. doi: 10.1016/j.jdent.2022.104098
30. Jeon S, Jo YH, Yoon HI, Han JS. Effect of phytochemical-filled microcapsules with antifungal activity on material properties and dimensional accuracy of denture base resin for three-dimensional printing. BMC Oral Health. (2022) 22(1):178. doi: 10.1186/s12903-022-02216-z
31. Freitas RFCP, Duarte S, Feitosa S, Dutra V, Lin WS, Panariello BHD, et al. Physical, mechanical, and anti-biofilm formation properties of CAD-CAM milled or 3D printed denture base resins: in vitro analysis. J Prosthodont. (2023) 32(S1):38–44. doi: 10.1111/jopr.13554
32. Barros MC, Mazzon RR, Soto AF, Duque TM, Lidani R, Teixeira CS, et al. Candida albicans adhesion on 3D-printed and thermopolymerizable polymethyl methacrylate for removable prostheses. Am J Dent. (2023) 36(3):130–5.37364190
33. Li P, Fernandez PK, Spintzyk S, Schmidt F, Yassine J, Beuer F, et al. Effects of layer thickness and build angle on the microbial adhesion of denture base polymers manufactured by digital light processing. J Prosthodont Res. (2023) 67(4):562–7. doi: 10.2186/jpr.JPR_D_22_00126
34. Koujan A, Aggarwal H, Chen PH, Li Z, Givan DA, Zhang P, et al. Evaluation of Candida albicans adherence to CAD-CAM milled, 3D-printed, and heat-cured PMMA resin and efficacy of different disinfection techniques: an in vitro study. J Prosthodont. (2023) 32(6):512–8. doi: 10.1111/jopr.13583
35. Silva MDDD, Nunes TSBS, Viotto HEDC, Coelho SRG, Souza RF, Pero AC. Microbial adhesion and biofilm formation by Candida albicans on 3D-printed denture base resins. PLoS One. (2023) 18(10):e0292430. doi: 10.1371/journal.pone.0292430
36. Osman RB, Khoder G, Fayed B, Kedia RA, Elkareimi Y, Alharbi N. Influence of fabrication technique on adhesion and biofilm formation of Candida albicans to conventional, milled, and 3D-printed denture base resin materials: a comparative in vitro study. Polymers (Basel). (2023) 15(8):1836. doi: 10.3390/polym15081836
37. Faggion CM Jr. Guidelines for reporting pre-clinical in vitro studies on dental materials. J Evid Based Dent Pract. (2012) 12(4):182–9. doi: 10.1016/j.jebdp.2012.10.001
38. Lundh A, Gøtzsche PC. Recommendations by cochrane review groups for assessment of the risk of bias in studies. BMC Med Res Methodol. (2008) 21(8):22–9. doi: 10.1186/1471-2288-8-22
39. Abualsaud R, Gad MM. Flexural strength of CAD/CAM denture base materials: systematic review and meta-analysis of in-vitro studies. J Int Soc Prev Community Dent. (2022) 12(2):160–70. doi: 10.4103/jispcd.JISPCD_310_21
40. Stansbury W, Idacavage MJ. 3D printing with polymers: challenges among expanding options and opportunities. Dent Mater. (2016) 32(1):54–64. doi: 10.1016/j.dental.2015.09.018
41. Revilla-León M, Jordan D, Methani MM, Piedra-Cascón W, Özcan M, Zandinejad A. Influence of printing angulation on the surface roughness of additive manufactured clear silicone indices: an in vitro study. J Prosthet Dent. (2021) 125(3):462–8. doi: 10.1016/j.prosdent.2020.02.008
42. Al-Dulaijan YA, Alsulaimi L, Alotaibi R, Alboainain A, Akhtar S, Khan SQ, et al. Effect of printing orientation and postcuring time on the flexural strength of 3D-printed resins. J Prosthodont. (2023) 32(S1):45–52. doi: 10.1111/jopr.13572
43. AlBin-Ameer MA, Alsrheed MY, Aldukhi IA, Matin A, Khan SQ, Abualsaud R, et al. Effect of protective coating on surface properties and Candida albicans adhesion to denture base materials. J Prosthodont. (2020) 29(1):80–6. doi: 10.1111/jopr.13118
44. Tsuji M, Ueda T, Sawaki K, Kawaguchi M, Sakurai K. Biocompatibility of a titanium dioxide-coating method for denture base acrylic resin. Gerodontology. (2016) 33(4):539–44. doi: 10.1111/ger.12204
Keywords: 3D printing, CAD-CAM milled, microbial adhesion, complete dentures, digital dentures
Citation: Alqarawi FK and Gad MM (2024) Tendency of microbial adhesion to denture base resins: a systematic review. Front. Oral. Health 5:1375186. doi: 10.3389/froh.2024.1375186
Received: 23 January 2024; Accepted: 7 May 2024;
Published: 16 May 2024.
Edited by:
Sigrun Eick, University of Bern, SwitzerlandReviewed by:
Janaina Habib Jorge, São Paulo State University, BrazilSudipto Datta, Indian Institute of Science (IISc), India
© 2024 Alqarawi and Gad. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammed M. Gad, mmjad@iau.edu.sa
 Firas K. Alqarawi
Firas K. Alqarawi Mohammed M. Gad
Mohammed M. Gad