Application of three-dimensional visualization technology in the anatomical variations of hilar bile ducts in Chinese population
- 1Guangdong Provincial Emergency Hospital, Guangdong Second Provincial General Hospital, Guangzhou, Guangdong, China
- 2The Second Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangdong Provincial Hospital of Chinese Medicine, Guangzhou, Guangdong, China
This study aimed to establish three-dimensional models of the biliary tract of Chinese people using the Hisense computer-aided surgery (CAS) system and to explore the branching patterns and variation types of the biliary system under the study of 3D reconstruction of the biliary tract. Three-dimensional models of the biliary tract were reconstructed in 50 patients using the Hisense CAS system. The branching patterns of intrahepatic bile ducts were observed. The biliary tract was classified according to the confluence of the right posterior sectoral duct (RPSD), right anterior sectoral duct (RASD) and left hepatic duct (LHD), and the presence or absence of accessory hepatic ducts. The 3D models of the bile ducts were successfully reconstructed in 50 Chinese patients. The branching patterns of the bile ducts were classified into seven types. The anatomy of the bile ducts was typical in 54% of cases (n = 27), showed triple confluence in 10% (n = 5), and crossover anomaly in 14% (n = 7), which means anomalous drainage of the RPSD into the LHD, anomalous drainage of the RPSD into the common hepatic duct (CHD) in 10% (n = 5), anomalous drainage of the RPSD into the cystic duct (CD) in 2% (n = 1), absence of left main hepatic duct in 1% (n = 1), presence of accessory duct in 8% (n = 4). Among them, there were three cases of accessory hepatic ducts coexisting with other variation types. By using the Hisense CAS system to establish 3D models of the biliary tract of the Chinese people, we established the branching model of the second-order bile ducts, which has important value for the classification of the biliary system and its variation types.
Introduction
Variations in the anatomy of the biliary tract have been proven to be of clinical significance (1). Accurate knowledge of these anatomical variants is crucial for surgeons to avoid complications (2). Correct preoperative understanding of the bile duct variations may help to formulate a preoperative simulation and surgical planning, which can increase the success rate of surgery, reduce operation-related complications, and improve the prognosis of patients (3). Several reports have described the anatomy of the biliary tract, including studies on the human biliary system in different ways, such as casting research, autopsy specimens, endoscopic retrograde cholangiopancreatography (ERCP), Magnetic resonance cholangiopancreatography (MRCP), angiography, and detailed descriptions of the biliary anatomy with different classification systems (2, 4–7). However, there are few studies on the variations in biliary anatomy using 3D visualization technology. Three-dimensional visualization technology based on CT or MRI has been a research hotspot in recent years, and it has been widely and maturely applied in the field of hepatobiliary surgery. Nevertheless, it has rarely been used in the study of the biliary tract, mainly because the biliary system, in general, is not well developed on CT images, and thus, its complete structure cannot be objectively described by the reconstruction software. Harms et al. (8) studied donor liver for living donor liver transplantation using three-dimensional visualization technology. Zeng et al. (9) studied the application of three-dimensional visualization in hilar cholangiocarcinoma and reconstructed individualized branches of intrahepatic bile ducts. Li et al. (10) evaluated the application value of 3D reconstructed models and 3D printed models in the training of choledochoscopy techniques. None of them, however, systematically described the anatomic variation types of bile ducts. The advent of digital medicine and three-dimensional visualization software has improved surgeons’ ability to identify the biliary tract on CT images; this, combined with the imaging characteristics of obstructive biliary tract diseases, has created conditions for the three-dimensional reconstruction of the biliary tract.
The Hisense computer-aided surgery (CAS) system, a three-dimensional reconstruction software based on CT images, can realize in-depth mining of CT image information and reproduce the anatomy of abdominal organs and vessels accurately. A solid understanding of individualized anatomic differences of the biliary system informs both the planning of the procedure and intraoperative decision-making. In the present article, we perform 3D modeling based on CT imaging data from patients with obstructive disease of the bile ducts using the Hisense CAS system to show the normal and abnormal anatomy of biliary trees of Chinese people based on the three-dimensional visualization technology; meanwhile, we analyze the branching pattern and variation types of Chinese biliary tract according to the three-dimensional reconstructed models.
Materials and methods
Research objects
From September 2019 to December 2020, 80 patients with obstructive disease of the bile ducts admitted to the Second People's Hospital of Guangdong Province were evaluated for study eligibility. These patients underwent enhanced CT scans of the upper abdomen. In that, 30 of them were excluded due to poor image quality or obscuration of biliary anatomy. Among them, 13 patients with poor cooperation resulted in more CT image artifacts, which affected bile duct reconstruction, and 17 patients had insufficient or uneven bile duct dilation, which affected bile duct alignment recognition. Hence, our final study group included 50 cases (30 males and 20 females; age range 29–85 years). With the approval of the ethics committee, all patients signed an informed consent form.
Inclusion criteria
The inclusion criteria included: (1) patients with clear CT images and well-dilated branches of the biliary tract below grade 2 (diameter greater than 0.5 mm); (2) patients from China. The exclusion criteria included: (1) patients with blurry CT images or CT artifacts, and patients whose intrahepatic bile ducts cannot be identified; (2) patients with a history of bile duct surgery, bile duct injury, hepatectomy, and liver transplantation.
CT data acquisition
CT scan images were obtained using a 256-slice spiral CT (Brilliance 256, Philips Healthcare, Best, The Netherlands), including plain scan and enhanced phase data. A non-ionic contrast agent (iopamidol, 100 ml: 37 g(I)) was used for enhanced scanning (arterial phase, portal phase, and venous phase). The software used for data processing and 3D reconstruction includes the RadiAnt DICOM Viewer and the Hisense CAS system. Patients orally took 500–1000 ml of clear liquid 20–30 min before the examination, and then another 500 ml before the start of the scan to fill the gastrointestinal tract (as a negative contrast agent). Patients were trained to hold their breath in full inspiration to maximize the control of artifacts due to respiratory motion, and took a supine scan from the top of the diaphragm to the lower edge of the liver. The acquisition parameters were set as follows: tube current, 300 mA; tube voltage, 120 kV; slice thickness, 1.0 mm; pitch, 0.993; and scan speed, 0.5 s/rotation. The plain scan is a high-resolution volume scan in the sub-millimeter state. A double-barrel high-pressure syringe was used, and the contrast agent bolus (dose 1.5 ml/kg) was injected into the cubital vein at a speed of 5 ml/s. The scan delay time after the arterial phase injection was 20–25 s, and the scan delay time after the intravenous phase injection was 50–55 s. After scanning, the image data were transferred to the postprocessing workstation and burned to a disc for storage.
3D reconstruction
The original 1 mm thin-slice CT scan data from the burned CD were extracted, including data in the plain scan phase, arterial phase, venous phase, and delayed phase. Collected data were converted into DICOM format by using a Radiant Dicom Viewer and then imported into the Hisense CAS system. In the mode of “3D reconstruct”, the appropriate phase of CT scan was selected, and the window width and window level were adjusted to perform 3D reconstruction of liver parenchyma, hepatic vascular system, bile duct system, and calculi, respectively. The reconstructed data in different phases were marked with different colors, and then a complete hepatobiliary system was constructed. The three-dimensional model of the liver and bile ducts was hidden, rotated, zoomed in, and transparent with the CAS system, and the three-dimensional model of the bile ducts was separately displayed to study the anatomy and variation of the bile ducts. Meanwhile, the length of the right hepatic duct (RHD) was also measured in three dimensions. The three-dimensional reconstruction software (the CAS system) used in this study was purchased by our research team at a cost of approximately 700,000 RMB. The software is mainly used for clinical research and preoperative evaluation. It can be used repeatedly, and the cost of each reconstruction in the later stage is about 3,000 RMB. The entire reconstruction process was performed by the personnel who have obtained the training certificate for system reconstruction. For cases of different complexity, it takes about 30–60 min to complete the entire reconstruction process.
Data analysis
The 3D models were reviewed by a senior consultant radiologist and a senior hepatobiliary surgeon. Anatomic variations were classified according to the Huang classification (2), based on the confluence of the RPSD, RASD, and LHD. SPSS statistical analysis software was used to calculate the type of biliary anatomy and the percentage analysis of the model in southern China; moreover, an appropriate chi-square test was used to test whether gender and variation are related, and a P less than 0.05 indicates statistical significance.
Ethical statement
The study protocol was approved by the ethics committee of the Guangdong Second Provincial General Hospital and written informed consents were obtained from all patients to undergo the study. The study application form and ethical review form are shown in the additional materials.
Results
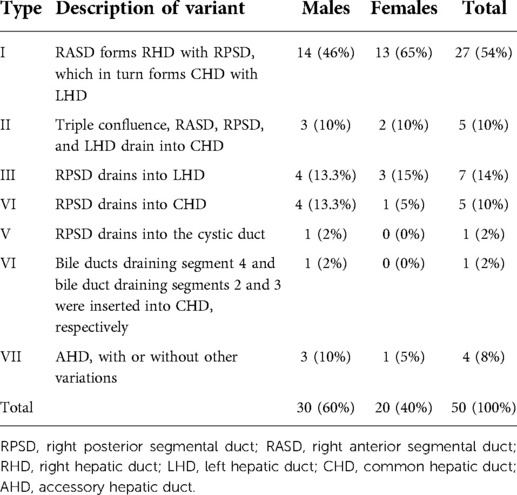
Three-dimensional reconstruction of the liver parenchyma, intrahepatic and extrahepatic bile ducts, and intrahepatic vessels was completed in 50 Chinese patients using the Hisense CAS system. The reconstructed hepatobiliary system was complete, which clearly showed the 3D structure of the intrahepatic ducts. Spatial configuration and abnormalities of these ducts could be observed by zooming in, zooming out, and all-around rotation. By hiding and transparency adjustment of the liver and intrahepatic vascular system, a three-dimensional model of the bile duct of Chinese people was obtained. The model was rotated and observed. The classification was conducted according to Huang's classification (2), based on the confluence of the RPSD, RASD, and LHD. The branching patterns were classified into seven types (Figure 1). A total of 27 patients (54%) had typical biliary tract anatomy (type I) (Figure 2A). Anatomic variations were found in 23 patients (46%), including five patients (10%) with type II (Figure 2B), seven patients (14%) with type III (Figure 2C), five patients (10%) with type IV (Figure 2D), one male patient (2%) with type V (Figure 2E), and one patient (2%) with type VI (Figure 2F); in addition, four cases (8%) had accessory hepatic ducts, among which three cases were accompanied by other variations (Figure 2H and I). The variation types and frequencies of the 50 cases in the three-dimensional model of the bile duct are shown in Table 1.
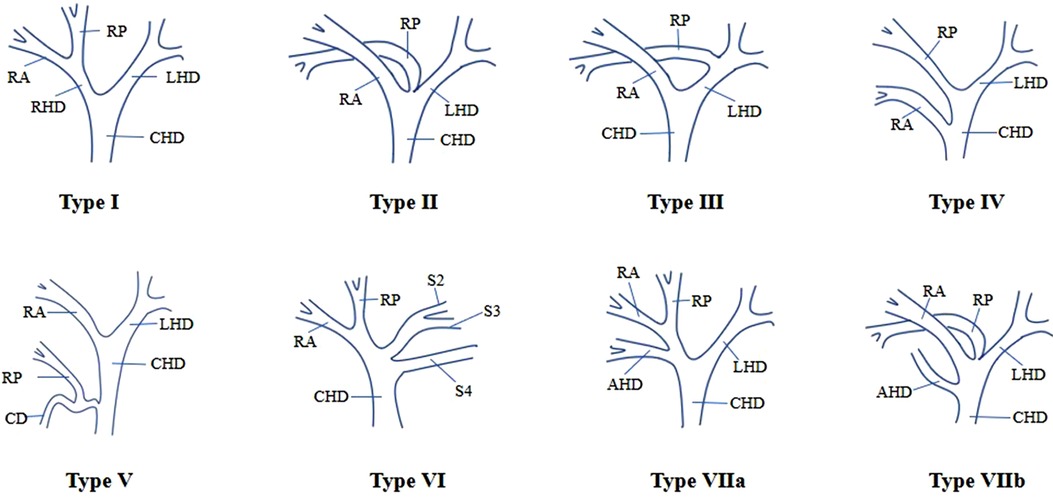
Figure 1. Intrahepatic bile duct anatomy based on three-dimensional biliary tract reconstruction. Type I shows a typical anatomical structure of the biliary tract. Type II is triple confluence, i.e., RASD, RPSD, and LHD confluence into the CHD. Type III shows abnormal RPSD drainage to LHD, abnormal RPSD drainage to the CHD, and abnormal RPSD drainage to the CD. In type VI, there is no true LHD, and the bile duct draining segment 4 and the bile duct draining segments 2 and 3 are inserted into the CHD, respectively. Type VII has AHD, and it can be divided into type VIIa and type VIIb, according to the opening position of AHD. In type VIIb, there are also type II variants besides the opening of AHD in the CHD. RPSD = right posterior segmental duct, RASD = right anterior segmental duct, RHD = right hepatic duct, LHD = left hepatic duct.
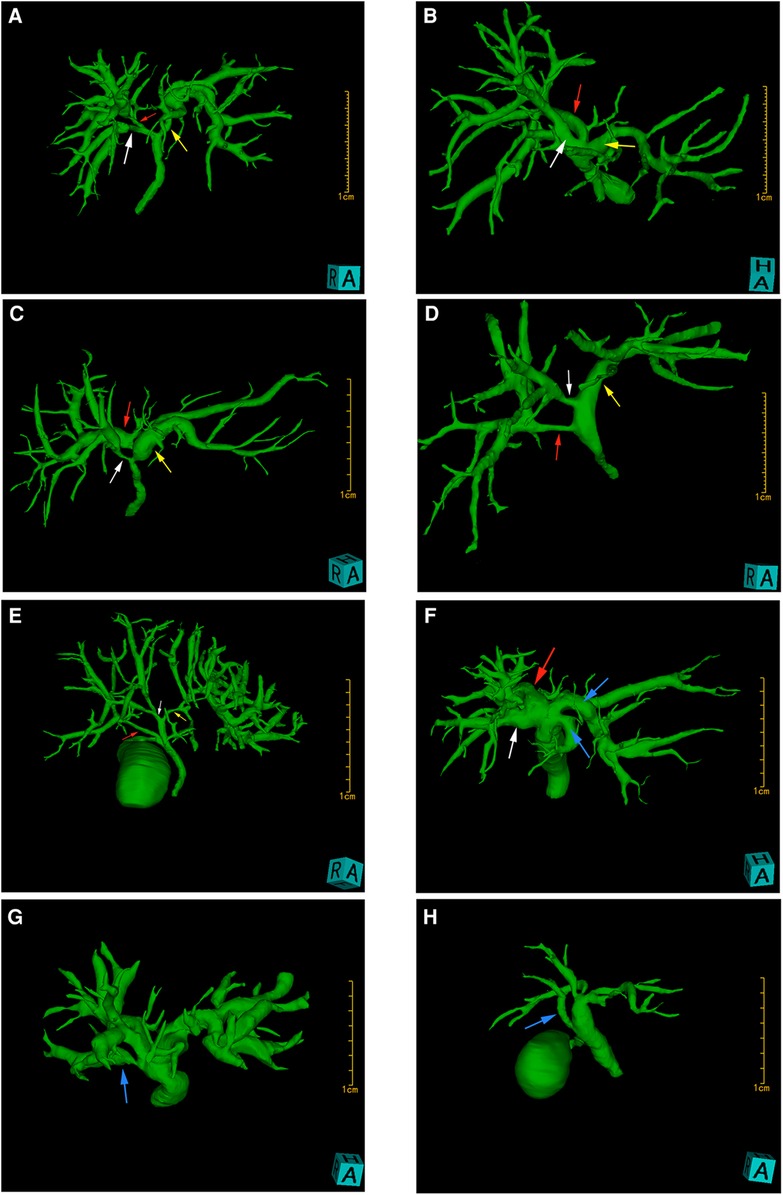
Figure 2. 3D biliary tract model reconstructed by the Hisense CAS system. The white arrowheads indicate RASD, the red arrowheads indicate RPSD, the yellow arrowheads indicate LHD, and the blue arrowheads indicate variant bile ducts. (A) shows typical intrahepatic bile duct anatomy (type I), i.e., RASD (white arrowhead) forms RHD with RPSD (red arrowhead), which in turn forms CHD with LHD. The bile duct shown in (B) is classified as type II, indicating triple confluence, i.e., RASD, RPSD, and LHD drain into the CHD. (C) is a type III variant showing abnormal RPSD drainage to LHD. (D) shows an abnormal RPSD drainage to CHD, and (E) presents a rare variant showing RPSD drainage to the cystic duct, and is classified as type V. In (F), the bile duct draining segment 4 (blue arrowhead) and the bile duct draining segments 2 and 3 (blue arrowhead) are inserted into CHD, respectively, and there is no left main hepatic duct in this variant. Accessory hepatic ducts (blue arrowhead) are present in both (G) and (H), which are classified as type VIIa and type VIIb, respectively, according to the opening position of the accessory hepatic ducts. In type VIIa, AHD is inserted into RHD, not accompanied by other types of variations, while in type VIIb, AHD can be observed opening into the hepatic duct, accompanied by a variation of type II.
Discussions
There are four sets of ductal systems in the liver, each with complex structures, among which the biliary tract has the highest rate of anatomical variations. Preoperative awareness of the pattern of these variations may help to prevent and manage biliary injuries during surgical procedures. Several imaging modalities for the evaluation of the biliary tract in vivo can be used. ERCP and percutaneous transhepatobiliary tract (PTC), as the gold standard for this purpose, can accurately show the course of the biliary tract; however, they are rarely used preoperatively because they are invasive methods and prone to complications such as acute pancreatitis and cholangitis (11). MRCP, as a standard and non-invasive examination method for evaluating the biliary system, can present a clear anatomical structure of the biliary system without the use of contrast agents and has a high sensitivity in the identification of variations (12), and 3D-MRCP, in particular, can provide relatively high-quality three-dimensional images, which has a high application value in the evaluation of biliary tract structure (13); nevertheless, disadvantages of MRCP include decreased spatial resolution, making MRCP less sensitive to abnormalities of peripheral intrahepatic duct (6), and thus, its efficacy in preoperative evaluation of biliary tract diseases and its guiding significance for biliary tract surgery is limited (14). In addition, the potential problems with MRCP also include image artifacts and difficulty in patient compliance, so it is generally not used as a preoperative examination for routine surgery (13). Some studies (15) even reported that MRCP was not effective in describing the branching pattern of the second-order bile duct and was insufficient to detect the variation of the bile duct preoperatively. As a non-invasive method, CT is a useful modality for the preoperative assessment of the biliary system, and its data acquisition is relatively simple and convenient. In this study, based on the CT image data, the Hisense CAS system was used to establish three-dimensional models of the biliary tract and identify the type of variation, which could help perform preoperative simulation programs, develop the best operation plans, and improve the accuracy and safety of actual surgery (16).
3D visualization technology is based on the reconstruction of CT image data. The reconstructed 3D model can provide more intuitive and comprehensive information on liver parenchyma and intrahepatic duct system and can be adjusted with different transparency and rotation angle so that surgeons can observe the anatomical structure of the bile duct from multiple directions and angles. Anatomic variation and lesion location of the biliary tract can be accurately identified (17). The three-dimensional visualization software can place the liver parenchyma, vascular system, and bile duct system in the same space, and display the spatial position relationship between the liver, intrahepatic vessels, and bile duct and lesions stereoscopically (18), which has an important guiding significance for hepatobiliary surgery. In addition, with the development of virtual reality technology and 3D printing technology, the reconstructed 3D model is applied to the preoperative simulation operation, making the actual operation safer and less traumatic (19, 20). Obstructed biliary tract disease leads to the dilation of intrahepatic and extrahepatic bile ducts, and the bile duct system is fully shown on CT images, which is significantly different from the CT values of other liver tissues. Based on this imaging feature, the present study can reconstruct a complete three-dimensional model of the bile duct system by using the Hisense CAS system. Its hidden and transparent functions can be used to display the biliary tract system in stereo. By rotating and zooming in, the anatomical structure of the biliary tract system can be observed from all angles and the variation of the biliary tract can be identified.
Anatomic variations of the biliary tract have been described by several classification systems (21). The frequency of biliary tract variations is influenced by region and ethnicity. Typical biliary anatomy is more common in Asians than in Europeans and Americans, probably because of the difference in embryo development, and a certain correlation with gender, as variations of the biliary tract are more common in females (22). Such findings were also reported in a study of MRCP in 1,011 inhabitants of the Aegean region of Turkey (23). However, in a study report of 150 Saudi Arabian population, no gender difference was detected (24). Similarly, in our study, Fisher's accurate test showed no significant correlation between the anatomic variations of the biliary tract and gender (P > 0.05). Although several earlier studies on biliary anatomy have varied in terms of research methods and ethnicity of the population studied, the results generally showed that the typical biliary anatomy (type I) was the most common biliary structure, occurring in approximately 55% to 79% of cases. Among the variant types, the right posterior hepatic duct (RPHD) drainage to the LHD (type III) was the most common, noted in about 9.3% to 28.7%. The so-called “trifurcation pattern” (type II) is the second most common, noted in about 9%–19%, and the insertion of the RPHD into the CHD or CD is the least common (4–6, 21, 23, 24). The Hisense CAS system analysis results showed that type I accounted for 54%, which was the typical biliary anatomical structure, types II and III were the most common variant types, accounting for 10% and 14% respectively, and types IV and V were the least common variant types, accounting for 10% and 2% respectively; these findings were similar to earlier literature reports (4–6, 21, 23, 24). In addition, we were surprised to note that some of the specific biliary tract types could not be explained according to the Huang classification. The bile duct variations shown in Figure 2F are defined as “type VI”, with a variation rate of 2%. This type of variation is described as the bile duct draining into the hepatic duct at segment 4 and the bile duct draining into segments 2 and 3, respectively, which is very similar to type 6 in Choi's classification system (4), i.e., the bile duct draining into the hepatic duct at segments 2 and 3, respectively. Accessory hepatic duct (AHD) is usually defined as the bile duct that merges with the extrahepatic bile duct and drains a certain segment of the liver or liver lobe. The report of its incidence varies widely in different literature, ranging from 1.9% to 31.4% (25). In our study, four cases (8%) had accessory hepatic ducts, of which one case was alone, two cases were accompanied by type II variation, and one case was accompanied by type VI variation. According to the classification proposed initially by Huang, the length of the RHD of type I was required to be greater than 1 cm. We used the Hisense CAS system to conduct three-dimensional measurements of the three-dimensional model of the biliary duct, and the results showed that in all the subtype biliary duct reconstruction models, five cases had the length of the RHD less than 1 cm. According to the classification, the type I prevalence decreases to 48%, which is still the most common type.
Preoperative assessment of the biliary tract anatomy plays a pivotal role in guiding surgery. In living donor right hepatectomy, if the type I bile duct has a longer RHD in the donor's liver, the difficulty of end-to-end bile duct anastomosis or biliary enterostomy can be reduced. When performing left hepatic resection on patients with type III bile duct, the greater the distance between RPHD insertion and the RHD and LHD junction, the more likely it is to damage or ligate the right posterior bile duct when the variation is unknown, resulting in hepatic cholestasis, cirrhosis, or bile leakage of the entire liver segment drained by the right posterior bile duct. In percutaneous transhepatic biliary drainage, if the LHD obstruction occurs in patients with type III bile duct, cholestasis in the right posterior lobe of the liver may occur. In addition to drainage of the left half of the liver, drainage of the right posterior lobe of the liver is also required. In percutaneous transhepatic choledochoscopic removal of stones, the selection of the lithotomy sinus tract directly affects the quality and efficiency of the operation, which should be determined according to the shape of the biliary tract. The most reasonable lithotomy fistula should be able to explore the stones without tearing the liver and biliary tract due to the excessive angle between the long axis of the choledochoscope and the lithotomy sinus tract. In laparoscopic cholecystectomy, anatomical abnormality of the bile duct is considered one of the risk factors for bile duct injury, with an incidence of 0.5%–1.7% (26). During laparoscopic cholecystectomy, attention should be paid to the existence of accessory hepatic ducts and types IV and V variations, because the Calot's triangle is covered by a thick layer of adipose tissue, and the lower insertion of the right posterior bile ducts or accessory hepatic ducts is prone to damage during separation. With preoperative knowledge regarding the existence of these variations, the vigilance of surgeons in this surgical area can be increased, and the ducts at Calot's triangle can be carefully isolated during operation to reduce the risk of iatrogenic bile duct injuries.
Prospects
The limitation of our study was that the selected subjects are all obstructive biliary tract diseases, and hence the results are biased, though the results are similar to other studies. In addition, sufficient reconstruction data should be included to more accurately describe the frequency of biliary anatomical variations in populations in southern China. We look forward to discovering new types of biliary variations based on three-dimensional visualization of the biliary tract and then combining them with the practice of hepatobiliary surgery, so as to propose a more suitable classification system.
Conclusions
Through the Hisense CAS system, we re-verified that type I remains the most common type in the Chinese population, while types II and III are the most common variants; in addition, we found that some specific biliary tract types defined as “type VI” could not be explained according to the Huang classification. By using 3D visualization technology to establish 3D models of the biliary tract of the Chinese people, we established the branching model of the second-order bile ducts, which has significant value for the classification of the biliary system and its variation types and for the reduction of postoperative complications.
Contribution to the field
There are four sets of ductal systems in the liver, each with complex structures, among which the biliary tract has the most anatomical variations. Preoperative awareness of the pattern of these variations may help to prevent and manage biliary injuries during surgical procedures. Several imaging modalities for the evaluation of the biliary tract in vivo can be used. ERCP and PTC, as the gold standards for this purpose, can accurately show the course of the biliary tract; however, they are rarely used preoperatively because they are invasive methods and prone to complications such as acute pancreatitis and cholangitis. As a non-invasive method, CT is applied as a useful modality for the preoperative assessment of the biliary system, and data acquisition is relatively simple and convenient. Moreover, preoperative assessment of the biliary tract anatomy plays a pivotal role in guiding surgery. In this study, based on the CT image data, the Hisense CAS system was used to establish three-dimensional models of the biliary tract and identify the type of variation, which could help perform preoperative simulation program, develop the best operation plans, and improve the accuracy and safety of actual surgery.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by the ethics committee of the Guangdong Second Provincial General Hospital. The patients/participants provided their written informed consent to participate in this study.
Author contributions
CL, XY, PG contributed to the conception and design of the study; XL, RD, YH, JQ, RL, SD, JZ, XZ and JD performed the research and analyzed the data; LC wrote the paper. All authors contributed to the article and approved the submitted version.
Funding
This research was supported by Guangzhou Science and Technology Planning Project (No. 201904010257), in part by the Project of Guangdong Medical Science and Technology Research Fund (No. A2021101), Guangdong Second Provincial General Hospital Youth Fund (No. YQ296-005) and Project of Administration of Traditional Chinese Medicine of Guangdong Province of China (No. 20202006).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sarawagi R, Sundar S, Raghuvanshi S, Gupta SK, Jayaraman G. Common and uncommon anatomical variants of intrahepatic bile ducts in magnetic resonance cholangiopancreatography and its clinical implication. Pol J Radiol. (2016) 81(0137-7138):250–5. doi: 10.12659/pjr.895827
2. Huang TL, Cheng YF, Chen CL, Chen TY, Lee TY. Variants of the bile ducts: clinical application in the potential donor of living-related hepatic transplantation. Transplant Proc. (1996) 28(3):1669–70.8658831
3. Mortelé KJ, Ros PR. Anatomic variants of the biliary tree: MR cholangiographic findings and clinical applications. AJR Am J Roentgenol. (2001) 177(2):389–94. doi: 10.2214/ajr.177.2.1770389
4. Choi JW, Kim TK, Kim KW, Kim AY, Kim PN, Ha HK, et al. Anatomic variation in intrahepatic bile ducts: an analysis of intraoperative cholangiograms in 300 consecutive donors for living donor liver transplantation. Korean J Radiol. (2003) 4(2):85–90. doi: 10.3348/kjr.2003.4.2.85
5. Kafle A, Adhikari B, Shrestha R, Ranjit N. Anatomic variations of the right hepatic duct: results and surgical implications from a cadaveric study. J Nepal Health Res Counc. (2019) 17(1):90–3. doi: 10.33314/jnhrc.2012
6. Karakas HM, Celik T, Alicioglu B. Bile duct anatomy of the Anatolian Caucasian population: Huang classification revisited. Surg Radiol Anat. (2008) 30(7):539–45. doi: 10.1007/s00276-008-0365-y
7. Reichert PR, Renz JF, D'Albuquerque LA, Rosenthal P, Lim RC, Roberts JP, et al. Surgical anatomy of the left lateral segment as applied to living-donor and split-liver transplantation: a clinicopathologic study. Ann Surg. (2000) 232(5):658–64. doi: 10.1097/00000658-200011000-00007
8. Harms J, Bartels M, Bourquain H, Peitgen HO, Schulz T, Kahn T, et al. Computerized CT-based 3D visualization technique in living related liver transplantation. Transplant Proc. (2005) 37(2):1059–62. doi: 10.1016/j.transproceed.2004.11.088
9. Zeng N, Yang J, Xiang N, Wen S, Zeng S, Qi S, et al. Application of 3D visualization and 3D printing in individualized precision surgery for Bismuth-Corlette type III and IV hilar cholangiocarcinoma. Nan Fang Yi Ke Da Xue Xue Bao. (2020) 40(8):1172–7. doi: 10.12122/j.issn.1673-4254.2020.08.15
10. Li A, Tang R, Rong Z, Zeng J, Xiang C, Yu L, et al. The use of three-dimensional printing model in the training of choledochoscopy techniques. World J Surg. (2018) 42(12):4033–8. doi: 10.1007/s00268-018-4731-6
11. Hirano Y, Tatsuzawa Y, Shimizu J, Kinoshita S, Kawaura Y, Takahashi S. Efficacy of multi-slice computed tomography cholangiography before laparoscopic cholecystectomy. ANZ J Surg. (2006) 76(8):693–5. doi: 10.1111/j.1445-2197.2006.03833.x
12. Limanond P, Raman SS, Ghobrial RM, Busuttil RW, Lu DS. The utility of MRCP in preoperative mapping of biliary anatomy in adult-to-adult living related liver transplant donors. J Magn Reson Imaging. (2004) 19(2):209–15. doi: 10.1002/jmri.10446
13. Kwon H, Reid S, Kim D, Lee S, Cho J, Oh J. Diagnosing common bile duct obstruction: comparison of image quality and diagnostic performance of three-dimensional magnetic resonance cholangiopancreatography with and without compressed sensing. Abdom Radiol (NY). (2018) 43(9):2255–61. doi: 10.1007/s00261-017-1451-6
14. Hyodo T, Kumano S, Kushihata F, Okada M, Hirata M, Tsuda T, et al. CT and MR cholangiography: advantages and pitfalls in perioperative evaluation of biliary tree. Br J Radiol. (2012) 85(1015):887–96. doi: 10.1259/bjr/21209407
15. Yeh BM, Breiman RS, Taouli B, Qayyum A, Roberts JP, Coakley FV. Biliary tract depiction in living potential liver donors: comparison of conventional MR, mangafodipir trisodium-enhanced excretory MR, and multi-detector row CT cholangiography–initial experience. Radiology. (2004) 230(3):645–51. doi: 10.1148/radiol.2303021775
16. Gao Y, Hu J, Zhang X, Zhang M, Wang D, Zheng X, et al. Use of Hisense computer-assisted surgery system enhances infrapyloric lymph node dissection for gastric cancer. J Surg Res. (2019) 242(0022-4804):31–9. doi: 10.1016/j.jss.2019.04.019
17. Fang CH, Li G, Wang P, Fan YF, Zhong SZ. Computer-aided rigid choledochoscopy lithotripsy for hepatolithiasis. J Surg Res. (2015) 195(1):105–12. doi: 10.1016/j.jss.2015.01.011
18. Xie A, Fang C, Huang Y, Fan Y, Pan J, Peng F. Application of three-dimensional reconstruction and visible simulation technique in reoperation of hepatolithiasis. J Gastroenterol Hepatol. (2013) 28(2):248–54. doi: 10.1111/jgh.12066
19. Ryu M, Cho A. Usefulness of image-navigated surgery in liver surgery. Nihon Geka Gakkai Zasshi. (2008) 109(2):71–6.18409583
20. Zheng YX, Yu DF, Zhao JG, Wu YL, Zheng B. 3D Printout models vs. 3D-rendered images: which is better for preoperative planning? J Surg Educ. (2016) 73(3):518–23. doi: 10.1016/j.jsurg.2016.01.003
21. Deka P, Islam M, Jindal D, Kumar N, Arora A, Negi SS. Analysis of biliary anatomy according to different classification systems. Indian J Gastroenterol. (2014) 33(1):23–30. doi: 10.1007/s12664-013-0371-9
22. Cucchetti A, Peri E, Cescon M, Zanello M, Ercolani G, Zanfi C, et al. Anatomic variations of intrahepatic bile ducts in a European series and meta-analysis of the literature. J Gastrointest Surg. (2011) 15(4):623–30. doi: 10.1007/s11605-011-1447-4
23. Uysal F, Obuz F, Uçar A, Seçil M, Igci E, Dicle O. Anatomic variations of the intrahepatic bile ducts: analysis of magnetic resonance cholangiopancreatography in 1011 consecutive patients. Digestion. (2014) 89(3):194–200. doi: 10.1159/000358558
24. Al-Muhanna AF, Lutfi AM, Al-Abdulwahhab AH, Al-Sharydah AM, Al-Quorain A, Al-Muhanna AF, et al. Magnetic resonance and retrograde endoscopic cholangiopancreatography-based identification of biliary tree variants: are there type-related variabilities among the Saudi population? Surg Radiol Anat. (2019) 41(8):869–77. doi: 10.1007/s00276-019-02249-0
25. Tanaka T, Nakada T, Ito T, Kominami R, Sonomura T, Kagaya M, et al. Topographical relationship between the accessory hepatic duct and the hepatic artery system. Anat Sci Int. (2021) 96(1):112–8. doi: 10.1007/s12565-020-00568-6
Keywords: three-dimensional reconstruction, biliary tract anatomy, biliary tract disease, Hisense computer-assisted surgery system, China region
Citation: Li X, Duan R, He Y, Qin J, Liu R, Dai S, Zhou J, Zeng X, Duan J, Gao P, Yang X and Li C (2022) Application of three-dimensional visualization technology in the anatomical variations of hilar bile ducts in Chinese population. Front. Surg. 9:934183. doi: 10.3389/fsurg.2022.934183
Received: 6 May 2022; Accepted: 29 June 2022;
Published: 2 August 2022.
Edited by:
Orestis Ioannidis, Aristotle University of Thessaloniki, GreeceReviewed by:
Savvas Konstantinos Symeonidis, G. Papanikolaou General Hospital, GreeceNicolas Jarufe, Las Condes Clinic, Chile
Fei Peng Zhu, Nanjing Medical University, China
© 2022 Li, Duan, He, Qin, Liu, Dai, Zhou, Zeng, Duan, Gao, Yang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Peng Gao gp628@sohu.com Xiaoqiao Yang gd2hxhnj@163.com Cheng Li gd2hlicheng@163.com
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
 Xiaofeng Li1,†
Xiaofeng Li1,†  Ruijian Liu
Ruijian Liu