Abstract
Human cells assemble to form tissues, which organize into organs and then combine into complex organisms capable of extraordinary functions. However, we are not alone. It may surprise you to know that we humans are made of more than just human cells. In fact, there are many more microbes (microorganisms) in and on our bodies than there are human cells making up our tissues and organs. But before you get squirmy and itchy about this idea, these microorganisms are our allies—they are often helpful and sometimes even essential for our health. Though we often associate microbes like bacteria, viruses, and fungi with disease, most microbes are not dangerous. This article will explore how the human body develops and becomes colonized by these microbes in a mutually beneficial partnership.
Introduction
The microbes (microorganisms) that live in our bodies and on our skin are called the human microbiota. These microbes are not merely accidental tourists that come and go, nor do they necessarily cause diseases. Emerging research is revealing new and important functions that the human microbiota provides for us [1]. The microbes establish a symbiotic relationship and become an important part of the functions of the human body. This symbiosis has prompted some scientists to call the human body a “symbiogenic superorganism,” which refers to the complex interactions between humans and their microbiota [2]! This article will explore how the human body develops, how microbes colonize various body compartments, and how this colonization is beneficial for both the human body and the microbes.
Microbial Colonization of the Human
Each new human begins with the union of an egg and a sperm. Genes from the mother and the father combine, creating a new and unique genetic combination. During the 9 months of development in the womb, the cells of the fetus develop and organize into tissues; tissues assemble into organs; and the organs work together to create the human organism. With everything in place, the fetus is ready to be born.
Humans are born into a world of microbes, and these microbes become an important part of the human body. The vast majority of these microbes do not cause disease, and some are absolutely essential for life on earth. Recent research suggests that the fetus’s first encounter with microbes may occur in the womb [3]. This colonization continues during the birth process when microbes from the mother take up residence inside of and all over the infant [1]. Once in the outside world, the newborn is exposed to an even wider array of microbes. These microbes attach to the baby’s skin or enter the baby’s body along the mucous linings of the eyes, nose, and mouth. Human caregivers can pass on microbes as they hold, feed, kiss, touch, and interact with the child. As the baby begins reaching out and touching things, it is not long before the hands go to the mouth and microbes hitch a ride into the baby’s body. The various microbial species reach many different parts of the body and begin to establish a safe haven, where the microbes acquire nutrients, multiply and thrive.
Different types of microbes prefer different locations for colonization. Microbes that enter the mouth get swallowed and colonize various segments of the digestive system [3]. Importantly, microbes must find a hospitable place where they will be assured plenty of nutrients and, in exchange, these “good” microbes perform important functions that our own cells cannot. The human body and its microbial inhabitants strike a kind of bargain that is beneficial to both—a symbiosis. Research has revealed that the types of microbes found in the gut may change with age, and that factors such as diet, stress, and hormones can also influence the composition of the microbiota [4]. Scientists hypothesize that alterations in the microbiome may change bodily function and may predict health and disease. This is a new and exciting area of research, with many implications for the field of medicine [5].
So, what are some of the benefits of having microbes living in the human body? Next, we will discuss three examples.
Microbes Train and Assist the Immune System
The human immune system helps us to recognize microbes that do not belong in the body and might cause us harm. These dangerous organisms are called pathogens. The immune system is not fully functional at birth and there is a process early in life during which the cells of the immune system “learn” what belongs in the body and what does not. It is during this same time that the “good” microbes are colonizing different compartments in the body, like the gut for example, and the microbiota actually becomes part of the immune defense against infection [5]. The digestive tract is basically a long tube open at two ends and lined by cells called mucosal epithelial cells, which secrete a moist, protective mucous layer. Underneath this layer, clusters of immune cells assemble and monitor what passes through the digestive tract, looking for the “bad” microbes that cause disease. The “good” microbes that have established themselves become recognized as part of the body.
If pathogens enter the body through contaminated food or water, they could get across the mucous barrier of the digestive tract and enter the bloodstream. Once there, they could travel anywhere in the body. The “good” resident microbes compete with the pathogens for nutrients and space, which slows down the growth of pathogens, preventing them from crossing the mucosal barrier (Figure 1). Some of our microbiota even secrete toxins that kill pathogenic microbes. If the protection provided by the microbiota fails, the immune system can respond to the invasion of pathogens and kill them or inactivate their disease-causing processes. Thus, the gut microbiota establishes a symbiosis within the human digestive tract, helping to protect the human from disease.
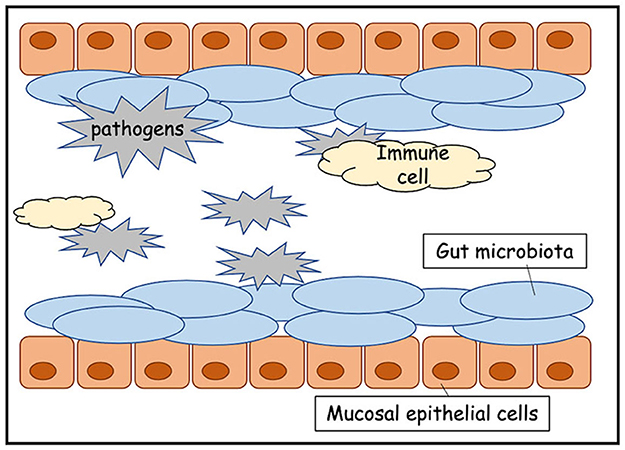
- Figure 1 - The insides of the intestines are lined with cells called mucosal epithelial cells, which produce a protective mucous layer.
- The gut microbiota helps to protect against pathogens, because the pathogens cannot compete with the gut microbes for space and nutrients. The gut microbiota protects the walls of the gut and those microbes are not attacked by cells of the immune system.
Microbes Help With the Digestion of Nutrients
The complex foods we eat are broken down into simple molecules that our cells can use to make energy. These simple molecules enter the bloodstream from the digestive tract through a process called absorption. Cells of the digestive tract secrete chemicals that breakdown food and then the cells absorb the nutrients that are produced. We eat some foods that our digestive system cannot breakdown. It is the microbes in the gut that help us digest those foods [6]. For example, cellulose, which is an essential component of plant cell walls, would be indigestible if not for our resident microbes. Cellulose is present in fruits and vegetables and is commonly referred to as fiber.
You may know that a healthy diet should contain fiber, which comes from various foods like grains, fruits, vegetables, beans, cereals, and nuts, to name a few. So, if human cells cannot breakdown fiber, why is it a recommended daily nutrient? Fiber is needed by our microbes! The gut microbiota digests fiber through a process called fermentation, to make energy for microbial cellular processes (Figure 2). Fermentation also produces simple molecules called short-chain fatty acids, which the mucosal epithelial cells that line the digestive tract use as a source of food.
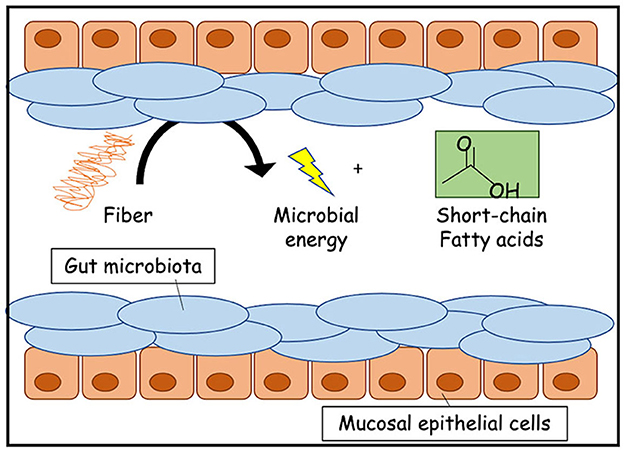
- Figure 2 - The gut microbiota helps us to digest dietary fiber.
- Through the fermentation process, fiber in our diets is converted into energy for the gut microbes and food (like short-chain fatty acids) for the cells of the digestive tract.
Microbes Communicate With the Brain
There is increasing evidence suggesting that the microbes in the human gut produce substances that have actions far beyond the digestive tract [7, 8]. So far, this has been studied mainly in laboratory animals, but if these actions also occur in humans, it may lead to a better understanding of what keeps people at a healthy weight [9]. Centers in the brain produce signals that we experience as hunger, which causes us to seek out food. When we have eaten enough for the body’s needs, there are signals that are sent from the gut to the brain that tell us we are full. The microbes in our gut may also be contributing signals that assist in regulating our food intake, the feeling of fullness, and body mass.
Gut microbes produce substances identical to chemicals used by the human nervous system to communicate with other cells [7]. Could the gut microbes affect the activity of the nervous system? Serotonin is one such chemical. It is produced by both brain cells and gut microbes. Serotonin helps to regulate our moods and is often used as a medication to treat certain diseases like depression. It is possible that microbially produced serotonin could activate the nervous system in the gut, which then communicates with the brain; or the serotonin produced by the gut microbiota might be absorbed and travel through the bloodstream to stimulate the brain. This microbe-derived substance could then contribute to mood and mental health (Figure 3) [7]. This could give a whole new meaning to having a “gut feeling” about something!
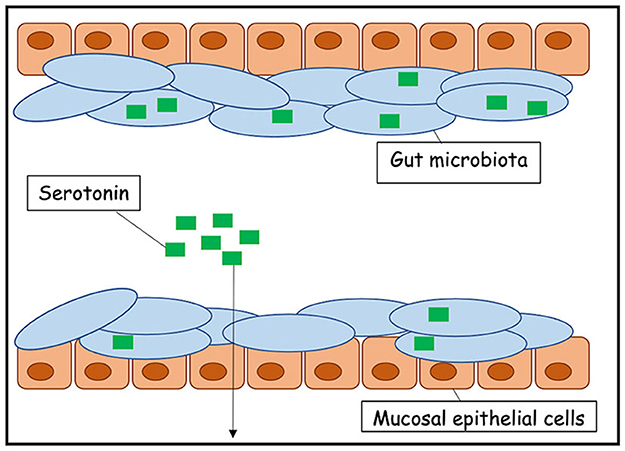
- Figure 3 - The gut microbiota can influence the activity of the brain.
- Gut microbes can produce serotonin, which is a chemical that can stimulate the brain to cause changes in mood and behavior.
Conclusion
Learning more about gut microbes and how to support their growth may help us think differently about how diseases arise and what therapies might restore health. In some cases, therapies may be used to promote a healthier relationship between humans and their resident microbes! The composition of the human microbiota differs across the human population depending on where people live, their diets, their occupations, and many other factors. There is much work ahead to identify healthy vs. disease-producing combinations of microbes, and to help us understand how to regulate that balance in favor of human health and wellness. Future studies focused on getting to know our microbial partners promise to produce some very exciting and beneficial partnerships!
Glossary
Microbes: ↑ Living organisms not visible to the human eye, also called microorganisms.
Microbiota: ↑ The various kinds of microbes that establish colonization in a particular region of the body, such as the gut or the skin.
Symbiosis: ↑ A relationship between two or more organisms that live together. This can have positive effect for both (mutualism); benefit one and harm the other (parasitism); or be neutral (commensalism).
Colonization: ↑ The growth of microbes in various regions of the body.
Pathogens: ↑ A microbe that causes disease.
Cellulose: ↑ A complex carbohydrate found in plant cell walls. It is in fruits and vegetables we eat but is indigestible in the human gut and commonly referred to as fiber.
Fermentation: ↑ A biochemical process that some cells use to make energy, ATP, when oxygen is not readily available.
Serotonin: ↑ One of the chemicals, neurotransmitters, used by neurons to communicate with other cells in the human nervous system.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Blaser, M. 2014. The microbiome revolution. J. Clin. Invest. 124:4162–5. doi: 10.1172/JCI78366
[2] ↑ Carrapiço, F. 2015. “Can we understand evolution without symbiogenesis?” in Reticulate Evolution. Interdisciplinary Evolution Research, Vol 3, eds N. Gontier (Cham: Springer). doi: 10.1007/978-3-319-16345-1_3
[3] ↑ Kundu, P., Blacher, E., Elinav, E., and Patterson, S. 2017. Our gut microbiome: the evolving inner self. Cell. 171:1481–93. doi: 10.1016/j.cell.2017.11.024
[4] ↑ Kim, S., and Jazwinski, S. M. 2018. The gut microbiota and healthy aging: a mini-review. Gerontology. 64:513–20. doi: 10.1159/000490615
[5] ↑ van de Gutche, M., Blottiere, H., and Dore, J. 2018. Humans as holobionts: implications for prevention and therapy. Microbiome. 6:81–7. doi: 10.1186/s40168-018-0466-8
[6] ↑ Makki, K., Deehan, E. C., Walter, J., and Bäckhed, F. 2018. The impact of dietary fiber on gut microbiota in host health and disease. Cell Host Microbe. 23:705–15. doi: 10.1016/j.chom.2018.05.012
[7] ↑ Cussotto, S., Sandhu, K., Dinan, T., and Cryan, J. 2018. The neuroendocrinology of the microbiota-gut-brain axis: a behavioral perspective. Front. Neuroendocrinol. 51:80–101. doi: 10.1016/j.yfrne.2018.04.002
[8] ↑ Collins, S., Surette, M., and Berick, P. 2012. The interplay between the intestinal microbiota and the brain. Nat. Rev. Microbiol. 10:735–42. doi: 10.1038/nrmicro2876
[9] ↑ O’Connor, A. 2021. How the Right Foods May Lead to a Healthier Gut and Better Health. New York, NY: New York Times.