Identifying Barriers and Facilitators to the Improvement of Healthcare Delivery and Ethics in Two Cameroonian Neurosurgical Centers
- 1Faculty of Health Sciences, University of Buea, Buea, Cameroon
- 2Department, Association of Future African Neurosurgeons, Yaounde, Cameroon
- 3Neurosurgery Unit, Surgery Department, Douala General Hospital, Douala, Cameroon
- 4Neurosurgery Unit, Surgery Department, Laquintinie Hospital, Douala, Cameroon
- 5Faculty of Medicine and Biomedical Sciences, Yaounde, Cameroon
- 6College of Medicine, University of Ibadan, Ibadan, Nigeria
- 7Neurosurgery Unit, Surgery Department, Jason Sendwe General Provincial Hospital, Lubumbashi, Democratic Republic of Congo
- 8College of Health Sciences, University of Zimbabwe, Harare, Zimbabwe
- 9Neurosurgery Division, Faculty of Health Sciences, University of Bamenda, Bambili, Cameroon
Background: Low-and middle-income countries (LMICs) are disproportionately affected by neurosurgical burden of disease. This health inequity causes constraints in decision-making. Neurosurgical ethics helps us to assess the moral acceptability and effectiveness of clinical decisions. We aimed to assess ethical neurosurgical care and its effect on patient satisfaction in Cameroon.
Methods: Two questionnaires hosted on Google Forms were administered among inpatients and staff at two Cameroonian neurosurgery centers. The questionnaires covered the factors influencing health outcomes and ethics. Data were collected from November 11, 2020, to March 11, 2021 and analyzed with SPSS v 26 to generate non-parametric tests with a threshold of significance at 0.05.
Results: Seventy patients and twenty healthcare providers responded to the survey. Most patients faced financial hardship (57.1%; 95% CI = 45.7–68.6%), and felt that this affected the care they received (P = 0.02). Patients noticed changes in the care plan and care delivery attributable to the neurosurgical units' lack of resources. According to the patients and caregivers, these changes happened 31.0–50.0% of the time (42.9%, 95% CI = 5.7–21.4%). The majority of patients were pleased with their involvement in the decision-making process (58.6%; 95% CI = 47.1–70.0%) and felt their autonomy was respected (87.1%; 95% CI = 78.6–94.3%).
Conclusion: Multiple challenges to neurosurgical ethical care were seen in our study. Multimodal interventions based on the four ethical principles discussed are necessary to improve ethical neurosurgical decision-making in this low resource setting.
Introduction
The majority of low- and middle-income countries (LMICs) currently struggle to provide adequate neurosurgical services, with African countries disproportionately affected due to factors such as an insufficient number of neurosurgeons, inadequate healthcare infrastructure, and a paucity of equipment and funding (1). The neurosurgical workforce density in Africa is 1: 4,000,000 (2–4), while the average percentage of the population with access to neurosurgical services within a 2-h window is 25.3% in sub-Saharan Africa (5). These factors complicate the delivery of neurosurgical services to already underserved populations (6).
Challenges in decision-making arise due to a lack of standardized guidelines for neurosurgical techniques and management protocols, limited knowledge of surgical techniques, limited exposure to real time intraoperative decision making, and lack of guidelines regarding best practices for postoperative care (7, 8). Consideration of the ethical dimensions of decision-making is necessary to evaluate both the effectiveness and equitability of neurosurgical decisions, particularly as technology and care paradigms advance. Traditionally, ethical analyses are based on four key principles: respect for patient autonomy, beneficence, non-maleficence, and justice according to Beauchamp and Childress (9). Respect for patient autonomy refers to the right of the patient to make informed decisions about their medical care. The principle of beneficence is the obligation of physicians to act for the benefit of the patient, while non-maleficence involves avoiding the causation of harm. Justice refers to the balancing risks and benefits, ranging from the fair treatment of individuals to equitable allocation of healthcare resources (9).
To the best of our knowledge, no existing study has examined ethical decision-making within neurosurgery in an under-resourced setting. This study aims to assess ethical dimensions in the delivery of neurosurgical care in Cameroon and their relationship with patient satisfaction and outcomes. Our study will inform strategies for optimizing ethical decision-making in the delivery of neurosurgical care within the constraints of LMICs.
Methods
Study Setting
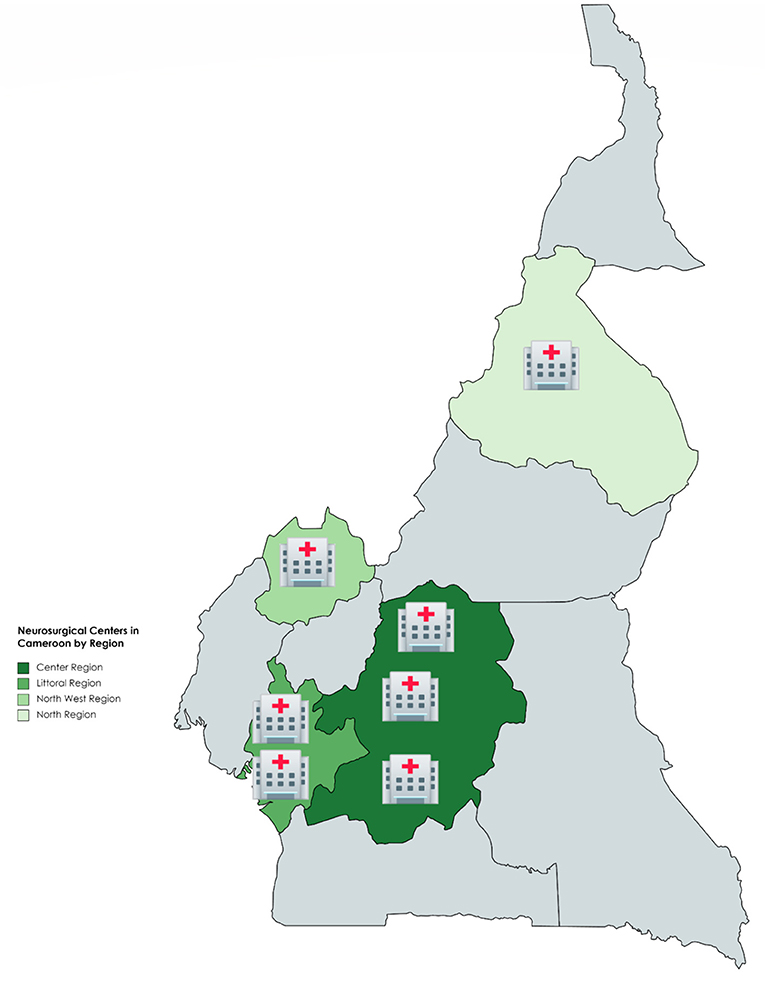
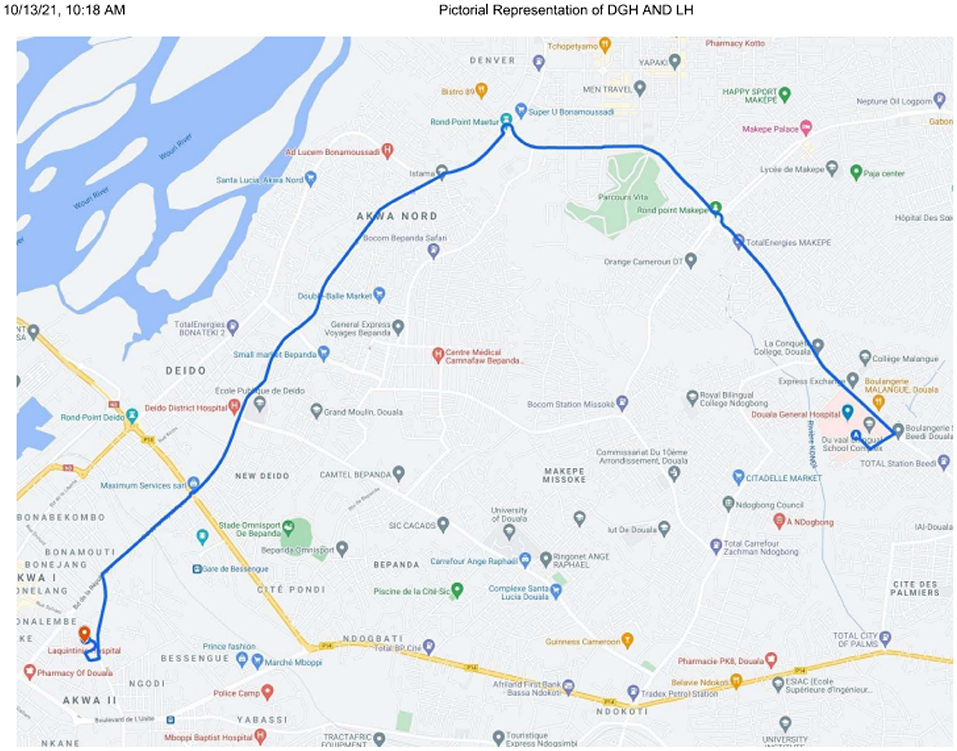
This study was carried out in two Cameroonian neurosurgical centers—Laquintinie Hospital (LH) and Douala General Hospital (DGH). Figure 1 demonstrates the neurosurgical centers in Cameroon by region. In descending order, the Center Region has three: Yaounde General Hospital, Central Hospital Yaounde and Center Emergency Yaounde; Littoral Region:DGH and LH; North West Region: Bamenda General Hospital; North Region: Garoua Regional Hospital. The distance between Douala and Garoua, Bamenda and Yaounde in descending order is 1,338.4, 321.2, and 232.7 km, respectively. Figure 2 illustrates a pictorial representation of DGH and LH. The distance between DGH and LH is 10.2 km. Health facilities in Cameroon are organized according to categories, with category one as most well-equipped and category seven as least equipped. The level of equipment of each of these neurosurgical centers was based on the availability and maintenance of the equipment used to manage the neurosurgical pathologies common in this setting. Douala General Hospital is a category one hospital, while Laquintinie Hospital is a category 2 facility (10).
Study Design
We conducted a cross-sectional survey among LH and DGH neurosurgery inpatients and personnel. This included patients who came to the surgical outpatient department for follow-up consultations after benefitting from surgical management of their neurosurgical disease and hospitalized patients in the postoperative period following a neurosurgical intervention. We did not include patients who were managed conservatively and medically for their neurosurgical diseases.
Study Period and Duration
Data were collected from November 11, 2020, to March 11, 2021.
Data Collection
Data were collected using Google Forms (Google LLC, California, USA) from November 11, 2020, to March 11, 2021.
Self-administered questionnaires designed in French and English were distributed among patients and healthcare workers who met the inclusion criteria. The patient questionnaire had six categories: sociodemographics (age, gender, level of education), resource allocation, variations in the standard of care, levels of satisfaction with the continuity of care and follow-up, cultural awareness, and disclosure of informed consent. The healthcare worker questionnaire had six categories: clinical roles, resource allocation, availability of resources, variations in the standard of care intraoperatively and postoperatively, continuity of care and follow-up, patient and procedure selection, cultural awareness, and disclosure and informed consent. The healthcare providers were also prompted to indicate other barriers and facilitators not mentioned in the questionnaire. Below is the patient and care provider's survey.
With respect to the ethical principles by Beauchamp and Childress, the survey was structured as follows: the third and fourth parts of the patient's survey evaluated maleficence and beneficence in neurosurgical care and the fifth part of the patient's survey measured autonomy. Justice was evaluated in parts of the second and third sections of the provider's survey.
Frequency, importance, and satisfaction were evaluated using Likert scales. Frequency was subdivided into: never (i.e., 0.0% of the time), occasionally (i.e., 1–30.0% of the time), sometimes (i.e., 31.0–50.0% of the time), usually (i.e., 51.0–80.0% of the time), and always (i.e., 81.0–100.0% of the time). Importance was subdivided into: very unimportant (0.0% importance), somewhat unimportant (1.0–30.0% importance), neutral (31.0–50.0% importance), somewhat important (51.0–80.0% importance), and very important (81.0–100.0% importance). Similarly, satisfaction was divided into very unsatisfied (0.0% satisfaction), unsatisfied (1–30% satisfaction), neutral (31–50% satisfaction), satisfied (51–80% satisfaction)n and very satisfied (81–100% satisfaction).
Data Analysis
Data were analyzed with SPSS v 26 to generate non-parametric tests with a threshold of significance at 0.05. Categorical quantitative sociodemographic data and responses were computed as frequencies and percentages, while age was computed as a mean with a 95% confidence interval. Data regarding patient information, resource availability, service delivery, and patient satisfaction were compared between the hospitals (DGH vs. LH) and healthcare provider roles (physician vs. nursing and operating room staff). Responses to the open-ended questions were organized into themes by the first and senior authors. The interrater reliability (96.0%) was calculated using Cohen's kappa.
Ethical Approval
The institutional review boards approved this study of DGH and LH (Ref 19AR/MINSANTE/HGD/DM/01/21 and 06394/AS/MINSANTE/DHL/CM). Patient consent for participation was obtained.
Results
Seventy patients and twenty healthcare providers responded to the survey. This corresponds to response rates of 31.8 and 71.4%, respectively. The mean age of the patients was 40.6 (95% CI = 36.2–45.3) years. Most of them were male (74.3%; 95% CI = 64.3–84.3%), and few had attained tertiary education (17.1%; 95% CI = 8.6–27.1%). Half of the healthcare providers were nurses (50.0%; 95% CI = 30.0–70.0%) (Table 1).
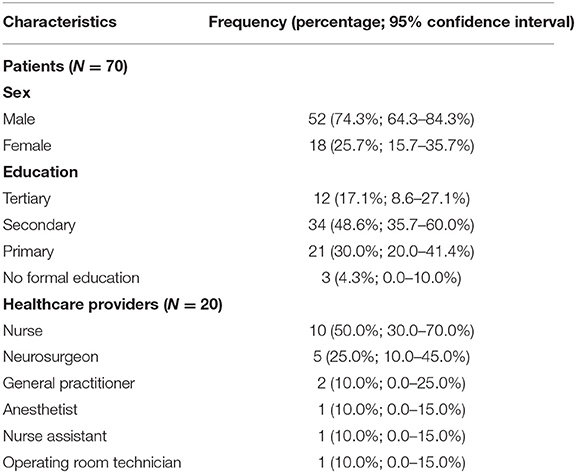
Table 1. Sociodemographic characteristics of patients and healthcare providers that responded to the survey.
Barriers to Care—Patient Perspective
Most patients faced financial hardship (57.1%; 95% CI = 45.7–68.6%), and they felt this stress affected the care they received (P = 0.02). Similarly, more than half of the patients spent between 80 and 99% of their annual household income on neurosurgical care-related expenses (54.3%; 95% CI = 42.9–65.7%) (Figure 3). As a result, 82.9% (95% CI = 72.9–91.4%) had to borrow or crowdfund money for their neurosurgical care expenses. Patients at LH were less likely to face financial hardship (OR = 5.33; 95% CI = 1.16–18.04; P = 0.03) and to borrow or crowdfund for their health expenses (OR = 6.15; 95% CI = 1.48–21.00; P = 0.02).
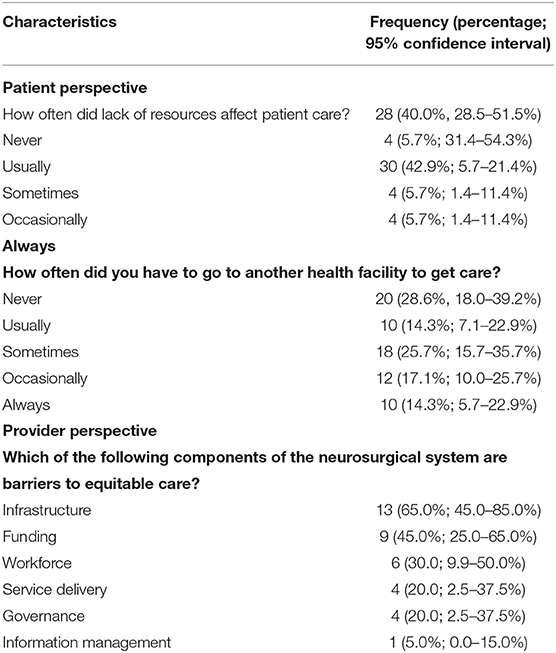
The patients noticed changes in the care plan and care delivery attributable to the neurosurgical units' lack of resources. These changes referred to alterations in the initial care plan midway its execution due to a discovery that some resources were not there and an initial divergence from a preferred plan because of lack of resources. According to the patients and caregivers, these changes happened 31.0–50.0% of the time (42.9%, 95% CI = 5.7–21.4%). Only 20 patients (28.6%, 95% CI = 18.0–39.2%) got all the needed services at one of the study sites. The other patients had to go to another facility to get care. DGH patients were less likely to move from one hospital to another because of a lack of resources (25.0 vs. 32.4%; P = 0.01).
Barriers to Care—Provider Perspective
Healthcare providers felt the greatest barriers to equitable access to care at the system level were lack of infrastructure (n = 13; 65.0%; 95% CI = 45.0–85.0%) and funding (n = 9; 45.0%; 95% CI = 25.0–65.0%) (Table 2).
Suboptimal infrastructures influenced their decision-making by relegating their expertise and implementing the standard of care guidelines after resource availability considerations (80.0%; 95% CI = 62.5–97.5%). Other significant determinants of care delivery included: case type and experience (Figure 4).
Patient Information
The majority of patients were pleased with their involvement in the decision-making process (58.6%; 95% CI = 47.1–70.0%) and felt their autonomy was respected (87.1%; 95% CI = 78.6–94.3%). Unfortunately, 51.4% (95% CI = 41.4–64.3%) did not receive enough information about the role and side effects of their prescribed medications. At discharge, only 70.0% (95% CI = 58.6–80.0%) of patients felt they had received comprehensive and digestible information on their management's next steps. Providers reported communicating information about the disease, therapeutic options, and therapy goals with patients and caregivers (85.0%; 95% CI = 70.0–100.0%). Despite sharing information with the patients and caregivers, healthcare providers reported communication challenges. These included fear of the unknown for patients and caregivers due to the uncertainty of the eventual outcome (55.0%; 95% CI = 35.0–75.0%), an inability for patients and caregivers to understand explanations (5.0%; 95% CI = 0.0–15.0%), and disagreements about the best course of action between patients and their families (5.0%; 95% CI = 0.0–15.0%).
Patient Satisfaction
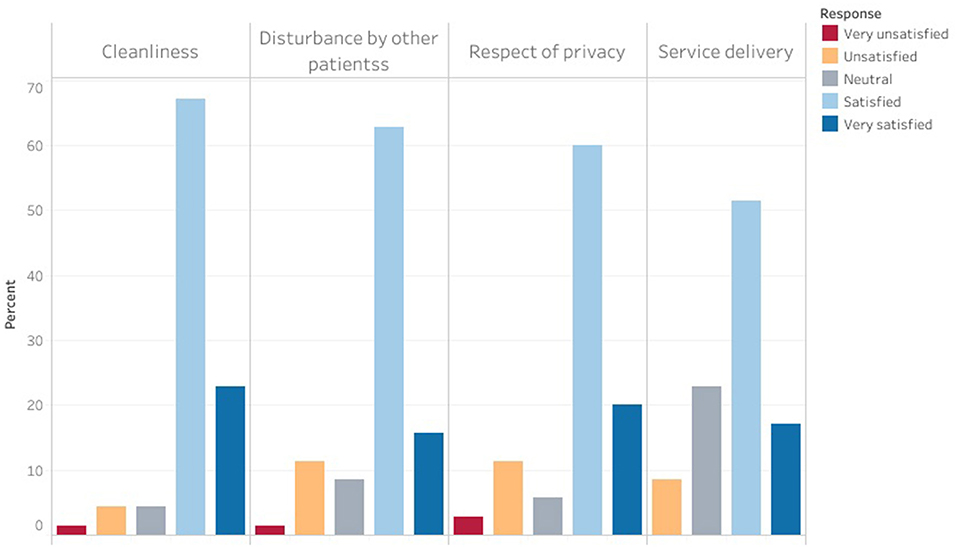
Patients and caregivers were generally satisfied with the service delivery and hospital environment (Figure 5).
Most providers reported regularly evaluating their patients (85.0%; 95% CI = 65.0–100.0%) especially in the postoperative period (90.0%; 95% CI = 75.0–100.0%). Also, they felt confident in their ability to recognize postoperative complications (95.0%; 95% CI = 85.0–100.0%).
With respect to the ethical principles by Beauchamp and Childress, we found that the principles of beneficence and maleficence were respected because most of the patients were satisfied with the service delivery and hospital environment. However, a good number of them felt their financial hardship affected the care they received. The principle of autonomy was respected as most of the patients were pleased with their involvement in the decision making process and most felt that their autonomy was respected.
Care providers had difficulties implementing the principle of Justice due to a lack of infrastructure and funding. In spite of this, they reported regularly communicating with their patients and following them up.
DGH patients were less likely to move from one hospital to another because most of the infrastructure and resources needed by the care providers were more available in DGH.
Discussion
In this study, we identified the determinants of ethical service delivery in two Cameroonian neurosurgery centers. To the best of our knowledge, this is the first study examining ethical dimensions of neurosurgical care in LMICs. Some patients observed changes in the care plan and services delivered due to a lack of resources. As a result, a quarter of patients transferred from one health facility to another when imaging services and medications were unavailable at one of the two neurosurgical centers. The proportion of patients who were required to transfer was lower among patients at DGH than those at LH. This is because most of the infrastructure and resources needed by the care providers were more available in DGH.
Healthcare providers equally reported that lack of infrastructure and funding adversely impacted neurosurgical care.
Information Provision and Informed Consent
Most patients did not understand the information they were given. This contrasted with the perception of healthcare providers, who reported communicating adequate information on the disease, therapeutic options, and treatment goals to patients and caregivers. Healthcare workers attributed unmet patient information needs to a lack of understanding on the part of patients. However, poor patient comprehension and low recall, accentuated further by low educational attainment, are likely responsible for this discrepancy (11, 12). Patient informational needs are frequently unmet, particularly regarding prognosis and follow-up after surgery and surgeon experience (13, 14). These findings highlight the need for neurosurgeons to remain aware of the discrepancy between their conceptualization of patient understanding and actual patient understanding, recognize common barriers to patient understanding, and attempt to minimize the effect of these barriers within the context of a patient encounter (11, 15).
Most patients reported their autonomy was respected, and were satisfied with their involvement in the decision-making process. Greater patient involvement in decision-making decreases patient anxiety and increases patient satisfaction (15). Current paradigms of patient involvement in neurosurgical decision-making focus on communication within consultations and the utilization of information conveyed by providers to decide regarding care (16). The informed consent process involves presenting the patient with information regarding their condition, possible treatments with associated risks and benefits, alternatives, and the risks and benefits of pursuing no treatment (17). Baseline patient health literacy and informational needs should guide discussions (17). Specialized interventions, such as specialized checklists for consent forms, question prompts, educational and interactive websites, and visual aids, are also necessary to facilitate patient understanding during the informed consent process (17). Augmented communication strategies, including providing quantifiable measures of success and risk, organizing the decision into a simple visual algorithm, utilizing methods to assess patient understanding such as teach-backs, and ensuring enough time for questions will optimize the informed consent process (17–19).
Together, these factors may improve patient understanding of their condition and treatment options, promoting patient-centered care and greater patient satisfaction. Importantly, informed consent is a continual process that requires continual information provision, assessment of patient understanding, and correction of misconceptions across the duration of care (17, 20, 21).
Ethical Decision-Making in Low Resource Settings
Numerous strategies exist for improving ethical decision-making in low resource settings. Institutions in low resource settings can employ a series of simple yet far-reaching interventions. These include creating a set of ethical standards with clear guidelines regarding best practices, increasing awareness regarding common ethical issues, analyzing ethical examples and employing counterexamples to train trainees and neurosurgeons in how to conceptualize ethical decisions, basing the discussions of cases on objective information rather than value judgments, and using cases to continually refine the approach of neurosurgeons to ethical decision-making (22–24). A novel concept is appointing “ethical champions,” who are individuals in institutions who are responsible for creating ethical standards and maintaining ethical oversight of care practices, to actively guide ethical decision-making while maintaining consideration of limited resources (21). Ethical champions use “ethical frames” to increase team ethical awareness and reduce moral disengagement and “business frames” depending on the perceived effect of the ethical decision on factors such as resource allocation (21). In any case, ethical decision-making must hold principles of respect for patient autonomy, beneficence, non-maleficence, and justice as foundational.
Limitations
This study had limitations. First, the study was conducted at the height of the COVID-19 pandemic, perhaps positively skewing patient responses given they received medical care during a challenging time. Second, we used a convenience sampling method which led to a small sample size, perhaps leading to excessive variability in survey responses. We also reported 95% confidence intervals to account for potential variability. Medical staff who did not respond were neuro-nurses and neuro anesthetists and patient caregivers may have been unwilling to participate given emotional stress, perhaps introducing non-response bias. In an effort to increase the response rate, we tried contacting the staff in person and on the phone at presumably convenient times and attempted to communicate clearly with caregivers and patients when they were visibly less stressed. Despite the aforementioned limitations, this study provides novel insight into ethical neurosurgical decision-making in Cameroon that may inform practices in other similar contexts.
Conclusion
We identified multiple challenges to ethical neurosurgical care in two Cameroonian centers. Lack of resources affected service delivery, and patients had poor comprehension and recall of information conveyed to them by neurosurgeons. Specialized interventions are necessary to improve the informed consent process, while comprehensive measures to expand the application of ethical thinking to clinical encounters may improve ethical neurosurgical decision-making in low resource settings. These measures should be instituted across all levels of care delivery. Given the ethical challenges faced by providers in low-resource settings exhibit substantial overlap, our findings may guide best practices for ethical decision-making in LMICs.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Dewan MC, Rattani A, Fieggen G, Arraez MA, Servadei F, Boop FA, et al. Global neurosurgery: the current capacity and deficit in the provision of essential neurosurgical care. Executive summary of the global neurosurgery initiative at the program in global surgery and social change. J Neurosurg. (2018) 130:1055–64. doi: 10.3171/2017.11.JNS171500
2. Attebery JE, Mayegga E, Louis RG, Chard R, Kinasha A, Ellegala DB. Initial audit of a basic and emergency neurosurgical training program in rural Tanzania. World Neurosurg. (2010) 73:290–5. doi: 10.1016/j.wneu.2010.02.008
3. Mansouri A, Chan V, Njaramba V, Cadotte DW, Albright AL, Bernstein M. Sources of delayed provision of neurosurgical care in a rural Kenyan setting. Surg Neurol Int. (2015) 6:32. doi: 10.4103/2152-7806.152141
4. Rabiu TB, Adetunmbi B. Posttraumatic seizures in a rural nigerian neurosurgical service. World Neurosurg. (2017) 104:367–71. doi: 10.1016/j.wneu.2017.04.133
5. Punchak M, Mukhopadhyay S, Sachdev S, Hung Y-C, Peeters S, Rattani A, et al. Neurosurgical care: availability and access in low-income and middle-income countries. World Neurosurg. (2018) 112:e240–54. doi: 10.1016/j.wneu.2018.01.029
6. Amadio JP. Neurosurgery ethics: perspectives from the field, circa 2015. AMA J Ethics. (2015) 17:3–5. doi: 10.1001/virtualmentor.2015.17.1.fred1-1501
7. Fezeu F, Ramesh A, Melmer PD, Moosa S, Larson PS, Henderson Jr F. Challenges and solutions for functional neurosurgery in developing countries. Cureus. (2018) 10:e3314. doi: 10.7759/cureus.3314
8. Gandy K, Castillo H, Rocque BG, Bradko V, Whitehead W, Castillo J. Neurosurgical training and global health education: systematic review of challenges and benefits of in-country programs in the care of neural tube defects. Neurosurg Focus. (2020) 48:E14. doi: 10.3171/2019.12.FOCUS19448
9. Beauchamp TL Beauchamp Beauchamp P of P SRS at the KI of ETL Childress JF Childress Childress UP HP of EJF. Principles of Biomedical Ethics. Michigan: Oxford University Press (2001). 470 p.
10. Health in Cameroon. In: Wikipedia (2021). Available online at: https://en.wikipedia.org/w/index.php?title=Health_in_Cameroon&oldid=998938516 (accessed June 19, 2021).
11. Shlobin NA, Clark JR, Hoffman SC, Hopkins BS, Kesavabhotla K, Dahdaleh NS. Patient education in neurosurgery: part 1 of a systematic review. World Neurosurg. (2020) 147:202–14. doi: 10.1016/j.wneu.2020.11.168
12. Matsuyama RK, Wilson-Genderson M, Kuhn L, Moghanaki D, Vachhani H, Paasche-Orlow M. Education level, not health literacy, associated with information needs for patients with cancer. Patient Educ Couns. (2011) 85:e229–36. doi: 10.1016/j.pec.2011.03.022
13. Perrenoud B, Velonaki V-S, Bodenmann P, Ramelet A-S. The effectiveness of health literacy interventions on the informed consent process of health care users: a systematic review protocol. JBI Evid Synth. (2015) 13:82–94. doi: 10.11124/jbisrir-2015-2304
14. Renovanz M, Haaf J, Nesbigall R, Gutenberg A, Laubach W, Ringel F, et al. Information needs of patients in spine surgery: development of a question prompt list to guide informed consent consultations. Spine J. (2019) 19:523–31. doi: 10.1016/j.spinee.2018.08.015
15. Shlobin N, Clark J, Hoffman S, Hopkins B, Kesavabhotla K, Dahdaleh N. Patient education in neurosurgery: part 2 of a systematic review. World Neurosurg. (2020) 147:169. doi: 10.1016/j.wneu.2020.11.169
16. Nicholas R, Solari A, Wilkie D. 029 Importance of face-to-face consultation in complex decision-making. J Neurol Neurosurg Psychiatry. (2019) 90:A17. doi: 10.1177/2055217320959802
17. Shlobin NA, Sheldon M, Lam S. Informed consent in neurosurgery: a systematic review. Neurosurg Focus. (2020) 49:E6. doi: 10.3171/2020.8.FOCUS20611
18. Jimison HB, Sher PP, Appleyard R, LeVernois Y. The use of multimedia in the informed consent process. J Am Med Inform Assoc. (1998) 5:245–56. doi: 10.1136/jamia.1998.0050245
19. Making Ethical Decisions: Process. Available online at: https://blink.ucsd.edu/finance/accountability/ethics/process.html (accessed September 19, 2021).
20. Chen A, Treviño LK, Humphrey SE. Ethical champions, emotions, framing, and team ethical decision making. J Appl Psychol. (2020) 105:245. doi: 10.1037/apl0000437
21. Ethical Champions | PRCA. Available online at: https://www.prca.org.uk/ethicalchampions (accessed January 19, 2021).
22. Cottone RR, Claus RE. Ethical decision-making models: a review of the literature. J Couns Dev. (2000) 78:275–83. doi: 10.1002/j.1556-6676.2000.tb01908.x
Keywords: Cameroon, ethics, neurosurgery, barriers, health outcomes, facilitators
Citation: Ankeambom TJ, Motah M, Ewane M, Shlobin NA, Mbangtang CB, Dada OE, Kabulo KDM, Tetinou F, Endalle G, Kanmounye US, Jokonya L and Esene IN (2022) Identifying Barriers and Facilitators to the Improvement of Healthcare Delivery and Ethics in Two Cameroonian Neurosurgical Centers. Front. Surg. 8:703867. doi: 10.3389/fsurg.2021.703867
Received: 30 April 2021; Accepted: 31 December 2021;
Published: 15 February 2022.
Edited by:
Ankit Mehta, University of Illinois at Chicago, United StatesReviewed by:
Cara Sedney, West Virginia University, United StatesWalt Johnson, Loma Linda University, United States
Copyright © 2022 Ankeambom, Motah, Ewane, Shlobin, Mbangtang, Dada, Kabulo, Tetinou, Endalle, Kanmounye, Jokonya and Esene. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tutuwan J. Ankeambom, dr.tutuwan@gmail.com
 Tutuwan J. Ankeambom
Tutuwan J. Ankeambom Mathieu Motah3
Mathieu Motah3  Celestin Bilong Mbangtang
Celestin Bilong Mbangtang Olaoluwa Ezekiel Dada
Olaoluwa Ezekiel Dada Francklin Tetinou
Francklin Tetinou Geneviève Endalle
Geneviève Endalle Ulrick Sidney Kanmounye
Ulrick Sidney Kanmounye