Comparison of different time intervals between laparoscopic cholecystectomy to endoscopic retrograde cholangiopancreatography for patients with cholecystolithiasis complicated by choledocholithiasis
- 1Department of Hepatopancreatobiliary Surgery, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, Zhejiang, China
- 2Department of Hepatopancreatobiliary Surgery, Enze Hospital, Taizhou Enze Medical Center (Group), Zhejiang, China
Background: Endoscopic retrograde cholangiopancreatography (ERCP) followed by laparoscopic cholecystectomy (LC) is a common strategy for treatment of patients with gallstones with co-existing stones in the common bile duct (CBD). We conducted this study to compare the effect of different time intervals between ERCP and LC.
Methods: A total of 214 patients who underwent elective LC after ERCP for gallstones and CBD stones between January 2015 and May 2021 were retrospectively reviewed. We compared the hospital stay, operation time, perioperative morbidity, and conversion rate to open cholecystectomy, according to the interval between ERCP and ERCP and LC, namely, one day, 2–3 days, and 4 days or more. A generalized linear model was used to analyze the differences among the groups for outcomes.
Results: There were a total of 214 patients with 52, 80, and 82 patients in group 1, group 2, and group 3 respectively. These groups did not differ significantly in terms of major complications or conversion to open surgery (p = 0.503 and p = 0.358, respectively). The generalized linear model showed that operation times in group 1 and group 2 were similar (odds ratio (OR) 0.144, 95% confidence interval (CI) 12.597, 8.511, p = 0.704), while operation time was significantly longer in group 3 than in group 1 (OR 4.005, 95% CI, 0.217, 20.837, p = 0.045). Post-cholecystectomy hospital stay was similar among the three groups, while post-ERCP hospital stay was significantly longer in group 3 compared with group 1.
Conclusion: We recommend that LC be performed within three days after ERCP to reduce operating time and hospital stay.
Introduction
Approximately 4.6%–20.8% of patients with gallstones are detected to have stones in the common bile duct (CBD) during intra-operative cholangiography (1, 2). The European Society of Gastrointestinal Endoscopy (ESGE) guideline recommends that common bile duct stones (CBDSs) may be treated by endoscopic retrograde cholangiopancreatography (ERCP) or surgically with CBD exploration during cholecystectomy (3). Four strategies are widely employed for the management of patients with gallstones and co-existing CBDSs: preoperative ERCP (PreERCP) plus laparoscopic cholecystectomy (LC); LC plus laparoscopic CBD exploration (LCBDE); LC plus intra-operative ERCP (IntraERCP), and LC plus post-cholecystectomy ERCP (PostERCP) (4). Several studies have demonstrated that a one-stage strategy including LCBDE and LC plus intraoperative ERCP is superior to a two-stage strategy (LC plus pre- or postoperative ERCP) in regards to complications, post-cholecystectomy hospitalization, and total costs (5, 6). However, performing LCBDE needs highly skilled and trained operators and is associated with the longest overall operative time as compared with the other procedures. The CBD stone-clearance rate is lowest and the incidence of the biliary leak is highest when adopting LC plus post-cholecystectomy ERCP (4). Further, due to the coordination required for surgeons, endoscopists, operating rooms, and surgical equipment, intra-operative ERCP may be difficult to perform in all hospitals. Thus, pre-operative ERCP followed by LC is a good choice because of its simplicity and accessibility.
However, the suitable interval time from ERCP to LC is still controversial and varies from hours to more than 6 weeks (7–17). It has been reported that delayed LC results in more morbidity and recurrent biliary symptoms (12). On the other hand, early LC can reduce re-admissions with gallstone-related symptoms and is not associated with worse surgical outcomes (8). Hence, early LC after ERCP in the same admission was adopted in our center. This study was conducted to compare the effect of different time intervals from ERCP to LC for patients with gallstones with co-existing CBDSs, in terms of conversion rate to open surgery, post-cholecystectomy complications, and length of hospital stay.
Patients and methods
We conducted a retrospective cohort study on patients with gallbladder stones with co-existing CBDSs, who underwent ERCP for clearance of CBDSs, followed by laparoscopic cholecystectomy (LC). The study was approved by the Ethics Committee of Enze hospital.
The inclusion criteria were: (1) both gallbladder stones and CBDSs confirmed by imaging (ultrasonography/magnetic resonance cholangiopancreatography/computer tomography alone, or combined); (2) patients who underwent ERCP and LC during the same hospital stay; and (3) patients with acute or chronic cholecystitis or acute cholangitis or mild biliary pancreatitis.
The exclusion criteria were: (1) patients with concomitant intrahepatic duct stones; (2) ERCP failure; (3) patients who underwent LC and other operations simultaneously; (4) patients who underwent LC and ERCP simultaneously.
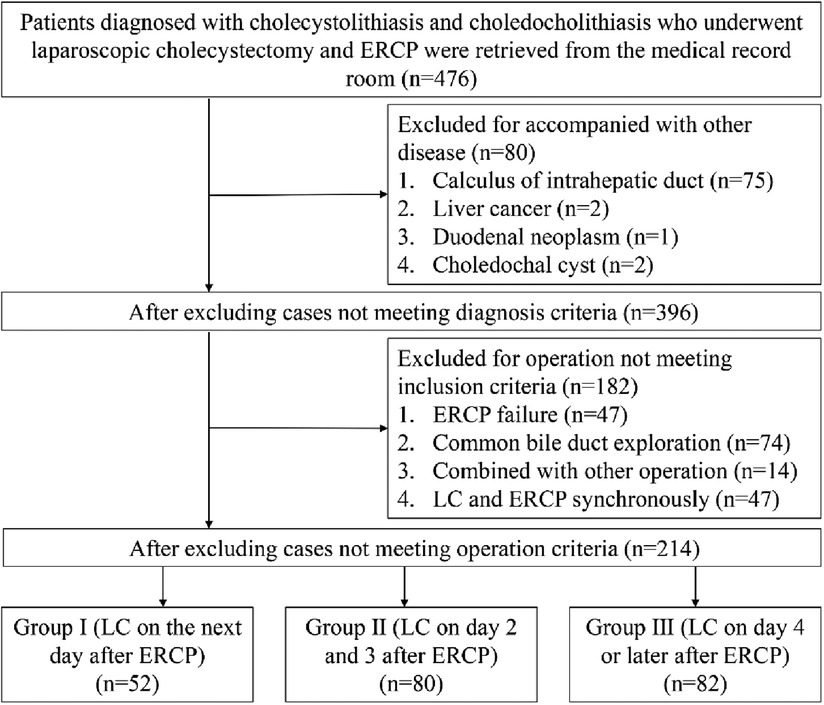
Between January 2015 and May 2021, a total of 214 patients at the Enze hospital fulfilled the inclusion criteria and were included in the study. Figure 1. shows the flow chart for selection of patients. Patients were divided into three groups based on the time interval from ERCP to LC. In group 1 (n = 52), LC was performed the next day after ERCP. In group 2 (n = 80), LC was done on day 2 or day 3 after ERCP, and in group 3 (n = 82), LC was performed on day 4 or later after ERCP, but in the same hospitalization. The assignment of patients to different groups depended on logistic issues, such as the availability of facilities (for example, operation was not done on weekends and holidays), and the individual decisions of the patients basing on the tolerance to postoperative discomfort with ERCP.
The following pre-operative parameters were recorded including age, gender, body mass index (BMI), complications, and reports of laboratory examination, and imaging. The three groups were compared statistically in terms of the operation time, post-cholecystectomy length of hospital stay, conversion rate to open surgery, residual calculi, and major morbidities such as biliary duct injury, post-cholecystectomy bleeding, and bile leak.
The ERCP procedure was accomplished with a standard duodenoscope via air insufflation (Olympus TJF) under sedation, with selective cannulation of the CBD, and if necessary, sphincterotomy (in a standard manner or with pre-cut technique) and stone removal were carried out. LC was done under general anesthesia and the three-port method was adopted. When gallbladder inflammation was heavy or gallbladder triangle anatomy was not clear, a fourth port was added. An abdominal drainage tube was placed only when the surgeon deemed it necessary.
Statistical analysis
Statistical analyses were carried out using the statistical package IBM SPSS Statistics for Windows, Version 26.0 (Armonk, NY). To determine whether the continuous variables were normally distributed, the Shapiro–Wilk test was used. Continuous variables were expressed as mean ± standard deviation or median and quartile, where applicable. Differences between the means of groups were evaluated via one-way ANOVA, and median values were compared via the Kruskal–Wallis test. Categorical data were compared via the chi-square or Fisher's exact test, where appropriate. When p-values from the one-way ANOVA, Kruskal–Wallis, or χ2 test results were statistically significant, a generalized linear model was used to test the true influence of the grouping factor on the results by including the grouping factor and other potential confounding factors. Statistical significance was defined as p < 0.05.
Results
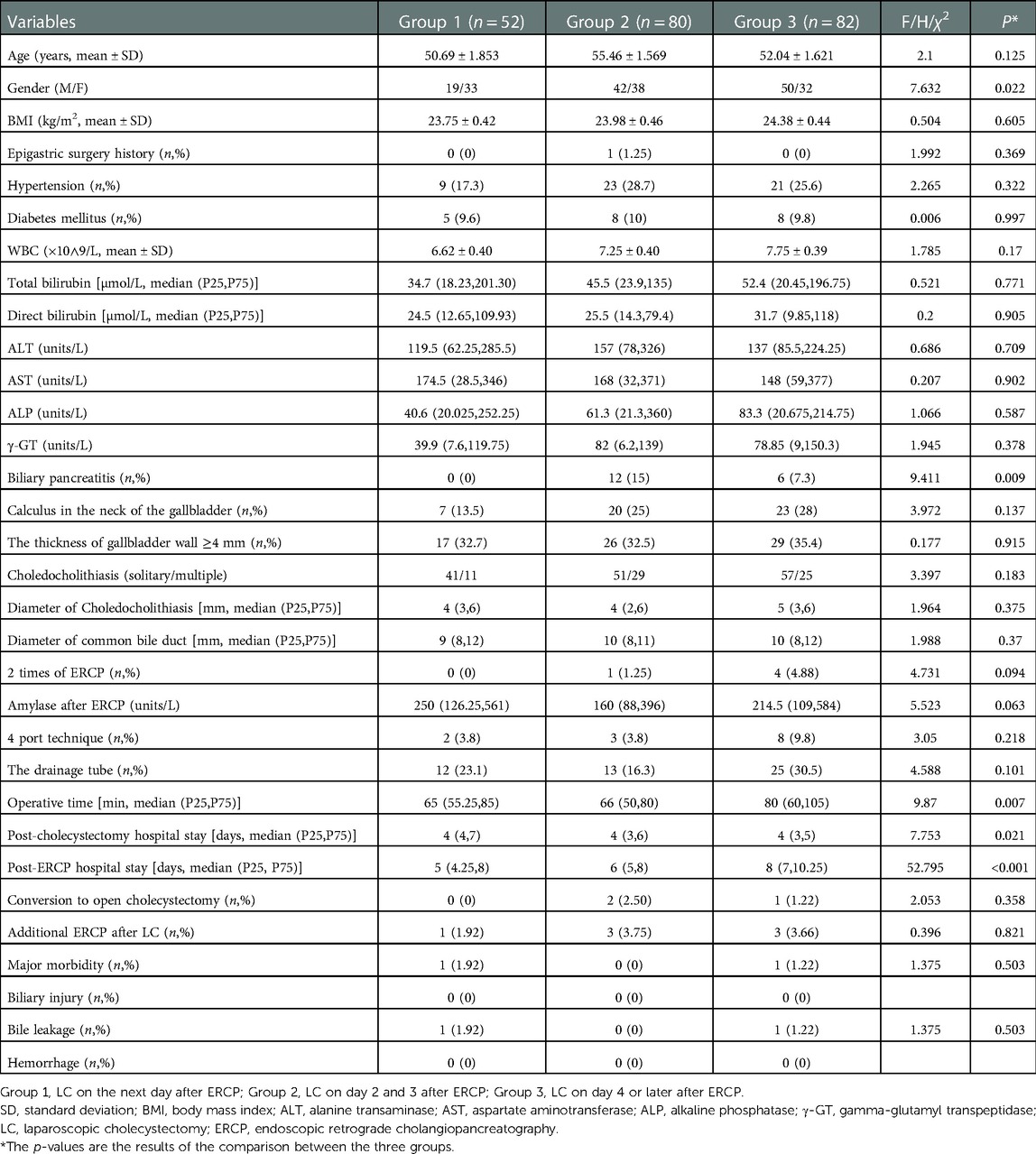
As shown in Figure 1, 476 patients were diagnosed with gallstones and CBD stones. After excluding those not meeting the inclusion criteria, 214 patients were enrolled for further analysis. Demographic and clinical data are shown in Table 1. Group 1 consisted of 52 patients, while groups 2 and 3 consisted of 80 and 82 patients, respectively. Age distribution among the three groups was similar, while gender distribution was significantly different with more females in group 1. The three groups did not differ significantly in comorbidity, blood tests, calculus in the neck of the gallbladder, the thickness of the gallbladder wall, common bile duct, stones in the common bile duct, and amylase after ERCP, except for the proportion of those with biliary pancreatitis.
Table 1 shows the operative times among the three groups. This was 65 min [interquartile range (IQR), 55.25–85 min], 66 min (IQR, 50–80 min), and 80 min (IQR, 60–105 min) in groups 1, 2, and 3, respectively and this difference was statistically significant (p = 0.007).
Elevated WBC was defined as a WBC count higher larger than 9.5 × 109/L based on the standards for testing instruments in our hospital.
WBC, white blood cell; TB, total bilirubin; DB, direct bilirubin; ALT, alanine transaminase; AST, aspartate aminotransferase; ALP, alkaline phosphatase; γ-GT, gamma-glutamyl transpeptidase; CBD, common bile duct; LC, laparoscopic cholecystectomy; ERCP, endoscopic retrograde cholangiopancreatography.
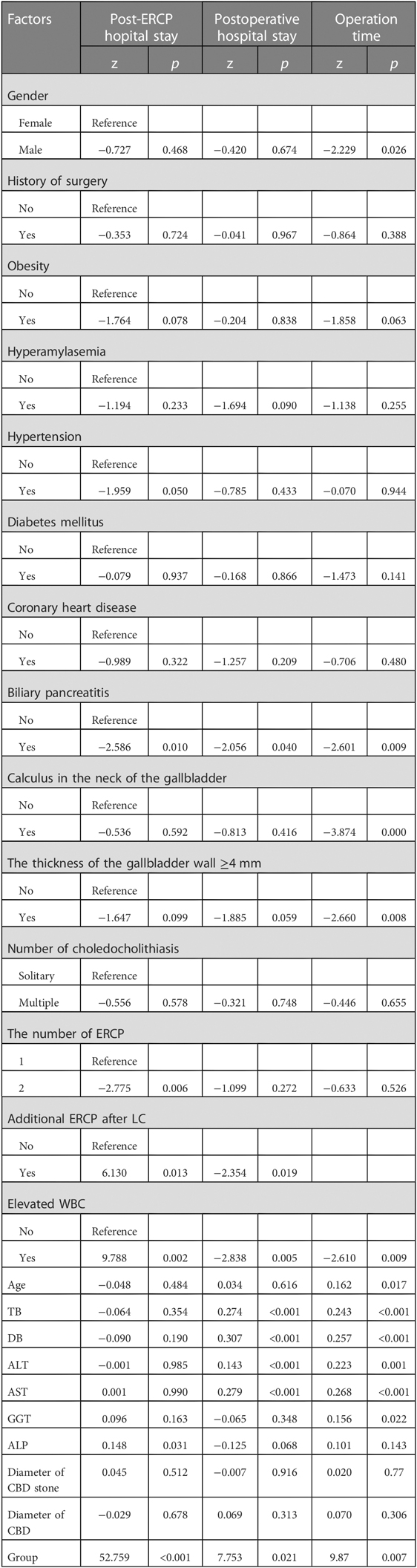
Univariate analysis (Table 2) showed that male gender, biliary pancreatitis, calculus in the neck of the gallbladder, the thickness of the gallbladder wall ≥4 mm, age, total bilirubin, direct bilirubin, alanine aminotransferase, aspartate aminotransferase, gamma-glutamyl transpeptidase, and different interval time between ERCP and LC were all risk factors.
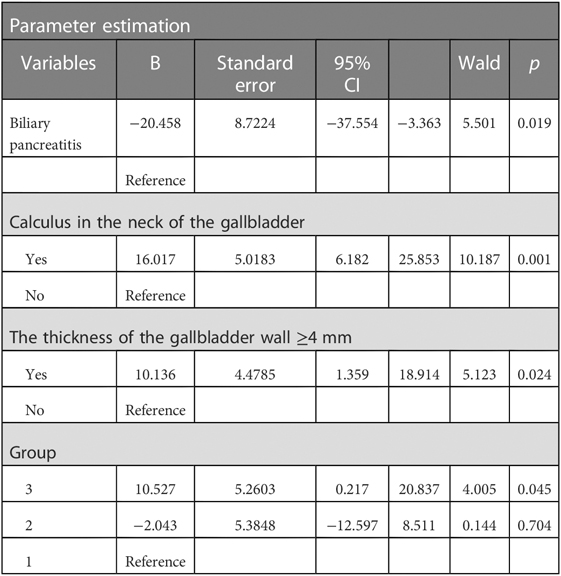
A generalized linear model was constructed as shown in Table 3. Biliary pancreatitis [odds ratio (OR) 5.501, p = 0.019], calculus in the neck of the gallbladder (OR 10.187, p = 0.001), the thickness of the gallbladder wall (OR 5.123, p = 0.024), and the interval time between LC and ERCP were risk factors for prolonged operation time. Among these groups, operation time in group 1 and group 2 was similar (OR 0.144, p = 0.704), while operation time was significantly longer in group 3 than in group 1 (OR 4.005, p = 0.045). The numbers of the conversions to open cholecystectomy were 0, 2, and 1 in groups 1, 2, and 3, respectively, and this difference was not statistically significant. The number of difficult surgeries that needed a four-port technique LC was 13 (6.1%) in total. A drainage tube was required in a total of 50 patients (23.4%). There was no significant difference among the three groups in terms of requiring a fourth port or a drainage tube.
Post-cholecystectomy complications: The overall morbidity rate was 4.2%, including retention of CBDS (3.3%) and bile leakage (0.9%). The retained stones were successfully removed by additional ERCP after LC and the bile leakage was managed by ultrasound-guided peritoneal puncture and catheter drainage plus antibiotics.
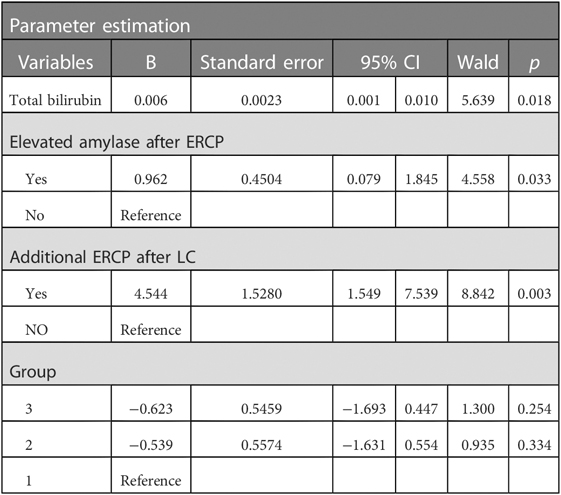
Post-cholecystectomy hospitalization was found to be significantly different among these groups by the Kruskal–Wallis test: 4 days (IQR, 4–7 days), 4 days (IQR, 3–6 days), and 4 days (IQR, 3–5 days), respectively, in groups 1, 2 and 3 (p = 0.021). However, as shown in Table 4, after controlling for confounding factors, the generalized linear model showed that only total bilirubin (OR 5.639, p = 0.018), elevated amylase after ERCP (OR 4.558, p = 0.033), and additional ERCP after LC (OR 8.842, p = 0.003) for retained common bile duct stone were risk factors for a prolonged post-cholecystectomy hospital stay.
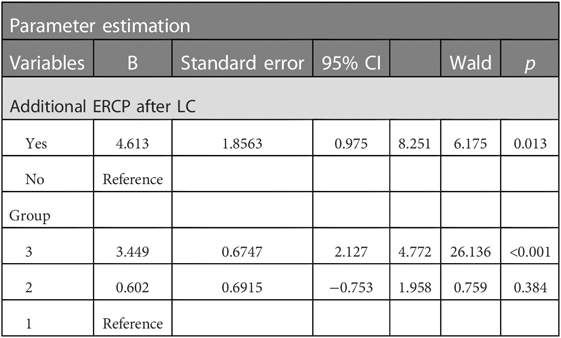
Post-ERCP hospitalization was also significantly different among the three groups by the Kruskal–Wallis test: 5 days (IQR, 4.25–8 days), 6 days (IQR, 5–8 days), and 8 days (IQR, 7–10.25 days), in groups 1, 2 and 3, respectively (p < 0.001). However, in the generalized linear model, as shown in Table 5, only additional ERCP after LC and interval time were risk factors for prolonged post-ERCP hospitalization. Compared with group 1, group 2 did not have significantly prolonged post-ERCP hospitalization (p = 0.384) while group 3 did (p < 0.001).
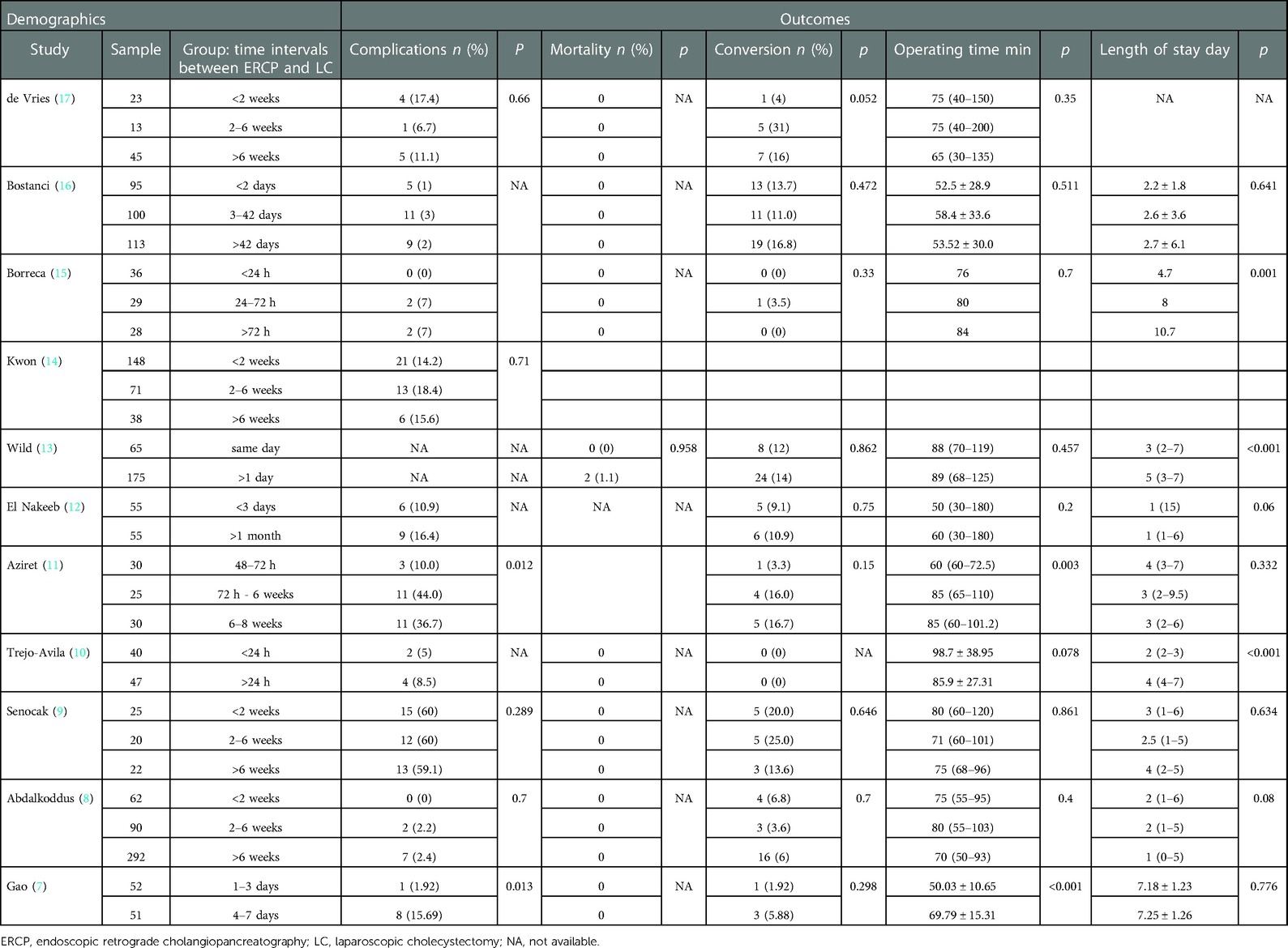
Additionally, we collected articles about the optimal timing for LC after ERCP shown in Table 6. The conversion rate to open surgery varies from 0% to 25% in various studies, and no significant difference was observed among different intervals. The complication rate varies from 0% to 25%, and two studies showed that performing LC within three days reduced the complication rate. Similarly, several studies reported that operative times were reduced when doctors perform LC within three days after ERCP was done. What is more, shorter hospitalization was observed when LC was done after ERCP was finished within one day. Interestingly, we did not find any article that reported any advantage when we prolong the interval between LC and ERCP on the aspect of conversion rate, complication, operative time, and hospitalization.
Discussion
Cholecystolithiasis complicated with choledocholithiasis is a common clinical situation. Several guidelines recommend that patients diagnosed with CBDSs be offered stone extraction, if possible (3, 18). LCBDE and LC plus intra-operative ERCP are both excellent strategies. However, they are not easily accessible in all centers. Thus, pre-operative ERCP plus LC is a commonly used approach. However, pre-operative ERCP can make cholecystectomy difficult due to bacterial colonization in the bile ducts resulting in infection of the hepatoduodenal ligament (19), and hence high-grade adhesions in the gallbladder triangle (16). Many clinicians have explored the ideal interval time from ERCP to LC, as shown in Table 6, but this is still controversial to date. Based on data shown in Table 6, this approach is safe because only two deaths have been reported so far and the complication rate is not high. The conversion rate to open surgery varies from 0% to 25% in various studies. Some studies have suggested that performing LC within three days post-ERCP is a better option because of fewer complications, shorter operative time, and shorter hospitalization. Aziret et al., and Gao et al. reported that performing LC within one to three days of ERCP was associated with a lower complication rate as compared with LC done four days or later. They also found that performing LC within one to three days of ERCP shortened the operative time (7, 11). Borreca et al., Wild et al., and Trejo-Avila et al. suggested performing LC within 24 h post-ERCP so that hospitalization could be significantly shortened (10, 13, 15).
LC is a gold standard operation for gallstones with or without acute cholecystitis, even with severe inflammation. We enrolled patients with acute cholecystitis, acute cholangitis, and mild biliary pancreatitis and had satisfactory outcomes. Our study did not find any difference in the conversion rate to open surgery or major operative complications among the three groups. The overall conversion rate and LC-related complications were both 1.4%. These were relatively low and consistent with the results of a study by Borreca et al. (15). As reported by Aziret et al. and Gao et al., operative time was significantly longer in patients receiving LC four days or later after ERCP (7, 11). These results indicate that LC should be done within three days after ERCP. We believe inflammation and adhesion around the gallbladder triangle caused by ERCP and by cholecystitis itself are similar. Early LC (performed within 1–3 days) has been recommended for acute cholecystitis to improve patient outcomes including fewer complications, shorter hospital stay, and hospitalization costs (20).
We found in our study that patients with biliary pancreatitis, calculus in the neck of the gallbladder, and gallbladder wall thickness ≥4 mm before ERCP had longer operative times, indicating that ERCP is not the only factor responsible for prolonged operative time. Extensive inflammation caused by gallstones, CBDSs, and bacteria in the bile can also make LC very difficult (17). Surgeons operating on patients with gallstones and co-existing CBDSs should be mindful of the fact that factors other than ERCP may contribute to difficulties during surgery, and should consider switching to open surgery if needed to reduce postoperative complications or delay surgery till inflammation subsides.
Length of hospital stay is an important standard because longer hospital stays mean higher hospitalization costs (15). Post-cholecystectomy hospital stay was similar among three groups, while post-ERCP hospital stay was significantly longer in group 3. These results indicated that early LC does not prolong post-cholecystectomy hospital stay. The time taken for waiting for LC after ERCP significantly prolongs the length of hospital stay after ERCP, and such a wait is probably unnecessary.
Based on our study and studies published previously, performing LC in the same admission as ERCP is safe and effective, even though these patients may have underlying acute cholecystitis, acute cholangitis, or mild biliary pancreatitis. Further, recurrent biliary symptoms and biliary complications including gallbladder perforation and recurrent choledocholithiasis can be reduced (12). Performing LC early within three days rather than four days or later after ERCP is recommended because of the reduced operating time and hospital stay, without increased complications and conversion rates. In patients with risk factors for difficult surgery, especially those with a high possibility of conversion to open cholecystectomy, attention is needed during surgery to reduce biliary injury. Percutaneous transhepatic gallbladder puncture drainage may have to be considered in some patients to overcome severe acute inflammation, prior to a second surgery (21).
The limitation of our study is that it was a single center retrospective study. The limitations of retrospective analysis are inevitable. A large, multicenter, randomized controlled trial is needed to address whether LC done within three days of ERCP is superior in terms of fewer post-cholecystectomy complications and shorter hospital stay as compared with LC done four days or later after ERCP.
In conclusion, LC performed within three days after ERCP is safe for patients with gallstone coexisting CBD stones, even in the presence of acute cholecystitis, acute cholangitis, and mild biliary pancreatitis, and is associated with fewer post-cholecystectomy complications and shorter hospital stay.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Enze Medical Center (Group) Enze Hospital Medical Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author contributions
LH, XS, and AW contributed to conception and design of the study. LH and XS organized the database. LH performed the statistical analysis. LH wrote the first draft of the manuscript. LH, XS, and AW wrote sections of the manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
We thank TopEdit (www.topeditsci.com) for its linguistic assistance during the preparation of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Collins C, Maguire D, Ireland A, Fitzgerald E, O’Sullivan GC. A prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy: natural history of choledocholithiasis revisited. Ann Surg. (2004) 239(1):28–33. doi: 10.1097/01.sla.0000103069.00170.9c
2. Borzellino G, Rodella L, Saladino E, Catalano F, Politi L, Minicozzi A, et al. Treatment for retained [corrected] common bile duct stones during laparoscopic cholecystectomy: the rendezvous technique. Arch Surg. (2010) 145(12):1145–9. doi: 10.1001/archsurg.2010.261
3. Manes G, Paspatis G, Aabakken L, Anderloni A, Arvanitakis M, Ah-Soune P, et al. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. (2019) 51(5):472–91. doi: 10.1055/a-0862-0346
4. Ricci C, Pagano N, Taffurelli G, Pacilio CA, Migliori M, Bazzoli F, et al. Comparison of efficacy and safety of 4 combinations of laparoscopic and intraoperative techniques for management of gallstone disease with biliary duct calculi: a systematic review and network meta-analysis. JAMA Surg. (2018) 153(7):e181167. doi: 10.1001/jamasurg.2018.1167
5. Lin Y, Su Y, Yan J, Li X. Laparoendoscopic rendezvous versus ERCP followed by laparoscopic cholecystectomy in the management of cholecystocholedocholithiasis: a systemic review and meta-analysis. Surg Endosc. (2020) 34(9):4214–24. doi: 10.1007/s00464-020-07698-y
6. Singh AN, Kilambi R. Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with gallbladder stones with common bile duct stones: systematic review and meta-analysis of randomized trials with trial sequential analysis. Surg Endosc. (2018) 32(9):3763–76. doi: 10.1007/s00464-018-6170-8
7. Gao MJ, Jiang ZL. Effects of the timing of laparoscopic cholecystectomy after endoscopic retrograde cholangiopancreatography on liver, bile, and inflammatory indices and cholecysto-choledocholithiasis patient prognoses. Clinics (Sao Paulo). (2021) 76:e2189. doi: 10.6061/clinics/2021/e2189
8. Abdalkoddus M, Franklyn J, Ibrahim R, Yao L, Zainudin N, Aroori S. Delayed cholecystectomy following endoscopic retrograde cholangio-pancreatography is not associated with worse surgical outcomes. Surg Endosc. (2022) 36(5):2987–93. doi: 10.1007/s00464-021-08593-w
9. Senocak R, Celik SU, Kaymak S, Hancerliogullari O. Perioperative outcomes of the patients treated using laparoscopic cholecystectomy after emergent endoscopic retrograde cholangiopancreatography for bile duct stones: does timing matter? Ulus Travma Acil Cerrahi Derg. (2020) 26(3):396–404. doi: 10.14744/tjtes.2020.94401
10. Trejo-Avila M, Solorzano-Vicuna D, Garcia-Corral R, Bada-Yllan O, Cuendis-Velazquez A, Delano-Alonso R, et al. Laparoscopic cholecystectomy after endoscopic treatment of choledocholithiasis: a retrospective comparative study. Updates Surg. (2019) 71(4):669–75. doi: 10.1007/s13304-019-00624-5
11. Aziret M, Karaman K, Ercan M, Vargol E, Toka B, Arslan Y, et al. Early laparoscopic cholecystectomy is associated with less risk of complications after the removal of common bile duct stones by endoscopic retrograde cholangiopancreatography. Turk J Gastroenterol. (2019) 30(4):336–44. doi: 10.5152/tjg.2018.18272
12. Nakeeb A E, Ezzet H, Askar W, El Hanafy E, Hamdy E, Atef E, et al. Early versus late cholecystectomy after clearance of common bile duct stones by endoscopic retrograde cholangiopancreatography: a prospective randomized study. Surg Laparosc Endosc Percutan Tech. (2016) 26(3):202–7. doi: 10.1097/SLE.0000000000000265
13. Wild JL, Younus MJ, Torres D, Widom K, Leonard D, Dove J, et al. Same-day combined endoscopic retrograde cholangiopancreatography and cholecystectomy: achievable and minimizes costs. J Trauma Acute Care Surg. (2015) 78(3):503–7; discussion 7–9. doi: 10.1097/TA.0000000000000552
14. Kwon YH, Cho CM, Jung MK, Kim SG, Yoon YK. Risk factors of open converted cholecystectomy for cholelithiasis after endoscopic removal of choledocholithiasis. Dig Dis Sci. (2015) 60(2):550–6. doi: 10.1007/s10620-014-3337-6
15. Borreca D, Bona A, Bellomo MP, Borasi A, De Paolis P. “Ultra-rapid” sequential treatment in cholecystocholedocholithiasis: alternative same-day approach to laparoendoscopic rendezvous. Updates Surg. (2015) 67(4):449–54. doi: 10.1007/s13304-015-0339-7
16. Bostanci EB, Ercan M, Ozer I, Teke Z, Parlak E, Akoglu M. Timing of elective laparoscopic cholecystectomy after endoscopic retrograde cholangiopancreaticography with sphincterotomy: a prospective observational study of 308 patients. Langenbecks Arch Surg. (2010) 395(6):661–6. doi: 10.1007/s00423-010-0653-y
17. de Vries A, Donkervoort SC, van Geloven AA, Pierik EG. Conversion rate of laparoscopic cholecystectomy after endoscopic retrograde cholangiography in the treatment of choledocholithiasis: does the time interval matter? Surg Endosc. (2005) 19(7):996–1001. doi: 10.1007/s00464-004-2206-3
18. Williams E, Beckingham I, El Sayed G, Gurusamy K, Sturgess R, Webster G, et al. Updated guideline on the management of common bile duct stones (CBDS). Gut. (2017) 66(5):765–82. doi: 10.1136/gutjnl-2016-312317
19. Reinders JS, Gouma DJ, Heisterkamp J, Tromp E, van Ramshorst B, Boerma D. Laparoscopic cholecystectomy is more difficult after a previous endoscopic retrograde cholangiography. HPB (Oxford). (2013) 15(3):230–4. doi: 10.1111/j.1477-2574.2012.00582.x
20. Gallaher JR, Charles A. Acute cholecystitis: a review. JAMA. (2022) 327(10):965–75. doi: 10.1001/jama.2022.2350
Keywords: gallstone, common bile duct stone, endoscopic retrograde cholongiopancreatography, laparoscopic cholecystectomy, timing
Citation: Hu L, Shi X and Wang A (2023) Comparison of different time intervals between laparoscopic cholecystectomy to endoscopic retrograde cholangiopancreatography for patients with cholecystolithiasis complicated by choledocholithiasis. Front. Surg. 9:1110242. doi: 10.3389/fsurg.2022.1110242
Received: 28 November 2022; Accepted: 29 December 2022;
Published: 15 March 2023.
Edited by:
Mahesh C. Misra, All India Institute of Medical Sciences, IndiaReviewed by:
Sinan Hatipoglu, Adiyaman University, TürkiyeKenan Yusif-zade, Independent researcher, Azerbaijan
© 2023 Hu, Shi and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aidong Wang wangaidong@enzemed.com
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
 Lingbo Hu
Lingbo Hu Xingpeng Shi
Xingpeng Shi Aidong Wang
Aidong Wang