Abstract
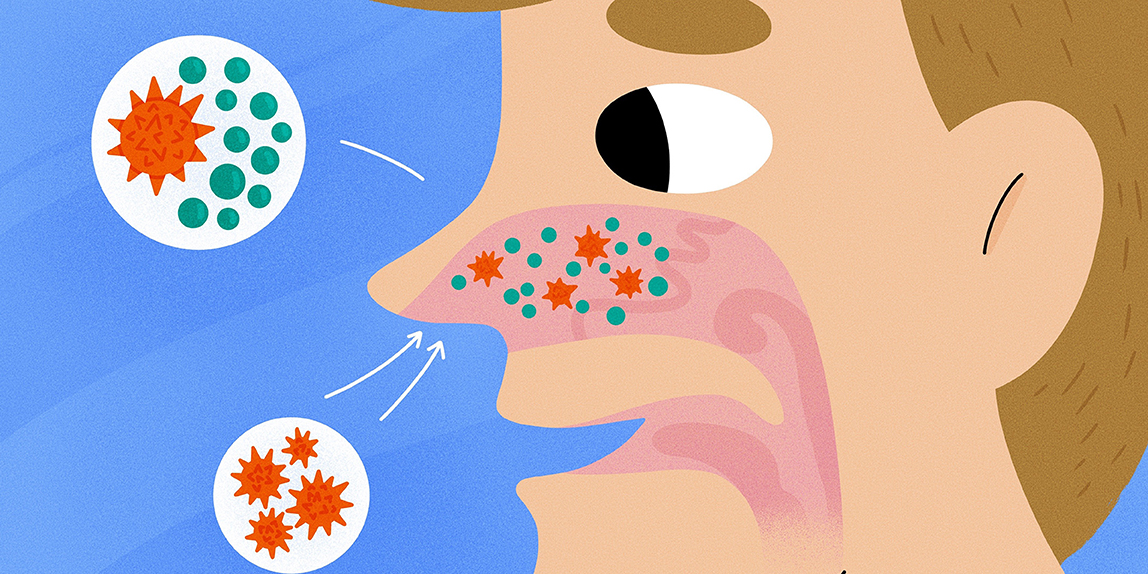
When people get infected with the SARS-CoV-2 virus, which causes COVID-19, why do some people get mildly sick while others get very sick? Although we know that SARS-CoV-2 enters the body via the nose and mouth, we do not fully understand how nasal cells respond to this infection or why some people get sicker than others. To answer these questions, we studied the immune response—the way the body fights infectious agents like bacteria and viruses—of cells from nasal swabs of healthy people and people with COVID-19. We found that nasal cells of very sick COVID-19 patients had a weaker immune response against the virus compared to that of cells from mildly sick patients, despite their virus levels being similar. Understanding how nasal cells interact with viruses and how their responses to infection are linked to how sick people get can help us better identify and manage the effects of viral infection.
Have you ever gotten sick at the same time as a friend, with a runny nose, cough, or chills, maybe by catching the same cold at school? A cold is actually a viral infection that can be caused by hundreds of different kinds of viruses, including coronaviruses. Even though you both caught the same cold, you might be sick for a week while your friend feels better in a few days. Why did you get sicker than your friend? Did your friend’s cells respond differently to infection than yours did? This difference in responses between individuals has also been seen with other respiratory viruses, including SARS-CoV-2 and the disease it causes, COVID-19 [1, 2]. We studied cells from nasal swabs of people without COVID-19 as well as people with mild or severe COVID-19, to better understand people’s varying responses to the virus and how these responses influence how sick people might get after infection.
Looking at the Nose Cell by Cell
To study the immune response of nasal cells infected with SARS-CoV-2, we used a technology called single-cell RNA sequencing (scRNA-seq) (Figure 1). While this may sound complicated, this technology simply lets us take a bunch of cells from nasal swabs and analyze them, cell by cell [3]. To illustrate, imagine a fruit salad with apples, pomegranates, and grapes. We can count how many of each type of fruit we have, determine which fruits have seeds, or compare how each fruit tastes. scRNA-seq lets us do something similar with mixtures of cells, allowing us to describe their similarities and differences by measuring what each cell is doing at a certain time. We do this by counting the mRNA molecules in individual cells, which tell us about that cell’s activity.
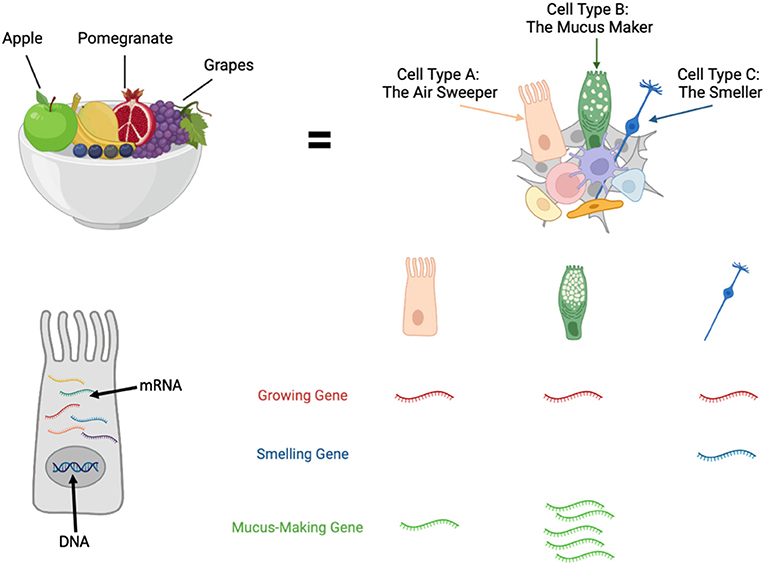
- Figure 1 - Using single-cell RNA sequencing, we can study gene expression on a cell-by-cell basis within a tissue or a mixture of cells.
- Counting the mRNA messages in each cell allows us to determine what kinds of cells are present and what those cells are doing. The scRNA-seq technology is similar to analyzing a fruit salad by studying the pieces of fruit one by one.
To make this clear, let us take a step back. Every human cell with a nucleus contains DNA—the genetic material passed down by our parents. Genes are bits of DNA that tell cells what to do—whether they should make a person’s eyes blue versus brown, or whether a cell should become a heart cell or a lung cell. The instructions in a cell’s genes are conveyed to the cell in the form of a message molecule called messenger RNA (mRNA). When a cell makes mRNA from a gene, it is said to be “expressing” that gene. The “single” part of “single-cell RNA sequencing” means we can study each cell one by one, while the “sequencing” part means we can read each cell’s mRNA to figure out what the cells are doing. Studying gene expression in this way can tell us what types of cells are present in a tissue, what they are doing there, and how healthy or sick those cells are. This powerful technology allowed us to see what nasal cells were doing in healthy and sick people.
We collected nasal swabs from over fifty people who visited the hospital (Figure 2). Swabs were classified based on whether the person had COVID-19 or not, and if they did, how bad they had it. We isolated cells from the swabs and used scRNA-seq to count how many specific RNA molecules each cell contained, as well as to read those messages to give us a look at their gene expression. This helped us determine how the nasal cells were responding to infection, known as their immune response. But what is an immune response, exactly?
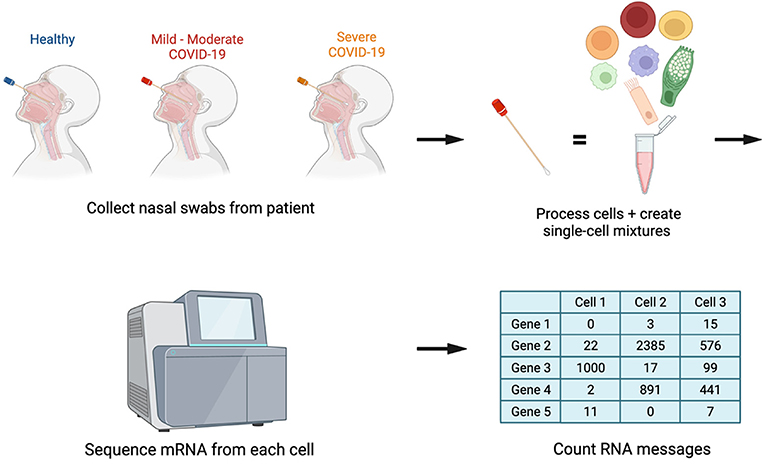
- Figure 2 - To study the immune responses of nasal cells from people with or without COVID-19, we collected nasal swabs from these individuals and processed the swabs to isolate the cells from them.
- The gene expression of individual cells within these mixtures was then analyzed using a machine called a sequencer, which counted each cell’s mRNA messages. The results tell us which cells were present and what those cells were doing.
What Is an Immune Response?
The immune response is the reaction the immune system mounts to protect a person exposed to potentially harmful organisms, like bacteria and viruses. The immune system recognizes certain “danger” proteins on the surfaces of these organisms, which signal that these organisms must be removed. You are probably familiar with the immune response that occurs when you get vaccinated against flu, for example. Vaccination trains the immune system to recognize and attack the virus before you actually catch it.
One of the first steps infected cells take is to release a substance called interferon, which tells other cells to fight back and stop the virus, thus “interfering” with its ability to spread. Interferon prompts cells to express certain genes, including virus-fighting genes called antiviral genes, which can help stop the virus from spreading and strengthen the immune response. In our work, we investigated what the immune response looked like in the nasal cells of healthy people and those fighting COVID-19, and whether there were any observable differences.
Investigating Cellular Responses to SARS-CoV-2 Infection
We used scRNA-seq to analyze the immune response of nasal cells from swabs taken from healthy people or people with mild or severe COVID-19, to try to understand why some people got very sick and others did not. In comparing gene expression, we found that cells from people who were mildly ill and those who were severely ill both showed higher levels of interferon-related antiviral genes compared to cells from healthy people. This illustrates that the infected cells were trying to defeat the virus, which is what we expect to happen. Cells from people with mild COVID-19 showed high levels of antiviral genes. However, cells from people with severe COVID-19 showed lower levels of these antiviral genes, even early on during the infection. In some cases, these cells even behaved like those from healthy patients—as if they were not fighting a virus at all! Because these cells were having difficulty responding to the virus, the immune response in these people was not very strong, which seemed to result in these individuals getting very sick. On the other hand, when the cells could fight back by initiating a strong immune response, individuals seemed to get only mildly sick.
You might be wondering, “What if the really sick people just had to fight off more virus than the slightly sick people?” Surprisingly, we found that even when the levels of virus were the same, individuals with severe COVID-19 still had a much weaker immune response overall (Figure 3). This might be because the nasal cells from individuals with severe COVID-19 are impaired in some way, preventing them from responding strongly to the virus through antiviral gene expression.
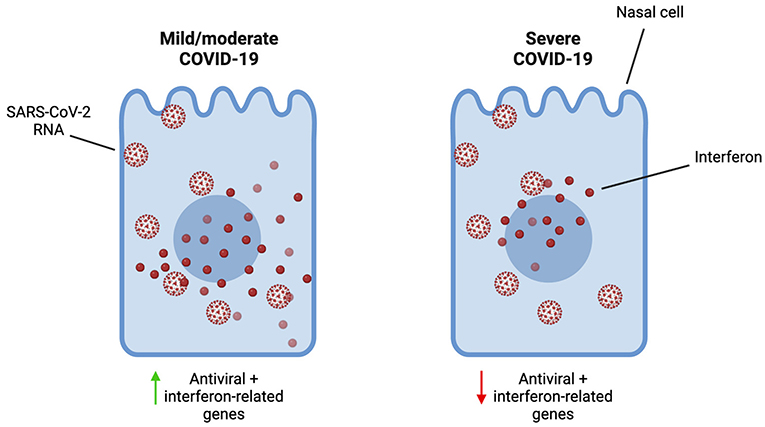
- Figure 3 - Despite having similar levels of SARS-CoV-2 RNA in the nose (meaning similar levels of virus), individuals with mild COVID-19 showed strong expression of antiviral and other interferon-related genes, while individuals with severe COVID-19 showed much lower expression of these genes.
- This signifies that the nasal cells of people who developed severe COVID-19 failed to mount a strong immune response to the virus.
We also wondered what types of nasal cells were getting infected with SARS-CoV-2. As we mentioned earlier, scRNA-seq let us determine which types of cells were present in the nasal swabs, based on their gene expression. We found that a large portion of the infected nasal cells were ciliated cells, goblet cells, and secretory cells. Ciliated cells are like cellular brooms that help sweep things out of the respiratory system, using tiny hair-like structures called cilia. Secretory and goblet cells secrete mucus, which helps trap viruses, bacteria, or allergens and move them out of the body. The fact that these cells were the ones infected most often might indicate that these cell types are especially good at helping the virus spread.
Although we are now aware of the differences in immune responses between healthy people and those experiencing varying severities of COVID-19, there are still unanswered questions waiting for curious minds like yours to help answer them. For instance, we still do not know why this difference in immune response is happening in the first place, whether this difference depends on other factors (like age), or why the interferon response varies so significantly between individuals. We also do not know how COVID-19 vaccines might influence this initial immune response, or how these responses might differ in other cell types or parts of the body besides the nose. More work on this immune response and the reasons why it might vary between individuals will need to be done by future scientists like you.
Conclusion
So, why do some people get mildly sick with COVID-19 while others get really sick? We think it has to do with how well their nasal cells can launch an immune response. In response to SARS-CoV-2, some individuals’ nasal cells cannot express enough antiviral and interferon-related genes, thus preventing them from ringing the alarm to alert other cells to fight. This results in a weakened immune response, which causes these people to get severely sick. However, some people’s nasal cells can launch a robust immune response, so they only get mildly sick.
As we learn more about viruses such as SARS-CoV-2 or influenza, it is important that we work to decipher the immune response on a cellular level, to better understand why and how people get sick. Studying how cells respond to viruses will not only help us learn more about the viruses themselves but might also teach us how to help people affected by them. Going forward, we hope that this work will lead to treatments that improve the lives of people dealing with viral infections.
Glossary
Single-Cell RNA Sequencing (scRNA-seq): ↑ A technology used to study cells’ behavior on a cell-by-cell basis, by studying their gene expression.
DNA: ↑ A molecule found in all living cells that contains genetic information instructing cells on what to do.
Gene: ↑ A specific part of DNA that contains instructions telling cells what to do or what type of cells to become.
Messenger RNA (mRNA): ↑ A molecule found in all living cells that is produced during gene expression.
Gene Expression: ↑ The process by which a gene’s information is expressed by a cell, where it is used to make RNA or protein that help that cell fulfill certain functions.
Immune Response: ↑ The reaction the body launches to recognize and defend itself against viruses, bacteria, and foreign substances.
Interferon: ↑ A substance made by the immune system that helps defend the body against viruses by stopping their spread, while signaling to other cells to do the same.
Antiviral Genes: ↑ Genes that help limit the spread of viruses within the body when expressed.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the authors of the original research paper for their scientific research on immune responses to SARS-CoV-2 infection. We especially thank the study participants and their families for making such contributions possible. Figures in this paper were made using BioRender.com.
Original Source Article
↑Ziegler, C. G. K., Miao, V. N., Owings, A. H., Navia, A. W., Tang, Y., Bromley, J. D., et al. 2021. Impaired local intrinsic immunity to SARS-CoV-2 infection in severe COVID-19. Cell 184: 4713–33.e22. doi: 10.1016/j.cell.2021.07.023.
References
[1] ↑ Guan, W. J., Ni, Z. Y., Hu, Y., Liang, W. H., Ou, C. Q., He, J. X., et al. 2020. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 382:1708–20. doi: 10.1056/NEJMoa2002032
[2] ↑ Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., Hu, Y., et al. 2020. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
[3] ↑ Kolodziejczyk, A. A., Kim, J. K., Svensson, V., Marioni, J. C., and Teichmann, S. A. 2015. The technology and biology of single-cell RNA sequencing. Mol. Cell 58:610–20. doi: 10.1016/j.molcel.2015.04.005