Impact of everolimus plus calcineurin inhibitor on formation of non-HLA antibodies and graft outcomes in kidney transplant recipients: 12-month results from the ATHENA substudy
- 1BIH Biomedical Innovation Academy, Berlin Institute of Health at Charité—Universitätsmedizin Berlin, Berlin, Germany
- 2Charité—Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Clinic for Nephrology and Critical Care Medicine, Campus Virchow-Klinikum, Berlin, Germany
- 3Transplant Centre Cologne, Cologne General Hospital, Cologne, Germany
- 4Institute of Transfusion Medicine, Kliniken der Stadt Köln, Cologne, Germany
- 5Department of Nephrology, University Hospital Frankfurt, Goethe University Frankfurt, Frankfurt, Germany
- 6III. Department of Medicine, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
- 7Nephrology, Kidney Center Heidelberg, University Hospital Heidelberg, Heidelberg, Germany
- 8Department of Internal Medicine, Transplant Nephrology, University Hospital of Münster, Münster, Germany
- 9Immunology, Novartis Pharma GmbH, Nürnberg, Germany
- 10Department of Hepatobiliary Surgery and Visceral Transplantation, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
- 11Organ Transplantation Center, The First Affiliated Hospital of University of Science and Technology of China, Anhui Provincial Hospital, Hefei, China
Background: Non-human leukocyte antigen (non-HLA) antibodies including antibodies targeting Angiotensin II type 1 (AT1R) and Endothelin-1 type A (ETAR) receptors represent a topic of interest in kidney transplantation (KTx). This exploratory substudy evaluated the impact of everolimus (EVR) or mycophenolic acid (MPA) in combination with tacrolimus (TAC) or cyclosporine A (CsA) in patients with preformed non-HLA antibodies, potentially associated rejections and/or their impact on renal function over 1 year.
Methods: All eligible patients were randomized (1:1:1) before transplantation to receive either EVR/TAC, EVR/CsA, or MPA/TAC regimen. The effect of these regimens on the formation of non-HLA antibodies within one year post de novo KTx and the association with clinical events was evaluated descriptively in randomized (n = 268) population.
Results: At Month 12, in EVR/TAC group, higher incidence of patients negative for AT1R- and ETAR-antibodies (82.2% and 76.7%, respectively) was noted, whereas the incidence of AT1R- and ETAR-antibodies positivity (28.1% and 34.7%, respectively) was higher in the MPA/TAC group. Non-HLA antibodies had no influence on clinical outcomes in any treatment group and no graft loss or death was reported.
Conclusions: The studied combinations of immunosuppressants were safe with no influence on clinical outcomes and suggested minimal exposure of calcineurin inhibitors for better patient management.
Clinical Trial Registration: https://clinicaltrials.gov/ (NCT01843348; EudraCT number: 2011-005238-21).
1. Introduction
Non-human leukocyte antigen (non-HLA) antibodies (Abs) against Angiotensin II type 1 receptor Abs (AT1R-Abs) and Endothelin-1 type A receptor Abs (ETAR-Abs) are responsible for activating signaling pathways associated with cell proliferation, vascular injury (1), increased risk of allograft rejection (2–5) and fibrosis in solid organ transplant recipients (6, 7) implicating their impact on post-transplant morbidity and mortality. Banasik et al. revealed that the existence of ETAR-Abs is linked to decreased kidney transplant (KTx) function in the first 12 months after transplantation (8). In KTx patients, high levels of AT1R- and/or ETAR-Abs are associated with morphological and functional allograft injury and graft loss (8–11). Further, increased levels of AT1R- and ETAR-Abs are also linked to cellular and antibody-mediated rejection with an influence on the early onset of microvasculopathy in patients after heart transplantation (12). Sorohan et al. reported that immunosuppression (induction and maintenance) with anti-thymocyte globulin and immediate-release tacrolimus (TAC) are independent risk factors for the development of non-HLA antibodies in KTx recipients (13). Considering the important role of non-HLA Abs on graft outcomes (14–16) evaluating the impact of immunosuppression on these Abs and clinical outcomes after organ transplantation is still an unmet need.
Everolimus (EVR), a mammalian target of rapamycin inhibitor (mTORi), acts through mechanisms complementary to calcineurin inhibitors (CNIs), such as TAC, thereby allowing reduction of CNI exposure (17). In addition, EVR is also associated with a decreased incidence of cancer (18, 19), and a beneficial effect on cardiovascular stability (20). Moreover, studies have reported that EVR reduces infections (21), particularly CMV (22–26) and BKV infections (26, 27), and has shown to improve COVID-19 vaccination response in KTx recipients (28). In a phase 3b, multicenter, open-label, 24-month study of 833 de novo (who received a first kidney transplant) living or deceased donor KTx recipients, the use of EVR was associated with a more than 60% reduction in cyclosporine A (CsA) exposure with comparable efficacy and renal function to a mycophenolic acid plus standard-exposure CsA (MPA + sCsA) regimen over a 2-year period (17, 29).
ATHENA, the to date largest randomized European kidney transplantation study, was a 12-month, prospective, multicenter, randomized, parallel group, open-label study undertaken in 612 de novo KTx recipients (ClinicalTrials.gov identifier: NCT01843348; EudraCT number: 2011-005238-21) that compared EVR in combination with TAC (EVR + TAC) or CsA (EVR + CsA) vs. MPA + TAC. The 12-month results from the ATHENA study showed that EVR + TAC or CsA has comparable efficacy to MPA + TAC although non-inferiority of renal function with EVR + TAC/CsA was not achieved (26). Given the paucity of literature on the effect of the immunosuppression on non-HLA antibody levels and their effects in de novo KTx recipients, this exploratory substudy in patients from the ATHENA study was the first to evaluate the impact of EVR or MPA in combination with CNI on preformed non-HLA antibody, potentially associated rejections and/or its impact on renal function from the time of transplantation (baseline) to one year.
2. Materials and methods
2.1. Study design and conduct
ATHENA was a 12-month, prospective, multicenter, randomized, controlled, parallel group, open label study in de novo KTx recipients. The study was conducted from December 27, 2012, through March 23, 2016, in Germany and France. Methods for the ATHENA study, including inclusion/exclusion criteria, the immunosuppression regimen, and patient stratification have been described in detail previously (26). Briefly, all eligible patients of low to moderate immunological risk were randomized in a 1:1:1 ratio prior to transplantation to receive either EVR/TAC, EVR/CsA, or MPA/TAC regimen (26, 30). All patients received basiliximab 20-mg induction therapy on day 0 and 4, and a minimum dose of 5-mg prednisolone or equivalent until month 12 (M12). The target EVR trough concentration in the EVR/TAC and EVR/CsA groups was in the range of 3 to 8 ng/ml throughout the study period. In the EVR/TAC and MPA/TAC groups, the target TAC trough concentration was in the range of 4 to 8 ng/ml until the end of M2 and in the range of 3 to 5 ng/ml thereafter. The CsA target range in the EVR/CsA group was 75 to 125 ng/ml until the end of M2 and 50 to 100 ng/ml thereafter. In the MPA/TAC group, MPA was given as enteric-coated mycophenolate sodium (1.44 g/d) or mycophenolate mofetil (2 g/d).
The study protocol and all amendments were reviewed and approved by the independent ethics committee or institutional review board for each center. The study was conducted according to the ethical principles of the Declaration of Helsinki. Informed consent was obtained from each patient in writing before randomization.
2.2. Study outcomes
This substudy investigated the effect of the three immunosuppressive regimens on preformednon-HLA Abs, potentially associated rejections and/or its impact on renal function over one year post de novo KTx. Blood samples of 5 ml were collected for all patients on the day of transplantation (baseline), M6 and M12. AT1R- and ETAR-Abs were measured by ELISA assays using commercially available kits (CellTrend GmbH, Luckenwalde, Germany) according to manufacturer's instructions. The samples were assayed on ELISA plates which were pre-coated with membrane extracts from Chinese Hamster Ovary cells overexpressing the human receptors AT1R and ETAR individually in their native conformation. Plates were then incubated for two hours at 4°C with serum samples obtained from patients. Following washing, plates were incubated with a labeled secondary antibody detecting human Abs. After a second phase of washing, presence of the labeled antibody was revealed, and optical density measured in Units/ml (U/ml) represented the level of non-HLA Abs in the serum samples (8).
2.3. Statistical analysis
Patients who received at least one dose of the study drug were considered in the intent-to-treat (ITT) population, and all ITT patients without any major protocol deviation were considered in the per-protocol (PP) population. The analysis set included all transplanted patients with at least one antibody assessment (either HLA and/or non-HLA). The analysis of non-HLA Abs was carried out descriptively. The embedded subgroups of non-HLA Abs were defined as follows: preformed non-HLA AT1R-Abs: >10 U/ml at baseline; preformed non-HLA ETAR-Abs: >10 U/ml at baseline.
3. Results
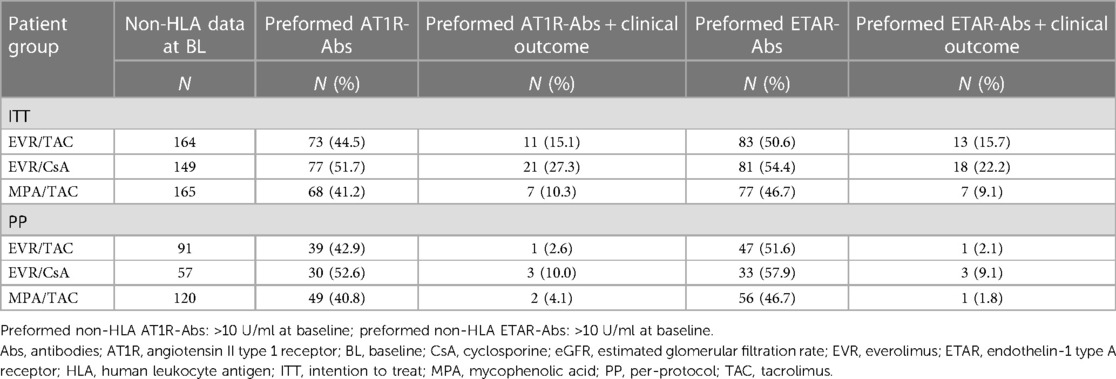
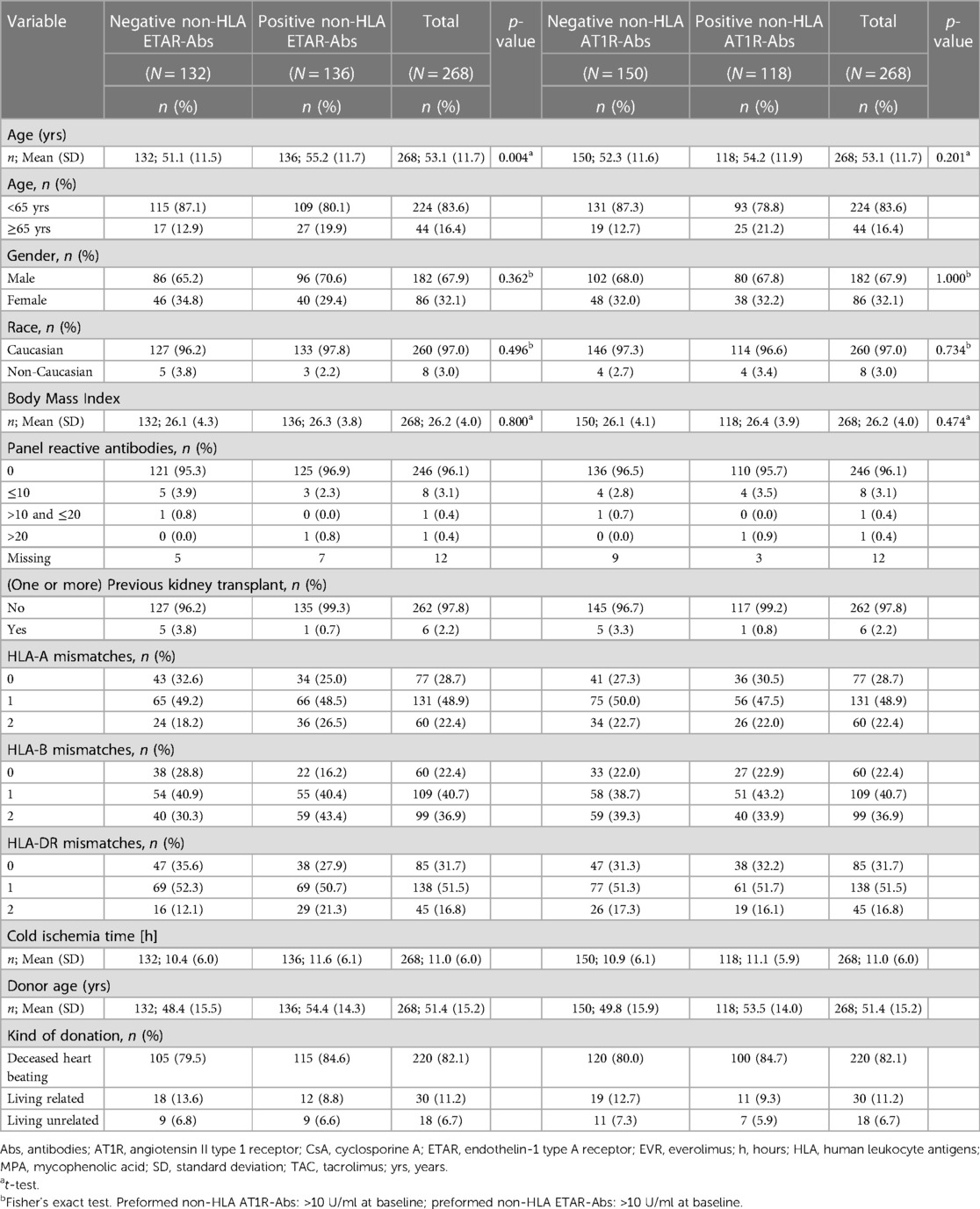
A total of 612 patients were included in this study. Since the non-HLA Abs data analysis was comparable in ITT (n = 478/612) and PP (n = 268/612), here we reported only the PP results (n = 268; EVR/TAC n = 91, EVR/CsA n = 57 and MPA/TAC n = 120 pts) (Table 1). The baseline and demographic details of the patients are presented in Table 2 and Supplementary Table S1. At baseline, 136 (51%) showed positivity for ETAR-Abs and 118 (44%) showed positivity for AT1R-Abs (Table 1); of which 34 (12.7%) patients showed positivity for only ETAR-Abs, 16 (6.0%) patients for only AT1R-Abs, whereas 102 patients (38.1%) showed positivity for both ETAR- and AT1R-Abs and 116 patients (43.3%) showed absence of both non-HLA Abs (cutoff >10 U/ml) (Supplementary Table S1). At baseline, higher incidence of patients positive for only AT1R- and only ETAR-Abs (42.9% and 51.6%, respectively) were noted in the EVR/CsA group, whereas in MPA/TAC, 40.8% and 46.7% patients were positive for only AT1R- and only ETAR-Abs, respectively (Table 3). At M6, no difference was noted in patients positive and negative for only AT1R-Abs in all treatment groups, whereas higher incidence of patients positive for ETAR-Abs were noted in EVR/CsA group and no difference was observed in patients negative for ETAR-Abs. At M12, the incidence of only AT1R- and only ETAR-Abs positivity (28.1% and 34.7%, respectively) was higher in the MPA/TAC group, whereas the higher incidence of patients negative for only AT1R- and only ETAR-Abs (82.2% and 76.7%, respectively) was noted in the EVR/TAC group. The number of patients with positive AT1R- and ETAR-Abs decreased at M6 in all treatment groups and at M12 in the EVR/TAC group while it increased slightly in MPA/TAC group at M12 (Table 3).
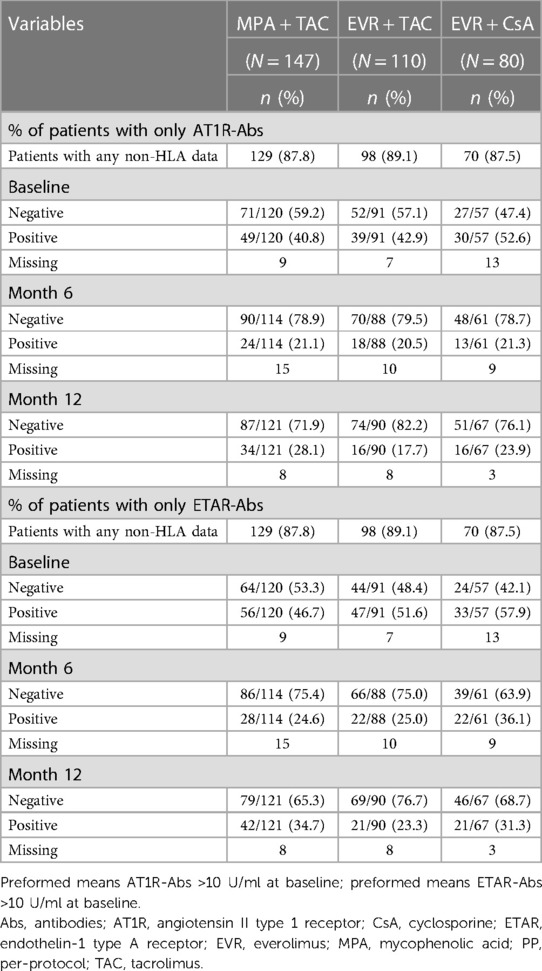
Table 3. Incidences of only AT1R-antibodies and only ETAR-antibodies at baseline, month 6 and month 12 by treatment (PP).
Preformed non-HLA Abs had no influence on clinical outcome in all treatment groups. At M12, out of 118 patients positive for only AT1R-Abs, only 1/39 (2.6%, EVR + TAC), 3/30 (10%, EVR + CsA) and 2/49 (4.1%, MPA + TAC) reported incidence of BPAR (Table 4). In patients positive for only ETAR-Abs (N = 136), similar figures were noted with 1/47 (2.1%, EVR + TAC), 3/33 (9.1%, EVR + CsA) and 1/56 (1.8%, MPA + TAC) patients who experienced BPAR at M12 (Table 4). Similarly in patients without non-HLA Abs, the number of BPAR events were very small in EVR/TAC and EVR/CsA groups but increased slightly in MPA/TAC group compared to patients with preformed non-HLA Abs. No graft loss or death was reported in any treatment groups irrespective of non-HLA Abs status at baseline.
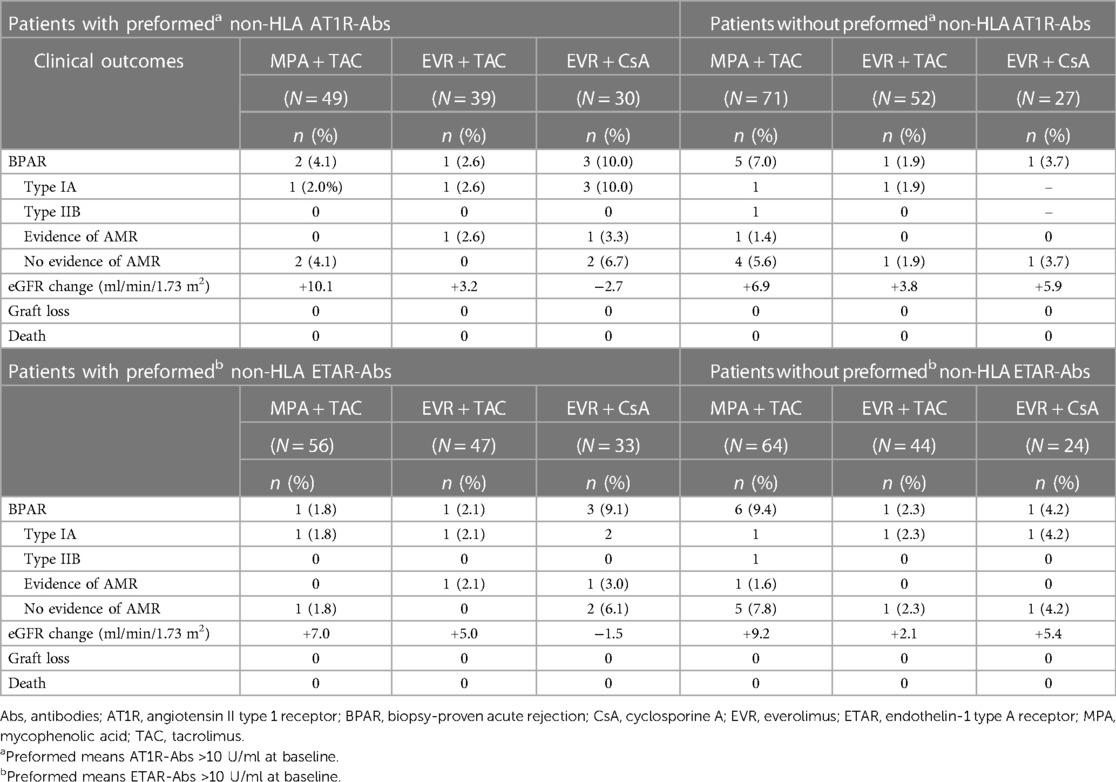
Table 4. Association of non-HLA antibodies expression and clinical outcome at month 12 by treatment.
Estimated glomerular filtration rate (eGFR) change from M1 to M12 was comparable in patients positive for performed non-HLA Abs vs. negative for non-HLA Abs (Table 4; Figures 1, 2). eGFR improvement was noted for EVR/TAC and MPA/TAC from baseline to Month 12, irrespective of non-HLA Abs positive status at baseline (AT1R-Abs: +3.2 ml/min/1.73 m2 and +10.1 ml/min/1.73 m2; ETAR-Abs: +5.0 ml/min/1.73 m2 and +7.0 ml/min/1.73 m2, respectively for EVR/TAC and MPA/TAC) or negative status at baseline (AT1R-Abs: +3.8 ml/min/1.73 m2 and +6.9 ml/min/1.73 m2; ETAR-Abs: +2.1 ml/min/1.73 m2 and +9.2 ml/min/1.73 m2). Patients who were on EVR/CsA with positive non-HLA Abs showed decrease in eGFR from M1 to M12 (AT1R-Abs: −2.7 ml/min/1.73 m2 and ETAR-Abs: −1.5 ml/min/1.73 m2; Figures 1, 2), whereas eGFR increased in patients that did not exhibit non-HLA Abs at baseline (AT1R-Abs: +5.9 ml/min/1.73 m2; ETAR-Abs: +5.4 ml/min/1.73 m2; Figures 1, 2).
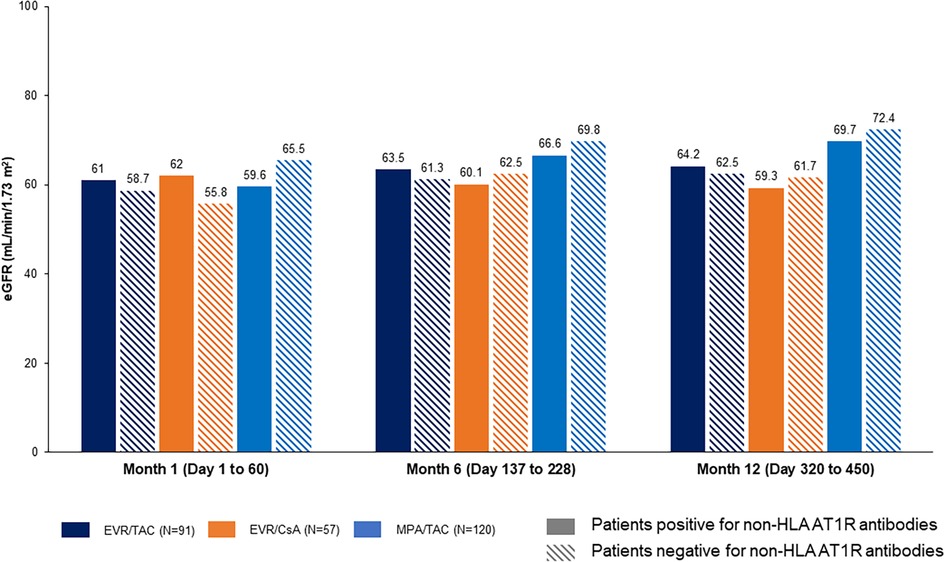
Figure 1. Influence of preformed non-HLA AT1R-antibodies on eGFR (Nankivell). Preformed non-HLA AT1R-Abs: >10 U/ml at baseline. Abs, antibodies; AT1R, angiotensin II type 1 receptor; CsA, cyclosporine; eGFR, estimated glomerular filtration rate; EVR, everolimus; HLA, human leukocyte antigens; MPA, mycophenolic acid; TAC, tacrolimus.
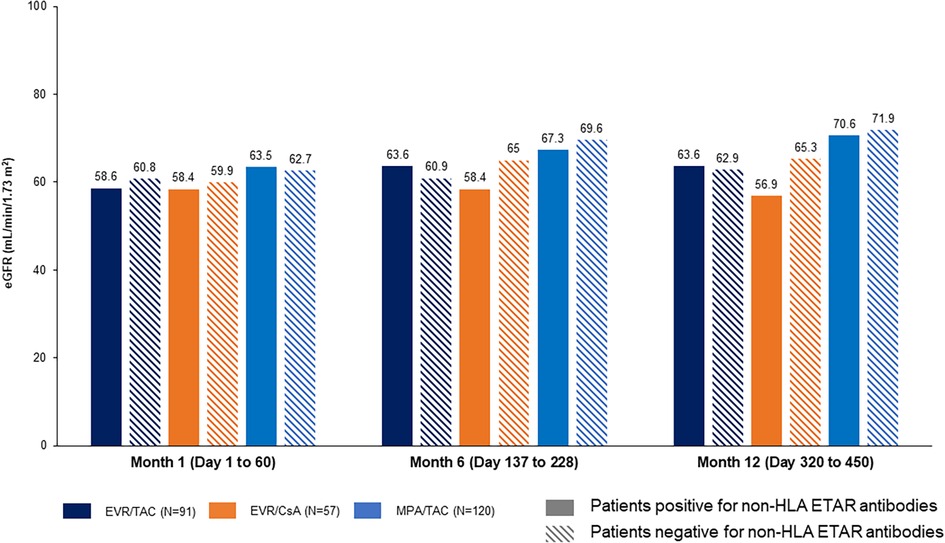
Figure 2. Influence of preformed non-HLA ETAR-antibodies on eGFR (Nankivell). Preformed non-HLA ETAR-Abs: >10 U/ml at baseline. Abs, antibodies; CsA, cyclosporine; eGFR, estimated glomerular filtration rate; ETAR, endothelin-1 type A receptor; EVR, everolimus; HLA, human leukocyte antigens; MPA, mycophenolic acid; TAC, tacrolimus.
4. Discussion
This exploratory ATHENA substudy was one of the first studies to compare the effect of EVR therapy with TAC or CsA vs. a MPA + TAC on de novo KTx patients regarding preformed non-HLA Abs, up to 12 months after transplantation.
Based on previous literature that preformed non-HLA Abs including Abs targeting AT1R and ETAR may have a very important role in affecting graft outcomes and survival after kidney transplantation, we were interested to look in a prospective trial with continuous immunosuppressive regimen exposure over 12 months and found that treatment with EVR or MPA with reduced CNI exposure was safe with no influence on graft outcomes. Results of biopsies in patients with a high level of these non-HLA Abs revealed featured characteristics of vascular acute or chronic injury (8–10). Banasik et al. conducted a study to evaluate the presence of non-HLA Abs at the time of transplant in 65 KTx recipients. The study results revealed that the high level of non-HLA Abs found in patients at the time of biopsy and graft loss in the non-HLA positive patients was also significantly higher (p = 0.00099) (10). In another study by Banasik et al., the presence of ETAR-Abs was evaluated in 116 KTx recipients, before and after transplantation. The study concluded that 47.4% of the analyzed KTx recipients were positive with ETAR-Abs before transplantation, and the presence of ETAR-Abs was linked to poor renal transplant function during the 1 year after transplantation (8).
Non-HLA Abs, specifically AT1R-Abs, are also responsible for activating the renin-angiotensin system. Studies have reported that AT1R-Abs have been linked to hypertension in pregnancy and malignant hypertension in non-transplant patients and are responsible for vascular pathology and severe hypertension in KTx recipients (31–34). Various treatment approaches, including valsartan, constitute an optimal therapy for the management of hypertension in KTx recipients. Dragun et al., examined losartan in KTx recipients with malignant hypertension and refractory rejection caused by AT1R-Abs. In comparison to individuals who did not take losartan, patients who did, demonstrated a much lower inflammatory infiltrate in the allograft biopsy and significantly higher graft survival (33).
It is considered that the primary target for non-HLA Abs is the vascular endothelium, which is responsible for hemodynamics regulation, angiogenic vascular remodeling, and metabolic, synthetic, and anti-inflammatory or antithrombogenic mechanisms (8). Various studies have reported that the significance of non-HLA Abs in KTx injury is unknown, although the impact of donor specific anti-HLA Abs is well understood (35–38). Banasik et al. reported that non-HLA Abs may participate in the arterial wall structural injury, which supports clothing and/or narrowing of arterial walls. Furthermore, non-HLA responses may be induced by cytokine-mediated endothelial cell activation (8). Additionally, AT1R-induced protein translation is mediated via the Akt-mTOR signaling pathway. Cellular metabolism, growth, proliferation, survival, and differentiation are all regulated by mTOR, specifically. It is the catalytic subunit of two mTOR signaling complexes, mTORC1 and mTORC2 (1). Recently, the ribosomal protein S6 kinase beta-1 (p-p70S6K) downstream effector of mTORC1 has been proposed as a diagnostic marker for antibody-mediated rejection in heart allografts (39). Various mTOR inhibitors including EVR are widely used in transplantation because of their antiproliferative effects (7, 40).
Our study is the first to definitively identify patients who were exclusively and only positive for preformed ETAR-Abs. From literature, different cut-offs have been used in the non-HLA Abs studies. Giral et al. and Lefaucheur C et al., considered the cut-off of AT1R-Abs at ≥10 U/ml and reported 47.2% and 20.1% of positivity in recipients, which was associated with high risk of developing acute rejection, antibody-mediated rejection and graft loss (2, 3). Taniguchi and Pearl MH et al. considered cut-off of AT1R-Abs at ≥15 U/ml and ≥17 U/ml, respectively, which was associated with allograft injury and graft failure (41, 42). Banasik et al. established the cut-off threshold of AT1R-Abs and ETAR-Abs of ≥9 U/ml and found higher risk of developing graft failure (9, 10). Moreover, in another study by Hiemann et al., in heart transplant recipients, the established cut-off threshold was ≥16 U/ml for the ETAR- and AT1R-Abs (12). In our study, we have set a cut-off threshold of >10 U/ml for both AT1R- and ETAR-Abs, and found 51% and 44% patients positive for ETAR-Abs and AT1R-Abs, respectively, at baseline.
Primary results of ATHENA study showed that EVR + reduced CNI is efficient, effective, and safe (good preservation of renal function and significant reduction of CMV and BKV infections in the EVR arm) (26). In addition to these results, the substudy presented here indicates that preformed non-HLA Abs have no correlation on clinical outcome. However, proportion of patients positive for non-HLA Abs from baseline to M12 reduced to a higher extent in EVR/TAC (AT1R-Abs: 42.9% to 17.7%; ETAR-Abs: 51.6% to 23.3%) compared to MPA/TAC (AT1R-Abs: 40.8% to 28.1%; ETAR-Abs: 46.7% to 34.7%) where it decreased from baseline to M6 but then increased slightly from M6 to M12. A possible explanation may be the specific ability of mTOR inhibitors to downregulate B-cells. In a comparative analysis of action of EVR and MPA on B-cell proliferation and differentiation into plasma cells, it was found that while MPA suppressed cell proliferation during initial phase of B-cell immune reaction, EVR could act in both early as well as later phase (43). A study showed that mTOR inhibitor reduced alloantibody production in transplant recipients via direct inhibition of alloprimed B cells while sparing the CD8+ antibody-suppressing T cells, and delayed graft rejection in both low and high alloantibody-producers (44). A recent study on molecular mechanism of action showed that non-HLA Abs targeting AT1R and ETAR induce endothelial injury via activation of PI3K/mTOR signaling, and the mTOR inhibitor, rapamycin abolish the activation of mTORC1 and mTORC2 after long term treatment with receptor antibodies. Thus, treatment with combination of mTOR inhibitors and receptor blockers may seem a future therapeutic approach in patients with non-HLA Abs-mediated allograft rejection (1). In line with the primary ATHENA study results (26), eGFR improvement was noted with MPA + TAC than in EVR groups. However, the number of patients was too low to draw any final conclusion. Liu et al. conducted a study in 79 recipients to evaluate the correlation between levels of AT1R- and ETAR-Abs and post-operative outcomes in KTx recipients. This study reported that the mean eGFR of patients was reduced significantly from 52.49 ± 24.96 to 42.58 ± 11.18 in the AT1R-Abs group and the AT1R- plus ETAR-Abs group showed a much lower eGFR (34.79 ± 15.27) (p = 0.008) (45). Various studies have reported that AT1R is an independent risk factor for graft loss and decline in eGFR (2, 8, 46). Hernández-Méndez et al. reported in a study of 111 patients that in KTx patients with AT1R-Abs, a lower median eGFR was observed compared to KTx patients with no Abs at 12 months (47). Our study also examined the patients solely positive for ETAR-Abs and evaluated the impact on clinical outcomes after transplantation. The findings showed that the ETAR-Abs were probably neutral, without any influence on the patients' clinical features.
The HLA antibodies may also play an important role in transplant rejection and patients with both HLA and non-HLA antibodies have been reported to have poor outcomes and lower graft survival (42). A separate substudy of ATHENA evaluated the effect of EVR vs. MPA in combination with reduced CNI on the formation of HLA antibodies and graft outcome in KTx patients (48). The results showed that incidence of de novo donor specific antibodies (DSA) was extremely low in all treatment groups. Similar to findings found for non-HLA, de novo DSA or preformed HLA antibodies had no influence on clinical outcomes in the first 12 months after KTx, irrespective of EVR or MPA exposure.
The main limitation of this study was that it was conducted for 12 months and there is lack of long-term data. The study was a post-hoc analysis and was not powered to detect statistically significant differences in clinical outcomes. A lack of differences between the groups may be due to small sample size. Other patient-related or immunological factors can contribute and additional research is needed to corroborate our findings and establish diagnostic or possibly targeted therapeutics.
In conclusion, given the existence of non-HLA Abs in up to 50% of patients and that preformed non-HLA Abs in all three immunosuppression regimens have no influence on clinical outcome, neither in terms of BPAR, AMR nor renal function, this study clearly demonstrated that the chosen combinations of immunosuppressants are safe and underscores the evidence of a minimal exposure of CNI for better patient management. However, further research on ETAR- and AT1R-Abs monitoring might be of interest in order to characterize immunological risk profiles in renal transplant recipients with high immunological risk and to identify potential immunologic events such as microvasculopathy and/or graft failure.
Data availability statement
Anonymized patient-level data from clinical trials may be shared by Novartis in a consortium called ClinicalStudyDataRequest.com (CSDR) in accordance with Novartis' policy for sharing clinical trial data. Requests to access the datasets should be directed to https://www.clinicalstudydatarequest.com/Study-Sponsors/Study-Sponsors-Novartis.aspx.
Ethics statement
The studies involving humans were approved by Ärztekammer Hamburg, Geschäftsstelle der Ethik-Kommission, Weidestr. 122 b, 22083 Hamburg. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AP: Writing – original draft, Writing – review & editing, Formal Analysis, Investigation. WA: Writing – original draft, Writing – review & editing. VD: Writing – original draft, Writing – review & editing. IH: Formal Analysis, Investigation, Writing – original draft, Writing – review & editing. FT: Formal Analysis, Writing – original draft, Writing – review & editing. CS: Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. BS: Writing – original draft, Writing – review & editing. DD: Conceptualization, Writing – original draft, Writing – review & editing. JH: Writing – original draft, Writing – review & editing. CS: Methodology, Writing – original draft, Writing – review & editing. AE: Formal Analysis, Writing – original draft, Writing – review & editing. BN: Writing – original draft, Writing – review & editing, Conceptualization, Methodology.
Funding
The author(s) declare financial support was received for research and publication of this article.
This study was funded by Novartis Pharma GmbH, Nuremberg, Germany.
Acknowledgments
In memoriam DD, our dear friend and always inspiring colleague, who passed away much too early. We would like to thank all investigators and participants involved in this study. We would also like to thank Sushant Thakur and Sarabjeet Kaur (Novartis Healthcare Pvt. Ltd., Hyderabad, India) for providing medical writing support and editorial assistance in accordance with Good Publication Practice guidelines (GPP 2022 (ismpp.org).
Conflict of interest
WA received consulting honoraria from Novartis. IH was in the advisory board of Novartis and received honoraria for lectures from Takeda, Biotest, MSD, CareDx, Novartis, Astellas, Bayer, and Astra Zeneca. FT has received study honoraria from Novartis, Sanofi, Astellas, Alexion, Hexal, Chiesi, and Pfizer. BS received study honoraria and was in the advisory board of Novartis. JH, CS, and AE are employees of Novartis. BN was in the advisory board and received funding from Novartis.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frtra.2023.1273890/full#supplementary-material
References
1. Catar RA, Wischnewski O, Chen L, Heidecke H, Rutz C, Schulein R, et al. Non-HLA antibodies targeting angiotensin II type 1 receptor and endothelin-1 type A receptors induce endothelial injury via beta2-arrestin link to mTOR pathway. Kidney Int. (2022) 101(3):498–509. doi: 10.1016/j.kint.2021.09.029
2. Giral M, Foucher Y, Dufay A, Duong Van Huyen JP, Renaudin K, Moreau A, et al. Pretransplant sensitization against angiotensin II type 1 receptor is a risk factor for acute rejection and graft loss. Am J Transplant. (2013) 13(10):2567–76. doi: 10.1111/ajt.12397
3. Lefaucheur C, Viglietti D, Bouatou Y, Philippe A, Pievani D, Aubert O, et al. Non-HLA agonistic anti-angiotensin II type 1 receptor antibodies induce a distinctive phenotype of antibody-mediated rejection in kidney transplant recipients. Kidney Int. (2019) 96(1):189–201. doi: 10.1016/j.kint.2019.01.030
4. El Band JEK, Llorente S, Martinez-Garcia P, Alfaro R, Jimenez-Coll V, Boix F, et al. Evaluation of antibodies directed against two GPCRs, anti-AT1R and anti-ETAR, on kidney transplant outcome. Curr Protein Pept Sci. (2021) 22(10):745–57. doi: 10.2174/1389203722666210706163149
5. Sikorska D, Kaminska D, Catar R, Banasik M, Heidecke H, Schulze-Forster K, et al. Non-HLA antibodies in hand transplant recipients are connected to multiple acute rejection episodes and endothelial activation. J Clin Med. (2022) 11(3):833. doi: 10.3390/jcm11030833
6. O'Leary JG, Demetris AJ, Philippe A, Freeman R, Cai J, Heidecke H, et al. Non-HLA antibodies impact on C4d staining, stellate cell activation and fibrosis in liver allografts. Transplantation. (2017) 101(10):2399–409. doi: 10.1097/TP.0000000000001853
7. Kardol-Hoefnagel T, Otten HG. A comprehensive overview of the clinical relevance and treatment options for antibody-mediated rejection associated with non-HLA antibodies. Transplantation. (2021) 105(7):1459–70. doi: 10.1097/TP.0000000000003551
8. Banasik M, Boratynska M, Koscielska-Kasprzak K, Krajewska M, Mazanowska O, Kaminska D, et al. The impact of non-HLA antibodies directed against endothelin-1 type A receptors (ETAR) on early renal transplant outcomes. Transpl Immunol. (2014) 30(1):24–9. doi: 10.1016/j.trim.2013.10.007
9. Banasik M, Boratynska M, Koscielska-Kasprzak K, Kaminska D, Bartoszek D, Zabinska M, et al. The influence of non-HLA antibodies directed against angiotensin II type 1 receptor (AT1R) on early renal transplant outcomes. Transpl Int. (2014) 27(10):1029–38. doi: 10.1111/tri.12371
10. Banasik M, Boratynska M, Koscielska-Kasprzak K, Kaminska D, Zmonarski S, Mazanowska O, et al. Non-HLA antibodies: angiotensin II type 1 receptor (anti-AT1R) and endothelin-1 type A receptor (anti-ETAR) are associated with renal allograft injury and graft loss. Transplant Proc. (2014) 46(8):2618–21. doi: 10.1016/j.transproceed.2014.09.029
11. Sorohan BM, Ismail G, Berechet A, Obrisca B, Constantinescu I, Maruntelu I, et al. The early impact of preformed angiotensin II type 1 receptor antibodies on graft function in a low immunological risk cohort of kidney transplant recipients. Transpl Immunol. (2021) 66:101389. doi: 10.1016/j.trim.2021.101389
12. Hiemann NE, Meyer R, Wellnhofer E, Schoenemann C, Heidecke H, Lachmann N, et al. Non-HLA antibodies targeting vascular receptors enhance alloimmune response and microvasculopathy after heart transplantation. Transplantation. (2012) 94(9):919–24. doi: 10.1097/TP.0b013e3182692ad2
13. Sorohan BM, Sinescu I, Tacu D, Bucsa C, Tincu C, Obrisca B, et al. Immunosuppression as a risk factor for De Novo angiotensin II type receptor antibodies development after kidney transplantation. J Clin Med. (2021) 10(22):5390. doi: 10.3390/jcm10225390
14. Butler CL, Hickey MJ, Jiang N, Zheng Y, Gjertson D, Zhang Q, et al. Discovery of non-HLA antibodies associated with cardiac allograft rejection and development and validation of a non-HLA antigen multiplex panel: from bench to bedside. Am J Transplant. (2020) 20(10):2768–80. doi: 10.1111/ajt.15863
15. See SB, Mantell BS, Clerkin KJ, Ray B, Vasilescu ER, Marboe CC, et al. Profiling non-HLA antibody responses in antibody-mediated rejection following heart transplantation. Am J Transplant. (2020) 20(9):2571–80. doi: 10.1111/ajt.15871
16. Dragun D, Catar R, Philippe A. Non-HLA antibodies in solid organ transplantation: recent concepts and clinical relevance. Curr Opin Organ Transplant. (2013) 18(4):430–5. doi: 10.1097/MOT.0b013e3283636e55
17. Tedesco-Silva H, Pascual J, Viklicky O, Basic-Jukic N, Cassuto E, Kim DY, et al. Safety of everolimus with reduced calcineurin inhibitor exposure in De Novo kidney transplants: an analysis from the randomized TRANSFORM study. Transplantation. (2019) 103(9):1953–63. doi: 10.1097/TP.0000000000002626
18. Hurvitz SA, Andre F, Jiang Z, Shao Z, Mano MS, Neciosup SP, et al. Combination of everolimus with trastuzumab plus paclitaxel as first-line treatment for patients with HER2-positive advanced breast cancer (BOLERO-1): a phase 3, randomised, double-blind, multicentre trial. Lancet Oncol. (2015) 16(7):816–29. doi: 10.1016/S1470-2045(15)00051-0
19. Merli M, Ferrario A, Maffioli M, Arcaini L, Passamonti F. Everolimus in diffuse large B-cell lymphomas. Future Oncol. (2015) 11(3):373–83. doi: 10.2217/fon.14.264
20. Baur B, Oroszlan M, Hess O, Carrel T, Mohacsi P. Efficacy and safety of sirolimus and everolimus in heart transplant patients: a retrospective analysis. Transplant Proc. (2011) 43(5):1853–61. doi: 10.1016/j.transproceed.2011.01.174
21. Mallat SG, Tanios BY, Itani HS, Lotfi T, McMullan C, Gabardi S, et al. CMV And BKPyV infections in renal transplant recipients receiving an mTOR inhibitor-based regimen versus a CNI-based regimen: a systematic review and meta-analysis of randomized, controlled trials. Clin J Am Soc Nephrol. (2017) 12(8):1321–36. doi: 10.2215/CJN.13221216
22. Nashan B, Gaston R, Emery V, Saemann MD, Mueller NJ, Couzi L, et al. Review of cytomegalovirus infection findings with mammalian target of rapamycin inhibitor-based immunosuppressive therapy in de novo renal transplant recipients. Transplantation. (2012) 93(11):1075–85. doi: 10.1097/TP.0b013e31824810e6
23. Nashan B. Early clinical experience with a novel rapamycin derivative. Ther Drug Monit. (2002) 24(1):53–8. doi: 10.1097/00007691-200202000-00010
24. Hauser IA, Marx S, Sommerer C, Suwelack B, Dragun D, Witzke O, et al. Effect of everolimus-based drug regimens on CMV-specific T-cell functionality after renal transplantation: 12-month ATHENA subcohort-study results. Eur J Immunol. (2021) 51(4):943–55. doi: 10.1002/eji.202048855
25. Radtke J, Dietze N, Spetzler VN, Fischer L, Achilles EG, Li J, et al. Fewer cytomegalovirus complications after kidney transplantation by de novo use of mTOR inhibitors in comparison to mycophenolic acid. Transpl Infect Dis. (2016) 18(1):79–88. doi: 10.1111/tid.12494
26. Sommerer C, Suwelack B, Dragun D, Schenker P, Hauser IA, Witzke O, et al. An open-label, randomized trial indicates that everolimus with tacrolimus or cyclosporine is comparable to standard immunosuppression in de novo kidney transplant patients. Kidney Int. (2019) 96(1):231–44. doi: 10.1016/j.kint.2019.01.041
27. Bussalino E, Marsano L, Parodi A, Russo R, Massarino F, Ravera M, et al. Everolimus for BKV nephropathy in kidney transplant recipients: a prospective, controlled study. J Nephrol. (2021) 34(2):531–8. doi: 10.1007/s40620-020-00777-2
28. Netti GS, Infante B, Troise D, Mercuri S, Panico M, Spadaccino F, et al. mTOR inhibitors improve both humoral and cellular response to SARS-CoV-2 messenger RNA BNT16b2 vaccine in kidney transplant recipients. Am J Transplant. (2022) 22(5):1475–82. doi: 10.1111/ajt.16958
29. Cibrik D, Silva HT Jr., Vathsala A, Lackova E, Cornu-Artis C, Walker RG, et al. Randomized trial of everolimus-facilitated calcineurin inhibitor minimization over 24 months in renal transplantation. Transplantation. (2013) 95(7):933–42. doi: 10.1097/TP.0b013e3182848e03
30. Sommerer C, Suwelack B, Dragun D, Schenker P, Hauser IA, Nashan B, et al. Design and rationale of the ATHENA study–A 12-month, multicentre, prospective study evaluating the outcomes of a de novo everolimus-based regimen in combination with reduced cyclosporine or tacrolimus versus a standard regimen in kidney transplant patients: study protocol for a randomised controlled trial. Trials. (2016) 17:92. doi: 10.1186/s13063-016-1220-9
31. Xia Y, Kellems RE. Angiotensin receptor agonistic autoantibodies and hypertension: preeclampsia and beyond. Circ Res. (2013) 113(1):78–87. doi: 10.1161/CIRCRESAHA.113.300752
32. Dragun D. Agonistic antibody-triggered stimulation of angiotensin II type 1 receptor and renal allograft vascular pathology. Nephrol Dial Transplant. (2007) 22(7):1819–22. doi: 10.1093/ndt/gfm072
33. Dragun D, Muller DN, Brasen JH, Fritsche L, Nieminen-Kelha M, Dechend R, et al. Angiotensin II type 1-receptor activating antibodies in renal-allograft rejection. N Engl J Med. (2005) 352(6):558–69. doi: 10.1056/NEJMoa035717
34. Wiwattanathum P, Ingsathit A, Thammanichanond D, Worawichawong S. Successful treatment of anti-angiotensin II type 1 receptor antibody-associated rejection in kidney transplantation: a case report. Transplant Proc. (2018) 50(3):877–80. doi: 10.1016/j.transproceed.2017.11.027
35. Banasik M, Boratynska M, Nowakowska B, Halon A, Koscielska-Kasprzak K, Drulis-Fajdasz D, et al. C4d deposition and positive posttransplant crossmatch are not necessarily markers of antibody-mediated rejection in renal allograft recipients. Transplant Proc. (2007) 39(9):2718–20. doi: 10.1016/j.transproceed.2007.08.064
36. Banasik M, Klinger M. Chronic allograft nephropathy–immunologic and nonimmunologic factors. Ann Transplant. (2006) 11(1):7–10.17025023
37. Mao Q, Terasaki PI, Cai J, Briley K, Catrou P, Haisch C, et al. Extremely high association between appearance of HLA antibodies and failure of kidney grafts in a five-year longitudinal study. Am J Transplant. (2007) 7(4):864–71. doi: 10.1111/j.1600-6143.2006.01711.x
38. Nowanska K, Wisnicki K, Kuriata-Kordek M, Krajewska M, Banasik M. The role of endothelin II type A receptor (ETAR) in transplant injury. Transpl Immunol. (2022) 70:101505. doi: 10.1016/j.trim.2021.101505
39. Li F, Wei J, Valenzuela NM, Lai C, Zhang Q, Gjertson D, et al. Phosphorylated S6 kinase and S6 ribosomal protein are diagnostic markers of antibody-mediated rejection in heart allografts. J Heart Lung Transplant. (2015) 34(4):580–7. doi: 10.1016/j.healun.2014.09.047
40. Gabardi S, Baroletti SA. Everolimus: a proliferation signal inhibitor with clinical applications in organ transplantation, oncology, and cardiology. Pharmacotherapy. (2010) 30(10):1044–56. doi: 10.1592/phco.30.10.1044
41. Pearl MH, Chen L, ElChaki R, Elashoff D, Gjertson DW, Rossetti M, et al. Endothelin type A receptor antibodies are associated with angiotensin II type 1 receptor antibodies, vascular inflammation, and decline in renal function in pediatric kidney transplantation. Kidney Int Rep. (2020) 5(11):1925–36. doi: 10.1016/j.ekir.2020.09.004
42. Taniguchi M, Rebellato LM, Cai J, Hopfield J, Briley KP, Haisch CE, et al. Higher risk of kidney graft failure in the presence of anti-angiotensin II type-1 receptor antibodies. Am J Transplant. (2013) 13(10):2577–89. doi: 10.1111/ajt.12395
43. Haneda M, Owaki M, Kuzuya T, Iwasaki K, Miwa Y, Kobayashi T. Comparative analysis of drug action on B-cell proliferation and differentiation for mycophenolic acid, everolimus, and prednisolone. Transplantation. (2014) 97(4):405–12. doi: 10.1097/01.TP.0000441826.70687.f6
44. Avila CL, Zimmerer JM, Elzein SM, Pham T, Abdel-Rasoul M, Bumgardner GL. mTOR inhibition suppresses posttransplant alloantibody production through direct inhibition of alloprimed B cells and sparing of CD8 + antibody-suppressing T cells. Transplantation. (2016) 100(9):1898–906. doi: 10.1097/TP.0000000000001291
45. Liu C, Kang ZY, Yin Z, Xiao Y, Liu W, Zhao Y, et al. Levels of angiotensin II type-1 receptor antibodies and endothelin-1 type-A receptor antibodies correlate with antibody-mediated rejection and poor graft function in kidney-transplantation patients. Transpl Immunol. (2022) 74:101674. doi: 10.1016/j.trim.2022.101674
46. Lee J, Huh KH, Park Y, Park BG, Yang J, Jeong JC, et al. The clinicopathological relevance of pretransplant anti-angiotensin II type 1 receptor antibodies in renal transplantation. Nephrol Dial Transplant. (2017) 32(7):1244–50. doi: 10.1093/ndt/gfv375
47. Hernandez-Mendez EA, Arreola-Guerra JM, Morales-Buenrostro LE, Ramirez JB, Calleja S, Castelan N, et al. Pre-transplant angiotensin II type 1 receptor antibodies: a risk factor for decreased kidney graft function in the early post-transplant period? Clin Transpl. (2013) 343–50.25095527
48. Arns W, Philippe A, Ditt V, Hauser IA, Thaiss F, Sommerer C, et al. Everolimus plus reduced calcineurin inhibitor prevents de novo anti-HLA antibodies and humoral rejection in kidney transplant recipients: 12-month results from the ATHENA study. Front Transpl. (2023) 2:1264903. doi: 10.3389/frtra.2023.1264903
Keywords: non-human leukocyte antigen, everolimus, kidney transplantation, angiotensin II type 1 receptor, endothelin-1 type A receptor
Citation: Philippe A, Arns W, Ditt V, Hauser IA, Thaiss F, Sommerer C, Suwelack B, Dragun D, Hillen J, Schiedel C, Elsässer A and Nashan B (2023) Impact of everolimus plus calcineurin inhibitor on formation of non-HLA antibodies and graft outcomes in kidney transplant recipients: 12-month results from the ATHENA substudy. Front. Transplant. 2:1273890. doi: 10.3389/frtra.2023.1273890
Received: 16 August 2023; Accepted: 31 October 2023;
Published: 21 November 2023.
Edited by:
Mary S Hayney, University of Wisconsin-Madison, United StatesReviewed by:
Zeynep Kendi Çelebi, Başkent University, TürkiyeMiha Arnol, University Medical Centre Ljubljana, Slovenia
© 2023 Philippe, Arns, Ditt, Hauser, Thaiss, Sommerer, Suwelack, Dragun, Hillen, Schiedel, Elsässer and Nashan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aurélie Philippe aurelie.philippe@bih-charite.de Björn Nashan bjoern.nashan@gmail.com
 Aurélie Philippe
Aurélie Philippe Wolfgang Arns
Wolfgang Arns Vanessa Ditt4
Vanessa Ditt4  Friedrich Thaiss
Friedrich Thaiss Barbara Suwelack
Barbara Suwelack Björn Nashan
Björn Nashan